- 1Clinical Futures: A Center of Emphasis within the CHOP Research Institute, Children’s Hospital of Philadelphia, Philadelphia, PA, United States
- 2Department of Pediatrics, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States
- 3Division of Hospital Medicine, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States
- 4Department of Pediatrics, College of Medicine, University of Cincinnati, Cincinnati, OH, United States
- 5Division of Medical Critical Care, Department of Pediatrics, Boston Children’s Hospital, Boston, MA, United States
- 6Department of Pediatrics, Harvard Medical School, Boston, MA, United States
- 7Department of Anesthesia and Perioperative Medicine, Medical University of South Carolina, Charleston, SC, United States
- 8Drexel University College of Medicine, Philadelphia, PA, United States
- 9Department of Pediatrics, St. Christopher’s Hospital for Children, Philadelphia, PA, United States
- 10James M. Anderson Center for Health Systems Excellence, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, United States
- 11Division of General Pediatrics, Department of Pediatrics, Boston Children's Hospital, Boston, MA, United States
- 12Division of Sleep and Circadian Disorders, Departments of Medicine and Neurology, Brigham and Women’s Hospital, Boston, MA, United States
- 13Department of Pediatrics, Department of Medicine, and Division of Sleep Medicine, Harvard Medical School, Boston, MA, United States
Communication underlies every stage of the diagnostic process. The Dialog Study aims to characterize the pediatric diagnostic journey, focusing on communication as a source of resilience, in order to ultimately develop and test the efficacy of a structured patient-centered communication intervention in improving outpatient diagnostic safety. In this manuscript, we will describe protocols, data collection instruments, methods, analytic approaches, and theoretical frameworks to be used in to characterize the patient journey in the Dialog Study. Our approach to characterization of the patient journey will attend to patient and structural factors, like race and racism, and language and language access, before developing interventions. Our mixed-methods approach is informed by the Systems Engineering Initiative for Patient Safety (SEIPS) 3.0 framework (which describes the sociotechnical system underpinning diagnoses within the broader context of multiple interactions with different care settings over time) and the Safety II framework (which seeks to understand successful and unsuccessful adaptations to ongoing changes in demand and capacity within the healthcare system). We will assess the validity of different methods to detect diagnostic errors along the diagnostic journey. In doing so, we will emphasize the importance of viewing the diagnostic process as the product of communications situated in systems-of-work that are constantly adapting to everyday challenges.
1 Introduction
Communication underlies every stage of the diagnostic process. As patients and families are present throughout the diagnostic process, effective communication with patients and families is both a definitional aspect of diagnostic excellence (1) and a pragmatic strategy for achieving it. Due to limitations of the current healthcare system, including fragmented outpatient care and limitations to access for patients who speak languages other than English, patients and families are often the ones communicating clinical information from one diagnostic encounter to another (2, 3). Research engaging families in safety reporting identified that families uncovered multiple diagnosis-related errors and adverse events, including delayed diagnoses of intussusception, aspiration pneumonia, and urosepsis (4, 5). The quality of bidirectional communication between patients, families/caregivers, and clinicians determines how diagnostic information is gathered, integrated into differential diagnoses, and communicated back to patients/caregivers, ultimately contributing to diagnostic outcomes. Yet, in spite of their important role in diagnostic communication, studies characterizing opportunities to improve diagnosis often lack the patient and family view (4, 6, 7).
In recognition of the critical shared role of patients, their families, and clinicians in diagnosis, the National Academy of Science, the National Quality Forum, the Institute for Healthcare Improvement, the US Center for Medicare & Medicaid Services, and the Children’s Hospital Association have all called for improved patient engagement in the diagnostic process (1, 6, 8, 9). Engaging patients more closely in diagnostic and safety research is respectful, ethical, and ensures safer care (10–12). Robust communication between patients, families/caregivers, and clinicians is more likely to generate resilience and safeguard against diagnostic failures and harm. Conversely, communication failures contribute to nearly half of malpractice claims, with more than half being provider-patient communication failures (13). In particular, there is ample opportunity to improve effective communication about diagnostic uncertainty (14–17).
Vulnerable populations, including families from racial/ethnic minority groups, those with lower incomes, and those who speak languages other than English disproportionately experience communication failures in health care (7, 18). Disparities have been characterized in the diagnosis of varying conditions including depression, appendicitis, acute myocardial infarction, and breast cancer (19–23). It is particularly important to understand how pediatric diagnostic processes differ for families who speak languages other than English. For example, patients with limited English proficiency are four times as likely to report having no qualified provider or interpreter who spoke their language, three times as likely to report incorrect or out of date medical records, and twice as likely to report not understanding the follow-up plan (24).
Effective communication is imperative and challenging in pediatrics, where different parents and/or other caregivers often hand off responsibility for clinic appointments or childcare. Often, children have a limited ability to convey symptoms, relying on multiple family caregivers. This is particularly true among children with complex or disabling conditions who average 6.5 (SD 6.5) outpatient visits annually, most to primary care (25). Most of these children (60%) will see a specialist at least once a year, 20% will visit the emergency room, and 10% will be admitted to the hospital (25, 26).
Diagnostic errors have been defined by the National Academy of Medicine as, “the failure to (a) establish an accurate and timely explanation of the patient’s health problem(s) or (b) communicate that explanation to the patients. This definition underscores this critical component that communication plays in avoiding delayed, missed, or wrong diagnoses. Opportunities to improve pediatric diagnosis, in terms of accuracy or communication, have not been well characterized (8). While an estimated 5% of adult primary care visits involve a diagnostic error (27), rates and characteristics of diagnostic errors are largely unquantified and undescribed in pediatric primary care. Research in specific disease conditions suggest that opportunities to improve pediatric diagnosis are common. Studies of hypertension or adolescent depression found that these diagnoses are missed 50% of the time in pediatric primary care (28). Up to 20% of children also have a delayed diagnosis of physical abuse (29–33). Diagnostic errors also occur with other common pediatric conditions, with misdiagnosis reported in 14% of asthma and 8% of appendicitis diagnoses (8). In a national study of pediatric health system leaders and parents, diagnostic safety was identified as a high priority topic for research (34). There is an urgent need to evaluate and develop interventions to improve diagnostic communication to prevent ongoing injury and death from diagnostic errors. This need is particularly urgent in primary care, where most of pediatric healthcare is delivered.
In this manuscript, we will describe the theoretical frameworks, protocols, data collection instruments, methods, and analytic approaches to be used in the Dialog Study. This study aims to characterize the pediatric diagnostic journey, focusing on communication as a source of resilience, in order to develop and adapt structured, patient-centered communication interventions for outpatient use, and to test the efficacy of such interventions in improving diagnostic safety. We will attend to patient and structural factors, like race and racism, and language and language access, before developing interventions.
2 Theoretical frameworks
Our mixed methods approach is grounded in the Systems Engineering Initiative for Patient Safety (SEIPS) 3.0 framework (35) which describes the sociotechnical system within the broader context of multiple clinical interactions that patients have in different care settings over time. We aimed to understand both the successful and unsuccessful adaptations to ongoing changes in demand and capacity within the healthcare system (36).
Recognizing that healthcare is “increasingly distributed over space and time,” Carayon et al. recently updated her widely used Systems Engineering Initiative for Patient Safety (SEIPS) framework, to characterize the patient journey in multiple care settings over time (35). Generally, the SEIPS framework allows for analysis of patient outcomes as a product of the interaction between structures (people, environment, tasks, tools) and processes (37, 38). Grounding the understanding of diagnostic safety as a longitudinal journey constructed by the dynamic interplay of sociotechnical elements will guide our observations, simulations, and analysis.
Our study investigates the diagnostic journey through both a traditional “error” perspective (Safety I) and approaches to avert errors and achieve diagnostic excellence (Safety II). Identifying both opportunities to improve diagnosis and drivers of diagnostic excellence is aligned with principles of “resilience engineering,” which posit that safety is a consequence of adapting to the changing conditions of systems function (39). In other words, harm occurs not because an otherwise stable system malfunctioned but rather because inappropriate adaptive actions were taken within an ever-changing, inherently error-prone environment. Thus, resilient systems can (1) respond (know what to do), (2) monitor (know what to look for), (3) learn from experience, and (4) anticipate (know what to expect) (40). We will assess the presence and interplay of these factors and the role of robust communication in their presence along the diagnostic journey.
SEIPS 3.0 and Safety II align to overcome limitations of approaches that seek improvement by rectifying piecemeal individual errors to instead explore how resilient people and systems deliver appropriate diagnoses and what systems barriers and facilitators shape these processes. It allows for the prospective identification of the everyday practices that contribute to effective diagnosis, rather than relying on retrospective assessment of failures. Informed by these frameworks, we will assess the validity of different methods to detect diagnostic errors along the diagnostic journey. In doing so, we will extend the idea that the diagnostic process is the product of communications situated in systems-of-work that are constantly adapting to everyday challenges.
3 Methods and analysis
3.1 Study design
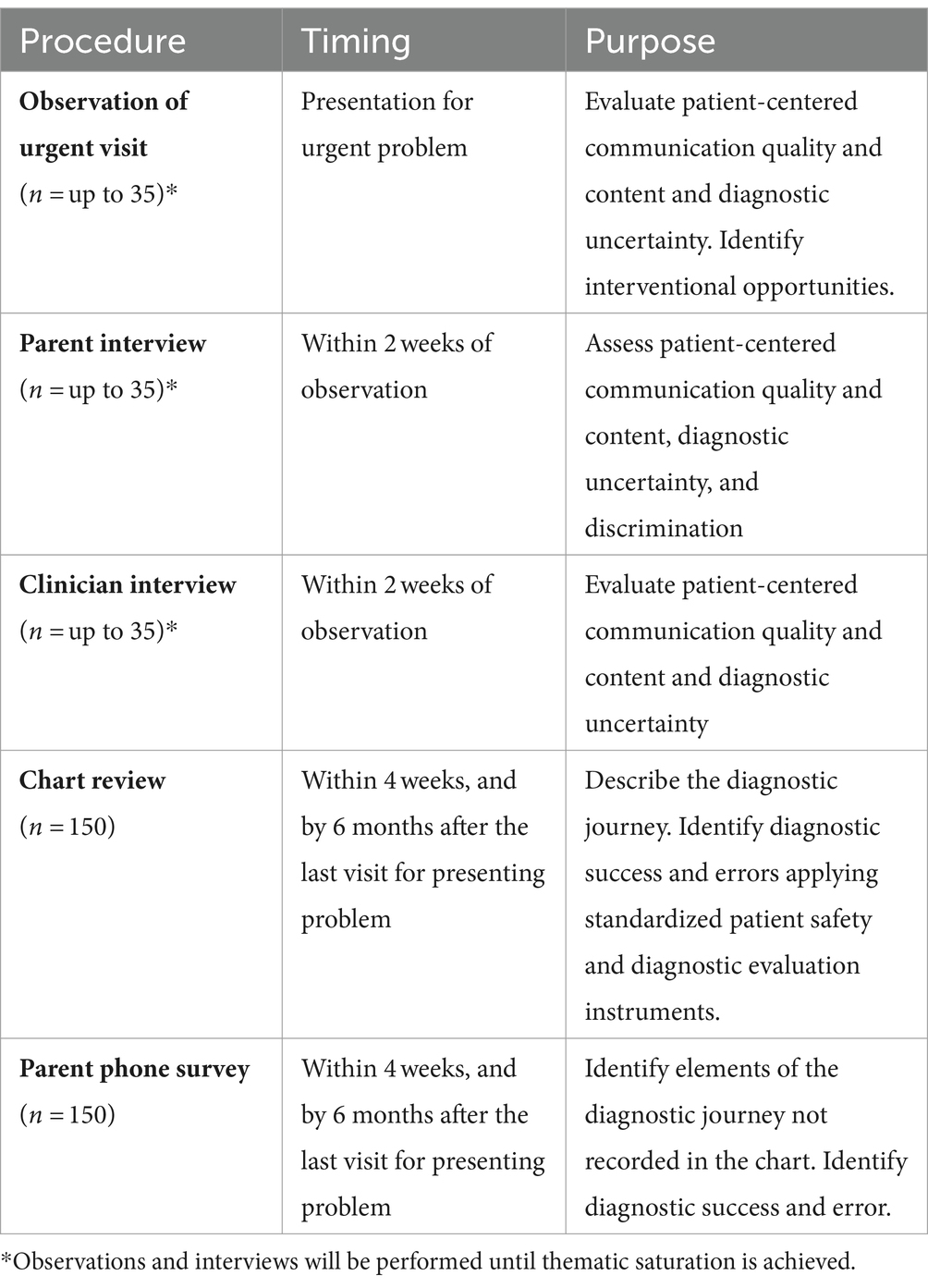
This is a prospective, mixed-methods, observational study aimed at characterizing opportunities to improve diagnosis and sources of systems resilience that drive diagnostic excellence for children with medical complexity presenting to primary care with acute concerns. We will adapt and test well-established patient safety research methods (including chart review, hospital incident reporting, family safety reporting, surveys, observations, and interviews) to characterize the diagnostic journey and associated successes and harms experienced by acutely ill children with multiple comorbid conditions and their families (Table 1). We will also apply reliable, valid, and novel ethnographic methods developed initially to understand the high rates of errors at home among outpatient children with chronic conditions (Table 1) (41). Ultimately (in subsequent phases of this initiative) findings will inform development and piloting of a communication-based intervention to improve diagnostic safety in this population.
A diagnostic journey as conceptualized in SEIPS 3.0 and the National Academies of Medicine starts at the first symptoms of a new problem at home leading to engagement with the healthcare system (1, 35). The healthcare team then engages in an iterative process of information gathering, information integration/interpretation, and formulation of a working diagnosis which is communicated to the patient and family and revisited as needed in response to treatment; success in this process determines outcomes for both the patient and system (1).
We will sample children followed at our primary care or complex care clinics (designed to care for patients with multi-specialty involvement, technology dependence, and/or neurologic impairment). Our preliminary chart review showed that diagnostic journeys for children with multiple chronic conditions lasted from one day to three weeks. We thus expect to capture the majority of diagnostic errors within six weeks of the initial presenting visit and will perform chart reviews and parent/caregiver phone surveys at that time. We will re-review all charts six months later to characterize the distribution of the duration of the diagnostic journey and assess the sensitivity of the six-week cutoff.
3.2 Setting
Data will be collected in five primary care and complex care ambulatory clinics associated with three children’s hospitals in the Northeast and Midwest. Clinic patient characteristics vary. Between 40 and 6% of patients identify as Hispanic, 45 to 27% of patients identify as Black, and 69 to 23% of patients identify as white. The majority of patients have public insurance (range across clinics 55 to 85%). Parental preference for a language other than English ranges from 20 to 8%.
3.3 Participant selection
We will recruit 150 patients age < 21 years with multiple chronic conditions (excluding mild asthma, eczema, allergies) presenting with irritability, vomiting, fever, abdominal pain, or other acute illness. We will review records of and conduct a brief phone survey (family safety reporting) with all participants. For the qualitative phase of the study, we will observe up to 35 of these patients’ clinic visits and invite parents/caregivers and a clinician from each observation to participate in interviews and additional, follow up phone surveys. To assure a comprehensive perspective on the diagnostic process, we will only include patients who receive primary care within our health systems. To understand differences in diagnostic processes by patient/family characteristics and parent/caregiver language, we will recruit patients with diverse racial and ethnic backgrounds and oversample patients with caregivers who prefer Spanish. Research assistants from diverse racial, ethnic, and language backgrounds will recruit outpatients by phone or in person. Participants will be compensated for interviews and observations. Consent will be obtained; assent will be obtained from the child where appropriate.
3.4 Methods
Chart reviews and brief phone surveys (150 patients) will be conducted to understand the longitudinal diagnostic journey, identify medical errors/harms, and characterize opportunities to improve diagnosis. Initial reviews will take place within 4 weeks of an acute care visit and will continue, with the goal of characterizing the diagnostic journey in its entirety, for up to 6 months. To further characterize the diagnostic journey, a trained research nurse will abstract the dates and locations of interactions with the health system, including in person, virtual, telephone, and portal message encounters. All pertinent communication and documentation regarding presenting, index-visit symptoms will be abstracted. We will detail “good catches” or “near misses” as sources of resilience. Charts will be reviewed for medical errors, associated harms, and harm severity (2, 42–47). In order to evaluate diagnosis, a structured EHR review tool [Revised SaferDx (48, 49)] will be applied to each case by two clinicians who will determine whether there were missed opportunities to improve diagnosis. Missed opportunities will be further classified using the modified DEER taxonomy to identify the phase of the diagnostic process involved (50). To maximize reliability, reviewers will receive didactic training practice on identical charts (45, 46). We will assess inter-reviewer reliability and discordant reviews will be adjudicated by a third, consensus reviewer.
In light of the inherent limitations of retrospective chart review, we will also conduct brief phone surveys with patients/families to identify aspects of the diagnostic journey not otherwise captured in the medical record including parent/caregiver perceptions of diagnostic excellence, error, communication, and systems resilience. Parent/caregiver phone surveys are routinely used in outpatient safety research to identify care processes and potential errors not recorded in the chart (51, 52). We developed a ten-minute, 15-item phone survey, adapting from previously developed tools to capture family safety reporting in the hospital (4, 5, 53, 54) The survey examines points along the diagnostic journey, including successes, failures, and errors at each point. Surveys will occur within 4 weeks, and by 6 months after the last known point of contact with the health care system for the diagnostic journey (e.g., last outpatient visit, last outpatient follow up after hospitalization, or hospital discharge).
Observations. A subset of up to 35 patients will be recruited to participate in ethnographic observations. Observations will aim to characterize variation in diagnosis-focused communication across the diagnostic process (1) including during the phases of information gathering, information interpretation and integration, and formulation/communication of the working diagnosis (and diagnostic uncertainty, if present). A trained research assistant will be physically present in the exam room, directly observe, and audio-record the patient’s entire clinic visit. The Hawthorne effect will be mitigated by having ethnographers shadow providers right before recruitment starts to increase clinic staff’s familiarity with the research team, training ethnographers to be inobtrusive, and triangulating data from observations with other data collected from interviews and chart review. We will utilize an iteratively-developed observational guide developed based on conceptual models of patient/family identity, clinician-patient communication and health outcomes (55), Safety II/resilience engineering (56), and the SEIPS 3.0 framework (35) (Figure 1). Portions of audio-recorded observations will be transcribed at a later date, if needed to understand communication content. Diagnostic successes and errors will be identified within and across SEIPS work system domains (37) and used to model the system and identify resilience (36).

Figure 1. Integrated conceptual model of the ways patient/caregiver identity, clinician-patient communication health outcomes, resilience engineering, and the systems engineering for patient safety framework intersect and should be evaluated during the diagnostic process.
Semi-structured interviews of parents/caregivers and clinicians who participate in observations will be performed by a trained interviewer in person or by phone, within 2 weeks of observation. The goal of these interviews is to reflect on interactions and processes during the observed clinic visit in order to obtain a deep understanding of how communication affects the diagnostic processes in light of patient and family characteristics, circumstances, and values. Interviews will explore parent/caregiver experiences in accessing care, perceived discrimination, and patient-centered communication (“When did the doctors listen to you?” “not listen?”) throughout the diagnostic process, from history taking to formulation of working diagnosis. Interviews may also ask about adaptive clinician approaches, and variation in parent/caregiver “speaking up.” The semi-structured interview guides were developed using the same frameworks as for the observation guide and will be pilot-tested with diverse participants and edited as needed for clarity. Interviews will be conducted by trained bilingual interviewers, audio-recorded, and transcribed by a HIPAA-compliant transcription and translation service. Surveys, administered concurrent to the interviews, will inform interpretation of qualitative data. Parents/caregivers will compete a 3-item health literacy survey (57). Clinicians participating in ethnography will complete the Team Dynamics survey (58).
3.5 Analysis of chart reviews
Descriptive statistics will be used to summarize demographics and aspects of diagnostic journeys, including duration (in days), number and types of contacts within healthcare, number of people, and clinics involved. Rates of medical and diagnostic errors will be estimated. Patient-days will be determined by calculating the number of days between first point of contact with the health system and the most-definitive diagnosis and treatment. Rates will be calculated per patient and per 1,000 patient-days. Tabulation of SaferDx (49) and DEER taxonomy (50) results will be used to ascertain rates and types of diagnostic successes and errors. In addition to establishing a baseline incidence of opportunities to improve diagnosis in this primary care cohort, our analysis will identify areas of vulnerability in the diagnostic process and elucidate the relationship between medical errors, diagnostic errors, and outpatient harm. In conjunction with qualitative analysis, our findings will focus and direct interventional efforts targeting opportunities identified in the evaluation of existing diagnostic processes.
Because of the small sample size, we will perform stratified analyses by site only and will not create adjusted models. Given the size of this study and the expected rate of diagnostic errors, we do not expect to quantitatively identify differences in rates of diagnostic errors by parent/caregiver preferred language, insurance status, or self-reported cultural, religious, gender, disabilities, or racial/ethnic identities. However, we do expect to note qualitative differences in diagnostic processes, which will inform future observational and interventional studies. Demographics of participants will be compared with those of eligible non-participants who declined or whom we were unable to consent for participation in order to evaluate for potential selection bias.
3.6 Qualitative analysis of observations and semi-structured interviews
Qualitative analysis will occur in tandem with ongoing observations and interviews to ensure fidelity to the guides, appropriate observation and interviewing techniques, and to enable detection of data saturation (the point at which no new major codes/themes emerge). Analyses will proceed through the development of mixed deductive/inductive codes and coding using the constant comparative method, culminating in overall thematic analysis of the coded data (59). We will develop deductive codes drawing on the literature and conceptual models of patient/family identity clinician-patient communication (55), Safety II (56), and the SEIPS 3.0 framework (35) used to generate the observation guide (Supplemental). Qualitative coding will be performed using Dedoose software (Version 9.0.17, SocioCultural Research Consultants, LLC, Los Angeles, CA, 2021) by assigning deductive (from a priori codebook) and inductive codes (from emergent themes) to text segments, grouping related codes, and iteratively revising the coding structure as new codes emerge. Group coding will be performed for qualitative data from the first 2–3 patients, revising the codebook as needed. Thereafter, qualitative data from each patient will be coded independently by two coders, resolving discrepancies at scheduled consensus meetings. We will develop definitions for diagnostic success and errors and use inductive thematic analysis to ascertain systems factors that appear to be contributing to the events. Directed content analysis will be used to identify the ways in which patients, families, and clinicians communicate along the diagnostic journey within and between systems of care. We will note successes, sources of resiliency, errors, and barriers or facilitators of the diagnostic process. We will compare processes and themes along major sub-groups. We will also characterize the diagnostic system, processes, and resilience at each site, comparing the similarities and differences, and thus identifying common themes and specific features.
Our ethnographic and chart review data will inform the development of process maps showing the entire diagnostic journey for children with multiple chronic conditions at each site and across sites, as well as process maps for families using Spanish for care. In our prior studies, such process maps have been pivotal in identifying points for intervention. Moreover, analysis of communication, patient/family-reported opportunities to improve diagnosis, and identification of the sources of resilience that can facilitate diagnostic excellence will focus intervention design on key aspects of diagnostic process.
4 Ethics and dissemination
Findings resulting from the described protocol will provide a basis for the development of interventions and methods to be used broadly in evaluating and improving the provision of diagnostic excellence in pediatric primary care. This study poses minimal risk to participants and has been approved by the single Institutional Review Board at Boston Children’s Hospital upon which the other sites are reliant. Consent and assent will be obtained as described above. In the unlikely event that we identify a serious diagnostic error in evolution or adverse event in evolution, we will address these directly with the clinical team, including the attending physician. The clinical team would follow their usual clinical procedure, including following institution-specific guidelines for error reporting.
5 Discussion
Our methods and outcomes are novel and represent an effort to evaluate and improve diagnostic communication longitudinally across time and care settings. Findings will help hone our understanding of the relationships between pediatric patients with medical complexity and clinicians, the ways patient/caregiver racial, ethnic, and linguistic identities intersect with communication and diagnostic outcomes, and the aspects of care that enable diagnostic excellence. With ethnography we will be able to evaluate systems resilience and when diagnostic communication processes “go well,” using a Safety II lens. In doing so, we will extend the idea that the diagnostic process is the product of communications situated in systems-of-work that are constantly adapting to the everyday challenges. Both ethnographic and chart review methods are meant to test and refine tools for identifying opportunities to improve diagnosis (Safety I). More broadly, we will assess the validity of different methods to detect diagnostic errors along the diagnostic journey. An outcome of this work will be evaluation and reflection on our methodology for detecting systems resilience, for detecting opportunities to improve diagnosis in primary care, for achieving across-site concordance in identifying opportunities to improve diagnosis, and for leveraging interdisciplinary expertise to evaluate cases. Our approach will allow us to learn about the diagnostic process for these vulnerable patients in primary care, but also extend and refine methods to be used to evaluate diagnostic performance and equity.
Ethics statement
The studies involving humans have been approved by the Single Institutional Review Board at Boston Children’s Hospital. The studies will be conducted in accordance with the local legislation and institutional requirements. The participants' guardians/next of kin will provide their written informed consent to participate prior to the commencement of the study and assent will be obtained from the child where appropriate.
Author contributions
IR: Conceptualization, Funding acquisition, Writing – original draft. TM: Funding acquisition, Methodology, Writing – review & editing. CC: Funding acquisition, Methodology, Writing – review & editing. KC: Methodology, Writing – review & editing. NK: Conceptualization, Writing – review & editing. PB: Funding acquisition, Methodology, Writing – review & editing. KM: Writing – review & editing, Methodology, Funding acquisition. AK: Funding acquisition, Methodology, Writing – review & editing. AC: Writing – review & editing, Funding acquisition, Methodology. EL: Writing – review & editing, Funding acquisition, Methodology. CL: Funding acquisition, Methodology, Writing – review & editing. KW: Funding acquisition, Methodology, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This project was funded as a Center for Diagnostic Excellence to Re-Engineering Patient and Family Communication to Improve Diagnostic Safety Resilience (R18HS029346–01) by the Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services (HHS). KM is supported by AHRQ T32 HS 000063. AK efforts were supported by R01HS028930.
Acknowledgments
We acknowledge with appreciation the efforts of the entire study team in conceptualizing and actualizing this work. Ursula Nawab, Christopher P. Bonafide, and Canita Brent, were involved in conceptualization of this protocol. Brenda Rosario Perez, Kimberly Asitimbay, and Samira Ahmed are indispensable research coordinators engaged in implementation of this protocol.
Conflict of interest
Kuzma is a consultant for the I-PASS Patient Safety Institute. The I-PASS Patient Safety Institute is a company that seeks to train institutions in best handoff practices and aid in their implementation. Landrigan has consulted with and holds equity in the I-PASS Institute, which seeks to train institutions in best handoff practices and aid in their implementation. In addition, Landrigan has received monetary awards, honoraria, and travel reimbursement from multiple academic and professional organizations for teaching and consulting on sleep deprivation, physician performance, handoffs, and safety, and has served as an expert witness in cases regarding patient safety and sleep deprivation. Walsh has served as a consultant for Sanofi and Research Triangle Institute.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Balogh, E, Miller, BT, and Ball, JInstitute of Medicine (U.S.). Committee on Diagnostic Error in Health Care; Board on Health Care Services; Institute of Medicine; The National Academies of Sciences, Engineering, and Medicine. In: Balogh EP, Miller BT, Ball JR, editors. Improving Diagnosis in Health Care. Washington (DC): National Academies Press (US) (2015).
2. Stille, CJ, McLaughlin, TJ, Primack, WA, Mazor, KM, and Wasserman, RC. Determinants and impact of generalist–specialist communication about pediatric outpatient referrals. Pediatrics. (2006) 118:1341–9. doi: 10.1542/peds.2005-3010
3. Stille, CJ, Primack, WA, McLaughlin, TJ, and Wasserman, RC. Parents as information intermediaries between primary care and specialty physicians. Pediatrics. (2007) 120:1238–46. doi: 10.1542/peds.2007-1112
4. Khan, A, Coffey, M, Litterer, KP, Baird, JD, Furtak, SL, Garcia, BM, et al. Families as partners in hospital error and adverse event surveillance. JAMA Pediatr. (2017) 171:372–81. doi: 10.1001/jamapediatrics.2016.4812
5. Khan, A, Furtak, SL, Melvin, P, Rogers, JE, Schuster, MA, and Landrigan, CP. Parent-reported errors and adverse events in hospitalized children. JAMA Pediatr. (2016) 170:e154608. doi: 10.1001/jamapediatrics.2015.4608
6. Bell, SK, Bourgeois, F, DesRoches, CM, Dong, J, Harcourt, K, Liu, SK, et al. Filling a gap in safety metrics: development of a patient-centred framework to identify and categorise patient-reported breakdowns related to the diagnostic process in ambulatory care. BMJ Qual Saf. (2022) 31:526–40. doi: 10.1136/bmjqs-2021-013672
7. Suurmond, J, Uiters, E, De Bruijne, MC, Stronks, K, and Essink-Bot, ML. Explaining ethnic disparities in patient safety: a qualitative analysis. Am J Public Health. (2010) 100:S113–7. doi: 10.2105/AJPH.2009.167064
8. Marshall, TL, Rinke, ML, Olson, APJ, and Brady, PW. Diagnostic error in pediatrics: a narrative review. Pediatrics. (2022) 149:e2020045948D. doi: 10.1542/peds.2020-045948D
10. Rees, P, Wimberg, J, and Walsh, KE. Patient and family partnership for safer health care. Pediatrics. (2018) 142:e20172847. doi: 10.1542/peds.2017-2847
11. Turakhia, P, and Combs, B. Using principles of co-production to improve patient care and enhance value. AMA J Ethics. (2017) 19:1125–31. doi: 10.1001/journalofethics.2017.19.11.pfor1-1711
12. Batalden, M, Batalden, P, Margolis, P, Seid, M, Armstrong, G, Opipari-Arrigan, L, et al. Coproduction of healthcare service. BMJ Qual Saf. (2016) 25:509–17. doi: 10.1136/bmjqs-2015-004315
13. Humphrey, KE, Sundberg, M, Milliren, CE, Graham, DA, and Landrigan, CP. Frequency and nature of communication and handoff failures in medical malpractice claims. J Patient Saf. (2022) 18:130–7. doi: 10.1097/PTS.0000000000000937
14. Gordon, GH, Joos, SK, and Byrne, J. Physician expressions of uncertainty during patient encounters. Patient Educ Couns. (2000) 40:59–65. doi: 10.1016/s0738-3991(99)00069-5
15. Wray, CM, and Loo, LK. The diagnosis, prognosis, and treatment of medical uncertainty. J Grad Med Educ. (2015) 7:523–7. doi: 10.4300/JGME-D-14-00638.1
16. Simpkin, AL, and Schwartzstein, RM. Tolerating uncertainty — the next medical revolution? N Engl J Med. (2016) 375:1713–5. doi: 10.1056/NEJMp1606402
17. Meyer, AND, Giardina, TD, Khanna, A, Bhise, V, Singhal, GR, Street, RL Jr, et al. Pediatric clinician perspectives on communicating diagnostic uncertainty. Int J Qual Health Care. (2019) 31:G107–12. doi: 10.1093/intqhc/mzz061
18. Okoroh, JS, Uribe, EF, and Weingart, S. Racial and ethnic disparities in patient safety. J Patient Saf. (2017) 13:153–61. doi: 10.1097/PTS.0000000000000133
19. Lukachko, A, and Olfson, M. Race and the clinical diagnosis of depression in new primary care patients. Gen Hosp Psychiatry. (2012) 34:98–100. doi: 10.1016/j.genhosppsych.2011.09.008
20. Goyal, MK, Chamberlain, JM, Webb, M, Grundmeier, RW, Johnson, TJ, Lorch, SA, et al. Racial and ethnic disparities in the delayed diagnosis of appendicitis among children. Acad Emerg Med. (2021) 28:949–56. doi: 10.1111/acem.14142
21. Moy, E, Barrett, M, Coffey, R, Hines, AL, and Newman-Toker, DE. Missed diagnoses of acute myocardial infarction in the emergency department: variation by patient and facility characteristics. Diagnosi. (2015) 2:29–40. doi: 10.1515/dx-2014-0053
22. Schulman, KA, Berlin, JA, Harless, W, Kerner, JF, Sistrunk, S, Gersh, BJ, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. (1999) 340:618–26. doi: 10.1056/NEJM199902253400806
23. Miller-Kleinhenz, JM, Collin, LJ, Seidel, R, Reddy, A, Nash, R, Switchenko, JM, et al. Racial disparities in diagnostic delay among women with breast cancer. J Am Coll Radiol. (2021) 18:1384–93. doi: 10.1016/j.jacr.2021.06.019
24. Bell, SK, Dong, J, Ngo, L, McGaffigan, P, Thomas, EJ, and Bourgeois, F. Diagnostic error experiences of patients and families with limited English-language health literacy or disadvantaged socioeconomic position in a cross-sectional US population-based survey. BMJ Qual Saf. (2023). 32:644–54. doi: 10.1136/bmjqs-2021-013937
25. Chien, AT, Toomey, SL, Kuo, DZ, van Cleave, J, Houtrow, AJ, Okumura, MJ, et al. Care quality and spending among commercially insured children with disabilities. Acad Pediatr. (2019) 19:291–9. doi: 10.1016/j.acap.2018.06.004
26. Chien, AT, Kuhlthau, KA, Toomey, SL, Quinn, JA, Okumura, MJ, Kuo, DZ, et al. Quality of primary care for children with disabilities enrolled in medicaid. Acad Pediatr. (2017) 17:443–9. doi: 10.1016/j.acap.2016.10.015
27. Singh, H, Giardina, TD, Meyer, AND, Forjuoh, SN, Reis, MD, and Thomas, EJ. Types and origins of diagnostic errors in primary care settings. JAMA Intern Med. (2013) 173:418–25. doi: 10.1001/jamainternmed.2013.2777
28. Rinke, ML, Singh, H, Heo, M, Adelman, JS, O'Donnell, HC, Choi, SJ, et al. Diagnostic errors in primary care pediatrics: project RedDE. Acad Pediatr. (2018) 18:220–7. doi: 10.1016/j.acap.2017.08.005
29. Jenny, C, Hymel, KP, Ritzen, A, Reinert, SE, and Hay, TC. Analysis of missed cases of abusive head trauma. JAMA. (1999) 281:621–6. doi: 10.1001/jama.281.7.621
30. Berger, RP, and Lindberg, DM. Early recognition of physical abuse: bridging the gap between knowledge and practice. J Pediatr. (2019) 204:16–23. doi: 10.1016/j.jpeds.2018.07.081
31. Letson, MM, Cooper, JN, Deans, KJ, Scribano, PV, Makoroff, KL, Feldman, KW, et al. Prior opportunities to identify abuse in children with abusive head trauma. Child Abuse Negl. (2016) 60:36–45. doi: 10.1016/j.chiabu.2016.09.001
32. Sheets, LK, Leach, ME, Koszewski, IJ, Lessmeier, AM, Nugent, M, and Simpson, P. Sentinel injuries in infants evaluated for child physical abuse. Pediatrics. (2013) 131:701–7. doi: 10.1542/peds.2012-2780
33. Thackeray, J, Minneci, PC, Cooper, JN, Groner, JI, and Deans, KJ. Predictors of increasing injury severity across suspected recurrent episodes of non-accidental trauma: a retrospective cohort study. BMC Pediatr. (2016) 16:8. doi: 10.1186/s12887-016-0540-y
34. Hoffman, JM, Keeling, NJ, Forrest, CB, Tubbs-Cooley, HL, Moore, E, Oehler, E, et al. Priorities for pediatric patient safety research. Pediatrics. (2019) 143:e20180496. doi: 10.1542/peds.2018-0496
35. Carayon, P, Wooldridge, A, Hoonakker, P, Hundt, AS, and Kelly, MM. SEIPS 3.0: human-centered design of the patient journey for patient safety. Appl Ergon. (2020) 84:103033. doi: 10.1016/j.apergo.2019.103033
36. Hollnagel, E, Wears, R, and Braithwaite, J. From safety-I to safety-II: a White paper. Australia: Published simultaneously by the University of Southern Denmark, University of Florida, USA, and Macquarie University. Resilient Health Care Net (2015).
37. Carayon, P, Schoofs Hundt, A, Karsh, B, Gurses, AP, Alvarado, CJ, Smith, M, et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care. (2006) 15:i50–8. doi: 10.1136/qshc.2005.015842
38. Holden, RJ, Carayon, P, Gurses, AP, Hoonakker, P, Hundt, AS, Ozok, AA, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. (2013) 56:1669–86. doi: 10.1080/00140139.2013.838643
39. Pariès, J, and Wreathall, J In: E Hollnagel, J Pariès, D Woods, and J Wreathall, editors. Resilience engineering in practice: A guidebook. 1st ed. London: CRC Press (2017)
40. Verhagen, MJ, de Vos, MS, Sujan, M, and Hamming, JF. The problem with making safety-II work in healthcare. BMJ Qual Saf. (2022) 31:402–8. doi: 10.1136/bmjqs-2021-014396
41. Walsh, KE, Stille, CJ, Mazor, KM, and Gurwitz, JH. Using home visits to understand medication errors in children In: K Henriksen, JB Battles, MA Keyes, and ML Grady, editors. Advances in patient safety: New directions and alternative approaches (Vol. 4: Technology and medication safety). Rockville, MD: Advances in Patient Safety. Agency for Healthcare Research and Quality (US) (2008)
42. Cifra, CL, Jones, KL, Ascenzi, JA, Bhalala, US, Bembea, MM, Newman-Toker, DE, et al. Diagnostic errors in a PICU: insights from the morbidity and mortality conference. Pediatr Crit Care Med. (2015) 16:468–76. doi: 10.1097/PCC.0000000000000398
43. Cifra, CL, Custer, JW, Singh, H, and Fackler, JC. Diagnostic errors in pediatric critical care: a systematic review. Pediatr Crit Care Med. (2021) 22:701–12. doi: 10.1097/PCC.0000000000002735
44. Walsh, KE, Roblin, DW, Weingart, SN, Houlahan, KE, Degar, B, Billett, A, et al. Medication errors in the home: a multisite study of children with cancer. Pediatrics. (2013) 131:e1405–14. doi: 10.1542/peds.2012-2434
45. Walsh, KE, Dodd, KS, Seetharaman, K, Roblin, DW, Herrinton, LJ, von Worley, A, et al. Medication errors among adults and children with cancer in the outpatient setting. J Clin Oncol. (2009) 27:891–6. doi: 10.1200/JCO.2008.18.6072
46. Landrigan, CP, Parry, GJ, Bones, CB, Hackbarth, AD, Goldmann, DA, and Sharek, PJ. Temporal trends in rates of patient harm resulting from medical care. N Engl J Med. (2010) 363:2124–34. doi: 10.1056/NEJMsa1004404
47. Bates, DW. Incidence of adverse drug events and potential adverse drug events: implications for prevention. JAMA. (1995) 274:29. doi: 10.1001/jama.1995.03530010043033
48. al-Mutairi, A, Meyer, AND, Thomas, EJ, Etchegaray, JM, Roy, KM, Davalos, MC, et al. Accuracy of the safer dx instrument to identify diagnostic errors in primary care. J Gen Intern Med. (2016) 31:602–8. doi: 10.1007/s11606-016-3601-x
49. Singh, H, Khanna, A, Spitzmueller, C, and Meyer, AND. Recommendations for using the revised safer dx instrument to help measure and improve diagnostic safety. Diagnosi. (2019) 6:315–23. doi: 10.1515/dx-2019-0012
50. Schiff, GD, Kim, S, Abrams, R, Cosby, K, Lambert, B, Elstein, AS, et al. Diagnosing diagnosis errors: lessons from a multi-institutional collaborative project In: K Henriksen, JB Battles, ES Marks, and DI Lewin, editors. Advances in patient safety: From research to implementation (volume 2: Concepts and methodology) : Advances in Patient Safety. Agency for Healthcare Research and Quality (US) (2005).
51. Kaushal, R, Goldmann, DA, Keohane, CA, Christino, M, Honour, M, Hale, AS, et al. Adverse drug events in pediatric outpatients. Ambul Pediatr. (2007) 7:383–9. doi: 10.1016/j.ambp.2007.05.005
52. Gandhi, TK, Weingart, SN, Borus, J, Seger, AC, Peterson, J, Burdick, E, et al. Adverse drug events in ambulatory care. N Engl J Med. (2003) 348:1556–64. doi: 10.1056/NEJMsa020703
53. Huth, K, Hotz, A, Emara, N, Robertson, B, Leaversuch, M, Mercer, AN, et al. Reduced postdischarge incidents after implementation of a hospital-to-home transition intervention for children with medical complexity. J Patient Saf. (2023) 19:493–500. doi: 10.1097/PTS.0000000000001155
54. Mercer, AN, Mauskar, S, Baird, J, Berry, J, Chieco, D, Copp, K, et al. Family safety reporting in hospitalized children with medical complexity. Pediatrics. (2022) 150:e2021055098. doi: 10.1542/peds.2021-055098
55. Street, RL, Makoul, G, Arora, NK, and Epstein, RM. How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient Educ Couns. (2009) 74:295–301. doi: 10.1016/j.pec.2008.11.015
56. Anderson, JE, Ross, AJ, Back, J, Duncan, M, Snell, P, Hopper, A, et al. Beyond ‘find and fix’: improving quality and safety through resilient healthcare systems. Int J Qual Health Care. (2020) 32:204–11. doi: 10.1093/intqhc/mzaa007
57. Chew, LD, Bradley, KA, and Boyko, EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. (2004) 36:588–94.
58. Song, H, Chien, AT, Fisher, J, Martin, J, Peters, AS, Hacker, K, et al. Development and validation of the primary care team dynamics survey. Health Serv Res. (2015) 50:897–921. doi: 10.1111/1475-6773.12257
Keywords: diagnosis, diagnostic process, patient safety, safety II, pediatrics, communication, primary care, ambulatory care
Citation: Rasooly IR, Marshall TL, Cifra CL, Catchpole K, Kuzma NC, Brady PW, Melton K, Khan A, Chien AT, Lipstein EA, Landrigan CP and Walsh KE (2024) Developing methods to identify resilience and improve communication about diagnosis in pediatric primary care. Front. Med. 11:1414892. doi: 10.3389/fmed.2024.1414892
Edited by:
Kenneth A. Mundt, University of Massachusetts Amherst, United StatesReviewed by:
Mark Graber, Stony Brook University, United StatesJeffrey A Gold, Oregon Health and Science University, United States
Copyright © 2024 Rasooly, Marshall, Cifra, Catchpole, Kuzma, Brady, Melton, Khan, Chien, Lipstein, Landrigan and Walsh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Irit R. Rasooly, cmFzb29seWlAY2hvcC5lZHU=
 Irit R. Rasooly
Irit R. Rasooly Trisha L. Marshall3,4
Trisha L. Marshall3,4 Christina L. Cifra
Christina L. Cifra Ken Catchpole
Ken Catchpole Nicholas C. Kuzma
Nicholas C. Kuzma Kathleen E. Walsh
Kathleen E. Walsh