- 1Shengli Clinical Medical College of Fujian Medical University, Fuzhou, China
- 2The School of Nursing, Fujian Medical University, Fuzhou, China
- 3Fujian Provincial Hospital, Fuzhou, China
- 4Fujian Medical University 2nd Affiliated Hospital, Quanzhou, China
Aim: In this study, we aimed to evaluate oral health strategies in rheumatoid arthritis (RA) patients with periodontitis.
Methods: We enrolled 110 RA patients with periodontitis who were diagnosed in a Grade A tertiary hospital into an oral health strategies program. The control and test groups comprised 55 cases each. The management effect was evaluated by self-care ability, oral health-related quality of life, RA-related clinical indicators, and the DAS28 score. The control group received routine nursing, whereas the test group was in a self-health management program for 3 months.
Results: After the intervention, compared to the control group, the test group showed better self-care ability, oral health-related quality of life score, RA-related clinical indicators, and DAS28 score (P < 0.05).
Conclusion: Our oral health strategies program slowed down the progression of the disease and can be popularized in patients.
1 Introduction
Rheumatoid arthritis (RA), a common autoimmune disease (1), is characterized by chronic aggressive arthritis (2) and a high disability rate (3). If it is not treated as per the standardized protocols, it can eventually lead to joint deformity and loss of function (4). Its pathophysiology and disease control are closely related to oral microbial infection. The prevalence of periodontitis is higher in patients with RA than in the normal population (5), and the presentation of the disease is more severe as well (6). Periodontitis is a chronic, infectious periodontal disease wherein microorganisms on the surface of the tooth (mainly gram-negative anaerobic bacteria) destroy periodontal support tissues and gradually form periodontal pockets, which in turn cause loss of clinical attachment and alveolar bone resorption (7). Both RA and periodontitis can destroy surrounding soft tissue and bone structure (8), and studies have shown that the pathogenesis of RA and periodontitis is similar, with both affecting each other (9–11). Their pathogenesis is also related in many ways, such as epidemiology, loci, the bacteria involved, and immune and inflammatory factors (12, 13). Periodontitis is a risk factor for RA, and inflammation in RA can be significantly alleviated by effective treatment of periodontitis, which is aimed at controlling bacterial plaque and reducing periodontal pathogens (14). Periodontal treatment is beneficial for the control of clinical symptoms of RA and the reduction of laboratory indicators (15). Oral care intervention is an important part of standardized periodontal basic treatment of patients with RA (16). It is an important way to keep the mouth clean and control plaque and an important means to prevent the occurrence and slow down the development of periodontitis (17), which directly translates into a better oral health of patients (18). However, traditional oral care for patients with RA has many shortcomings. These patients may have limited movement of their hands and joints due to the illness, preventing them from maintaining proper oral hygiene (19). This results in a large accumulation of oral plaque and increases the risk of periodontitis. Consequently, patients are likely to develop and exhibit negative emotions like helplessness, irritability, and anxiety due to periodontal discomfort, and physical and psychological discomfort leads to reduced food and water intake (20).
Green tea contains tea polyphenols, which have antibacterial, anti-inflammatory, and anti-oxidative properties, among other biological activities. They can inhibit the growth of various bacteria. Therefore, green tea-based oral care strategies may help improve oral health and control disease in RA patients. It is recommended that RA patients undergo regular oral examinations and care to maintain a clean and healthy mouth. In addition, drinking green tea may also help relieve RA symptoms. This study aims to explore the use of green tea oral care solutions for oral cleaning, to guide patients on proper oral care practices and oral health maintenance, and to slow down the progression of RA disease activity.
2 Materials and methods
2.1 Design and randomization
Random number series were generated using EXCEL by clinical epidemiologists who were not involved in this study. Random numbers ranging from 1 to 110 were put into sealed, light-tight envelopes and kept safe. The person who performed this randomization was not familiar with this subject. After enrolling the patients into the study, a random sequence was generated using a table of random numbers. The numbers were ordered from small to large; those numbered 1–55 were assigned to the intervention group, and those numbered 56–110 were assigned to the control group. Each of the random numbers was assigned using non-transparent sealed envelopes. Individuals responsible for sample collection and data analysis were blinded to group assignment.
This study was approved by the Ethics Committee of Fujian Provincial Hospital (ethics approval number: K2020-08-006). It was performed in strict adherence with moral principles and with a rigorous scientific research attitude. It followed the principle of “voluntariness, confidentiality, and harmlessness” and ensured all patients' willingness to participate in this study.
2.2 Participants selection
This study enrolled RA patients with periodontitis who were hospitalized in the Department of Rheumatology and Immunology of Fujian Provincial Hospital between December 2019 and December 2020. Only those who met the following inclusion and exclusion criteria were selected. The inclusion criteria were as follows: (1) patients who were diagnosed as having RA by a rheumatologist and an immunologist according to the RA diagnostic criteria of ACR/EULAR in 2010 (21) in a tertiary A hospital and who were also diagnosed as having periodontitis as per the criteria for periodontitis detailed in “Periodontology” published in 2012 (22); (2) patients who agreed to receive an oral periodontal examination and could cooperate with completing the questionnaire survey and providing written informed consent; (3) patients with no fewer than two functional teeth in at least one 1/6 quadrant; (4) patients who could complete the examination on time and appear for timely follow-up visits to cooperate with this study; and (5) patients aged 18–75 years old. The exclusion criteria were as follows: (1) patients having other inflammatory diseases or systemic diseases (e.g., Sjogren's syndrome, systemic lupus erythematosus, and allergic purpura); (2) pregnant and lactating women, patients with disabilities, and patients with diabetes, cardiovascular disease, liver cirrhosis, or mental illness;(3) patients having had periodontal treatment within the last 3 months; and (4) edentulous patients.
2.3 Sample size calculation
According to the results of Chen et al. (23), it was estimated that each group needed 38 participants, and assuming a dropout rate of 20%, we concluded that the sample size needed was 46 participants per group. Therefore, 55 participants were recruited in each of the two groups (experimental and control groups).
2.4 Interventions
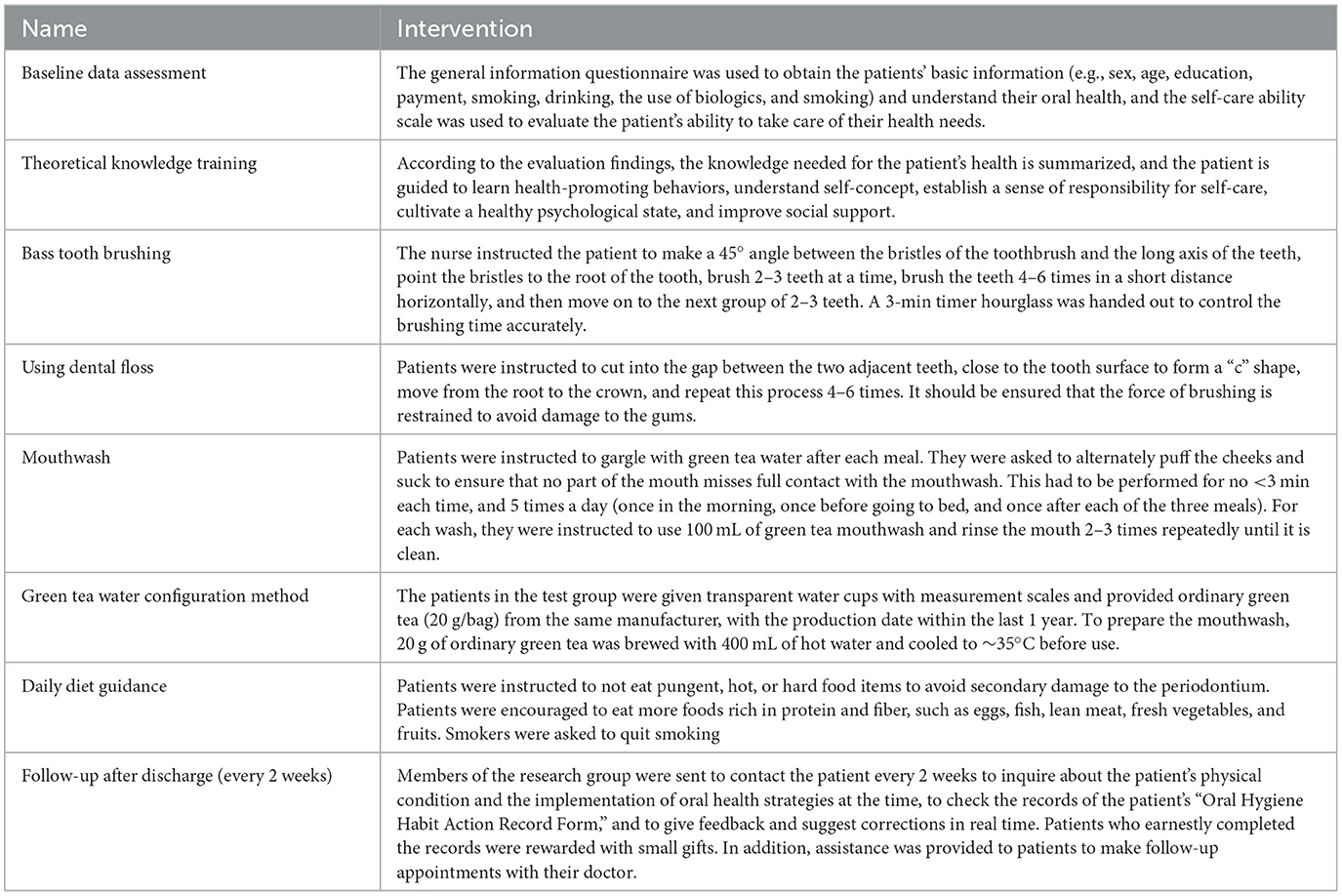
The control group received routine nursing, including admission education, disease-related knowledge introduction, medication guidance, and discharge education. The intervention received by the test group patients was oral health strategies, which included the following: (1) Baseline data collection was performed on the first day of admission with “one-on-one” on-site guidance. (2) Theoretical knowledge training was given on the third day of admission (training duration: 20–30 min), which was administered in the form of individual missionary education, group education, and group discussions. (3) Training was given on oral care skills on the 4th day of admission (training duration: 40–45 min), and in this training, an oral skills operation video was shown to the patients using a projector. The investigators then combined the oral model to demonstrate the basics of the Bass brushing teeth technique, the use of dental floss sticks, and the use of the right green tea mouthwash. Patients were encouraged to give feedback on the spot and were sent the oral skill operation video course package over WeChat so they could rewatch it if they wanted. (4) Daily dietary guidance training was held on the morning of the fifth day after admission (training duration: 10–20 min), and it was administered as on-site guidance, individual missionary education, and group education. Finally, (5) timely follow-up visits were conducted after discharge. Specific intervention measures are listed in Table 1.
2.5 Evaluation index
The evaluation index included general information and the findings on the Self-Care Competence Scale (ESCA) (24), Oral Health Impact Profile (the Oral Health Impact Profile, OHIP-14) (25), and DAS28 Scoring Form (26). For data collection, the paper questionnaire was used to collect data when the patients were admitted to the hospital and 3 months after the intervention. Oral health-related examinations were recorded by professionally trained periodontists before and 3 months after the intervention.
2.6 Statistical methods
EpiData version 3.1 (EpiData Software, Odense, Denmark) was used for data entry with the double-entry principle and to check for consistency. If any data inconsistencies were found, the original questionnaire responses were checked for confirmation in time. The data were statistically analyzed using IBM SPSS 25.0. Enumeration data were described by frequency and percentage and analyzed by the X2 test or Fisher's exact probability method. The measurement data were normally distributed, and the homogeneity of variance was described by mean ± standard deviation (χ ± s). Within-group comparisons were performed using the paired t-test, and the between-group comparisons were performed using two independent samples t-test; the measurement data were non-normally distributed. The measurement data were non-normally distributed and described as the median (25% quantile to 75% quantile). Nonparametric tests were used, with the Wilcoxon rank sum test used for intra-group comparisons and the Mann–Whitney U-test used for inter-group comparisons.
2.7 Safety
Throughout the study, no adverse events or deaths occurred in either group.
2.8 Sample loss instructions
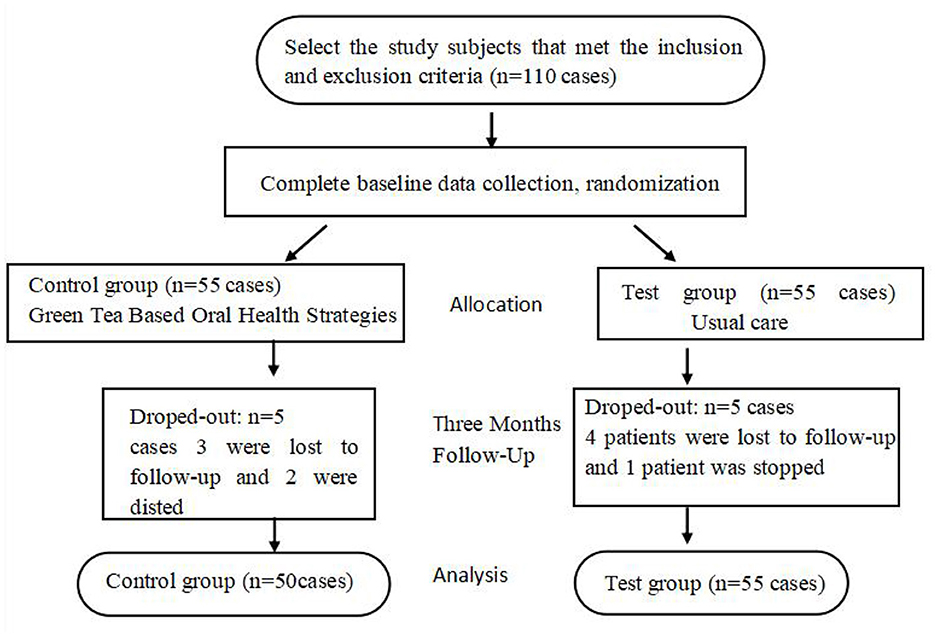
In test group four patients were lost to follow-up, and one patient was suspended due to change in disease condition; in control group three patients were lost to follow-up, and two patients were suspended due to change in disease condition. Finally, 100 study subjects completed all the data collection, as shown in Figure 1.
3 Results
In this study, 110 patients were included, including 55 patients in the experimental group and 55 patients in the control group.
In the experimental group, four patients were lost to follow-up, and one patient's enrollment was canceled due to the change of condition. In the control group, three patients were lost to follow-up, and two patients' enrollment was canceled due to the change of condition. Finally, 100 patients provided all the required data, with 50 patients in each group.
3.1 Comparison of the general data of the two patient groups
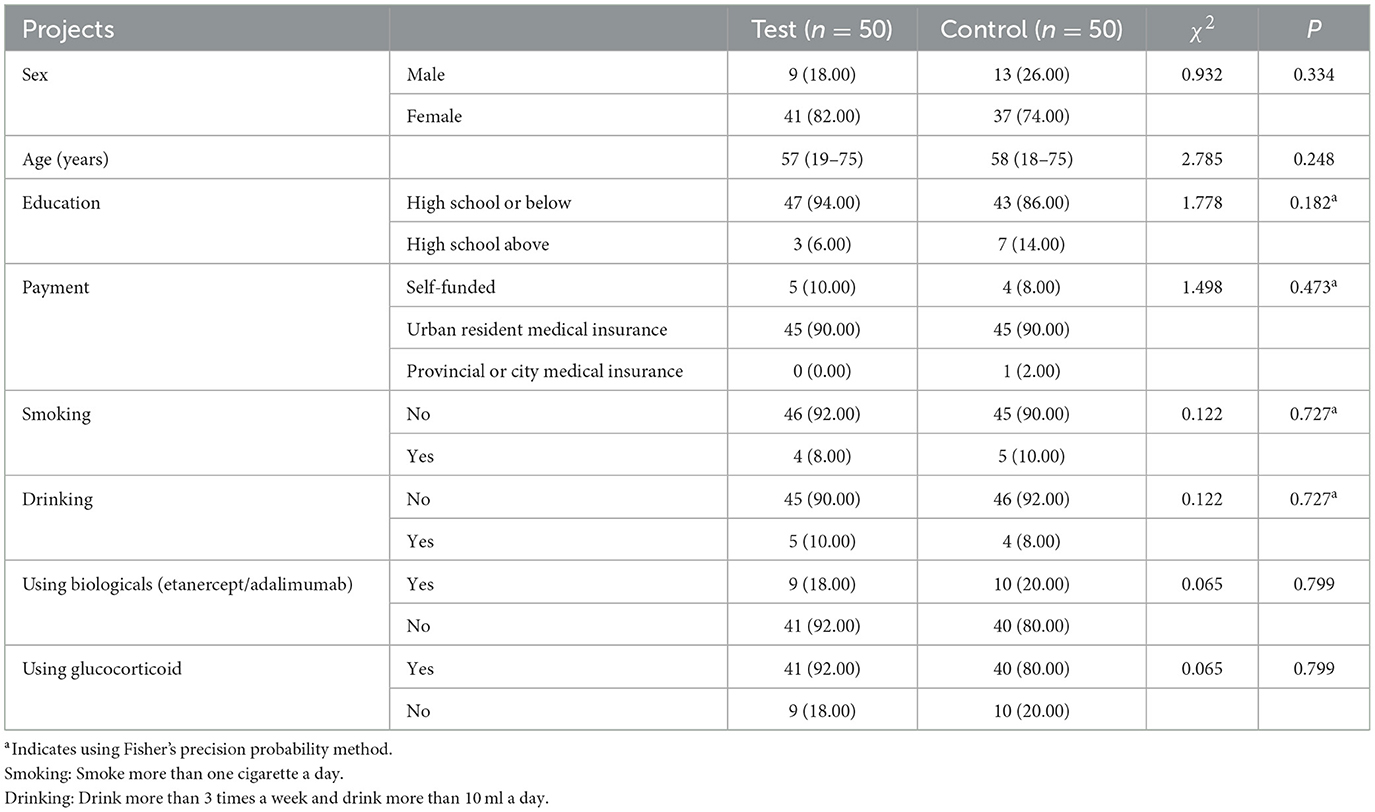
The general data of the two patient groups were comparable with no significant difference (P > 0.05; Table 2).
3.2 The outcome indicators of the two patient groups before and after the intervention
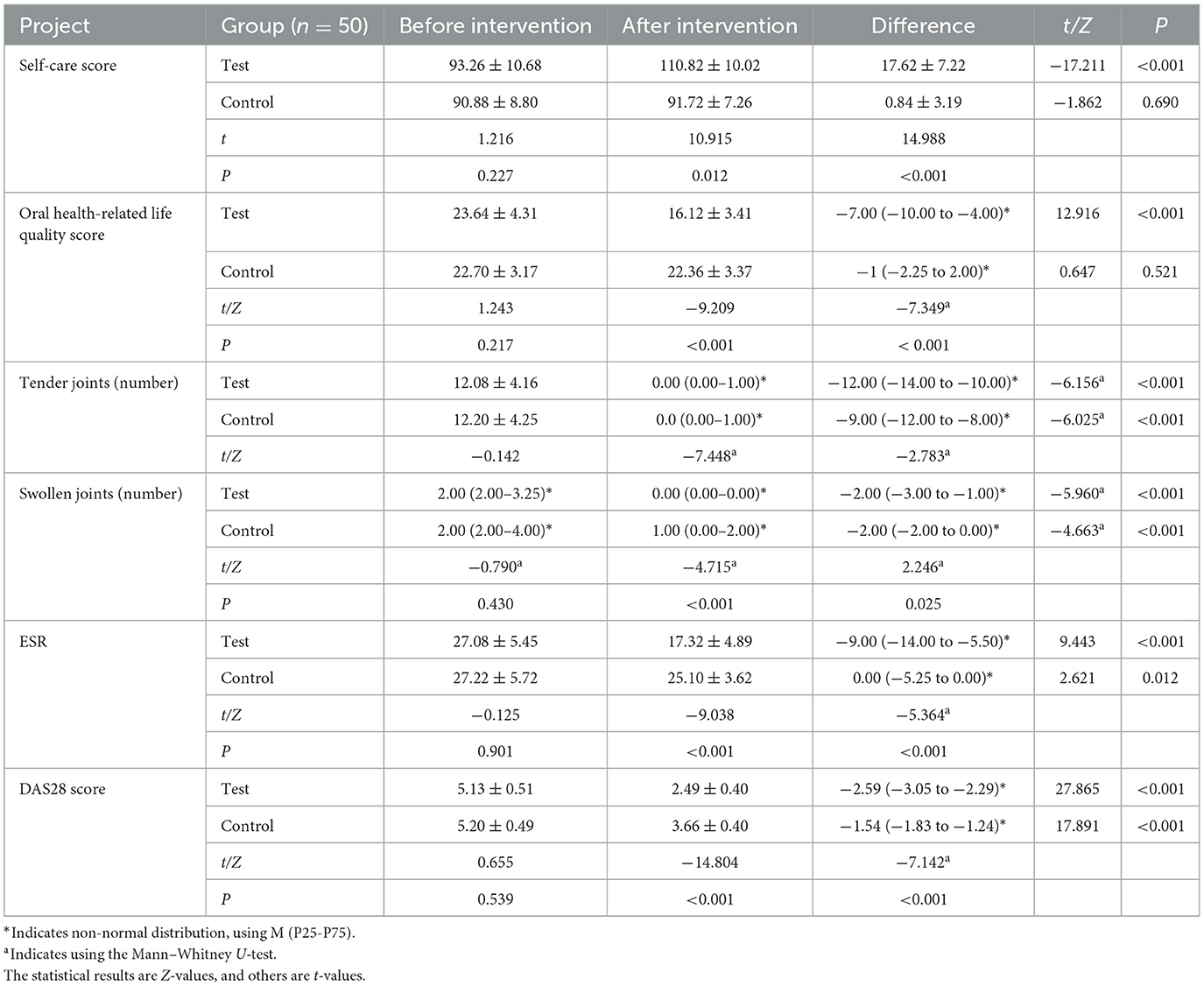
After the intervention, patients' self-care ability, oral health-related quality of life, RA-related clinical indicators, DAS28 score, and other indicators were significantly higher in the test group than in the control group (P < 0.05; Table 3).
4 Discussion
4.1 Oral health strategies is beneficial to improve the self-care ability of RA patients with periodontitis
Self-care ability is the ability to achieve self-care through purposeful learning (27), which can promote and maintain the development of individual physical and mental health (28). Joint dysfunction and the consequently decreased self-care ability in patients with RA likely affect their oral hygiene behavior (29), and the use of immunosuppressants and hormones increases their vulnerability to developing oral microbial infections, resulting in cumulative damage to oral health status. The prognosis of patients with RA is closely associated with their self-care behavior (30).
This study revealed improved self-care ability of patients in the test group after the intervention, upholding the ability of the training program to improve their self-care ability. After training, the patients in the test group became more self-dependent, showed better mental states, and could master more comprehensive systematic oral self-care skills and knowledge. This empowered them to actively participate in the whole process of disease diagnosis, treatment, nursing, and rehabilitation, and this active participation translated into better self-care ability, early body recovery, shorter hospitalization time, and early return to normal daily life.
4.2 Oral health strategies is positive to improve the periodontal health status and oral health-related quality of life in patients with RA and periodontitis
The pathogenesis of periodontitis is complex, and the course of treatment is long, making effective oral care absolutely essential (31). However, in the passive oral cleaning process, nurses traditionally use cotton balls to wipe the patient's mouth. This requires the patients to keep their mouth open for a long time, making them prone to muscle fatigue and often causing nausea, retching, and other types of discomfort. Furthermore, as the passive cotton ball wiping method lacks a mouthwash step, oral bacteria tend to remain lodged in the corners of the mouth, which greatly shortens the duration of fresh breath, thus often leading to bad mental states, such as low self-esteem and emotional tension, in patients.
In this study, after 3 months of intervention and follow-up, RA patients with periodontitis showed significantly improved periodontal health status, which is also attributable to the program conforming to the patients' daily work and rest habits. Furthermore, the training also enhanced patients' awareness of the disease prevention and treatment, thus increasing their understanding of periodontitis-related risk factors, promoting the development of scientific oral hygiene habits, and improving the efficacy of their oral cleaning process. Upon admission, a periodontal specialist performed thorough oral cleaning, descaling, and plaque removal. Good oral care skills, such as correct way of using the tooth brush, rational use of dental floss, and green tea mouthwash can effectively maintain the dental health of patients with RA, and this is conducive to repairing damaged periodontal tissue and effectively preventing disease recurrence. The tea polyphenols in the green tea mouthwash used in this study could effectively inhibit the growth of bacteria and reduce dentin sensitivity (32), and they are used as an adjunctive treatment for chronic inflammatory diseases (33).
Oral health is reflective of an individual's health status and quality of life to a certain extent (34). Notably, the effects and consequences of periodontal disease may not be limited to the oral cavity. There is an association between periodontal disease and RA (35). In a previous study, participants were more willing to receive oral health education from a rheumatologist or dentist (36). In patient-centered dental care, it is important to recognize the physical effects of oral diseases and the psychosocial barriers that develop because of disease-related parameters (37). In patients with RA, regular oral examinations are reportedly needed to improve periodontal health (38). The present study showed that the oral health-related quality of life of patients in the test group was markedly improved. Our program combines patients' self-care needs and self-care ability, thus improving upon the traditional oral care model and allowing patients to take control of their oral health. After implementing the oral health strategies, the patients were encouraged to improve their self-responsibility and oral hygiene status, thus reducing oral infections and improving their oral comfort and quality of life.
4.3 Oral health strategies is favorrable to control oral disease in RA patients' activity
RA and periodontitis can cause continuous pathological bone resorption and harm health (39). Previous oral ulcers were reported in 30% of the patients (40). Controlling local periodontal infection and inflammation can reduce the systemic inflammatory response, which in turn helps improve the activity of patients with RA (41). The key to ensuring proper oral care and managing RA is maintaining awareness about them (42). In this study, we used the DAS28 score, which is the clinically relevant index of RA. It is a comprehensive evaluation index of long-term clinical attention and has been widely used to measure the activity of patients with RA.
In the test group, RA-related clinical indicators and DAS28 scores were significantly lower after the intervention than they were before the intervention (P < 0.05). The patients in the control group received conventional drug treatment for the disease, and even in these patients, the clinical indicators of the disease improved compared with before the treatment. Between-group comparisons showed that the differences in RA-related clinical indicators and the DAS28 score before and after the intervention were significantly greater in the test group than in the control group (P < 0.05), indicating that intervention measures can improve patients' RA-related clinical indicators, thus reducing patients activity, which is consistent with a previous study (43).
The final sample size collected in this study (50 cases in test group and control group) was small. To improve the reliability of the study results, further studies with larger sample sizes are needed. In this study, only inpatients from the rheumatism immunology department of a tertiary hospital were selected. The feasibility and scientific nature of the results in different regions need to be further verified. The intervention time of this study is 3 months, and future studies should implement a longer intervention time to improve the reliability of their study results. Tea mouthwash cannot replace periodontal treatment and should be used only as an adjunctive tool to enhance its results.
5 Conclusion
Green Tea Based Oral Health Strategies for RA patients with periodontitis is beneficial to improve the oral self-care ability of these patients; furthermore, it is optimistic to improve their oral health-related quality of life, periodontal health indicators, and activity levels. This study provides a reference basis for clinical oral care interventions for RA patients with periodontitis and adds new information for clinical medical staff to conduct oral health strategies.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Fujian Provincial Hospital Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
SL: Data curation, Funding acquisition, Investigation, Writing – original draft. SJ: Conceptualization, Formal analysis, Project administration, Writing – review & editing. RL: Data curation, Project administration, Supervision, Validation, Writing – review & editing. BC: Formal analysis, Resources, Supervision, Validation, Writing – review & editing. FG: Writing – review & editing. SZ: Writing – review & editing. LC: Investigation, Methodology, Project administration, Resources, Writing – review & editing. HL: Data curation, Formal analysis, Project administration, Resources, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Joint Funds for the Innovation of Science and Technology, Fujian province of China (2023Y9317), and the Natural Science Foundation of the Fujian Province of China (2022J01403).
Acknowledgments
We thank the research team and the participants for their cooperation and great commitment to this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ACR, American College of Rheumatology; BOP, Bleeding On Probing; CAL, Clinical Attachment Loss; CEJ, Cemento-enamel Junction; DAS28, Disease Activity Score in 28 Joints; ESCA, Exercise of Self-care Agency; ESR, Erythrocyte Sedimentation Rate; EULAR, European League Against Rheumatism; OHIP, Oral Health Impact Profile.
References
1. Zlatkovic-Svenda M, Rouse M, Radak-Perovic M, Stojanovic R, Vujasinovic-Stupar N, Lazovic-Popovic B, et al. Adaptation and validation of the Rheumatoid Arthritis Quality of Life (RAQoL) questionnaire for use in Serbia. Rheumatol Int. (2017) 37:641–6. doi: 10.1007/s00296-016-3586-0
2. Huang J, Fu X, Chen X, Li Z, Huang Y, Liang C. Promising therapeutic targets for treatment of rheumatoid arthritis. Front Immunol. (2021) 12:686155. doi: 10.3389/fimmu.2021.686155
3. Smolen JS, Aletaha D, Barton A, Burmester GR, Emery P, Firestein GS, et al. Rheumatoid arthritis. Nat Rev Dis Primers. (2018) 4:18001. doi: 10.1038/nrdp.2018.1
4. Larice S, Ghiggia A, Di Tella M, Romeo A, Gasparetto E, Fusaro E, et al. Pain appraisal and quality of life in 108 outpatients with rheumatoid arthritis. Scand J Psychol. (2020) 61:271–80. doi: 10.1111/sjop.12592
5. Wen S, Beltrán V, Chaparro A, Espinoza F, Riedemann JP. Association between chronic periodontitis and rheumatoid arthritis. A systematic review. Rev Med Chil. (2019) 147:762–75. doi: 10.4067/S0034-98872019000600762
6. Wolff B, Berger T, Frese C, Max R, Blank N, Lorenz HM, et al. Oral status in patients with early rheumatoid arthritis: a prospective, case-control study. Rheumatology. (2014) 53:526–31. doi: 10.1093/rheumatology/ket362
7. Nakayama K. Porphyromonas gingivalis and related bacteria: from colonial pigmentation to the type IX secretion system and gliding motility. J Periodontal Res. (2015) 50:1–8. doi: 10.1111/jre.12255
8. Zhang J, Xu C, Gao L, Zhang D, Li C, Liu J. Influence of anti-rheumatic agents on the periodontal condition of patients with rheumatoid arthritis and periodontitis: a systematic review and meta-analysis. J Periodontal Res. (2021) 56:1099–115. doi: 10.1111/jre.12925
9. Leech MT, Bartold PM. The association between rheumatoid arthritis and periodontitis. Best Pract Res Clin Rheumatol. (2015) 29:189–201. doi: 10.1016/j.berh.2015.03.001
10. Zaatout N. Presence of non-oral bacteria in the oral cavity. Arch Microbiol. (2021) 203:2747–60. doi: 10.1007/s00203-021-02300-y
11. Kurgan S, Fentoglu Ö, Önder C, Serdar M, Eser F, Tatakis DN, et al. The effects of periodontal therapy on gingival crevicular fluid matrix metalloproteinase-8, interleukin-6 and prostaglandin E2 levels in patients with rheumatoid arthritis. J Periodontal Res. (2016) 51:586–95. doi: 10.1111/jre.12337
12. de Molon RS, Rossa C Jr, Thurlings RM, Cirelli JA, Koenders MI. Linkage of periodontitis and rheumatoid arthritis: current evidence and potential biological interactions. Int J Mol Sci. (2019) 20:4541. doi: 10.3390/ijms20184541
13. Hussain SB, Botelho J, Machado V, Zehra SA, Mendes JJ, Ciurtin C, et al. Is there a bidirectional association between rheumatoid arthritis and periodontitis? A systematic review and meta-analysis. Semin Arthritis Rheum. (2020) 50:414–22. doi: 10.1016/j.semarthrit.2020.01.009
14. Zini A, Mazor S, Timm H, Barker ML, Grender JM, Gerlach RW, et al. Effects of an oral hygiene regimen on progression of gingivitis/early periodontitis: a randomized controlled trial. Can J Dent Hyg. (2021) 55:85–94.
15. Yang N-Y, Wang C-Y, Chyuan I-T, Wu K-J, Tu Y-K, Chang C-W, et al. Significant association of rheumatoid arthritis-related inflammatory markers with non-surgical periodontal therapy. J Formos Med Assoc. (2018) 117:1003–10. doi: 10.1016/j.jfma.2017.11.006
16. Juan CY, Hsu CW, Lu MC. Increased dental visits in patients with rheumatoid arthritis: a secondary cohort analysis of population based claims data. BMC Oral Health. (2022) 22:609. doi: 10.1186/s12903-022-02661-w
17. Worthington HV, MacDonald L, Poklepovic Pericic T, Sambunjak D, Johnson TM, Imai P, et al. Home use of interdental cleaning devices, in addition to toothbrushing, for preventing and controlling periodontal diseases and dental caries. Cochr Database Syst Rev. (2019) 4:Cd012018. doi: 10.1002/14651858.CD012018.pub2
18. Niesten D. Oral health care and oral health-related quality of life of frail and care-dependent older people. Ned Tijdschr Tandheelkd. (2017) 124:589–92. doi: 10.5177/ntvt.2017.11.17168
19. Monsarrat P, Vergnes J-N, Cantagrel A, Algans N, Cousty S, Kémoun P, et al. Effect of periodontal treatment on the clinical parameters of patients with rheumatoid arthritis: study protocol of the randomized, controlled ESPERA trial. Trials. (2013) 14:253. doi: 10.1186/1745-6215-14-253
20. Rogers AA, Willumsen T, Strømme H, Johnsen JK. Top-down self-regulation processes as determinants of oral hygiene self-care behaviour: a systematic scoping review. Clin Exp Dent Res. (2022) 8:807–26. doi: 10.1002/cre2.548
21. Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO III, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. (2010) 69:1580–8.
23. Chen L, Cao H, Wu X, Xu X, Ji X, Wang B, et al. Effects of oral health intervention strategies on cognition and microbiota alterations in patients with mild Alzheimer's disease: a randomized controlled trial. Geriatr Nurs. (2022) 48:103–10. doi: 10.1016/j.gerinurse.2022.09.005
24. Kearney BY, Fleischer BJ. Development of an instrument to measure exercise of self-care agency. Res Nurs Health. (1979) 2:25–34. doi: 10.1002/nur.4770020105
25. Guo L, Söderhamn U, McCallum J, Ding X, Gao H, Guo Q, et al. Testing and comparing two self-care-related instruments among older Chinese adults. PLoS ONE. (2017) 12:e0182792. doi: 10.1371/journal.pone.0182792
26. van Riel PL, Renskers L. The Disease Activity Score (DAS) and the Disease Activity Score using 28 joint counts (DAS28) in the management of rheumatoid arthritis. Clin Exp Rheumatol. (2016) 34(5 Suppl. 101):S40–4.
27. Xu X, Han J, Li Y, Sun X, Lin P, Chen Y, et al. Effects of orem's self-care model on the life quality of elderly patients with hip fractures. Pain Res Manag. (2020) 2020:5602683. doi: 10.1155/2020/5602683
28. Patra C. Patient care, self-care. AMA J Ethics. (2021) 23:E428–429. doi: 10.1001/amajethics.2021.428
29. Minnock P, McKee G, Kelly A, Carter SC, Menzies V, O'Sullivan D, et al. Nursing sensitive outcomes in patients with rheumatoid arthritis: a systematic literature review. Int J Nurs Stud. (2018) 77:115–29. doi: 10.1016/j.ijnurstu.2017.09.005
30. Zuidema R, van Dulmen S, Nijhuis-van der Sanden M, Meek I, van den Ende C, Fransen J, et al. Efficacy of a web-based self-management enhancing program for patients with rheumatoid arthritis: explorative randomized controlled trial. J Med Internet Res. (2019) 21:e12463. doi: 10.2196/12463
31. Kapila YL. Oral health's inextricable connection to systemic health: special populations bring to bear multimodal relationships and factors connecting periodontal disease to systemic diseases and conditions. Periodontol 2000. (2021) 87:11–6. doi: 10.1111/prd.12398
32. Melok AL, Lee LH, Mohamed Yussof SA, Chu T. Green tea polyphenol epigallocatechin-3-gallate-stearate inhibits the growth of Streptococcus mutans: a promising new approach in caries prevention. Dent J. (2018) 6:38. doi: 10.3390/dj6030038
33. Lippert A, Renner B. Herb-drug interaction in inflammatory diseases: review of phytomedicine and herbal supplements. J Clin Med. (2022) 11:1567. doi: 10.3390/jcm11061567
34. Schmalz G, Noack S, Patschan S, Patschan D, Müller GA, Rupprecht A, et al. Disease activity, morning stiffness and missing teeth are associated with oral health-related quality of life in individuals with rheumatoid arthritis. Clin Oral Investig. (2020) 24:3559–66. doi: 10.1007/s00784-020-03226-3
35. Falcao A, Bullón P. A review of the influence of periodontal treatment in systemic diseases. Periodontol 2000. (2019) 79:117–28. doi: 10.1111/prd.12249
36. Protudjer JLP, Billedeau C, Hurst K, Schroth R, Stavropoulou C, Kelekis-Cholakis A, et al. Oral health in rheumatoid arthritis: listening to patients. JDR Clin Trans Res. (2022) 7:127–34. doi: 10.1177/23800844211012678
37. Schmalz G, Patschan S, Patschan D, Ziebolz D. Oral-health-related quality of life in adult patients with rheumatic diseases-a systematic review. J Clin Med. (2020) 9:1172. doi: 10.3390/jcm9041172
38. Shrestha S, Pradhan S, Adhikari B. Prevalence of periodontitis among rheumatoid arthritis patients attending tertiary hospital in Nepal. J Nepal Health Res Counc. (2020) 17:543–7. doi: 10.33314/jnhrc.v17i4.1841
39. Silvestre FJ, Silvestre-Rangil J, Bagán L, Bagán JV. Effect of nonsurgical periodontal treatment in patients with periodontitis and rheumatoid arthritis: a systematic review. Med Oral Patol Oral Cir Bucal. (2016) 21:e349–54. doi: 10.4317/medoral.20974
40. Magdy E, Ali S. Stratification of methotrexate-induced oral ulcers in rheumatoid arthritis patients. Spec Care Dentist. (2021) 41:367–71. doi: 10.1111/scd.12575
41. de Pablo P, Serban S, Lopez-Oliva I, Rooney J, Hill K, Raza K, et al. Outcomes of periodontal therapy in rheumatoid arthritis: the OPERA feasibility randomized trial. J Clin Periodontol. (2023) 50:295–306. doi: 10.1111/jcpe.13756
42. Radwan-Oczko M, Duś-Ilnicka I, Richards P, Thomsen AM, Rasmussen C. Evaluation of oral health status and oral care of patients with rheumatoid arthritis. Int J Dent. (2020) 2020:8896766. doi: 10.1155/2020/8896766
43. Posada-López A, Botero JE, Pineda-Tamayo RA, Agudelo-Suárez AA. The effect of periodontal treatment on clinical and biological indicators, quality of life, and oral health in rheumatoid arthritis patients: a quasi-experimental study. Int J Environ Res Public Health. (2022) 19:1789. doi: 10.3390/ijerph19031789
Keywords: rheumatoid arthritis, periodontitis, self-health management, oral care, self-care ability
Citation: Lan S, Jin S, Lin R, Chen B, Gao F, Zhang S, Chen L and Li H (2024) Effects of green tea based oral health strategies on disease activity in rheumatoid arthritis. Front. Med. 11:1413753. doi: 10.3389/fmed.2024.1413753
Received: 07 April 2024; Accepted: 14 October 2024;
Published: 05 November 2024.
Edited by:
Ryu Watanabe, Osaka Metropolitan University, JapanReviewed by:
Abdelhadi Hbibi, International University of Rabat, MoroccoDorota Formanowicz, Poznan University of Medical Sciences, Poland
Copyright © 2024 Lan, Jin, Lin, Chen, Gao, Zhang, Chen and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hong Li, bGVlaG9uZzk5JiN4MDAwNDA7MTI2LmNvbQ==
†These authors have contributed equally to this work
 Sanrong Lan
Sanrong Lan Shuang Jin1,2†
Shuang Jin1,2† Hong Li
Hong Li