
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Med. , 15 May 2024
Sec. Gastroenterology
Volume 11 - 2024 | https://doi.org/10.3389/fmed.2024.1413254
This article is part of the Research Topic Diverticulitis - A Neglected Disease Despite its Clinical Burden View all 4 articles
 Stefan Chiorescu1,2
Stefan Chiorescu1,2 Mihaela Mocan3,4*
Mihaela Mocan3,4* Maria Elena Santa5
Maria Elena Santa5 Florin Mihăileanu1,2
Florin Mihăileanu1,2 Roxana Mihaela Chiorescu3,4
Roxana Mihaela Chiorescu3,4Introduction: Jejunal diverticulosis is a rare condition. Most of the time, it is asymptomatic; but it can cause severe complications such as intestinal perforation, mechanical occlusion, and hemorrhage.
Case presentation: A patient aged 78 years, with a history of biological aortic valve prosthesis, atrial fibrillation, type 2 diabetes mellitus, and chronic obstructive pulmonary disease, presented in the emergency department for acute abdominal pain in the lower abdominal floor, nausea, and inappetence. Abdominal computed tomography revealed an inflammatory block in the hypogastrium, agglutinated small intestinal loops, fecal stasis, and air inclusions. Pulled mesentery and associated internal hernia are suspected. Exploratory laparotomy was performed, revealing an inflammatory block in the hypogastrium, whose dissection revealed inner purulent collection and the appearance of jejunal diverticulitis, a diagnosis confirmed by histopathological examination. Segmental resection of the jejunum with double-layer terminal–terminal enteroenteric anastomosis, lavage, and drainage was performed. The evolution was favorable.
Conclusion: Based on our brief review, the diagnosis of complicated jejunal diverticulosis is difficult and sometimes not accurately established, even by high-resolution imaging techniques, with diagnostic laparotomy being necessary for these situations. Surgical treatment should be considered before severe complications develop.
Jejunal diverticulosis is a rare pathology that occurs in 0.3–1.3% of patients (1). Most often, it is asymptomatic; but sometimes it can give serious complications such as diverticulitis, perforation, mechanical occlusion, and hemorrhage. Due to its position, most of the time, high-evolution imaging techniques cannot establish the diagnosis. Therefore, this diagnosis should be considered in patients with intense abdominal pain localized periumbilically or in the hypogastrium. Performing an emergency laparoscopy is preferable to a conservative medical attitude in these situations. We present the case of a 78-year-old woman who presented with a complication of small intestine diverticulosis – diverticulitis and intestinal perforation requiring emergency surgery.
This paper aims to describe a case of small intestine diverticulitis and intestinal perforation and review the cases of small intestine diverticulitis published in the last 10 years to determine the best method of diagnosis and appropriate conservative or surgical treatment for these cases.
A 78-year-old female patient was referred to our emergency department with complaints of lower abdominal pain, slowed gastrointestinal transit, nausea, loss of appetite, and fatigue.
Her medical history was significant for hypertension, biological aortic valve, mitral valve regurgitation, atrial fibrillation, heart failure NYHA II/III, chronic obstructive pulmonary disease Gold II, type 2 diabetes mellitus, and dyslipidemia. There was no relevant family history. Her medication history consisted of Perindopril 10 mg/Indapamide 2.5 mg, Acenocoumarol 2 mg/day, Digoxin 0.25 mg/day, 5/7 days, Budesonide 160 microg/Formoterol 4.5 micron 2× two puffs/day, and Metformin 1,000 mg/day.
The pain was moderate without irradiation. There were no aggravating or relieving factors. The symptoms were worsening in the last 4 days before admission.
On admission, the patient had a body temperature of 37.7°C, a pulse rate of 80 beats/min, a blood pressure of 140/80 mmHg, and a saturation of 96% in ambient air. Physical examination revealed a new periumbilical mass associated with lower abdominal tenderness but no rigidity or rebound tenderness.
Blood tests showed leukocytosis (22 × 109/L), neutrophilia (20.09 × 109/L), C-reactive protein >30 mg/dL, procalcitonin 9.5 ng/mL, creatinine = 3.42 mg/dL, urea = 127 mg/dL, and INR > 9.
An abdominal ultrasound was performed, which revealed intestinal loops with peristalsis present at the level of the descending colon – a slightly dilated intestinal loop with a slightly thickened intestinal wall. We completed with abdominal and pelvic computer tomography scan (CT), which showed an inflammatory block at the level of the hypogastrium – thin intestinal loops, agglutinated, forming a lesional block of 90/69/60 mm, with fecal stasis and air inclusions. Adjacent fat infiltrated, with multiple fluid fuses present. Pulled mesentery and mesenteric vessels – an associated internal hernia is suspected (Figure 1).
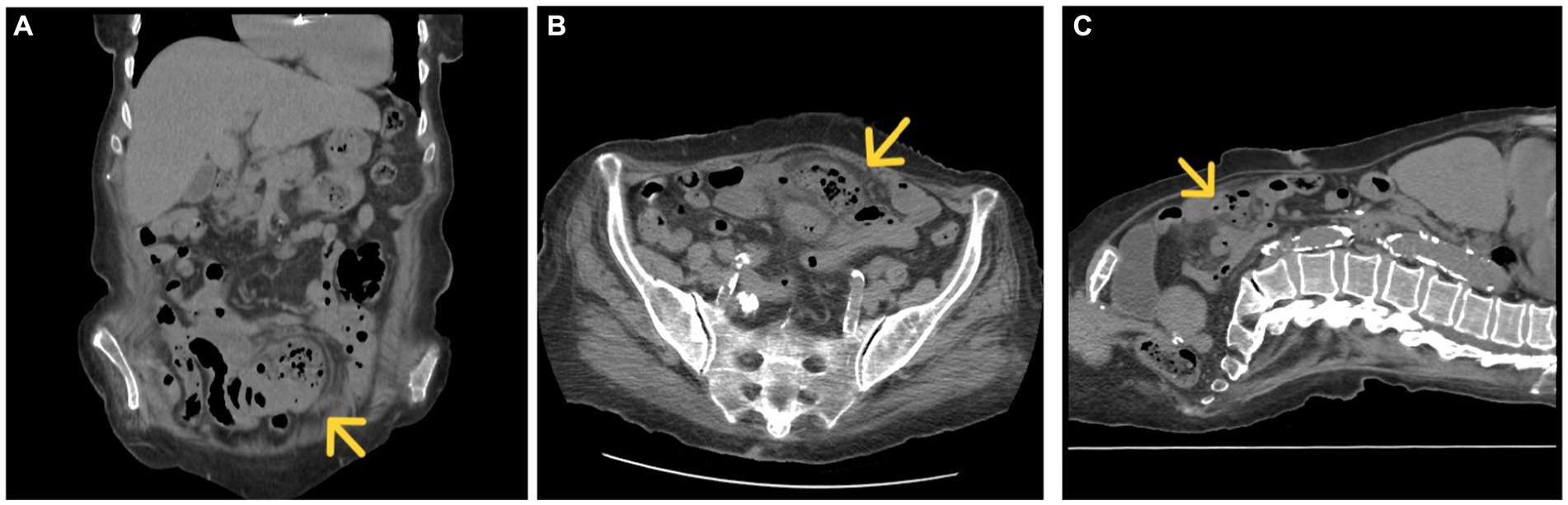
Figure 1. CT, coronal (A), axial (B), and sagittal section (C) inflammatory block marked with a yellow arrow.
An echocardiogram reported neurofunctional biological aortic valve, concentric left ventricular hypertrophy, and mitral valve regurgitation. There were no vegetations of valves observed.
Due to high suspicion of intestinal subocclusion, the patient underwent exploratory laparotomy via a median incision. The abdominal cavity was explored, detecting an epigastric inflammatory block that includes several loops of the small intestine (jejunum and ileum) and omentum, the dissection of which reveals the minimal interileal purulent collection and a tumor at about 50 cm from the duodenojejunal angle, with the appearance of diverticulitis. At 40 cm from the duodenojejunal angle, another uncomplicated intestinal diverticulum of about 2 cm diameter is identified (Figure 2).
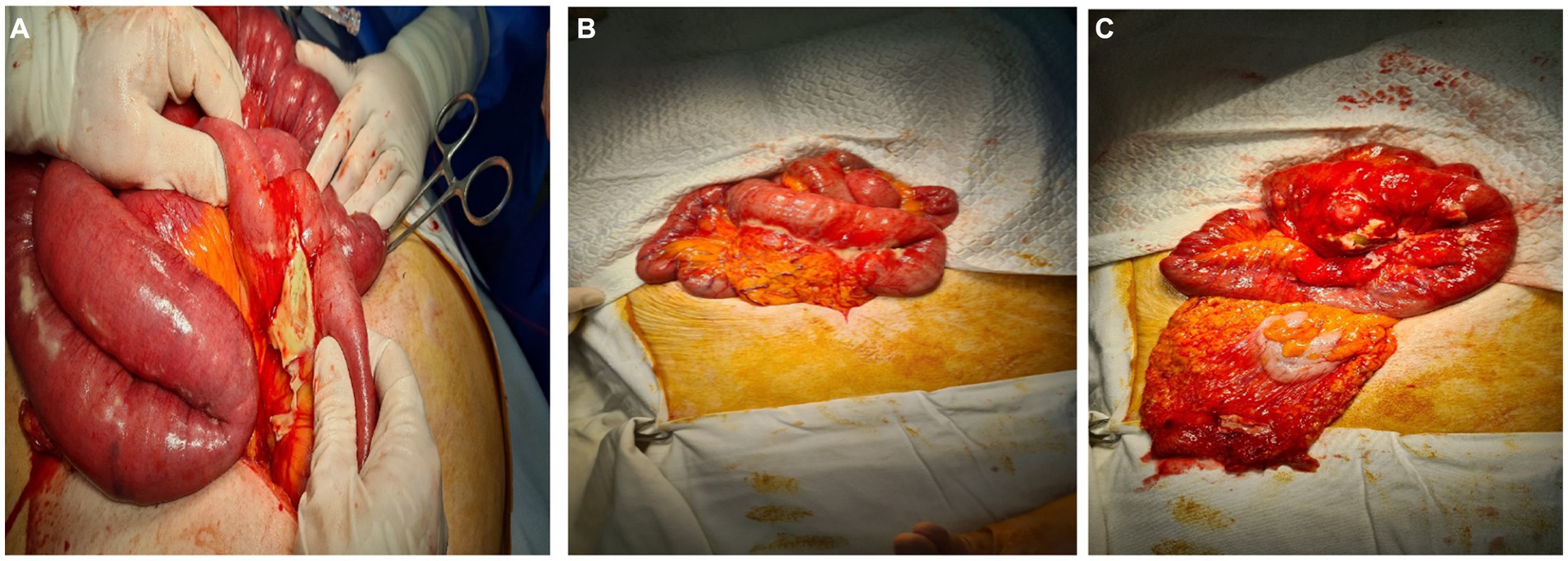
Figure 2. (A–C) Intraoperative appearance. Intestinal inflammatory block, the dissection of which reveals an abscessed jejunal diverticulum.
We performed segmental resection of the jejunum with terminal–terminal enteroenteric anastomosis.
in a double layer, lavage, and drainage. IV fluids, Ceftriaxone 2 g/day once daily, Metronidazole 500 mg every 8 h, probiotics, and Famotidine 20 mg were administered. The treatment of associated diseases continued.
On Day 4, the patient had normal gastrointestinal transit. During hospitalization, the patient presented one episode of upper gastrointestinal bleeding. The patient underwent an esogastroduodenal endoscopy, which revealed a Forrest III antral gastric ulcer and congestive corporeal gastritis without an active source of bleeding. Under treatment with proton pump inhibitors, erythrocyte mass transfusion evolution was favorable. The patient was discharged home on day 21.
Histopathological examination confirmed the diagnosis of jejunal diverticulitis. Stasis, hemorrhagic areas, and lymphoid follicles were observed at the resection margins. The intestinal wall shows areas of necrosis spread throughout its thickness, hemorrhagic areas, abscesses, and a marked transparietal predominantly neutrophilic inflammatory infiltrate. At the level of the diverticulum, fibrin–hematic exudate is observed at the level of the serosa, vascular stasis, hemorrhagic areas, and mixed inflammatory infiltrate, with the presence of lymphoid follicles and erosions at the level of the mucosa (Figures 1, 2).
Diverticula are hernias of the mucosa and submucosa through the muscular layer of the intestinal wall. It is usually located in the sigmoid and descending colon (1).
Localization in the small intestine is rare; the incidence varies between 0.5 and 2.3%. It is usually identified at the level of the proximal jejunum (75%), with the ileum being identified only in 5% of cases (1). Jejunal diverticula are usually multiple and occur more frequently in men in the sixth or seventh decade (2, 3).
Diverticula form in the intestinal wall, in areas of low resistance, due to increased intraluminal pressure (4). They may have a genetic determinism that should be suspected, especially in the case of diffuse forms (5, 6). It is located more frequently in the jejunum than the ileum because the penetrating jejunal arteries have a larger diameter. Other favorable factors for the appearance of diverticles are dysmotility and abnormalities in the mesenteric plex (1, 4). They differ from Merkel diverticula, because they appear on the mesenteric margin (1).
Clinically, jejunal diverticulosis is usually asymptomatic (80%) of cases. When it is symptomatic, it is manifested by nonspecific abdominal pain, transit disorders (diarrhea/constipation), and flatulence (1, 7). Complications of jejunal diverticulosis occur in about 10% of cases, most commonly consisting of acute diverticulitis, mechanical obstruction, volvulus, perforation, peritonitis, and hemorrhage (1, 4). Perforation with peritonitis can be caused by an inflammatory diverticulum or a ruptured diverticular abscess, as was the case with our patient.
Because of its nonspecific symptoms and because it is rare, jejunal diverticulitis is often misinterpreted as appendicitis, peptic ulcer, cholecystitis, Crohn’s disease, or colonic diverticulitis (8). To avoid misdiagnosis, which inevitably leads to delayed treatment, clinicians should be aware of this entity.
Abdominal ultrasonography is used to establish the diagnosis at the first stage. This can sometimes indicate a thickened intestinal wall, irregular-looking formations related to the intestine, hypoechogenic having a hyperechogenic center – characteristic aspect for diverticula, and hyperechogenic tissue around these formations, indicating infiltration of surrounding fat or air bubbles (9).
Computed tomography (CT) is more sensitive in the diagnosis of acute diverticulitis and its complications compared to abdominal ultrasound and is therefore preferred (1, 10).
CT scans identify diverticular inflammation characterized by peridiverticular edema and thickening of the diverticular wall (8). The presence of pneumoperitoneum is not a definite sign of peritonitis, because the thin wall of the diverticulum can allow air to pass through (9).
CT diagnosis is difficult and remains uncertain in advanced local forms, in which diverticula can no longer be identified due to extensive local inflammation that causes fluid and gaseous infiltration. Highlighting other diverticula on the mesenteric edge of the loop of the small intestine helps clarify the diagnosis (9).
Selective mesenteric angiography or CT angiography may be used to locate active bleeding in cases of jejunal diverticular hemorrhage (11).
Treatment of diverticulitis can be conservative and medical (antibiotic therapy, according to table) (10).
The most common bacterial etiology of diverticulitis are:
1. Enterobacteriaceae: Escherichia coli, Klebsiella sp., aerobic high gram-negative bacillus.
2. Bacteroides species.
3. Enterococcus species: Enterococcus faecalis most common, Enterococcus faecium.
4. Pseudomonas aeruginosa: 3–15% (12) (see Table 1).
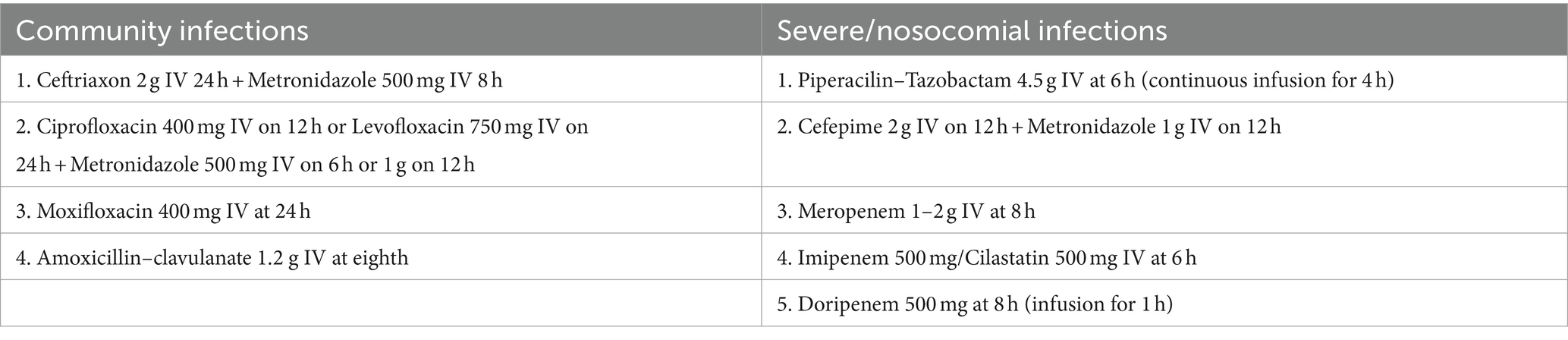
Table 1. Antibiotic treatment in case of acute diverticulitis (12).
The average duration of antibiotic treatment is 5–10 days. The criteria for discontinuing treatment are clinical improvement, normalization of leukocytes, and resumption of intestinal transit (12).
In the case of localized limited perforation, conservative management treatment may be indicated in hemodynamically stable patients (4, 7), with the caveat that surgery should be performed if clinical improvement is not achieved within 48–72 h. In patients with peridiverticular abscess, antibiotic treatment and image-guided drainage (CT) may theoretically be sufficient, depending on the size of the collection and the possibility of a percutaneous approach (8).
For perforated jejunal diverticula, with peritonitis, or in the case of abuse or significant bleeding, literature data recommend emergency laparotomy, segmental intestinal resection, and primary anastomosis to avoid complications (13). Resection should be limited to the intestinal loop with complicated diverticulum (local abscess, peritonitis, or bleeding) to prevent short bowel syndrome (4, 11). An exception is pan-jejunoileal diverticulosis, for which conservative treatment may be preferred. This is because surgery can lead to severe malnutrition (3).
Risk factors for unfavorable evolution are old age, comorbidities, delay in diagnosis, and duration interval between perforation and surgery (9).
No consensus exists on the therapeutic strategy and management of jejunales diverticulitis (8).
To determine the best diagnostic method for complicated jejunal diverticulitis and the most appropriate treatment, we searched PubMed, MedNar, and Cochrane Library electronic databases for literature reviews on cases of jejunal diverticulitis published between 1.01.2014 and 31.12.2023. We considered the following terms in the studies’ title or abstract: “jejunal diverticulitis.” We excluded studies in languages other than English and French and excluded articles that did not cover several cases. The results are summarized in Table 2.
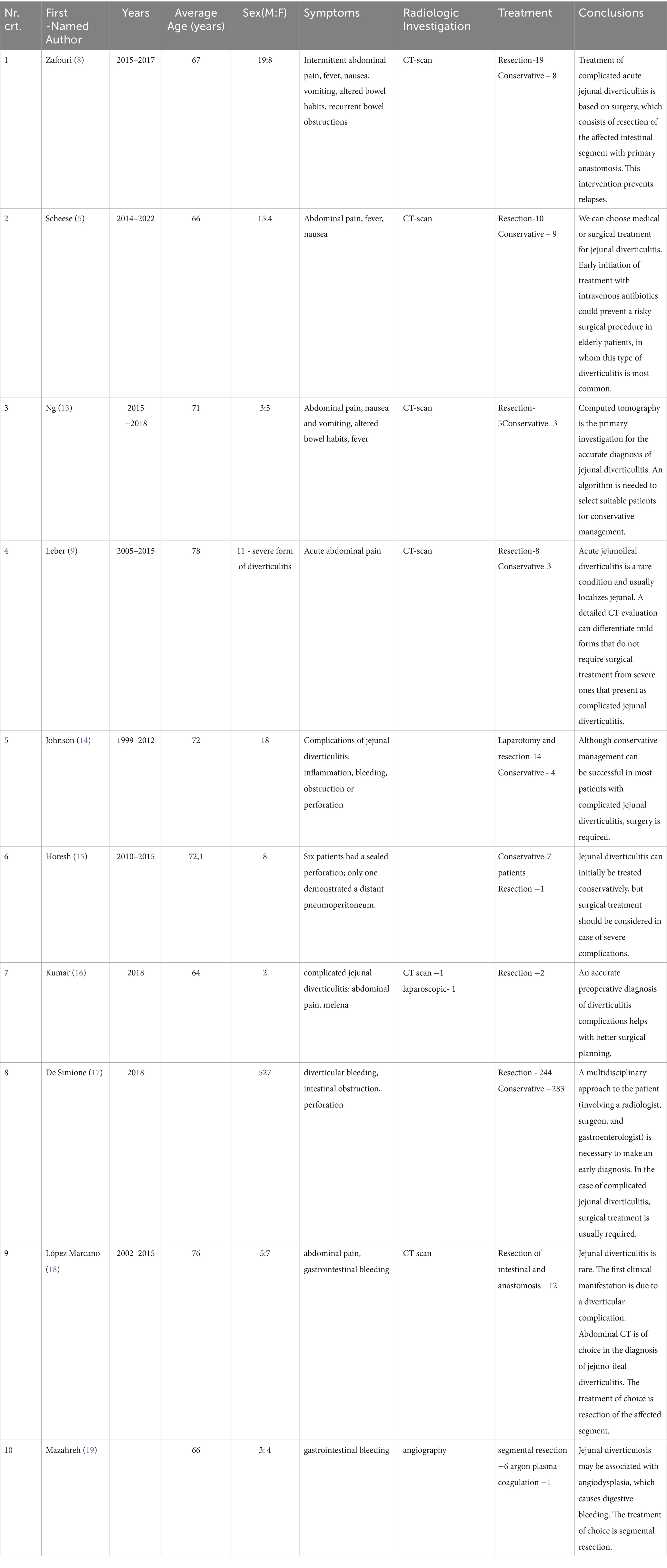
Table 2. Management of patients with acute diverticulitis according to specialized reviews from 2014–2023.
As Table 2 shows, a CT scan is more sensitive in diagnosing acute diverticulitis, but angiography is used in cases of gastrointestinal bleeding. Sometimes, exploratory laparoscopy is needed for diagnosis.
Thus, surgical treatment remains the management of choice in patients with jejunal diverticulitis, possibly due to late diagnosis in the complication phase (8).
In our case, due to advanced local inflammation, the diagnosis could not be established correctly by CT, and the abscessed and perforated intestinal diverticulum was misinterpreted as an internal hernia with intestinal occlusion. It was necessary to perform a laparotomy for diagnostic purposes and surgical treatment. The postoperative evolution was favorable, although the patient had an increased surgical risk of presenting multiple comorbidities.
Diagnosing complicated jejunal diverticulosis is complex and sometimes not accurately established, even by high-resolution imaging, such as a CT scan, the more sensitive diagnostic technique. Diagnostic laparotomy is necessary in these situations. Surgical treatment should be considered in complicated jejunal diverticulitis before severe complications develop.
SC: Writing – original draft, Writing – review & editing, Investigation, Methodology. MM: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. MS: Investigation, Writing – original draft, Writing – review & editing. FM: Investigation, Methodology, Writing – original draft, Writing – review & editing. RC: Writing – original draft, Writing – review & editing.
The author(s) declare that financial support was received for this article’s research, authorship, and publication. The publication fees were partially reimbursed by the University of Medicine and Pharmacy, Cluj-Napoca, Romania.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Pajtak, R, Ramadan, A, and Strauss, P. Strangulated diverticulum: a new acute complication of small bowel diverticulosis. J Surg Case Rep. (2023) 5:rjad253. doi: 10.1093/jscr/rjad253
2. Karas, L, Asif, M, Chun, V, and Khan, FA. Complicated small bowel diverticular disease: a case series. BMJ Case Rep. (2017) 2017:bcr2017219699. doi: 10.1136/bcr-2017-219699
3. Prough, H, Jaffe, S, and Jones, B. Jejunal Diverticulitis. J Surg Case Rep. (2019) 1:rjz005. doi: 10.1093/jscr/rjz005
4. Khan, M, Arshad, R, Malik, I, Kamran, A, Gul, F, and Lee, KY. Jejunal diverticulosis presenting as intestinal obstruction - a case report of a rare association. Clin Case Rep. (2023) 11:e7033. doi: 10.1002/ccr3.7033
5. Scheese, D, Alwatari, Y, Khan, J, and Slaughter, A. Complicated jejunal diverticulitis: a case report and review of literature. Clin Case Reports. (2022) 10:e657011. doi: 10.1002/ccr3.6570
6. Barbaro, MR, Cremon, C, Fuschi, D, Marasco, G, Palombo, M, Stanghellini, V, et al. Pathophysiology of diverticular disease: from diverticula formation to symptom generation. Int J Mol Sci. (2022) 23:6698. doi: 10.3390/ijms23126698
7. Khsiba, A, Bradai, S, Mahmoudi, M, Mohamed, AB, Bradai, J, Bouzaidi, K, et al. Jejunal diverticulitis as a rare cause of abdominal pain: a case report. Pan Afr Med J. (2022) 17:222. doi: 10.11604/pamj.2022.41.222.29095
8. Zafouri, EB, Ben Ismail, I, Sghaier, M, Rebii, S, and Zoghlami, A. Jejunal diverticulitis: a new case report and a literature review. Int J Surg Case Rep. (2022) 97:107395. doi: 10.1016/j.ijscr.2022.107395
9. Lebert, P, Ernst, O, and Zins, M. Acquired diverticular disease of the jejunum and ileum: imaging features and pitfalls. Abdom. Radiol. (2019) 44:1734–43. doi: 10.1007/s00261-019-01928-1
10. Rangan, V, and Lamont, JT. Small bowel diverticulosis: pathogenesis, clinical management, and new concepts. Curr Gastroenterol Rep. (2022) 22:4. doi: 10.1007/s11894-019-0741-2
11. Lin, CH, Hsieh, HF, Yu, CY, Yu, JC, Chan, DC, Chen, TW, et al. Diverticulosis of the jejunum with intestinal 5416Obstruction: a case report. World J Gastroenterol. (2005) 11:5416. doi: 10.3748/wjg.v11.i34.5416
12. CDC. Antibiotic Use in the United States, 2020 Update: Progress and Opportunities. Atlanta, GA: US Department of Health and Human Services, CDC, (2021)
13. Ng, ZQ, Theophilus, M, Navadgi, S, Menon, T, and Wijesuriya, R. Jejunal diverticulitis: a single-Center experience and proposed management algorithm. Surg Infect. (2019) 20:499–503. doi: 10.1089/sur.2019.070
14. Johnson, KN, Fankhauser, GT, Chapital, AB, Merritt, MV, and Johnson, DJ. Emergency management of complicated jejunal diverticulosis. Am Surg. (2014) 80:600–3. doi: 10.1177/000313481408000625
15. Horesh, N, Klang, E, Gravetz, A, Nevo, Y, Amiel, I, Amitai, MM, et al. Jejunal Diverticulitis. J Laparoendosc Adv Surg Tech A. (2016) 26:596–9. doi: 10.1089/lap.2016.0066
16. Kumar, D . Complicated jejunal diverticulitis with unusual presentation. Radiol Case Rep. (2018) 13:58–64. doi: 10.1016/j.radcr.2017.10.002
17. De Simone, B, Alberici, L, Ansaloni, L, Sartelli, M, Coccolini, F, and Catena, F. Not all diverticulites are colonic: small bowel diverticulitis - a systematic review. Minerva Chir. (2019) 74:137–45. doi: 10.23736/S0026-4733.18.07745-3
18. López Marcano, AJ, Ramia, JM, De la Plaza, LR, Alonso, S, Gonzales Aguilar, JD, and Kühnhardt Barrantes, AW. Complicated jejunoileal diverticular disease: a 12 cases' serie and literature review. Rev Gastroenterol Peru. (2017) 37:240–5.
Keywords: intestinal perforation, jejunal diverticulosis, diverticulitis, segmental resection, surgical treatment
Citation: Chiorescu S, Mocan M, Santa ME, Mihăileanu F and Chiorescu RM (2024) Acute complicated jejunum diverticulitis: a case report with a short literature review. Front. Med. 11:1413254. doi: 10.3389/fmed.2024.1413254
Received: 06 April 2024; Accepted: 23 April 2024;
Published: 15 May 2024.
Edited by:
Savvas Papagrigoriadis, IASO General Hospital, GreeceReviewed by:
Anestis Charalampopoulos, University General Hospital Attikon, GreeceCopyright © 2024 Chiorescu, Mocan, Santa, Mihăileanu and Chiorescu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mihaela Mocan, bWloYWVsYS5tb2NhbkBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.