- 1Department of Public Health and Community Medicine, Faculty of Medicine, Al-Balqa Applied University, Al-Salt, Jordan
- 2Faculty of Nursing, Yarmouk University, Irbid, Jordan
- 3Department of Community Medicine, Public Health and Family Medicine, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan
- 4College of Nursing, King Saud University, Riyadh, Saudi Arabia
- 5Division of Cardiology, Department of Internal Medicine, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan
- 6Applied Science Research Center, Applied Science Private University, Amman, Jordan
- 7Specialty Hospital, Amman, Jordan
- 8School of Nursing, California State University, Los Angeles, CA, United States
- 9Istishari Hospital, Amman, Jordan
Background: An elevated risk of stroke is linked to atrial fibrillation (AF). Effective care and prevention measures for individuals with AF require an understanding of the factors impacting the incidence of stroke in this population. Evidence regarding the incidence of stroke among patients with AF is insufficient in Jordan. This study aimed to determine the incidence of stroke and its associated factors among patients with AF in Jordan.
Methods: The Jordan Atrial Fibrillation Registry JoFib was used to identify a total of 2020 AF patients meeting the study inclusion and exclusion criteria. Demographics, clinical characteristics, and the CHA2DS2-VASc score-based evaluation of stroke risk were extracted from the registry.
Results: This study encompassed 2020 participants diagnosed with AF, with 925 (45.8%) being men and 1,095 (54.2%) women. The one-year stroke incidence among the 2020 AF patients was 3.4%. Notably, stroke incidence significantly increased with age (p = 0.04) and was associated with the history of stroke (7.4% vs. 2.7%), hypertension (3.9% vs. 1.9%), and diabetes (5.1% vs. 2.1%). In the multivariate analysis, diabetes (OR = 2.6, 95% CI: 1.5–4.4, p = 0.001) and history of stroke (OR = 2.6, 95% CI: 1.5–4.6, p = 0.001) were significantly associated with stroke incidence.
Conclusion: This study emphasizes Jordan’s high stroke rate among AF patients. Diabetes and prior stroke history are associated with increased odds of stroke, like all stroke patients. These results highlight the necessity for specialized management strategies among AF patients and highlight the significance of thorough risk assessment and focused interventions to reduce stroke risk in AF patients.
Introduction
The most prevalent persistent cardiac arrhythmia, atrial fibrillation (AF), is linked to higher rates of morbidity, increased use of medical resources, and mortality. With an estimated 2–4 percent prevalence, AF affects approximately 33 million persons worldwide (1, 2). Given that a sizable percentage of patients go undetected, it is anticipated that this estimate will be underestimated (3). According to epidemiological research, more than 5.6 million Americans are likely to get AF by 2050, and by 2060, there will be 17.9 million AF patients in Europe who are older than 55 (4, 5).
A number of conditions, including coronary artery disease, heart failure, diabetes, obesity, and hypertension, are linked to an increased risk of AF (5). Likewise, these variables are linked to a higher chance of stroke and death in AF patients (3, 5, 6). Hemorrhagic strokes are caused by abrupt bleeding in the brain, while ischemic strokes are caused by obstructed blood flow to the brain. Stroke is attributed to many etiologies like atherosclerosis, cardioembolism (mainly associated with AF), small vessel disease, hypertension, aneurysm rupture, and others (7). Recent research addressed services for stroke patients in Jordan and the region with identified improvements strategies like accreditation, specialized training, and quality registries (8, 9). Patients with AF have a nearly five-fold increased risk of stroke compared to those without AF (2, 10), which accounts for around 25% of all stroke types (11). The main components of CHADS2-VASc score, which are used to assess the risk of stroke in patients with AF (12), include metabolic abnormalities linked to an elevated risk of stroke in patients with AF, the scoring items include established history of stroke/transient ischemic attack/thromboembolic event, in addition to congestive heart failure, hypertension, Age ≥ 75 years, diabetes mellitus, vascular disease (prior myocardial infarction MI, peripheral artery disease PAD, or aortic plaque), age 65 to 74 years, and sex category (female sex) (13, 14).
When compared to other forms of strokes, AF-related strokes are more deadly and cause greater death rates (11). Patients who get a stroke due to AF are twice as likely to end up bedridden as those who experience a stroke from another cause, which can be attributed to known AF before stroke (15, 16). Because of the nature of these occurrences, stroke linked to AF eventually results in a significant financial burden due to an increase in readmissions (11).
There is a lack of prior research on the incidence of stroke among patients with AF and its related variables in the Middle East, namely in Jordan. The usage of oral anticoagulants and the clinical characteristics of AF were the primary topics of the scant investigations conducted in the Middle East (17–19). Determining the incidence of stroke and the factors that contribute to it is crucial for comprehensive therapy of AF. Thus, the purpose of this study was to determine the incidence of stroke and its associated factors among patients with AF in Jordan.
Materials and methods
Study population
The Jordan Atrial Fibrillation (JoFIB) registry is a prospective, multicenter observational registry that, from May 2019 to January 2021, included consecutive AF patients who were over the age of eighteen in 19 hospitals and 11 outpatient clinics throughout Jordan. The methodology was already released in print (20). As an overview, data were gathered at enrollment and one, six, and 12 months following the initial examination utilizing a standardized clinical data form. A 12-lead electrocardiogram (EKG) rhythm strip lasting more than 30 s, more than one episode of AF on an ambulatory EKG monitor, or a previous diagnosis made by a treating cardiologist were used to confirm the diagnosis of AF. The usage of OACs and other pharmaceutical drugs, laboratory results, EKG, clinical and demographic profiles, and transthoracic echocardiographic features were all included in the baseline data. The classification of AF kinds, such as paroxysmal, persistent, long-standing, and permanent, and the computation of each patient’s CHA2DS2-VASc and HAS-BLED scores were done using standard definitions (12, 21). The 2019 focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation was used to analyze eligibility for oral anticoagulant medicines (22).
Inclusion criteria and baseline data collection
Patients with AF who were above 18 years old and had been diagnosed with the condition with a 12-lead EKG rhythm strip lasting more than 30 s or an ambulatory EKG monitor displaying more than one episode of AF met the inclusion criteria. Demographics (age, gender, smoking history), clinical traits body mass index [BMI], self-reported comorbidities (ischemic heart disease, hypertension, diabetes, and dyslipidemia), and the CHA2DS2-VASc score were used to estimate the risk of stroke with no cut-off value for inclusion in the study (12, 23, 24).
Ethical considerations
The study’s participating hospitals, which included Amman Surgical Hospital, Arab Medical Center, Essra Hospital, Ibn Haitham Hospital, Islamic Hospital, Istishari Hospital, Jordan Hospital, Khalidi Medical Center, King Abdullah University Hospital, King Hussein Medical Center, Prince Hamza Hospital, Prince Hashem Hospital, Queen Alia Cardiac Center, Salt Medical Center, and Specialist Hospital, all received ethical approval (approval number 10/2021/415). Written informed permission was acquired by each subject. The study was registered with the unique identifier NCT03917992 on clinicaltrials.gov. There was no patient or public participation in the planning, execution, reporting, or distribution of this study.
Statistical analysis
Data analysis was done with IBM SPSS version 20. Continuous variables (means and standard deviation [SD]) and categorical variables (percentages) were described via descriptive statistics. The chi-square test was used to compare the incidence of stroke among different variable categories. To identify the factors associated with stroke, binary logistic regression was conducted. A p < 0.05 was considered statistically significant.
Results
Characteristics of participants
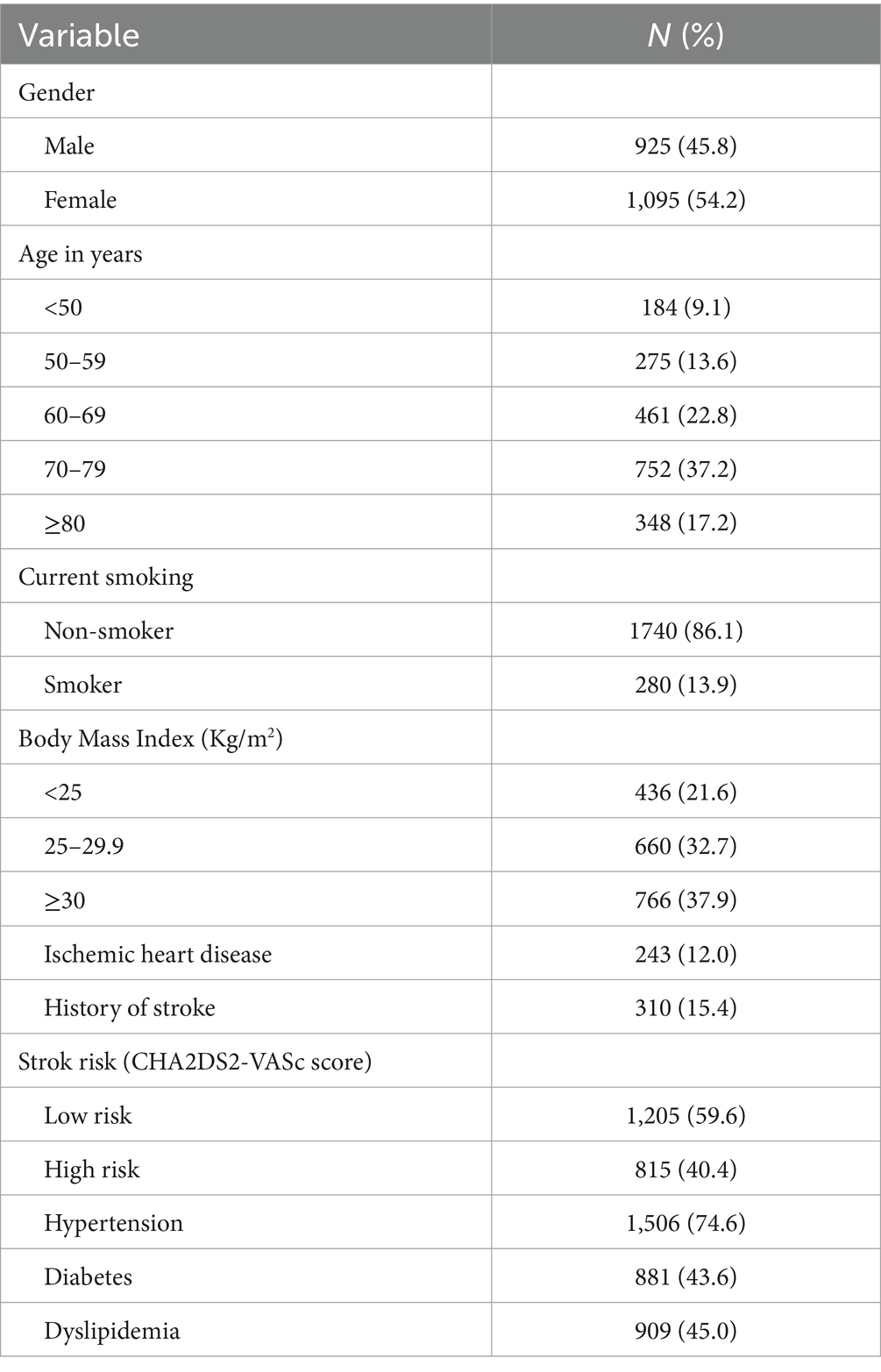
Our study encompassed 2020 participants diagnosed with AF, with 925 (45.8%) being men and 1,095 (54.2%) women. A total of 752 (37.2%) patients were aged 70–79 years old, and 348 (17.2%) were aged 80 or older. Among participants, 280 (13.9%) were smokers and 1,136 (76.8%) had a BMI of 25 kg/m2 or higher. Ischemic heart disease was present in 243 (12.0%) participants, while 310 (15.4%) had a history of stroke. Utilizing the CHA2DS2VAS score, stroke risk assessment categorized 815 (40.4%) patients as high risk and 1,205 (59.6%) as low risk. Hypertension was the most common comorbidity, affecting 1,506 (74.6%) patients, followed by diabetes in 881 (43.6%) and dyslipidemia in 909 (45.0%). Detailed patient characteristics specific to Jordanian AF patients are outlined in Table 1.
One-year incidence of stroke among AF patients
Table 2 delineates the one-year stroke incidence among the 2020 AF patients, indicating an overall incidence of 3.4%. Notably, stroke incidence significantly increased with age (p = 0.04) and was associated with the history of stroke (7.4% vs. 2.7%), hypertension (3.9% vs. 1.9%), and diabetes (5.1% vs. 2.1%).
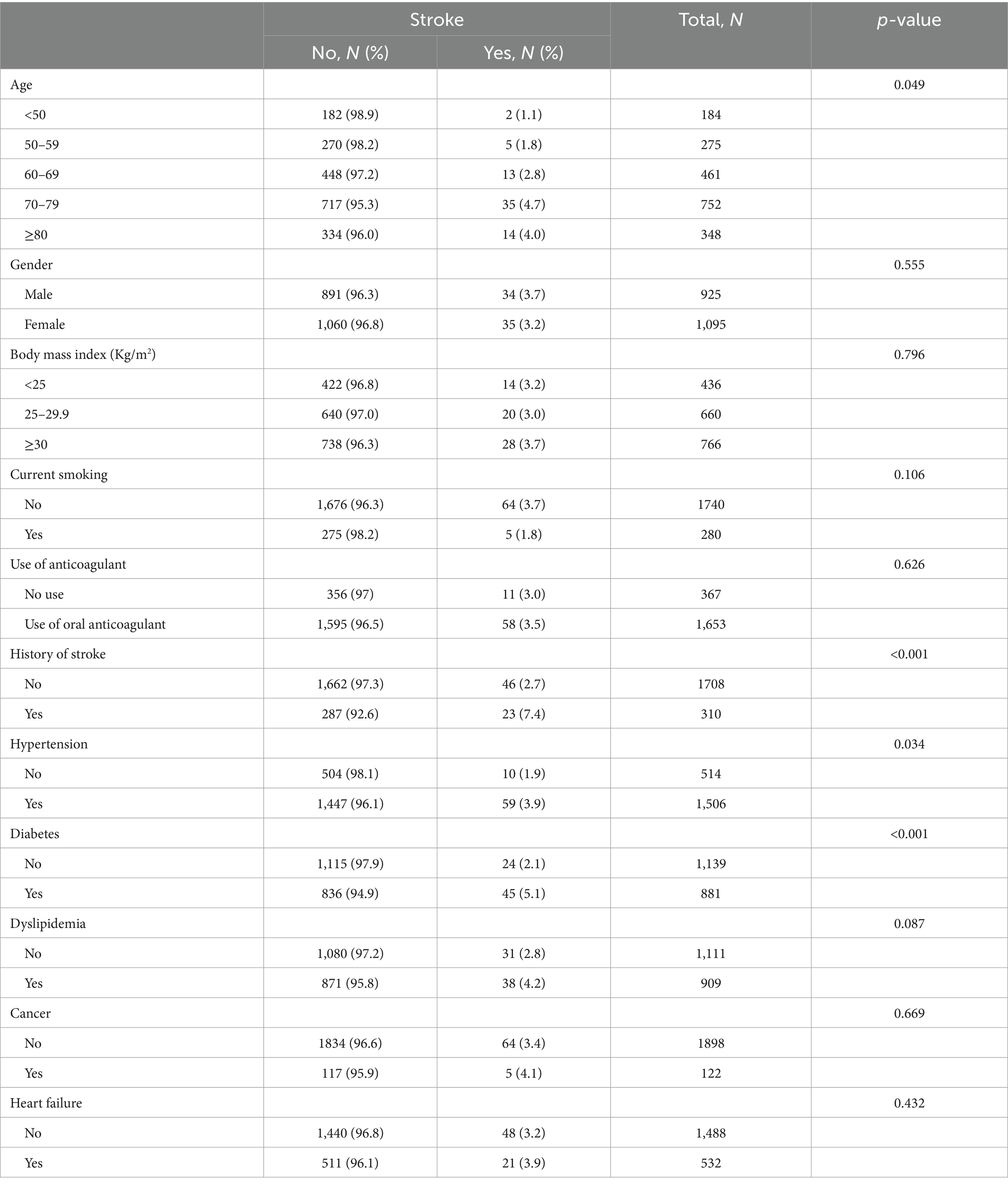
Table 2. One-year stroke incidence among patients with atrial fibrillation according to demographic and clinical characteristics, N = 2020.
Stroke incidence in relation to prescribed medications
No statistically significant associations were found between oral anticoagulant usage or antiplatelet drugs and stroke risk (p > 0.05). However, a noteworthy correlation (p < 0.001) was observed between ticagrelor usage and stroke occurrence. Additionally, correlations were found between stroke incidence and beta blockers (p = 0.040), amiodarone (p = 0.035), calcium channel blockers (CCBs) (p < 0.001), and statins (p = 0.035). No significant correlations were found with other medications. The association of stroke with prescribed medications are provided in Table 3.
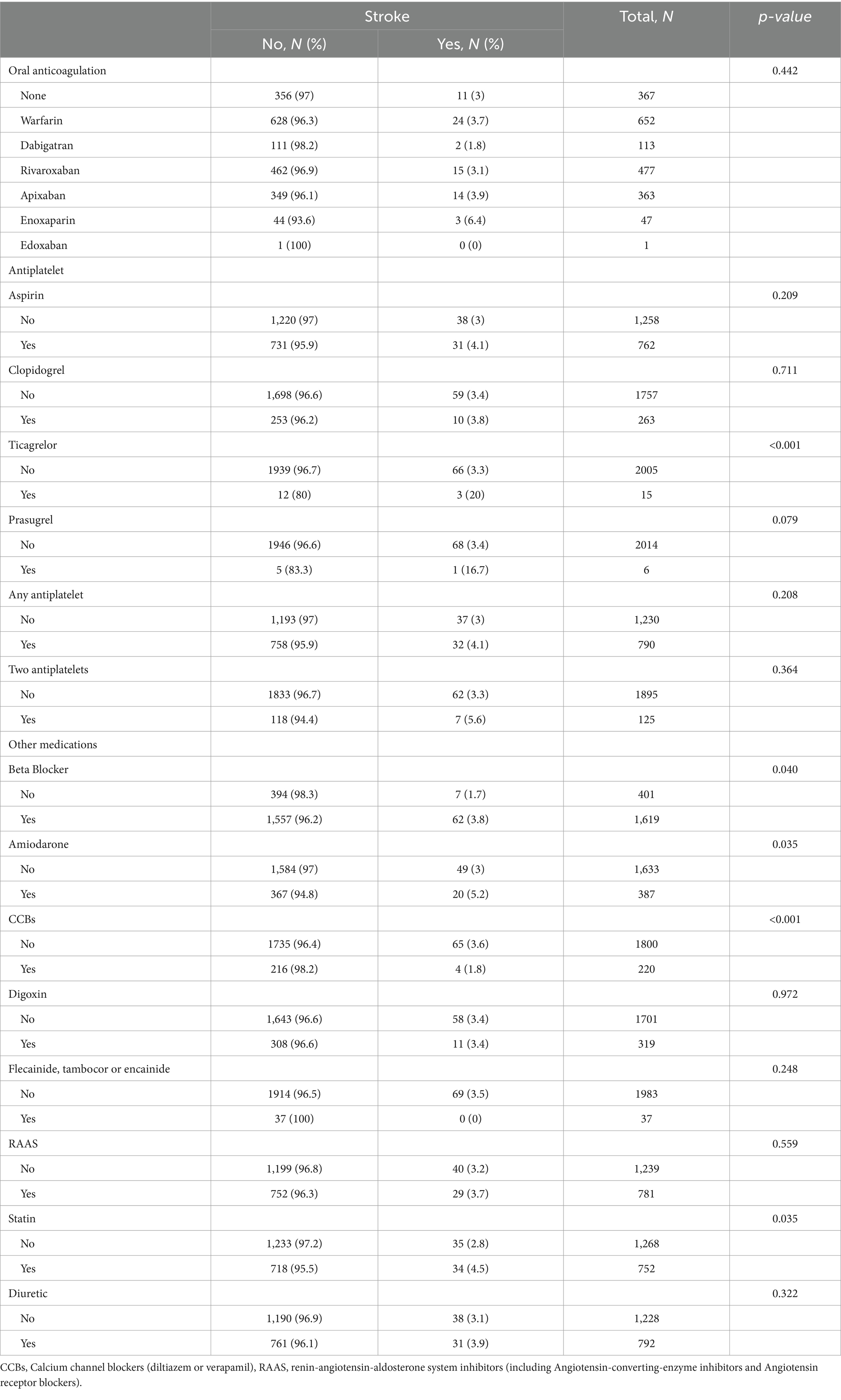
Table 3. The one-year incidence of stroke among patients with atrial fibrillation according to prescribed medications, N = 2020.
Factors associated with one-year stroke incidence among AF patients
Multivariate analysis (Table 4) identified risk factors for stroke in AF patients after adjusting for variables including age, BMI, hypertension, and anticoagulant use. Diabetes (OR = 2.6, 95% CI: 1.5–4.4, p = 0.001) and history of stroke (OR = 2.6, 95% CI: 1.5–4.6, p = 0.001) were significantly associated with stroke incidence.
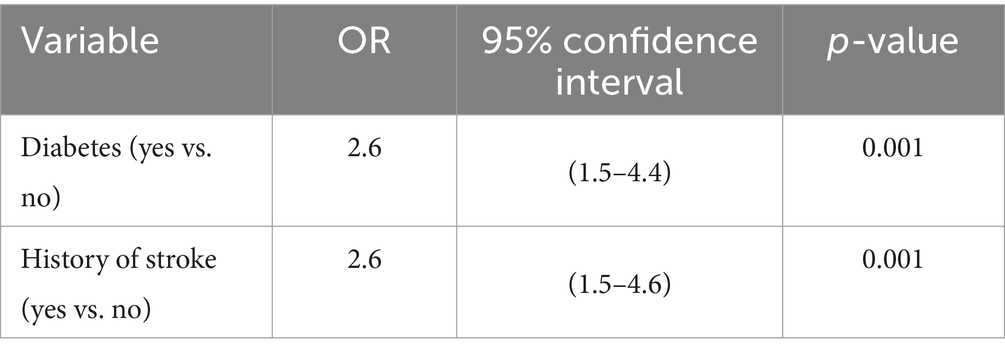
Table 4. Multivariate analysis of factors associated with stroke among patients with atrial fibrillation, N = 2020.
Discussion
In the present study, relevant data of AF patients were extracted from a national clinical trial, the Jordan Atrial Fibrillation Registry, and were assessed for stroke incidence and trends regarding associated factors to stroke burden in Jordan. This study serves as a continuum of efforts to better understand AF status and its associated comorbidities, including stroke. This is the largest study reporting stroke incidence in AF patients among Jordanian population.
According to our study’s findings, 3.4% of individuals with AF had a stroke within a year. Interestingly, the likelihood of stroke in this cohort was found to be significantly increased by the presence of diabetes or a history of prior stroke. Our observed rate of stroke incidence is in line with earlier studies carried out in Jordan, which found that patients with AF had a 4.5% one-year risk of stroke/systemic embolization (17). Furthermore, our results are consistent with regional and international research that reports stroke incidence rates in people with AF ranging from 2 to 10% (25–27).
Regionally, fragmented evidence has reported incidence of stroke among AF patients (28). Stroke in AF patients was reported to be 6.4% in Qatar (29), 9.8% in Iraq (30), 10.8% in Egypt (31), 13.5% in Saudi Arabia (32), and 14.0% in Palestine (33). A study by Zubaid. et al. (34) reported 9.0% stroke prevalence among AF patients at an extensive survey of 23 hospitals in six middle-east gulf countries (Bahrain, Kuwait, Qatar, Oman, United Arab Emirates, and Yemen).
It is in line with previous research to identify diabetes as a major risk factor for stroke in patients with AF. Diabetes mellitus is known to raise the risk of thromboembolism by a number of pathological processes, such as impaired fibrinolysis, hypercoagulability, and endothelial dysfunction (35). Patients diagnosed with diabetes had significantly higher hazard ratios for both ischemic and hemorrhagic strokes, according to research from the Emerging Risk Factors Collaboration (35, 36). As a result, it is especially important to manage AF patients who also have diabetes, with anticoagulant therapy being essential in preventing strokes, according to new guidelines from the American Heart Association (24). Furthermore, concomitant conditions such hypertension, diabetes, congestive heart failure, dyslipidemia, coronary heart disease, sleep apnea, tobacco use, and obesity that are linked to an elevated risk of AF have also been linked to an increased risk of stroke (37–40). These systemic vascular risk factors lead to atrial cardiomyopathy, which can induce AF and thromboembolism. Following the beginning of AF, the atrial contractile function and the underlying atrial cardiomyopathy deteriorate, raising the risk of thromboembolism and providing an explanation for the rise in stroke risk (41).
Despite the scope of our study, it’s worth mentioning other perspectives for the mechanism attributing the cause of AF to stroke itself (42). Associations between abnormal autonomic innervation and AF have been established, with insults to the central nervous system, such as stroke, believed to play a significant role in AF’s pathogenesis (43). AF is diagnosed in about 7% of acute ischemic stroke patients within the first 3–5 days post-stroke, increasing to 25% with prolonged monitoring, a condition termed AF diagnosed after stroke (AFDAS) (16, 44, 45). AFDAS has been classified into ECG-detected AF and AF detected on a prolonged cardiac monitor (PCM-detected AF), with ECG-detected AF associated with a higher risk of recurrent ischemic stroke (46). Several mechanisms, including cardiac autonomic nervous system imbalances and stroke location within the brain, have been proposed for AF development post-stroke (47, 48). Additionally, the ‘catecholamine surge hypothesis’ and Stroke-Heart syndrome have been identified as potential contributors (44). Nevertheless, until further evidence is available, patients with AFDAS should receive anticoagulation as per current clinical practice.
Our results highlight the significance of a comprehensive care strategy for patients with AF, encompassing the timely identification, evaluation, and treatment of coexisting metabolic disorders like diabetes to reduce the risk of stroke and avoid unfavorable health consequences. It may be possible to improve the overall cardiovascular prognosis of AF patients with diabetes by teaching them about the significance of medication adherence, dietary changes, and timely medical treatment (49, 50).
Likewise, a history of stroke was found to be an additional independent risk factor that was substantially linked to an elevated risk of stroke in individuals with AF. People who have had a prior stroke are known to have a higher chance of having another one; recurrence rates range from about 30 to 43% (51–53). One of the strongest independent risk factors linked to the occurrence of strokes was a prior history of stroke, which is consistent with earlier studies conducted in Jordan (17).
These results emphasize how important it is to implement focused interventions to improve stroke preventive methods in AF patients who have previously experienced a stroke. In this high-risk subgroup, improving adherence to anticoagulant therapy and lifestyle adjustments ought to be prioritized. Furthermore, it is critical to improve public understanding and awareness of stroke risk factors and management, especially in areas like Jordan where the stroke burden is still high (54–58). Raising awareness and gaining information can help identify stroke symptoms early and get patients access to timely care, which will ultimately improve patient outcomes and lessen the burden of stroke-related morbidity and mortality in the general community.
Our study is strong in two areas. It is the first study of its kind on AF conducted in the Middle East today. The majority of earlier research on AF was carried out five to 10 years ago. Second, the study is the first multi-center investigation of the warfarin population in the area.
To ensure transparency and scientific validity, this study does come with limitations. Observational studies may introduce bias which is mainly sampling bias. Not every research subject has been enrolled in the study in order. Additionally, while other patients in the nation may be managed by their family medicine physicians, internists, or general physicians, all study participants had their AF managed by cardiologists at health facilities. Moreover, extensive associations related to variations in exact treatment regimens with incidence of stroke among AF patients cannot be concluded. Also, the study did not specify sub-types of stroke nor the types of AF and included all types of both conditions in the final analysis.
Conclusion
In line with earlier studies conducted in the area, the 1-year stroke incidence among patients with AF in Jordan was determined to be roughly 3%. Aligned with their influence on stroke population, our research highlights the importance of diabetes and prior stroke as important risk factors for stroke incidence in patients with AF. Nevertheless, more long-term studies are necessary to fully stratify the risk of diabetes, prior strokes, and their corresponding correlations with stroke in AF patients. Further research may also examine the possible influence of therapies aimed at these risk factors on reducing the incidence of stroke and enhancing the prognosis of individuals with AF. Improved knowledge of these correlations may help develop specialized treatment plans meant to lessen the impact of stroke morbidity and mortality among individuals with AF.
Data availability statement
Data supporting the findings of this research are available upon reasonable request from the corresponding author.
Ethics statement
The study was conducted in accordance with the Declaration of Helsinki. The study was approved by the Institutional Review Board of the following participating healthcare settings: King Abdullah University Hospital, Amman Surgical Hospital, Arab Medical Center, Essra Hospital, Salt Medical Center, Islamic Hospital, Jordan Hospital, Khalidi Medical Center, King Hussein Medical Center, Prince Hamza Hospital, Istishari Hospital, Prince Hashem Hospital, Queen Alia Cardiac Center, Specialist Hospital, and Ibn Haitham Hospital. The participants provided their written informed consent to participate in this study.
Author contributions
TA-S: Conceptualization, Formal analysis, Methodology, Project administration, Resources, Software, Supervision, Writing – original draft, Writing – review & editing. OA: Data curation, Formal analysis, Methodology, Resources, Software, Writing – original draft, Writing – review & editing. YK: Conceptualization, Data curation, Formal analysis, Methodology, Resources, Validation, Writing – original draft, Writing – review & editing. HA: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. OQ: Methodology, Resources, Validation, Writing – original draft, Writing – review & editing. MJ: Methodology, Resources, Validation, Writing – original draft, Writing – review & editing. AA: Methodology, Resources, Validation, Writing – original draft, Writing – review & editing. RA-A: Investigation, Methodology, Resources, Validation, Writing – original draft, Writing – review & editing. TZ: Methodology, Resources, Validation, Writing – original draft, Writing – review & editing. AH: Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We acknowledge participants for their participation in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Chung, MK, Eckhardt, LL, Chen, LY, Ahmed, HM, Gopinathannair, R, Joglar, JA, et al. Lifestyle and risk factor modification for reduction of atrial fibrillation: a scientific statement from the American Heart Association. Circulation. (2020) 141:e750–72. doi: 10.1161/CIR.0000000000000748
2. Abellana, R, Gonzalez-Loyola, F, Verdu-Rotellar, JM, Bustamante, A, Palà, E, Clua-Espuny, JL, et al. Predictive model for atrial fibrillation in hypertensive diabetic patients. Eur J Clin Investig. (2021) 51:e13633. doi: 10.1111/eci.13633
3. Alshehri, AM. Stroke in atrial fibrillation: review of risk stratification and preventive therapy. J Fam Community Med. (2019) 26:92. doi: 10.4103/jfcm.JFCM_99_18
4. Krijthe, BP, Kunst, A, Benjamin, EJ, Lip, GY, Franco, OH, Hofman, A, et al. Projections on the number of individuals with atrial fibrillation in the European Union, from 2000 to 2060. Eur Heart J. (2013) 34:2746–51. doi: 10.1093/eurheartj/eht280
5. Wańkowicz, P, Nowacki, P, and Gołąb-Janowska, M. Atrial fibrillation risk factors in patients with ischemic stroke. Arch Med Sci. (2021) 17:19–24. doi: 10.5114/aoms.2019.84212
6. Lip, GY. The ABC pathway: an integrated approach to improve AF management. Nat Rev Cardiol. (2017) 14:627–8. doi: 10.1038/nrcardio.2017.153
7. Jaberinezhad, M, Farhoudi, M, Nejadghaderi, SA, Alizadeh, M, Sullman, MJM, Carson-Chahhoud, K, et al. The burden of stroke and its attributable risk factors in the Middle East and North Africa region, 1990–2019. Sci Rep. (2022) 12:2700. doi: 10.1038/s41598-022-06418-x
8. Aref, H, El Nahas, N, Alrukn, SA, Khan, M, Kesraoui, S, Alnidawi, F, et al. Stroke services in MENA: what is there and what is needed. PLoS One. (2023) 18:e0288030. doi: 10.1371/journal.pone.0288030
9. Al Hashmi, AM, Shuaib, A, Imam, Y, Amr, D, Humaidan, H, Al Nidawi, F, et al. Stroke services in the Middle East and adjacent region: a survey of 34 hospital-based stroke services. Front Neurol. (2022) 13:1016376. doi: 10.3389/fneur.2022.1016376
10. January, CT, Wann, LS, Alpert, JS, Calkins, H, Cigarroa, JE, Cleveland, JC, et al. AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and the Heart Rhythm Society. J Am Coll Cardiol. (2014) 64:e1–e76. doi: 10.1161/CIR.0000000000000040
11. Sanders, GD, Lowenstern, A, Borre, E, Chatterjee, R, Goode, A, Sharan, L, et al. Stroke prevention in patients with atrial fibrillation: A systematic review update. Rockville (MD): Agency for Healthcare Research and Quality. (Comparative Effectiveness Reviews, No. 214.) (2018). Available at: https://www.ncbi.nlm.nih.gov/books/NBK534141/
12. Lip, GY, Nieuwlaat, R, Pisters, R, Lane, DA, and Crijns, HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. (2010) 137:263–72. doi: 10.1378/chest.09-1584
13. Wang, J, Zhang, D-P, Liu, HB, Zhong, JC, and Yang, XC. Should atrial fibrillation patients with hypertension as an additional risk factor of the CHA2DS2-VASc score receive oral anticoagulation? J Geriatr Cardiol. (2018) 15:229–34. doi: 10.11909/j.issn.1671-5411.2018.03.005
14. Fohtung, RB, and Rich, MW. Identification of patients at risk of stroke from atrial fibrillation. Risk. (2016) 5:6. doi: 10.15420/usc.2016:1:1
15. Paciaroni, M, Agnelli, G, Caso, V, Venti, M, Milia, P, Silvestrelli, G, et al. Atrial fibrillation in patients with first-ever stroke: frequency, antithrombotic treatment before the event and effect on clinical outcome. J Thromb Haemost. (2005) 3:1218–23. doi: 10.1111/j.1538-7836.2005.01344.x
16. Sposato, LA, Chaturvedi, S, Hsieh, C-Y, Morillo, CA, and Kamel, H. Atrial fibrillation detected after stroke and transient ischemic attack: a novel clinical concept challenging current views. Stroke. (2022) 53:e94–e103. doi: 10.1161/STROKEAHA.121.034777
17. Hammoudeh, A, Khader, Y, Tabbalat, R, Badaineh, Y, Kadri, N, Shawer, H, et al. One-year clinical outcome in middle eastern patients with atrial fibrillation: the Jordan atrial fibrillation (JoFib) study. J Vasc Med. (2022) 2022. doi: 10.2139/ssrn.4028720
18. Christiansen, CB, Gerds, TA, Olesen, JB, Kristensen, SL, Lamberts, M, Lip, GY, et al. Atrial fibrillation and risk of stroke: a nationwide cohort study. Europace. (2016) 18:1689–97. doi: 10.1093/europace/euv401
19. Alhaddad, Z, Hammoudeh, A, Khader, Y, and Alhaddad, IA. Demographics and risk profile of elderly middle eastern patients with atrial fibrillation: the Jordan atrial fibrillation (JoFib) study. Vasc Health Risk Manag. (2022) 18:289–95. doi: 10.2147/vhrm.s360822
20. Hammoudeh, AJ, Khader, Y, Kadri, N, Al-Mousa, E, Badaineh, Y, Habahbeh, L, et al. Adherence to the 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline on the use of oral anticoagulant agents in middle eastern patients with atrial fibrillation: the Jordan atrial fibrillation (JoFib) study. J Vasc Med. (2021) 2021:1–9. doi: 10.1155/2021/5515089
21. Pisters, R, Lane, DA, Nieuwlaat, R, de Vos, CB, Crijns, HJ, and Lip, GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the euro heart survey. Chest. (2010) 138:1093–100. doi: 10.1378/chest.10-0134
22. January, CT, Wann, LS, Calkins, H, Chen, LY, Cigarroa, JE, Cleveland, JC, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm Society. J Am Coll Cardiol. (2019) 74:104–32. doi: 10.1016/j.jacc.2019.01.011
23. Ibdah, R, Obeidat, O, Khader, Y, Al-Nusair, J, Abusurrah, O, Obeidat, A, et al. Validation of CHA2DS2 VASc score predictability of stroke and systemic embolization in a middle eastern population with AF: the Jordan atrial fibrillation (JoFib) study. Vasc Health Risk Manag. (2023) 19:255–64. doi: 10.2147/vhrm.S404575
24. January, CT, Wann, LS, Calkins, H, Chen, LY, Cigarroa, JE, Cleveland, JC Jr, et al. AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm Society in collaboration with the Society of Thoracic Surgeons. Circulation. (2019) 140:e125–51. doi: 10.1161/CIR.0000000000000665
25. Zubaid, M, Rashed, WA, Alsheikh-Ali, AA, Al-Zakwani, I, AlMahmeed, W, Shehab, A, et al. Management and 1-year outcomes of patients with atrial fibrillation in the Middle East: gulf survey of atrial fibrillation events. Angiology. (2015) 66:464–71. doi: 10.1177/0003319714536980
26. Healey, JS, Oldgren, J, Ezekowitz, M, Zhu, J, Pais, P, Wang, J, et al. Occurrence of death and stroke in patients in 47 countries 1 year after presenting with atrial fibrillation: a cohort study. Lancet. (2016) 388:1161–9. doi: 10.1016/S0140-6736(16)30968-0
27. Li, Y-G, Miyazawa, K, Wolff, A, Zubaid, M, Alsheikh-Ali, AA, Sulaiman, K, et al. One-year risks of stroke and mortality in patients with atrial fibrillation from different clinical settings: the Gulf SAFE registry and Darlington AF registry. Int J Cardiol. (2019) 274:158–62. doi: 10.1016/j.ijcard.2018.08.091
28. El-Hajj, M, Salameh, P, Rachidi, S, and Hosseini, H. The epidemiology of stroke in the Middle East. Eur Stroke J. (2016) 1:180–98. doi: 10.1177/2396987316654338
29. Imam, YZ, Kamran, S, Akhtar, N, Deleu, D, Singh, R, Malik, RA, et al. Incidence, clinical features and outcomes of atrial fibrillation and stroke in Qatar. Int J Stroke. (2020) 15:85–9. doi: 10.1177/1747493019830577
30. Al-Asadi, JN, and Habib, HA. Risk factors and 30-day case fatality of first-ever stroke in Basrah. Iraq Niger Med J. (2014) 55:209–13. doi: 10.4103/0300-1652.132041
31. Abdelnabi, M, Almaghraby, A, Saleh, Y, Özden Tok, Ö, Kemaloğlu Öz, T, Abdelkarim, O, et al. Frequency of de novo atrial fibrillation in patients presenting with acute ischemic cerebrovascular stroke. Egypt Heart J. (2020) 72:18. doi: 10.1186/s43044-020-00050-8
32. AlAmri, AS, AlShehri, AM, AlShammari, RZ, AlAmri, RA, AlMulhim, LA, and AlGhamdi, MF. Prevalence of atrial fibrillation among Saudi patients who had stroke: a retrospective cross-sectional study at a university hospital. Inte J Med Dev Count. (2022) 6:333–9. doi: 10.24911/IJMDC.51-1639698513
33. Sweileh, WM, Sawalha, AF, Al-Aqad, SM, Zyoud, SH, and Al-Jabi, SW. The epidemiology of stroke in northern Palestine: a 1-year, hospital-based study. J Stroke Cerebrovasc Dis. (2008) 17:406–11. doi: 10.1016/j.jstrokecerebrovasdis.2008.06.008
34. Zubaid, M, Rashed, WA, Alsheikh-Ali, AA, AlMahmeed, W, Shehab, A, Sulaiman, K, et al. Gulf survey of atrial fibrillation events (gulf SAFE). Circ Cardiovasc Qual Outcomes. (2011) 4:477–82. doi: 10.1161/CIRCOUTCOMES.110.959700
35. Ugowe, FE, Jackson, LR, and Thomas, KL. Atrial fibrillation and diabetes mellitus: Can we modify stroke risk through glycemic control. Am Heart Assoc. (2019) 12:e007351. doi: 10.1161/CIRCEP.119.007351
36. Collaboration ERF. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. (2010) 375:2215–22. doi: 10.1016/S0140-6736(10)60484-9
37. Rogers, PA, Bernard, ML, Madias, C, Thihalolipavan, S, Mark Estes, NA, and Morin, DP. Current evidence-based understanding of the epidemiology, prevention, and treatment of atrial fibrillation. Curr Probl Cardiol. (2018) 43:241–83. doi: 10.1016/j.cpcardiol.2017.06.001
38. Kornej, J, Börschel, CS, Benjamin, EJ, and Schnabel, RB. Epidemiology of atrial fibrillation in the 21st century. Circ Res. (2020) 127:4–20. doi: 10.1161/CIRCRESAHA.120.316340
39. Chung, S-C, Sofat, R, Acosta-Mena, D, Taylor, JA, Lambiase, PD, Casas, JP, et al. Atrial fibrillation epidemiology, disparity and healthcare contacts: a population-wide study of 5.6 million individuals. Lancet Reg Health Europe. (2021) 7:100157. doi: 10.1016/j.lanepe.2021.100157
40. She, R, Yan, Z, Hao, Y, Zhang, Z, Du, Y, Liang, Y, et al. Comorbidity in patients with first-ever ischemic stroke: disease patterns and their associations with cognitive and physical function. Frontiers in aging. Neuroscience. (2022) 14:14. doi: 10.3389/fnagi.2022.887032
41. Kamel, H, and Healey, JS. Cardioembolic stroke. Circ Res. (2017) 120:514–26. doi: 10.1161/CIRCRESAHA.116.308407
42. Elsheikh, S, Hill, A, Irving, G, Lip, GYH, and Abdul-Rahim, AH. Atrial fibrillation and stroke: state-of-the-art and future directions. Curr Probl Cardiol. (2024) 49:102181. doi: 10.1016/j.cpcardiol.2023.102181
43. Kamel, H, Okin, PM, Elkind, MSV, and Iadecola, C. Atrial fibrillation and mechanisms of stroke. Stroke. (2016) 47:895–900. doi: 10.1161/STROKEAHA.115.012004
44. Scheitz, JF, Nolte, CH, Doehner, W, Hachinski, V, and Endres, M. Stroke–heart syndrome: clinical presentation and underlying mechanisms. Lancet Neurol. (2018) 17:1109–20. doi: 10.1016/S1474-4422(18)30336-3
45. Cerasuolo, JO, Cipriano, LE, and Sposato, LA. The complexity of atrial fibrillation newly diagnosed after ischemic stroke and transient ischemic attack: advances and uncertainties. Curr Opin Neurol. (2017) 30:28–37. doi: 10.1097/wco.0000000000000410
46. Alvarado-Bolaños, A, Ayan, D, Khaw, AV, Mai, LM, Mandzia, JL, Bogiatzi, C, et al. Differences in stroke recurrence risk between atrial fibrillation detected on ECG and 14-day cardiac monitoring. Stroke. (2023) 54:2022–30. doi: 10.1161/STROKEAHA.123.043672
47. Sörös, P, and Hachinski, V. Cardiovascular and neurological causes of sudden death after ischaemic stroke. Lancet Neurol. (2012) 11:179–88. doi: 10.1016/s1474-4422(11)70291-5
48. Palareti, G, Legnani, C, Cosmi, B, Antonucci, E, Erba, N, Poli, D, et al. Comparison between different D-dimer cutoff values to assess the individual risk of recurrent venous thromboembolism: analysis of results obtained in the DULCIS study. Int J Lab Hematol. (2016) 38:42–9. doi: 10.1111/ijlh.12426
49. Cutugno, CL. Atrial fibrillation: updated management guidelines and nursing implications. Am J Nurs. (2015) 115:26–38. doi: 10.1097/01.NAJ.0000465028.05223.39
50. Nesheiwat, Z, Goyal, A, Jagtap, M, and Shammas, A. Atrial fibrillation (nursing). Stat pearls. Florida: Stat Pearls Publishing (2021).
51. Burn, J, Dennis, M, Bamford, J, Sandercock, P, Wade, D, and Warlow, C. Long-term risk of recurrent stroke after a first-ever stroke. Oxfordshire Commun Stroke Project. (1994) 25:333–7. doi: 10.1161/01.str.25.2.333
52. Hardie, K, Hankey, GJ, Jamrozik, K, Broadhurst, RJ, and Anderson, C. Ten-year risk of first recurrent stroke and disability after first-ever stroke in the Perth community stroke study. Stroke. (2004) 35:731–5. doi: 10.1161/01.Str.0000116183.50167.D9
53. Hardie, K, Jamrozik, K, Hankey, GJ, Broadhurst, RJ, and Anderson, C. Trends in five-year survival and risk of recurrent stroke after first-ever stroke in the Perth community stroke study. Cerebrovasc Dis. (2005) 19:179–85. doi: 10.1159/000083253
54. Barakat, M, Jirjees, F, Al-Obaidi, H, Hussain, K, El Hadidi, S, Mansour, S, et al. Factors associated with knowledge and awareness of stroke among the Jordanian population: a cross-sectional study. F1000Res. (2021) 10:1242. doi: 10.12688/f1000research.74492.2
55. Al-Obaidi, H, Khidhair, Z, Jirjees, F, Barakat, M, AlSalamat, H, Kharaba, Z, et al. Factors associated with knowledge and awareness of stroke in the Iraqi population: a cross-sectional study. Front Neurol. (2023) 14:14. doi: 10.3389/fneur.2023.1144481
56. Jirjees, F, Al-Obaidi, H, Barakat, M, Kharaba, Z, AlSalamat, H, Khidhair, Z, et al. Knowledge and awareness of stroke in the United Arab Emirates: a cross-sectional study of the general population. F1000Res. (2023) 12:1112. doi: 10.12688/f1000research.134328.2
57. Alzayer, R, Barakat, M, Jirjees, F, Alhamdan, A, Aloraifej, S, Cherri, S, et al. Knowledge and awareness of stroke and associated factors in the Saudi general population: a cross-sectional study. Front Neurol. (2023) 14:1225980. doi: 10.3389/fneur.2023.1225980
Keywords: atrial fibrillation, metabolic abnormalities, stroke risk, diabetes, Jordan
Citation: Al-Shatanawi TN, Alkouri O, Khader Y, ALSalamat H, Qaladi OA, Jarrah M, Ababneh A, Al-Awaisheh R, Zamil T and Hammoudeh A (2024) The one-year incidence of stroke in patients with atrial fibrillation in Jordan and its associated factors. Front. Med. 11:1408249. doi: 10.3389/fmed.2024.1408249
Edited by:
Mohamed F. Doheim, University of Pittsburgh Medical Center, United StatesReviewed by:
Francesco Cacciatore, University of Naples Federico II, ItalyAbdullah M. Al-Qudah, University of Pittsburgh Medical Center, United States
Mostafa Meshref, Al-Azhar University, Egypt
Copyright © 2024 Al-Shatanawi, Alkouri, Khader, ALSalamat, Qaladi, Jarrah, Ababneh, Al-Awaisheh, Zamil and Hammoudeh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tariq N. Al-Shatanawi, dGFsc2hhdGFuYXdpQGJhdS5lZHUuam8=
 Tariq N. Al-Shatanawi
Tariq N. Al-Shatanawi Osama Alkouri
Osama Alkouri Yousef Khader
Yousef Khader Husam ALSalamat
Husam ALSalamat Omar Aawadh Qaladi
Omar Aawadh Qaladi Mohamad Jarrah
Mohamad Jarrah Anas Ababneh2,6
Anas Ababneh2,6 Ayman Hammoudeh
Ayman Hammoudeh