- 1DARTNet Institute, Aurora, CO, United States
- 2Department of Family and Community Medicine, University of Toronto, Toronto, ON, Canada
- 3Ministry of Health of the Autonomous City of Buenos Aires, Buenos Aires, Argentina
- 4Department of Family Medicine and Primary Care, The University of Hong Kong-Shenzhen Hospital, Shenzhen, China
- 5Department of Family Medicine and Primary Care, School of Clinical Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China
- 6Research Unit for General Practice, NORCE Norwegian Research Centre AS, Bergen, Norway
- 7Center for Research in Primary Health Care (CINAPS), Universidad Peruana Cayetano Heredia, Lima, Peru
- 8North York General Hospital, Toronto, ON, Canada
- 9Department of General Practice and Primary Care, The University of Melbourne, Melbourne, VIC, Australia
- 10Division of Family Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
- 11School of Medical Sciences, Division of Diabetes, Endocrinology and Gastroenterology, University of Manchester, Manchester, United Kingdom
- 12Department of Public Health and Caring Sciences, Uppsala University, Uppsala, Sweden
- 13Centre for Epidemic Interventions Research, Norwegian Institute of Public Health, Oslo, Norway
- 14Department of General Practice, University of Oslo, Oslo, Norway
- 15Nuffield Department of Primary Care Health Sciences, University of Oxford, Oxford, United Kingdom
- 16National Centre for Emergency Primary Health Care, NORCE Norwegian Research Centre, Bergen, Norway
- 17Departments of Research and Innovation and Family Medicine-North York General Hospital, Toronto Western Family Health Team-University Health Network, Toronto, ON, Canada
Objectives: The majority of patients with respiratory illness are seen in primary care settings. Given COVID-19 is predominantly a respiratory illness, the INTernational ConsoRtium of Primary Care BIg Data Researchers (INTRePID), assessed the pandemic impact on primary care visits for respiratory illnesses.
Design: Definitions for respiratory illness types were agreed on collectively. Monthly visit counts with diagnosis were shared centrally for analysis.
Setting: Primary care settings in Argentina, Australia, Canada, China, Norway, Peru, Singapore, Sweden and the United States.
Participants: Over 38 million patients seen in primary care settings in INTRePID countries before and during the pandemic, from January 1st, 2018, to December 31st, 2021.
Main outcome measures: Relative change in the monthly mean number of visits before and after the onset of the pandemic for acute infectious respiratory disease visits including influenza, upper and lower respiratory tract infections and chronic respiratory disease visits including asthma, chronic obstructive pulmonary disease, respiratory allergies, and other respiratory diseases.
Results: INTRePID countries reported a marked decrease in the average monthly visits for respiratory illness. Changes in visits varied from −10.9% [95% confidence interval (CI): −33.1 to +11.3%] in Norway to −79.9% (95% CI: −86.4% to −73.4%) in China for acute infectious respiratory disease visits and − 2.1% (95% CI: −12.1 to +7.8%) in Peru to −59.9% (95% CI: −68.6% to −51.3%) in China for chronic respiratory illness visits. While seasonal variation in allergic respiratory illness continued during the pandemic, there was essentially no spike in influenza illness during the first 2 years of the pandemic.
Conclusion: The COVID-19 pandemic had a major impact on primary care visits for respiratory presentations. Primary care continued to provide services for respiratory illness, although there was a decrease in infectious illness during the COVID pandemic. Understanding the role of primary care may provide valuable information for COVID-19 recovery efforts and planning for future global emergencies.
1 Introduction
In the 3 years since the World Health Organization (WHO) declared COVID-19 a global pandemic, there have been over 659 million cases with over 6.5 million deaths worldwide (1, 2). The COVID-19 pandemic has presented unprecedented challenges to primary health care globally. Governments have implemented policies to prioritize using healthcare resources to treat COVID-19 patients and prevent the spread of the disease, such as quarantines, virtual work/school, wearing a mask, and social distancing. Although changes occurred rapidly in response to the COVID-19 pandemic (3), we have not yet determined the implications of these changes for other respiratory diseases. Numerous papers describe the potential and real impact of COVID-19 on primary care (4, 5). Huston et al. described the role of primary care in triaging and treating patients with COVID-19 in six well-resourced countries, including Australia, New Zealand, Canada, the Netherlands, the United Kingdom, and the United States (6). They discussed the negative impact of COVID-19 on access to primary care, the stress of decreased patient encounters on financial viability, and the capacity of primary care to respond to such a widespread pandemic. Research has identified socioeconomic disadvantage as an independent risk factor for death following a COVID-19 infection in individuals with type 2 diabetes (7) and those with other long-term conditions (8). There was wide variation in COVID-19 mortality rate between countries (9).
Upper respiratory illness is one of the most common diagnoses seen in primary care, accounting for 5–20% of ambulatory visits (10–13). Each year, in the United States alone, 20 million people with respiratory illnesses account for 64 million visits to primary care (14). Primary care serves over 90% of patients with lower respiratory illness or pneumonia. Since COVID-19 is predominantly a respiratory illness, primary care practices have been on the front lines of care for COVID-19 patients. Their role includes diagnosis, triage to the appropriate level of care, supportive care, treatments, and immunizations since they became available. While primary care has continued to provide in-person and virtual visits throughout the pandemic, the impact of COVID-19 on primary care visits for respiratory illness is unknown.
The INTernational ConsoRtium of Primary Care BIg Data Researchers (INTRePID) began as a collaboration between primary care researchers across the globe in response to the COVID-19 pandemic (15). INTRePID participants provide de-identified aggregated electronic data from electronic health records and billing claims data. Data are harmonized and analyzed centrally at the University of Toronto Department of Family and Community Medicine.
While respiratory infection is among the most common diagnoses in primary care, there is limited evidence of the impact of COVID-19 on respiratory illness care in primary care (12). The purpose of this paper is to describe the international experience of primary care practices related to respiratory illness before and during the COVID-19 pandemic.
2 Materials and methods
2.1 Study design
This study employed a retrospective observational design to investigate the impact of the COVID-19 pandemic on primary care visits for respiratory illnesses across 9 countries. The study period spanned from January 1, 2018, to December 31, 2021.
2.2 Data sources
Data for this study were gathered from diverse sources, including electronic medical records and billing claims. Specifically, information was sourced from visits to primary care physicians in Australia, Canada, China, Norway, Singapore, Sweden, and the United States. Moreover, data were obtained from primary care clinics in Argentina and Peru, encompassing visits to various healthcare providers within a primary care setting.
The dataset covers the period from January 1, 2018, to December 31, 2021, with the exception of Peru, where visit data was available only from January 2019. Although the onset of the pandemic varied across countries, for the purpose of this study, we defined the pre-pandemic period as January 2018 to March 2020, and the pandemic period as April 2020 to December 2021 in all countries except for China, where the pandemic was declared by the end of January 2020.
The representativeness of the data regarding primary care physician visits varied by country (Supplementary Table S1). Further detailed information about the INTRePID datasets can be found elsewhere, as described in prior publications (16, 17).
2.3 Primary outcome
The primary outcome was monthly visits for respiratory conditions across different countries, taking into account both virtual and in-person visits and categorizing them based on the type of respiratory condition, regardless of age, gender or other demographic factors. Virtual visits included video-calls and telephone consultations between patients and primary care physicians. Consultations associated with diagnostic codes for respiratory conditions were identified in each country and divided into eight groups: asthma, emphysema/chronic obstructive pulmonary disease (COPD), respiratory allergies, other respiratory diseases, lower respiratory tract infection (LRTI), upper respiratory tract infection (URTI), influenza and COVID-19. Because of variations in reporting, we use the general term influenza to include all reported influenza-like illnesses. COVID-19 includes both suspected and confirmed cases as some coding systems do not differentiate between the two. These groups were also combined to form two major categories, chronic respiratory diseases (asthma, COPD, respiratory allergies, other respiratory diseases) and infectious respiratory diseases (LRTI, URTI, influenza, COVID-19). Singapore data specific to COVID-19 were unavailable in the first year of the pandemic because they were recorded in a different system. See Supplementary Tables S2–S10 for a full description of diagnostic codes and description of the billing coding systems used for categorization in each of the countries.
2.4 Statistical analysis
We conducted an analysis to compare pre-pandemic and pandemic time periods to determine the impact of COVID-19 on primary care for each country. We calculated the difference between the average volume of respiratory monthly visits before and after the onset of the COVID-19 pandemic in each country, along with 95% confidence intervals (CI) and associated p-values using Welch’s t-test, with a significance level of 0.05. This statistical approach was chosen to account for potential variations in sample sizes and variances between the two time periods. Additionally, we computed the percent change in average monthly visits from pre-pandemic to pandemic, along with 95% CI, for all countries and conditions.
Accounting for the variation within the different studied groups, we calculated the standardized difference in means using Cohen’s d test with Hedges correction. This adjustment accounts for biases in small sample sizes. Cohen’s d is defined as the difference in means divided by an estimate of the pooled standard deviation and incorporates a correction factor based on the size of the samples being compared (18, 19).
Furthermore, we visually presented the proportion of respiratory visits as a percentage of total visits by respiratory condition and by modality (in-person vs. virtual). These visit rates were calculated using total monthly visits (of any reason) as denominators except in Sweden and Peru. For these countries, we used total coded visits as the denominator, as uncoded visits were more likely to be with other health-care providers and potentially occurred concomitantly with a visit to a primary care physician. We generated a plot illustrating the trends in respiratory visits throughout the studied timeframe, alongside a trendline representing the incidence of new COVID-19 cases per 100,000 population. The data points for this plot were extracted from https://ourworldindata.org/coronavirus (20).
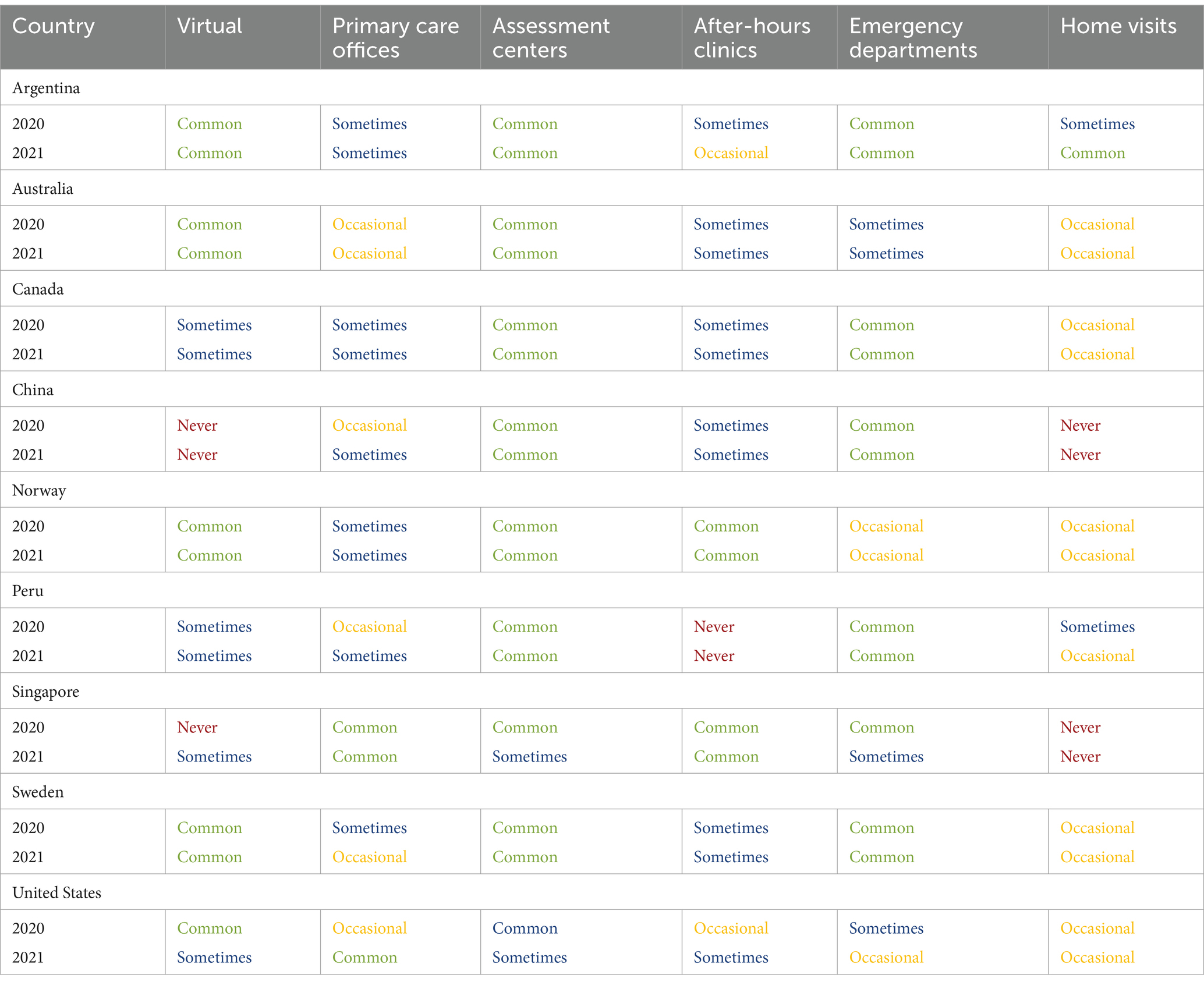
We supplemented our data analysis by conducting a survey among INTRePID collaborators, who served as points of contact in each country and were actively engaged in their local, regional, and national COVID response efforts. The survey aimed to describe the accessibility of care for patients with COVID-19 during the first and second years of the pandemic. Based on the framework developed by Huston et al. (6), which delineates the roles of various healthcare sectors in COVID-19 assessment, our survey employed a 5-point Likert scale offering respondents a range of options to indicate the frequency of occurrence for specific scenarios or activities related to COVID-19 care accessibility. Respondents could select from the following response options: “always,” “common,” “sometimes,” “occasionally,” and “never..” Refer to Supplementary Table S11 for a comprehensive description of the questionnaire employed.
2.5 Patient and public involvement
Patients and the public were not involved in the study design phase due to its highly technical nature; however, members of the public in INTRePID countries read the manuscript to ensure acceptable methods and interpretation. Specifically, the Patient and Clinician Engagement (PaCE) group, a well-established international patient advisory committee within the North American Primary Care Research Group (NAPCRG) (21), confirmed that our study was of public interest and offered important feedback on our results and discussion.
3 Results
For all INTRePID countries, when comparing the pandemic period with the pre-pandemic period, there was a decrease in infectious disease visits that was greater than the decrease observed for chronic respiratory illness visits (Figures 1, 2; Table 1). Decreases in the average number of monthly visits for acute infections ranged from −10.9% in Norway to −79.9% in China and were statistically significant in all countries (p = <0.05) except Norway. In Argentina and Norway, the reduction in acute respiratory infections was less pronounced because COVID-19 consultations contributed to almost half of these visits (Figure 3; Supplementary Figure S1). Decreases in chronic respiratory illness visits ranged from −2.1% to −59.9% and showed a statistically significant drop in China, Norway, Singapore, and the United States (Table 1; Figure 2). There was a drop in mean visit rates in all countries for most acute infectious respiratory conditions, with Singapore and the USA showing substantial declines in all sub-categories (Table 2; Supplementary Figure S2). Statistically significant changes in the average number of visits between the pandemic and pre-pandemic periods coincided with high standardized mean differences (exceeding 0.8 standard deviation units) (Tables 1, 2). It was interesting to note that in countries such as Canada, Norway, Peru, Sweden and in the US the patterns of respiratory condition visits in our primary care setting grossly mimicked the national COVID-19 waves (Figure 3).
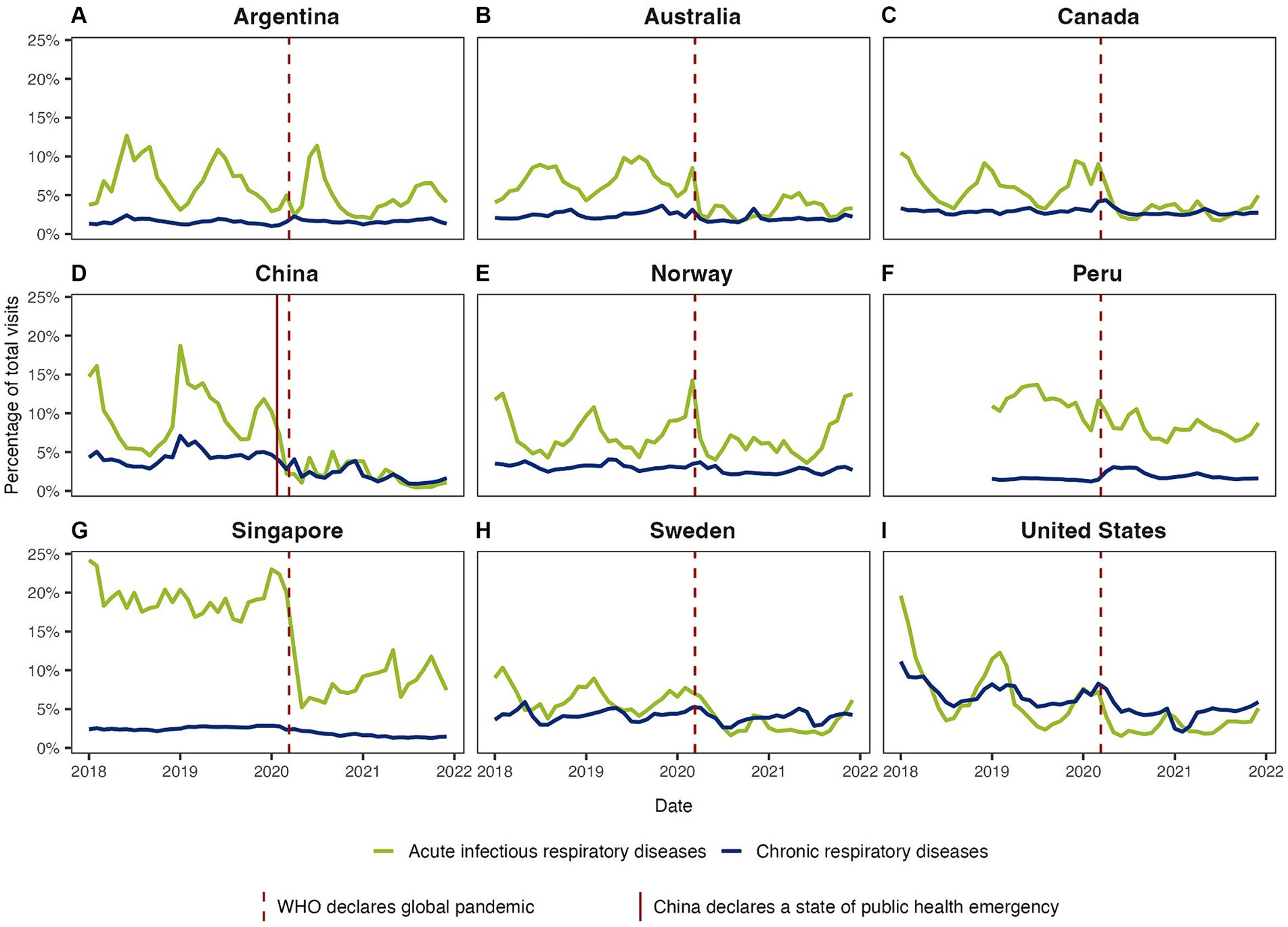
Figure 1. Overall visit rates for infectious and chronic respiratory illness during the pre-pandemic and pandemic periods in (A) Argentina, (B) Australia, (C) Canada, (D) China, (E) Norway, (F) Peru, (G) Singapore, (H) Sweden, and (I) United States. Trendlines show the monthly rates of respiratory visits over time. The rates were calculated by dividing the number of respiratory visits by the total visits to primary care services within each month and are expressed as percentages (%).
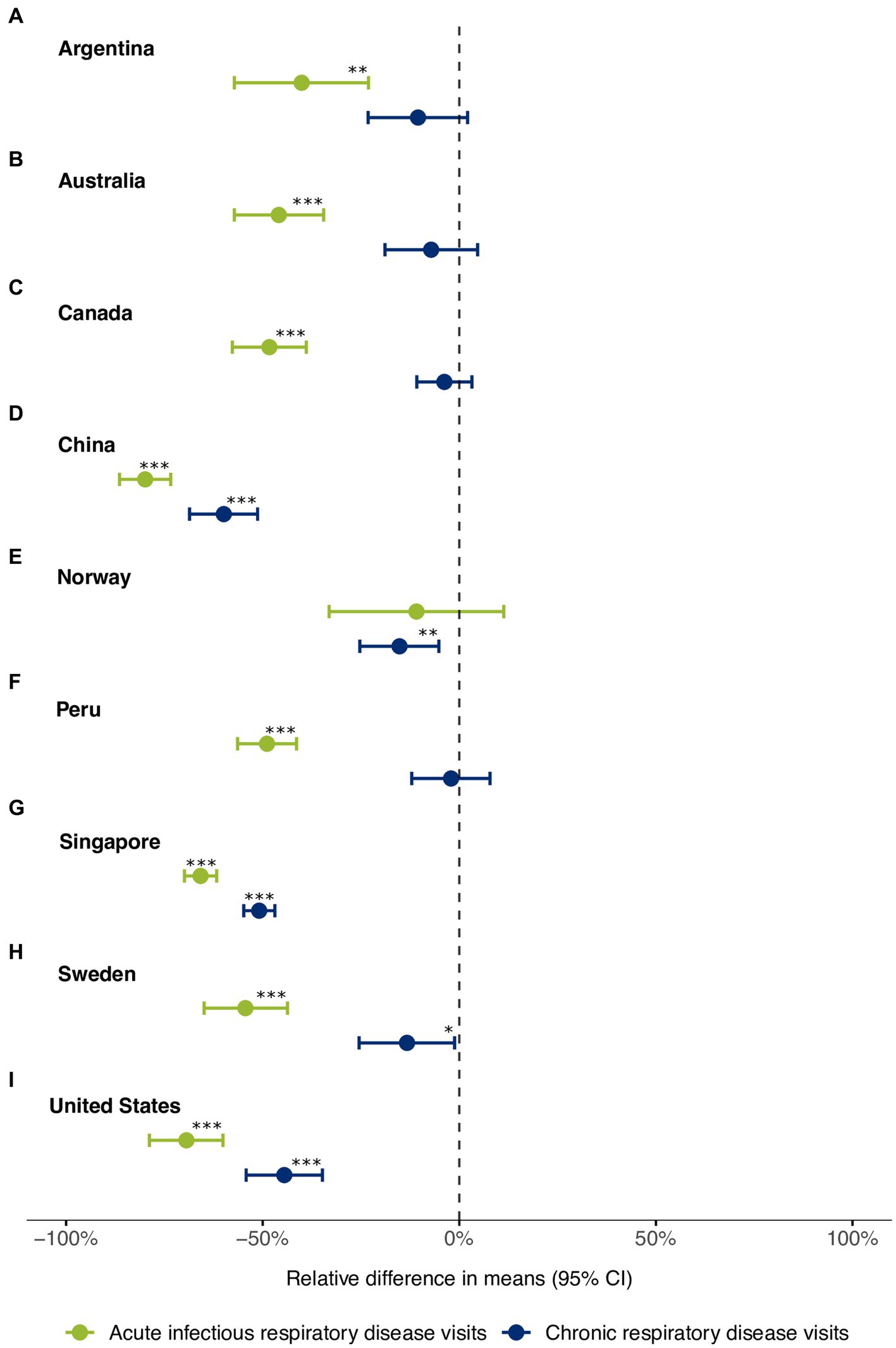
Figure 2. Relative difference in mean monthly visits for acute and chronic respiratory conditions between the pre-pandemic and the pandemic periods in (A) Argentina, (B) Australia, (C) Canada, (D) China, (E) Norway, (F) Peru, (G) Singapore, (H) Sweden, and (I) United States. Differences in mean monthly visits, 95% confidence intervals, and p-values were calculated using Welch’s t-test. The dots represent the relative difference in means between the two periods and are expressed as percentages (%). The error bars denote the 95% confidence intervals. Significance levels are indicated as follows: *p < 0.05; **p < 0.01; ***p < 0.001.
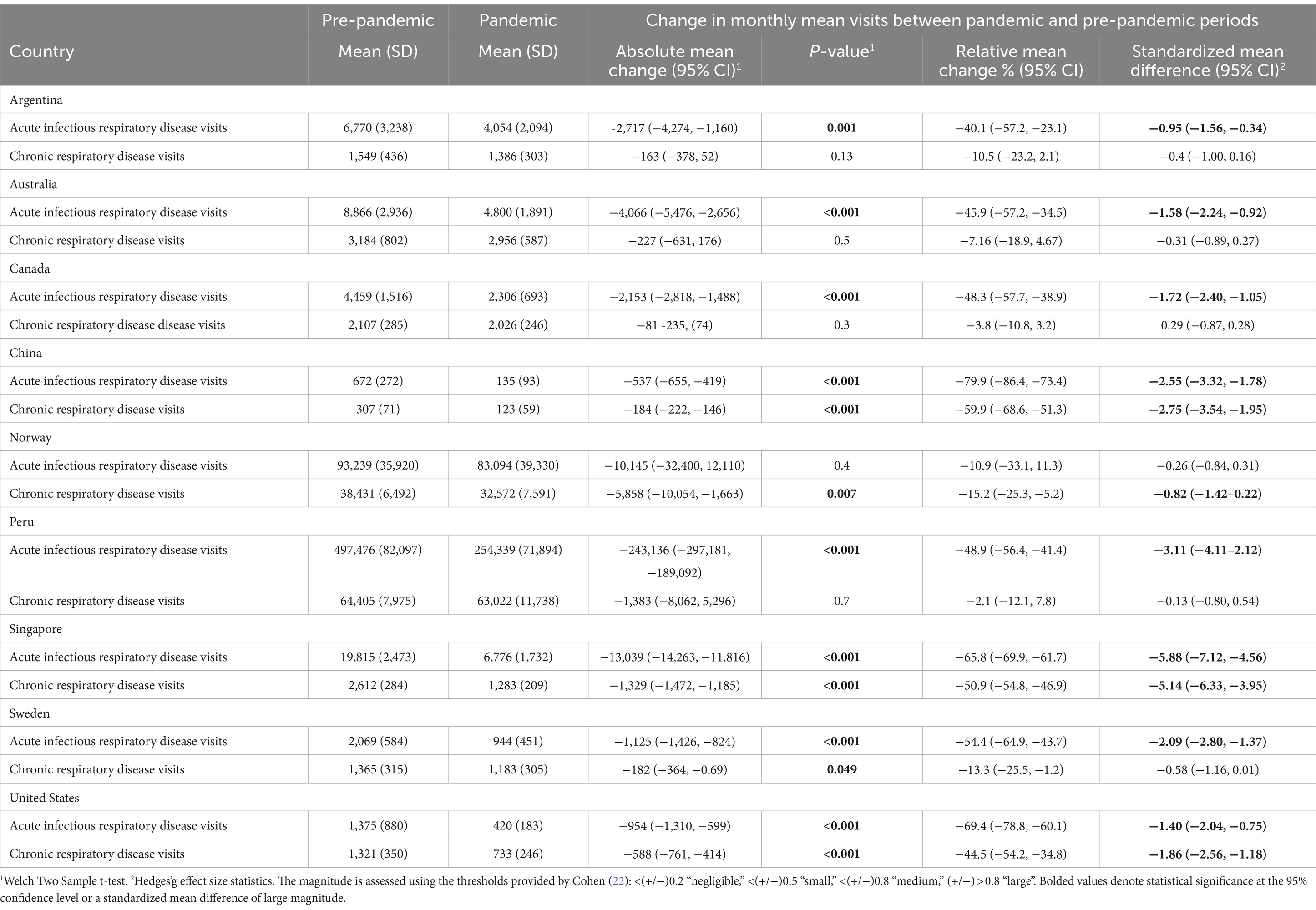
Table 1. Change in average monthly acute and chronic respiratory visits in the pre-pandemic and pandemic periods.
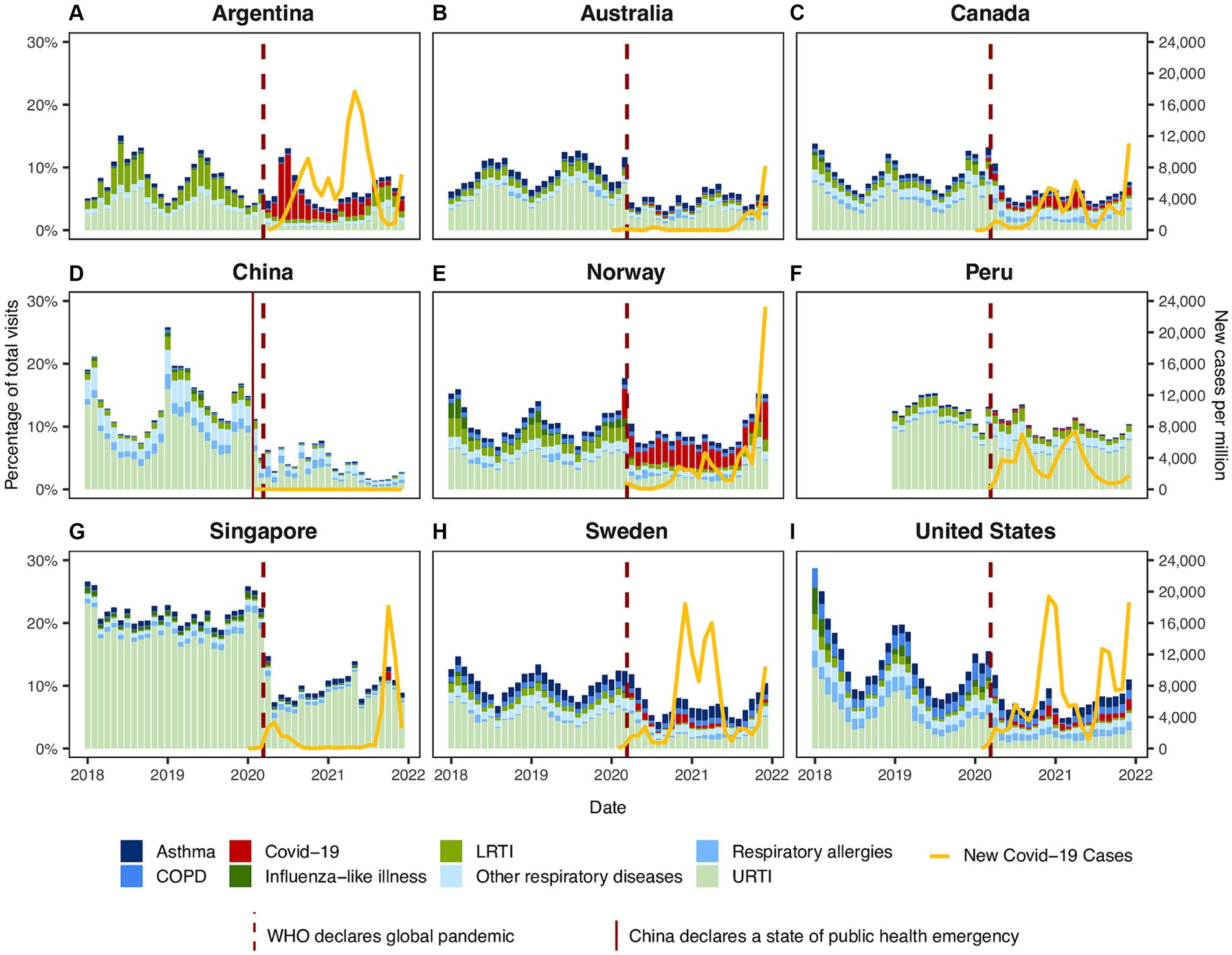
Figure 3. Respiratory visit rates by respiratory conditions in (A) Argentina, (B) Australia, (C) Canada, (D) China, (E) Norway, (F) Peru, (G) Singapore, (H) Sweden, and (I) United States. Stack column charts display monthly rates for different categories of respiratory visits. The rates were calculated by dividing the number of respiratory visits by the total visits to primary care services within each month and are expressed as percentages (%). The yellow line represents number of new COVID-19 cases per million. Source: https://ourworldindata.org/coronavirus (20).
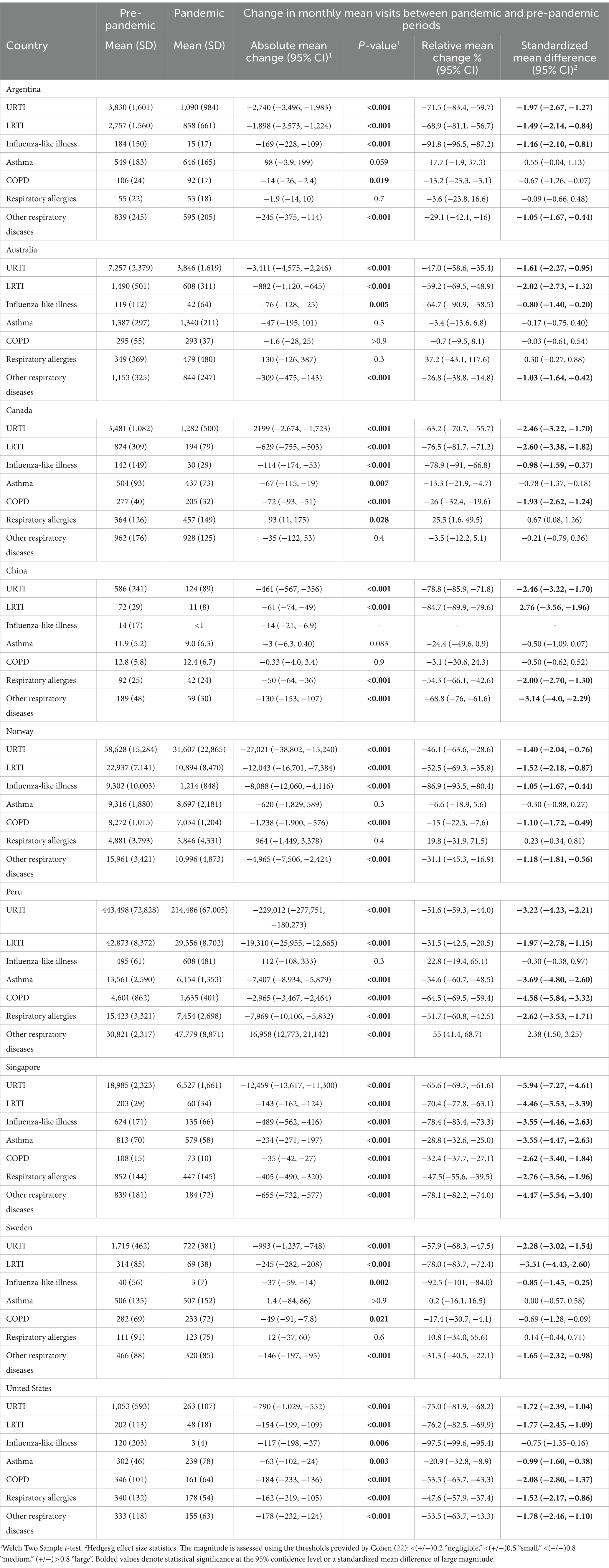
Table 2. Change in average monthly respiratory visits by category in the pre-pandemic and pandemic periods.
Most of the INTRePID countries reported less seasonal variation for infectious respiratory disease during the pandemic compared to the pre-pandemic period. Supplementary Figures S3–S10 show monthly rates of respiratory visits by category in each country. These data demonstrated no influenza spike during the first 2 years of the pandemic (Supplementary Figure S3). Similar to influenza, visits for other URTI declined across INTRePID countries (Supplementary Figure S4). As expected, with a decline in influenza, LRTIs, including pneumonia, decreased dramatically during the pandemic (Supplementary Figure S5).
Primary care visits for COVID-19 varied between the INTRePID countries with different fluctuations over time. Australia, China, Singapore, and Peru had few COVID-19 visits in primary care (0–1.3% of total visits). Conversely, Argentina and Norway reported large numbers of primary care COVID-19 visits accounting for 5.9–10.4% of visits. Canada, Sweden, and the United States had a moderate rate of COVID-19 visits accounting for 1.6–2.6% of all visits (Figure 3; Supplementary Figures S1, S6).
Seasonal variation for respiratory allergies continued throughout the pandemic (Supplementary Figure S7). COPD visits were fairly constant during the pandemic with slight variation. Norway, Canada, and the United States reported a modest decline in COPD visits, while the other countries were essentially unchanged (Supplementary Figure S8). Asthma visit rates showed little change during the pandemic (Supplementary Figure S9).
Virtual visits for respiratory conditions in Canada were more common than in-person visits. In Norway, virtual visit rates were comparable to in-person visit rates, while in other countries, virtual visit rates were either negligible or lower than in-person visits during the pandemic (Figure 4).
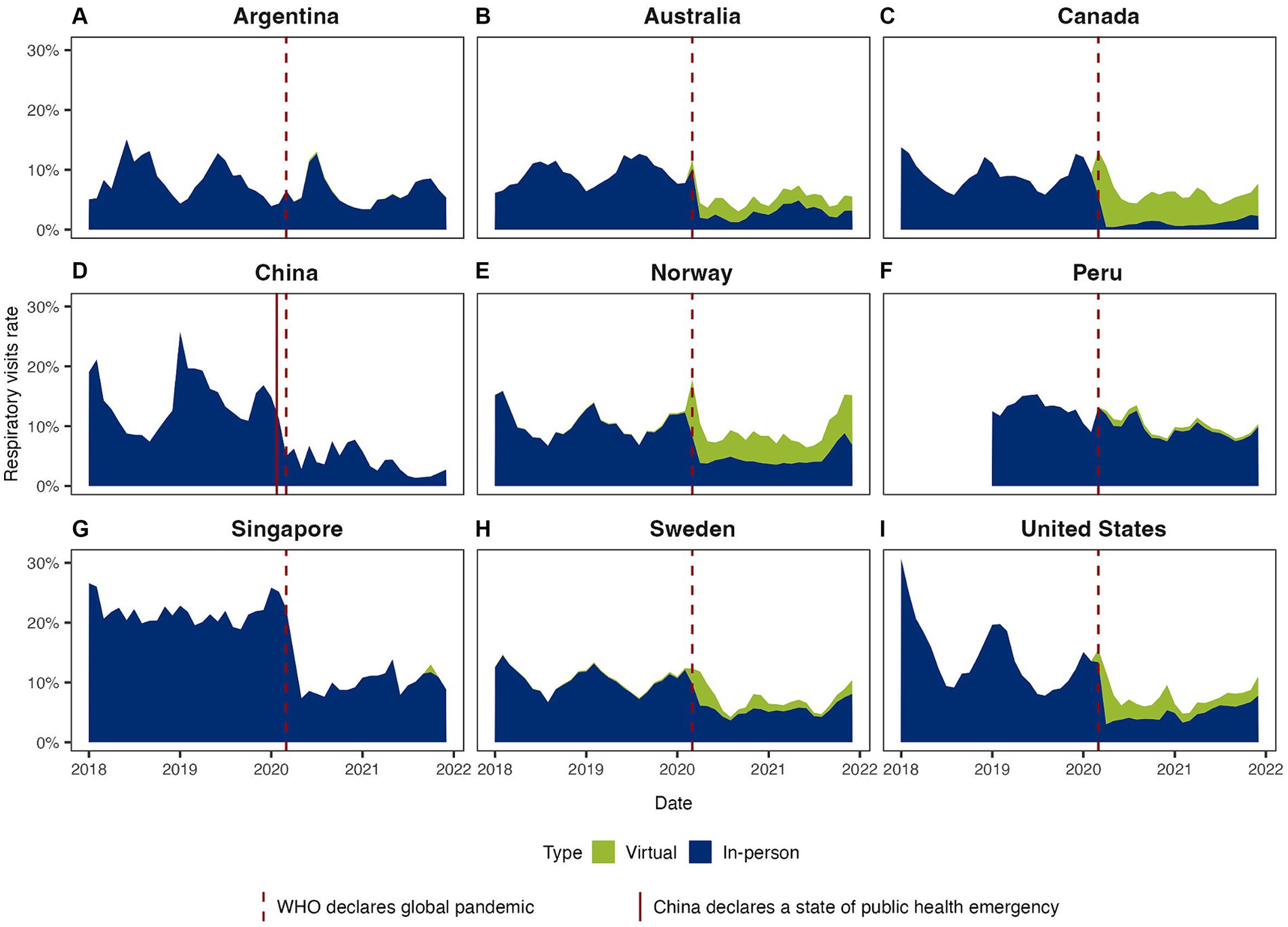
Figure 4. Respiratory visit rates by visit modality (virtual vs. in-person) in (A) Argentina, (B) Australia, (C) Canada, (D) China, (E) Norway, (F) Peru, (G) Singapore, (H) Sweden, and (I) United States. Area graphs illustrate respiratory visit rates by modality of care. The rates were calculated by dividing the number of respiratory visits by the total visits to primary care services within each month and are expressed as percentages (%).
The survey conducted among INTRePID representatives from participating countries revealed that assessment centers were the most frequent sites for COVID-19 diagnosis in both the first and second years of the pandemic (Table 3). Many countries mentioned emergency departments as sites for COVID-19 diagnosis, although their prevalence slightly decreased during the second year of the pandemic. Primary care settings occasionally served as sites for COVID-19 assessment, with a slight increase noted during 2021. In contrast, virtual visits were prevalent throughout the first two years of the pandemic. Table 3 summarizes the survey responses.
4 Discussion
4.1 Impact of COVID-19 pandemic on primary care visits for respiratory illnesses
Our study found a notable decline in the rate and average monthly volume of primary care visits for respiratory concerns following the onset of the COVID-19 pandemic. Acute respiratory infection visits experienced a more pronounced decrease compared to non-infectious chronic respiratory illness visits. This trend suggests that COVID-19 mitigation measures likely impacted infections such as influenza and URTIs, while chronic respiratory illnesses such as COPD and asthma were less amenable to these efforts. Predictably, COVID-19 had a lesser effect on seasonal respiratory illnesses such as allergies. Our findings align with existing research demonstrating a decrease in respiratory virus activity during the COVID-19 pandemic. This decline has been linked to reductions in cases of acute respiratory illnesses and influenza-like illnesses. Furthermore, studies have shown a positive impact on chronic respiratory diseases, with fewer hospital admissions for asthma and COPD exacerbations during the pandemic’s early stages, which coincides with the implementation of national lockdowns and non-pharmaceutical interventions (23).
The changes observed in non-infectious respiratory illnesses might stem from reduced access to in-person primary care or insufficient reporting of virtual visits not accounted for in the available data. Before COVID-19, only a few primary care practices conducted virtual visits, and there may have been delays in recording, coding, and reporting virtual visits during the early phase of the pandemic.
4.2 Regional variations in respiratory illness visits
While non-COVID-19 acute infection visits generally decreased, this change varied across countries participating in INTRePID. For example, respiratory illness accounted for 21.8% of visits in Singapore before the onset of the COVID-19 pandemic. This rate dropped below 10% of visits in the first few months of the pandemic and slowly levelled out at just over 10% of visits, with very few attributed to COVID-19. Prior to COVID-19, there was seasonal variation in Canada, with peaks near 15% of primary care visits attributed to respiratory illness. While there was an overall decrease in the rate of respiratory illness, it still hovered around 5%, with a significant number of COVID-19 patients. Our results were similar to those found in the United Kingdom, showing a marked decline in acute respiratory illness with flattening of seasonal variation while maintaining the usual incidence and seasonal variation associated with allergic rhinitis (24).
The variation in respiratory illness visits across countries also highlights differences in the location of COVID-19 infection care within our study population. Reflecting the diverse healthcare landscapes and pandemic responses globally, the dominant sites of COVID-19 care varied significantly. These variations encompass the dominant sites of COVID-19 care, including primary care versus other facilities, and align with the fluctuating waves of COVID-19 infections across the globe. Huston et al. studied the primary care and public health response to COVID-19 in 6 countries in early 2020 at the start of the pandemic (6). They found that COVID-19 assessment centers were the dominant location for triage of potential COVID-19 cases. In accordance with the Houston et al. study, neither their analysis nor our study identified primary care practices as the predominant COVID-19 testing and assessment locations in Australia, Canada, or the United States. Devi and colleagues reported that the majority of patients in their multi-country study had seen a health professional during the pandemic (63%) (25). This was even higher in Argentina, the only country that overlaps our research, which may explain the smaller drop in overall visit volume seen in this country.
4.3 Impact of COVID-19 pandemic on infectious respiratory illnesses
There is evidence that many infectious respiratory illnesses were much less common during the first 1–2 years of the COVID-19 pandemic (26, 27). Stephenson reported that while overall ambulatory visits dropped by just 5% between 2019 and 2020, the number of “common cold” visits dropped by 51% (3). Rodgers et al. reported that during the first few months of the pandemic, respiratory visits to the emergency department (ED) were twice the pre-pandemic rate; however, by the end of 2020, ED respiratory infections were below pre-pandemic rates (28). Liu et al. found lower rates of most respiratory pathogens among hospitalized children with lower respiratory tract infections (29). Lockdowns, social distancing, and mask mandates may have contributed to protection from COVID-19 (30, 31) and many other endemic and seasonal infections such as respiratory syncytial virus (RSV), influenza and other common rhino and adenoviruses (32, 33). The lower rate of respiratory infections seen among INTRePID participants may indicate the response to robust public health measures aimed at minimizing the spread of contagious illness. With the reduction in COVID-19 mitigation efforts in 2021, there was a resurgence in common respiratory infections (34, 35). Most recent evidence from December 2022 in the United States and Norway revealed major increases in RSV and influenza (36). Renati and Linder reported that a majority of acute respiratory infections may not require a clinical consultation (37). The additional fear of transmission and the restrictions in place in many healthcare settings may have been enough to keep patients with mild to moderate COVID-19 infection away from the clinic. Bullen et al., in a 9-country survey, found that 60% of physicians and pharmacists reported patient “reluctance to visit a healthcare setting.” (38).
Insights gained from previous pandemics provide crucial context for understanding the dynamics of viral interactions during outbreaks. For instance, the emergence of influenza A (H1N1) pandemic in 2009 had a significant impact on the circulation of other respiratory viruses between 2009 and 2011 (39). Studies observed unusual patterns in virus activity following the influenza A (H1N1) pandemic peak. Research conducted in France suggested a delay in the circulation of respiratory syncytial virus (RSV) during the 2009–2010 season, compared to previous years (40). Similarly, a study conducted in the United Kingdom found that some cases initially diagnosed as influenza during the summer outbreak were actually caused by other respiratory viruses (41). These findings underscore the interplay between dominant strains like the influenza A (H1N1) during the 2009 pandemic and other respiratory viruses. While our study focused on acute respiratory visits without examining the specific viruses involved, similar dynamics were observed during the COVID-19 pandemic (39).
4.4 Role of primary care in pandemic response
Goodyear-Smith and colleagues found that the perceived strength of the primary care system was not associated with a lower COVID-19 mortality rate (42). However, they also found that the perceived strength of a pandemic plan with robust implementation was associated with lower COVID-19 mortality. Local, regional, and national planning for COVID-19 recovery should also include planning for the management and resurgence of other respiratory infections. Primary care plays a crucial role in vaccination and may need to be part of post-pandemic immunization catchup and annual management (43, 44). Virtual visits may also play an important role in primary care and require further research to maximize their impact.
4.5 Limitations
This research comes with some limitations. First, we collected data from numerous sources with large variations in availability. While some INTRePID countries provided comprehensive national-level data, others provided limited data from a few clinics or regions. For instance, data from Peru (45) include over 8000 primary care practices, representing nearly 70% of the population. Data from smaller samples, such as those from China and the US, may not reflect the regional variation nor the national experience in primary care. Also, the usage of country names to define the regions is primarily for clarity and comprehension purposes rather than a direct comparison between the entire country populations. However, we have at least in part achieved a global footprint in relation to the sampling frame.
Our aim was not necessarily to compare countries to each other but rather to compare pre-pandemic with COVID-19 pandemic time periods among the participating INTRePID countries. We present unadjusted analyses as social and demographic variables were not available among all participant data. As many countries managed COVID-19 outside of the typical primary care setting, the COVID-19-related visits presented here reflect the impact on and role of primary care in the typical primary care settings rather than the full impact of COVID-19 in the community.
Moreover, primary care physicians staffed COVID-19 assessment clinics established outside the conventional primary care settings in numerous INTRePID countries. However, the visit rates for these patients were not accounted for in our data, except in Norway.
Another limitation arises from the reliance on coding systems themselves. For instance, due to the emergence of COVID-19 as a new diagnosis, some coding systems did not differentiate between suspected and confirmed cases. Unfortunately, this limitation in data availability prevented us from making a stratified analysis of suspected and confirmed cases. However, given the widespread epidemic nature of COVID-19, in the midst of a local wave, it is likely that most suspected cases were true COVID-19 infections.
We acknowledge that COVID-19-related visits to primary care do not reflect COVID-19 cases or death rates (20). The results presented in this study do not represent the impact of the global COVID-19 pandemic on primary care. We show the impact of the pandemic within each of the participant countries and particular regions involved.
Telehealth virtual visits are a safe and effective alternative to in-person clinic visits (14). While it has limitations, such as the inability to perform physical exams (46), it allows for efficient triage, effective symptom assessment, and the provision of timely medical advice, especially during times when in-person visits were restricted. Many primary care practices increased their use of virtual telehealth visits throughout the COVID-19 pandemic, particularly in the first year of the pandemic. While the INTRePID data included in-person as well as virtual visits, the rapid shift to virtual visits may not have generated a full encounter in the medical record or billing number in some countries, resulting in a loss of primary care practice visit data. Virtual visits, particularly early in the pandemic, may have been audio only and did not generate a full encounter in some countries’ medical or billing records.
5 Conclusion
The COVID-19 pandemic resulted in a major impact on primary care visits and reasons for visits. As expected from widespread physical distancing and mask mandates, there was a decreased rate of respiratory illness presentation in primary care after the start of the pandemic. INTRePID countries exhibited substantial variations. Primary care in all countries continued to provide service, in-person and through virtual telehealth consultation, for respiratory conditions as well as other health needs. Primary care is pivotal in epidemic and pandemic infection management. Understanding the role of primary care may provide valuable information for COVID-19 recovery efforts and planning for future global pandemic emergencies.
5.1 Implications for future research
Future research should explore the long-term impact of the pandemic on primary care utilization patterns and healthcare delivery. Further investigation into the effectiveness of virtual visits and strategies to address the underreporting of encounters is warranted. Moreover, understanding the interplay between pandemic response measures and the resurgence of respiratory infections will inform future public health interventions and pandemic preparedness efforts. This study also identifies the urgent need to consider methods to harmonize and curate data from various sources as a method to conduct robust international primary care research.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: All relevant data is contained within the article. The original contributions presented in the study are included in the article and supplementary files, further inquiries can be directed to the corresponding author. However, data sharing is governed by local regulations, which differ across countries. Individual-level data is not accessible to the public due to research ethics approval restrictions. Analytic code for data analysis is available upon request. Requests to access these datasets should be directed to ay50dUB1dG9yb250by5jYQ==.
Ethics statement
The studies involving humans were approved by this study received Research Ethics Board approval from the University of Toronto #40943. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
JW: Conceptualization, Investigation, Methodology, Visualization, Writing – original draft. AB: Conceptualization, Formal analysis, Investigation, Methodology, Writing – review & editing. ML: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – review & editing. PZ: Data curation, Investigation, Validation, Writing – review & editing. WW: Data curation, Investigation, Validation, Writing – review & editing. KW: Data curation, Investigation, Validation, Writing – review & editing. WP: Data curation, Investigation, Validation, Writing – review & editing. JS-V: Data curation, Investigation, Validation, Writing – review & editing. LS: Data curation, Investigation, Validation, Writing – original draft. AN: Data curation, Investigation, Validation, Writing – review & editing. J-AM-N: Data curation, Investigation, Validation, Writing – review & editing. ZJL: Data curation, Investigation, Validation, Writing – review & editing. ZL: Data curation, Investigation, Validation, Writing – review & editing. AH: Conceptualization, Writing – review & editing. AL: Data curation, Investigation, Validation, Writing – review & editing. RK: Data curation, Investigation, Validation, Writing – review & editing. CH: Data curation, Investigation, Validation, Writing – review & editing. LG: Data curation, Investigation, Validation, Writing – review & editing. GG: Data curation, Investigation, Validation, Writing – review & editing. SF: Data curation, Investigation, Validation, Writing – review & editing. SL: Data curation, Investigation, Validation, Writing – review & editing. MC-F: Data curation, Investigation, Validation, Writing – review & editing. VB: Data curation, Investigation, Validation, Writing – review & editing. KT: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study received funding support from the Rathlyn Foundation Primary Care EMR Research and Discovery Fund.
Acknowledgments
Australian data were de-identified patient data from the Patron primary care data repository (extracted from consenting general practices), which has been created and is operated by the Department of General Practice, University of Melbourne (www.gp.unimelb.edu.au/datafordecisions). Norwegian data were provided from the project from ‘COVID-19 outbreak in Norway – Epidemiology, health care utilization and primary care management – CONOPRI’, supported by a grant from the Trond Mohn Foundation (Grant no. TMS2020TMT06). Thank you Sigurd Storehaug Arntzen, Data Analyst at the Norwegian Institute of Public Health, who helped in the collection of the data from Norway and; Weihui Yan, Research Assistant at the University of Hong Kong Shenzhen Hospital, who participated in the collection and analysis of the China data and Jemisha Apajee, Data Analyst at the University of Toronto who helped in the analysis of the data.
Conflict of interest
JW holds the position of Vice President and is employed by the DARTNet Institute, a non-profit organization specializing in primary care research. AB and ML work for the University of Toronto and part of their salary is supported by grants. WP has received grant funding from NIMCH, sits on the advisory board of AT Still Research Foundation, has stock in Moderna, Johnson and Johnson, Eli Lilly, Novo Nordisk, Styker, Amgen, Novartis, and Pfizer; and received supplies from Boehringer Ingelheim and AstraZeneca. RK teaches at the Swedish advanced training program in quality improvement and owns stocks in the Swedish healthcare company Ambea. SL is the director of the Royal College of General Practitioners (RCGP) Research and Surveillance Center (RSC) as part of his academic post at Oxford. He has received payment to his research group for health services and primary care research from the University of Oxford and the University of Surrey and a wide range of grant funding through his university for vaccine-related research from AstraZeneca, GSK, Sanofi, Segirus and Takeda. MC-F receives honoraria and stocks from the Peruvian Cayetano Heredia University (Universidad Peruana Cayetano Heredia). KT receives a Chair in Family and Community Medicine Research in Primary Care at UHN and a Research Scholar award from the Department of Family and Community University of Toronto. KT received grants from the following organizations in the past 3 years: The Canadian Institutes of Health Research, Rathlyn Foundation Primary Care EMR Research and Discovery Fund, College of Family Physicians of Canada/Foundation for Advancing Family Medicine/CMA Foundation Heart and Stroke Foundation of Ontario, Department of Defense United States of America, St. Michael’s Hospital Foundation, Ontario Health Data Platform First Movers Fund, Queen’s University CSPC Research Initiation Grant, Diabetes Canada, Heart and Stroke Foundation and Brain Canada Heart-Brain IMPACT Award, CANSSI ICES Data Access Grant, North York General Hospital Exploration Fund, CFPC Janus Grant. All funding sources were not involved in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and the decision to submit the article for publication. The researchers are all independent of funders, and KT, AB, ML had full access to all the data and authors from each country had full access to the country-specific data in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1343646/full#supplementary-material
References
1. Worldometer. COVID - Coronavirus Statistics - Worldometer. (2023). Available at: https://www.worldometers.info/coronavirus/ (Accessed November 16, 2023).
2. World Health Organization. Coronavirus disease 2019 (COVID-19): situation report, 73. (2020). Available at: https://www.who.int/publications/m/item/situation-report---73 (Accessed November 16, 2023).
3. Stephenson, E, Butt, DA, Gronsbell, J, Ji, C, O’Neill, B, Crampton, N, et al. Changes in the top 25 reasons for primary care visits during the COVID-19 pandemic in a high-COVID region of Canada. PLoS One. (2021) 16:e0255992. doi: 10.1371/journal.pone.0255992
4. Desborough, J, Dykgraaf, SH, Phillips, C, Wright, M, Maddox, R, Davis, S, et al. Lessons for the global primary care response to COVID-19: a rapid review of evidence from past epidemics. Fam Pract. (2021) 38:811–25. doi: 10.1093/fampra/cmaa142
5. Rawaf, S, Allen, LN, Stigler, FL, Kringos, D, Quezada Yamamoto, H, Van Weel, C, et al. Lessons on the COVID-19 pandemic, for and by primary care professionals worldwide. Eur J Gen Pract. (2020) 26:129–33. doi: 10.1080/13814788.2020.1820479
6. Huston, P, Campbell, J, Russell, G, Goodyear-Smith, F, Phillips, RL, Van Weel, C, et al. COVID-19 and primary care in six countries. BJGP Open. (2020) 4:1128. doi: 10.3399/bjgpopen20X101128
7. Heald, AH, Jenkins, DA, Williams, R, Sperrin, M, Mudaliar, RN, Syed, A, et al. Mortality in people with type 2 diabetes following SARS-CoV-2 infection: a population level analysis of potential risk factors. Diabetes Ther. (2022) 13:1037–51. doi: 10.1007/s13300-022-01259-3
8. McGowan, VJ, and Bambra, C. COVID-19 mortality and deprivation: pandemic, syndemic, and endemic health inequalities. Lancet Public Health. (2022) 7:e966–75. doi: 10.1016/S2468-2667(22)00223-7
9. Wang, H, Paulson, KR, Pease, SA, Watson, S, Comfort, H, Zheng, P, et al. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. Lancet. (2022) 399:1513–36. doi: 10.1016/S0140-6736(21)02796-3
10. Pace, WD. Seasonal variation in diagnoses and visits to family physicians. Ann Fam Med. (2004) 2:411–7. doi: 10.1370/afm.73
11. Binns, HJ, Lanier, D, Pace, WD, Galliher, JM, Ganiats, TG, Grey, M, et al. Describing primary care encounters: the primary care network survey and the National Ambulatory Medical Care Survey. Ann Fam Med. (2007) 5:39–47. doi: 10.1370/afm.620
12. Finley, CR, Chan, DS, Garrison, S, Korownyk, C, Kolber, MR, Campbell, S, et al. What are the most common conditions in primary care? Systematic review. Can Fam Physician. (2018) 64:832–40.
13. Wandell, P, Carlsson, AC, Wettermark, B, Lord, G, Cars, T, and Ljunggren, G. Most common diseases diagnosed in primary care in Stockholm, Sweden, in 2011. Fam Pract. (2013) 30:506–13. doi: 10.1093/fampra/cmt033
14. Westfall, JM, Jetty, A, Petterson, S, and Jabbarpour, Y. Site of care for COVID-19-like respiratory illnesses. J Am Board Fam Med. (2021) 34:S26–8. doi: 10.3122/jabfm.2021.S1.200204
15. INTRePID. About us. (2023). Available at: https://www.intrepidprimarycare.org/about-us (Accessed November 16, 2023).
16. INTRePID. Data sources. (2023). Available at: https://www.intrepidprimarycare.org/resources (Accessed November 16, 2023).
17. Silva-Valencia, J, Lapadula, C, Westfall, JM, Gaona, G, De Lusignan, S, Kristiansson, RS, et al. Effect of the COVID-19 pandemic on mental health visits in primary care: an interrupted time series analysis from nine INTRePID countries. eClinicalMedicine. (2024) 70:102533. doi: 10.1016/j.eclinm.2024.102533
18. Austin, PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commu Stat. (2009) 38:1228–34. doi: 10.1080/03610910902859574
19. Taylor, JM, and Alanazi, S. Cohen’s and hedges’ g. J Nurs Educ. (2023) 62:316–7. doi: 10.3928/01484834-20230415-02
20. Mathieu, E, Ritchie, H, Rodés-Guirao, L, Appel, C, Giattino, C, Hasell, J, et al. Coronavirus Pandemic (COVID-19). Our World in Data. (2020). Available at: https://ourworldindata.org/coronavirus (Accessed November 16, 2023).
21. Patient and Clinician Engagement Program. (2023). Available at: https://napcrg.org/programs/engagement-pace/patient-and-clinician-engagement-pace-program/ (Accessed November 16, 2023).
23. Chow, EJ, Uyeki, TM, and Chu, HY. The effects of the COVID-19 pandemic on community respiratory virus activity. Nat Rev Microbiol. (2023) 21:195–210. doi: 10.1038/s41579-022-00807-9
24. RCGP RSC Workload Observatory. (2023). Available at: https://orchid.phc.ox.ac.uk/surveillance/clinical-informatics/rcgp-rsc-workload-observatory (Accessed November 16, 2023).
25. Devi, R, Goodyear-Smith, F, Subramaniam, K, McCormack, J, Calder, A, Parag, V, et al. The impact of COVID-19 on the Care of Patients with Noncommunicable Diseases in low- and middle-income countries: an online survey of patient perspectives. J Patient Exp. (2021) 8:237437352110340. doi: 10.1177/23743735211034091
26. Sinha, P, Reifler, K, Rossi, M, and Sagar, M. Coronavirus disease 2019 mitigation strategies were associated with decreases in other respiratory virus infections. Open forum. Infect Dis. (2021) 8:ofab105. doi: 10.1093/ofid/ofab105
27. Redlberger-Fritz, M, Kundi, M, Aberle, SW, and Puchhammer-Stöckl, E. Significant impact of nationwide SARS-CoV-2 lockdown measures on the circulation of other respiratory virus infections in Austria. J Clin Virol. (2021) 137:104795. doi: 10.1016/j.jcv.2021.104795
28. Rodgers, L, Sheppard, M, Smith, A, Dietz, S, Jayanthi, P, Yuan, Y, et al. Changes in seasonal respiratory illnesses in the United States during the coronavirus disease 2019 (COVID-19) pandemic. Clin Infect Dis. (2021) 73:S110–7. doi: 10.1093/cid/ciab311
29. Liu, P, Xu, M, Cao, L, Su, L, Lu, L, Dong, N, et al. Impact of COVID-19 pandemic on the prevalence of respiratory viruses in children with lower respiratory tract infections in China. Virol J. (2021) 18:159. doi: 10.1186/s12985-021-01627-8
30. Bernal, JL, Sinnathamby, MA, Elgohari, S, Zhao, H, Obi, C, Coughlan, L, et al. The impact of social and physical distancing measures on COVID-19 activity in England: findings from a multi-tiered surveillance system. Eur Secur. (2021) 26:1062. doi: 10.2807/1560-7917.ES.2021.26.11.2001062
31. Heald, AH, Stedman, M, Tian, Z, Wu, P, and Fryer, AA. Modelling the impact of the mandatory use of face coverings on public transport and in retail outlets in the UK on COVID-19-related infections, hospital admissions and mortality. Int J Clin Pract. (2021) 75:e13768–8. doi: 10.1111/ijcp.13768
32. Oh, DY, Buda, S, Biere, B, Reiche, J, Schlosser, F, Duwe, S, et al. Trends in respiratory virus circulation following COVID-19-targeted nonpharmaceutical interventions in Germany, January - September 2020: analysis of national surveillance data. Lancet Reg Health Eur. (2021) 6:100112. doi: 10.1016/j.lanepe.2021.100112
33. Ullrich, A, Schranz, M, Rexroth, U, Hamouda, O, Schaade, L, Diercke, M, et al. Impact of the COVID-19 pandemic and associated non-pharmaceutical interventions on other notifiable infectious diseases in Germany: an analysis of national surveillance data during week 1–2016 – week 32–2020. Lancet Reg Health Eur. (2021) 6:100103. doi: 10.1016/j.lanepe.2021.100103
34. Amar, S, Avni, YS, O’Rourke, N, and Michael, T. Prevalence of common infectious diseases after COVID-19 vaccination and easing of pandemic restrictions in Israel. JAMA Netw Open. (2022) 5:e2146175. doi: 10.1001/jamanetworkopen.2021.46175
35. Foley, DA, Yeoh, DK, Minney-Smith, CA, Martin, AC, Mace, AO, Sikazwe, CT, et al. The Interseasonal resurgence of respiratory syncytial virus in Australian children following the reduction of coronavirus disease 2019–related public health measures. Clin Infect Dis. (2021) 73:e2829–30. doi: 10.1093/cid/ciaa1906
36. Walker, AS. Just How Bad Is the ‘Tripledemic’? (2022). Available at: https://www.nytimes.com/interactive/2022/12/16/us/covid-flu-rsv-tripledemic-data.html (Accessed November 16, 2023).
37. Renati, S, and Linder, JA. Necessity of office visits for acute respiratory infections in primary care. Fam Pract. (2016) 33:312–7. doi: 10.1093/fampra/cmw019
38. Bullen, C, McCormack, J, Calder, A, Parag, V, Subramaniam, K, Majumdar, A, et al. The impact of COVID-19 on the care of people living with noncommunicable diseases in low- and middle-income countries: an online survey of physicians and pharmacists in nine countries. Prim Health Care Res Dev. (2021) 22:e30. doi: 10.1017/S146342362100030X
39. Mak, GC, Wong, AH, Ho, WYY, and Lim, W. The impact of pandemic influenza a (H1N1) 2009 on the circulation of respiratory viruses 2009–2011. Influenza Other Respir Viruses. (2012) 6:e6–e10. doi: 10.1111/j.1750-2659.2011.00323.x
40. Casalegno, JS, Ottmann, M, Bouscambert-Duchamp, M, Valette, M, Morfin, F, and Lina, B. Impact of the 2009 influenza a(H1N1) pandemic wave on the pattern of hibernal respiratory virus epidemics, France, 2009. Euro Surveill. (2010) 15:19485. doi: 10.2807/ese.15.06.19485-en
41. Tanner, HE, Curran, MD, Boxall, EH, and Osman, H. Viral respiratory infections during the 2009 influenza a(H1N1) outbreak in the west midlands region. UK Epidemiol Infect. (2012) 140:1551–6. doi: 10.1017/S0950268811002251
42. Goodyear-Smith, F, Kinder, K, Mannie, C, Strydom, S, Bazemore, A, and Phillips, RL. Relationship between the perceived strength of countries’ primary care system and COVID-19 mortality: an international survey study. BJGP Open. (2020) 4:1129. doi: 10.3399/bjgpopen20X101129
43. Wilkinson, E, Jetty, A, Petterson, S, Jabbarpour, Y, and Westfall, JM. Primary Care’s historic role in vaccination and potential role in COVID-19 immunization programs. Ann Fam Med. (2021) 19:351–5. doi: 10.1370/afm.2679
44. Westfall, JM, Liaw, W, Griswold, K, Stange, K, Green, LA, Phillips, R, et al. Uniting public health and primary Care for Healthy Communities in the COVID-19 era and beyond. J Am Board Fam Med. (2021) 34:S203–9. doi: 10.3122/jabfm.2021.S1.200458
45. Carrillo-Larco, RM, Guzman-Vilca, WC, Leon-Velarde, F, Bernabe-Ortiz, A, Jimenez, MM, Penny, ME, et al. Peru – Progress in health and sciences in 200 years of independence. Lancet Reg Health Am. (2022) 7:100148. doi: 10.1016/j.lana.2021.100148
Keywords: COVID-19, acute respiratory illness, chronic respiratory illness, primary care, asthma, COPD, reason for visit, international comparison
Citation: Westfall JM, Bonilla AO, Lapadula MC, Zingoni PL, Wong WCW, Wensaas KA, Pace WD, Silva-Valencia J, Scattini LF, Ng APP, Manski-Nankervis J-A, Ling ZJ, Li Z, Heald AH, Laughlin A, Kristiansson RS, Hallinan CM, Goh LH, Gaona G, Flottorp S, de Lusignan S, Cuba-Fuentes MS, Baste V and Tu K (2024) Changes in primary care visits for respiratory illness during the COVID-19 pandemic: a multinational study by the International Consortium of Primary Care Big Data Researchers (INTRePID). Front. Med. 11:1343646. doi: 10.3389/fmed.2024.1343646
Edited by:
Ozgur Karcioglu, University of Health Sciences (Turkey), TürkiyeReviewed by:
Hasan Bayram, Koç University, TürkiyeAlma Nurtazina, Semey State Medical University, Kazakhstan
Karthik Gnanapandithan, Mayo Clinic Florida, United States
Copyright © 2024 Westfall, Bonilla, Lapadula, Zingoni, Wong, Wensaas, Pace, Silva-Valencia, Scattini, Ng, Manski-Nankervis, Ling, Li, Heald, Laughlin, Kristiansson, Hallinan, Goh, Gaona, Flottorp, de Lusignan, Cuba-Fuentes, Baste and Tu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Karen Tu, ay50dUB1dG9yb250by5jYQ==
 John M. Westfall
John M. Westfall Angela Ortigoza Bonilla
Angela Ortigoza Bonilla María C. Lapadula
María C. Lapadula Paula L. Zingoni3
Paula L. Zingoni3 William C. W. Wong
William C. W. Wong Javier Silva-Valencia
Javier Silva-Valencia Jo-Anne Manski-Nankervis
Jo-Anne Manski-Nankervis Adrian H. Heald
Adrian H. Heald Christine M. Hallinan
Christine M. Hallinan Gabriela Gaona
Gabriela Gaona Signe Flottorp
Signe Flottorp Simon de Lusignan
Simon de Lusignan María S. Cuba-Fuentes
María S. Cuba-Fuentes Valborg Baste
Valborg Baste Karen Tu
Karen Tu on behalf of INTRePID
on behalf of INTRePID