
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 17 April 2024
Sec. Intensive Care Medicine and Anesthesiology
Volume 11 - 2024 | https://doi.org/10.3389/fmed.2024.1325358
 Amina Abdulmelik1
Amina Abdulmelik1 Mebratu Tila1*
Mebratu Tila1* Takele Tekilu2
Takele Tekilu2 Ashebir Debalkie1
Ashebir Debalkie1 Elias Habtu1
Elias Habtu1 Ashagrie Sintayehu1
Ashagrie Sintayehu1 Getahun Dendir1
Getahun Dendir1 Naol Gordie1
Naol Gordie1 Abel Daniel3
Abel Daniel3 Mohammed Suleiman Obsa4
Mohammed Suleiman Obsa4Background: Intraoperative cardiac complications are a common cause of morbidity and mortality in non-cardiac surgery. The risk of these complications increased with the average age increasing from 65. In a resource-limited setting, including our study area, the magnitude and associated factors of intraoperative cardiac complications have not been adequately investigated. The aim of this study was to assess the magnitude and associated factors of intraoperative cardiac complications among geriatric patients undergoing non-cardiac surgery.
Methods: An institutional-based multi-center cross-sectional study was conducted on 304 geriatric patients at governmental hospitals in the southern region of Ethiopia, from 20 March 2022 to 25 August 2022. Data were collected by chart review and patient interviews. Epi Data version 4.6 and SPSS version 25 were used for analysis. The variables that had association (p < 0.25) were considered for multivariable logistic regression. A p value < 0.05 was considered significant for association.
Result: The overall prevalence of intraoperative cardiac complications was 24.3%. Preoperative ST-segment elevation adjusted odds ratio (AOR = 2.43, CI =2.06–3.67), history of hypertension (AOR = 3.42, CI =2.02–6.08), intraoperative hypoxia (AOR = 3.5, CI = 2.07–6.23), intraoperative hypotension (AOR = 6.2 9, CI =3.51–10.94), age > 85 years (AOR = 6.01, CI = 5.12–12.21), and anesthesia time > 3 h (AOR =2.27, CI = 2.0.2–18.25) were factors significantly associated with intraoperative cardiac complications.
Conclusion: The magnitude of intraoperative cardiac complications was high among geriatric patients who had undergone non-cardiac surgery. The independent risk factors of intraoperative cardiac complications for this population included age > 85, ST-segment elevation, perioperative hypertension (stage 3 with regular treatment), duration of anesthesia >3 h, intraoperative hypoxia, and intraoperative hypotension. Holistic preoperative evaluation, optimization optimal and perioperative care for preventing perioperative risk factors listed above, and knowing all possible risk factors are suggested to reduce the occurrence of complications.
Intraoperative cardiac complication (ICC) is defined as follows: any death, unless unequivocal non-cardiac cause can be established; non-fatal cardiac arrest (absence of cardiac rhythm or the presence of chaotic rhythm requiring any component of basic or advanced cardiac life support) and at least one of the ischemic symptoms (1). Intraoperative management of geriatric surgical patients is becoming an increasingly important component of surgical and anesthetic practice in the 21st century. With an average age of 65, the risk of cardiac complications is increasing (2).
A study of more than 100,000 patients, which included geriatric and non-cardiac surgical patients, showed that at least 30% of mortality during the surgical period was caused by cardiac complications. As a result, more than 3,600 patients die each year due to cardiac complications of non-cardiac surgery in the Netherlands alone (1).
ICC definition: If any of the following ICCs are present during the intraoperative period. These include congestive heart failure, non-fatal cardiac arrest, elevation or depression of the ST segment, and cardiac death (2).
According to the World Health Organization (WHO), most developed countries have accepted the chronological age of 65 years and above as a definition of the elderly. Although there are different ways to classify this population, some studies have classified elderly adults between the ages of 65 and 74 as “youngest-old,” those between ages 75 and 84 as “middle-aged,” and those over 85 as “oldest-old (3).”
Notably, cardiovascular events are relatively frequent in non-cardiac surgery, with an estimated prevalence of 1%–5% and intraoperative infarctions cause mortality in the range of 25%–40% (3).
Major non-cardiac surgery is associated with incidence of cardiac death between 0.5% and 1.5% and major cardiac complications between 2.0% and 3.5%. When applied to the European population, these figures translate into 150,000–250,000 life-threatening cardiac complications due to non-cardiac surgical procedures annually (4). The manifestations of intraoperative cardiac complications (ICC) are usually subtle; therefore, doctors discover perioperative myocardial infarction (PMI) very late, leading to a 30%–70% mortality rate. Despite decades of research on the prediction and prevention of cardiac events, the prevalence of ICC has remained constant, risk factors in the elderly may differ significantly from those in the general population, and the prevalence of ICC remains elevated (5, 6). Major cardiac complications associated with abdominal and non-cardiac thoracic surgery are a common cause of mortality and serious morbidity in elderly patients (3, 7). The oldest age group underwent the smallest range of procedures; hip fracture, hip replacement, and cataract procedures comprised greater than 35% of all surgeries. Mortality and complications were increased in the geriatric compared with younger adults (5).
In general, elderly people face chronic illnesses that have risk of intraoperative cardiac complications. According to ICD-9 codes 375–449, cardiac death was identified as the leading cause of death as indicated on the patient’s death certificate (8, 9). A study of more than 100,000 patients, which included geriatric and non-cardiac surgical patients, showed that at least 30% of mortality during the surgical period was caused by cardiac complications. As a result, more than 3,600 patients die each year of cardiac complications of non-cardiac surgery in the Netherlands alone (10). Intraoperative mortality occurred in 1,877 (1.7%) patients and cardiovascular mortality in 543 (0.5%) cases. The study also enrolled 3,893 surgical patients, of whom 136 (3.5%) had intraoperative cardiac death. The study enrolled 8,351 patients undergoing non-cardiac surgery, Intraoperative mortality occurred in 226 patients (2.7%), of whom 133 (1.6%) suffered cardiovascular death (11).
Hypertension and diabetes are common diseases that result in cardiac morbidity and mortality. At the same time, major surgical procedures are being performed on elderly patients with increasing frequency. The risk of heart complications increases as one’s age approaches 65 years. Several studies have described the association between cardiac morbidity and mortality in patients undergoing non-cardiac surgery, but few data are available to guide preoperative risk stratification. In addition, these studies fail to address the question the factors associated with intraoperative cardiac morbidity and mortality (12).
Despite advances in patient management, morbidity and mortality secondary to ICC remain significantly high in developed countries, including the United States. In a resource-limited setting such as Ethiopia, including our study area, the magnitude and associated factors of ICC have not been adequately investigated.
Most studies on this topic did not include common associated factors that are included in this study, such as preoperative coexisting disease. Therefore, this study will fill the gap and have a positive impact on identifying associated factors that were not included in prior studies. In addition, some studies on current topics produced contradictory results and were unable to reach a consensus on the magnitude and associated factors, resulting in a longer length of stay, higher healthcare costs, and a worse prognosis. This might be a source of difficulty among health professionals in making decisions for geriatric patients undergoing non-cardiac surgery. Previous studies that were conducted on the ICC used retrospective data from a single institution with a small sample size, which was stated as a limitation in their study. To provide only preliminary data regarding intraoperative cardiac complications, this was multi-center study that used primary data. This will resolve the limitation. The findings of this study would help anesthesia professionals, physicians, and PACU nurses to know and provide optimal management during perioperative care. The aim of the current study was to assess the magnitude and associated factors of intraoperative cardiac complications among geriatric patients undergoing non-cardiac surgery.
This study was conducted at three selected public hospitals in the Southern Nation Nationality and People Region (SNNPR), Ethiopia, from 20 March 2022 to 25 August 2022. SNNPR is one of the largest regions in Ethiopia, accounting for more than 10% of the country’s land area and with an estimated population of 20,768,000 nearly a fifth of the country’s population. Administratively, the region is divided into 14 zones, 1 city administration, and 4 special districts. According to the regional health bureau’s annual report, there are 21 governmental hospitals (13).
Wolaita Sodo University Comprehensive and Specialized Hospital (WSUCSH) was established in 1920 E. C and is located in Wolaita Sodo town, 380 km south of Addis Ababa. It has served as a comprehensive and specialized since 2021, which delivers different medical services for outpatients, emergency operation rooms (OPD rooms), gynecology and obstetrics, and inpatients for approximately 450–500 patients per day for 24 h. The total service coverage of the hospital is approximately 3 million people in catchment areas (14).
Worabe Comprehensive and Specialized Hospital (WCSH) is located in the Site found in Zone, Southern Ethiopia in Worabe Town, which is located 172 km southwest of Addis Ababa, Ethiopia’s capital. It was established in 2014. It has 200 beds. The services in the hospital include outpatient department (OPD), inpatient, operation room gynecology and obstetrics, emergency, laboratory, pharmacy, and imaging services (15). Nigist Eleni Mohammed Memorial Referral Hospital (NEMMRH), Hadiya zone, Hosanna, Southern Ethiopia is located approximately 232 km southwest of Addis Ababa. The hospital was established in 1990. The hospital is well-equipped with medical equipment and staff. It has 9 wards and a total of 220 beds, including 8 and 7 beds in neonatal and adult ICUs (intensive care), respectively. The main health services in this hospital are inpatient, operation room, gynecology and obstetrics, and emergency and critical care (16).
An institution-based multi-center cross-sectional study design was employed.
The sample of 304 participants was determined using a single population formula for a finite population with assumptions of 95% CI, marginal error (d) = 5%, and prevalence (p) = 0.26.
Therefore, the sample size required is 295. By considering a 5% non-response rate, the total sample size is 304.
The proportional allocation of sample size was applied to hospitals using last year’s performance report for the randomly selected hospital. Here, hospitals serve as strata; the patients, wherever they appear, are similar regarding the surgical procedures being performed, the level of health professionals, and hospital facilities, so no design effect was used. Patients over 65 years of age who had an electrocardiogram performed per institutional guidelines, ASA I and ASA II, and elective surgeries were included. Vascular surgery, eye surgery intraoperative lidocaine infiltration, or more during the same hospitalization were excluded from the study.
We pretest 5% of sample size on Hawassa Comprehensive Specialized Hospital. Two MSc students of advanced clinical anesthesia and two MSc advanced clinical anesthesia were at the end of surgery by chart reviewing using structured data collection tool. Preoperative ECGs were analyzed a using the Minnesota Codes, to determine evidence of myocardial infarction (MI) and other ECG abnormalities in patients undergoing surgery in a standardized fashion. Utilising preoperative risk factors according to Lee’s Revised Cardiac Risk Index (RCRI for Pre-Operative Risk), patients with comorbidities were predefined (17), and the patients were determined according to the number of comorbidities such as ischemic heart disease, CHF, and insulin use. Patients were deemed to have ischemic heart disease if they had a history of MI, any history of angina pectoris, or cardiac chest pain. In addition, patients with a creatinine level of >2 mg/dL will be assessed for intraoperative cardiac complications (18). Intraoperative vital signs: Blood pressure and heart rate were recorded, and 6-lead ECG was performed.
Patients were assessed for any signs and symptoms of ICC including unstable angina, acute myocardial infarction (AMI), new-onset severe arrhythmia, heart failure (HF), non-fatal cardiac arrest, cardiac death, ST-segment elevation as major criteria and symptoms of ischemia such as chest pain or dyspnea, ECG changes indicating new ischemia, new ST-T changes bundle branch block, and new pathological Q waves on ECG (19).
The patient who developed one of the major criteria and at least one symptom of ischemic was considered an intraoperative cardiac complication.
The data were entered into Epi data version 4.6 before being transferred to SPSS version 25 for analysis. Depending on the distribution, categorical variables are displayed as number frequencies and percentages. Multicollinearity was tested using the coefficients’ covariance matrix, and VIF was checked. A binary logistic regression model was used. The variables that had association (p < 0.25) were entered and analyzed by a multivariable logistic regression model to identify the independent effect of different factors. Adjusted odds ratio (AOR) with a 95% CI was used to identify the strength of the association. Statistical significance was declared at a p-value of <0.05.
Outcome Measurement has been measured through clinical and intraoperative routine monitoring of blood pressure (BP), pulse rate, oxygen saturation (SpO2), and ECG changes.
ICC definition at least one of the following ICCs occurring intraoperative: cardiac death, non-fatal cardiac arrest, ST-segment elevation or depression; congestive heart failure (20).
Cardiac death: any death, unless an unequivocal non-cardiac cause could be established (18, 19, 21).
Adults between the ages of 65 and 74 years as the youngest-old, those between ages 75 and 84 years as middle-old, and those aged over 85 years as the oldest-old (22).
The institutional review board of Wolaita Sodo University, College of Health Science and Medicine, granted ethical clearance and approval under project number CHSM-ERC-03-12, reference number CRCD 82-02-14. An official letter of support and permission to conduct out the study was received from WSUCSH and other rest of the study area hospitals. Informed consent was obtained from the participants.
Of 304 geriatric patients, 100% were included in the analysis. Of the total patients included in the analysis, 52.6% and 47.4% were male and female patients, respectively. Most of the patients (71.7%) were aged between 75 and 84 years, and 22 (7.2%) of the study patients were obese with a BMI of over 30. The majority of the study population (60.2%) was from rural areas, and 33.6% of the study population was from WSUSCH. The demographic characteristics of the 304 patients are shown in Table 1.

Table 1. Socio-demographic factors of the study population at selected public hospitals in SSNPR, Ethiopia, from March 2022 to August 2022.
Among 304 geriatric patients undergoing elective non-cardiac surgery at selected SNNPR governmental hospitals in Ethiopia, the Overall magnitude of ICCs was 74 (24.3%) (Figure 1).
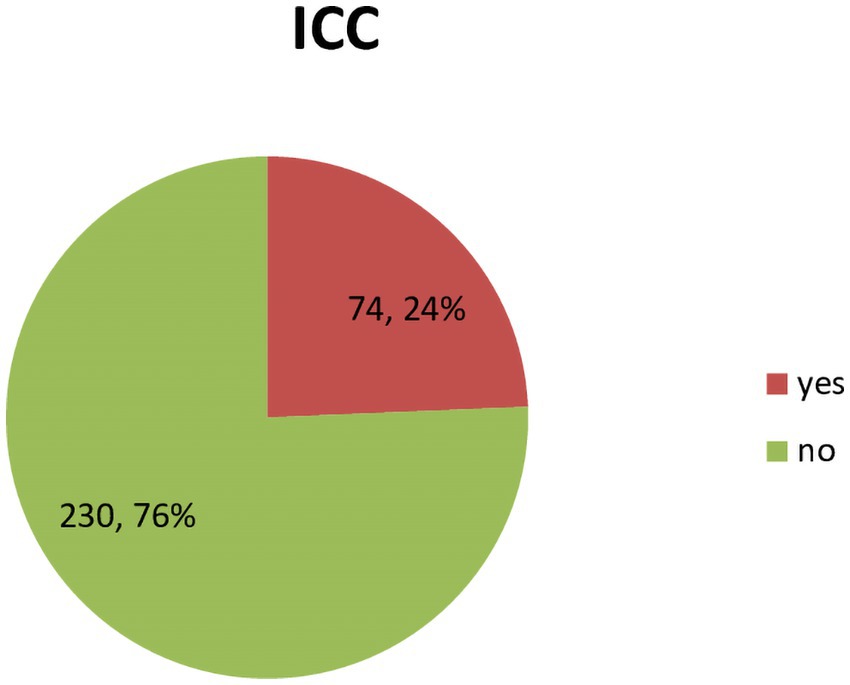
Figure 1. Overall magnitude of intraoperative cardiac complications at selected SNNPR governmental hospitals, from March 2022 to August 2022.
ICC complications occurred in 74 (24%) of the study population. Among patients who developed ICC, intraoperative ST abnormality on ECG was the major complication accounting for approximately30 (10.2%) (Figure 2).
Among patients who developed ICC, 92 (33.3%) had ischemic complications; in addition, intraoperative MI was 46 (15.1%; Table 2).
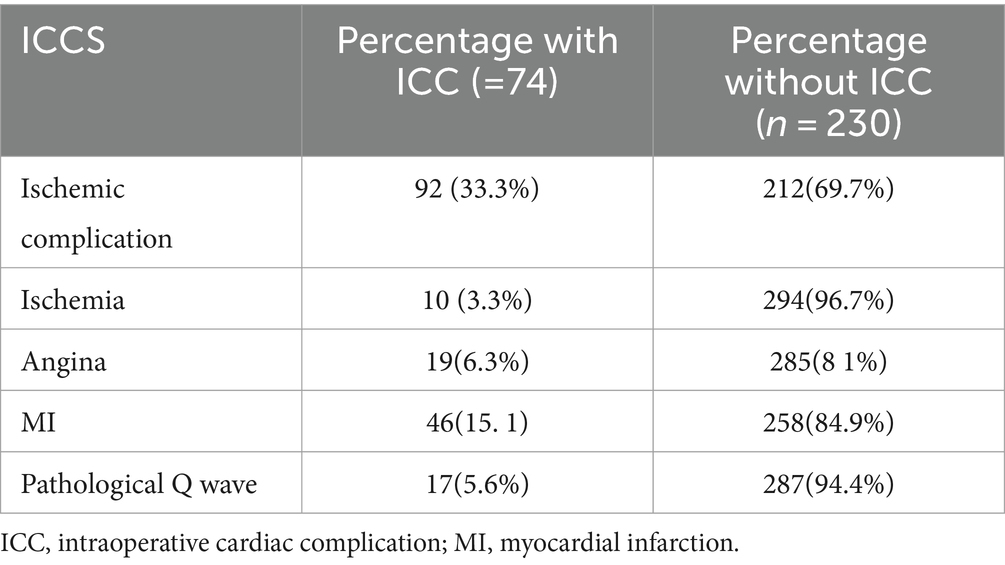
Table 2. Number of patients with ischemic complications at selected SNNPR governmental hospitals, from March 2022 to August 2022.
Output of binary logistic regression analysis finding: age, BMI, University of California and Los Angeles (UCL), ASA, history of hypertension, history of angina, and preoperative ECG abnormalities, as preoperative associated factors, are a potential candidate for the final model (with a p-value < 0.25). On the other hand, the Revised Cardiac Risk Index (RCRI), preoperative Hgb, history of HF, and preoperative creatinine did not show any association after binary logistic regression.
Intraoperative-associated factors that were a potential candidate for the final model (with a p-value of <0.25) after binary logistic regression analysis included intraoperative hypotension, type of surgery, duration of anesthesia, intraoperative hypoxia, and intraoperative blood loss. In contrast, the type of anesthesia used, type of surgery, maintenance agents, and intraoperative blood transfusion were not candidates for the final model after binary logistic regression analysis.
Factors associated with ICC were analyzed using binary logistic regression, and variables with a p-value of <0.25 were used in the model for final analysis. Accordingly, the output of the multiple logistic regression model revealed six independent factors: Patients aged >85 years were six times more likely to develop intraoperative cardiac complications when compared with patients aged 85 years (AOR = 6.01, CI = 5.12–12.21). The result indicates that patients who had a preoperative history of hypertension were more than three times more likely to develop intraoperative cardiac complications than those patients who had no history of hypertension (AOR =3.424, CI =2.02–6.080). The study showed that ST-segment abnormality was two times more likely to develop intraoperative cardiac complications when compared with other ECG findings (AOR = 2.433, CI = 2.06–3.67) (Figure 3; Table 3). Among intraoperative factors, intraoperative hypotension was identified as the strongest preoperative associated factor of ICC with [AOR of 6.20, CI = 6.20(3.5–110.9)]. A patient under anesthesia for more than 3 h was two times more likely to develop intraoperative cardiac complication compared to those patients under anesthesia for less than 3 h (AOR =2.27, CI = 2.0.2–18.25). The most significant preoperative related factors of ICC were found to be patients who experienced intraoperative hypoxia, as they were three times more likely to experience intraoperative cardiac problems than those who did not (AOR = 3.598, CI = 2.07–6.23) (Table 3).
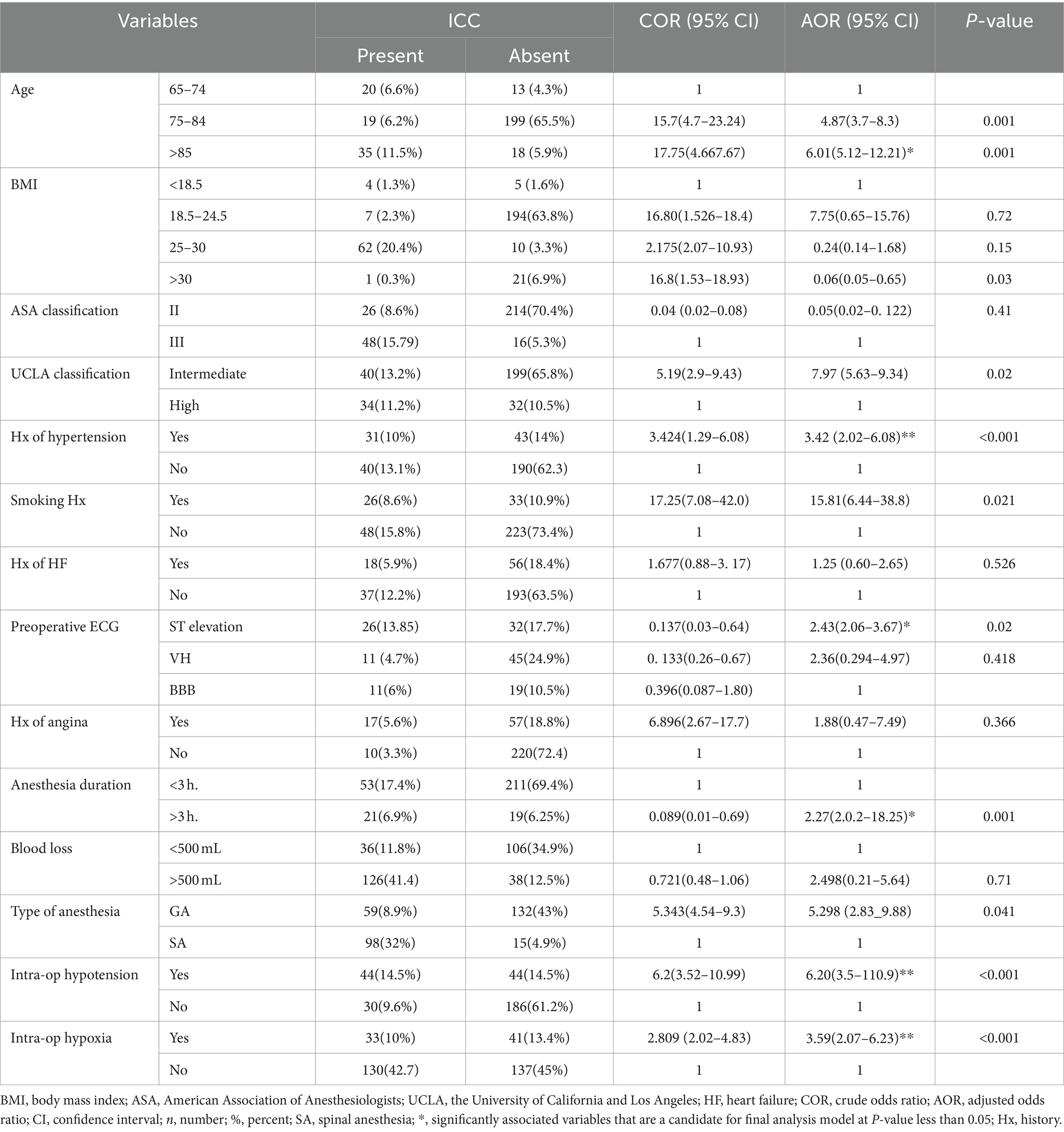
Table 3. Output of multiple logistic regression analysis showing independent predictors of ICC among surgical elective patients at governmental hospitals from March 2022 to August 2022.
One of the major challenges in the management of geriatric surgical patients is the prediction of intraoperative cardiac complications. In this study, the prevalence of intraoperative cardiac complications among elderly patients who underwent non-cardiac surgery was 24.3%.
Intraoperative ST abnormality on ECG was the major complication, accounting for approximately 30 (10.2%). In addition, 92 (33.3%) patients with ischemic complications and intraoperative MI accounted for 46 (15.1%). Age > 85 years, preoperative history of hypertension, ST-segment abnormality, intraoperative hypotension, patient under anesthesia for more than 3 h, and intraoperative hypoxia compared to the counterpart are the strongest perioperative factors associated with ICC. In most studies, the occurrence of ICC and intraoperative ischemic complications were more or less similar in frequency among geriatric populations (18, 23). This could be a result of interindividual differences in anesthetic management in terms of their preoperative assessment, intraoperative care, and management during surgery, which may also affect the severity of intraoperative cardiac problems.
The findings of this study are higher than the results of research conducted in university hospitals located in different regions of China (9.1%) and at Peking Union Medical College Hospital in China (19.4%) (14, 24). The findings of this study are also higher than the findings of the studies conducted in Europe, which were in the range of 0.5–3.5% ICC reported by various authors (25, 26). Poor surgical case selection, lack of progress in the preoperative management of cardiovascular risk factors and disease, and outdated surgical and anesthesia techniques used during surgery, including the inability to use minimally invasive surgical interventions that would shorten the duration of anesthesia, could all be contributing factors to the observed increase. Therefore, perioperative optimization and intraoperative best management together can reduce ICC.
In this study, age > 85 years was strongly associated with ICC, which agrees with previous studies conducted in Chinese in 2004 and 2017 (18, 27). Even though all subjects of this study were elderly, over 65 years of age, it was still associated factor of ICC. This might be because of age-related cardiovascular changes such as a decrease in number of cardiac myocytes, and the remaining myocytes undergo hypertrophy and a poor response to hemodynamic change, which can lead to ICC. Therefore, knowing physiological changes and avoiding intraoperative hemodynamic instability can help decrease ICC. However, the findings of current study disagree with the findings of the studies reported in most central and eastern European countries, including the USA (28, 29). In many central and eastern European countries, the mortality rates of geriatric patients have declined in those aged over 65 years. Significant variations exist and may be due to differences in the underlying disease, sociodemographic factors, and quality of care.
The present study indicates that preoperative ECG (ST abnormality) was positively associated with ICC. Similar to these studies, studies conducted in the Chinese population identified the significance of ST-segment abnormalities in addition to clinical characteristics as an independent risk factor for ICC (18, 30).
However, studies done in Asia and California’s San Francisco University reported ECG findings of LVH and BBB increased the odds of developing a subsequent intraoperative cardiac complication seven to nine times (31), which was not shown in this study. Similar controversy exists regarding the predictive value of ST-wave changes to ICC (17, 18). The study population (vascular verses general surgery), the Sokolow-Lyon verses Minnesota Code for LVH criteria, associated factors, and the age of patients enrolled may be reasons for variation from current study result. This finding suggests that evaluating preoperative ECG and intraoperative monitoring in geriatric patients undergoing non-cardiac surgery could be critical.
In this study, intraoperative hypoxia was positively associated with ICC. This might be because the mismatch between oxygen supply and demand and the catecholamine stress caused by pain, which increases the oxygen consumption of the heart, is the classic mechanism of ICC (12). The present finding is consistent with many previous studies (18, 24). This finding is also similar to the study that examined the electronic anesthetic records of 95,407 patients and discovered that the prevalence of intraoperative hypoxia was 6.8% (32). These findings indicate that a surprisingly high percentage of patients (10%) who had sustained hypoxemia during surgery developed ICC. However, the present finding disagrees with the finding of the study conducted at the University of California, San Francisco, which reported a low prevalence of hypoxia with a low association with ICC (30). The differences may be because the current study was conducted on participants with underlying different types of disease, whereas other studies were conducted only on patients with CVD.
There was a strong association between intraoperative hypotension and ICC found in this study, which can be explained by the higher risk of hypotension causing myocardial injury, myocardial infarction, and cardiogenic shock in patients undergoing non-cardiac surgery (33–35), which is consistent with the studies that provide evidence that hypotension is associated with a 36% increase in the risk of cardiovascular events, which causes decreases in both systemic vascular resistance and cardiac output, which results in cardiac complications (24, 36), but the findings of this study disagree with the findings of the study reported in China (18). This variation might be due to differences in the underlying disease and the quality of intraoperative management. Maintained preloading to the heart during surgery, anesthesia management, and provide adequate intravenous fluids can be satisfactory in most cases.
This study found that the duration of anesthesia (>3 h) was a significant factor associated with ICC. The justification could be that as time is prolonged, the increment of blood loss, anesthetic use, and hemodynamic instability can occur, which led the patient to have ICC. Several studies have hypothesized and reported associations between prolonged anesthesia time and cardiac complications (13, 37). However, the evidence for the duration of anesthesia and its influence on intraoperative cardiac complications remains poor, particularly in the surgical literature, which did not report it as an independent predictor of ICC (18, 30). The observed variation may be due to the differences in the advancement of surgical and anesthesia management in the study area, which significantly decrease the duration. Improving perioperative surgical and anesthesia management with available resources can minimize the duration of surgery.
This study also indicated stage 3 hypertension with regular treatment as associated factor of ICCs. Multiple studies have shown that not only is it safe to treat hypertension in geriatrics but also that it will decrease stroke, HF, myocardial infarction, and all other causes of mortality in non-cardiac surgery (25, 26). A study that enrolled 587 geriatric patients in America in the College of Cardiology and the Chinese population demonstrated that a history of hypertension requiring medication was a significant risk factor for developing cardiac complications (18, 38), but there are also legitimate concerns that tight BP control may increase the risk of hypotension in the geriatric population. Therefore, the combination of preoperative optimization and maintaining intraoperative hemodynamic stability can decrease ICC.
Several associated factors considered important by others were not show significance in our study, including a history of MI, gender, and classification of surgical risk (18). Furthermore, there was also no significant association seen between intra-operative blood loss of less than two units of blood and an ASA categorisation of greater than three (30). The reason for this difference could be that there were few patients with these diagnoses and most were successfully stabilized preoperatively, which could also be secondary to the difference in study population attributed to the optimization of patients before elective surgery and improvements in the surgical procedure. In general, the preoperative physical functional status according to RCRI is clinically very important/significant toward ICC, but in our study it is not statically significant.
Limited resources to print intraoperative ECG could make the interpretation more accurate.
There was an adequate sample size within the planned period as this was a multi-center study.
This study showed that intraoperative cardiac complications are common among geriatric patients who undergo non-cardiac surgery at SNNPR governmental hospitals. The associated factors of intraoperative cardiac complications for this population included age > 85 years, ST-segment elevation, perioperative hypertension (stage 3 with regular treatment), duration of anesthesia >3 h, Intraoperative hypoxia, and intraoperative hypotension.
Pre-surgical evaluation and prevention of intraoperative hypoxia and hypotension may help to reduce the number of intraoperative cardiac complications.
Healthcare providers including the anesthetist should be aware of all possible factors and develop a strateg1y to minimize the complication.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by College of Health Science WSU Ethical Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
AA: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing. MT: Formal analysis, Supervision, Writing – review & editing. TT: Investigation, Methodology, Validation, Writing – review & editing. ADe: Investigation, Software, Writing – review & editing. EH: Data curation, Investigation, Software, Writing – review & editing. AS: Formal analysis, Investigation, Writing – review & editing. GD: Formal analysis, Investigation, Methodology, Software, Writing – review & editing. NG: Data curation, Formal analysis, Investigation, Software, Writing – review & editing. ADa: Formal analysis, Software, Supervision, Writing – review & editing. MS: Formal analysis, Investigation, Methodology, Software, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research project was funded by the Wolaita Sodo University.
The authors would like to thank the Wolaita Sodo University College of Medicine and Health Science School of Anesthesia for giving them this wonderful opportunity to write this thesis.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could understood as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
BBB, Bundle Branch Block; BP, Blood Pressure; CAD, Coronary Arterial Disease; CHF, Congestive Heart Disease; CVD, Cardio Vascular Disease; ECG, Echocardiography; GA, General Anesthesia; ICC, Intraoperative Cardiac Complication; MACEs, Major Adverse Cardiac Events; MAP, Mean Arterial Pressure; NEMMRH, Nigist Eleni Mohammed Memorial Referral Hospital; NIBP, Non-Invasive Blood Pressure; POISE, Perioperative Ischemic Evaluation; RA, Regional Anesthesia; RCRI, Revised Cardiac Risk Index; WCSH, Worabe Comprehensive Specialized Hospital; WSUCSH, Wolaita Sodo university comprehensive specialized hospital.
1. Mohr, DN . Estimation of surgical risk in the elderly: a correlative review. J Am Geriatr Soc. (1983) 31:99–102.
2. Ramesh, B, Pillai, VS, Koshy, RC, and Jagathnath Krishna, KM. Role of preoperative investigations in elderly patients undergoing oncosurgical procedures–a retrospective review audit. J Anaesthesiol Clin Pharmacol. (2018) 34:535–9. doi: 10.4103/joacp.JOACP_147_17
3. Mohr, DN . Estimation of surgical risk in the elderly: a correlative review. J Am Geriatr Soc. (1983) 31:99–102. doi: 10.1111/j.1532-5415.1983.tb05421.x
4. Nyaaba, GN, Stronks, K, de-Graft Aikins, A, Kengne, AP, and Agyemang, C. Tracing Africa’s progress towards implementing the non-communicable diseases global action plan 2013–2020: a synthesis of WHO country profile reports. BMC Public Health. (2017) 17:1–13. doi: 10.1186/s12889-017-4199-6
5. Barnett, ML, Olenski, AR, and Jena, AB. Opioid-prescribing patterns of emergency physicians and risk of long-term use. N Engl J Med. (2017) 376:663–73. doi: 10.1056/NEJMsa1610524
6. Sirisaengchaikul, P, and Arunakul, I-O. Incidence of perioperative myocardial infarction in patients who underwent preoperative evaluation by internist for intermediate and high risk non-cardiac surgery. J Med Assoc Thail. (2017) 100:29.
7. Yu, Z, Jin, J, Tin, A, Köttgen, A, Yu, B, Chen, J, et al. Polygenic risk scores for kidney function and their associations with circulating proteome, and incident kidney diseases. J Am Soc Nephrol. (2021) 32:3161–73. doi: 10.1681/ASN.2020111599
8. Tegels, JJW, de Maat, MFG, Hulsewé, KWE, Hoofwijk, AGM, and Stoot, JHMB. Value of geriatric frailty and nutritional status assessment in predicting postoperative mortality in gastric cancer surgery. J Gastrointest Surg. (2014) 18:439–46. doi: 10.1007/s11605-013-2443-7
9. Alterovitz, SS, and Mendelsohn, GA. Relationship goals of middle-aged, young-old, and old-old internet daters: an analysis of online personal ads. J Aging Stud. (2013) 27:159–65. doi: 10.1016/j.jaging.2012.12.006
10. Mitsutake, S, Ishizaki, T, Teramoto, C, Shimizu, S, and Ito, H. Peer reviewed: patterns of co-occurrence of chronic disease among older adults in Tokyo, Japan. Prev Chronic Dis. (2019) 16:E11. doi: 10.5888/pcd16.180170
11. Eisenberg, MJ, London, MJ, Leung, JM, Browner, WS, Hollenberg, M, Tubau, JF, et al. Monitoring for myocardial ischemia during noncardiac surgery: a technology assessment of transesophageal echocardiography and 12-lead electrocardiography. JAMA. (1992) 268:210–6. doi: 10.1001/jama.1992.03490020058031
12. Weiser, TG, Haynes, AB, Molina, G, Lipsitz, SR, Esquivel, MM, Uribe-Leitz, T, et al. Size and distribution of the global volume of surgery in 2012. Bull World Health Organ. (2016) 94:201–209F. doi: 10.2471/BLT.15.159293
13. Phan, K, Kim, JS, Kim, JH, Somani, S, di’Capua, J, Dowdell, JE, et al. Anesthesia duration as an independent risk factor for early postoperative complications in adults undergoing elective ACDF. Glob Spine J. (2017) 7:727–34. doi: 10.1177/2192568217701105
14. Pacifico, J, Geerlings, MAJ, Reijnierse, EM, Phassouliotis, C, Lim, WK, and Maier, AB. Prevalence of sarcopenia as a comorbid disease: a systematic review and meta-analysis. Exp Gerontol. (2020) 131:110801. doi: 10.1016/j.exger.2019.110801
15. Štern, D, Payer, C, Giuliani, N, and Urschler, M. Automatic age estimation and majority age classification from multi-factorial MRI data. IEEE J Biomed Health Inform. (2018) 23:1392–403. doi: 10.1109/JBHI.2018.2869606
16. Li-wei, HL, Saeed, M, Talmor, D, Mark, R, Malhotra, A, et al. Methods of blood pressure measurement in the ICU. Crit Care Med. (2013) 41:34–40. doi: 10.1097/CCM.0b013e318265ea46
17. Raslau, D, Bierle, DM, Stephenson, CR, Mikhail, MA, Kebede, EB, and Mauck, KF. Preoperative cardiac risk assessment. Mayo Clin Proc. (2020) 95:1064–79. doi: 10.1016/j.mayocp.2019.08.013
18. Liu, Z, Xu, G, Xu, L, Zhang, Y, and Huang, Y. Perioperative cardiac complications in patients over 80 years of age with coronary artery disease undergoing noncardiac surgery: the incidence and risk factors. Clin Interv Aging. (2020) 15:1181–91. doi: 10.2147/CIA.S252160
19. Smilowitz, NR, Gupta, N, Ramakrishna, H, Guo, Y, Berger, JS, and Bangalore, S. Perioperative major adverse cardiovascular and cerebrovascular events associated with noncardiac surgery. JAMA Cardiol. (2017) 2:181–7. doi: 10.1001/jamacardio.2016.4792
20. Davies, A, Wellard-Cole, L, Rangan, A, and Allman-Farinelli, M. Validity of self-reported weight and height for BMI classification: a cross-sectional study among young adults. Nutrition. (2020) 71:110622. doi: 10.1016/j.nut.2019.110622
21. Costa, JR, Sousa, A, Moreira, AC, Costa, RA, Cano, M, Maldonado, G, et al. Incidence and predictors of very late (≥ 4 years) major cardiac adverse events in the DESIRE (drug-eluting stents in the real world)-late registry. J Am Coll Cardiol Intv. (2010) 3:12–8. doi: 10.1016/j.jcin.2009.10.022
22. Wondiye, K, Asseffa, NA, Gemebo, TD, and Astawesegn, FH. Predictors of undernutrition among the elderly in Sodo zuriya district Wolaita zone, Ethiopia. BMC Nutr. (2019) 5:1–7. doi: 10.1186/s40795-019-0320-9
23. Xu, L, Yu, C, Jiang, J, Zheng, H, Yao, S, Pei, L, et al. Major adverse cardiac events in elderly patients with coronary artery disease undergoing noncardiac surgery: a multicenter prospective study in China. Arch Gerontol Geriatr. (2015) 61:503–9. doi: 10.1016/j.archger.2015.07.006
24. Kouz, K, Hoppe, P, Briesenick, L, and Saugel, B. Intraoperative hypotension: pathophysiology, clinical relevance, and therapeutic approaches. Indian J Anaesth. (2020) 64:90–6. doi: 10.4103/ija.IJA_939_19
25. Devereaux, P, and Sessler, DI. Cardiac complications in patients undergoing major noncardiac surgery. N Engl J Med. (2015) 373:2258–69. doi: 10.1056/NEJMra1502824
26. Hammond, G, and Rich, MW. Hypertensive heart failure in the very old. Heart Fail Clin. (2019) 15:477–85. doi: 10.1016/j.hfc.2019.06.001
27. Liu, LL, Dzankic, S, and Leung, JM. Preoperative electrocardiogram abnormalities do not predict postoperative cardiac complications in geriatric surgical patients. J Am Geriatr Soc. (2002) 50:1186–91. doi: 10.1046/j.1532-5415.2002.t01-1-50303.x
28. Coetzee, E, Biccard, BM, Dyer, RA, Meyersfeld, ND, Chishala, C, and Mayosi, BM. Incidence of myocardial injury after non-cardiac surgery: experience at Groote Schuur hospital, Cape Town, South Africa. South Afr Med J. (2018) 108:408–12. doi: 10.7196/SAMJ.2018.v108i5.12784
29. Colebunders, R, Siewe Fodjo, JN, Vanham, G, and van den Bergh, R. A call for strengthened evidence on targeted, non-pharmaceutical interventions against COVID-19 for the protection of vulnerable individuals in sub-Saharan Africa. Int J Infect Dis. (2020) 99:482–4. doi: 10.1016/j.ijid.2020.08.060
30. Liu, ZJ, Yu, CH, Xu, L, Han, W, Jiang, JM, and Huang, YG. Risk factors for perioperative major cardiac events in Chinese elderly patients with coronary heart disease undergoing noncardiac surgery. Chin Med J. (2013) 126:3464–9. doi: 10.3760/cma.j.issn.0366-6999.20122793
31. van Klei, WA, Bryson, GL, Yang, H, Kalkman, CJ, Wells, GA, and Beattie, WS. The value of routine preoperative electrocardiography in predicting myocardial infarction after noncardiac surgery. Ann Surg. (2007) 246:165–70. doi: 10.1097/01.sla.0000261737.62514.63
32. Ehrenfeld, JM, Funk, LM, van Schalkwyk, J, Merry, AF, Sandberg, WS, and Gawande, A. The incidence of hypoxemia during surgery: evidence from two institutions. Can J Anaesth. (2010) 57:888–97. doi: 10.1007/s12630-010-9366-5
33. Angelousi, A, Girerd, N, Benetos, A, Frimat, L, Gautier, S, Weryha, G, et al. Association between orthostatic hypotension and cardiovascular risk, cerebrovascular risk, cognitive decline and falls as well as overall mortality: a systematic review and meta-analysis. J Hypertens. (2014) 32:1562–71. doi: 10.1097/HJH.0000000000000235
34. Admass, BA, Ego, BY, Tawye, HY, and Ahmed, SA. Preoperative investigations for elective surgical patients in a resource limited setting: systematic review. Ann Med Surg. (2022) 82:104777. doi: 10.1016/j.amsu.2022.104777
35. Nanayakkara, S, Marwick, TH, and Kaye, DM. The ageing heart: the systemic and coronary circulation. Heart. (2017) 104:370–6. doi: 10.1136/heartjnl-2017-312114
36. Vernooij, L, van Klei, WA, Machina, M, Pasma, W, Beattie, WS, and Peelen, LM. Different methods of modelling intraoperative hypotension and their association with postoperative complications in patients undergoing non-cardiac surgery. Br J Anaesth. (2018) 120:1080–9. doi: 10.1016/j.bja.2018.01.033
37. Pronovost, PJ, Goeschel, CA, and Wachter, RM. The wisdom and justice of not paying for “preventable complications”. JAMA. (2008) 299:2197–9. doi: 10.1001/jama.299.18.2197
Keywords: magnitude, associated factors, intraoperative, cardiac complications, geriatrics, non-cardiac surgery
Citation: Abdulmelik A, Tila M, Tekilu T, Debalkie A, Habtu E, Sintayehu A, Dendir G, Gordie N, Daniel A and Suleiman Obsa M (2024) Magnitude and associated factors of intraoperative cardiac complications among geriatric patients who undergo non-cardiac surgery at public hospitals in the southern region of Ethiopia: a multi-center cross-sectional study in 2022/2023. Front. Med. 11:1325358. doi: 10.3389/fmed.2024.1325358
Received: 21 October 2023; Accepted: 04 March 2024;
Published: 17 April 2024.
Edited by:
Marcos Ferreira Minicucci, São Paulo State University, BrazilReviewed by:
Panpan Fang, First Affiliated Hospital of Anhui Medical University, ChinaCopyright © 2024 Abdulmelik, Tila, Tekilu, Debalkie, Habtu, Sintayehu, Dendir, Gordie, Daniel and Suleiman Obsa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mebratu Tila, mebratutila@gmail.com
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.