
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Med. , 20 May 2024
Sec. Family Medicine and Primary Care
Volume 11 - 2024 | https://doi.org/10.3389/fmed.2024.1305190
This article is part of the Research Topic The Newer Paradigms in Hypertension Research and Management View all 10 articles
 Sonal J. Patil1*
Sonal J. Patil1* Vishwa Bhayani2
Vishwa Bhayani2 Yilin Yoshida3
Yilin Yoshida3 Leila Bushweller4
Leila Bushweller4 Eno-Obong Udoh4
Eno-Obong Udoh4 Irina Todorov5
Irina Todorov5 Robert Saper5
Robert Saper5 Kurt C. Stange6
Kurt C. Stange6 Shari Bolen7
Shari Bolen7Introduction: Lay advisor interventions improve hypertension outcomes; however, the added benefits and relevant factors for their widespread implementation into health systems are unknown. We performed a systematic review to: (1) summarize the benefits of adding lay advisors to interventions on hypertension outcomes, and (2) summarize factors associated with successful implementation in health systems using the Reach, Effectiveness, Adoption, Implementation, Maintenance (RE-AIM) framework.
Methods: We systematically searched several databases, including Ovid MEDLINE, CINAHL, PsycINFO from January 1981 to May 2023. All study designs of interventions delivered solely by lay advisors for adults with hypertension were eligible. If both arms received the lay advisor intervention, the study arm with lower intensity was assigned as the low-intensity intervention.
Results: We included 41 articles, of which 22 were RCTs, from 7,267 screened citations. Studies predominantly included socially disadvantaged populations. Meta-analysis (9 RCTs; n = 4,220) of eligible lay advisor interventions reporting outcomes showed improved systolic blood pressure (BP) [−3.72 mm Hg (CI –6.1 to −1.3; I2 88%)], and diastolic BP [−1.7 mm Hg (CI −1 to −0.9; I2 7%)] compared to control group. Pooled effect from six RCTs (n = 3,277) comparing high-intensity with low-intensity lay advisor interventions showed improved systolic BP of −3.6 mm Hg (CI –6.7 to −0.5; I2 82.7%) and improved diastolic BP of −2.1 mm Hg (CI –3.7 to −0.4; I2 70.9%) with high-intensity interventions. No significant difference in pooled odds of hypertension control was noted between lay advisor intervention and control groups, or between high-intensity and low-intensity intervention groups. Most studies used multicomponent interventions with no stepped care elements or reporting of efficacious components. Indicators of external validity (adoption, implementation, maintenance) were infrequently reported.
Discussion: Lay advisor interventions improve hypertension outcomes, with high intensity interventions having a greater impact. Further studies need to identify successful intervention and implementation factors of multicomponent interventions for stepped upscaling within healthcare system settings as well as factors used to help sustain interventions.
Hypertension is the leading risk factor for heart disease, and 31.3% of adults worldwide have hypertension (1, 2). It is estimated that only 13.8% of patients with hypertension globally achieve hypertension control (2). Traditional clinic-based care has not successfully improved hypertension control rates, which are worse in underserved communities (1). Community-based support improves outcomes in socially disadvantaged populations, especially when delivered by lay advisors who belong to the same social groups (3). Prior reviews of lay health advisors and community health workers (CHWs) have shown improved blood pressure and hypertension control (4–6). These reviews have been limited by including studies that evaluated lay advisor interventions with team-based care or additional health professional interventions and infrequent inclusion of broader community-based lay advisors such as barbers and faith-based lay advisors. Most health systems do not have the resources and staff to include multilevel interventions as reimbursement structure for team-based care is unclear, and it is difficult to know which level of intervention intensity can improve outcomes and in which contexts. The Community Preventive Services Task Force’s (CPSTF) systematic review of CHW interventions for heart disease and stroke prevention reported an evidence gap in incremental effectiveness of CHW interventions (7). Therefore, there is a need to identify the sole benefit of adding lay advisors to improve their adoption into routine healthcare teams, assess their generalizability or external validity, and understand the level of intensity and context needed to have an impact on blood pressure.
Thus, we conducted a systematic review which aims to assess the additional benefit of lay advisor interventions (including varying intensity levels) on hypertension outcomes from a health system perspective. We defined lay advisor interventions as those provided by anyone who does not have a health professional degree, including CHWs, health coaches, hairdressers, and faith-based workers. We aim to summarize reported factors that may inform decisions on implementation choices in clinical settings using the Reach, Effectiveness, Adoption, Implementation, and Maintenance (RE-AIM) framework, which is useful for assessing internal and external validity and context of interventions (8).
The PRISMA statement was used to report the findings of this systematic review (9).
(See Supplementary material S1 for the detailed search strategy for the Ovid MEDLINE database)
Librarians with expertise in screening citations for systematic reviews searched English language articles from 1981 through May 2023, using Ovid MEDLINE, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, CINAHL, PsycINFO, Scopus, World Health Organization International Clinical Trials Registry Platform (WHO ICTRP), ClinicalTrials.gov, and Sociological Abstracts. We reviewed references in published reviews for any additional articles. Two reviewers (SJP and VB) independently screened citations and confirmed the final included studies.
Groups of search terms included keywords for (1): lay lead, peer, community health worker, promotora, expert patient, barber, hairdresser, volunteer aide, faith-based, and (2); hypertension, high blood pressure, blood pressure.
Randomized and non-randomized studies published in English where the lay advisor intervention was evaluated as a sole additional intervention in adults with hypertension were included. As this review is designed for upscaling lay advisor interventions for hypertension care from a health system perspective, we did not include population-level screening studies that excluded adults with hypertension or population-level studies that did not report outcomes for the proportion of individuals diagnosed with hypertension. We excluded studies focused on pregnancy related hypertension disorders (preeclampsia, gestational hypertension).
We defined lay advisor interventions as those including navigation, education, or support provided by anyone who does not have a health professional degree, as they typically belong to the same social groups as study participants (10). Common lay advisor interventions include promotoras, health coaches, peer supporters, faith-based workers, hairdressers, and community health workers. We excluded studies that included additional health professional intervention, including physician education or intervention components, as it is typically uncompensated time. We excluded studies of blood pressure screenings in the community or health insurance linkages where patients with hypertension were excluded or there was no follow-up information on the group of patients with confirmed clinical diagnosis of hypertension. If both arms received the lay advisor intervention, the study arm with lower intensity was assigned as the low-intensity intervention. We assigned low-intervention intensity when the lay advisors delivered a synchronous intervention targeting hypertension education or management. It was not considered an intervention if the lay advisors only checked BP or collected data.
We included control groups where the only difference between the intervention and control group was the lay advisor delivered intervention. We included studies even if the control group received any form of low-intensity lay advisor interventions to provide insight into the incremental benefit of low-intensity versus high-intensity lay advisor interventions. Pre-post, process evaluations, and non-randomized studies were included. Studies that compared lay advisor interventions with active comparators such as health professionals or research staff were excluded.
For quantitative outcomes, the primary outcome was reduction in blood pressure (BP). We included change in systolic BP and diastolic BP as our joint primary outcome. Secondary outcome was the difference in the change in the proportion of patients with controlled hypertension from baseline to post intervention between intervention and control arms. If reported, we used the proportion of patients with BP <140/90 mmHg to define controlled hypertension if the study did not explicitly state the proportion of patients with controlled hypertension (2). For RE-AIM dimension outcomes, we looked at the characteristics and presence or absence of each RE-AIM dimension component.
Two authors assessed study quality using the Cochrane Collaboration’s risk of bias tool for RCTs (11). The primary author (S.J.P.) made final decisions where conflicts existed after reviewing all the articles independently.
Two authors independently reviewed titles, abstracts, and full articles to identify eligible studies and conflicts were resolved by joint re-review and consensus. Prior to data extraction, two authors created a codebook with all variables of interest. Two authors extracted data independently, and discrepancies were resolved by consensus between reviewers or by a third author if needed.
We extracted data on characteristics of the study setting, participants, lay advisor training and recruitment, and intervention characteristics. We defined any intervention with more than one component as multicomponent intervention. For example, if an intervention included education sessions and recurring follow-up telephone calls, it was considered a multicomponent intervention.
Quantitative values and measures of statistical variation for BP and hypertension control rates were extracted from baseline and at the end of the study. When there were multiple study arms, we included quantitative values for the two arms, where the only difference was the lay advisor-led intervention or varying levels of lay advisor intervention.
Internal and external validity indicators using RE-AIM coding and scoring: A previously published tool was used to code eligible articles on the degree to which internal and external validity indicators of the RE-AIM framework were reported (12). We looked at protocols if referenced in the main articles. Supplementary Table S1 details how each dimension and component of RE-AIM was defined and measured.
A descriptive synthesis of the study setting, participants, lay advisors, intervention components, and control group was performed and reported as a study description table. Proportions of total, RCTs, and nonRCT studies reporting each of the RE-AIM dimensions and components are reported as a table. Quantitative synthesis: If we had three or more eligible studies of added lay advisor intervention or varying levels of lay advisor interventions, the primary author (SJP.) performed the statistical analysis using Comprehensive Meta-analysis Software version 3 (Biostat Inc., Englewood, NJ). We adjusted sample sizes for cluster RCTs using the documented intra-cluster coefficient (ICC) (13). We used the random-effects model to compute conservative effect sizes incorporating both within-study and between-study variations. We calculated the difference in means with 95% confidence intervals, and we considered a p-value of <0.05 statistically significant for all analyses other than the Q statistic. A correlation coefficient of 0.5 was assumed between initial and final values. Heterogeneity among studies was evaluated using the Q statistic, with a p-value <0.10 indicating heterogeneity, and using I2 statistics (I2 values <40% may indicate less substantial heterogeneity and 75–100% indicates substantial heterogeneity) (14). If substantial heterogeneity existed, we planned a priori meta-regression if we had 20 or more studies or subgroup analysis if we had <10 studies. We identified the following study characteristics that may explain between-study variability: presence or absence of intention to treat analysis; presence or absence of home visits; settings in developed or developing countries; lay advisor training duration; study duration; and intervention components of group education, individualized intervention, or combined intervention. Publication bias was assessed with funnel plots and the Egger regression test (15). We conducted sensitivity analysis by removing one study at a time.
Of 7,267 unique citations, 41 studies were eligible for inclusion in our review. See PRISMA Flow Diagram. (Figure 1) All study characteristics are shown in Table 1.
Of the 41 articles meeting inclusion criteria, 22 were RCTs (16–37) and 19 were non-randomized studies including process assessments and matched cohort studies (38–56). Of the 22 RCTs, 13 RCTs were done in the US (16, 17, 21, 24, 26, 27, 29–31, 33, 35–37). Of the 19 non-randomized studies, 14 were done in the United States. Twenty-nine studies were from developed economies, and 12 were from developing economies. Studies mainly included racial/ethnic minority populations or were conducted in socioeconomically deprived areas of the country. Seven RCTs conducted in the United States included low-intensity lay advisor interventions in the control group (21, 24, 27, 30, 31, 35, 37). The participants’ mean age was 54 years and, in most studies, varied between 50 to 65 years.
Most studies mentioned lay advisors were matched demographically with study participants. The least intense interventions were outreach phone calls to promote access to care (29). Most intense intervention included monthly group education with home visits every other month with follow-up biweekly phone calls (35). Other than two studies, all lay advisor interventions were multicomponent. Seven studies compared low-intensity interventions with high-intensity lay advisor interventions. No studies specifically compared stratified or stepped care models of modifying lay advisor intervention intensity based on patient characteristics or hypertension control state with usual care.
Supplementary Table S2 summarizes the assessment of risk of bias for individual randomized studies. All studies had at least one domain judged as unclear risk of bias and 18 studies had at least one domain, mainly blinding or intention to treat, regarded as high risk of bias. No studies had all domains regarded as low risk of bias. Dropout rates varied from 0 to 31% and 6 RCTs had dropout rates of >20% with higher dropouts from intervention groups.
Of RCTs where control groups did not receive any lay advisor interventions, nine reported systolic BP outcomes, eight reported diastolic BP outcomes and six reported hypertension control outcomes at baseline and end of study. See Table 2 for improvement in BP and hypertension control noted in all included RCTs and Table 3 for improvement in BP and hypertension control in included non-RCTs.
The overall pooled effect of lay advisor interventions from nine RCTs (n = 4,220 participants) showed a mean improvement in systolic BP of −3.7 mmHg (CI –6.1 to –1.3; p 0.002, I2 88%). (Figure 2) A sensitivity analysis where each study was removed had no significant impact on the results. (Supplementary Figure S1: Forest plot with each study removed) The pooled effect from eight RCTs (n = 3,056) of lay advisor interventions which measured diastolic BP showed an improvement of −1.8 mmHg (CI –2.5 to –1.0; p < 0.001, I2 7%). (Figure 3) A sensitivity analysis where each study was removed had no significant impact on the results. (See Supplementary Figure S2).
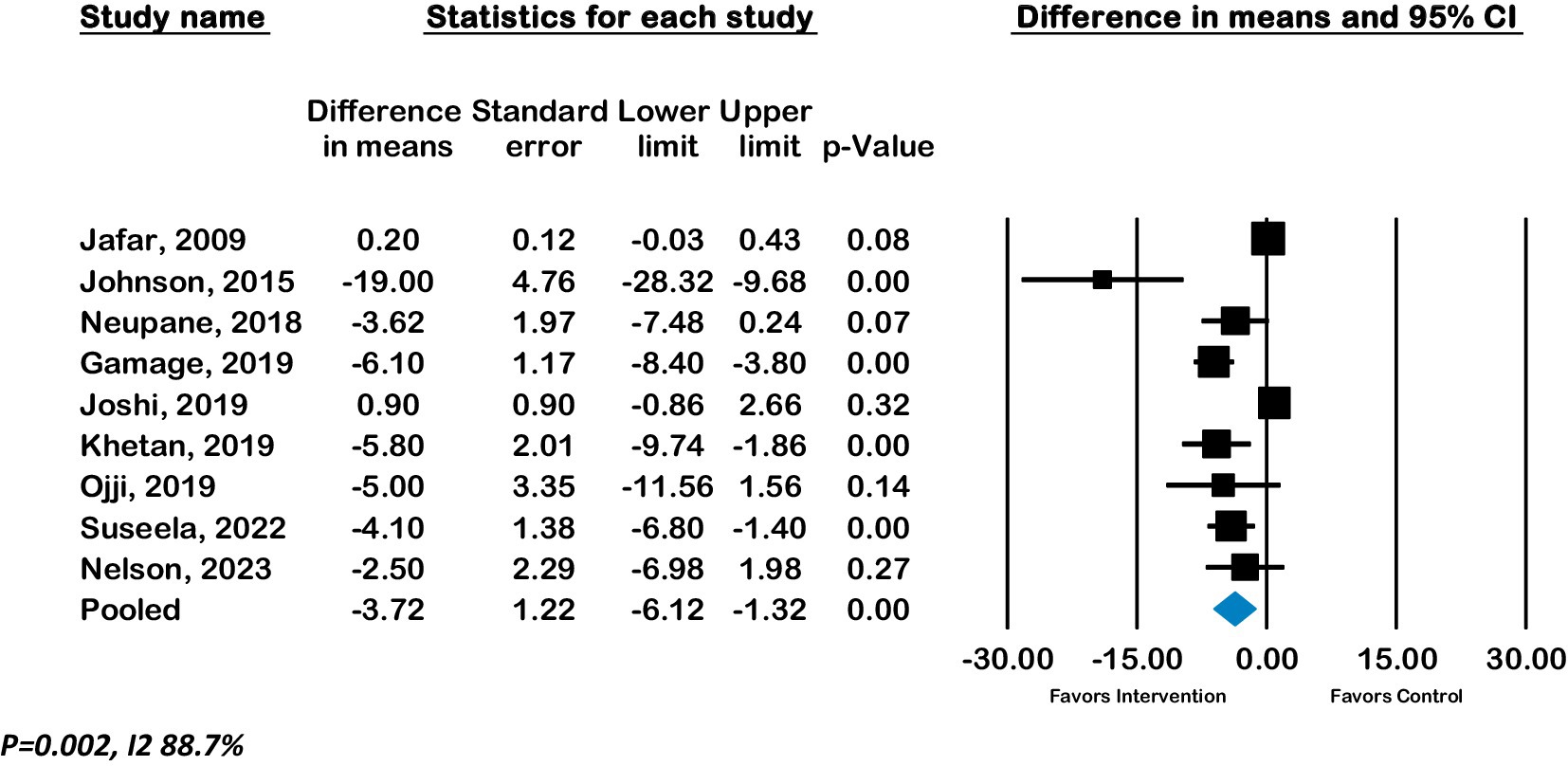
Figure 2. Forest plot of Systolic BP - Effect of lay advisor interventions on Systolic BP compared to control group.
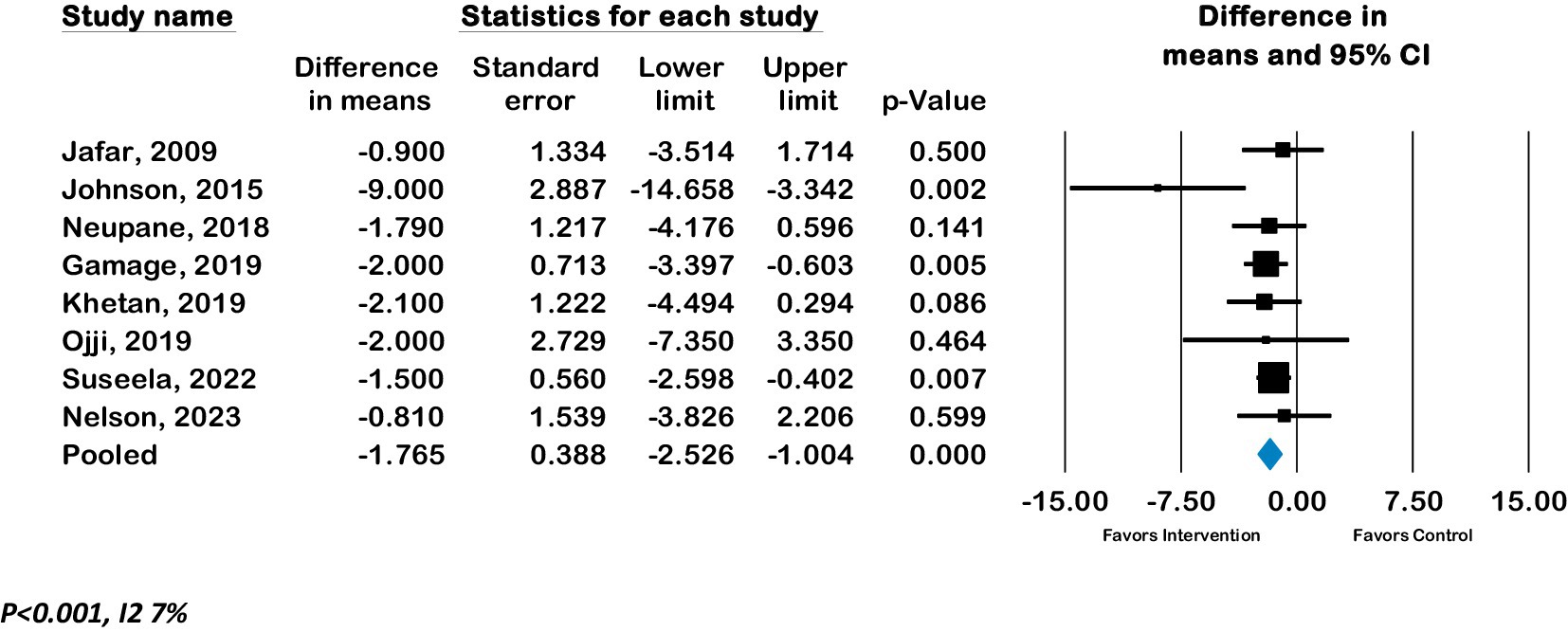
Figure 3. Forest plot of Diastolic BP - Effect of lay advisor interventions on Diastolic BP compared to control group.
Meta-analysis of six RCTs (n = 3,762) showed a pooled odds ratio of 1.2 (CI 0.75 to 2.0; p = 0.4, I2 85.8%) for controlled hypertension with lay advisor interventions compared to the control group. (See Figure 4).
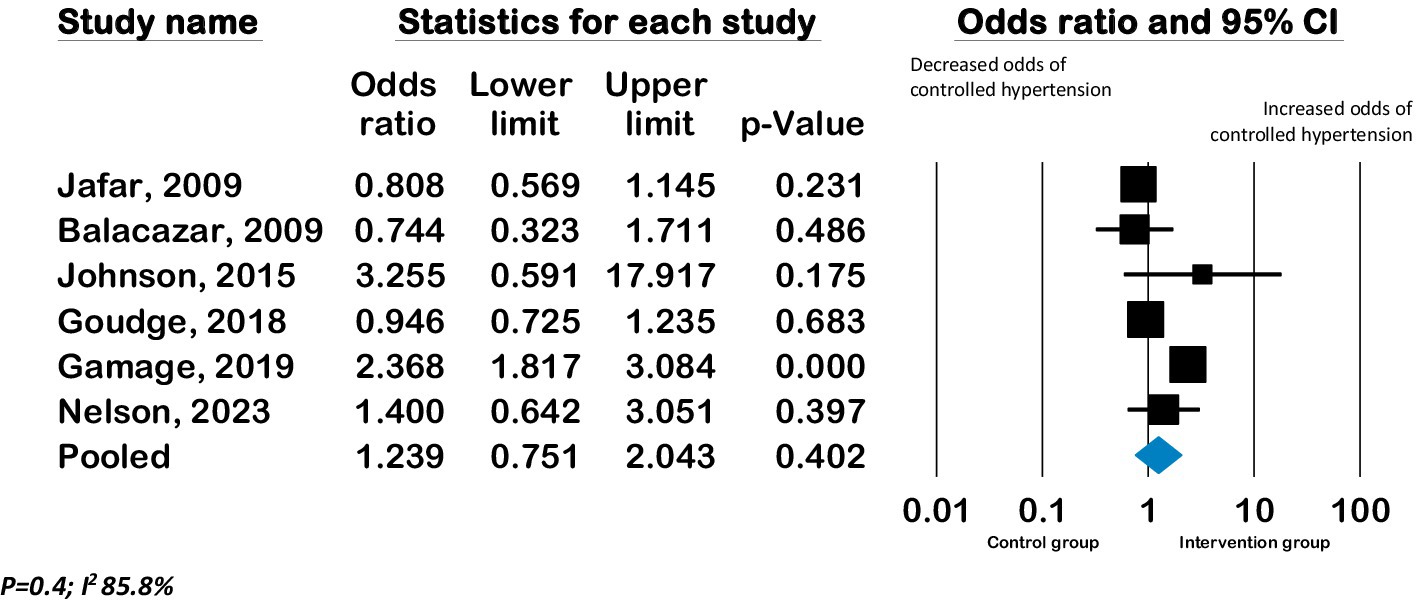
Figure 4. Forest plot of pooled effect on hypertension control - Effect of lay advisor interventions on hypertension control compared to control group.
Subgroup analyses of studies grouped by presence of intention to treat did not show any significant differences in BP between groups. (Supplementary Figures S3, S4) There were not enough studies to conduct subgroup analyses of studies grouped by developed or developing country setting, and mode of interventions. The funnel plot and Eggers regression test (p = 0.008) indicate publication bias for systolic BP outcomes but not for diastolic BP or hypertension control outcomes. (Supplementary Figures S5, S6).
Seven RCTs from the United States compared low-intensity interventions with high-intensity interventions, of which six reported BP outcomes. Pooled effect from these six RCTs (n = 2,644) showed a mean improvement in systolic BP of −3.6 mmHg (CI –6.7 to −0.46; p 0.02, I2 82.7%) and in diastolic BP of −2.1 mmHg (CI –3.7 to −0.4; p 0.01, I2 70.9%) in high-intensity lay advisor interventions compared to low-intensity interventions (See Figures 5, 6). The funnel plot and Eggers regression test (p = 0.4) did not indicate publication bias for these pooled BP outcomes. A sensitivity analysis where each study was removed showed reduced significance of results. (See Supplementary Figures S7, S8) Meta-analysis of seven RCTs (n = 3,277) showed a pooled odds ratio of 1.29 (CI 0.79 to 2.1; p = 0.3, I2 90.79%) for controlled hypertension with high-intensity lay advisor interventions compared to the low-intensity lay advisor intervention group (Supplementary Figure S10). There were not enough studies in groups to conduct subgroup analyses for high intensity compared to low intensity interventions.
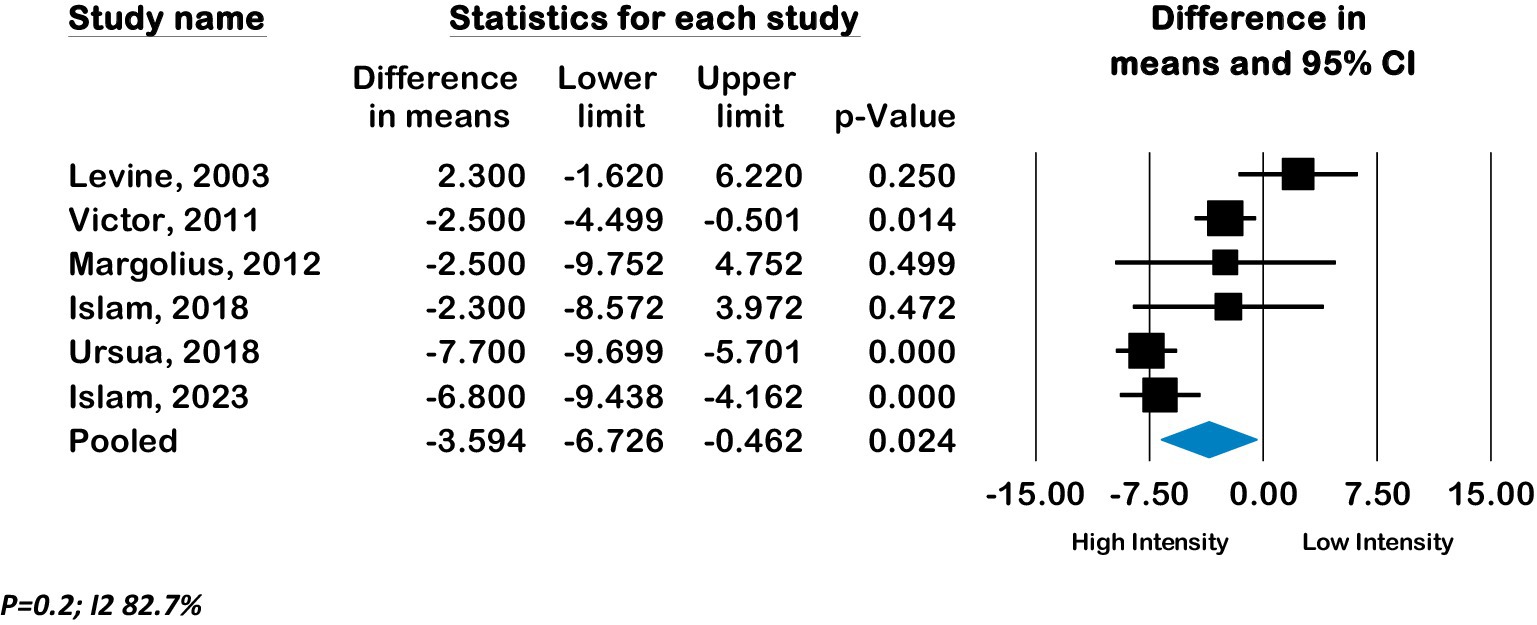
Figure 5. Forest plot of pooled effect of high intensity compared to low intensity interventions on Systolic BP.
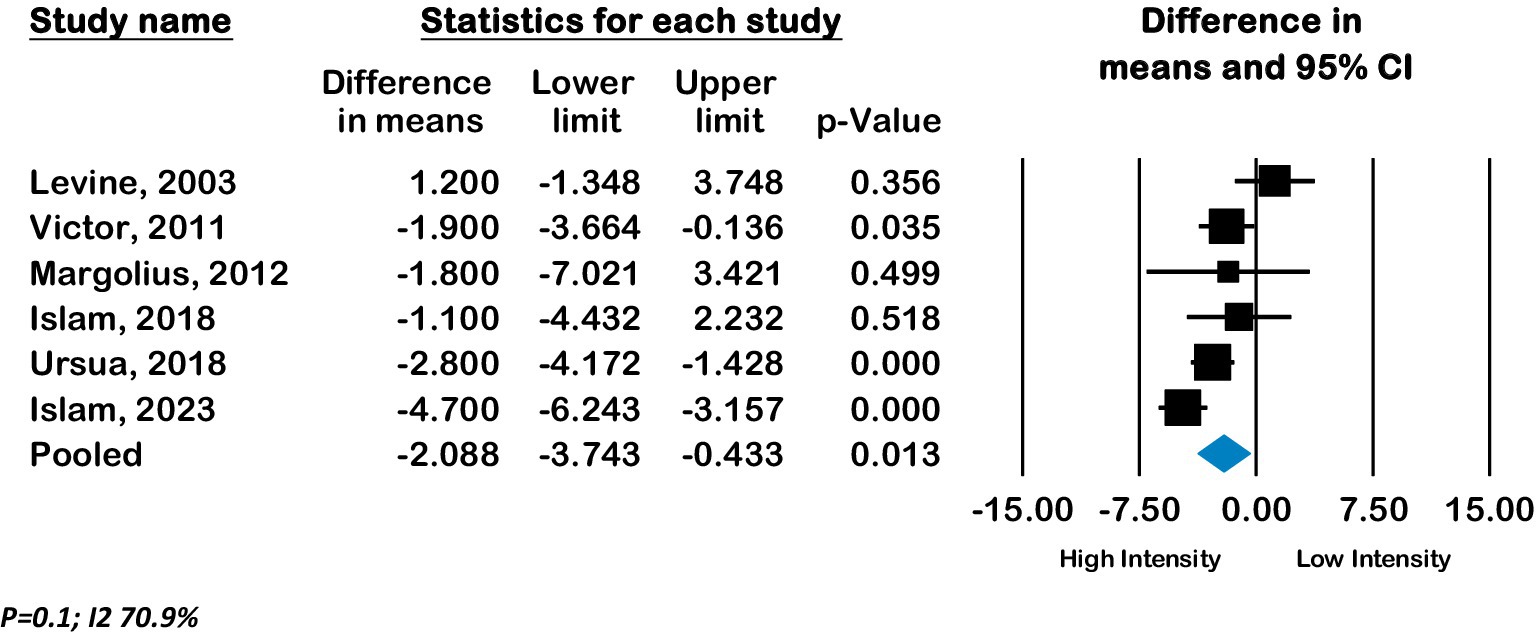
Figure 6. Forest plot of pooled effect of high intensity compared to low Intensity interventions on Diastolic BP.
There was no significant difference in the frequency of reporting of RE-AIM components between randomized and non-randomized studies other than qualitative assessments of efficacy, which were more frequently reported in nonRCTs. See Table 4 and Supplementary Table S1. One study specifically reported study results in RE-AIM format (45) and one recent study specifically reported reach and adoption of peer coaching intervention in primary care practices (33, 57).
Six of the nine studies with sample sizes >1000 were conducted in developing countries (18–20, 23, 25, 34) and three were done in the United States (27, 31, 45). Participation rate varied from 2 to 98% with clinic-based recruitment showing higher participation rates compared to population-level recruitment. When reported, nonparticipating individuals had higher systolic BP or a lower proportion of their BP controlled at baseline, but this information was not reported in most studies (18, 29). Clinic-based recruitment showed higher participation rates as fewer patients needed to be approached in clinics (denominators were lower) with higher recruitment success (21).
Eight non-randomized studies reported qualitative assessments to understand outcomes (39, 41, 42, 50–53, 56); one of these was mainly a process evaluation of a sustained peer leader program for Veterans (39). One pragmatic randomized study included process evaluation in their protocol, but published article mentions challenges with balancing external validity and intervention assessments (19, 58). Few studies reported reasons for lay advisor withdrawals, which included personal reasons of health issues or relocation as well as an inability to perform certain required intervention tasks such as properly reading BP measurements (25, 39).
Method to identify the target delivery agent was reported mainly as the selection and nomination of volunteers with matching sociodemographic characteristics to participants. Two studies reported adding activities to a pre-existing program, but repeated visitor rate (43%) was only reported in one study (39, 44). One author of a randomized study shared a follow-up process evaluation using mixed methods assessment with surveys and focus group discussions (18, 59).
Four studies mention compensation for lay advisors reflecting the pay scale of the respective countries otherwise studies reported lay advisor compensation for completing study activities (18, 25, 28, 32). One study reported CHWs worked 40 to 60 h per month to care for 120 participants (28).
Seven studies indicate the continued feasibility of maintaining intervention using already available infrastructure or public funding (25, 28, 32, 39, 44, 45, 60).
We contribute to the literature by reporting a systematic review that evaluates the additional benefit of lay advisor interventions for hypertension outcomes where the lay advisor interventions are the sole additional intervention. We limited contamination by separating the analysis where the control group received any lay advisor intervention to inform this additional benefit and to inform differing intensity levels of interventions. We note improvement in blood pressure outcomes with added lay advisor interventions compared to usual care and with high-intensity interventions compared to low-intensity interventions in populations with lower socioeconomic states or racial/ethnic minority populations. Control groups and low-intensity interventions also showed BP improvements in most studies. No studies examined the impact of minimally burdensome lay advisor interventions with stepped-up care to high-intensity interventions in people with continued unmet needs.
Our results are similar to most reviews showing positive effects of CHWs on hypertension outcomes. Previous Community Preventive Services Task Force (CPSTF) found that team-based care with community health workers (CHWs) is effective for hypertension and cardiovascular disease prevention, but they did not look at the add-on benefit of CHWs (4). Team-based care and lay advisor interventions are difficult to translate into clinical care settings as reimbursement policies remain unclear for both, and staff time is limited (4, 5, 61). A recent review reported individual studies of CHW interventions in low-income and middle-income countries showed improved hypertension control (6). Most previous reviews focused on CHW interventions delivered by mainly government-trained CHWs or CHWs specifically recruited for the studies; lay advisors such as barbers and faith-based workers are infrequently included in previous reviews. We included a broader lay advisor definition and assessed the additional benefit of adopting lay advisors for hypertension care without adding burden to already overworked limited clinic staff within health systems. No previous reviews have compared the effectiveness of varying intensities of lay advisor interventions on hypertension outcomes. We strengthen the literature by showing the additional benefit of lay advisors interventions for improving hypertension outcomes and showing increasing effects with higher intensity interventions. Lastly, this is the first comprehensive systematic review of the state of lay advisor interventions for hypertension from internal and external validity perspectives using the RE-AIM framework. We also demonstrate areas for needed future research such as reporting on elements of the RE-AIM framework for the context of and validity of interventions as well as the need for examining stepped-up intervention intensity approaches for patients with continued uncontrolled hypertension which may help balance the intervention burden and limited healthcare resources.
Similar to most literature, our RE-AIM assessments show frequent reporting of individual-level (Reach, Effectiveness) but insufficient reporting of organizational-level dimensions (Adoption, Implementation, and Maintenance) that affect the external validity of the interventions. Below we discuss each element of the RE-AIM Framework.
Characteristics or contexts that interact with an individual’s willingness to participate may influence the potential of these interventions to improve health disparities, as most studies included socially disadvantaged populations.
Studies have rarely reported reasons for improvement in outcomes and characteristics of participants who may not benefit from these interventions or continue to have unmet needs. Assessments of multicomponent interventions to identify the least and most efficacious individual components are missing and may help tailor upscaling.
It is unclear what characteristics or contextual factors would encourage the uptake of a lay advisor role by individuals not already engaged in community-level leadership. Settings for lay advisor interventions were mostly predetermined with outside funding; hence, the characteristics of settings that otherwise may or may not participate are unclear.
The time required for interventions’ key components and supervision needs to be quantified from the individual and organizational perspectives. Costs from a societal perspective or grant-funded compensation are frequently reported but may not be helpful for health systems with limited resources or budget margins.
Our review has several limitations due to the way studies report information and limitations of meta-analyses. We strictly limited our review to studies with lay advisor-delivered intervention without additional health professional or research staff-delivered components. We did not want to combine two interventions with unclear reimbursement structures, and lay advisors are generally not yet part of core healthcare teams; however, lay advisors alone can provide support. Specifically, our exclusion of any physician education or training component limited a few key studies (62–65). We excluded these studies because physician-directed interventions may individually improve outcomes, and hypertension is routinely managed in time-restricted primary care clinic visits along with multiple concerns and health maintenance (66, 67). Secondly, as health systems may or may not be involved in community-level screenings but are typically held accountable for hypertension outcomes in their patient populations, we limited community-level screening studies to those reporting hypertension outcomes. Third, high heterogeneity was noted with diverse intervention components and intensity variations but planned meta-regression and subgroup analysis to explain the variation could not be done due to limited number of eligible studies; nevertheless, the increasing dose–response gradient with increasing intervention intensity supports directionality of the intervention effects. Literature syntheses can make sense of this heterogeneity if studies also report contextual factors affecting individual intervention component acceptability and efficacy.
Our review has strong implications for future research. Reporting of most and least efficacious components of multicomponent interventions to tailor stepped upscaling of lay advisor interventions is needed. Studies mainly included adults representing the working population’s age where stepped-care models may be important to reducing intervention burden and balancing healthcare resource allocations. Tailoring lay advisor services within health systems that serve diverse patient populations has been understudied as most studies targeted socially disadvantaged population groups. Pragmatic trial designs such as hybrid effectiveness implementation trials may be helpful to evaluate not only how the intervention works but also how to successfully implement the interventions in diverse settings. Qualitative assessments of why and how the lay advisor interventions reach the targeted population, improve outcomes, and can be maintained are areas for future research. Future mixed methods assessments need to contribute to understanding the facilitators and barriers to engaging patients in the interventions, retaining a lay advisor workforce, and sustainability of the intervention at an individual and organizational level.
Add-on and high intensity lay advisor interventions may improve blood pressure outcomes in socially disadvantaged populations, but studied interventions are heterogeneous. Future studies need to identify the intervention’s most efficacious components and include assessments of stepped upscaling. Future research should focus on mixed methods assessments to identify explanatory processes for effectiveness and engagement at the individual, lay advisor, and setting levels to inform the real-world implementation of these interventions.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
SP: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. VB: Data curation, Formal analysis, Validation, Writing – original draft, Writing – review & editing. YY: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. LB: Data curation, Validation, Writing – original draft. E-OU: Data curation, Validation, Writing – original draft. IT: Data curation, Validation, Writing – original draft. RS: Supervision, Writing – review & editing. KS: Methodology, Supervision, Writing – review & editing. SB: Methodology, Supervision, Visualization, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. Source of funding and support statement: Patil was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number KL2 TR002346. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. No financial disclosures were reported by remaining authors of this paper. No other sources of support reported by remaining authors of this paper.
We acknowledge librarians Gwendolyn Wilson (University of Missouri) and Mary Schleicher (Cleveland Clinic) for their help with the database searches, removing of duplicates, and exporting citations in Rayyan and Covidence software.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1305190/full#supplementary-material
1. Virani, SS, Alonso, A, Aparicio, HJ, Benjamin, EJ, Bittencourt, MS, Callaway, CW, et al. Heart disease and stroke Statistics-2021 update: a report from the American Heart Association. Circulation. (2021) 143:e254–743. doi: 10.1161/CIR.0000000000000950
2. Mills, KT, Stefanescu, A, and He, J. The global epidemiology of hypertension. Nat Rev Nephrol. (2020) 16:223–37. doi: 10.1038/s41581-019-0244-2
3. Sigmund, CD, Carey, RM, Appel, LJ, Arnett, DK, Bosworth, HB, Cushman, WC, et al. Report of the National Heart, Lung, and Blood Institute working group on hypertension: barriers to translation. Hypertension. (2020) 75:902–17. doi: 10.1161/HYPERTENSIONAHA.119.13887
4. Chattopadhyay, SK, Jacob, V, Mercer, SL, Hopkins, DP, Elder, RW, and Jones, CD. Community guide cardiovascular disease economic reviews: tailoring methods to ensure utility of findings. Am J Prev Med. (2017) 53:S155–63. doi: 10.1016/j.amepre.2017.06.012
5. Derington, CG, King, JB, Bryant, KB, McGee, BT, Moran, AE, Weintraub, WS, et al. Cost-effectiveness and challenges of implementing intensive blood pressure goals and team-based care. Curr Hypertens Rep. (2019) 21:91. doi: 10.1007/s11906-019-0996-x
6. Mbuthia, GW, Magutah, K, and Pellowski, J. Approaches and outcomes of community health worker’s interventions for hypertension management and control in low-income and middle-income countries: systematic review. BMJ Open. (2022) 12:e053455. doi: 10.1136/bmjopen-2021-053455
7. Cardiovascular disease: interventions engaging community health workers: systematic review Atlanta, GA: The Community Guide (2015). Available at: https://www.thecommunityguide.org/findings/heart-disease-stroke-prevention-interventions-engaging-community-health-workers.html.
8. Glasgow, RE, Harden, SM, Gaglio, B, Rabin, B, Smith, ML, Porter, GC, et al. RE-AIM planning and evaluation framework: adapting to new science and practice with a 20-year review. Front Public Health. (2019) 7:7. doi: 10.3389/fpubh.2019.00064
9. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
10. Barnett, ML, Lau, AS, and Miranda, J. Lay health worker involvement in evidence-based treatment delivery: a conceptual model to address disparities in care. Annu Rev Clin Psychol. (2018) 14:185–208. doi: 10.1146/annurev-clinpsy-050817-084825
11. Higgins, JPT, Altman, DG, and Sterne, JAC. Assessing risk of bias in included studies In: JPT Higgins and S Green, editors. Cochrane handbook for systematic reviews of interventions. Version 5.1.0. Oxford: Cochrane Collaboration (2011)
12. Kessler, RS, Purcell, EP, Glasgow, RE, Klesges, LM, Benkeser, RM, and Peek, CJ. What does it mean to "employ" the RE-AIM model? Eval Health Prof. (2013) 36:44–66. doi: 10.1177/0163278712446066
13. Higgins, JPT, Deeks, JJ, and Altman, DG. Approximate analyses of cluster-randomized trials for a meta-analysis: effective sample sizes In: JPT Higgins and S Green, editors. Cochrane handbook for systematic reviews of interventions. Version 5.1.0. Oxford: Cochrane Collaboration (2011)
14. Deeks, JJ, Higgins, JPT, and Altman, DG. Identifying and measuring heterogeneity In: JPT Higgins and S Green, editors. Cochrane handbook for systematic reviews of interventions. Version 5.1.0. Oxford: Cochrane Collaboration (2011)
15. Egger, M, Davey, SG, Schneider, M, and Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
16. Balcazar, HG, Byrd, TL, Ortiz, M, Tondapu, SR, and Chavez, M. A randomized community intervention to improve hypertension control among Mexican Americans: using the promotoras de salud community outreach model. J Health Care Poor Underserved. (2009) 20:1079–94. doi: 10.1353/hpu.0.0209
17. Dye, CJ, Williams, JE, and Evatt, JH. Activating patients for sustained chronic disease self-management: thinking beyond clinical outcomes. J Prim Care Community Health. (2016) 7:107–12. doi: 10.1177/2150131915626562
18. Gamage, DG, Riddell, MA, Joshi, R, Thankappan, KR, Chow, CK, Oldenburg, B, et al. Effectiveness of a scalable group-based education and monitoring program, delivered by health workers, to improve control of hypertension in rural India: a cluster randomised controlled trial. PLoS Med. (2020) 17:e1002997. doi: 10.1371/journal.pmed.1002997
19. Goudge, J, Chirwa, T, Eldridge, S, Gómez-Olivé, FXF, Kabudula, C, Limbani, F, et al. Can lay health workers support the management of hypertension? Findings of a cluster randomised trial in South Africa. BMJ Glob Health. (2018) 3:e000577. doi: 10.1136/bmjgh-2017-000577
20. Joshi, R, Agrawal, T, Fathima, F, Usha, T, Thomas, T, Misquith, D, et al. Cardiovascular risk factor reduction by community health workers in rural India: a cluster randomized trial. Am Heart J. (2019) 216:9–19. doi: 10.1016/j.ahj.2019.06.007
21. Margolius, D, Bodenheimer, T, Bennett, H, Wong, J, Ngo, V, Padilla, G, et al. Health coaching to improve hypertension treatment in a low-income, minority population. Ann Fam Med. (2012) 10:199–205. doi: 10.1370/afm.1369
22. Ojji, DB, Baldridge, AS, Ojji, AI, Shedul, LG, Ojji, OI, Egenti, NB, et al. Feasibility and effect of community health worker support and home monitoring for blood pressure control in Nigeria: a randomised pilot trial. Cardiovasc J Afr. (2020) 31:51–3. doi: 10.5830/CVJA-2019-066
23. Poggio, R, Melendi, SE, Beratarrechea, A, Gibbons, L, Mills, KT, Chen, CS, et al. Cluster randomized trial for hypertension control: effect on lifestyles and body weight. Am J Prev Med. (2019) 57:438–46. doi: 10.1016/j.amepre.2019.05.011
24. Ursua, RA, Aguilar, DE, Wyatt, LC, Trinh-Shevrin, C, Gamboa, L, Valdellon, P, et al. A community health worker intervention to improve blood pressure among Filipino Americans with hypertension: a randomized controlled trial. Prev Med Rep. (2018) 11:42–8. doi: 10.1016/j.pmedr.2018.05.002
25. Neupane, D, McLachlan, CS, Mishra, SR, Olsen, MH, Perry, HB, Karki, A, et al. Effectiveness of a lifestyle intervention led by female community health volunteers versus usual care in blood pressure reduction (COBIN): an open-label, cluster-randomised trial. Lancet Glob Health. (2018) 6:e66–73. doi: 10.1016/S2214-109X(17)30411-4
26. Johnson, W, Ezeugwu, C, Monroe, D, Breunig, IM, and Shaya, F. A pilot study evaluating a community-based intervention focused on the ISHIB IMPACT cardiovascular risk reduction toolkit in African American patients with uncontrolled hypertension. Ethn Dis. (2015) 25:162–7.
27. Victor, RG, Ravenell, JE, Freeman, A, Leonard, D, Bhat, DG, Shafiq, M, et al. Effectiveness of a barber-based intervention for improving hypertension control in black men: the BARBER-1 study: a cluster randomized trial. Arch Intern Med. (2011) 171:342–50. doi: 10.1001/archinternmed.2010.390
28. Khetan, A, Zullo, M, Rani, A, Gupta, R, Purushothaman, R, Bajaj, NS, et al. Effect of a community health worker-based approach to integrated cardiovascular risk factor control in India: a cluster randomized controlled trial. Glob Heart. (2019) 14:355–65. doi: 10.1016/j.gheart.2019.08.003
29. Krieger, J, Collier, C, Song, L, and Martin, D. Linking community-based blood pressure measurement to clinical care: a randomized controlled trial of outreach and tracking by community health workers. Am J Public Health. (1999) 89:856–61. doi: 10.2105/AJPH.89.6.856
30. Levine, DM, Bone, LR, Hill, MN, Stallings, R, Gelber, AC, Barker, A, et al. The effectiveness of a community/academic health center partnership in decreasing the level of blood pressure in an urban African-American population. Ethn Dis. (2003) 13:354–61.
31. Morisky, DE, Lees, NB, Sharif, BA, Liu, KY, and Ward, HJ. Reducing disparities in hypertension control: a community-based hypertension control project (CHIP) for an ethnically diverse population. Health Promot Pract. (2002) 3:264–75. doi: 10.1177/152483990200300221
32. Jafar, TH, Hatcher, J, Poulter, N, Islam, M, Hashmi, S, Qadri, Z, et al. Community-based interventions to promote blood pressure control in a developing country: a cluster randomized trial. Ann Intern Med. (2009) 151:593–601. doi: 10.7326/0003-4819-151-9-200911030-00004
33. Safford, MM, Cummings, DM, Halladay, J, Shikany, JM, Richman, J, Oparil, S, et al. The design and rationale of a multicenter real-world trial: the southeastern collaboration to improve blood pressure control in the US Black Belt – addressing the triple threat. Contemp Clin Trials. (2023) 129:107183. doi: 10.1016/j.cct.2023.107183
34. Suseela, RP, Ambika, RB, Mohandas, S, Menon, JC, Numpelil, M, Vasudevan, BK, et al. Effectiveness of a community-based education and peer support led by women’s self-help groups in improving the control of hypertension in urban slums of Kerala, India: a cluster randomised controlled pragmatic trial. BMJ Glob Health. (2022) 7:e010296. doi: 10.1136/bmjgh-2022-010296
35. Islam, NS, Wyatt, LC, Ali, SH, Zanowiak, JM, Mohaimin, S, Goldfeld, K, et al. Integrating community health workers into community-based primary care practice settings to improve blood pressure control among south Asian immigrants in new York City: results from a randomized control trial. Circ Cardiovasc Qual Outcomes. (2023) 16:e009321. doi: 10.1161/CIRCOUTCOMES.122.009321
36. Nelson, KM, Taylor, L, Williams, JL, Rao, M, Gray, KE, Kramer, CB, et al. Effect of a peer health coaching intervention on clinical outcomes among US veterans with cardiovascular risks: the vet-COACH randomized clinical trial. JAMA Netw Open. (2023) 6:e2317046. doi: 10.1001/jamanetworkopen.2023.17046
37. Islam, NS, Wyatt, LC, Taher, MD, Riley, L, Tandon, SD, Tanner, M, et al. A culturally tailored community health worker intervention leads to improvement in patient-centered outcomes for immigrant patients with type 2 diabetes. Clin Diabetes. (2018) 36:100–11. doi: 10.2337/cd17-0068
38. Dye, CJ, Williams, JE, and Evatt, JH. Improving hypertension self-management with community health coaches. Health Promot Pract. (2015) 16:271–81. doi: 10.1177/1524839914533797
39. Hayes, A, Morzinski, J, Ertl, K, Wurm, C, Patterson, L, Wilke, N, et al. Preliminary description of the feasibility of using peer leaders to encourage hypertension self-management. WMJ. (2010) 109:85–90.
40. Hovell, MF, Geary, DC, Black, DR, Kamachi, K, and Kirk, R. The effects of lay counseling on medication adherence and blood pressure: adjunctive treatment for hypertension. Patient Educ Couns. (1984) 6:91–4. doi: 10.1016/0738-3991(84)90040-5
41. Woods, SS, and Costanzo, CL. Community lay worker guided home-based monitoring program for hypertension control. J Dr Nurs Pract. (2016) 9:249–56. doi: 10.1891/2380-9418.9.2.249
42. Isiguzo, GC, Santo, K, Panda, R, Mbau, L, Mishra, SR, Ugwu, CN, et al. Adherence clubs to improve hypertension Management in Nigeria: Clubmeds, a feasibility study. Glob Heart. (2022) 17:1–13. doi: 10.5334/gh.1109
43. Sánchez, V, Cacari Stone, L, Moffett, ML, Nguyen, P, Muhammad, M, Bruna-Lewis, S, et al. Process evaluation of a promotora de salud intervention for improving hypertension outcomes for Latinos living in a rural U.S.-Mexico border region. Health Promot Pract. (2014) 15:356–64. doi: 10.1177/1524839913516343
44. Truncali, A, Dumanovsky, T, Stollman, H, and Angell, SY. Keep on track: a volunteer-run community-based intervention to lower blood pressure in older adults. J Am Geriatr Soc. (2010) 58:1177–83. doi: 10.1111/j.1532-5415.2010.02874.x
45. Reininger, BM, Mitchell-Bennett, LA, Lee, M, Yeh, PG, Davé, AC, Park, SK, et al. Scaling a community-wide campaign intervention to manage hypertension and weight loss. Front Med (Lausanne). (2021) 8:661353. doi: 10.3389/fmed.2021.661353
46. Schwalm, J-D, McCready, T, Lear, SA, Lamelas, P, Garis, L, Musa, H, et al. Exploring new models for cardiovascular risk reduction: the heart outcomes prevention and evaluation 4 (HOPE 4) Canada pilot study. CJC Open. (2021) 3:267–75. doi: 10.1016/j.cjco.2020.10.006
47. Samuel-Hodge, CD, Gizlice, Z, Allgood, SD, Bunton, AJ, Erskine, A, Leeman, J, et al. A hybrid implementation-effectiveness study of a community health worker-delivered intervention to reduce cardiovascular disease risk in a rural, underserved non-Hispanic Black population: the CHANGE study. Am J Health Promot. (2022) 36:948–58. doi: 10.1177/08901171221078272
48. Hess, PL, Reingold, JS, Jones, J, Fellman, MA, Knowles, P, Ravenell, JE, et al. Barbershops as hypertension detection, referral, and follow-up centers for black men. Hypertension. (2007) 49:1040–6. doi: 10.1161/HYPERTENSIONAHA.106.080432
49. Yi, SS, Wyatt, LC, Patel, S, Choy, C, Dhar, R, Zanowiak, JM, et al. A faith-based intervention to reduce blood pressure in underserved metropolitan New York immigrant communities. Prev Chronic Dis. (2019) 16:E106. doi: 10.5888/pcd16.180618
50. Ursua, RA, Aguilar, DE, Wyatt, LC, Katigbak, C, Islam, NS, Tandon, SD, et al. A community health worker intervention to improve management of hypertension among Filipino Americans in New York and New Jersey: a pilot study. Ethn Dis. (2014) 24:67–76.
51. Thomas, N, Ewart, C, Lewinson Roberts, D, and Brown, A. “You can change the world with a haircut”: evaluating the feasibility of a barber-led intervention for men of Black and ethnic minority heritage to manage high blood pressure. J Prim Care Community Health. (2023) 14:215013192311683. doi: 10.1177/21501319231168336
52. Bush, K, Patrick, C, Elliott, K, Morris, M, Tiruneh, Y, and McGaha, P. Unsung heroes in health education and promotion: how community health workers contribute to hypertension management. Front Public Health. (2023) 11:11. doi: 10.3389/fpubh.2023.1088236
53. Brewer, LC, Jones, C, Slusser, JP, Pasha, M, Lalika, M, Chacon, M, et al. mHealth intervention for promoting hypertension self-management among African American patients receiving Care at a Community Health Center: formative evaluation of the FAITH! Hypertension app. J Med Internet Res. (2023) 7:e45061. doi: 10.2196/45061
54. Kisigo, GA, Mgeta, F, Mcharo, O, Okello, E, Wajanga, B, Kalokola, F, et al. Peer counselor intervention for reducing mortality and/or hospitalization in adults with hypertensive urgency in Tanzania: a pilot study. Am J Hypertens. (2023) 36:446–54. doi: 10.1093/ajh/hpad037
55. Rimawi, A, Shah, A, Louis, H, Scales, D, Kheiran, JA, Jawabreh, N, et al. Community health worker program outcomes for diabetes and hypertension control in West Bank refugee camps: a retrospective matched cohort study. Glob Health Sci Pract. (2022) 10:e2200168. doi: 10.9745/GHSP-D-22-00168
56. Manavalan, P, Madut, DB, Wanda, L, Msasu, A, Mmbaga, BT, Thielman, NM, et al. A community health worker delivered intervention to address hypertension among adults engaged in HIV care in northern Tanzania: outcomes from a pilot feasibility study. J Clin Hypertens (Greenwich). (2022) 24:1095–104. doi: 10.1111/jch.14518
57. Shikany, JM, Safford, MM, Cherrington, AL, Halladay, JR, Anabtawi, M, Richman, EL, et al. Recruitment and retention of primary care practices in the southeastern collaboration to improve blood pressure control. Contemp Clin Trials Commun. (2023) 32:101059. doi: 10.1016/j.conctc.2023.101059
58. Thorogood, M, Goudge, J, Bertram, M, Chirwa, T, Eldridge, S, Gómez-Olivé, FX, et al. The Nkateko health service trial to improve hypertension management in rural South Africa: study protocol for a randomised controlled trial. Trials. (2014) 15:435. doi: 10.1186/1745-6215-15-435
59. Riddell, MA, Mini, GK, Joshi, R, Thrift, AG, Guggilla, RK, Evans, RG, et al. ASHA-led Community-based groups to support control of hypertension in rural India are feasible and potentially scalable. Front Med. (2021) 8:8. doi: 10.3389/fmed.2021.771822
60. Beasley, JM, Shah, M, Wyatt, LC, Zanowiak, J, Trinh-Shevrin, C, and Islam, NS. A community health worker–led intervention to improve blood pressure control in an immigrant community with comorbid diabetes: data from two randomized, controlled trials conducted in 2011–2019. Am J Public Health. (2021) 111:1040–4. doi: 10.2105/AJPH.2021.306216
61. Zhang, D, Wang, G, and Joo, H. A systematic review of economic evidence on community hypertension interventions. Am J Prev Med. (2017) 53:S121–30. doi: 10.1016/j.amepre.2017.05.008
62. He, J, Irazola, V, Mills, KT, Poggio, R, Beratarrechea, A, Dolan, J, et al. Effect of a community health worker-led multicomponent intervention on blood pressure control in low-income patients in Argentina: a randomized clinical trial. JAMA. (2017) 318:1016–25. doi: 10.1001/jama.2017.11358
63. Peiris, D, Praveen, D, Mogulluru, K, Ameer, MA, Raghu, A, Li, Q, et al. SMARThealth India: a stepped-wedge, cluster randomised controlled trial of a community health worker managed mobile health intervention for people assessed at high cardiovascular disease risk in rural India. PLoS One. (2019) 14:e0213708. doi: 10.1371/journal.pone.0213708
64. Pladevall, M, Brotons, C, Gabriel, R, Arnau, A, Suarez, C, de la Figuera, M, et al. Multicenter cluster-randomized trial of a multifactorial intervention to improve antihypertensive medication adherence and blood pressure control among patients at high cardiovascular risk (the COM99 study). Circulation. (2010) 122:1183–91. doi: 10.1161/CIRCULATIONAHA.109.892778
65. Cooper, LA, Roter, DL, Carson, KA, Bone, LR, Larson, SM, Miller, ER 3rd, et al. A randomized trial to improve patient-centered care and hypertension control in underserved primary care patients. J Gen Intern Med. (2011) 26:1297–304. doi: 10.1007/s11606-011-1794-6
66. Haverfield, MC, Tierney, A, Schwartz, R, Bass, MB, Brown-Johnson, C, Zionts, DL, et al. Can patient-provider interpersonal interventions achieve the quadruple aim of healthcare? A systematic review. J Gen Intern Med. (2020) 35:2107–17. doi: 10.1007/s11606-019-05525-2
Keywords: allied health personnel, lay advisors, community health workers, health care systems, implementation sciences, hypertension, RE-AIM
Citation: Patil SJ, Bhayani V, Yoshida Y, Bushweller L, Udoh E-O, Todorov I, Saper R, Stange KC and Bolen S (2024) Lay advisor interventions for hypertension outcomes: A Systematic Review, Meta-analysis and a RE-AIM evaluation. Front. Med. 11:1305190. doi: 10.3389/fmed.2024.1305190
Received: 07 November 2023; Accepted: 22 April 2024;
Published: 20 May 2024.
Edited by:
Komal Marwaha, Texas Tech University Health Sciences Center, United StatesReviewed by:
Elaine C. Khoong, University of California, San Francisco, United StatesCopyright © 2024 Patil, Bhayani, Yoshida, Bushweller, Udoh, Todorov, Saper, Stange and Bolen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sonal Patil, c3BhdGlsQG1ldHJvaGVhbHRoLm9yZw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.