
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 08 February 2024
Sec. Obstetrics and Gynecology
Volume 11 - 2024 | https://doi.org/10.3389/fmed.2024.1296910
Objective: This study aimed to evaluate perioperative antibiotic use for induced abortion and its association with lower genital tract infections (LGTI) two weeks post-surgery in China.
Methods: We conducted a prospective cohort study of women seeking induced abortion. We interviewed participants on the day of surgery and two weeks after, and evaluated preoperative tests, gynecological exams, perioperative antibiotic usage, postoperative vaginal microbiota, and LGTI diagnosis. Multivariate logistic regression was used to assess the association between the perioperative antibiotic use and LGTI risk.
Results: We recruited 8,190 women undergoing induced abortion at 27 participating hospitals. Of these, 95% had gynecological exams, but over 80% lacked tests for vaginal microbiota, chlamydia, and gonorrhea. Approximately 20% of those examined had increased vaginal discharge and abnormal vaginal cleanliness. The positive rates for gram-positive rods, fungi, and trichomonas were 38.6, 2.4, and 0.3%, respectively. More than three-quarters (78.5%) of participants received antibiotics, mainly second-gen cephalosporins (36.8%) and nitroimidazoles (12.3%). LGTI rates two weeks post-surgery were 2.7% for antibiotic recipients and 3.1% for non-recipients, with no statistically significant difference (p > 0.05). Logistic regression showed no association between perioperative antibiotic use and LGTI risk (OR = 1.01, 95% CI 0.59–1.74). However, this risk increased with abnormal preoperative discharge tests (OR = 1.39, 95% CI 1.04–1.86).
Conclusion: Most Chinese women undergoing induced abortion used perioperative antibiotics, but this did not significantly reduce LGTI risk. Instead, this risk was related to abnormal preoperative discharge tests. Standardization of perioperative antibiotic use for induced abortion is recommended, and prophylactic treatment in Chinese abortion services warrants further investigation.
• This study aims to address the knowledge gap regarding the practical effectiveness of perioperative antibiotic prophylaxis in induced abortion surgeries.
• This study challenges the efficacy of perioperative antibiotic prophylaxis during induced abortion in reducing postoperative lower genital tract infections, shedding light on potential reconsiderations of current medical practices.
Induced abortion is a legal procedure in China and is commonly used as a back-up or therapeutic method to terminate pregnancies due to unwanted or pathological pregnancies (1). The number of induced abortions in China in recent decades has been between 9 and 10 million per year, and the incidence of abortion was approximately 28.88 per 1,000 women of reproductive age in 2019 (2). Previous studies have shown that induced abortion may result in pain, bleeding, incomplete abortion, lower genital tract infection (LGTI) and other complications (3), and the risk of LGTI increases with the number of abortions (4). LGTI refers to infections that occur in the reproductive organs located in the lower part of the female reproductive system, such as the vagina and cervix (5), and was a common complication of induced abortion (6). It has been reported that the rate of infections requiring antimicrobial treatment after early induced abortion ranges from 0.01 to 2.44% (6). The presence of preoperative LGTI not only delays the optimal timing of treatment but also increases the risk of postoperative tubal adhesions, cervical adhesions, tubal obstruction, and chronic pelvic pain, as well as the risk of ectopic pregnancy, spontaneous abortion, placental adhesion, or implantation, thus significantly compromising women’s reproductive health (7). The World Health Organization’s “Safe Abortion: Technical and Policy Guidance for Health Systems” (8) recommends the prophylactic use of antibiotics to reduce the risk of infection following abortion. The American College of Obstetricians and Gynecologists (6) recommends the prophylactic use of antibiotics, preferably doxycycline, nitroimidazoles and tetracyclines, for all women undergoing a surgical abortion, but acknowledges the need to consider potential side effects. The Society of Obstetricians and Gynecologists of Canada (9) recommends the preoperative use of antibiotics, including doxycycline, metronidazole, and beta-lactams, for all women undergoing surgical abortion. These options are commonly used, and none is superior to others. The “Chinese Expert Consensus on the Prophylactic Use of Antibiotics in Induced Abortion (2019)” (10) and the “Chinese Expert Consensus on Screening, Diagnosis, and Treatment of LGTI during the Perioperative Period of Induced Abortion (2022)” (11) also recommend the prophylactic use of antibiotics, including doxycycline 200 mg, minocycline 200 mg, azithromycin 500 mg, or metronidazole 1 g before surgical abortion. However, there are few clinical studies evaluating the effectiveness of prophylactic use of antibiotics for induced abortion in China. We therefore conducted this multicentre prospective cohort study to understand the status of preoperative laboratory and gynecological examinations and perioperative antibiotic use in induced abortion and their association with LGTI, with the aim of providing evidence for clinical practice in abortion services in China.
A total, 27 hospitals with outpatient induced abortion services were selected from 16 provinces in the eastern (Fujian, Shandong, Shanghai, Tianjin, Zhejiang), central (Guangxi, Jilin, Jiangxi, Shanxi) and western (Inner Mongolia, Guizhou, Shaanxi, Xinjiang, Yunnan, Sichuan, Chongqing) regions of China. Each institution recruited women who met the inclusion criteria for induced abortion on a continuous basis for two consecutive months in 2019.
We conducted this prospective observational cohort study, which was approved by The Ethics Committee of the Shanghai Institute of Planned Parenthood research (IRB number: PJ2019-22). Women seeking an induced abortion at the study sites were invited to participate in this study. Inclusion criteria for participants were as follows: women aged 18 years or older, intrauterine pregnancy confirmed by ultrasound, voluntary acceptance of induced abortion In early pregnancy (<10 gestational weeks), no contraindications to surgical abortion, being able to understand and answer survey questions, being willing to participate in this study and sign an informed consent form, and being willing to undergo follow-up when returning for a medical examination two weeks after surgery. Patients were excluded if they had undergone an in-patient abortion, medical abortion, spontaneous abortion, or other pathological abortion, if they had a serious chronic disease, or if the physician deemed them inappropriate to participate in this study.
Participants underwent routine pre-and post-operative examinations, and laboratory tests at the hospital. Data on the examinations and tests were extracted from the hospital’s electronic medical record, including temperature, pulse, and relevant gynecological examinations such as the cervix, uterus, and adnexa; detection of vaginal microbiota morphology such as vaginal cleanliness, discharge, and microbial flora; the metabolic products of aerobic bacteria, anaerobic bacteria, fungi, trichomonas, and pH value, etc. Information on antibiotic use was collected at the follow-up interviews two weeks after surgery, including the name of the antibiotics, use dosage, medication regimen, and duration of use. The diagnosis of LGTI was extracted from participants’ medical records, which was diagnosed mainly based on associated symptoms (itching or burning of the vulva), and lab examination of vaginal discharge. We added up the abnormal results of all the laboratory tests and defined a new variable to measure the number of abnormal vaginal discharge tests.
We used EpiData 3.1 for data entry and R 4.0.2 software for data analysis. We used frequencies and percentages to describe the distribution of categorical data, and the chi-squared test to compare the difference in the distribution between categories of baseline characteristics. In addition, a two-level multivariate logistic regression model was used to control for potential confounders and to examine the effectiveness of perioperative antibiotic use on LGTI at two weeks postabortion. A p-value of less than 0.05 was considered statistically significant.
A total of 8,190 women who underwent induced abortion were recruited for this study. Most participants were from tertiary hospitals (84.7%) and maternal and child hospitals (MCHs) (56.4%). The average age of the participants was 29.69 ± 5.98 years, with the majority aged 26–35 years (55.7%). Most participants (72.1%) were married, 40.4% had a bachelor’s degree or higher education level, and 22.5 and 38.4% were employed in manual and intellectual labor, respectively. The majority (73.9%) had their first sexual experience between the ages of 18 and 25 years. The majority (91.9%) reported no sexual intercourse during menstruation, and 59.8% had a history of gynecological and/or obstetric infectious diseases. (Table 1).
As presented in Table 2, the majority of participants had routine gynecological examinations. For example, uterine mobility and tenderness, cervical tenderness, lower abdominal tenderness, pelvic examination, and perianal examination were reported in over 95% of women, and body temperature, cervical smear, and external genitalia were reported more than 80% of participants. Abnormal findings are generally low, most ranging from 0.2 to 0.6%, with a few over 2%, and cervical erosion (21.3%) and cervical smear color (8.4%) being the most common abnormalities.
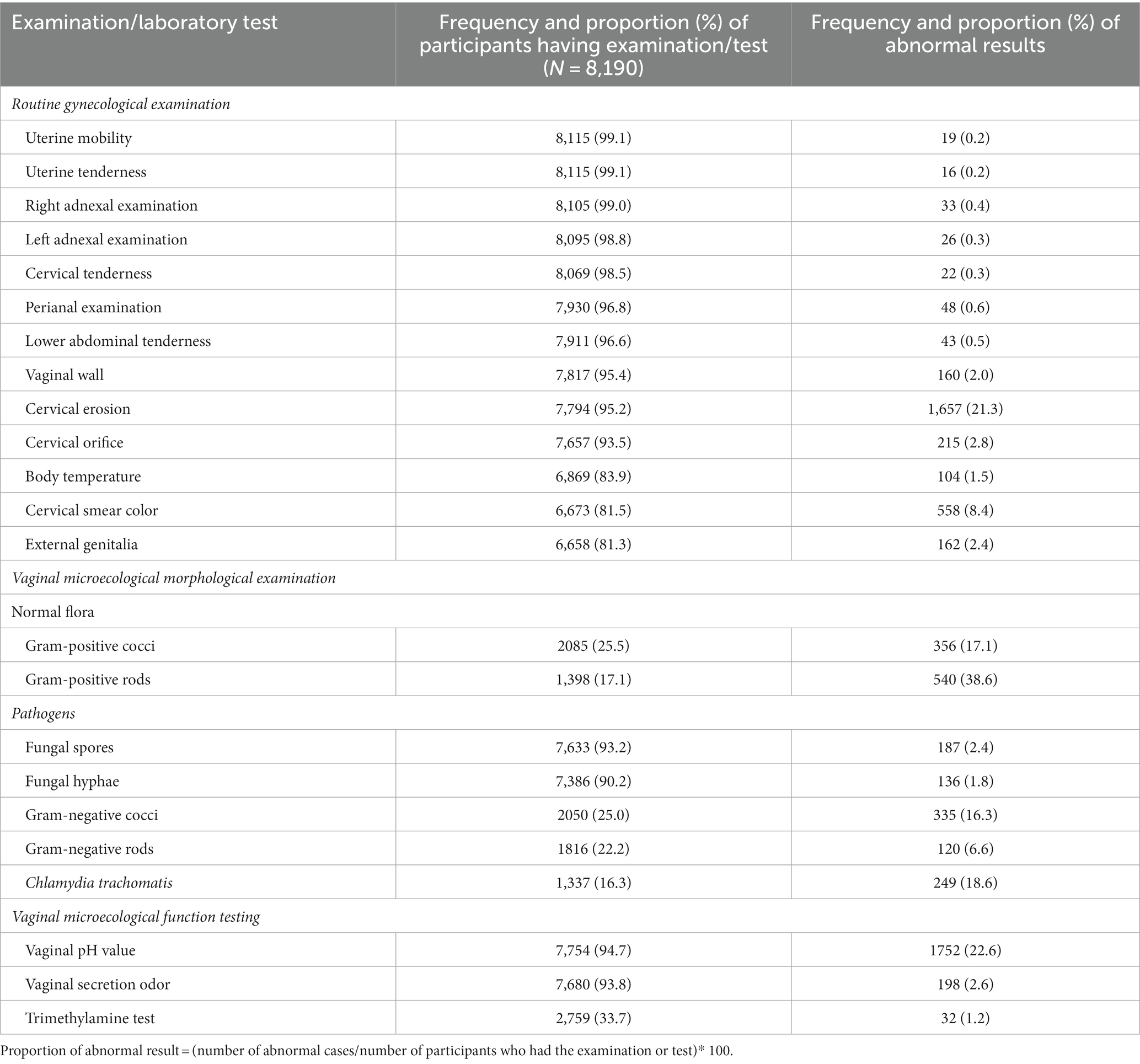
Table 2. Routine gynecological examinations and vaginal microecological laboratory tests for women seeking abortion services.
Testing for vaginal microecological morphology varied between normal flora and potential pathogens. A quarter or less had been tested for gram-positive cocci (25.5%) and rod (17.1%), with positive rates of 17.1 and 38.6%, respectively. A similar proportion of women had been tested for gram-negative cocci (25.0%) and rods (22.2%) and Chlamydia trachomatis (16.3%), with positive rates of 16.3, 6.6 and 18.6%, respectively. More than 90% had fungal spore and hyphae testing, of which 2.4 and 1.8% were positive, respectively.
Trimethylamine, vaginal secretion odor and pH value are indicators of vaginal microecological function. One third of the women had a trimethylamine test, and about 94% had vaginal secretion and PH value tests, with positive rates of 1.2, 2.6 and 22.6%, respectively.
Of all the study participants, 78.5% (6,427) used antibiotics in the perioperative period, and all the antibiotics were included in the Chinese guideline. The use of antibiotics was significantly higher in second-level MCHs (96.0%, 1,899/2,318) than in tertiary general hospitals (81.9%, 1,899/2,318), tertiary MCHs (75.0%, 3,462/4,618), and second-level general hospitals (74.2%, 470/633) (p < 0.001). The most commonly used antibiotics were second-generation cephalosporins (36.8%, 2,367), followed by nitroimidazoles (12.3%, 788), macrolides (7.5%, 484), tetracyclines (4.9%, 312), and lincomycin (3.4%, 220). Only 51 women (0.8%) used quinolones. In addition, 126 women (2.2%) used antifungals. Of all the antibiotic users, 4,297 (66.9%) used only one type of antibiotic, most commonly the second-generation cephalosporins (37.1%, 1,593); 964 (15.0%) used two or three types of antibiotics, with more than half (482) combining nitroimidazoles and second-generation cephalosporins (Table 3).
Table 4 shows the incidence of LGTI by women’s characteristics. As can be seen in the table, the incidence of LGTI in women who used antibiotics and those who did not was 2.7 and 3.1%, respectively. The result of the chi-square test shows no significant difference in the rate between the two groups (p = 0.513). In addition, we used a two-level logistic regression model adjusting for hospital factors, women’s demographics, and perioperative variables, and found no significant difference in the risk of LGTI two weeks post-induced abortion between those using antibiotics and those not using them (OR = 1.01, 95% CI 0.59–1.74). However, the risk increased with the number of abnormal discharge tests (OR = 1.39, 95% CI 1.04–1.86). No significant associations were observed with hospital factors, women’s demographics, and age at first sexual intercourse (Table 4).
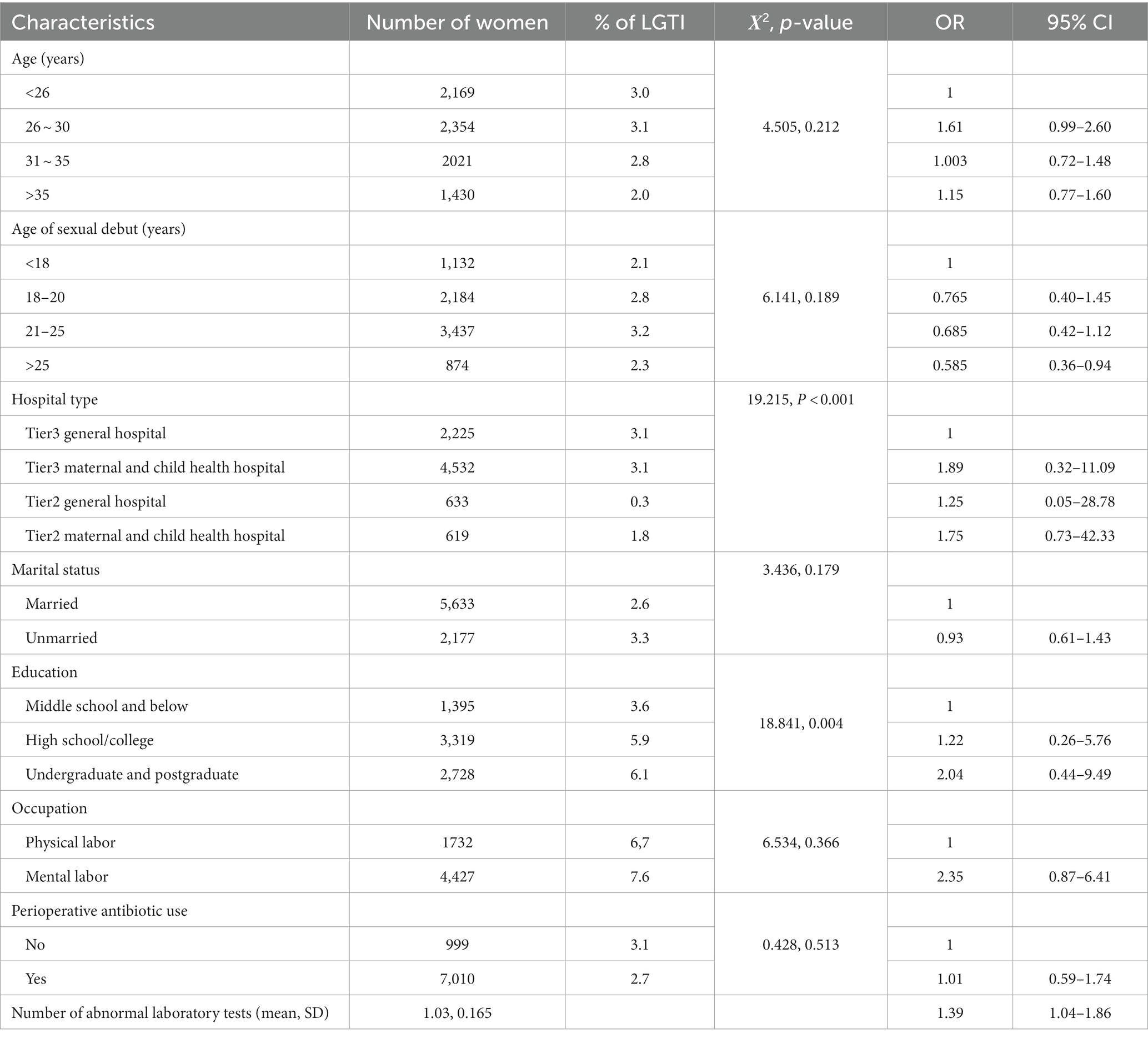
Table 4. Lower genital tract infection (LGTI) two weeks after abortion: incidence by women’s characteristics and results of two-level logistic regression analysis.
The surgical procedure of induced abortion is considered to be a clean-contaminated procedure, as it causes a degree of trauma to the female uterine cavity, which can disrupt the normal barrier function of the cervix (10). For this reason, routine screening for LGTI is usually required before induced abortion. This study found that the majority (>90%) of patients in China underwent routine vaginal secretion tests and gynecological examinations before abortion. Although these tests and examinations were inexpensive and easily accessible for general screening purposes, they may not detect specific pathogenic microorganisms. More than 70% of women undergoing induced abortion in this study were not tested for potentially pathogenic microorganisms in the vagina, such as gram-negative/positive cocci/bacteria, mycoplasma, and chlamydia. This posed a higher risk of missed diagnoses, as pathogenic microorganisms may enter the uterine cavity through the cervix during the invasive procedure, leading to complications such as uterine and pelvic infections, and, in the long term, tubal obstruction (11). We recommend an increase in testing for vaginal pathogenic microorganisms prior to an induced abortion surgery to facilitate timely intervention and to reduce the risk of LGTI following the procedure.
Findings of this study showed that abnormal amount of vaginal discharge and abnormal vaginal cleanliness were most frequent in Chinese women seeking abortion services, accounting for about one-fifth of participants who had a vaginal examination. These results were similar to those reported by Sun and colleagues in China (19.6%) (12). The results of the vaginal microbiota testing showed that the prevalence of gram-positive cocci and bacilli, and gram-negative cocci and bacilli was 38.6, 17.1, 16.3 and 6.6%, respectively, and the prevalence of fungi and trichomonas was 2.4 and 0.3%, respectively. These findings suggest that a significant number of Chinese women undergoing induced abortion were positive for conditional vaginal pathogenic microorganisms. Providers should pay due attention to screening for vaginal pathogens before performing abortion.
Approximately four out of five (78.5%) of women undergoing induced abortion received prophylactic antibiotic treatment in the perioperative period. Either the international guidelines [i.e., the World Health Organization’s “Safe Abortion: Technical and Policy Guidance for Health Systems” (8) and the American College of Obstetricians and Gynecologists’ “SFP guideline 20,102” (6)] or the national expert consensus [i.e., the “Chinese Expert Consensus on the Prophylactic Use of Antibiotics in Induced Abortion (2019)” (10)] recommend the prophylactic use of antibiotics before induced abortion surgery. However, a significant proportion of service provides in China did not follow these recommendations. Unexpectedly, the antibiotic use rate was lower in general hospitals and tertiary hospitals than in MCHs and secondary hospitals. This may be due to the differences in evaluation regulations between hospitals in China regarding the antibiotic use. According to the “Circular on Further Strengthening the Management of Antimicrobial Drugs to Curb Drug Resistance “issued by the Ministry of Health (13), the use of antimicrobial drugs is included as an indicator in the evaluation of hospital level and clinical performance. The top-to-bottom hospital evaluation regulation may need be revised to allow the use of antibiotics in abortion services in all levels and types of hospitals to avoid conflicts between clinical need and hospital evaluation regulations.
Previous studies have shown that the pathogens of LGTI after induced abortion are mainly Escherichia coli, Staphylococcus aureus, and sexually transmitted pathogens such as Neisseria gonorrhoeae and Chlamydia trachomatis (6). The “Chinese Expert Consensus on the Prophylactic Use of Antibiotics in Induced Abortion (2019)” (10) suggests that prophylactic antibiotics should be effective against aerobic bacteria, anaerobic bacteria, and sexually transmitted disease pathogens. Second-generation cephalosporins, metronidazole, doxycycline, and azithromycin are recommended for first-line use. In this study, we found that the most commonly used antibiotics during the perioperative period of induced abortion in China were second-generation cephalosporins (36.8%), which are effective against gram-positive cocci and gram-negative bacilli. Nitroimidazoles was the second most used antibiotics (12.3%). Previous literature reports that anaerobic spore bacteria are common in postoperative infections after gynecological surgery, and nitroimidazoles are the preferred drugs for the treatment and prevention of anaerobic bacterial infections and trichomoniasis (14). Macrolides accounted for 7.5%, tetracyclines 4.8% and quinolones 0.8% of the antibiotics used. Azithromycin, tetracycline, and quinolones (e.g., levofloxacin) are mainly used to treat Chlamydia trachomatis and Mycoplasma dentalium (14). In the group of women who received two or more types of antibiotics, more than half of them used both nitroimidazoles and second-generation cephalosporins. This combination is one of the drug regimens recommended by the Chinese expert consensus (10).
Furthermore, with an increase in the number of induced abortion procedures, the risk of genital tract infection increases correspondingly (11). This study found that the incidence of LGTI was lower in women who used antibiotics in the perioperative period (2.7%) than that in non-users (3.1%), but the difference was not statistically significant. This conclusion remained after controlling for potential confounders using a two-level multivariate logistic regression model. The main reason for this may be that this study was conducted in a real-world setting and did not establish standardized protocols for antibiotic use and diagnosis of LGTI. The lack of standardization may have led to a certain degree of misclassification and under-diagnosis of LGTI, thereby reducing the effectiveness of antibiotic prophylaxis. Nevertheless, we found that the more positive tests in the preoperative vaginal discharge, the higher the risk of postoperative LGTI (OR = 1.39, 95% CI 1.04–1.86). For those with more than one abnormal vaginal discharge test, we recommend testing for vaginal pathogenic microorganisms and administering antibiotics accordingly.
In summary, about four out of five women who had an induced abortion in China took antibiotics in the perioperative period. However, the use of antibiotics did not significantly reduce the risk of LGTI two weeks after abortion. Instead, the risk was significantly associated with the number of abnormal preoperative vaginal discharge tests. We recommend that the use of antibiotics in the perioperative period of induced abortion should be further standardized. In addition, the effectiveness of prophylactic treatment in the abortion service in China needs further study.
This study was conducted in 27 hospitals in 16 out of 31 provinces in mainland China with a sample size of 8,190. To our knowledge, this is the largest study compared with previous similar studies in China. However, it should be noted that this is an observational study conducted in a real-world setting. The diagnostic of LGTI and laboratory testing methods may vary between hospitals, leading to potential information bias in the results.
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding authors.
The studies involving humans were approved by the Medical Ethical Committee, Shanghai Institute of Planned Parenthood Research. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
JD: Writing – original draft. YZ: Data curation, Writing – review & editing. XG: Writing – review & editing. YC: Funding acquisition, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The Chinese Society of Family Planning, Chinese Medical Association coordinated this study. The authors sincerely thank Zhang Xuesong, Yao Xiaoying, Qian Zhida, Teng Lirong, Wang Yu, and Liao Shujie, who acted as the provincial coordinators, and all the hospital investigators who contributed greatly to this study’s data collection, including Xiaoye Wang (Third Hospital of Peking University), Yuan Lin (Fujian Provincial Maternity and Child Health Care Hospital), Xiaoli Jiang (First Affiliated Hospital of Guangxi Medical University), Ya Zhang (People’s Hospital of Xishui County, Guizhou Province), Xiaoling Hu (Jilin Provincial Maternity and Child Health Care Hospital), Liqun Wang (Jiangxi Provincial Maternity and Child Health Care Hospital), Jing Li (People’s Hospital of Jinxi County), Yu Wang (Shengjing Hospital, China Medical University), Jiandong Song (Inner Mongolia Medical University Affiliated Hospital), Yu Lin (Shandong Provincial Maternity and Child Health Care Hospital), Xinying Du (People’s Hospital of Weifang City, Shandong Province), Li Shan (Northwest Women and Children’s Hospital), Lina Zhang (Taiyuan Maternal and Child Health Care Hospital), Xiaoying Yao (Fudan University Affiliated Obstetrics and Gynecology Hospital), Jing Wang (Dahua Hospital, Shanghai), Xiangying Gu (Tianjin Medical University General Hospital), Jianmei Wang (Second Hospital of Tianjin Medical University), Caixia Yang (Baodi District People’s Hospital, Tianjin), Anxin Xia (Tianjin Permanent Hospital), Xiaojun Wang, Xianfeng Li (Xinjiang Uygur Autonomous Region Maternity and Child Health Care Hospital), Juan Li (Honghe Prefecture Maternity and Child Health Care Hospital, Yunnan Province), Xu (Chuxiong Prefecture Maternity and Child Health Care Hospital, Yunnan Province), Chaying He (Hangzhou Maternity and Child Health Care Hospital), Xiaojie Wu (Jiaxing Maternity and Child Health Care Hospital), Weixin Liu (Sichuan Provincial Maternity and Child Health Care Hospital), Xiaojing Dong (The Second Affiliated Hospital of Chongqing Medical University), Jing Guo (Xi’an Central Hospital).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Wang, T, and Jiang, Q. Recent trend and correlates of induced abortion in China: evidence from the 2017 China fertility survey. BMC Womens Health. (2022) 22:469. doi: 10.1186/s12905-022-02074-5
2. National Health Commission of the People's Republic of China . China health and wellness yearbook. Beijing: China Health and Wellness Yearbook Press (2023).
3. Islam, N, Furuya-Kanamori, L, Mahmood, S, and Thalib, L. Prophylactic antibiotics for preventing genital tract infection in women undergoing surgical procedures for incomplete abortion: a systematic review and meta-analysis of randomised controlled trials. BJOG Int J Obstetr Gynaecol. (2021) 128:1273–81. doi: 10.1111/1471-0528.16637
4. Zhang, RJ, Zhang, XJ, Lv, XJ, Zhu, YP, Ge, XJ, Huang, W, et al. Study on the correlation between induced abortion and reproductive tract infections. Zhonghua Liu Xing Bing Xue Za Zhi. (2011) 32:29–32.
5. Brunham, RC, and Paavonen, J. Reproductive system infections in women: lower genital tract syndromes. Pathogens Dis. (2020) 78:1–9. doi: 10.1093/femspd/ftaa022
6. Achilles, SL, and Reeves, MF. Prevention of infection after induced abortion: release date October 2010: SFP guideline 20102. Contraception. (2011) 83:295–09. doi: 10.1016/j.contraception.2010.11.006
7. Ravel, J, Moreno, I, and Simón, C. Bacterial vaginosis and its association with infertility, endometritis, and pelvic inflammatory disease. Am J Obstet Gynecol. (2021) 224:251–7. doi: 10.1016/j.ajog.2020.10.019
8. WHO . WHO guidelines approved by the guidelines review committee. Clinical practice handbook for safe abortion. Geneva: World Health Organization Copyright © World Health Organization (2014).
9. Costescu, D, and Guilbert, É. No. 360-induced abortion: surgical abortion and second trimester medical methods. J Obstetr Gynaecol. (2018) 40:750–83. doi: 10.1016/j.jogc.2017.12.010
10. Chinese Medical Association Family Planning Branch . Consensus of Chinese experts on the prophylactic use of antimicrobial drugs in induced abortion surgery. Chin J Fam Plann Gynecol. (2019) 11:10–2.
11. Chinese Medical Association family planning branch, Chinese Medical Association obstetrics and gynecology branch infectious disease collaboration group, Chinese eugenics and eugenics association reproductive health and birth defect prevention professional committee . Consensus of Chinese experts on screening, diagnosis, and treatment of reproductive tract infections during the perioperative period of induced abortion. Chin J Pract Gynecol Obstetr. (2022) 10:996–00.
12. LLS . Analysis of influencing factors and preventive measures for reproductive tract infections in women undergoing induced abortion. Pract Prevent Med. (2012) 19:1365–6.
13. Xiao, Y, Shen, P, Zheng, B, Zhou, K, Luo, Q, and Li, L. Change in antibiotic use in secondary and tertiary hospitals Nationwide after a National Antimicrobial Stewardship Campaign was Launched in China, 2011-2016: an observational study. J Infect Dis. (2020) 221:S148–55. doi: 10.1093/infdis/jiz556
Keywords: induced abortion, antibiotics, lower genital tract infection, risk, perioperative period
Citation: Ding J, Zhang Y, Gu X and Che Y (2024) Failure to reduce the risk of postoperative lower genital tract infection with perioperative antibiotic prophylaxis during induced abortion: a real-world study. Front. Med. 11:1296910. doi: 10.3389/fmed.2024.1296910
Received: 04 October 2023; Accepted: 25 January 2024;
Published: 08 February 2024.
Edited by:
Andrea Tinelli, Veris delli Ponti Hospital, ItalyReviewed by:
Nongyao Kasatpibal, Chiang Mai University, ThailandCopyright © 2024 Ding, Zhang, Gu and Che. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: XiangYing Gu, Z3h5NjI4M0AxNjMuY29t; Yan Che, Y2hleWFuMjAwNEAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.