- 1Institute for Global Health Innovations, Duy Tan University, Da Nang, Vietnam
- 2Faculty of Nursing, Duy Tan University, Da Nang, Vietnam
- 3Department of Global Public Health, Karolinska Institutet, Stockholm, Sweden
- 4Hanoi Obstetrics and Gynecology Hospital, Hanoi, Vietnam
- 5Institute of Health Economics and Technology (iHEAT), Hanoi, Vietnam
- 6Bloomberg School of Public Health, Johns Hopkins University, Baltimore, MD, United States
- 7Lee Kong Chian School of Medicine, Nanyang Technological University Singapore, Singapore, Singapore
- 8Department of Psychological Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
- 9Institute for Health Innovation and Technology (iHealthtech), National University of Singapore, Singapore, Singapore
Background: Understanding childbirth delivery and pain relief method preferences is important as a part of the shared decision-making process between pregnant women and health professionals. This study aimed to examine the preferences for childbirth delivery modes and pain relief methods and factors related to these preferences among pregnant women in Vietnam.
Methods: A cross-sectional survey on pregnant women was conducted in two obstetrics hospitals in Vietnam. Face-to-face interviews using a structured questionnaire were performed to collect information about sociodemographic characteristics, pregnancy characteristics, preferences for different childbirth delivery modes, and pain relief methods. Multivariate logistic regression was employed for determining associated factors with the preferences.
Results: Of 576 pregnant women, 34% of participants preferred cesarean section. Most of the sample did not have any preferences for specific pharmacological pain relief methods (70.1%), while support from partner/relatives was the most preferable non-pharmacological method (61.3%), following by water birth (11.1%) and acupuncture (9.9%). Desire to have another baby, relatives’ experience, selection date of birth, and instrumental social support were major drivers of the cesarean section selection. This preference was an important factor in the preference for pharmacological pain relief. Meanwhile, high levels of informational and emotional support were associated with non-pharmacological method preference.
Conclusion: This study highlighted a high preference rate for cesarean section in urban pregnant women in Vietnam. Holistic approaches from family, health facility, and policy should be performed to diminish the cesarean rate preference and promote the use of non-pharmacological pain relief methods during birth.
1 Introduction
The choice of childbirth delivery method is one of the most crucial concerns of women before and during pregnancy (1, 2). Vaginal delivery has advantages including less postpartum pain, fewer labor and delivery complications, requiring a short hospital stay, and the immediate ability to breastfeed (3). However, this method cannot be performed if the pregnant women have some specific conditions such as a large baby, head-pelvis incompatibility, or fetal distress, where cesarean delivery is preferable as a lifesaving method for both mothers and children (4, 5). In general, cesarean deliveries are recommended that should be performed for medical reasons, not due to preferences (5). Because, the cesarean section may pose great complications like hysterectomy, abnormal placentation, uterine rupture, or stillbirth, as well as increase the risk of preterm birth in the next pregnancies (6).
The rate of cesarean section is rising by over 15% in many nations worldwide exceeding the cesarean rate recommended by World Health Organization (WHO) (7). Particularly, global literature recognized that overall, approximately 21.1% of pregnant women preferred cesarean section (8), and this rate varied across countries, especially high-income countries such as 34% in Australia, 32.2% in the United States, 26.2% in the United Kingdom, 26% in Canada, and 50.4% in Turkey (8). Furthermore, this review has indicated that several factors such as fear of labor pain and safety of baby, previous birth experience, fear of postnatal complications, consultation of health professionals, social and cultural influences, and access to information are recognized pervasive causes of this phenomenon (8). Besides, the preference for cesarean section is more common among women aged over 30, living in urban settings, having higher socioeconomic status, and fearing vaginal delivery than others (9, 10). This preference is also observed in pregnant women with high gestation weeks. Particularly, the rate of preference for cesarean section changed from 14% in the first trimester to 21% in the third trimester (11).
Another part of decision-making during childbirth delivery is the pain relief method. There are two types of pain relief methods during the labor process including pharmacological and non-pharmacological interventions (12). Pharmacological interventions consisted of the use of epidurals and opioids, while non-pharmacological interventions included massage and relaxation methods such as yoga, music, breathing techniques, shiatsu, reflexology, and others. Several previous publications proved that the main reason for women’s preference for pharmacological and cesarean section is their fear of suffering severe pain during childbirth and lack of knowledge regarding the possible adverse consequences of these methods after delivery (8, 13). Particularly, although pharmacological methods may more effectively reduce labor pain, they may have several negative side effects such as postnatal back pain and difficulty in breastfeeding (14). Meanwhile, non-pharmacological methods, which can be performed by the husband/relatives or healthcare workers not only can decrease labor pain but also reduce the risk of childbirth complications among those using analgesia (15). Moreover, these methods enhance bonding between pregnant women with midwives and obstetricians (14) as well as enhance the feeling of joyfulness and empower women in childbirth delivery (14), reduce childbirth fear (16), diminish the labor time and elevate the satisfaction after delivery compared to the pharmacological interventions (17, 18). Thus, timely providing appropriate pain relief methods is a critical factor in reducing the preference for cesarean delivery. Furthermore, women can find information related to pain relief methods in some sources such as family and friends, healthcare professionals, books, the internet, and antenatal classes before and during pregnancy to select preferable pain relief methods for themselves (19–21).
In Vietnam, the Ministry of Health enacted nationwide guidelines for reproductive health services in 2017 (22). However, these guidelines have mainly focused on medical techniques of childbirth and postnatal care for the mother as well as the child (22). There is no recommendation regarding the rate of the cesarean section, even though this method has been overused in Vietnam, particularly in urban areas (23). The rate of cesarean delivery has remarkedly increased from 9.9% in 2002 to 27.5% in 2021 (24). The cesarean section rate was higher in urban areas (38.5%) than that in rural areas (12.4%) (25). In Vietnam, only one qualitative study was performed to determine the perceptions of pregnant women on the factors associated with the significant increase of cesarean section (4) and the findings indicated that fear of labor pain was the main reason for this phenomenon. Besides, there is a lack of quantitative evidence about this issue. Moreover, the preference for pain relief methods among pregnant women has not yet been investigated in Vietnam. To date, all obstetrics hospitals in Vietnam provided pharmacological interventions to release the labor pain according to the guideline, but non-pharmacological intervention services have not been yet mentioned or delivered. This study aimed to examine the preferences for childbirth delivery modes and pain relief methods and factors related to these preferences among pregnant women in Vietnam. The findings of this study would partly contribute to evaluating the feasibility and acceptability of non-pharmacological methods in labor pain relief.
2 Methods
2.1 Study design and participants
A cross-sectional study was conducted in two hospitals in Vietnam, including Hanoi Obstetrics & Gynecology hospital and Ca Mau Obstetrics & Pediatrics provincial hospital from January to February 2021. The eligibility criteria for participating as follows: (1) Aged 18 and older; (2) Agree to participate in research; (3) Planning to deliver in the selected hospital; (4) Being able to answer the interview questionnaire; and (5) Visit the hospital for regular antenatal care during the study period. Pregnant women were conveniently approached and recruited for this study when they visited these hospitals.
In this study, sample size computations were performed to estimate population proportion with a specified relative precision. We used confidence level (%) α = 0.05, expected population proportion p = 39% (26), and relative precision ε = 0.1. To prevent not responses or dropout, we added 15% of the sample size, resulting in the necessary sample size was 690 participants. At the end of the data collection process, 669 participants agreed to participate in this study (response rate = 95%). After excluding those not completing the questionnaire about delivery method, using pain relief with/ without medicine, the data of 576 participants were included in the data analysis process (completion rate 86.1%).
2.2 Data collection and measurement
In this study, a structured questionnaire was used for face-to-face interviews. To construct this research instrument, a standard procedure was applied. In the first stage, we carried out a systematic review to explore the gaps in research problems as well as important facets of the topic of interest from the previous evidence. From that, an initial research instrument was developed and covered all aspects of the topic of interest. In all stages of the research questionnaire development process, we invited several experts in obstetrics and gynecology, health services providers, and policymakers to jointly discuss and deliberate from the translating, rephrasing, piloting, as well as shortening the questionnaire.
The final version of the research instrument consists of five major components: 1) Demographic characteristics; 2) Pregnancy characteristics; 3) Preference for delivery method and reasons; 4) Preference for pain relief during and after delivery (with pharmacological and non-pharmacological interventions) and reasons, and 5) Social support. Furthermore, before the official data collection processing, we piloted this questionnaire among 30 pregnant women of different ages, periods of pregnancy, and living locations to test the language, logical order, and meaning of each question of the research instrument once again. After the research instrument had been revised, we removed all of the piloted data. During the data collection process, face-to-face interviews with participants were conducted within 15–20 min by research team members who were well-trained to use the research instrument.
2.2.1 Demographic and pregnancy characteristics
Participants were asked a number of questions about their information, including age, education, occupation, living arrangement, and monthly household income. Pregnancy characteristics consisted of the number of pregnancies, complications of pregnancy, source of maternal care information (health professionals, internet/social networks, friends/relatives, radio & television, smartphone applications, newspapers & books, phone messages, or posters/banners) and desire to have another baby. Fear of childbirth was asked with 11-point rating scales from 0 “No fear” to 10 “Extreme fear.” We also asked pregnant women that whether they decided the day and time for childbirth for fortune or not.
2.2.2 Preferences for childbirth delivery methods
To ask participants about the type of preferred delivery method, we used the question “What delivery method do you prefer during this pregnancy?” with 2 answer options (Vaginal delivery/Caesarean). Besides, other questions related to the reasons for choosing the type of delivery (Experience from a previous pregnancy/ Consultation of healthcare staff/ Experience from acquaintances, friends/ Consider my physical health/ Consider the cost/ Others), “Has your family members ever had a cesarean section?” or “Did you ever heard about cesarean section?” with answer options (Yes/No).
2.2.3 Preferences for pain relief methods
A question “Which pharmacological method do you prefer for pain relief during childbirth delivery?” was used with different response options (e.g., Do not use/ Spinal anesthesia/ Epidural anesthesia/ Intravenous/ Intramuscular Labor Pain Relief/ Depends on the doctor). In addition, we asked the reasons for the preference (including experience from a previous pregnancy; experience from acquaintances/friends; consultation of healthcare staff; consider physical health; consider the cost; and others).
Another question, “Do you want to use non-pharmacological pain relief method?” was asked to learn about the non-pharmacological method that participants wanted to use such as relatives support and care during delivery, using water for pain relief, hypnotherapy for pain relief, acupuncture, acupressure pain relief, or transcutaneous electrical stimulation for pain relief.
Preferable methods of pain relief after childbirth were also asked participants with options including Do not use/ Epidural and continuous anesthesia for 48 h after surgery/ Infusion of pain relievers intravenously 6 h or vial/ Injections of pain relievers or morphine/ Put pain relief in the anus/ Depends on the doctor/ Others. The reason for this preference was also asked.
2.2.4 Social support
The Perinatal Infant Care Social Support (PICSS) instrument was used to evaluate social support (27). This instrument consisted of 22 items and divided into four subscales: Informational support (7-item); Instrumental support (7-item); Emotional support (4-item); Appraisal support (4-item). A 4-Likert scale was used to respond for each item, from 1 “Totally disagree” to 4 “Totally agree.” The total score of each subscale was summed, and a higher score indicated higher social support. The Cronbach’s alpha was good at 0.85.
2.3 Statistical analysis
Stata software version 16 was used to analyze the data. Descriptive statistical analysis was performed. Chi-squared and Wilcoxon rank-sum tests were utilized to compare sociodemographic characteristics, pregnancy characteristics, reasons for preferring childbirth delivery methods, preferable pain relief methods between those preferring vaginal delivery and cesarean section. A value of p (p) <0.05 was considered statistically significant. Multivariate Logistic Regression models were employed to determine factors associated with the preferable types of delivery method and pain relief methods during childbirth. A forward stepwise selection was used to construct the reduced model, which only included independent variables having a value of p of log-likelihood ratio test less than 0.2.
3 Results
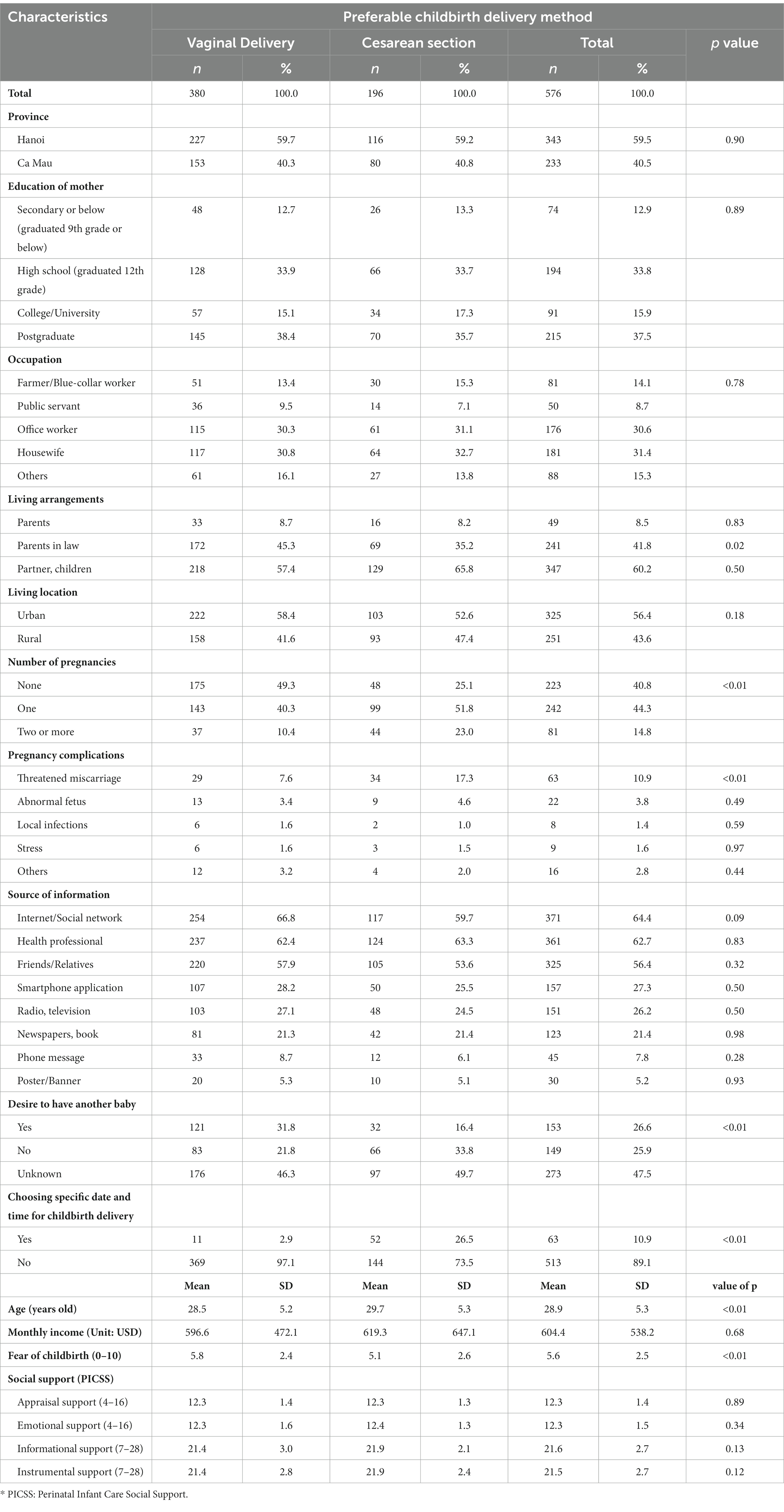
Table 1 shows that among 576 pregnant women, 34% of participants preferred cesarean section (95%CI = 30.1–38.1%), while 66.0% of them preferred vaginal delivery (95%CI = 61.9–68.8%).
Among 576 pregnant women, the mean age was 28.9 years (Table 2). Table 2 also shows that the significant differences between those preferring vaginal delivery and cesarean section were observed regarding age, living with parents-in-law, the number of pregnancies, having experience with threatened miscarriage during pregnancy, desire to have another baby, choosing a specific date and time for delivery, and fear of childbirth (p < 0.05).
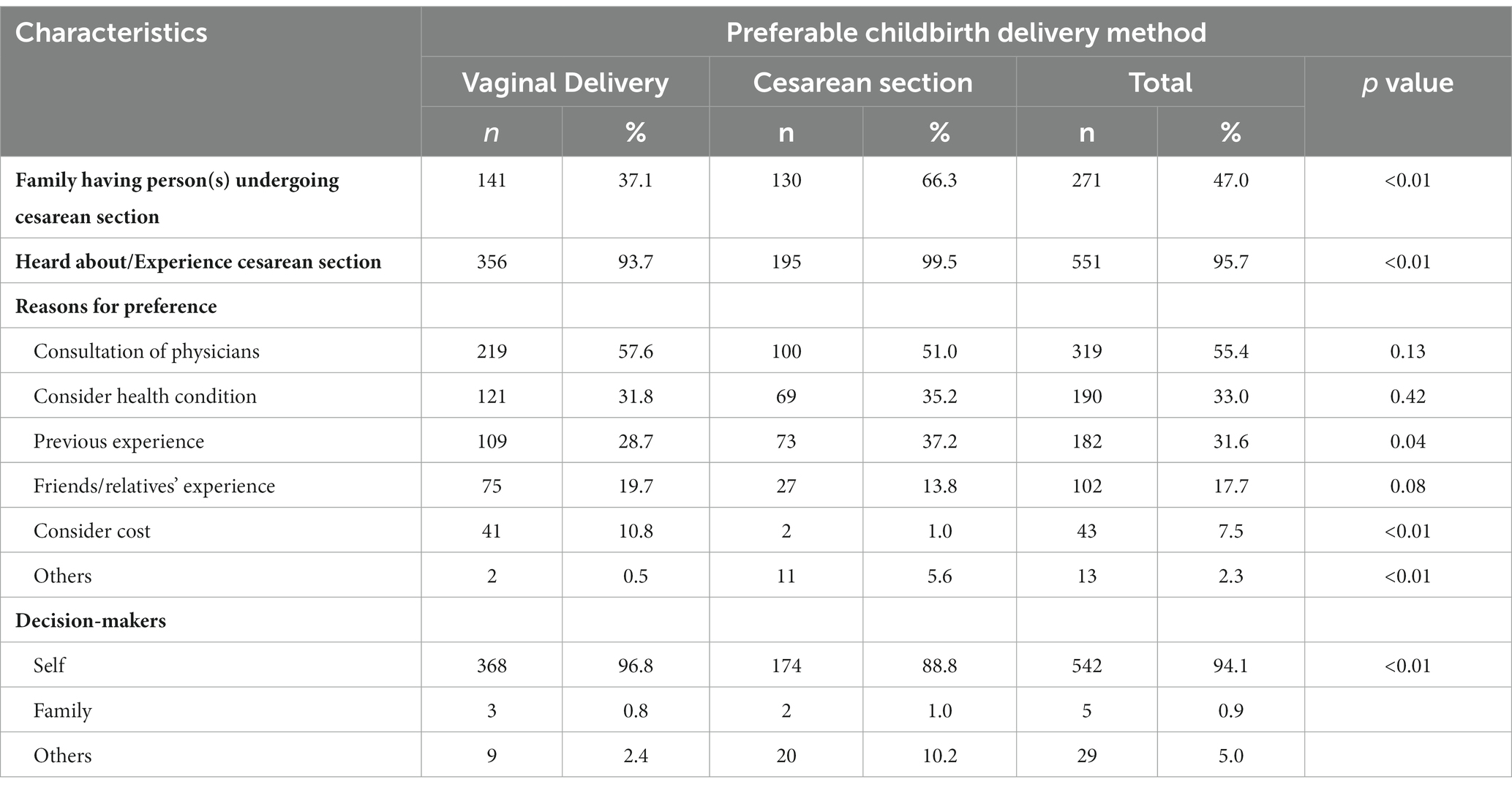
Table 3 indicates that out of the participants who preferred cesarean section, there were 66.3 and 99.5% of them had other family members undergoing the same delivery method and had heard/experienced the cesarean section method, respectively. In terms of the reason for delivery mode preferences, consultation of physicians (vaginal delivery: 57.6% and cesarean section: 51.0%) was the most common reason for both vaginal delivery preference and cesarean section preference, followed by considering health condition (vaginal delivery: 31.8% and cesarean section: 35.2%), and previous experience (vaginal delivery: 28.7% and cesarean section: 37.2%). The delivery methods among the participants were mostly decisions by themselves or their families. However, the proportion of participants preferring cesarean section and vaginal delivery based on the consult from others (such as physicians) was 10.2 and 2.4%, respectively.
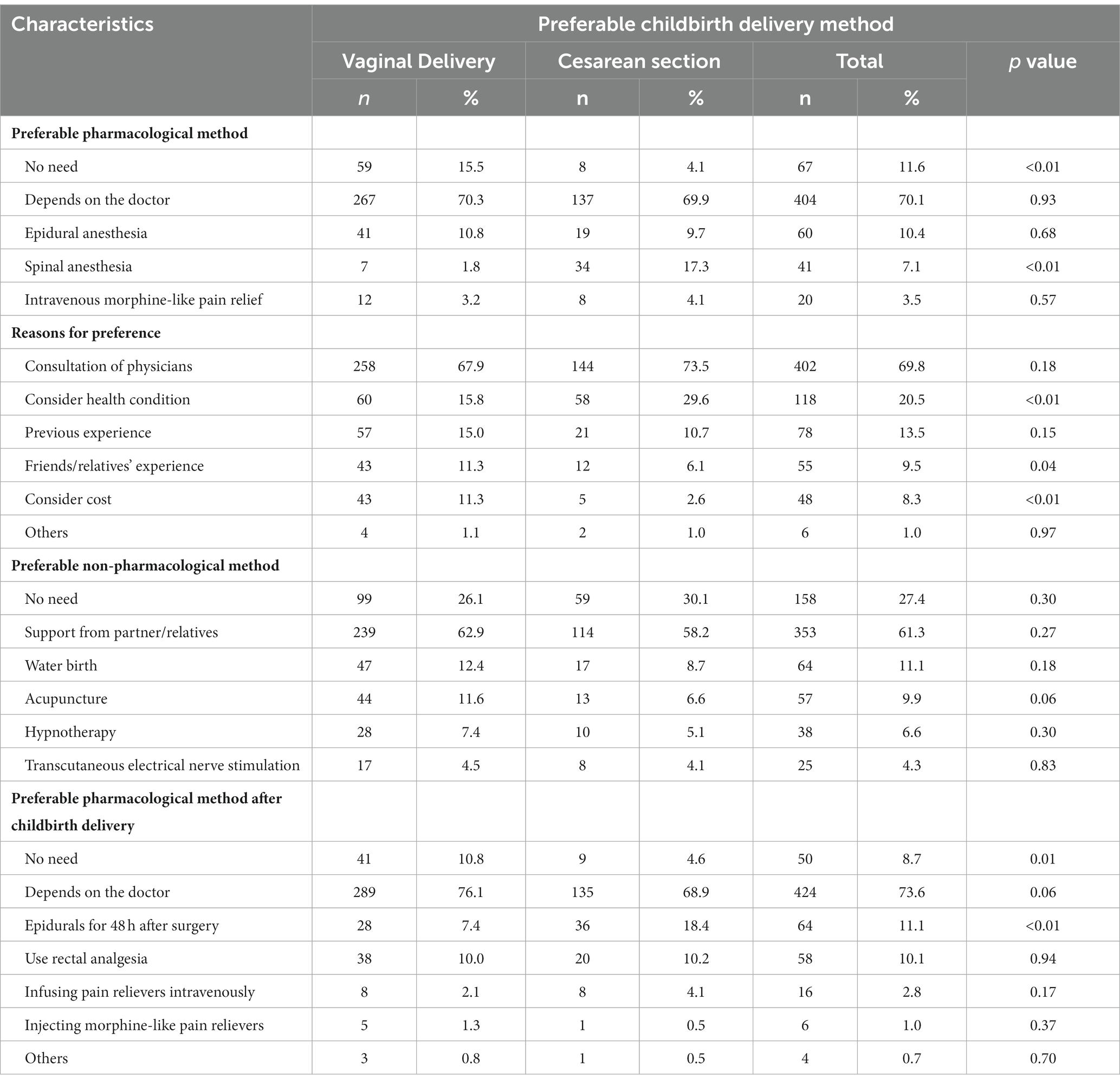
Table 4 shows that regarding pharmacological methods, most of the sample did not have specific methods (70.1%) and based on consultation of physicians (69.8%), while 11.6% of pregnant women reported that they did not need these methods. Meanwhile, regarding non-pharmacological methods, support from partner/relatives was the most preferable method (61.3%), following by water birth (11.1%) and acupuncture (9.9%).
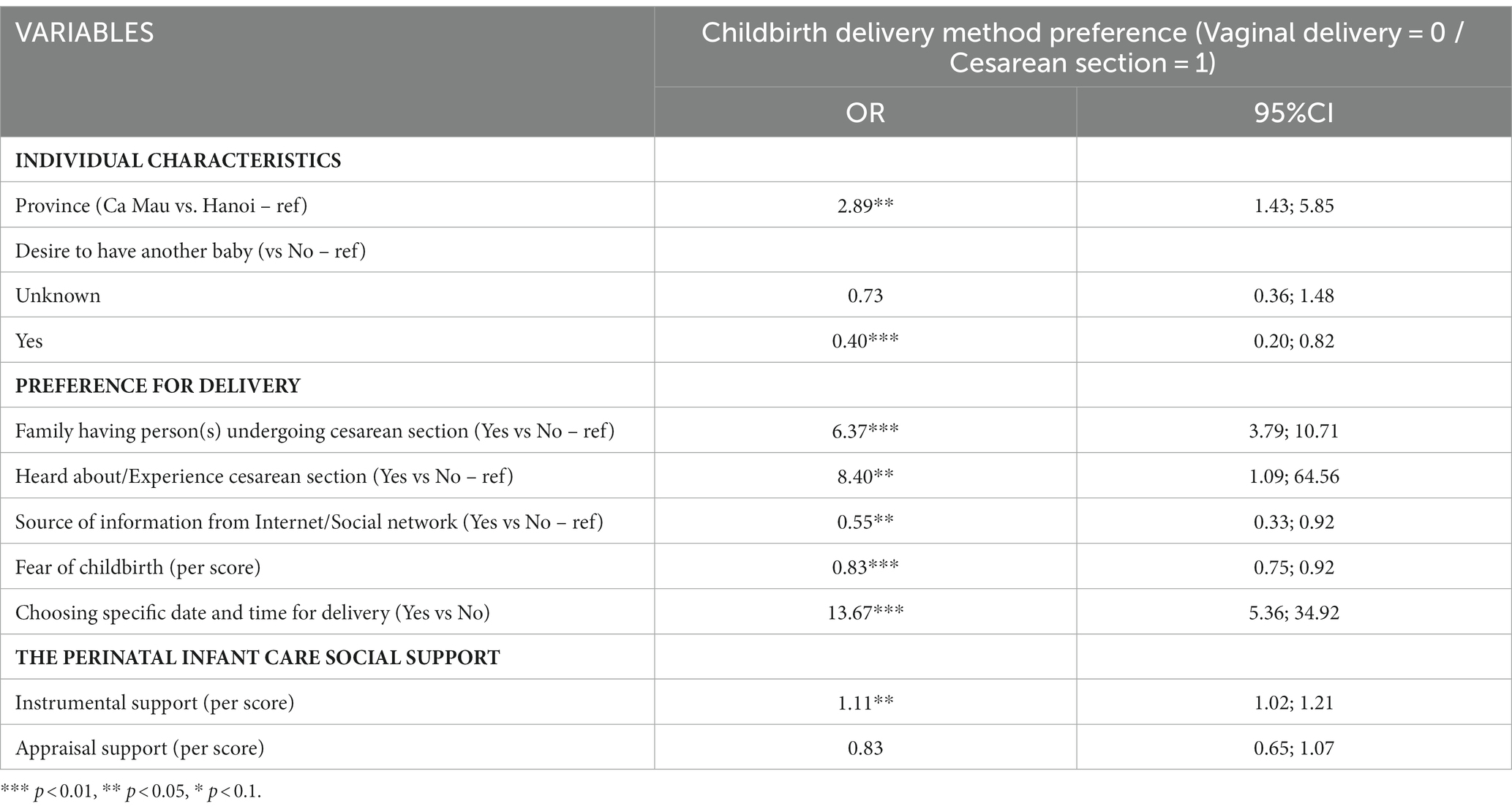
Results of multivariate logistic regression are shown in Table 5. Only variables selected via the stepwise process were presented. Women desiring to have another baby (OR = 0.40, 95%CI = 0.20–0.82), receiving information from the Internet/Social network (OR = 0.55, 95%CI = 0.33–0.92) and having a higher level of childbirth fear (OR = 0.83, 95%CI = 0.75–0.92) were less likely to prefer cesarean section. Meanwhile, women having family members undergoing cesarean section (OR = 6.37, 95%CI = 3.79–10.71) or hearing about cesarean section (OR = 8.40, 95%CI = 1.09–64.56) were more likely to prefer cesarean delivery. When the score of instrumental support increased by 1 point, they tended to have higher odds of preferring cesarean sections about 1.11 times (OR = 1.11, 95%CI = 1.02–1.21). Women intending to choose a specific date and time for childbirth delivery had a strong likelihood of preferring cesarean section compared to those not intending (OR = 13.67, 95%CI = 5.36–34.92).
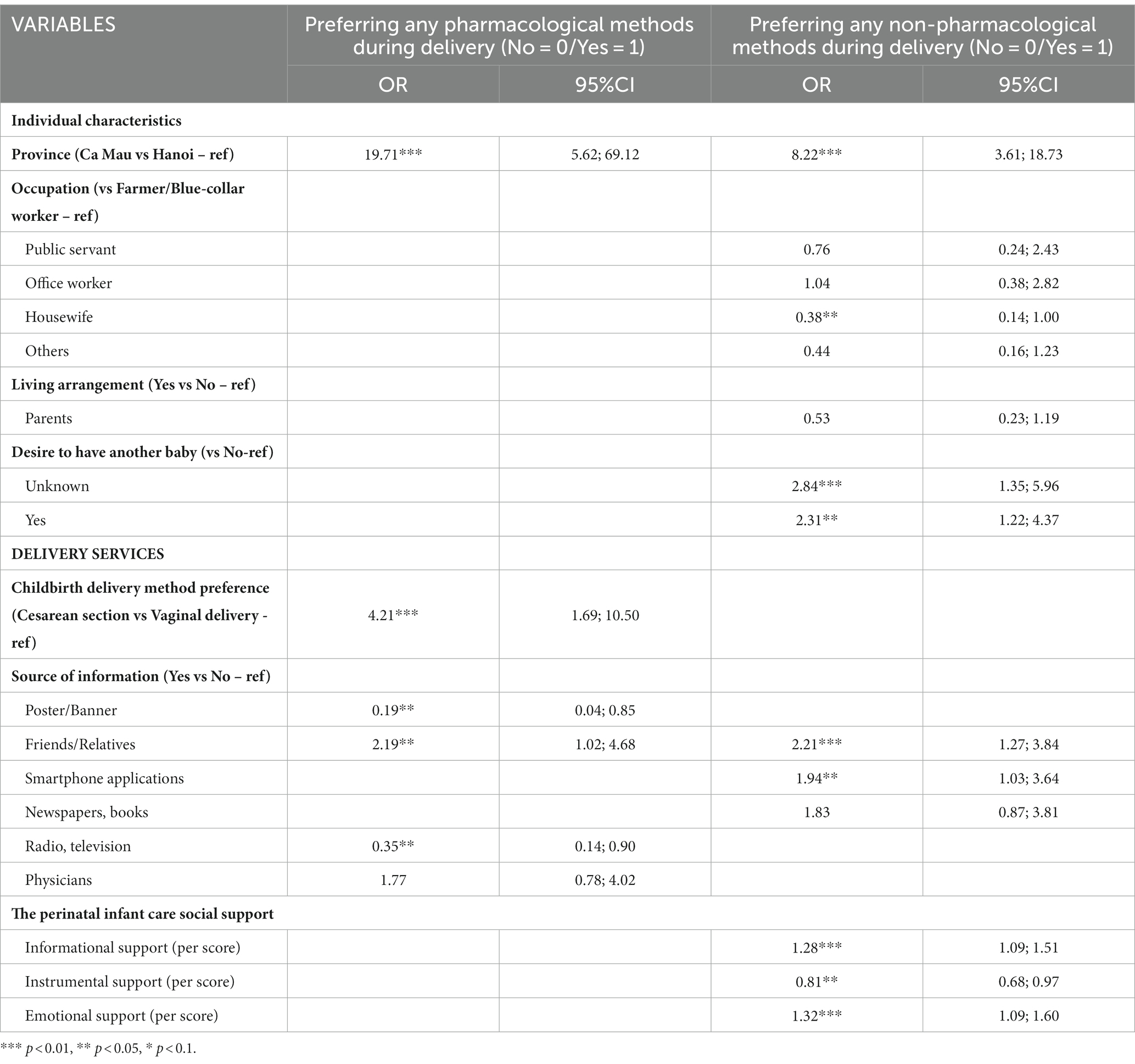
Table 6 illustrates that pregnant women desiring to have another baby tended to have higher odds of preferring non-pharmacological relief methods compared to those who have no desire (OR = 2.31; 95%CI = 1.22–4.37). In terms of source of health information, people who received information from friends or relatives were more likely to have higher odds of preferring both pharmacological relief methods (OR = 2.19, 95%CI = 1.02–3.68) and non-pharmacological relief methods (OR = 2.21; 95%CI = 1.27–3.84). Furthermore, people using smartphone applications as a health information resource tended to prefer non-pharmacological relief methods (OR = 2.94; 95%CI = 1.03–3.64). Regarding social support, when the score of informational support (OR = 1.28; 95%CI = 1.09–1.51) and emotional support (OR = 1.32; 95%CI = 1.09–1.60) increased by 1 point, they were also more likely to prefer non-pharmacological relief methods.
4 Discussion
Study results suggested that although the majority of our pregnant women preferred vaginal delivery, the proportion of individuals having demands on cesarean section was high. In this study, more than a third of pregnant women preferred cesarean delivery, which was significantly higher than the overall preference rate with 15.6% (28), as well as this rate in other countries (5, 29–32). The differences might be due to different demographic characteristics and pregnancy status in these studies. In addition, our study was conducted in urban obstetrics hospitals; thus, the rate of preference for cesarean sections might be higher than in other studies. Global research also showed that the proportion of urban women who preferred this method was higher than that in rural areas (5, 28). However, this result seemed to be consistent with the proportion of cesarean section performance in urban Vietnam (38.5%) which was reported in the previous study (25).
The most common reasons for this preference included the doctor’s recommendation, considering own health and based on previous experience, which echoed previous research in Vietnam and other countries when revealing that these factors were also the main reasons for the woman’s request for cesarean delivery (4, 33–35).
Notably, our study indicated that fear of childbirth and desire to have another baby were negatively associated with the preference for cesarean section. This was contradicted with previous findings in other studies, which showed that fear of childbirth was a significant predictor for the cesarean delivery preference (36–38). However, several prior studies indicated that fear of childbirth did not have any association with this preference (10, 39). Reasons for this phenomenon are not clear, but we supposed that the fear of postpartum pain was an important factor in explaining this problem. Research in Japan showed that pregnant women were aware that postoperative pain after the cesarean section was much more severe than postpartum vaginal pain; hence, they preferred vaginal birth over cesarean section even if they could tolerate pain (39). In addition, we believed that this phenomenon could be justified based on the decision-making process of the pregnant woman and the physicians in the hospitals where we performed this study. In these hospitals, pregnant women were thoroughly consulted about the childbirth delivery process, including the advantages and disadvantages of each method during and after the delivery. For instance, the cesarean section may increase the risk of postpartum complications such as hysterectomy, abnormal placentation, uterine rupture, or stillbirth, as well as increase the risk of preterm birth in the next pregnancies (6). For women with a high degree of fear of giving birth and having a desire to have another baby, health professionals performed mindfulness therapies to help reduce anxiety, and stress for women as well as prevent health problems in the next pregnancy.
Results of our study were similar to previous studies showing that women whose relatives have had a cesarean section or have heard and experienced a cesarean section were more likely to prefer the cesarean delivery method when giving birth (5, 40–42). One important socio-cultural factor we found in the study was that the choice of a specific date and time for childbirth was strongly associated with the preference for a cesarean section. This result reinforces the findings of previous studies in Vietnam and China (4, 11). In fact, in Vietnam, in some pregnant women and their families, the choice of birth date plays an important role when they conceive that having a baby at a good date and time of birth can help their family get fortune, success, and happiness as the baby harmonized with their parents (4). Although the proportion of mothers choosing a date of birth in our sample was only over 10%, results of the regression model showed that this factor played a very important role in determining the cesarean section preference. Additionally, research showed that instrumental support was related to a preference for cesarean section. In the PICSS scale, instrumental support is defined as hand-on assistance with baby care or housework (43). Indeed, the health of pregnant women after cesarean delivery was significantly reduced compared to those who delivered vaginally, hence, it is difficult for them to guarantee the ability to conduct housework and childcare. A high level of instrumental support meant that it could increase the woman’s confidence in giving birth as well as preferring cesarean section in this delivery (43). Hence, it is difficult for them to guarantee the ability to conduct housework and childcare of pregnant women after cesarean delivery.
When evaluating preference for pain relief methods, study results showed that most women did not have any specific preference but mainly relied on physician’s advice. This finding is understandable when knowledge of pain relief methods is not common but requires careful consultation from health workers based on the condition and needs of the pregnant woman. Results of multivariate analysis showed that women who preferred cesarean section were more likely to choose pharmacological pain relief methods during childbirth compared to women who preferred vaginal delivery. This was appropriate when cesarean section is a complex process, and anesthesia measures should be used appropriately to minimize maternal pain and burden, as well as release the mothers’ anxiety related to negative birth experience (12, 44–46).
Our study also found that when evaluating mothers’ preference for pain relief approaches, around three-quarters of women indicated their need for non-pharmacological, and the most common method was support from partner/family members. This result was similar to several previous studies when indicating that 94% of women preferred this non-pharmacological pain relief approach (47), and support persons played the most important role in pain relief and significantly reduced labor time and analgesics’ need (48). This can be explained by the outstanding benefits of non-pharmacological pain relief methods compared to others as well as these benefits not only positively affected the mother during birth, but also offered them a positive experience with childbirth delivery and prepared them for new motherhood experience (14). In addition, childbirth delivery was a painful and lonely process, and having support from husbands or parents during labor helped pregnant women improve their self-efficacy and self-care ability to cope with labor pain (49). In Vietnam, the involvement of the support person in pain relief during childbirth has not been implemented widely due to concerns about hospital hygiene and infection. However, these barriers should be improved with holistic approaches, enabling pregnant women to be beneficial in minimizing their labor pain. We also found that the preference for the non-pharmacological method was driven by some factors such as the desire to have more children, finding health information from friends/relatives, and smartphone applications. In practice, smartphone applications are the common information sources for pregnant women to update current trends on pain relief methods during childbirth delivery. From that, they can consider different options and then choose preferable pain relief methods for themselves.
The findings of this study suggested several clinical and public health implications. First, pregnant women should be consulted on how to access and evaluate formal information in different sources, thereby increasing their knowledge about the benefits and risks of each delivery method, which assisted them in choosing the most appropriate method. Family members of pregnant women also need to be aware of these measures and avoid pressure in choosing the birth delivery method. Second, medical staff during routine antenatal care also need to offer reasonable advice and emphasize that the cesarean section is only suitable for medical reasons, as well as should not use the method to choose the time of giving birth according to pregnant women’s needs. Third, it is necessary to promulgate policies and regulations to limit cesarean sections for any reason other than medical reasons to reduce the rate of cesarean section. Fourth, obstetrics hospitals can consider developing and implementing a variety of non-pharmacological pain relief services during and after delivery. Acceptance and willingness to pay studies for these services should be performed in the future.
Our research had the strength of being conducted in two medical centers in different regions of Vietnam, which might increase the generalizability of our results. However, some limitations of the study should be noted. First, we used a convenient sampling method to recruit participants, leading to a decrease in the representativeness of our sample. Second, we used the cross-sectional study design for this study. This limited the ability to build causal relationships between preferences and related factors.
5 Conclusion
This study highlighted a high preference rate for cesarean section in urban pregnant women in Vietnam. Desire to have another baby, relative’s experience, preference for birth date, and instrumental social support were major drivers of the cesarean section preference. This preference was the important factor for the preference for pharmacological pain relief. Meanwhile, a high level of informational and emotional support was associated with non-pharmacological method preference. Holistic approaches from family, health facility, and policy should be performed to diminish the cesarean rate preference and promote the use of non-pharmacological pain relief methods during birth.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by The Institutional Review Board of the Hanoi Obstetrics and Gynecology Hospital approved the study protocol (Code: 07 QD/PS-TTĐT). Information about the objectives of the study, the participant's right to withdraw at any time, and contact information for members of the research group were completely provided to participants. Written informed consent was obtained from all study participants before recruitment and participation. All methods were carried out in accordance with relevant guidelines and regulations or the declaration of Helsinki. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
TN: Conceptualization, Data curation, Formal analysis, Software, Supervision, Writing – original draft, Writing – review & editing. LN: Conceptualization, Formal analysis, Software, Writing – original draft, Writing – review & editing. HN: Data curation, Methodology, Supervision, Writing – original draft, Writing – review & editing. VD: Data curation, Investigation, Software, Writing – original draft, Writing – review & editing. TV: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. CL: Formal analysis, Methodology, Writing – review & editing. MZ: Methodology, Writing – original draft, Writing – review & editing. RH: Conceptualization, Methodology, Supervision, Writing – review & editing. CH: Conceptualization, Methodology, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The article process charge of this paper was supported by NUS Department of Psychological Medicine (R-177-000-100-001, R- 177-000-003-001, and R177000702733) and NUS iHeathtech Other Operating Expenses (R-722-000-004-731).
Acknowledgments
The authors would like to acknowledge support from all pregnant women who participated in the study, the National University of Singapore, and all collaborators.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Martos, T, Sallay, V, Rafael, B, and Konkoly, TB. Preferred ways of giving birth in non-pregnant and pregnant nulliparous women: the role of control beliefs. J Psychosom Obstet Gynaecol. (2020) 42:201–11. doi: 10.1080/0167482X.2019.1710486
2. Lowe, NK. The nature of labor pain. Am J Obstet Gynecol. (2002) 186:S16–24. doi: 10.1067/mob.2002.121427
3. Buhimschi, CS, and Buhimschi, IA. Advantages of vaginal delivery. Clin Obstet Gynecol. (2006) 49:167–83. doi: 10.1097/01.grf.0000198186.71542.03
4. Takegata, M, Smith, C, Nguyen, HAT, Thi, HH, Thi Minh, TN, Day, LT, et al. Reasons for increased caesarean section rate in Vietnam: a qualitative study among Vietnamese mothers and health care professionals. Healthcare. (2020) 8. doi: 10.3390/healthcare8010041
5. Kosan, Z, Kavuncuoglu, D, Calıkoglu, EO, and Aras, A. Delivery preferences of pregnant women: do not underestimate the effect of friends and relatives. Journal of Gynecology Obstetrics and Human Reproduction. (2019) 48:395–400. doi: 10.1016/j.jogoh.2019.03.009
6. Sandall, J, Tribe, RM, Avery, L, Mola, G, Visser, GHA, Homer, CSE, et al. Short-term and long-term effects of caesarean section on the health of women and children. Lancet. (2018) 392:1349–57. doi: 10.1016/S0140-6736(18)31930-5
7. Betran, AP, Ye, J, Moller, AB, Zhang, J, Gulmezoglu, AM, and Torloni, MR. The increasing trend in caesarean section rates: global, regional and National Estimates: 1990-2014. PLoS One. (2016) 11:e0148343. doi: 10.1371/journal.pone.0148343
8. Coates, D, Thirukumar, P, Spear, V, Brown, G, and Henry, A. What are women’s mode of birth preferences and why? A systematic scoping review. Women Birth. (2020) 33:323–33. doi: 10.1016/j.wombi.2019.09.005
9. Tilden, EL, Cheyney, M, Guise, JM, Emeis, C, Lapidus, J, Biel, FM, et al. Vaginal birth after cesarean: neonatal outcomes and United States birth setting. Am J Obstet Gynecol. (2017) 216:403.e1–8. doi: 10.1016/j.ajog.2016.12.001
10. Kjerulff, KH, Attanasio, LB, Edmonds, JK, and Repke, JT. Mode of delivery preference among pregnant nulliparous women. J Women's Health (2002). 2019;28:874–884, doi: 10.1089/jwh.2018.6989
11. Long, Q, Kingdon, C, Yang, F, Renecle, MD, Jahanfar, S, Bohren, MA, et al. Prevalence of and reasons for women’s, family members’, and health professionals’ preferences for cesarean section in China: a mixed-methods systematic review. PLoS Med. (2018) 15:e1002672. doi: 10.1371/journal.pmed.1002672
12. Madden, KL, Turnbull, D, Cyna, AM, Adelson, P, and Wilkinson, C. Pain relief for childbirth: the preferences of pregnant women, midwives and obstetricians. Women and birth: journal of the Australian College of Midwives. (2013) 26:33–40. doi: 10.1016/j.wombi.2011.12.002
13. Khalesi, ZB. Relationship between Primigravid women’s awareness, attitude, fear of childbirth, and mode of delivery preference. European Journal of Obstetrics & Gynecology and Reproductive Biology: X. (2022) 14:100143. doi: 10.1016/j.eurox.2022.100143
14. Thomson, G, Feeley, C, Moran, VH, Downe, S, and Oladapo, OT. Women's experiences of pharmacological and non-pharmacological pain relief methods for labour and childbirth: a qualitative systematic review. Reprod Health. (2019) 16:71. doi: 10.1186/s12978-019-0735-4
15. Gribel, GPC, Coca-Velarde, LG, and Moreira de Sá, RA. Influence of non-pharmacological obstetric interventions on adverse outcomes of childbirth under regional analgesia. J Perinat Med. (2020) 48:495–503. doi: 10.1515/jpm-2019-0366
16. Duncan, LG, and Bardacke, N. Mindfulness-based childbirth and parenting education: promoting family mindfulness during the Perinatal period. J Child Fam Stud. (2010) 19:190–202. doi: 10.1007/s10826-009-9313-7
17. GöNenÇ, IM, and Terzioglu, F. Effects of massage and acupressure on relieving labor pain, reducing labor time, and increasing delivery satisfaction. J Nurs Res. (2020) 28:e68. doi: 10.1097/jnr.0000000000000344
18. Czech, I, Fuchs, P, Fuchs, A, Lorek, M, Tobolska-Lorek, D, Drosdzol-Cop, A, et al. Pharmacological and non-pharmacological methods of labour pain relief-establishment of effectiveness and comparison. Int J Environ Res Public Health. (2018) 15. doi: 10.3390/ijerph15122792
19. Barakzai, A, Haider, G, Yousuf, F, Haider, A, and Muhammad, N. Awareness of women regarding analgesia during labour. J Ayub Med Coll Abbottabad. (2010) 22:73–5.
20. Raynes-Greenow, CH, Nassar, N, Torvaldsen, S, Trevena, L, and Roberts, CL. Assisting informed decision making for labour analgesia: a randomised controlled trial of a decision aid for labour analgesia versus a pamphlet. BMC Pregnancy Childbirth. (2010) 10:15. doi: 10.1186/1471-2393-10-15
21. Raynes-Greenow, CH, Roberts, CL, McCaffery, K, and Clarke, J. Knowledge and decision-making for labour analgesia of Australian primiparous women. Midwifery. (2007) 23:139–45. doi: 10.1016/j.midw.2006.06.004
22. National Guidelines for Reproductive Health Services. Decision 4128/QĐ-BYT (Hướng dẫn quốc gia về các dịch vụ chăm sóc sức khỏe sinh sản, Quyết định 4128/QĐ-BYT), Vietnam Ministry of Health (2017).
23. Verma, V, Vishwakarma, RK, Nath, DC, Khan, HTA, Prakash, R, and Abid, O. Prevalence and determinants of caesarean section in south and south-east Asian women. PLoS One. (2020) 15:e0229906. doi: 10.1371/journal.pone.0229906
24. UNICEF. UNICEF data: Monitoring the situation of children and women. Available at: https://data.unicef.org/resources/data_explorer/unicef_f/?ag=UNICEF&df=GLOBAL_DATAFLOW&ver=1.0&dq=VNM.MNCH_INSTDEL+MNCH_SAB+MNCH_BIRTH18+MNCH_CSEC..&startPeriod=2000&endPeriod=2021. (Accessed February 25, 2021).
25. Toan Khanh, T, Eriksson, B, Nhat An, P, Thi Kim Chuc, N, Bondjers, G, and Gottvall, K. Technology preference in choices of delivery care utilization from user perspective –a community study in Vietnam. American journal of public health Research. (2013) 1:10–7. doi: 10.12691/ajphr-1-1-2
26. Tran, T, Eriksson, B, An, P, Chuc, N, Bondjers, G, and Gottvall, K. Technology preference in choices of delivery care utilization from user perspective –a community study in Vietnam. American J Public Health Research. (2013) 1:10–7. doi: 10.12691/ajphr-1-1-2
27. Leahy-Warren, P, McCarthy, G, and Corcoran, P. First-time mothers: social support, maternal parental self-efficacy and postnatal depression. J Clin Nurs. (2012) 21:388–97. doi: 10.1111/j.1365-2702.2011.03701.x
28. Mazzoni, A, Althabe, F, Liu, NH, Bonotti, AM, Gibbons, L, Sánchez, AJ, et al. Women's preference for caesarean section: a systematic review and meta-analysis of observational studies. BJOG. (2011) 118:391–9. doi: 10.1111/j.1471-0528.2010.02793.x
29. Ryding, EL, Lukasse, M, Kristjansdottir, H, Steingrimsdottir, T, and Schei, B. On behalf of the Bidens study g. pregnant women’s preference for cesarean section and subsequent mode of birth – a six-country cohort study. J Psychosom Obstet Gynecol. (2016) 37:75–83. doi: 10.1080/0167482X.2016.1181055
30. Lindstad Løvåsmoen, EM, Nyland Bjørgo, M, Lukasse, M, Schei, B, and Henriksen, L. Women's preference for caesarean section and the actual mode of delivery - comparing five sites in Norway. Sex Reprod Healthc. (2018) 16:206–12. doi: 10.1016/j.srhc.2018.04.009
31. Zhang, H, Wu, J, Norris, J, Guo, L, and Hu, Y. Predictors of preference for caesarean delivery among pregnant women in Beijing. J Int Med Res. (2017) 45:798–807. doi: 10.1177/0300060517696217
32. Torloni, MR, Betrán, AP, Montilla, P, Scolaro, E, Seuc, A, Mazzoni, A, et al. Do Italian women prefer cesarean section? Results from a survey on mode of delivery preferences. BMC Pregnancy Childbirth. (2013) 13:78. doi: 10.1186/1471-2393-13-78
33. Buyukbayrak, EE, Kaymaz, O, Kars, B, Karsidag, AY, Bektas, E, Unal, O, et al. Caesarean delivery or vaginal birth: preference of Turkish pregnant women and influencing factors. Journal of obstetrics and gynaecology: the journal of the Institute of Obstetrics and Gynaecology. (2010) 30:155–8. doi: 10.3109/01443610903461436
34. Ford, J, Grewal, J, Mikolajczyk, R, Meikle, S, and Zhang, J. Primary cesarean delivery among parous women in the United States, 1990-2003. Obstet Gynecol. (2008) 112:1235–41. doi: 10.1097/AOG.0b013e31818ce092
35. Bt Maznin, NL, and Creedy, DK. A comprehensive systematic review of factors influencing women's birthing preferences. JBI library of systematic reviews. (2012) 10:232–306. doi: 10.11124/jbisrir-2012-46
36. Nieminen, K, Stephansson, O, and Ryding, EL. Women's fear of childbirth and preference for cesarean section–a cross-sectional study at various stages of pregnancy in Sweden. Acta Obstet Gynecol Scand. (2009) 88:807–13. doi: 10.1080/00016340902998436
37. Stoll, K, Edmonds, JK, and Hall, WA. Fear of childbirth and preference for Cesarean delivery among young American women before childbirth: a survey study. Birth (Berkeley, Calif). (2015) 42:270–6. doi: 10.1111/birt.12178
38. Størksen, HT, Garthus-Niegel, S, Adams, SS, Vangen, S, and Eberhard-Gran, M. Fear of childbirth and elective caesarean section: a population-based study. BMC Pregnancy Childbirth. (2015) 15:221. doi: 10.1186/s12884-015-0655-4
39. Takegata, M, Haruna, M, Morikawa, M, Yonezawa, K, Komada, M, and Severinsson, E. Qualitative exploration of fear of childbirth and preferences for mode of birth among Japanese primiparas. Nursing & health sciences. (2018) 20:338–45. doi: 10.1111/nhs.12571
40. Faisal-Cury, A, and Menezes, PR. Factors associated with preference for cesarean delivery. Rev Saúde Pública. (2006) 40:226–32. doi: 10.1590/S0034-89102006000200007
41. Yamasmit, W, and Chaithongwongwatthana, S. Attitude and preference of Thai pregnant women towards mode of delivery. J Med Assoc Thail. (2012) 95:619–24.
42. Yilmaz, SD, Bal, MD, Beji, NK, and Uludag, S. Women’s preferences of method of delivery and influencing factors. Iran Red Crescent Med J. (2013) 15:683–9. doi: 10.5812/ircmj.11532
43. Leahy-Warren, P, Mulcahy, H, and Lehane, E. The development and psychometric testing of the Perinatal Infant care social support (PICSS) instrument. J Psychosom Res. (2019) 126:109813. doi: 10.1016/j.jpsychores.2019.109813
44. Tebekaw, Y, James Mashalla, Y, and Thupayagale-Tshweneagae, G. Factors influencing Women’s preferences for places to give birth in Addis Ababa. Ethiopia Obstetrics and Gynecology International. (2015) 2015:439748:1–7. doi: 10.1155/2015/439748
45. Lindholm, A, and Hildingsson, I. Women's preferences and received pain relief in childbirth - a prospective longitudinal study in a northern region of Sweden. Sex Reprod Healthc. (2015) 6:74–81. doi: 10.1016/j.srhc.2014.10.001
46. Alehagen, S, Wijma, B, and Wijma, K. Fear of childbirth before, during, and after childbirth. Acta Obstet Gynecol Scand. (2006) 85:56–62. doi: 10.1080/00016340500334844
47. Green, JM, Coupland, VA, and Kitzinger, J. Great expectations: A prospective study of women's expectations and experiences of childbirth. Butterworth-Heinemann (1998).
48. Bohren, MA, Hofmeyr, GJ, Sakala, C, Fukuzawa, RK, and Cuthbert, A. Continuous support for women during childbirth. Cochrane Database Syst Rev. United Kingdom (2017) 2017. doi: 10.1002/14651858.CD003766.pub6
Keywords: childbirth delivery, pain relief, pregnant women, women’s health, Vietnam
Citation: Nguyen TT, Nguyen LH, Nguyen HTT, Dam VAT, Vu TMT, Latkin CA, Zhang MWB, Ho RCM and Ho CSH (2024) Preferences for childbirth delivery and pain relief methods among pregnant women in Vietnam. Front. Med. 11:1290232. doi: 10.3389/fmed.2024.1290232
Edited by:
Simcha Yagel, Hadassah Medical Center, IsraelReviewed by:
Enrique Reyes-Muñoz, Instituto Nacional de Perinatología (INPER), MexicoTimothy Abiola Olusesan Oluwasola, University of Ibadan, Nigeria
Copyright © 2024 Nguyen, Nguyen, Nguyen, Dam, Vu, Latkin, Zhang, Ho and Ho. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tham Thi Nguyen, bmd1eWVudGhpdGhhbTExQGR1eXRhbi5lZHUudm4=
 Tham Thi Nguyen
Tham Thi Nguyen Long Hoang Nguyen3
Long Hoang Nguyen3 Ha Thu Thi Nguyen
Ha Thu Thi Nguyen Vu Anh Trong Dam
Vu Anh Trong Dam Thuc Minh Thi Vu
Thuc Minh Thi Vu Carl A. Latkin
Carl A. Latkin Melvyn W. B. Zhang
Melvyn W. B. Zhang Roger C. M. Ho
Roger C. M. Ho Cyrus S. H. Ho
Cyrus S. H. Ho