- 1Department of Neuroradiology, Clinic of Radiology & Nuclear Medicine, University Hospital Basel, Basel, Switzerland
- 2Department of Diagnostic and Interventional Neuroradiology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany
- 3Department of Radiology and Neuroradiology, Stadtspital Zürich, Zürich, Switzerland
- 4Department of Interventional Radiology, Clinic of Radiology & Nuclear Medicine, University Hospital Basel, Basel, Switzerland
- 5Department of Radiology, Ludwig-Maximilians-University (LMU) Munich, Munich, Germany
Purpose: To describe a novel ultrasound-guided technique for percutaneous radiofrequency ablation of vascular malformations—the “moving shot technique.”
Methods: Preliminary observational cohort study, conducted from June 1, 2019, to January 31, 2021, including all consecutive patients diagnosed with vascular malformations who were treated with ultrasound-guided radiofrequency ablation using the moving shot technique. Only patients who had undergone at least one unsuccessful previous treatment were included (sclerotherapy with ethanol/aethoxysklerol or embolization/surgery).
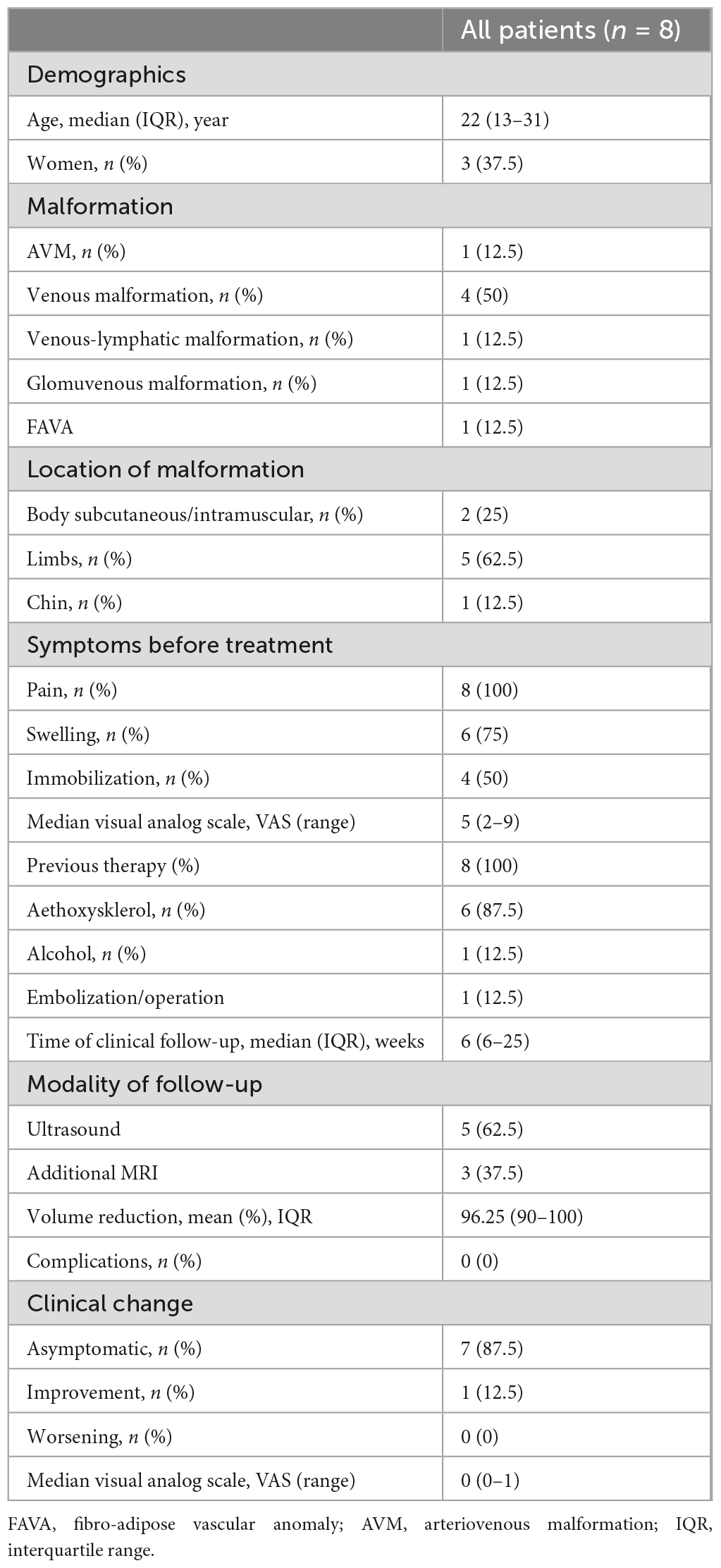
Results: Eight patients with a median age of 22 years (interquartile range, 13–31) were included. Patients had different vascular malformations consisting of 1 arteriovenous malformation, 4 venous malformations, and 1 each a mixed venous-lymphatic malformation, a glomuvenous malformation and a FAVA (fibroadipose vascular anomaly). Malformations were located at the limbs in 5 patients (62.5%), the subcutaneous/intramuscular tissue of the body in 2 patients (25%) and at the chin in 1 patient (12.5%). Clinical symptoms were pain in 8 patients (100%), swelling in 6 patients (75%), and partial immobility in 4 patients (50%). All patients showed an improvement of clinical symptoms after treatment with 7 (87.5%) being completely asymptomatic and 1 (12.5%) showing improvement of immobility and pain. No procedural complications, such as nerve damage or skin burns occurred.
Conclusion: The moving shot technique using ultrasonography-guided radiofrequency ablation is a promising technique for the interventional treatment of vascular malformations and should be validated in multicenter-approaches.
Introduction
Vascular malformations are abnormalities in blood vessel morphogenesis with an overall prevalence of approximately 1.2–1.5% (1, 2). According to the classification of the International Society for the Study of Vascular Anomalies (ISSVA) (3–5) vascular malformations are divided in slow-flow and high-flow lesions, related to the flow pattern, which is crucial both for treatment decision and the prognosis (6). Slow flow malformations include venous malformation (VM), lymphatic malformation (LM), or arteriovenous malformation (AVM). Slow-flow malformations represent the majority (>90%) of vascular malformations and among these, venous malformations (VMs) are the most common type (2).
For the treatment of vascular malformations, several interventional therapies such as percutaneous sclerotherapy or embolization have been reported, mostly depending on the flow pattern (7, 8). Especially lesions involving the skin or adjacent to neurovascular structures are prone to major procedural complications such as soft tissue necrosis or nerve palsy (9). Ultrasonography (US)-guided radiofrequency ablation (RFA) has been used to treat various types of benign and malignant tumors in many organs including hepatocellular carcinomas, hepatic metastases, and thyroid nodules (10–12). One recent study described the use of US-RFA for venous malformations and found a good safety profile. yin The combination with the moving shot technique, which is established for RFA of thyroid nodules (11, 12) may enable a complete treatment of malformations with a low complication rate. Hence, we report our experience with this new technique and hypothesized that it can be used for effective therapy of different types of vascular malformations safely.
Materials and methods
Patients
This preliminary observational cohort study, conducted from June 1, 2019, to January 31, 2021, included all consecutive patients diagnosed with vascular malformations who were treated with US-RFA using the moving shot technique. All patients had undergone at least one unsuccessful previous treatment (sclerotherapy with ethanol/aethoxysklerol or embolization/surgery). The study was approved by the local ethics committee in accordance with the Declaration of Helsinki, with waiver of informed consent.
Vascular malformation were classified according to the classification of the International Society for the Study of Vascular Anomalies (ISSVA) (3). Further, AVMs were classified using the Schobinger classification as a clinical assessment of vascular shunting (13) and the Cho classification describing angiographic characteristics (14). Venous malformations were classified using the Puig classification containing information on venous drainage patterns (15).
Outcomes measures
Clinical outcome parameters included visual analogue scales (VAS) to measure pain severity before and after treatment as well as assessment of movement of limbs at admission and post-interventional stage. This data were collected by the treating interventional radiologist, when seeing the patient for pre-interventional and post-interventional clinics. CIRSE classification system for complications was applied to measure per-interventional complications (16). The volume calculations of the malformations in admission and follow-up imaging were performed using a three-dimensional semi-automatic technique with an established open-source software (Medical Imaging Toolkit; MITK, Istituto di Calcolo ad Alte Prestazioni, Napoli, Italy) (17, 18).
Equipment and technique
We used an 18-gauge, monopolar, modified, internally cooled electrode with a 0.7–1.5 cm active tip and a 7–10 cm shaft length, specifically developed for thyroid lesions (11). A peristaltic pump (all HS AMICA, Spain) continuously infused cold saline (0°C) into the lumen of the electrodes to maintain the temperature of the electrode. Ablation was performed using 20–70 watts in pulsing mode. The electrode tip was initially positioned under US-guidance at a deep part of the malformation. The electrode tip moves slowly but at continuous speed in order to prevent the RFA cut-off phenomenon. When an echogenic area was detected at the tip of the electrode, it was repositioned looking for malformative vessels under US-guidance in the Duplex mode. The RFA starts at the parts further away from the US-transducer and moves to the closer parts because gas from the denaturation may reduce image quality. Treatment success was demonstrated by US and by controlling the temperature of the tissue around the needle which should be >50°C for 5 min or once >60°C (19).
Statistical analysis
Univariable distribution of metric variables is described by median and interquartile range. For categorial data, absolute and relative frequencies are given. Due to small sample size only descriptive statistics were used. All statistical analyses were performed using SPSS, version 22 (IBM Software, Chicago, IL, USA).
Results
Patients
Overall, eight patients were included; five (62.5%) were male, and three (37.5%) were female. Median age was 22 years [total range, 11–56; interquartile range (IQR), 13–31]. One patient had an arteriovenous malformation (classified as Schobinger II and Cho IIIb), four had venous malformations (2x Puig type I, 1x type II and 1x type III), and one each had a mixed venous-lymphatic malformation, a glomuvenous malformation and a FAVA (fibroadipose vascular anomaly). Malformations were located at the limbs in 5 patients (62.5%), the body in 2 patients (25%) and at the chin in 1 patient (12.5%). Clinical symptoms were pain in eight patients (100%, median VAS 5), swelling in six patients (75%), and partial immobility in four patients (50%, 4 of 5 patients with limb malformations). Median time of clinical follow-up was 6 weeks (IQR 6–25) (Table 1). Patients who were asymptomatic at 6-week follow-up were not further followed.
Outcome and safety
All patients showed an improvement of clinical symptoms after treatment with seven (87.5%) being completely asymptomatic and one (12.5%) showing improvement of symptoms and just slight remaining pain. Median VAS for quantification of pain decreased from 5 (range 2–9) at admission to 0 (range 0–1) at follow-up. All patients could move normally at follow-up with no residual immobility.
All patients underwent imaging to determine the degree of volume reduction of the malformation; five (62.5%) had ultrasound and three (37.5%) had additional magnetic resonance imaging. Mean volume of the malformation at admission was 76 cm3 and mean reduction was 96% (to a mean of 3 cm3, IQR 90–100). No procedural complications, such as nerve damage or skin burns occurred. There was no deviation from the normal post-therapeutic course (according to CIRSE classification system for complications) (16).
Discussion
Our study describes the moving shot technique using US-RFA in patients with different types of vascular malformations. In our preliminary experience the mean reduction of the volume of the treated malformations was 96%, clinical symptoms improved in all patients (with 87% being completely asymptomatic) and a good safety profile.
Whereas a recent study described a similar approach for the treatment of venous malformation, our study also included other types of vascular malformations such as AVMs, and thereby provides first evidence that a broad spectrum of malformations may be treated using this technique.
For venous malformations, besides conservative management, invasive therapy is indicated in symptomatic VMs to reduce symptoms such as pain, hemorrhage, and impairment of neighboring structures. For VMs percutaneous sclerotherapy is the first-choice invasive treatment method and can be combined with laser therapy or surgical procedures (20, 21). However, evidence is low and the choice for the invasive method remains a shared decision between the patient and a multidisciplinary team of specialists (22, 23). Likewise symptomatic macrocystic lymphatic malformations can effectively be treated using percutaneous sclerotherapy with a good safety profile (24), whereas for microcystic LMs percutaneous sclerotherapy may be less effective and requires other sclerosants such as Picibanil, Bleomycin, and Doxycycline (8).
For high-flow vascular malformations such as AVMs invasive therapy is indicated in patients with progressive symptoms according to the Schobinger classification. Here, embolization is the first choice with a relatively low morbidity but may be prone to recurrence (20, 25).
The main advantage of RFA compared to other embolization techniques or sclerotherapies is that the vessels of the malformation are completely ablated and no material such as onyx remains, which may lead a complete remodeling of the tissue and thereby to a larger proportion of patients with clinical improvement. Moreover, the nidus may sometimes be difficult to reach using embolization techniques. Therefore, US-RFA offers another, technically completely different approach, which may lead to lower recurrence rates in cases where embolization therapy is difficult due to anatomical reasons or the arterial supply of the AVM (26).
Our study has limitations such as the retrospective single-center design and the small sample size. Moreover, imaging follow-up was not homogenous as only three patients underwent additional MRI.
Conclusion
The moving shot technique using ultrasound-guided radiofrequency ablation is a promising technique for the interventional treatment of different types of vascular malformations.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics committee of University of Basel. The studies were conducted in accordance with the local legislation and institutional requirements. The Ethics Committee/Institutional Review Board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because this was a retrospective analysis.
Author contributions
PS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review and editing. MP: Funding acquisition, Resources, Supervision, Validation, Writing – review and editing. KB: Supervision, Validation, Writing – review and editing. CZ: Supervision, Validation, Writing – review and editing. MW: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review and editing. MT: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review and editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Nguyen HL, Bonadurer GF, Tollefson MM. Vascular malformations and health-related quality of life a systematic review and meta-analysis. JAMA Dermatol. (2018) 154:661–9. doi: 10.1001/jamadermatol.2018.0002
2. Sadick M, Müller-Wille R, Wildgruber M, Wohlgemuth WA. Vascular anomalies (Part I): classification and diagnostics of vascular anomalies. RoFo. (2018) 190:825–35. doi: 10.1055/a-0620-8925
3. Monroe EJ. Brief description of ISSVA classification for radiologists. Tech Vasc Interv Radiol. (2019) 22:100628. doi: 10.1016/j.tvir.2019.100628
4. Wassef M, Borsik M, Cerceau P, Faucon B, Laurian C, Le Clerc N, et al. Classification of vascular tumours and vascular malformations. Contribution of the ISSVA 2014/2018 classification. Ann Pathol. (2021) 41:58–70. doi: 10.1016/j.annpat.2020.11.004
5. Kunimoto K, Yamamoto Y, Jinnin M. ISSVA classification of vascular anomalies and molecular biology. Int J Mol Sci. (2022) 23:2358. doi: 10.3390/ijms23042358
6. Greene AK, Liu AS, Mulliken JB, Chalache K, Fishman SJ. Vascular anomalies in 5621 patients: guidelines for referral. J Pediatr Surg. (2011) 46:1784–9. doi: 10.1016/j.jpedsurg.2011.05.006
7. Wassef M, Blei F, Adams D, Alomari A, Baselga E, Berenstein A, et al. Vascular anomalies classification: recommendations from the international society for the study of vascular anomalies. Pediatrics. (2015) 136:e203–14. doi: 10.1542/peds.2014-3673
8. Müller-Wille R, Wildgruber M, Sadick M, Wohlgemuth WA. Vascular anomalies (Part II): interventional therapy of peripheral vascular malformations. RoFo. (2018): doi: 10.1055/s-0044-101266 [Epub ahead of print].
9. Lee KB, Kim DI, Oh SK, Do YS, Kim KH, Kim YW. Incidence of soft tissue injury and neuropathy after embolo/sclerotherapy for congenital vascular malformation. J Vasc Surg. (2008) 48:1286–91. doi: 10.1016/j.jvs.2008.06.058
10. Hong K, Georgiades CS, Geschwind JF. Technology insight: image-guided therapies for hepatocellular carcinoma - Intra-arterial and ablative techniques. Nat Clin Pract Oncol. (2006) 3:315–24. doi: 10.1038/ncponc0512
11. Baek JH, Moon WJ, Kim YS, Lee JH, Lee D. Radiofrequency ablation for the treatment of autonomously functioning thyroid nodules. World J Surg. (2009) 33:1971–7. doi: 10.1007/s00268-009-0130-3
12. Sung JY, Baek JH, Jung SL, Kim JH, Kim KS, Lee D, et al. Radiofrequency ablation for autonomously functioning thyroid nodules: a multicenter study. Thyroid. (2015) 25:112–7. doi: 10.1089/thy.2014.0100
13. Kohout MP, Hansen M, Pribaz JJ, Mulliken JB. Arteriovenous malformations of the head and neck: natural history and management. Plast Reconstr Surg. (1998) 102:643–54. doi: 10.1097/00006534-199809030-00006
14. Cho SK, Do YS, Shin SW, Kim DI, Kim YW, Park KB, et al. Arteriovenous malformations of the body and extremities: analysis of therapeutic outcomes and approaches according to a modified angiographic classification. J Endovasc Ther. (2006) 13:527–38. doi: 10.1583/05-1769.1
15. Puig S, Aref H, Chigot V, Bonin B, Brunelle F. Classification of venous malformations in children and implications for sclerotherapy. Pediatr Radiol. (2003) 33:99–103. doi: 10.1007/s00247-002-0838-9
16. Filippiadis DK, Binkert C, Pellerin O, Hoffmann RT, Krajina A, Pereira PL. Cirse quality assurance document and standards for classification of complications: the cirse classification system. Cardiovasc Intervent Radiol. (2017) 40:1141–6. doi: 10.1007/s00270-017-1703-4
17. Brokinkel B, Stummer W, Sporns P. Simpson grade IV resections of skull base meningiomas: does the postoperative tumor volume impact progression? J Neurooncol. (2018) 137:219–21. doi: 10.1007/s11060-017-2715-2
18. Hess K, Spille DC, Adeli A, Sporns PB, Brokinkel C, Grauer O, et al. Brain invasion and the risk of seizures in patients with meningioma. J Neurosurg. (2019) 130:789–96. doi: 10.3171/2017.11.JNS172265
19. Rhim H, Goldberg SN, Dodd GD, Solbiati L, Lim HK, Tonolini M, et al. Essential techniques for successful radio-frequency thermal ablation of malignant hepatic tumors. Radiographics. (2001) 21 Spec No:S17–35. doi: 10.1148/radiographics.21.suppl_1.g01oc11s17
20. Ranieri M, Wohlgemuth W, Müller-Wille R, Prantl L, Kehrer A, Geis S, et al. Vascular malformations of upper and lower extremity - From radiological interventional therapy to surgical soft tissue reconstruction - An interdisciplinary treatment. Clin Hemorheol Microcirc. (2017) 67:355–72. doi: 10.3233/CH-179216
21. Schmidt VF, Masthoff M, Goldann C, Brill R, Sporns PB, Segger L, et al. Multicentered analysis of percutaneous sclerotherapies in venous malformations of the face. Front Med. (2022) 9:1066412. doi: 10.3389/fmed.2022.1066412
22. Van Der Vleuten CJ, Kater A, Wijnen MH, Schultze Kool LJ, Rovers MM. Effectiveness of sclerotherapy, surgery, and laser therapy in patients with venous malformations: a systematic review. Cardiovasc Intervent Radiol. (2014) 37:977–89. doi: 10.1007/s00270-013-0764-2
23. Schmidt VF, Olivieri M, Häberle B, Masthoff M, Deniz S, Sporns PB, et al. Interventional treatment options in children with extracranial vascular malformations. Hamostaseologie. (2022) 42:131–41. doi: 10.1055/a-1728-5686
24. Alomari AI, Karian VE, Lord DJ, Padua HM, Burrows PE. Percutaneous sclerotherapy for lymphatic malformations: a retrospective analysis of patient-evaluated improvement. J Vasc Interv Radiol. (2006) 17:1639–48. doi: 10.1097/01.RVI.0000239104.78390.E5
25. Schmidt VF, Masthoff M, Brill R, Sporns PB, Köhler M, Schulze-Zachau V, et al. Image-guided embolotherapy of arteriovenous malformations of the face. Cardiovasc Intervent Radiol. (2022) 45:992–1000. doi: 10.1007/s00270-022-03169-0
Keywords: radiofrequency ablation, moving shot technique, vascular malformation, ultrasound, arteriovenous malformation, AVM, venous malformation (VM), lymphatic malformation (LM)
Citation: Sporns PB, Psychogios M, Blackham K, Zech C, Wildgruber M and Takes M (2024) Ultrasonography-guided radiofrequency ablation of vascular malformations—The moving shot technique. Front. Med. 10:1345904. doi: 10.3389/fmed.2023.1345904
Received: 28 November 2023; Accepted: 18 December 2023;
Published: 12 January 2024.
Edited by:
Max Masthoff, University Hospital Münster, GermanyReviewed by:
Nguyen Minh Duc, Pham Ngoc Thach University of Medicine, VietnamPhilipp Schindler, University Hospital Münster, Germany
Copyright © 2024 Sporns, Psychogios, Blackham, Zech, Wildgruber and Takes. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Peter B. Sporns, cGV0ZXIuc3Bvcm5zQGhvdG1haWwuZGU=
†These authors have contributed equally to this work
 Peter B. Sporns
Peter B. Sporns Marios Psychogios2
Marios Psychogios2 Moritz Wildgruber
Moritz Wildgruber