- 1The College of Life Sciences, Northwest University, Xi’an, Shaanxi, China
- 2Department of Respiratory and Critical Care Medicine, Xi’an No.3 Hospital, The Affiliated Hospital of Northwest University, Xi’an, China
Non-small cell lung cancer (NSCLC) overwhelmingly represents the predominant histological subtype of lung cancer, with lung adenocarcinoma emerging as the most prevalent form. Conventional Western medical treatments encompass a spectrum of modalities, including surgical interventions, cytotoxic chemotherapy, radiotherapy, targeted pharmacotherapy, and immunotherapy. In contrast, Traditional Chinese Medicine (TCM) methodologies encompass traditional Chinese medicine treatments, acupuncture therapies, and tuina treatments. While conventional Western medicine has made remarkable strides in the treatment of lung cancer, it is important to acknowledge the limitations inherent in singular treatment approaches. Consequently, the quest for a more comprehensive and integrative therapeutic paradigm becomes imperative. A deficiency of evaluation criteria specific to lung adenocarcinoma treatment in the realm of TCM represents an outstanding challenge in need of resolution. Nonetheless, in the backdrop of the continuous evolution of lung adenocarcinoma treatment modalities, the amalgamation of Chinese and Western medical approaches for treating this condition has exhibited a promising trajectory. It not only contributes to mitigating toxicity and augmenting efficacy but also serves to reduce a spectrum of postoperative complications, thereby enhancing the quality of patients’ survival and extending life expectancy. This article furnishes a comprehensive survey of the research advancements in the integration of Chinese and Western medical approaches for treating lung adenocarcinoma. It elucidates the merits and demerits of individual and combined therapeutic strategies, surmounts current limitations, underscores the virtues of amalgamating Chinese and Western medical paradigms, and offers a more holistic, integrated, and efficacious treatment blueprint.
1 Causes of lung adenocarcinoma
Lung cancer stands as the predominant malignant ailment in China, with a staggering annual incidence of 789,000 new cases and approximately 631 deaths (1). Non-small cell lung cancer, chiefly represented by lung adenocarcinoma, encompasses a spectrum of clinicopathological types, including invasive adenocarcinoma (IAC), invasive adenocarcinoma variants, micro-invasive adenocarcinoma (MIA), and pre-infiltrative lesions; the latter category further bifurcates into adenocarcinoma in situ (AIS) and Atypical adenoma hyperplasia (AAH) (2). Notably, early-stage lung adenocarcinoma patients typically remain asymptomatic and are often incidentally diagnosed during routine physical examinations. However, the highly infiltrative and metastatic nature of lung adenocarcinoma occasionally results in distant metastases upon diagnosis. Patients in the intermediate and advanced stages of the disease frequently manifest conspicuous symptoms, primarily characterized by hemoptysis, chest tightness, dyspnea, and bone pain, among others (2).The therapeutic management of lung adenocarcinoma in Western medicine varies based on disease staging. In the early stages, surgical resection assumes a pivotal role, achieving a curative effect through tumor excision. In contrast, late-stage patients typically undergo conventional chemotherapy, radiotherapy, targeted pharmacotherapy, and immunomodulation to gain control over the disease, alleviate symptoms, and extend survival (3).
Chinese medicine’s approach to lung adenocarcinoma centers on the modification and regulation of the body’s internal milieu using traditional Chinese medicine components. This approach aims to bolster immunity, reduce adverse reactions, and enhance clinical efficacy. Modalities include traditional Chinese medicine treatments, acupuncture, and tuina therapy, among others (4). While Western medicine has made substantial strides in treating lung adenocarcinoma in recent years, improving patient survival rates, the associated adverse reactions and toxic side effects detrimentally impact patients’ quality of life (5).
In contrast, Traditional Chinese Medicine (TCM) boasts several advantages in the treatment of lung adenocarcinoma. It emphasizes evidence-based and individualized treatment plans tailored to patients’ specific conditions (6). However, standardized diagnostic and therapeutic criteria for TCM treatment of lung adenocarcinoma have not been universally established, representing an ongoing challenge in this field (7).
To address the need for a more comprehensive and integrated approach, the combination of Chinese and Western medicine has emerged as a compelling research focus (8). This integrated approach capitalizes on Western medicine’s direct targeting of tumors and Chinese medicine’s role in enhancing immune function, thereby improving treatment compliance and efficacy. This synergistic approach not only reduces toxicity and enhances efficiency but also mitigates post-surgery complications, enhances the quality of life, and extends survival (9). The combination of Traditional Chinese Medicine and Western medicine in the management of lung adenocarcinoma represents a holistic and synergistic treatment strategy, harnessing the strengths of both paradigms. It takes into account patients’ specific conditions and physical status, facilitating the formulation of scientifically grounded treatment plans (10). Consequently, the combination of Chinese and Western medicine emerges as a superior approach to lung cancer treatment. This article offers a comprehensive review of the utilization of Chinese medicine, and Western medicine, and their synergistic combination in the recent treatment of lung adenocarcinoma.
1.1 Western medicine to the etiology of lung adenocarcinoma
Within the purview of Western medicine, the precise etiology of lung adenocarcinoma remains enigmatic, and its pathogenesis is postulated to stem from a myriad of factors, as gleaned from clinical observations (11). These contributory factors encompass an array of determinants, such as long-term tobacco smoking, environmental pollution, occupational exposures, genetic predisposition, and concomitant chronic respiratory ailments (12). Notably, while chronic tobacco smoke exposure ranks as the most prevalent cause, lung adenocarcinoma manifests in approximately 15–20% of non-smokers, often attributed to a complex interplay of environmental and genetic influences (9). Literature within the field has reported that variances in the germline ancestry of lung adenocarcinoma may also exert an influence on the subsequent selection of somatic mutations, thereby contributing to the development of diverse subtypes of this cancer (13).
Furthermore, obesity, recognized as a risk factor for various malignancies, has been posited to exert differential effects on the idiosyncratic incidence patterns among lung adenocarcinoma patients (14). Clinical presentations among individuals afflicted by lung adenocarcinoma predominantly encompass persistent cough, chest pain, hemoptysis, dyspnea, chest constriction, and fever.
1.2 Understanding of etiology and pathogenesis of lung adenocarcinoma in traditional Chinese medicine
From a TCM perspective, lung adenocarcinoma is perceived as a manifestation of the body’s internal imbalance, reflecting disturbances not only within the body but also in the intricate interplay with the external environment. This pathological state is characterized by the depletion of vital qi, internal deficiencies, external pathogenic factors, and a profound disruption in the harmonious equilibrium between yin and yang.
Under these conditions, malignancy can take root as malevolent influences exploit the body’s weakened state, infiltrating the lungs and precipitating dysfunctional pulmonary processes (15). Consequently, the disease primarily emerges as a consequence of deficiency and is considered a “real” ailment. The underlying root of this ailment lies in the deficiency of vital qi, with associated symptoms marked by the accumulation of phlegm, stagnation of qi, blood stasis, and the accumulation of toxic elements within the pulmonary system, all contributing to the pathogenesis of lung adenocarcinoma (16).
By the principles of Chinese medicine, the lung is associated with the emotion of sadness and is intrinsically linked to the water element, the source of phlegm. Women, often more susceptible to emotional distress and prone to stagnation, may experience deficiencies in vital qi, ultimately fostering the formation of pulmonary “rocks.” Notably, lung adenocarcinoma is typified by coldness, fluid coagulation, and a propensity toward qi stagnation and blood stasis, rendering it prone to metastasis. These factors collectively contribute to the higher incidence of lung adenocarcinoma among the female population (17).
2 Overview of lung adenocarcinoma treated by Western medicine
Lung adenocarcinoma, originating from lung epithelial cells, is generally less aggressive than small-cell lung cancer. Its development is typically gradual, often remaining asymptomatic in its early stages (18). The international TNM staging system classifies lung adenocarcinoma into four stages: stage I for early-stage disease and stages II, III, and IV for intermediate and advanced stages (19). Each stage and subtype of lung adenocarcinoma warrants specific treatment approaches.
2.1 Surgical treatment
In the early stages, radical surgical resection stands as the optimal treatment approach for tumors. For stage I lung adenocarcinoma with high-risk factors, the gold standard of treatment is lobectomy combined with mediastinal lymph node dissection (20). Older patients typically undergo wedge resection or lobectomy as the standard treatment. In cases of local and regional advancement, combining surgical intervention with drug therapy and radiotherapy has shown promise in enhancing patient survival (21). Surgical treatment offers the advantage of directly excising tumors and affected organs comprehensively, irrespective of cell proliferative status or treatment sensitivity. This approach aims to completely remove the tumor and associated local tissues while preserving healthy lung tissue, it can also better understand the situation of regional lymph node metastasis and effectively control the further enlargement and spread of lung cancer, thereby achieving a radical therapeutic outcome and enhancing the patient’s quality of survival.
2.2 Chemotherapy
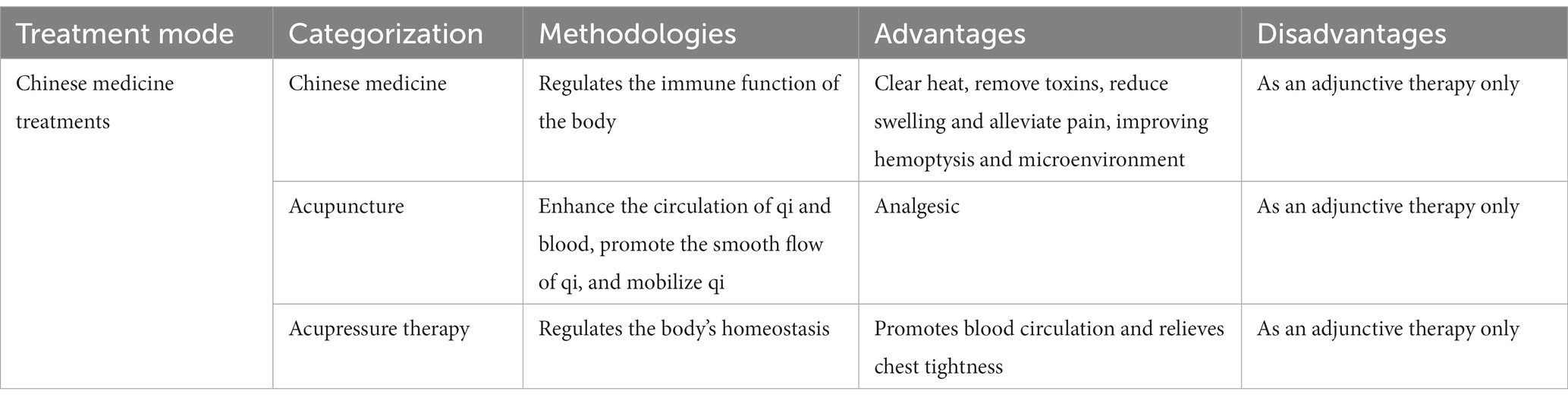
Early-stage lung adenocarcinoma often presents with subtle or no clinical symptoms, and symptoms typically become evident in the middle or advanced stages of the disease. This necessitates systemic treatments, which can limit the applicability of surgical methods. Depending on disease type and stage, appropriate radiotherapy methods can be selected, and conventional chemotherapy is employed in various contexts, including neoadjuvant chemotherapy, postoperative chemotherapy, and combined radiotherapy and chemotherapy (22). Research has demonstrated that platinum-based adjuvant chemotherapy significantly enhances the survival rates of patients with completely resected stage II or stage III lung adenocarcinoma, particularly when tailored to individual patients through biomarker screening (23). Previous experiments have indicated that for stage IV lung adenocarcinoma patients, a radiotherapy regimen followed by a combination of cisplatin and other chemotherapy agents can enhance the efficacy of radiotherapy while mitigating its side effects (24). Postoperative chemotherapy plays a pivotal role in reducing the incidence of lung adenocarcinoma and extending patient survival. Systemic chemotherapy not only controls tumor growth, reduces symptoms, and improves quality of life, but also delays metastasis to other organs. Paclitaxel as a natural compound is widely used as a chemotherapeutic drug, by inhibiting mitosis and triggering apoptosis of cancer cells, thus effectively preventing the proliferation of cancer cells, with good anti-tumor effects and few side effects (25). Camptothecin is a quinoline alkaloid, as a natural antitumor drug, mainly sensitive to proliferating cells, blocking cell division of cell cycle-specific antitumor drugs, in combination with cisplatin can enhance the sensitivity of lung cancer cells to cisplatin (26).
2.3 Targeted drug therapy
Targeted drugs represent a potent therapeutic avenue for lung adenocarcinoma, precisely honing in on specific molecules within the cancer cells, including EGFR, ALK, KRAS, ROS1, BRAF, and more. This precision inhibits the growth and dissemination of cancerous cells effectively (27). However, drug resistance remains a challenge in the targeted treatment of lung adenocarcinoma, necessitating the exploration of new mutant genes to catalyze breakthroughs in this therapeutic approach (28). Emerging studies have identified three genes, namely CDCA8, MCM6, and TTK, as potential novel drug targets, harboring pivotal roles in restraining lung cancer cell proliferation, exerting anti-tumor activities, and potentially enhancing patient survival (29). Targeted drug therapy is a purposive treatment with the advantages of less damage to normal cells, less harm to the body, and better therapeutic effects.
2.4 Radiotherapy
Radiotherapy stands as an effective approach for alleviating symptoms and bolstering local lesion control in patients grappling with advanced lung adenocarcinoma. It achieves this by employing high-energy rays to eliminate tumor cells, thereby restraining tumor growth (30). Research has highlighted that, alongside induction systemic therapy and maintenance therapy, stereotactic radiotherapy substantially extends progression-free survival from 3.5 months to an impressive 9.7 months in lung adenocarcinoma patients (31). Additionally, the application of stereotactic radiotherapy in patients with low metastatic burden significantly enhances survival rates. This reflects not only a breakthrough in augmenting the survival prospects of advanced lung adenocarcinoma patients but also demonstrates the benefits of local consolidation interventions (32).
Previous investigations have demonstrated that employing moderate radiation therapy doses in lung adenocarcinoma patients can enhance overall survival without elevating the incidence of radiation pneumonitis (33). Radiation therapy is uniquely suited to treating multiple lesions throughout the body and having a low impact on the entire body due to its lack of site restriction as well as its lesser vascular restriction.
2.5 Immunotherapy
Amid the ongoing progress in molecular and immune research along with the development of related drugs, immunotherapy has swiftly emerged as a linchpin in the management of operable and metastatic lung adenocarcinoma. This represents a pivotal advancement in lung adenocarcinoma treatment in recent years, primarily due to its capacity to engage the body’s immune system to combat tumor cells through activation or enhancemen (34).
Immunotherapy can be delineated into two distinct modalities. Monotherapy acts to impede the interaction between tumor cells and the immune system, thereby triggering the immune system’s assault on tumor cells. In contrast, employing a combined approach involving chemotherapy and immunotherapy serves to ameliorate the side effects stemming from chemotherapy (35). Ginsenoside is a natural steroid that enhances and regulates the immune function, which not only inhibits the proliferation of lung adenocarcinoma, induces apoptosis of cancer cells, inhibits the inflammatory response of the body, but also plays a role in lung protection (36). Resveratrol is a natural polyphenolic compound with anti-free radical and antioxidant properties, which exerts anti-lung adenocarcinoma effects by modulating anti-inflammatory and hormonal effects (37). Therefore, the advantage of immunotherapy is that it allows tumors to achieve sustained remission and the adverse effects produced are relatively mild; as a popular treatment modality, immunotherapy, especially combination therapy, is widely used in the treatment of patients with lung adenocarcinoma, which creates more possibilities for the improvement of patients’ quality of survival.
2.6 Microbial gut flora therapy
The gut microbiota plays a pivotal role as an immunomodulator, exerting influence over the therapeutic response and effectiveness of certain immunotherapeutic agents. It has been established that the composition of the gut microbiota can correlate with both positive and negative treatment outcomes (38). Consequently, research into the tumor gut microbiome has been a topic of fervent discussion in recent years.
Several studies have illuminated the potential of interventions like Bifidus tetra punctate tablets to enhance the gut microbiota of lung adenocarcinoma patients. These interventions have shown significant promise, not only in regulating the patient’s intestinal microecology and augmenting immunity but also as adjunctive antitumor therapies when combined with conventional chemotherapy, with minimal drug toxicity (39). Subsequent research has revealed notable disparities in the gut flora of lung cancer patients compared to individuals with benign lung lesions, further substantiating the existence of specific intestinal microorganisms within the tumor population (40). These findings not only underscore the significance of the gut microbiota in lung adenocarcinoma but also open up new avenues for its treatment.
2.7 Summary
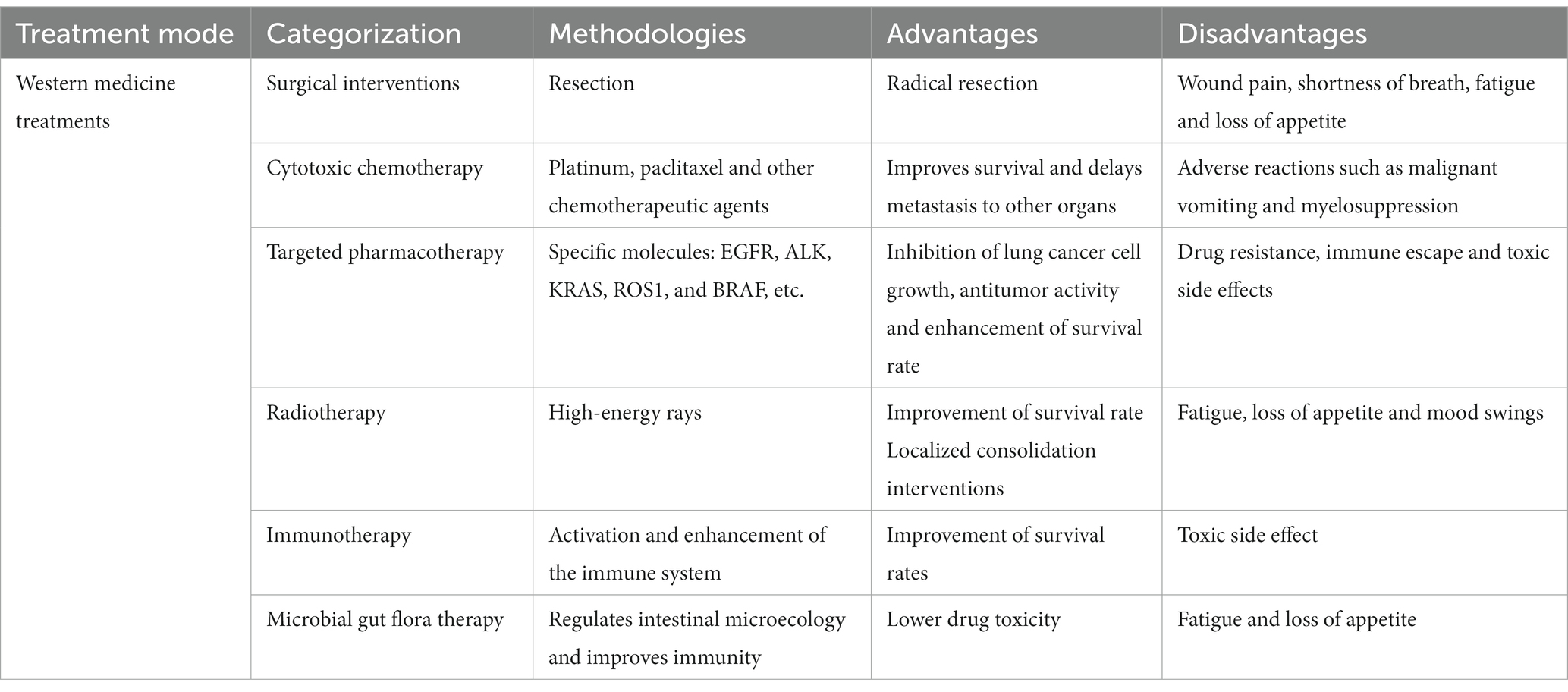
In recent years, Western medical approaches to lung adenocarcinoma have indeed achieved significant breakthroughs. This progress encompasses not only a diverse array of treatment modalities but also notable enhancements in the overall survival rates of patients. Nevertheless, it is essential not to overlook the associated challenges. Western medical treatment may give rise to issues such as toxic side effects, adverse reactions, drug resistance, and immune evasion. These phenomena consistently impact the quality of life of patients, and addressing these challenges represents a crucial imperative for the medical community moving forward. The advantages and disadvantages of Western medicine in the treatment of lung adenocarcinoma are shown in Table 1.
3 Status of traditional Chinese medicine treatment of lung adenocarcinoma
The most significant departure from Western medicine lies in its emphasis on holistic regulation. Chinese medicine perceives a close interconnection between tumor development and the status of other internal organs such as the spleen, stomach, liver, and kidneys (16). Consequently, traditional Chinese medicine aims to harmonize these organs, fostering the revitalization of vital qi, with the overarching goal of bolstering the body’s resilience, combating cancer, and dispersing nodules through a comprehensive and synergistic approach. The principle of “supporting the positive and dispelling the evil” constitutes a fundamental tenet in the treatment of malignant tumors, aiming to enhance the patient’s overall immunity (41). This approach aligns closely with the core concept of immunotherapy in Western medicine, which seeks to mitigate drug resistance and prevent tumor immunity evasion. In both traditional Chinese medicine and Western medicine, the shared objective is to eliminate cancer cells within the body by stimulating the regrowth of immune cells and enhancing immune function. Additionally, these therapies work toward regulating the tumor microenvironment, thereby contributing to the treatment of lung adenocarcinoma. In the context of traditional Chinese medicine, lung adenocarcinoma is categorized as a syndrome associated with “plaque” and “lung accumulation.” It is often attributed to deficiencies in positive qi and insufficient spleen qi. Treatment approaches typically revolve around nurturing the earth element and generating gold, fortifying the Middle Earth, and bolstering qi. One notable example is the “soup from the Discussion of Internal and External Injuries,” which epitomizes this methodology (42). Given the intricate and varied disease presentations among lung adenocarcinoma patients, traditional Chinese medicine adopts a dialectical treatment approach that underscores the importance of “when the positive qi is in memory, the evil can not be interfered with.” This involves focusing on the sonification of the spleen and kidney, strengthening and safeguarding the positive qi while concurrently addressing detoxification and the dispersal of nodules. The treatment strategy further encompasses activating blood circulation, dispelling blood stasis to counteract the toxicity of cancer, and is marked by an individualized and flexible use of herbal medicines (43).
3.1 Herbal medicine for the treatment of lung adenocarcinoma
Traditional Chinese medicine (TCM) often categorizes lung adenocarcinoma into four distinct types based on the disease’s different stages and characteristics: deficiency of lung spleen and qi, deficiency of qi and yin, internal obstruction of blood stasis and toxicity, dampness and phlegm obstruction. Treatment is then tailored to these specific types and stages, with a primary focus on supporting the positive qi as the initial step, followed by attacking the pathogenic factors and ultimately complementing treatment with tonification (44). The primary objective of traditional Chinese medicine in the treatment of lung adenocarcinoma is to regulate the body’s immune function, induce apoptosis in tumor cells, and inhibit tumor cell proliferation. There are many compounds with medicinal value in flavonoids, which not only have cough suppressant, expectorant, asthma, and antibacterial activities but also have anti-free radical and antioxidant effects. In clinical flavonoids practice, certain herbs like Lobelia and Mulberry leaf have been noted for their ability to clear heat, remove toxins, reduce swelling, and alleviate pain, making them valuable in the treatment of lung cancer (45). Scutellaria barbata, for example, is employed for dispersing blood stasis, halting bleeding, promoting diuresis, and reducing swelling, making it suitable for addressing conditions like lung carbuncle, pulmonary tuberculosis with hemoptysis, and various types of bruises and injuries (46).
Recent reports have also highlighted the anticancer efficacy of active ingredients found in herbs that promote blood circulation and alleviate blood stasis. These components significantly enhance hemodynamics and the microenvironment, reduce thrombosis, boost blood flow, and subsequently inhibit lung cancer invasion and metastasis (47). The advantage of traditional Chinese medicine in treating lung adenocarcinoma is that it can provide evidence-based treatment according to the cause and development of the patient’s disease, enhance the immunity of the patient’s body, improve the quality of life, and prolong the growth period.
3.2 Acupuncture for lung adenocarcinoma
Acupuncture and moxibustion represent traditional Chinese medicine therapies rooted in the principles of yin and yang, the five elements, qi, blood, bodily fluids, internal organs, meridians, and the dynamics of the five movements and six qi (48). In the context of treating lung adenocarcinoma, acupuncture, and moxibustion primarily aim to enhance the circulation of qi and blood, promote the smooth flow of qi, and mobilize qi. It’s crucial to note that while acupuncture and moxibustion can provide valuable support, they cannot cure lung adenocarcinoma and should be considered as complementary therapies.
The selection of specific acupuncture points and needling techniques is tailored to the individual patient’s condition, with the objective of either tonifying deficiencies or promoting detoxification through various approaches. If the patient exhibits weakness in positive qi, tonification methods are employed; conversely, if pathogenic factors are dominant, detoxification methods are applied, or a combination of both strategies may be utilized. Ultimately, the goal is to strengthen the positive qi and dispel pathogenic influences (49).
Studies have demonstrated the benefits of acupuncture in alleviating lung cancer-related symptoms such as cough and phlegm, facilitating phlegm expectoration, and reducing the frequency of coughing (50). When used in conjunction with pharmacological interventions, it can yield significant analgesic effects (51). Acupuncture treatment has shown promising benefits in reducing patients’ adverse effects, relieving pain, and controlling tumor persistence.
3.3 Acupressure therapy for lung adenocarcinoma
Tui na practitioners employ a variety of techniques, including massage, manual acupoint stimulation, and structural adjustments, to rebalance the body’s state based on the specific needs of their patients. In the context of treating lung adenocarcinoma, tui na serves to promote blood circulation and alleviate pain (52). The primary techniques utilized in tui na include kneading, pinching, pushing, holding, and pressing, with a focus on areas related to the lungs and the back.
Research has indicated that daily kneading and pressing along the lung meridian represents an effective tui na method that can stimulate the functioning of internal organs, thus contributing to the equilibrium of yin and yang within the body (53). Appropriate massage techniques help facilitate phlegm discharge, enhance blood circulation, and alleviate symptoms like chest tightness, thereby ensuring the patient’s respiratory tract remains clear and relieving lung cancer-related symptoms such as cough, chest tightness, and shoulder and back pain (54). The most significant advantage of Tui Na treatment for lung adenocarcinoma is that it relieves the patient’s pain and can also be used as an adjunct to acupuncture as a way to increase the range of motion in the joints.
3.4 Summary
Chinese medicine treatment of lung adenocarcinoma exhibits several distinctive characteristics, including a multifaceted approach, consideration of multiple perspectives, and targeting various facets of the condition. Currently, Chinese medicine treatment for lung adenocarcinoma has evolved and is demonstrating promising results, whether used independently or in conjunction with Western medicine. However, it’s essential to acknowledge that traditional Chinese medicine’s effectiveness in treating lung adenocarcinoma is not universally precise. While these therapies primarily focus on safeguarding lung function, they may not consistently inhibit cancer cell growth or exhibit potent cytotoxic effects on lung cancer cells. Furthermore, there remains a lack of standardized diagnostic and treatment criteria within traditional Chinese medicine for lung adenocarcinoma. The absence of unified typing standards and evaluation criteria contributes to the complexity of treatment. Consequently, relying solely on Chinese medicine for the treatment of lung adenocarcinoma may not guarantee a complete cure. Instead, it is often advisable to incorporate Chinese medicine as a complementary therapy alongside Western medical approaches to optimize the chances of success and enhance the overall therapeutic outcome. The advantages and disadvantages of Chinese medicine in the treatment of lung adenocarcinoma are shown in Table 2.
4 Treatment of lung adenocarcinoma with the combination of traditional Chinese and Western medicine
4.1 Combined operation of traditional Chinese medicine
Surgical treatment is often considered the best approach for patients in the early stages of lung adenocarcinoma to achieve a radical cure. However, some patients may experience various uncomfortable symptoms post-surgery, including mood disorders, wound pain, asthma, fatigue, and loss of appetite. These symptoms can significantly impact the patient’s quality of life and hinder their postoperative recovery (55). Some patients are also intolerant to surgical treatment, and there are also problems such as large postoperative trauma, susceptibility to complications, and recurrence rates. Western medical treatments may have limitations in addressing these specific aspects of postoperative discomfort. Chinese medicine, rooted in a “people-oriented” treatment philosophy, offers a holistic approach that can provide valuable support for patients during their recovery (56). Research has indicated that the use of flavonoids in Chinese medicine as an adjuvant therapy following radical surgery can have several benefits for non-small cell lung cancer (NSCLC) patients. This approach has been shown to extend the survival period and enhance the quality of life for these patients. Additionally, Chinese medicine adjuvant therapy may reduce the rate of tumor recurrence and metastasis in lung cancer patients (57). Studies conducted by Li TM and others, employing Chinese herbal medicine (CHM) from Taiwan as a postoperative treatment for lung cancer patients, demonstrated a significant improvement in patient survival. The results indicated a lower mortality risk ratio in the group receiving CHM, highlighting the potential of Chinese medicine as an adjuvant therapy in reducing mortality rates among lung cancer patients (58).
4.2 Chinese medicine combined with Western medicine chemical treatment
For patients with intermediate and advanced lung adenocarcinoma, conventional treatment typically revolves around chemotherapy, with a common regimen involving platinum-containing double drugs. This chemotherapy approach is versatile and can be applied as a standalone treatment or in combination with other modalities, allowing for tailored treatment plans based on the patient’s specific condition. These plans may encompass preoperative treatment, postoperative adjuvant therapy, or late-stage treatment. However, chemotherapy, especially when used in combination, can come with side effects that some patients may find challenging to tolerate. Common adverse reactions include malignant vomiting and myelosuppression, which can lead to a reduced capacity for chemotherapy (59). For neoadjuvant chemotherapy, although it can control the growth of tumor cells, the disadvantages of adverse effects and reduced patient tolerance to surgery should not be ignored. Traditional Chinese medicine, grounded in the principle of maintaining the dynamic balance of the body, offers an alternative approach.
Song et al. (60) found that triptolide, as a world-recognized natural antitumor drug, can specifically target different cell signaling pathways associated with lung cancer progression; when co-administered with cisplatin, it can inhibit the expression of the nuclear factor κB (NFκB) signaling pathway and NFκB-regulated drug-resistance genes, and thus play a role in drug-resistant retroviral processes. Research conducted by Guo et al. (61) divided patients with stage IV lung adenocarcinoma into two groups: one receiving platinum-based chemotherapy alone and the other receiving a combination of traditional Chinese medicine alongside chemotherapy. The results indicated a noteworthy difference in survival outcomes. Patients who received only chemotherapy had a one-year survival rate of just 27%, which fell short of the average survival period (with an average survival time of 5 months). In contrast, patients who received traditional Chinese medicine alongside chemotherapy achieved a one-year survival rate of 88%, with an average survival time of 27 months. This difference was statistically significant (p < 0.0001), highlighting the potential of traditional Chinese medicine to enhance the survival rate of stage IV lung adenocarcinoma patients undergoing second-line chemotherapy.
In a study conducted by Lu et al. (62), 60 patients with advanced lung adenocarcinoma were randomly divided into two groups: the control group consisting of 27 patients, and the observation group consisting of 33 patients. The control group received pemetrexed combined with cisplatin regimen chemotherapy, while the observation group received Shengmai capsules in addition to the control group’s treatment. The study’s results revealed that the effective rate was 60.61% in the observation group and 62.96% in the control group. Importantly, the difference between the two groups was not statistically significant (p>0.05). Additionally, when comparing serum carcinoembryonic antigen (CEA) levels between the two groups before treatment (22.36 + 5.35 μg/L in the control group, 21.19 + 4.69 μg/L in the observation group), there was no statistically significant difference (p>0.05). However, after treatment, both groups exhibited lower CEA levels compared to before treatment (18.77 + 5.92 μg/L in the control group, 13.57 + 5.59 μg/L in the observation group), with the CEA level in the observation group being lower than that in the control group (p<0.05). This outcome suggests that the combination of traditional Chinese medicine with a chemotherapy regimen can mitigate the toxic effects of chemotherapy.
In light of these findings, it is evident that tailoring treatment approaches to individual patient differences in clinical practice, such as combining chemotherapy with traditional Chinese medicine treatment, can effectively reduce toxicity while improving patients’ survival prognosis and overall clinical outcomes.
4.3 Chinese medicine combined with targeted drug therapy
Targeted drug therapy is primarily designed to inhibit the proliferation of tumor cells and induce apoptosis by acting on specific targets that play a role in tumor cell growth and metastasis. While targeted drug therapy has revolutionized personalized cancer treatment in modern oncology, it also comes with challenges such as drug resistance, immune evasion, and various toxic side effects, including skin rashes, diarrhea, and liver function impairment (63). These adverse reactions can be severe enough to cause some patients to discontinue treatment, ultimately limiting the clinical utility of targeted drugs and the potential societal benefits they offer. In traditional Chinese medicine, the adverse reactions associated with targeted drug therapy are often attributed to pathogenic factors such as heat and toxicity. For these types of adverse reactions, the treatment approach typically involves clearing heat, detoxifying, and dispersing wind to expel the pathogenic factors from the body.
Jiao et al. (64) conducted a study to investigate the combination of traditional Chinese and Western medicine in lung adenocarcinoma patients to delay acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitor (EGFR-TKI). Patients were randomly assigned to two groups: the experimental group received EGFR-TKI along with traditional Chinese medicine, while the control group received EGFR-TKI alone. The results revealed that the survival period of the EGFR-TKI + traditional Chinese medicine group was 13.50 months, whereas the EGFR-TKI group had a survival period of 10.94 months. This difference was statistically significant (p < 0.05), indicating a significant extension in overall survival for the experimental group. Additionally, the experimental group exhibited a significantly higher overall quality of life improvement rate (20.54%) compared to the control group (15.98%). This difference was statistically significant (p = 0.0160). These findings demonstrate that the combined treatment of traditional Chinese medicine with targeted drugs can effectively delay resistance to EGFR-TKI, enhance the quality of life for patients, and broaden the application of targeted drugs.
4.4 TCM combined with radiation therapy
Radiotherapy is a crucial approach in cancer treatment, utilizing radiation to target and treat tumor lesions. It is known for its localized application and wide range of therapeutic applications, offering targeted treatment options (22). However, the side effects of radiotherapy should not be ignored. After radiotherapy, patients with mild symptoms will experience fatigue, loss of appetite, and emotional uncertainty; some patients who have received radiotherapy for a long period will experience skin damage, esophageal damage, and lung damage, and in severe cases, they will experience radiation pneumonitis, radiation esophagitis, and bone marrow suppression, etc. (65). Incorporating Chinese medicine as an adjunct to radiotherapy can effectively mitigate the toxic side effects experienced by patients following radiotherapy. It helps alleviate post-radiotherapy discomfort, enhances patient compliance, and improves treatment efficacy (66).
In a study led by Du et al. (67), gefitinib and three-dimensional conformal radiotherapy were employed for treating 60 patients with advanced lung adenocarcinoma presenting with symptoms of breath and yin deficiency. Additionally, traditional Chinese medicine was integrated into the treatment protocol by administering Guiqi Yiyuan Cream orally to another 60 patients in the control group. The study outcomes revealed significant differences in favor of the treatment group. After 7 weeks of continuous treatment, the treatment group exhibited a higher total effective rate (70.00% vs. 51.57%) and total control rate (86.67% vs. 80.00%) compared to the control group, with these differences being statistically significant (p < 0.05). Moreover, the incidence rates of malignancy, diarrhea, and rash in the control group were notably higher (65.00, 20.00, and 13.33%, respectively) than those in the treatment group (28.33, 6.67, and 3.33%, respectively), and these differences were statistically significant (p < 0.05 or p < 0.01). These findings underscore the remarkable clinical efficacy of combining Guiqi Yiyuan Cream with gefitinib and radiotherapy in treating advanced lung adenocarcinoma with breath and yin deficiency syndrome. This combined approach significantly improves patient prognosis and extends their survival. Traditional Chinese medicine offers unique advantages in reducing the adverse effects of radiotherapy while enhancing tumor tissue sensitivity to radiation and thereby improving treatment effectiveness. Some studies have demonstrated that traditional Chinese medicine’s heat-clearing and detoxification properties, as well as its ability to promote blood circulation and eliminate blood stasis, can sensitize tumor tissues to radiotherapy (68).
4.5 TCM combined with immunotherapy
The introduction of immune checkpoint inhibitors marked a significant advancement in the treatment of early-stage tumors, offering the potential for personalized cancer treatment by harnessing the body’s natural tumor-fighting mechanisms (69). While targeted therapies like immunotherapy have shown great promise in treating cancer, they also come with the challenge of identifying and managing their toxic side effects. These side effects can include conditions like rash, itching, diarrhea, thyroid dysfunction, colitis, and pneumonia. Western medicine approaches immunotherapy with careful consideration of each patient’s variability and sensitivity to these toxicities. Tailored dosing is often necessary to optimize the benefits while minimizing adverse effects (70).
Here, traditional Chinese medicine can play a valuable role as an adjuvant therapy following immunotherapy. For instance, Qingzao Lung Rescue Soup has been found to effectively extend the survival period of non-small cell lung cancer patients, enhance the host’s immune response, and improve overall survival rates (71). Acupuncture, too, offers advantages in immunotherapy for non-small cell lung cancer. Scholars like Mao Jinfeng and colleagues have discovered that wheat grain moxibustion at the foot-sanli point can complement Western medicine treatments for advanced non-small cell lung cancer, boosting the immune function of patients who are tumor-free post-surgery. This combination treatment approach is well-received, well-tolerated, and safe, making it a promising option for clinical use (72). The cases and efficacy of combined Chinese and Western medicine in the treatment of lung adenocarcinoma are shown in Table 3.
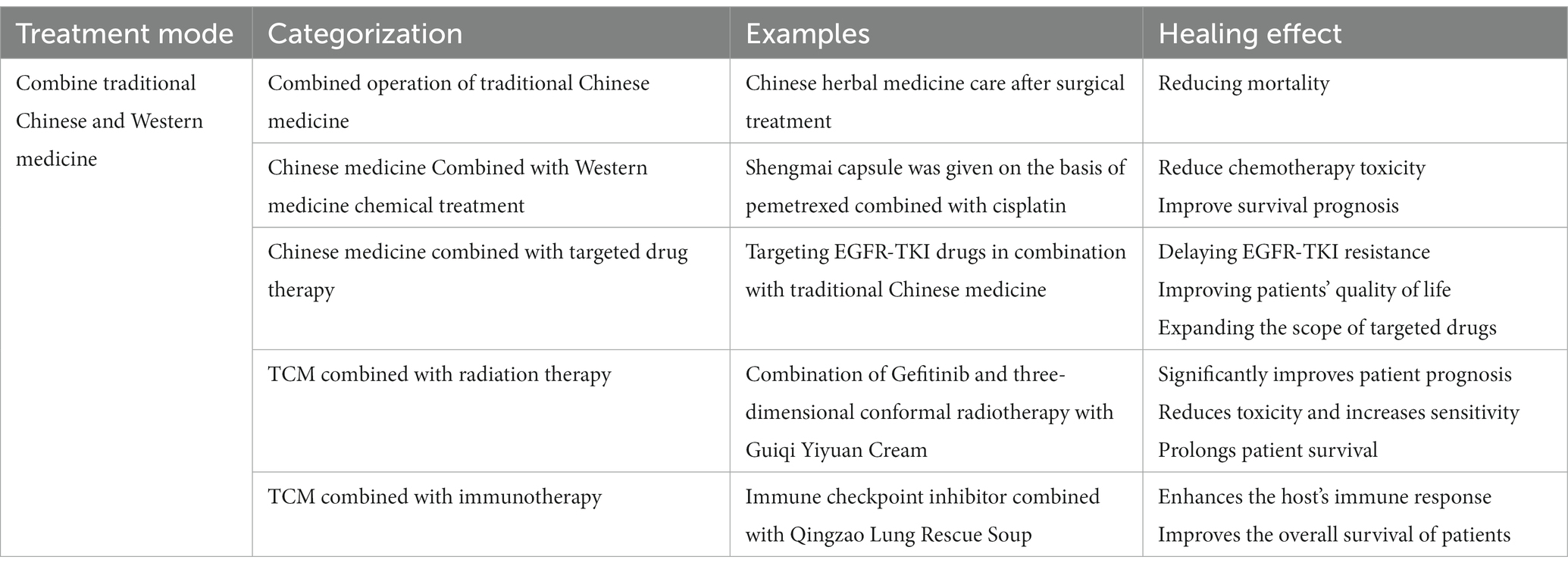
Table 3. Case and efficacy of combined Chinese and Western medicine in the treatment of lung adenocarcinoma.
5 Summary
Over the years, a range of treatment modalities, including surgery, chemotherapy, targeted drugs, radiation therapy, immunotherapy, and interventions in the intestinal flora, have played pivotal roles in managing lung adenocarcinoma across its different stages. These treatments are continually evolving with advancements in society and medical science. However, it’s important to acknowledge that these Western treatments often come with varying degrees of adverse effects for patients. Chinese medicine, with its emphasis on the holistic balance of the body and a “patient-centric” treatment approach, presents a significant advantage when combined with Western medicine. The integration of Chinese medicine into Western medicine regimens helps mitigate the drawbacks of Western treatments (73). This combined approach can contribute to improved patient well-being by reducing toxic side effects, preventing tumor recurrence and metastasis, stabilizing the patient’s emotional state, alleviating clinical symptoms, and extending the patient’s survival period.
The effectiveness of combined Chinese and Western medicine treatment compared to individual medication still lacks robust multi-center, randomized controlled, large-sample clinical data for confirmation. Additionally, the field of Chinese medicine lacks standardized criteria for the dialectical classification of lung adenocarcinoma and evaluation criteria for the disease. Further, there is limited experimental validation of the interactions between Chinese and Western medicine treatments for lung adenocarcinoma and how these interactions affect the internal environment of the body. Research into the mechanisms underlying the reduction of toxicity in combined Chinese and Western medicine treatment is also a promising future direction that requires rigorous investigation through high-quality clinical studies.
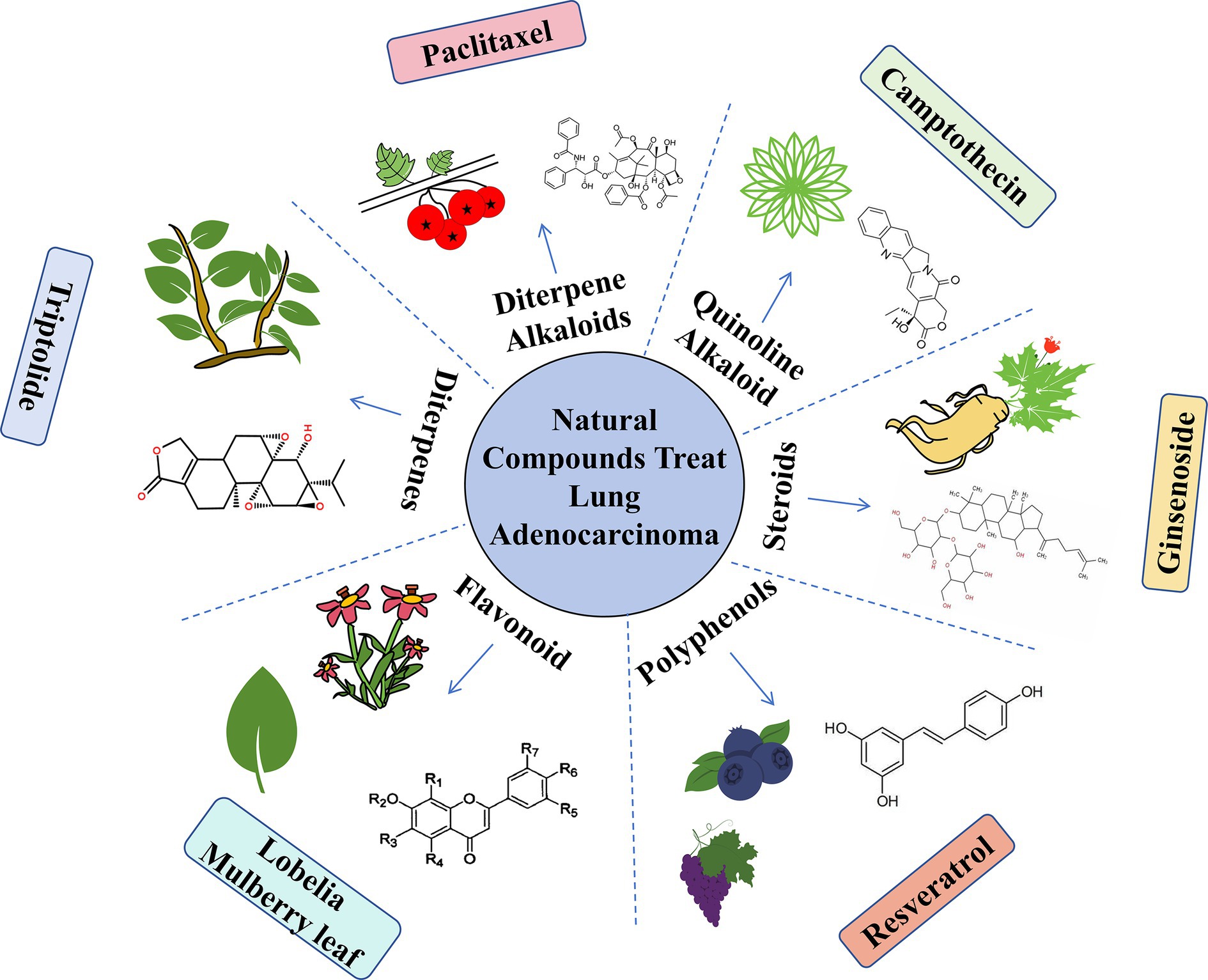
In conclusion, the integration of Chinese and Western medicines in cancer treatment remains a major area of interest and will continue to advance based on a solid and innovative theoretical foundation. We anticipate breakthroughs in this field that will bring hope to patients with cancer. Natural compounds mentioned in this article are shown in Figure 1. The comparison between Western medicine and Chinese medicine in the treatment of lung adenocarcinoma is shown in Figure 2.
Author contributions
HJ: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft. LB: Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Shaanxi Key Research and Development Program (No. 2023-YBSF-528).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zheng, R, Zhang, S, Zeng, H, Wang, S, Sun, K, Chen, R, et al. Cancer incidence and mortality in China, 2016. J Natl Cancer Cent. (2022) 2:1–9. doi: 10.1016/j.jncc.2022.02.002
2. Zhu, J, Wang, W, Xiong, Y, Xu, S, Chen, J, Wen, M, et al. Evolution of lung adenocarcinoma from preneoplasia to invasive adenocarcinoma. Cancer Med. (2023) 12:5545–57. doi: 10.1002/cam4.5393
3. Denisenko, TV, Budkevich, IN, and Zhivotovsky, B. Cell death-based treatment of lung adenocarcinoma. Cell Death Dis. (2018) 9:117. doi: 10.1038/s41419-017-0063-y
4. Consentino, R, Santos, MJ, Matos, LC, and Machado, J. Bibliometric analysis of traditional Chinese medicine scientific production between 1982 and 2016 indexed in PubMed. Medicines (Basel). (2018) 5:41. doi: 10.3390/medicines5020041
5. Duma, N, Santana-Davila, R, and Molina, JR. Non-small cell lung cancer: epidemiology, screening, diagnosis, and treatment. Mayo Clin Proc. (2019) 94:1623–40. doi: 10.1016/j.mayocp.2019.01.013
6. Kodack, DP, Farago, AF, Dastur, A, Held, MA, Dardaei, L, Friboulet, L, et al. Primary patient-derived cancer cells and their potential for personalized cancer patient care. Cell Rep. (2017) 21:3298–309. doi: 10.1016/j.celrep.2017.11.051
7. Peng, L, Zhang, K, Li, Y, Chen, L, Gao, H, and Chen, H. Real-world evidence of traditional Chinese medicine (TCM) treatment on cancer: a literature-based review. Evid Based Complement Alternat Med. (2022) 2022:1–10. doi: 10.1155/2022/7770380
8. Xu, LL, Zhang, SF, Wang, YL, Luo, YB, Fang, ZH, Fang, Y, et al. The efficacy of long-term Chinese herbal medicine use on lung cancer survival time: a retrospective two-center cohort study with propensity score matching. Evid Based Complement Alternat Med. (2021) 2021:1–13. doi: 10.1155/2021/5522934
9. Seguin, L, Durandy, M, and Feral, CC. Lung adenocarcinoma tumor origin: a guide for personalized medicine. Cancers. (2022) 14:1759. doi: 10.3390/cancers14071759
10. Liauw, W. Western medicine and traditional Chinese medicine: encouraging the twain to meet. Intern Med J. (2021) 51:833–4. doi: 10.1111/imj.15362
11. Castelletti, N, Kaiser, JC, Simonetto, C, Furukawa, K, Küchenhoff, H, and Stathopoulos, GT. The risk of lung adenocarcinoma from smoking and radiation arises in distinct molecular pathways. Carcinogenesis. (2019) 40:1240–50. doi: 10.1093/carcin/bgz036
12. Cierpiał-Wolan, M, Wójcik, S, Gawełko, J, and Czarnota, M. Does the level of air pollution affect the incidence of lung adenocarcinoma in south-eastern Poland? Int J Environ Res Public Health. (2023) 20:3177. doi: 10.3390/ijerph20043177
13. Schenk, A, López, S, Kschischo, M, and McGranahan, N. Germline ancestry influences the evolutionary disease course in lung adenocarcinomas. Evol Appl. (2020) 13:1550–7. doi: 10.1111/eva.12964
14. Kim, HR, Kim, SY, Kim, CH, Yang, SH, Lee, JC, Choi, CM, et al. Sex-specific incidence of EGFR mutation and its association with age and obesity in lung adenocarcinomas: a retrospective analysis. J Cancer Res Clin Oncol. (2017) 143:2283–90. doi: 10.1007/s00432-017-2473-8
15. Dashtdar, M, Dashtdar, MR, Dashtdar, B, Kardi, K, and Shirazi, M. The concept of wind in traditional Chinese medicine. J Pharmacopuncture. (2016) 19:293–302. doi: 10.3831/KPI.2016.19.030
16. So, TH, Chan, SK, Lee, VH, Chen, BZ, Kong, FM, and Lao, LX. Chinese medicine in cancer treatment – how is it Practised in the east and the west? Clin Oncol (R Coll Radiol). (2019) 31:578–88. doi: 10.1016/j.clon.2019.05.016
17. Wu, F, Wang, L, and Zhou, C. Lung cancer in China: current and prospect. Curr Opin Oncol. (2021) 33:40–6. doi: 10.1097/CCO.0000000000000703
18. Hutchinson, BD, Shroff, GS, Truong, MT, and Ko, JP. Spectrum of lung adenocarcinoma. Semin Ultrasound CT MR. (2019) 40:255–64. doi: 10.1053/j.sult.2018.11.009
19. Goldstraw, P, Chansky, K, Crowley, J, Rami-Porta, R, Asamura, H, Eberhardt, WEE, et al. The IASLC lung cancer staging project: proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol. (2016) 11:39–51. doi: 10.1016/j.jtho.2015.09.009
20. Matsuura, Y, Ninomiya, H, Ichinose, J, Nakao, M, Okumura, S, Nishio, M, et al. Prognostic impact and distinctive characteristics of surgically resected anaplastic lymphoma kinase-rearranged lung adenocarcinoma. J Thorac Cardiovasc Surg. (2022) 163:441–451.e1. doi: 10.1016/j.jtcvs.2020.09.120
21. Petrella, F, Rizzo, S, Casiraghi, M, Bardoni, C, Mohamed, S, Musso, V, et al. State of the art and new perspectives in the surgical treatment of lung cancer: a narrative review. Transl Cancer Res. (2022) 11:3869–75. doi: 10.21037/tcr-22-1491
22. Li, X, Wang, J, Chang, X, Gao, Z, Teng, F, Meng, X, et al. Optimal initial time point of local radiotherapy for Unresectable lung adenocarcinoma: a retrospective analysis on overall arrangement of local radiotherapy in advanced lung adenocarcinoma. Front Oncol. (2022) 12:793190. doi: 10.3389/fonc.2022.793190
23. Liu, D, Nakashima, N, Nakano, J, Tarumi, S, Matsuura, N, Nakano, T, et al. Customized adjuvant chemotherapy based on biomarker examination May improve survival of patients completely resected for non-small-cell lung cancer. Anticancer Res. (2017) 37:2501–7. doi: 10.21873/anticanres.11591
24. Su, SF, Li, M, Geng, YC, Yang, WG, Ma, Z, Li, QS, et al. Randomized phase II study of pemetrexed-cisplatin or docetaxel-cisplatin plus thoracic intensity-modulated radiation therapy in patients with stage IV lung adenocarcinoma. Am J Cancer Res. (2019) 9:1235–45.
25. Zhu, Z, Chen, D, Zhang, W, Zhao, J, Zhi, L, Huang, F, et al. Modulation of alternative splicing induced by paclitaxel in human lung cancer. Cell Death Dis. (2018) 9:491. doi: 10.1038/s41419-018-0539-4
26. Xie, J, Wang, H, Huang, Q, Lin, J, Wen, H, Miao, Y, et al. Enhanced cytotoxicity to lung cancer cells by mitochondrial delivery of camptothecin. Eur J Pharm Sci. (2023) 189:106561. doi: 10.1016/j.ejps.2023.106561
27. Ettinger, DS, Wood, DE, Aisner, DL, Akerley, W, Bauman, JR, Bharat, A, et al. Non-small cell lung cancer, version 3.2022, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. (2022) 20:497–530. doi: 10.6004/jnccn.2022.0025
28. Sánchez-Fdez, A, Re-Louhau, MF, Rodríguez-Núñez, P, Ludeña, D, Matilla-Almazán, S, Pandiella, A, et al. Clinical, genetic and pharmacological data support targeting the MEK5/ERK5 module in lung cancer. NPJ Precis Oncol. (2021) 5:78. doi: 10.1038/s41698-021-00218-8
29. Graves, OK, Kim, W, Özcan, M, Ashraf, S, Turkez, H, Yuan, M, et al. Discovery of drug targets and therapeutic agents based on drug repositioning to treat lung adenocarcinoma. Biomed Pharmacother. (2023) 161:114486. doi: 10.1016/j.biopha.2023.114486
30. Jumeau, R, Vilotte, F, Durham, AD, and Ozsahin, EM. Current landscape of palliative radiotherapy for non-small-cell lung cancer. Transl Lung Cancer Res. (2019) 8:S192–201. doi: 10.21037/tlcr.2019.08.10
31. Iyengar, P, Wardak, Z, Gerber, DE, Tumati, V, Ahn, C, Hughes, RS, et al. Consolidative radiotherapy for limited metastatic non-small-cell lung cancer: a phase 2 randomized clinical trial. JAMA Oncol. (2018) 4:e173501. doi: 10.1001/jamaoncol.2017.3501
32. Gomez, DR, Tang, C, Zhang, J, Blumenschein, GR Jr, Hernandez, M, Lee, JJ, et al. Local consolidative therapy vs. maintenance therapy or observation for patients with Oligometastatic non-small-cell lung cancer: long-term results of a multi-institutional, phase II, randomized study. J Clin Oncol. (2019) 37:1558–65. doi: 10.1200/JCO.19.00201
33. Peters, S, Felip, E, Dafni, U, Belka, C, Guckenberger, M, Irigoyen, A, et al. Safety evaluation of nivolumab added concurrently to radiotherapy in a standard first line chemo-radiotherapy regimen in stage III non-small cell lung cancer-the ETOP NICOLAS trial. Lung Cancer. (2019) 133:83–7. doi: 10.1016/j.lungcan.2019.05.001
34. Bader, JE, Voss, K, and Rathmell, JC. Targeting metabolism to improve the tumor microenvironment for cancer immunotherapy. Mol Cell. (2020) 78:1019–33. doi: 10.1016/j.molcel.2020.05.034
35. Zhu, L, and Qin, J. Coexistence of a novel SETD2-ALK, EML4-ALK double-fusion in an advanced lung adenocarcinoma patient after alectinib resistant and response to immunotherapy combined with chemotherapy: a case report. Discov Oncol. (2023) 14:44. doi: 10.1007/s12672-023-00654-x
36. Wang, L, Zhang, Y, Song, Z, Liu, Q, Fan, D, and Song, X. Ginsenosides: a potential natural medicine to protect the lungs from lung cancer and inflammatory lung disease. Food Funct. (2023) 14:9137–66. doi: 10.1039/D3FO02482B
37. Innets, B, Thongsom, S, Petsri, K, Racha, S, Yokoya, M, Moriue, S, et al. Akt/mTOR targeting activity of resveratrol derivatives in non-small lung cancer. Molecules. (2022) 27:8268. doi: 10.3390/molecules27238268
38. Szczyrek, M, Bitkowska, P, Chunowski, P, Czuchryta, P, Krawczyk, P, and Milanowski, J. Diet, microbiome, and cancer immunotherapy-a comprehensive review. Nutrients. (2021) 13:2217. doi: 10.3390/nu13072217
39. Lomeli, BK, Galbraith, H, Schettler, J, Saviolakis, GA, el-Amin, W, Osborn, B, et al. Multiple-ascending-dose phase 1 clinical study of the safety, tolerability, and pharmacokinetics of CRS3123, a narrow-Spectrum agent with minimal disruption of Normal gut microbiota. Antimicrob Agents Chemother. (2019) 64:e01395–19. doi: 10.1128/AAC.01395-19
40. Wang, RP, Wang, XH, Li, ZM, and Sun, JR. Changes in serum inflammatory factors, adiponectin, intestinal flora and immunity in patients with non-small cell lung cancer. Eur Rev Med Pharmacol Sci. (2020) 24:10566–72. doi: 10.26355/eurrev_202010_23412
41. Matos, LC, Machado, JP, Monteiro, FJ, and Greten, HJ. Understanding traditional Chinese medicine therapeutics: an overview of the basics and clinical applications. Healthcare (Basel). (2021) 9:257. doi: 10.3390/healthcare9030257
42. Hu, J, Li, X, Fang, Y, and Peng, J. Efficacy and safety of Buzhong Yiqi decoction in improving cancer-related fatigue and immunity of cervical carcinoma patients: a protocol of randomized controlled trial. Medicine (Baltimore). (2021) 100:e27938. doi: 10.1097/MD.0000000000027938
43. Zhang, Y, Liang, Y, and He, C. Anticancer activities and mechanisms of heat-clearing and detoxicating traditional Chinese herbal medicine. Chin Med. (2017) 12:20. doi: 10.1186/s13020-017-0140-2
44. Wu, Y, Wang, W, Yu, Z, Yang, K, Huang, Z, Chen, Z, et al. Mushroom-brush transitional conformation of mucus-inert PEG coating improves co-delivery of oral liposome for intestinal metaplasia therapy. Biomater Adv. (2022) 136:212798. doi: 10.1016/j.bioadv.2022.212798
45. Du, XQ, Shi, LP, Cao, WF, Chen, ZW, Zuo, B, and Hu, JY. Add-on effect of honeysuckle in the treatment of coronavirus disease 2019: a systematic review and Meta-analysis. Front Pharmacol. (2021) 12:708636. doi: 10.3389/fphar.2021.708636
46. Wang, Q, Acharya, N, Liu, Z, Zhou, X, Cromie, M, Zhu, J, et al. Enhanced anticancer effects of Scutellaria barbata D. Don in combination with traditional Chinese medicine components on non-small cell lung cancer cells. J Ethnopharmacol. (2018) 217:140–51. doi: 10.1016/j.jep.2018.02.020
47. Wu, S, Sun, Z, Guo, Z, Li, P, Mao, Q, Tang, Y, et al. The effectiveness of blood-activating and stasis-transforming traditional Chinese medicines (BAST) in lung cancer progression-a comprehensive review. J Ethnopharmacol. (2023) 314:116565. doi: 10.1016/j.jep.2023.116565
48. Lin, ML, Wu, HC, Hsieh, YH, Su, CT, Shih, YS, Lin, CW, et al. Evaluation of the effect of laser acupuncture and cupping with ryodoraku and visual analog scale on low back pain. Evid Based Complement Alternat Med. (2012) 2012:521612:1–7. doi: 10.1155/2012/521612
49. He, Y, Guo, X, May, BH, Zhang, AL, Liu, Y, Lu, C, et al. Clinical evidence for Association of Acupuncture and Acupressure with Improved cancer Pain: a systematic review and Meta-analysis. JAMA Oncol. (2020) 6:271–8. doi: 10.1001/jamaoncol.2019.5233
50. Wagner, L, Cramer, H, Klose, P, Lauche, R, Gass, F, Dobos, G, et al. Herbal medicine for cough: a systematic review and Meta-analysis. Forsch Komplementmed. (2015) 22:359–68. doi: 10.1159/000442111
51. Swarm, RA, Paice, JA, Anghelescu, DL, Are, M, Bruce, JY, Buga, S, et al. Adult cancer pain, version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. (2019) 17:977–1007. doi: 10.6004/jnccn.2019.0038
52. Emtiazy, M, and Abrishamkar, M. The effect of massage therapy on Children's learning process: a review. Iran J Med Sci. (2016) 41:S64.
53. Wang, LN, and He, W. Nursing experience of abdominal massage intervention for gastrointestinal dysfunction after lung transplantation. Transpl Immunol. (2022) 72:101590. doi: 10.1016/j.trim.2022.101590
54. Zhou, Z, Wang, Y, Zhang, C, Meng, A, Hu, B, and Yu, H. Design and massaging force analysis of wearable flexible single point massager imitating traditional Chinese medicine. Micromachines (Basel). (2022) 13:370. doi: 10.3390/mi13030370
55. Bao, J, Wu, Z, Zhang, C, Zhang, M, Wang, Y, Li, H, et al. Efficacy and mechanism of osimertinib combined with bevacizumab in the treatment of postoperative EGFR positive stage II-IIIA lung adenocarcinoma. Am J Transl Res. (2022) 14:633–42.
56. Yao, CL, Zhang, JQ, Li, JY, Wei, WL, Wu, SF, and Guo, DA. Traditional Chinese medicine (TCM) as a source of new anticancer drugs. Nat Prod Rep. (2021) 38:1618–33. doi: 10.1039/d0np00057d
57. Zhao, X, Dai, X, Wang, S, Yang, T, Yan, Y, Zhu, G, et al. Traditional Chinese medicine integrated with chemotherapy for stage II-IIIA patients with non-small-cell lung cancer after radical surgery: a retrospective clinical analysis with small sample size. Evid Based Complement Alternat Med. (2018) 2018:1–7. doi: 10.1155/2018/4369027
58. Li, TM, Yu, YH, Tsai, FJ, Cheng, CF, Wu, YC, Ho, TJ, et al. Characteristics of Chinese herbal medicine usage and its effect on survival of lung cancer patients in Taiwan. J Ethnopharmacol. (2018) 213:92–100. doi: 10.1016/j.jep.2017.10.031
59. Jang, YJ, Hyun, D, Choi, CM, Lee, DH, Kim, SW, Yoon, S, et al. Optimizing palliative chemotherapy for advanced invasive mucinous adenocarcinoma of the lung. BMC Cancer. (2021) 21:731. doi: 10.1186/s12885-021-08472-6
60. Song, JM, Molla, K, Anandharaj, A, Cornax, I, O Sullivan, MG, Kirtane, AR, et al. Triptolide suppresses the in vitro and in vivo growth of lung cancer cells by targeting hyaluronan-CD44/RHAMM signaling. Oncotarget. (2017) 8:26927–40. doi: 10.18632/oncotarget.15879
61. Guo, H, Liu, JX, Xu, L, Madebo, T, and Baak, JP. Traditional Chinese medicine herbal treatment may have a relevant impact on the prognosis of patients with stage IV adenocarcinoma of the lung treated with platinum-based chemotherapy or combined targeted therapy and chemotherapy. Integr Cancer Ther. (2011) 10:127–37. doi: 10.1177/1534735410387599
62. Lu, M, Shen, JL, Zhang, T, Hu, XF, and Xu, DD. Shengmai capsule combined with chemotherapy in the treatment of advanced lung adenocarcinoma. New Chin Med. (2022) 54:150–3. doi: 10.13457/j.cnki.jncm.2022.08.035
63. Zheng, SY, Shen, W, Peng, YM, Cui, HJ, Duan, H, Qiu, YQ, et al. Treatment of severe rash caused by crizotinib with both traditional Chinese medicine and Western medicine: two case reports and literature review. Medicine. (2018) 97:e13088. doi: 10.1097/MD.0000000000013088
64. Jiao, L, Xu, J, Sun, J, Chen, Z, Gong, Y, Bi, L, et al. Chinese herbal medicine combined with EGFR-TKI in EGFR mutation-positive advanced pulmonary adenocarcinoma (CATLA): a multicenter, randomized, double-blind, placebo-controlled trial. Front Pharmacol. (2019) 10:732. doi: 10.3389/fphar.2019.00732
65. Wang, Y, Wu, G, Li, R, Luo, Y, Huang, X, He, L, et al. Chinese medicine combined with EGFR-TKIs prolongs progression-free survival and overall survival of non-small cell lung cancer (NSCLC) patients harboring EGFR mutations, compared with the use of TKIs alone. Front Public Health. (2021) 9:677862. doi: 10.3389/fpubh.2021.677862
66. Nowak, P, Bil-Lula, I, and Śliwińska-Mossoń, M. A cross-talk about Radioresistance in lung cancer-how to improve Radiosensitivity according to Chinese medicine and medicaments that commonly occur in pharmacies. Int J Mol Sci. (2023) 24:11206. doi: 10.3390/ijms241311206
67. Du, SG, Li, JT, Liang, JQ, Li, J, Wang, GC, Wang, QS, et al. Clinical observation of Guiqi Yiyuan ointment combined with gefitinib and radiotherapy in the treatment of 60 cases of qi-yin deficiency syndrome in advanced lung adenocarcinoma. J Gansu Univ Tradit Chin Med. (2021) 38:51–5. doi: 10.16841/j.issn1003-8450.2021.03.11
68. Song, G, Jiang, T, Wang, Y, Gu, T, and Li, W. Observation of the curative effect of acupuncture for Tonifying kidney and removing blood stasis combined with radiofrequency surgery in patients with NSCLC and the diagnostic efficacy of combined detection of NTx, BGP, and CYFRA21-1 in the occurrence of bone metastases. Contrast Media Mol Imaging. (2022) 2022:1–7. doi: 10.1155/2022/8157157
69. Zhan, X, Feng, S, Zhou, X, Liao, W, Zhao, B, Yang, Q, et al. Immunotherapy response and microenvironment provide biomarkers of immunotherapy options for patients with lung adenocarcinoma. Front Genet. (2022) 13:1047435. doi: 10.3389/fgene.2022.1047435
70. Sepesi, B, Cascone, T, Chun, SG, Altan, M, and le, X. Emerging therapies in thoracic malignancies—immunotherapy, targeted therapy, and T-cell therapy in non–small cell lung cancer. Surg Oncol Clin. (2020) 29:555–69. doi: 10.1016/j.soc.2020.06.009
71. Liao, YH, Li, CI, Lin, CC, Lin, JG, Chiang, JH, and Li, TC. Traditional Chinese medicine as adjunctive therapy improves the long-term survival of lung cancer patients. J Cancer Res Clin Oncol. (2017) 143:2425–35. doi: 10.1007/s00432-017-2491-6
72. Tian, C, Fan, Y, Xu, J, Huang, Y, Wang, W, Wang, S, et al. The efficacy and safety of acupuncture and moxibustion combined with western medicine for obsessive-compulsive disorder: a protocol for systematic review and meta-analysis. Medicine (Baltimore). (2020) 99:e21395. doi: 10.1097/MD.0000000000021395
Keywords: combined Chinese and Western medicine treatment, lung adenocarcinoma, review, Western medicine, Chinese medicine
Citation: Jiang H and Bu L (2024) Progress in the treatment of lung adenocarcinoma by integrated traditional Chinese and Western medicine. Front. Med. 10:1323344. doi: 10.3389/fmed.2023.1323344
Edited by:
Roberto Carbone, University of Genoa, ItalyReviewed by:
Bao-ping Tian, Zhejiang University School of Medicine, ChinaJia-Xin Li, Macau University of Science and Technology, Macao SAR, China
Copyright © 2024 Jiang and Bu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lina Bu, YnVsaW5hMjAyMkBtZWQubnd1LmVkdS5jbg==
 Hongxin Jiang
Hongxin Jiang Lina Bu
Lina Bu