- 1Faculdade de Medicina, Universidade de Lisboa, Lisbon, Portugal
- 2Hospital de Vila Franca de Xira, Vila Franca de Xira, Portugal
MASLD prevalence is growing towards the leading cause of end-stage liver disease. Up to today, the most effective treatment is weight loss. Weight loss interventions are moving from lifestyle changes to bariatric surgery or endoscopy, and, more recently, to a new wave of anti-obesity drugs that can compete with bariatric surgery. Liver-targeted therapy is a necessity for those patients who already present liver fibrosis. The field is moving fast, and in the near future, we will testify to a disruptive change in MASLD treatment, similar to the paradigm-shift that occurred for hepatitis C almost one decade ago with direct antiviral agents.
1 Introduction
Metabolic-associated steatotic liver disease (MASLD) is a global pandemic, affecting 2 out of 5 persons worldwide (1). Recently, a study on the NHANES database showed a prevalence of steatotic liver disease of 42%, with almost all patients presenting metabolic dysfunction, of whom almost 90% had MASLD and 8% Met-ALD (that is the combination of MASLD with moderate alcohol intake) (2). In the last half-century, its prevalence increased by 50%, with a striking acceleration in its growth in the last two decades (1), when the incidence of MASLD is estimated to have tripled (3). Aligned with these statistics, MASLD is the contributor to the burden of cirrhosis and liver cancer with the most rapid global growth (4), being already the second cause of liver transplantation, and the first among women (5).
The main driver of MASLD is obesity and adiposopathy (6), as well as the metabolic disturbances that come with it such as insulin-resistance/type 2 diabetes mellitus (T2DM), dyslipidemia, and hypertension (7). When considering the treatment of patients with MASLD, we must take into consideration that 90–95% of patients will not progress to liver cirrhosis, and the ones that progress to liver cirrhosis take 20 to 25 years (8). Also, MASLD pathology is a highly dynamic entity, with the possibility to regress, which may occur in the very short time when it comes to steatosis, and longer, but still possible, for fibrosis, when adiposopathy is mitigated. Importantly, patients with MASLD have an almost two-fold increase in mortality compared to the general population, which increases with the prevalence and severity of liver fibrosis, being up to 4-fold in those with F4 fibrosis/cirrhosis (9). The severity of fibrosis associates not only with liver-related mortality but also with overall and cardiovascular mortality (10). The main causes of death are cancer, cardiovascular disease, and only in third place liver disease (9). Remarkably, the obesity-associated risk for cancer seems to be dependent on the development of MASLD (11).
MASLD patients should be managed by multidisciplinary teams composed by hepatologists, endocrinologists, cardiologists, physical and rehabilitation doctors, dietitians, and psychologists (12). The ideal treatment for MASLD should target not only the progression of liver disease but also the metabolic risk factors that promote cardiovascular disease and cancer. Because MASLD is a slowly progressive disease, clinical endpoints are difficult to achieve and assess in clinical trials. As such, the most aspired endpoint is fibrosis reversal, since fibrosis severity is the main prognostic factor in MASLD, not only regarding liver progression and outcomes, as well as extra-hepatic cardiovascular endpoints. Finally, the ideal treatment for MASLD should have a solid safety profile, in order not to induce harm in asymptomatic patients that may continue morbid event-free for decades. Currently, there is still no drug approved for the treatment of MASLD, but we are living in exciting times, with strong joined efforts in the quest to find new efficient drugs.
This review will summarize how MASLD patients should be managed today, as well as the recent advances in the field and what to expect in the near future.
2 Management of adiposopathy
MASLD is the hepatic expression of adiposopathy, which occurs when the adipose tissue capacity is surpassed by surplus energy (6). Severe obesity systematically exceeds the adipose tissue capacity (13), but each individual has its own intrinsic threshold, which may be surpassed even in the range of normal body weight index (BMI) (14, 15). Adiposopathy promotes MASLD but also metabolic dysfunction, cardiovascular disease, and cancer. As such, all patients with MASLD, whatever the severity of the pathology, are at risk of increased all-cause mortality, mostly at the expense of cancer and cardiovascular-related mortality (9). Hence, all patients with MASLD should be managed by targeting adiposopathy, decreasing the adipose tissue burden, and improving its function.
Weight loss is an efficient strategy to improve MASLD. Indeed, loss of at least 5% of body weight associates with steatosis regression, 7% loss with metabolic-associated steatohepatitis (MASH) resolution, and 10% or more with fibrosis regression in up to 80% of the patients (16). This could not be equalized, until now, by any drug therapy. Even in patients already with liver cirrhosis, weight loss achieved with a hypocaloric diet and exercise is still beneficial, since it induces a decrease in portal hypertension (17).
2.1 Lifestyle interventions
Recent studies with the NHANES database showed that a healthy diet and physical activity synergically protect from MASLD. The protective effect of diet could be virtually explained by lower BMI and waist circumference, whereas the latter would only be responsible for about half the attributable benefits of physical activity (18). Similarly, in patients with MASLD, a healthy diet and physical activity can decrease all-cause and cardiovascular mortality. There is no lower threshold above which physical activity protects from mortality, and any increase in exercise can still have a positive impact on survival (19).
Regarding diet recommendations, patients should be advised to engage in a hypocaloric diet, with a 500 to 1,000 kcal deficit, in order to promote weight loss. The relative importance of energy intake quantity over the quality of nutrients in the diet is debatable, with epidemiological studies showing discrepant results (20). However, there is strong evidence that high fructose consumption promotes MASLD development and progression (21). Furthermore, the type of fat consumed may have a role, with some evidence that high cholesterol and saturated fatty acids intake promotes MASLD, fibrosis, and hepatocellular carcinoma, whereas omega-3 polyunsaturated fatty acids showed a potential role in hepatocellular carcinoma protection (22–24). Finally, consumption of animal proteins, particularly from red meat seems to be associated with insulin resistance and MASLD (25).
Different diets have been proposed, the most accepted one being the Mediterranean diet (MD). The MD is a health-promoting diet that consists of a high consumption of plant-based foods such as vegetables and fruits, whole grains, seeds, nuts, and legumes; and a low consumption of sugars and refined carbohydrates. It favors fish over meat, being particularly scarce in red meat. The primary source of fat comes from monounsaturated fatty acids-rich olive oil (26). Small studies and meta-analyses suggest that the MD is associated with an improvement in liver enzymes, steatosis, and even liver fibrosis evaluated by non-invasive tests (NIT) (27, 28). Importantly, in the general population and in MASLD patients, MD seems to be associated with a lower risk of T2DM, cardiovascular and cancer mortality, including from liver cancer (29–31).
Another popular diet is intermittent fasting. These diets allow ad libitum energy intake but are restricted to a limited time window. Focusing on an eating window rather than caloric intake, has the advantage of potentially higher adherence compared to calorie-restricted diets, since simply skipping a meal can promote by itself a restriction in caloric intake and weight loss (32). Intermittent fasting also seems to improve metabolic dysfunction with better glucose and blood pressure control (33), liver steatosis, and liver fibrosis assessed by NIT (34). However, the level of evidence resumes small studies with weak endpoints, and it is not more effective than other diets with calorie restriction regarding weight loss or metabolic dysfunction (35). Also, when engaging in intermittent fasting, one should take into consideration that the choice of meal to skip may matter, since diurnal circadian rhythms may have an impact on health. For example, epidemiological studies suggest that skipping breakfast was associated with overweight and obesity (36), a higher risk of T2DM (37), cardiovascular mortality (38), as well as, gastrointestinal and liver cancer (39).
Coffee consumption provided that sugar/sweeteners are not added, seems to have a protective role, with a reported association between intake of at least two coffees a day with a lower risk of steatosis and liver fibrosis (40, 41), and 3 coffees with a decreased risk for hepatocellular carcinoma (42). The beneficial effects are transversal for regular and decaffeinated coffee (43).
Regarding alcohol intake, even though there is no robust scientific evidence to recommend complete abstinence in all MASLD patients, we should not advise patients to drink alcohol. Large epidemiological studies even suggest that in patients with MASLD, very mild alcohol consumption (that is, less than one drink a day) was associated with a decreased all-cause mortality, but only in nonsmokers and without significant fibrosis (44, 45). Having said that, alcohol and metabolic dysfunction are synergic in inducing liver disease (46–48), and a recent systematic review suggested that any alcohol intake might increase the risk of progression of liver disease in MASLD patients (49). In patients with cirrhosis, any alcohol intake was associated with increased mortality (50) and risk of hepatocellular carcinoma (51).
Physical activity, particularly recreational and not occupational, associated with weight loss and a protective effect against liver steatosis (52), even when weight loss was not achieved. Both aerobic and anaerobic exercises should be advised, and any increase in physical activity seems beneficial, even though the goal should be at least 45 min of moderate-intensity exercise, 3 times per week (53).
Interventions in lifestyle are hindered by a low success rate in achieving weight loss, lower than 10% (16). Furthermore, only up to one-fourth of those achieving weight loss are able to maintain the weight, and 60% of patients regain weight within the first year (54).
These statistics should not persuade us to enroll patients in lifestyle interventions. Indeed, even when patients regain weight after achieving weight loss during lifestyle interventions, the beneficial effects of the transient weight loss on liver steatosis and metabolic dysfunction seems to persist for at least 2 years (55).
2.2 Bariatric surgery
Bariatric or metabolic surgery is an approved intervention to manage patients with morbid obesity (BMI at least 40 kg/m2), grade II obesity (BMI 34.9 to 40 kg/m2) with at least one weight-related comorbidity, or patients with T2DM and grade I obesity who maintain poor metabolic control after lifestyle intervention and pharmacotherapy (56). Indeed, compared with conventional treatment, bariatric surgery associated with long-term weight loss, decreased incidence of T2DM, improvement in glucose metabolism control in diabetics translating in lower rates of diabetes-related complications (57), and an up to 50% decrease in all-cause and cardiovascular mortality (58, 59) with an increase in life expectancy of 6 years (up to 9 years in diabetic patients) (60).
Bariatric surgery is also effective in the treatment of MASLD, inducing long-term effects that sustain at least 5 years. Observational studies suggested that bariatric surgery promotes steatosis resolution, MASH resolution without worsening fibrosis in around 80%, and fibrosis regression in 70%. More than 50% of the patients may achieve complete fibrosis resolution, even the ones with advanced fibrosis at baseline. The beneficial effects seem dependent on weight loss (61–63). A recent open-label trial randomized almost 300 patients with MASH for lifestyle intervention or bariatric surgery, and showed that surgery was associated with a one-year 70% higher chance of achieving fibrosis improvement of at least one stage and with a 50% decreased risk of worsening fibrosis (64). Importantly, in MASLD patients, bariatric surgery was associated with a decreased risk of major liver and cardiovascular outcomes (65, 66).
There are two types of bariatric surgery: (1) Restrictive, which restricts the calorie intake through decreasing the stomach capacity; and (2) Restrictive and Malabsorptive, which bypass the proximal small bowel leading to a decreased absorptive surface and a hormonal effect that improves insulin resistance. Examples of restrictive surgeries are Adjustable Gastric Banding and Sleeve Gastrectomy. Examples of restrictive and malabsorptive surgeries are Roux-en-Y Gastric Bypass and Biliopancreatic Diversion with Duodenal Switch (67). Restrictive surgeries induce less weight loss but at the expense of lower adverse effects as compared with malabsorptive surgeries (67). The effect on MASLD seems dependent on the type of surgery performed. Indeed, adjustable gastric banding seems less effective in improving liver histology (68), whereas sleeve gastrectomy and gastric bypass seem similarly effective (69–71).
The complication rate of bariatric surgery does not seem to increase in patients with MASH (72). However, bariatric surgery should be proposed with caution to patients with liver cirrhosis, since mortality rates surpass 1%. Decompensated cirrhosis is an absolute contraindication for bariatric surgery since mortality rates increase to almost 20% (73). In the context of liver transplantation, surgery could be offered before the transplant in well-compensated cirrhotics. Furthermore, the Mayo Clinic is undergoing a prospective program of simultaneous liver transplantation and sleeve gastrectomy with promising results (74, 75). Bariatric surgery after liver transplantation also seems feasible, even though the level of evidence is low (76).
2.3 Endoscopic bariatric interventions
The field of endoscopic bariatric interventions has evolved dramatically in the past years, with the development of several new interventions. We have now available intragastric devices that restrict food intake (balloons, endoscopic sleeve gastroplasty, and aspiration therapy) and small bowel devices that target metabolic profile and insulin resistance (endobarrier and duodenal mucosal resurfacing). Intragastric balloons are the oldest technology and work by filling the stomach with a balloon, which decreases its capacity promoting early satiety. Endoscopic sleeve gastroplasty consists of a decrease in stomach size by applying full-thickness bites with a suturing device causing apposition of tissue along the greater curvature. Aspiration therapy consists of applying a percutaneous gastrostomy tube, which allows the partial drainage of the gastric food content after a meal. Endobarrier consists of the application of a plastic liner, 60 cm long, anchored to the duodenal bulb, which prevents duodenal absorption. Last, duodenal mucosa resurfacing consists of the hydrothermal ablation of 10 cm of the duodenal mucosa, which decreases its absorptive function (67).
Even though the level of evidence for the beneficial effects of these interventions in the management of MASLD patients is low, a recent meta-analysis with 863 patients, suggests that globally these procedures may result in histologic improvement (77). The intragastric balloon seems to have only a transient effect on weight, with most patients regaining weight after balloon removal (78), and as such it does not seem an adequate long-term therapy (79). On the contrary, a study with a 2-year follow-up of obese MASLD patients submitted to endoscopic sleeve gastroplasty did show a sustained effect on weight, as well as an improvement in liver histology, with 20% of the patients that presented baseline F3-F4 fibrosis regressing for F0-F2 fibrosis (80). After these encouraging results, a randomized controlled trial comparing surgical versus endoscopic gastric sleeve interventions, the TESLA-NASH study, is ongoing (81). Regarding endobarrier and duodenal mucosa resurfacing, both have shown, in preliminary studies, to improve steatosis and fibrosis assessed by NIT (82, 83).
2.4 Weight loss drugs
The pharmacological treatment of obesity is undergoing exciting advances in the last 5 years. The oldest generation of anti-obesity drugs could achieve a very mild weight loss of 3 to 8% (84). The first change in paradigm was the realization that anti-diabetic drugs that act as glucacon-like peptide-1 (GLP-1) receptor agonists were able to promote weight loss through its pleiotropic action promoting satiety, delaying gastric emptying, aside from its metabolic effects (85). One example is liraglutide, which showed in the SCALE studies, that it could promote weight loss of 6–8% of body weight, at a dose of 3.0 mg daily (86, 87). Liraglutide also showed in a small phase 2 study, the LEAN study, with 52 patients, to induce higher resolution of steatohepatitis (39% vs. 9%) and lower progression of fibrosis (9% vs. 36%) compared to placebo, even though it did not associate with improvement in fibrosis (88). Histological response was not associated with higher weight loss, suggesting that the beneficial effects in the liver surpass its effects promoting weight loss.
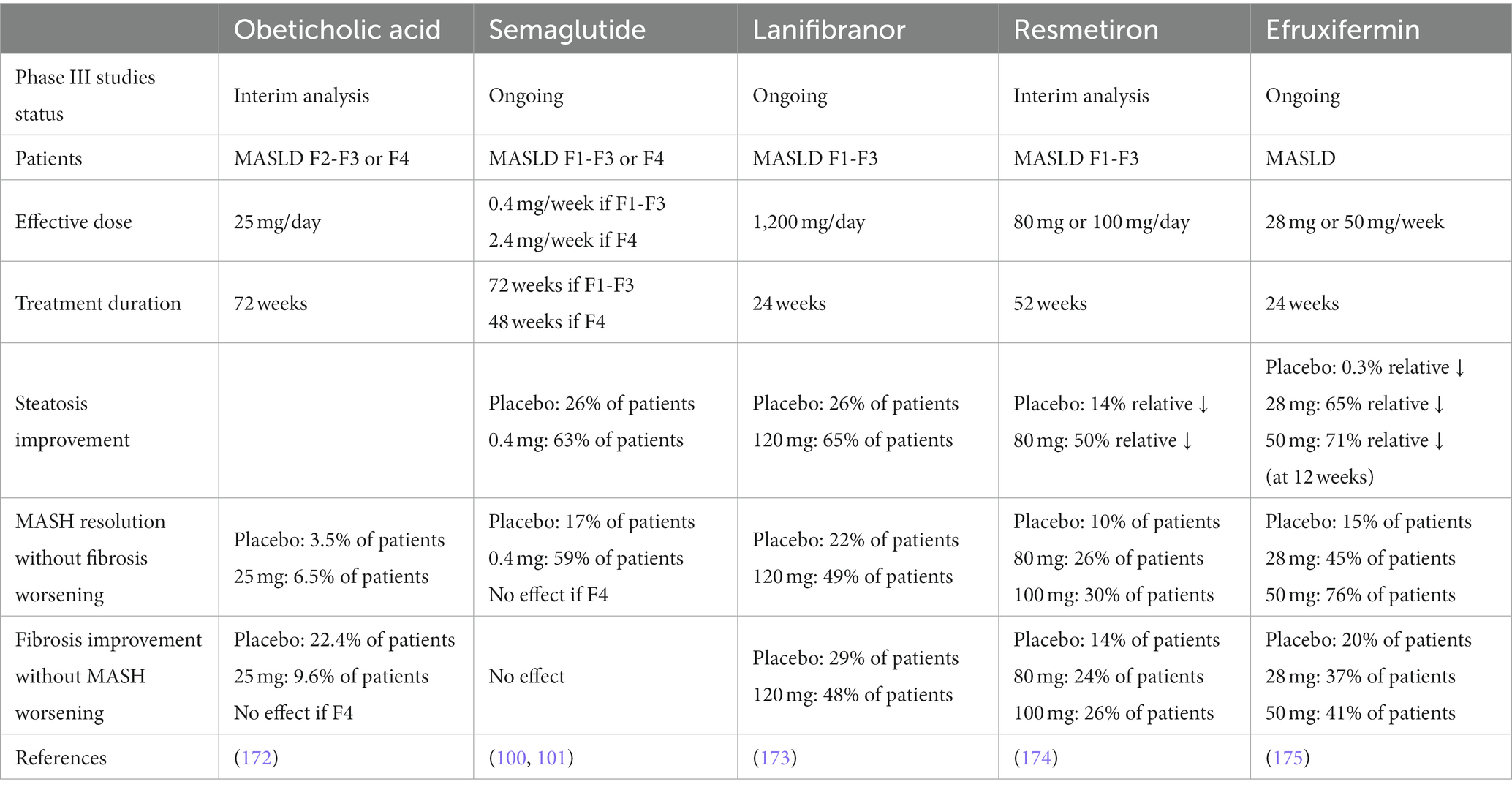
Semaglutide, another GLP-1 receptor agonist, is more potent than liraglutide in promoting weight loss, at the dose of 2.4 mg per week (89, 90). The STEP studies showed an average weight loss of 12% (91–95). Besides its effects on glucose control, it also improved lipid profile and blood pressure, even when compared to patients losing the same weight on placebo (91, 96). These metabolic effects may explain why semaglutide treatment is associated with an almost 25% decrease in major adverse cardiovascular events, decreased all-cause and cardiovascular mortality (97–99). Semaglutide was already studied in phase 2 and 3 studies as a treatment for MASLD. A phase 2b study enrolled 320 patients with MASH and fibrosis F1 to F3, who were treated with increasing doses of semaglutide or placebo (100). The highest dose of semaglutide was 0.4 mg per week, which is much lower than the dose used to treat obesity. It reached its primary endpoint with two times the proportion of MASH resolution compared to placebo (40% vs. 17%). It did not promote fibrosis improvement, even though there was a dose-dependent lower probability of worsening fibrosis. Subsequently, other phase 2 study, enrolling 71 patients with MASLD-associated cirrhosis, treated with 2.4 mg per week of semaglutide, controlled with placebo, failed to show an improvement in fibrosis or MASH (101). There was a skew for worse fibrosis (higher percentage of patients with ISHAK grade 6 and higher hepatic collagen proportion), but we might assume that after cirrhosis development semaglutide is no longer effective. A phase 3 trial is ongoing, the ESSENCE trial (NCT04822181), that started, in 2021, recruiting of patients with MASH and stage F2 or F3 fibrosis, treated with semaglutide 2.4 mg per week, controlled with placebo. Histological endpoints will be evaluated at weeks 72 and 240, as well as clinical endpoints such as histological progression into cirrhosis, hepatic decompensation, death or liver transplantation.
The subsequent advance in anti-obesity treatment was the development of dual incretins, such as tirzepatide, a dual GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) agonist, and cotadutide, a dual GLP-1 and glucagon agonist. Tirzepatide adds the beneficial effects of GLP-1 to the enhancement in adipose tissue function mediated by GIP. A set of studies, the SURPASS-1/5, designed to evaluate tirzepatide as a treatment for T2DM, found it could induce impressive weight loss, of around 20% of body weight (102–106). These results were replicated in a phase 3 clinical trial designed to evaluate weight loss in patients without T2DM, the SURMOUNT-1 (84). A substudy of SURPASS-3, a randomized clinical trial in T2DM patients on metformin, which enrolled 296 patients, showed that tirzepatide treatment associated with an almost 50% relative decrease in liver fat content (LFC) assessed by MRI-PDFF that correlated with weight loss and decreases in visceral and abdominal subcutaneous tissue (107). Furthermore, a post-hoc analysis of a phase 2 trial in T2DM patients, also reported an association between treatment with tirzepatide for 26 weeks and a decrease in NIT of hepatocyte apoptosis (K18 fragments) and fibrosis (propeptide of type III collagen, ProC3) (108). It is currently ongoing a phase 2 study specifically in MASH patients, with histological endpoints, the SYNERGY NASH study (NCT0416673).
Several dual GLP-1 and glucagon agonists are in evaluation with potential benefits in MASH: cotadutide, efinopegdutide, and pemvidutide. The glucagon activity adds potential value since it promotes hepatic lipolysis and fat mobilization, as well as increases energy expenditure. However, it has the potential to increase glucose and insulin levels (109). Cotadutide is a peptide with the glucagon sequence modified at some amino-acids and with the addition of a palmitic fatty acid side chain that prolongs its activity. Those modifications resulted in a dual GLP-1 receptor and glucagon receptor agonist activity, which is 2-fold more potent for GLP-1 receptor (110). Cotadutide showed to promote similar weight loss as liraglutide, and lower than semaglutide, but it seems better than liraglutide in promoting a decrease of liver fibrosis when assessed by non-invasive scores and ProC3, in overweight/obese T2DM patients (111, 112). Cotadutide treatment also resulted in an improvement in lipid profile, decreasing LDL-cholesterol and triglycerides (111). Efinopegdutide is a synthetic peptide of oxyntomodulin (a peptide product of the proglucagon gene produced in the small bowel in response to food ingestion) conjugated to the constant region of human IgG4, which results in a longer half-life. It has dual GLP-1 and glucagon agonistic properties, with a relative potency of 2:1 (113). It achieved a weight loss of around 10% in 6 months at a dose of 10 mg per week, performing better than liraglutide and semaglutide regarding weight loss and improvement in lipid profile (109, 113, 114). However, efinopegdutide was less tolerated than liraglutide, and it did not improve glycated hemoglobin, increasing glucose and insulin levels (109, 114). A phase 2a study in 145 patients with MASLD showed efinopegdutide treatment to induce an astonishing relative decrease of LFC by MRI-PDFF, on average higher than 70%, which was superior to the one achieved by semaglutide even at the same weight loss (113). Pemvidutide is a peptide with a balanced GLP-1 and glucagon agonist activity, conjugated with a glycolipid surfactant that prolongs its half-life, allowing weekly administrations (115). After enthusiastic results in preclinical mouse models of MASH, as compared with semaglutide and elafibranor (115), pemvidutide was recently evaluated in a phase 1b study in patients with NAFLD, showing again impressive improvement in LFC of around 75% at 6 months, as well as of liver volume (116). A phase 2b study, the IMPACT NASH trial (NCT05989711), is ongoing, in 190 NASH patients, with histological endpoints, which is expected to be presented in 2025.
More recently, a triple hormone agonist approach allowed a step forward in weight loss therapy. Retatrutide is a triple GLP-1, GIP, and glucagon agonist, which showed a dose-dependent weight loss (117), achieving weight loss of around 25% of body weight at a 12 mg dose per week during 48 weeks (118). A subgroup analysis in patients with MASLD showed an average of over 80% decrease of liver fat content, with all patients decreasing at least 30% and around 90% achieving MASLD resolution, at 8 mg or 12 mg dose (119).
In conclusion, there has been a paradigm shift in the pharmacological treatment of obesity, in the post-incretin era, which might dethrone bariatric surgery in the near future.
3 Drugs approved for other indications that may have an impact in MASLD
Current guidelines consider two drugs on the market that are approved for other conditions: vitamin E and pioglitazone, under specific circumstances (12).
Vitamin E was studied for MASH in the PIVENS trial. The PIVENS trial randomized 247 non-diabetic patients with non-cirrhotic MASH to either vitamin E 800 IU per day, pioglitazone 30 mg per day, or placebo, during 96 weeks (120). The results fell short since there was no improvement in liver fibrosis. However, there was an improvement in steatohepatitis and hepatocyte stress/ballooning, independent of weight loss. Those results placed vitamin E as an attractive drug, in an era when there are no approved drugs for MASLD, in patients with steatohepatitis who could not achieve weight loss. However, vitamin E treatment for MASH was never consensual, since the benefit was weak and there are some concerns regarding safety such as a possible increase in mortality for doses higher than 400 IU per day, which was not confirmed in prospective studies (121). There remains conflicting evidence for prostate cancer (122) and for a possible increased risk for hemorrhagic stroke (123). Indeed, there is limited evidence from some observational studies and 2 out of 4 randomized controlled trials suggesting a mild increase in the risk for hemorrhagic stroke and a possible decreased risk in ischemic stroke (121), which was attributed to its antiplatelet actions (124). Subsequently, 3 meta-analyses of smaller studies on vitamin E, suggest not only a benefit in steatosis and inflammation, as well as in liver fibrosis (125–127), particularly for doses higher than 500 IU per day, for longer than 20 months (127). Lastly, a retrospective study that evaluated 180 patients with MASH and advanced fibrosis (F3 or F4) treated with vitamin E 800 IU/day for longer than 2 years, as compared with 90 propensity-matched controls, showed vitamin E to be associated with an increased transplant-free survival (90% vs. 78% at 10 years, with a number needed to treat, NNT, of just 4.28) and decreased rates of hepatic decompensation (37% vs. 62% at 10 years, with a NNT 6.43) (128).
Pioglitazone was also studied in the PIVENS study, at a dose of 30 mg/day, and, similarly to vitamin E, failed to demonstrate improvement in liver fibrosis, even though it did improve steatohepatitis (120). Subsequently, smaller studies and a meta-analysis did show an improvement in liver fibrosis, but only in patients with T2DM (129–131). There are also some safety concerns, such as weight gain, water retention, increased risk for osteoporosis (132), and bladder cancer (133). Of note, pioglitazone does not induce heart failure, on the contrary, it even seems to improve cardiac function and reduce cardiovascular major events (134–136). However, it does increase the rate of hospitalization in patients with heart failure by promoting water retention (137). Finally, regarding the risk of bladder cancer, the NNT to potentially cause an additional case of bladder cancer is 899 to 6,380 (138), which is in convincing contrast to the NNT of 2–12 to reverse a case of MASH (139). PXL065 is a promising deuterium-stabilized R-pioglitazone stereoisomer that retains the effects of pioglitazone in glucose metabolism and in the liver, but has minimal PPAR-γ activity and hence does not promote weight gain or water retention, unlike the S-stereoisomer of pioglitazone (140). Recently, a phase 2 placebo-controlled study, the DESTINY-1, evaluated increasing doses of PXL065 in 117 patients with fibrotic (F1 to F3) MASH. It showed promising results with a dose–response increased probability of improvement in at least one stage in fibrosis, which was associated with an improvement in glucose control and adipocyte function (expressed as an increase in adiponectin), without an increase in body weight or peripheral edema (141).
Another class of anti-diabetics, sodium-glucose cotransporter-2 inhibitors (SGLT-2i) may also be of benefit, even though studies with strong endpoints including liver biopsy are lacking. Treatment with SGLT-2i drugs, such as empagliflozin, seems to induce mild weight loss, as well as important reductions in liver fat content (over 20% relative decrease) and might decrease the risk of fibrosis progression according to small studies with NIT’s assessment of liver fibrosis (142, 143). Importantly, SGLT-2i have important cardiorenal protective effects, being associated with overall and cardiovascular mortality (144–147).
4 New drugs in development
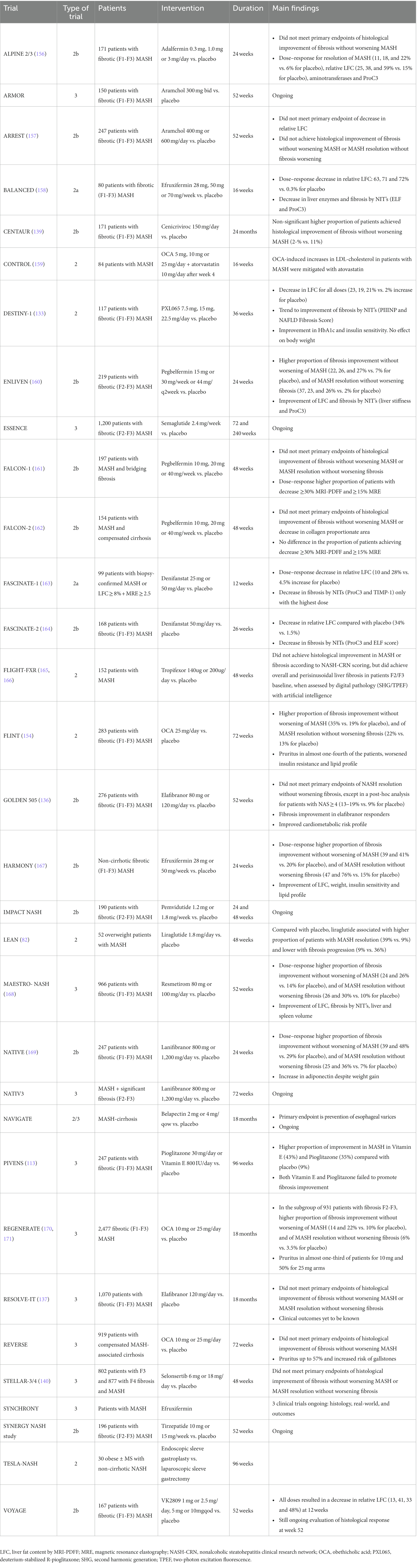
Intense research is ongoing in the quest to find drugs that reach the requisites for FDA approval for MASLD. The landscape of clinical trials is wide, and drugs must demonstrate growing robustness when moving toward phase 3 studies. After safety phase 1 studies, phase 2a studies rely on non-invasive endpoints after 24 weeks, phase 2b on histological endpoints in 6 to 24 months, and phase 3 on clinical outcomes after up to 5 years. For FDA approval, a drug must demonstrate hard clinical endpoints such as progression into cirrhosis and hepatic decompensation (148). However, FDA might give conditional approval if, in phase 2 studies, the drug is able to resolve MASH without fibrosis worsening or improve fibrosis without MASH worsening (149). Up to today, no drug has been approved by the FDA.
Several new drugs have failed the requirements when already in phase 2 or 3 studies, which acted in different mechanisms: the metabolism-modulator elafibranor (PPAR-α/δ agonist) (150, 151), the anti-inflammatory cenicriviroc (CCR-2/5 agonist) (152, 153), the apoptosis inhibitor selonsertib (ASK-1 inhibitor) (154), and the anti-fibrotic simtuzumab (antibody against LOXL-2) (155). The most recent drug to be discontinued, even after a positive phase 3 trial, is obeticholic acid (OCA).
Five drugs have now reached phase III trials: OCA, semaglutide, lanifibranor (a pan-PPAR agonist), resmetirom (a thyroid hormone receptor-β, THR-β, agonist), and efruxifermin (a FGF-21 agonist) (Tables 1, 2).
4.1 Obeticholic acid (OCA) and FXR agonists
OCA is a semi-synthetic 6α-ethyl derivative of the bile acid chenodeoxycholic acid, a first-in-class farsenoid-X receptor (FXR) agonist (159). FXR is a nuclear receptor highly expressed in the liver, but also in the small bowel, which is activated by bile acids. It has pleotrophic actions, modulating bile acids, cholesterol, and glucose metabolism, as well as lipogenesis (176). It also modulates vascular remodeling, inflammation (170, 171), fibrogenesis (177), and the intestinal barrier integrity (178, 179). FXR activation upregulates fibroblast growth factor-19 (FGF-19) and FGF-21, which also have direct anti-steatogenic and anti-fibrotic properties (180).
Preclinical studies in animal models of MASH suggested that OCA could be an effective treatment for improving steatohepatitis and fibrosis (165, 166, 181). After a proof-of-concept study in 64 T2DM patients with MASLD treated with OCA controlled with placebo showing a decrease in liver enzymes (182), a phase 2b trial, the FLINT trial, in 283 patients, brought huge enthusiasm towards OCA, because it was the first time a drug demonstrated an improvement in liver fibrosis in non-cirrhotic MASH (183). The study was even terminated earlier, with 64 patients not performing the programmed liver biopsy, because it reached the primary endpoint of improvement of at least 2 points in NAS score without worsening fibrosis. The study raised some concerns, however, since it induced pruritus in almost one-fourth of the patients, worsened insulin resistance and lipid profile with an increase in total and LDL-cholesterol, and a decrease in HDL-cholesterol (184). Having said that, the CONTROL study showed that the detrimental effect on the lipid profile could be prevented with concomitant treatment with atorvastatin (185). Importantly, studies in compensated cholestatic cirrhosis suggested that treatment with OCA increases almost 4-fold the risk of hepatic decompensation (186).
A phase 3 trial, with 2,477 patients enrolled, the REGENERATE, in pre-cirrhotic MASH, treated with OCA 10 or 25 mg, controlled with placebo, confirmed the positive results in 2 interim analyses at 18 months, the first analysis after histological evaluation by a single-pathologist (169) and the second one by a consensus panel of 3 pathologists (172). The analysis of 931 patients with fibrosis F2 or F3 showed a higher percentage of patients achieving fibrosis improvement (22% versus 10%), and MASH resolution (6.5% versus 3.5%) when treated with 25 mg of OCA compared to placebo (172). Liver stiffness and NITs for fibrosis decreased regardless of histologic response (187). Of note, pruritus occurred in one-third of the patients with the lowest dose and around half with the highest one. Dyslipidemia was very frequent in almost half the patients, and there was a slight increase in gallstone-related events. There were no differences between OCA and placebo in cardiovascular events (172).
A cost-effectiveness study suggested that treatment with OCA would only be cost-effective if the price of the drug would decrease by 78% (188).
A press release from September 2022 by Intercept Pharmaceuticals reported the results of the REVERSE study, a phase 3 study of OCA in compensated cirrhosis, which failed to improve fibrosis by histology, even though it had a positive impact on liver stiffness.
Two applications for FDA accelerated approval, after the first interim analysis in 2020 and, more recently, after the second in 2023, were denied on the basis of promising yet inconclusive benefits with safety concerns regarding pruritus, lipid profile, gallstone complications and rare drug-induced liver injury (DILI) in patients with advanced fibrosis or cirrhosis (189). In consequence, the company abandoned OCA as a treatment for MASLD.
Different non-bile acids FXR agonists either steroidal such as EDP-395 (190) and non-steroidal such as cilofexor (191) and tropifexor (192, 193) have been evaluated for MASH treatment, but results were not convincing, either alone or in combination with other drugs (194–196).
4.2 Lanifibranor and other PPAR agonists
PPARs are nuclear receptors that act as lipid sensors, being naturally activated by fatty acids or derivatives. PPARs are pleiotropic with multiple metabolic and immunomodulatory effects. There are different types of PPAR. PPAR-α is highly expressed in the liver, and its main action is the regulation of fatty acid oxidation. An example of PPAR-α agonists is fibrates, which are used to treat hypertriglyceridemia. PPAR-γ is highly expressed in the adipose tissue being crucial for adipocyte differentiation, and promotes whole-body glucose tolerance by promoting repression of adipocyte lipolysis by insulin. An example of PPAR-γ is thiazolidinedione used to treat T2DM. PPAR-δ is highly expressed in the liver and the muscle, where it modulates glucose metabolism towards a less glycolytic and more oxidative profile, improving lipid and glucose metabolism (197).
Lanifibranor is a pan-PPAR agonist that showed, in multiple preclinical models of MASH, to improve liver histology including fibrosis, as well as promote weight loss, and better glucose and lipid profile (198). A phase 2b study, the NATIVE, in 247 patients with non-cirrhotic MASH, showed promising results, with a higher percentage of patients with MASH resolution without worsening fibrosis (9% for placebo vs. 25% for 800 mg/day vs. 35% for 1,200 mg after 24 weeks) and with fibrosis improvement without worsening MASH (29% vs. 39% vs. 48%). It was well tolerated, with an increase in adiponectin despite weight gain, and an improvement in lipid profile (173). A phase 3 study (NCT04849728), NATIV3, is currently ongoing, which evaluates a 72-week treatment with lanifibranor 800 mg/day or 1,200 mg/day, controlled for placebo in non-cirrhotic patients with MASH and significant fibrosis (F2 or F3). It is expected to be finished in 2026.
Saroglitazar is a dual PPAR-α/γ agonist that promotes insulin resistance and protects from atherogenic dyslipidemia promoting a decrease in small dense LDL and triglycerides (158, 168, 199). Small phase 2 and observational studies suggest saroglitazar has beneficial effects in steatosis, MASH and fibrosis by NITs (167, 199–201), which places saroglitazar as a promising drug. Phase 2b studies with histological endpoints are ongoing (NCT02704403).
4.3 Resmetiron and other thyroid-mimetics
MASLD is associated with hypothyroidism (161, 162), and particularly relative intrahepatic hypothyroidism (202), through a shift in conversion of T4 to the inactive hormone rT3 as opposed to the active T3, as well as a decrease in the hepatic expression of THR (160, 202).
There are two THR: THR-β which mediates the beneficial effects in lipid metabolism, and THR-α which mediates the adverse effects, including cardiac effects. Resmetirom is a THR-β agonist with specific uptake into the liver (203). Preclinical studies in animal models of MASH showed histological benefits in the liver, and improvement of glucose and lipid metabolism, independent of body weight (204).
A phase 2b study (174) in 125 patients with MASH and LFC at least 10% by MRI-PDFF, treated with resmetirom 80 mg or placebo, during 36 weeks, showed a relative decrease of the LFC of 37% compared to 8% with placebo, which is higher than the anti-steatogenic effects of OCA or lanifibranor. A higher proportion of patients achieved MASH resolution (27% vs. 6%), but there was no difference in fibrosis improvement assessed by histology, even though there was an improvement in NIT such as ELF, Pro-C3, and transient elastography (205). Resmetirom was well tolerated and induced advantageous changes in lipid profile, decreasing LDL-cholesterol, triglycerides, and lipoprotein(a) (174).
Preliminary results of a phase 3 trial were recently presented at the EASL meeting, the MAESTRO-NASH, which evaluated the effect of 52 weeks of treatment with resmetirom 80 mg or 100 mg, compared with placebo, in 966 patients with fibrosing, non-cirrhotic MASH (F1-F3). There were dose–response increased proportions of patients achieving MASH resolution without worsening of fibrosis (10% vs. 26% vs. 30%) and of fibrosis improvement without worsening of NAS score (14% vs. 24% vs. 26%). It was also associated with impressive improvements in steatosis, NIT assessed fibrosis, liver and spleen volume (206).
Three other phase 3 studies are currently ongoing: MAESTRO-NAFLD-1 and its open-label extension MAESTRO-NAFLD-OLE, and MAESTRO-NASH-outcomes in cirrhotic patients.
VK2809 is another THRβ liver-specific agonist, which showed in phase 2a and 2b in fibrotic MASH, the VOYAGE study, reductions in LFC after 12 weeks. We are still waiting for the histologic results after 52 weeks.
4.4 Efruxifermin and other FGF-21 agonists
FGF-21 orchestrates energy metabolism, promoting fatty acid oxidation in the liver, insulin sensitivity in peripheral tissues, and acting in the brain decreasing sweet and alcohol preference. Furthermore, even though it is a non-mitogenic hormone, it promotes tissue repair, blunting oxidative stress, inflammation, and fibrogenesis (207).
Efruxifermin is a fusion protein of the human IgG1 Fc domain linked to modified human FGF-21, with a long half-life allowing weekly administration. A phase 2a trial, the BALANCED trial, in 80 patients with non-cirrhotic, fibrotic (F1-F3) MASH, evaluated the effect of 16 weeks of treatment with ascending doses of efruxifermin, controlled with placebo (208). Treatment resulted in a dose–response decrease in relative LFC, over 70% for the highest doses. It also resulted in a decrease in NIT of liver fibrosis ProC3 and ELF score (208). A second phase 2a study in 30 patients with compensated MASH-associated cirrhosis also showed it to be safe, and to result in improvement of glucose metabolism (lowering glycated hemoglobin) and NIT of fibrosis (ELF, FAST score, and ProC3) (209). Of note, treatment with efruxifermin was associated with the development of anti-drug antibodies in 72% of the patients, though its clinical implications are yet to be known (208).
A phase 2b study, the HARMONY, enrolled 128 patients with non-cirrhotic, fibrotic (F1-F3) MASH patients treated with 28 mg or 50 mg of efruxifermin per week or placebo, for 96 weeks. Treatment resulted in a dose–response increase in the proportion of patients achieving fibrosis improvement without worsening of MASH (39 and 41% vs. 20% for placebo), and MASH resolution without worsening of fibrosis (47 and 76% vs. 15% for placebo) (175).
A phase 3 program consisting of 3 trials, SYNCHRONY Histology, SYNCRONY Real-World, and SYNCHRONY Outcomes is currently undergoing to evaluate safety and efficacy of efruxifermin in patients with MASH, including long-term clinical outcomes, according to Akero Therapeutics press release, November 13, 2023.
Two other FGF-21 agonists are under investigation: pegbelfermin and pegozafermin. Both are pegylated FGF-21 agonists. Regarding pegbelfermin, after a small phase 2a study in patients with T2DM and obesity showing a relative decrease of MRI-PDFF up to 56% after 12 weeks of treatment (156), two phase 2b studies, the FALCON-1 and -2 in patients with MASH and advanced fibrosis (F3) or compensated cirrhosis, respectively, confirmed efficacy in decreasing LFC and NIT of fibrosis but did not achieve histological fibrosis improvement (163, 210). Pegozafermin was first evaluated in a 12-week phase 1/2 study in patients with phenotypic MASH diagnosed by transient elastography of ≥7 kPa associated with central obesity and either T2DM or elevated aminotransferases, which resulted in decreased liver enzymes and MRI-PDFF (164). A phase 3b study, the ENLIVEN trial, in 219 patients with MASH and significant fibrosis (F2-F3), compared placebo with different doses of pegozafermin (211). Pegozafermin treatment resulted in a higher proportion of patients achieving the primary endpoints fibrosis improvement without worsening MASH and MASH resolution without fibrosis worsening. It is also associated with a decrease of MRI-PDFF up to 50% (lower than the one achieved with efruxifermin) and improvement in lipid profile (157).
4.5 Other strategies in development
FGF-19 is a gut hormone induced by FXR activation, which has beneficial effects in bile acids, carbohydrates, and energy homeostasis, being downregulated in patients with MASH (212). It has, however, a potential carcinogenic effect (213), promoting hepatocellular carcinoma and associating with worse prognosis (214). Adalfermin is an engineered FGF-19 analog that lacks tumorigenic potential due to a 5 amino-acids deletion in the amino-terminus (215) that results in the inability to activate STAT-3 (216). It showed beneficial histological effects in animal models of MASH (217). Phase 2a studies suggested that adelfermin could improve LFC and fibrosis by NITs and histology (218–220). A phase 2b study, ALPINE 2/3, in 171 patients with fibrotic (F1-F3) MASH, treated with increasing doses of adelfermin for 24 weeks, controlled for placebo, did not achieve its primary endpoint of fibrosis improvement without worsening of MASH, even though it did show a dose–response for resolution of MASH without worsening of fibrosis (221).
Strategies that act directly on lipid metabolism are ongoing. Different enzymes in lipogenesis have been targeted: acetyl-CoA carboxylase inhibitor firsocostat, fatty acid synthase inhibitor denifanstat, DGAT2 inhibitors, and stearoyl CoA-desaturase-1 inhibitor aramchol. All of them consistently showed improvements in LFC, in small trials (195, 222–225). Aramchol was evaluated in a phase 2b study, ARREST, in patients with MASH, which failed to achieve histological benefit in MASH or fibrosis (226). A phase 3 trial, ARMOR study (NCT04104321), is currently ongoing.
Anti-fibrotic strategies are still ongoing, even after the major failure of simtuzumab, a monoclonal antibody that binds to LOXL2 (an enzyme responsible for elastin and collagen crosslinking), and acts as an immunomodulator (155). Belapectin, a galectin-3 inhibitor, was evaluated in a phase 2b study in patients with MASH-associated cirrhosis with portal hypertension and found that in patients with esophageal varices, 52 weeks of treatment associated with a decrease in portal pressure and a decreased risk of new varices development (227). A phase 2/3 trial, the NAVIGATE (NCT0436868), for the prevention of esophageal varices in MASH-cirrhosis is ongoing.
Lastly, the field is also moving toward directed therapies with oligonucleotide-based therapies that target genes with variants initially identified in genome-wide association studies, to be associated with risk for MASH. For example, patients with PNPLA3 148 M variant, which has detrimental effects on lipid remodeling in hepatocytes, can be targeted for PNPLA3 therapeutic oligonucleotide inhibition, which is already ongoing. A similar approach could be offered for patients who do not present the protective loss-of-function variant on HSD17B13 (i.e., insertion of adenine in a donor splice site in exon 6) (228).
5 Conclusion
MASLD, the liver manifestation of adiposopathy, is a condition that is associated with increased all-cause mortality, but only a minority of patients will progress to end-stage liver disease. As such, adiposopathy and lifestyle exercise-promoting interventions should be offered to all patients.
Weight loss is the most efficient strategy, and all tools must be considered, such as lifestyle intervention, bariatric surgery and endoscopy, and most recently, the growing panoply of highly efficient anti-obesity drugs.
Intense research is being performed to find a drug that acts specifically in liver disease, for those patients with fibrotic MASH that are at-risk of progressive liver disease. The pathway for MASH-effective drug discovery is not easy, but 3 strong candidates are already in advanced research, namely resmetirom, lanifibranor, and efruximin.
The near future holds for a shift in the paradigm of MASH treatment, possibly with combination and precision therapy targeting particular deranged pathways for each patient.
Author contributions
MVM: Conceptualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Younossi, ZM, Golabi, P, Paik, JM, Henry, A, Van Dongen, C, and Henry, L. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): a systematic review. Hepatology. (2023) 77:1335–47. doi: 10.1097/HEP.0000000000000004
2. Ciardullo, S, Carbone, M, Invernizzi, P, and Perseghin, G. Exploring the landscape of steatotic liver disease in the general US population. Liver Int. (2023) 43:2425–33. doi: 10.1111/liv.15695
3. Le, MH, Le, DM, Baez, TC, Wu, Y, Ito, T, Lee, EY, et al. Global incidence of non-alcoholic fatty liver disease: A systematic review and meta-analysis of 63 studies and 1,201,807 persons. J Hepatol. (2023) 79:287–95. doi: 10.1016/j.jhep.2023.03.040
4. Paik, JM, Golabi, P, Younossi, Y, Srishord, M, Mishra, A, and Younossi, ZM. The growing burden of disability related to nonalcoholic fatty liver disease: data from the global burden of disease 2007-2017. Hepatol Commun. (2020) 4:1769–80. doi: 10.1002/hep4.1599
5. Younossi, ZM, Stepanova, M, Ong, J, Trimble, G, AlQahtani, S, Younossi, I, et al. Nonalcoholic steatohepatitis is the Most rapidly increasing indication for liver transplantation in the United States. Clin Gastroenterol Hepatol. (2021) 19:580–589.e5. doi: 10.1016/j.cgh.2020.05.064
6. Machado, MV, and Diehl, AM. Pathogenesis of nonalcoholic steatohepatitis. Gastroenterology. (2016) 150:1769–77. doi: 10.1053/j.gastro.2016.02.066
7. Younossi, ZM, Stepanova, M, Younossi, Y, Golabi, P, Mishra, A, Rafiq, N, et al. Epidemiology of chronic liver diseases in the USA in the past three decades. Gut. (2020) 69:564–8. doi: 10.1136/gutjnl-2019-318813
8. Allen, AM, Therneau, TM, Ahmed, OT, Gidener, T, Mara, KC, Larson, JJ, et al. Clinical course of non-alcoholic fatty liver disease and the implications for clinical trial design. J Hepatol. (2022) 77:1237–45. doi: 10.1016/j.jhep.2022.07.004
9. Simon, TG, Roelstraete, B, Khalili, H, Hagström, H, and Ludvigsson, JF. Mortality in biopsy-confirmed nonalcoholic fatty liver disease: results from a nationwide cohort. Gut. (2021) 70:1375–82. doi: 10.1136/gutjnl-2020-322786
10. Ng, CH, Lim, WH, Lim, GEH, Tan, DJH, Syn, N, Muthiah, MD, et al. Mortality outcomes by fibrosis stage in nonalcoholic fatty liver disease: A systematic review and Meta-analysis. Clin Gastroenterol Hepatol. (2023) 21:931–939.e5. doi: 10.1016/j.cgh.2022.04.014
11. Allen, AM, Hicks, SB, Mara, KC, Larson, JJ, and Therneau, TM. The risk of incident extrahepatic cancers is higher in non-alcoholic fatty liver disease than obesity – A longitudinal cohort study. J Hepatol. (2019) 71:1229–36. doi: 10.1016/j.jhep.2019.08.018
12. Rinella, ME, Neuschwander-Tetri, BA, Siddiqui, MS, Abdelmalek, MF, Caldwell, S, Barb, D, et al. AASLD practice guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology. (2023) 77:1797–835. doi: 10.1097/HEP.0000000000000323
13. Machado, MV, Marques Vidal, P, and Cortez, PH. Hepatic histology in obese patients undergoing bariatric surgery. J Hepatol. (2006) 45:600–6. doi: 10.1016/j.jhep.2006.06.013
14. Machado, MV, Policarpo, S, Coutinho, J, Carvalhana, S, Leitão, J, Carvalho, A, et al. What is the role of the new index relative fat mass (RFM) in the assessment of nonalcoholic fatty liver disease (NAFLD)? Obes Surg. (2020) 30:560–8. doi: 10.1007/s11695-019-04213-8
15. Machado, MV. Nonalcoholic fatty liver disease in lean subjects: is it all metabolic-associated fatty liver disease? Hepatoma Res. (2020) 2020:84. doi: 10.20517/2394-5079.2020.90
16. Romero Gómez, M, Zelber Sagi, S, and Trenell, M. Treatment of NAFLD with diet, physical activity and exercise. J Hepatol. (2017) 67:829–46. doi: 10.1016/j.jhep.2017.05.016
17. Berzigotti, A, Albillos, A, Villanueva, C, Genescá, J, Ardevol, A, Augustín, S, et al. Effects of an intensive lifestyle intervention program on portal hypertension in patients with cirrhosis and obesity: the SportDiet study. Hepatology. (2017) 65:1293–305. doi: 10.1002/hep.28992
18. Vilar‐Gomez, E, Nephew, LD, Vuppalanchi, R, Gawrieh, S, Mladenovic, A, Pike, F, et al. High-quality diet, physical activity, and college education are associated with low risk of NAFLD among the US population. Hepatology. (2022) 75:1491–506. doi: 10.1002/hep.32207
19. Vilar-Gomez, E, Vuppalanchi, R, Gawrieh, S, Pike, F, Samala, N, and Chalasani, N. Significant dose-response Association of Physical Activity and Diet Quality with Mortality in adults with suspected NAFLD in a population study. Am J Gastroenterol. (2023) 118:1576–91. doi: 10.14309/ajg.0000000000002222
20. Machado, MV. What should we advise MAFLD patients to eat and drink? Metab Target Organ Damage. (2021) 1:9. doi: 10.20517/mtod.2021.11
21. Jensen, T, Abdelmalek, MF, Sullivan, S, Nadeau, KJ, Green, M, Roncal, C, et al. Fructose and sugar: A major mediator of non-alcoholic fatty liver disease. J Hepatol. (2018) 68:1063–75. doi: 10.1016/j.jhep.2018.01.019
22. Bjermo, H, Iggman, D, Kullberg, J, Dahlman, I, Johansson, L, Persson, L, et al. Effects of n-6 PUFAs compared with SFAs on liver fat, lipoproteins, and inflammation in abdominal obesity: a randomized controlled trial. Am J Clin Nutr. (2012) 95:1003–12. doi: 10.3945/ajcn.111.030114
23. Zhao, L, Deng, C, Lin, Z, Giovannucci, E, and Zhang, X. Dietary fats, serum cholesterol and liver Cancer risk: A systematic review and Meta-analysis of prospective studies. Cancers. (2021) 13:1580. doi: 10.3390/cancers13071580
24. Sawada, N, Inoue, M, Iwasaki, M, Sasazuki, S, Shimazu, T, Yamaji, T, et al. Consumption of n-3 fatty acids and fish reduces risk of hepatocellular carcinoma. Gastroenterology. (2012) 142:1468–75. doi: 10.1053/j.gastro.2012.02.018
25. Zelber-Sagi, S, Ivancovsky-Wajcman, D, Isakov, NF, Webb, M, Orenstein, D, Shibolet, O, et al. High red and processed meat consumption is associated with non-alcoholic fatty liver disease and insulin resistance. J Hepatol. (2018) 68:1239–46. doi: 10.1016/j.jhep.2018.01.015
26. Davis, C, Bryan, J, Hodgson, J, and Murphy, K. Definition of the Mediterranean diet; a literature review. Nutrition. (2015) 7:9139–53. doi: 10.3390/nu7115459
27. Haigh, L, Kirk, C, El Gendy, K, Gallacher, J, Errington, L, Mathers, JC, et al. The effectiveness and acceptability of Mediterranean diet and calorie restriction in non-alcoholic fatty liver disease (NAFLD): A systematic review and meta-analysis. Clin Nutr. (2022) 41:1913–31. doi: 10.1016/j.clnu.2022.06.037
28. Kawaguchi, T, Charlton, M, Kawaguchi, A, Yamamura, S, Nakano, D, Tsutsumi, T, et al. Effects of Mediterranean diet in patients with NAFLD: A systematic review, Meta-analysis, and Meta-regression analysis of randomized controlled trials. Semin Liver Dis. (2021) 41:225–34. doi: 10.1055/s-0041-1723751
29. Kouvari, M, Boutari, C, Chrysohoou, C, Fragkopoulou, E, Antonopoulou, S, Tousoulis, D, et al. Mediterranean diet is inversely associated with steatosis and fibrosis and decreases ten-year diabetes and cardiovascular risk in NAFLD subjects: results from the ATTICA prospective cohort study. Clin Nutr. (2021) 40:3314–24. doi: 10.1016/j.clnu.2020.10.058
30. Becerra-Tomás, N, Blanco Mejía, S, Viguiliouk, E, Khan, T, Kendall, CW, Kahleova, H, et al. Mediterranean diet, cardiovascular disease and mortality in diabetes: A systematic review and meta-analysis of prospective cohort studies and randomized clinical trials. Crit Rev Food Sci Nutr. (2020) 60:1207–27. doi: 10.1080/10408398.2019.1565281
31. Morze, J, Danielewicz, A, Przybyłowicz, K, Zeng, H, Hoffmann, G, Schwingshackl, L, et al. An updated systematic review and meta-analysis on adherence to mediterranean diet and risk of cancer. Eur J Nutr. (2021) 60:1561–86. doi: 10.1007/s00394-020-02346-6
32. Kang, J, Ratamess, NA, Faigenbaum, AD, Bush, JA, Beller, N, Vargas, A, et al. Effect of time-restricted feeding on anthropometric, metabolic, and fitness parameters: A systematic review. J Am Nutr Assoc. (2022) 41:810–25. doi: 10.1080/07315724.2021.1958719
33. Sutton, EF, Beyl, R, Early, KS, Cefalu, WT, Ravussin, E, and Peterson, CM. Early time-restricted feeding improves insulin sensitivity, blood pressure, and oxidative stress even without weight loss in men with prediabetes. Cell Metab. (2018) 27:1212–1221.e3. doi: 10.1016/j.cmet.2018.04.010
34. Lange, M, Nadkarni, D, Martin, L, Newberry, C, Kumar, S, and Kushner, T. Intermittent fasting improves hepatic end points in nonalcoholic fatty liver disease: A systematic review and meta-analysis. Hepatol Commun. (2023) 7:e0212. doi: 10.1097/HC9.0000000000000212
35. Liu, D, Huang, Y, Huang, C, Yang, S, Wei, X, Zhang, P, et al. Calorie restriction with or without time-restricted eating in weight loss. N Engl J Med. (2022) 386:1495–504. doi: 10.1056/NEJMoa2114833
36. Ma, X, Chen, Q, Pu, Y, Guo, M, Jiang, Z, Huang, W, et al. Skipping breakfast is associated with overweight and obesity: A systematic review and meta-analysis. Obes Res Clin Pract. (2020) 14:1–8. doi: 10.1016/j.orcp.2019.12.002
37. Bi, H, Gan, Y, Yang, C, Chen, Y, Tong, X, and Lu, Z. Breakfast skipping and the risk of type 2 diabetes: a meta-analysis of observational studies. Public Health Nutr. (2015) 18:3013–9. doi: 10.1017/S1368980015000257
38. Rong, S, Snetselaar, LG, Xu, G, Sun, Y, Liu, B, Wallace, RB, et al. Association of Skipping Breakfast with Cardiovascular and all-Cause Mortality. J Am Coll Cardiol. (2019) 73:2025–32. doi: 10.1016/j.jacc.2019.01.065
39. Liu, T, Wang, Y, Wang, X, Liu, C, Zhang, Q, Song, M, et al. Habitually skipping breakfast is associated with the risk of gastrointestinal cancers: evidence from the Kailuan cohort study. J Gen Intern Med. (2023) 38:2527–36. doi: 10.1007/s11606-023-08094-7
40. Wijarnpreecha, K, Thongprayoon, C, and Ungprasert, P. Coffee consumption and risk of nonalcoholic fatty liver disease: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. (2017) 29:e8–e12. doi: 10.1097/MEG.0000000000000776
41. Chen, YP, Lu, FB, Hu, YB, Xu, LM, Zheng, MH, and Hu, ED. A systematic review and a dose-response meta-analysis of coffee dose and nonalcoholic fatty liver disease. Clin Nutr. (2019) 38:2552–7. doi: 10.1016/j.clnu.2018.11.030
42. Kennedy, OJ, Roderick, P, Buchanan, R, Fallowfield, JA, Hayes, PC, and Parkes, J. Coffee, including caffeinated and decaffeinated coffee, and the risk of hepatocellular carcinoma: a systematic review and dose-response meta-analysis. BMJ Open. (2017) 7:e013739. doi: 10.1136/bmjopen-2016-013739
43. Xiao, Q, Sinha, R, Graubard, BI, and Freedman, ND. Inverse associations of total and decaffeinated coffee with liver enzyme levels in National Health and nutrition examination survey 1999-2010. Hepatology. (2014) 60:2091–8. doi: 10.1002/hep.27367
44. Åberg, F, Puukka, P, Salomaa, V, Männistö, S, Lundqvist, A, Valsta, L, et al. Risks of light and moderate alcohol use in fatty liver disease: follow-up of population cohorts. Hepatology. (2020) 71:835–48. doi: 10.1002/hep.30864
45. Hajifathalian, K, Sagvand, BT, and McCullough, AJ. Effect of alcohol consumption on survival in nonalcoholic fatty liver disease: A National Prospective Cohort Study. Hepatology. (2019) 70:511–21. doi: 10.1002/hep.30226
46. Åberg, F, Puukka, P, Salomaa, V, Männistö, S, Lundqvist, A, Valsta, L, et al. Combined effects of alcohol and metabolic disorders in patients with chronic liver disease. Clin Gastroenterol Hepatol. (2020) 18:995–997.e2. doi: 10.1016/j.cgh.2019.06.036
47. Díaz, LA, Arab, JP, Louvet, A, Bataller, R, and Arrese, M. The intersection between alcohol-related liver disease and nonalcoholic fatty liver disease. Nat Rev Gastroenterol Hepatol. (2023) 20:764–83. doi: 10.1038/s41575-023-00822-y
48. Åberg, F, Byrne, CD, Pirola, CJ, Männistö, V, and Sookoian, S. Alcohol consumption and metabolic syndrome: clinical and epidemiological impact on liver disease. J Hepatol. (2023) 78:191–206. doi: 10.1016/j.jhep.2022.08.030
49. Jarvis, H, O'Keefe, H, Craig, D, Stow, D, Hanratty, B, and Anstee, QM. Does moderate alcohol consumption accelerate the progression of liver disease in NAFLD? A systematic review and narrative synthesis. BMJ Open. (2022) 12:e049767. doi: 10.1136/bmjopen-2021-049767
50. Louvet, A, Bourcier, V, Archambeaud, I, d’Alteroche, L, Chaffaut, C, Oberti, F, et al. Low alcohol consumption influences outcomes in individuals with alcohol-related compensated cirrhosis in a French multicenter cohort. J Hepatol. (2023) 78:501–12. doi: 10.1016/j.jhep.2022.11.013
51. Ascha, MS, Hanouneh, IA, Lopez, R, Tamimi, TAR, Feldstein, AF, and Zein, NN. The incidence and risk factors of hepatocellular carcinoma in patients with nonalcoholic steatohepatitis. Hepatology. (2010) 51:1972–8. doi: 10.1002/hep.23527
52. Byambasukh, O, Zelle, D, and Corpeleijn, E. Physical activity, fatty liver, and glucose metabolism over the life course: the lifelines cohort. Am J Gastroenterol. (2019) 114:907–15. doi: 10.14309/ajg.0000000000000168
53. Machado, MV. Aerobic exercise in the Management of Metabolic Dysfunction Associated Fatty Liver Disease. Diabetes Metab Syndr Obes. (2021) 14:3627–45. doi: 10.2147/DMSO.S304357
54. Haufe, S, Haas, V, Utz, W, Birkenfeld, AL, Jeran, S, Böhnke, J, et al. Long-lasting improvements in liver fat and metabolism despite body weight regain after dietary weight loss. Diabetes Care. (2013) 36:3786–92. doi: 10.2337/dc13-0102
55. Malespin, MH, Barritt, AS, Watkins, SE, Schoen, C, Tincopa, MA, Corbin, KD, et al. Weight loss and weight regain in usual clinical practice: results from the TARGET-NASH observational cohort. Clin Gastroenterol Hepatol. (2020) 20:2393–5. doi: 10.1016/j.cgh.2021.01.023
56. Cornier, MA. A review of current guidelines for the treatment of obesity. Am J Manag Care. (2022) 28:S288–96. doi: 10.37765/ajmc.2022.89292
57. Mingrone, G, Panunzi, S, De Gaetano, A, Guidone, C, Iaconelli, A, Capristo, E, et al. Metabolic surgery versus conventional medical therapy in patients with type 2 diabetes: 10-year follow-up of an open-label, single-Centre, randomised controlled trial. Lancet. (2021) 397:293–304. doi: 10.1016/S0140-6736(20)32649-0
58. Sjöström, L, Narbro, K, Sjöström, CD, Karason, K, Larsson, B, Wedel, H, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. (2017) 357:741–52. doi: 10.1056/NEJMoa066254
59. Wiggins, T, Guidozzi, N, Welbourn, R, Ahmed, AR, and Markar, SR. Association of bariatric surgery with all-cause mortality and incidence of obesity-related disease at a population level: A systematic review and meta-analysis. PLoS Med. (2020) 17:e1003206. doi: 10.1371/journal.pmed.1003206
60. Syn, NL, Cummings, DE, Wang, LZ, Lin, DJ, Zhao, JJ, Loh, M, et al. Association of metabolic-bariatric surgery with long-term survival in adults with and without diabetes: a one-stage meta-analysis of matched cohort and prospective controlled studies with 174 772 participants. Lancet. (2021) 397:1830–41. doi: 10.1016/S0140-6736(21)00591-2
61. Lassailly, G, Caiazzo, R, Buob, D, Pigeyre, M, Verkindt, H, Labreuche, J, et al. Bariatric surgery reduces features of nonalcoholic steatohepatitis in morbidly obese patients. Gastroenterology. (2015) 149:379–88. doi: 10.1053/j.gastro.2015.04.014
62. Lassailly, G, Caiazzo, R, Ntandja-Wandji, LC, Gnemmi, V, Baud, G, Verkindt, H, et al. Bariatric surgery provides Long-term resolution of NASH and regression of fibrosis. Gastroenterology. (2020) 159:1290–1301.e5. doi: 10.1053/j.gastro.2020.06.006
63. Lee, Y, Doumouras, AG, Yu, J, Brar, K, Banfield, L, Gmora, S, et al. Complete resolution of nonalcoholic fatty liver disease after bariatric surgery: A systematic review and meta-analysis. Clin Gastroenterol Hepatol. (2019) 17:1040–1060.e11. doi: 10.1016/j.cgh.2018.10.017
64. Verrastro, O, Panunzi, S, Castagneto-Gissey, L, De Gaetano, A, Lembo, E, Capristo, E, et al. Bariatric-metabolic surgery versus lifestyle intervention plus best medical care in non-alcoholic steatohepatitis (BRAVES): a multicentre, open-label, randomised trial. Lancet. (2023) 401:1786–97. doi: 10.1016/S0140-6736(23)00634-7
65. Aminian, A, Al-Kurd, A, Wilson, R, Bena, J, Fayazzadeh, H, Singh, T, et al. Association of Bariatric Surgery with Major Adverse Liver and Cardiovascular Outcomes in patients with biopsy-proven nonalcoholic steatohepatitis. JAMA. (2021) 326:2031–42. doi: 10.1001/jama.2021.19569
66. Elsaid, MI, Li, Y, Bridges, JFP, Brock, G, Minacapelli, CD, and Rustgi, VK. Association of Bariatric Surgery with Cardiovascular Outcomes in adults with severe obesity and nonalcoholic fatty liver disease. JAMA Netw Open. (2022) 5:e2235003. doi: 10.1001/jamanetworkopen.2022.35003
67. Yeoh, A, Wong, R, and Singal, AK. The role bariatric surgery and endobariatric therapies in nonalcoholic steatohepatitis. Clin Liver Dis. (2023) 27:413–27. doi: 10.1016/j.cld.2023.01.009
68. Caiazzo, R, Lassailly, G, Leteurtre, E, Baud, G, Verkindt, H, Raverdy, V, et al. Roux-en-Y gastric bypass versus adjustable gastric banding to reduce nonalcoholic fatty liver disease: a 5-year controlled longitudinal study. Ann Surg. (2014) 260:893–9. doi: 10.1097/SLA.0000000000000945
69. Baldwin, D, Chennakesavalu, M, and Gangemi, A. Systematic review and meta-analysis of Roux-en-Y gastric bypass against laparoscopic sleeve gastrectomy for amelioration of NAFLD using four criteria. Surg Obes Relat Dis. (2019) 15:2123–30. doi: 10.1016/j.soard.2019.09.060
70. Pedersen, JS, Rygg, MO, Serizawa, RR, Kristiansen, VB, Albrechtsen, NJW, Gluud, LL, et al. Effects of Roux-en-Y gastric bypass and sleeve gastrectomy on non-alcoholic fatty liver disease: A 12-month follow-up study with paired liver biopsies. J Clin Med. (2021) 10:3783. doi: 10.3390/jcm10173783
71. Seeberg, KA, Borgeraas, H, Hofsø, D, Småstuen, MC, Kvan, NP, Grimnes, JO, et al. Gastric bypass versus sleeve gastrectomy in type 2 diabetes: effects on hepatic steatosis and fibrosis: A randomized controlled trial. Ann Intern Med. (2022) 175:74–83. doi: 10.7326/M21-1962
72. Weingarten, TN, Swain, JM, Kendrick, ML, Charlton, MR, Schroeder, BJ, Lee, REC, et al. Nonalcoholic steatohepatitis (NASH) does not increase complications after laparoscopic bariatric surgery. Obes Surg. (2021) 21:1714–20. doi: 10.1007/s11695-011-0521-z
73. Bai, J, Jia, Z, Chen, Y, Li, Y, Zheng, S, and Duan, Z. Bariatric surgery is effective and safe for obese patients with compensated cirrhosis: a systematic review and meta-analysis. World J Surg. (2022) 46:1122–33. doi: 10.1007/s00268-021-06382-z
74. Heimbach, JK, Watt, KDS, Poterucha, JJ, Ziller, NF, Cecco, SD, Charlton, MR, et al. Combined liver transplantation and gastric sleeve resection for patients with medically complicated obesity and end-stage liver disease. Am J Transplant. (2013) 13:363–8. doi: 10.1111/j.1600-6143.2012.04318.x
75. Zamora Valdes, D, Watt, KD, Kellogg, TA, Poterucha, JJ, Di Cecco, SR, Francisco-Ziller, NM, et al. Long-term outcomes of patients undergoing simultaneous liver transplantation and sleeve gastrectomy. Hepatology. (2018) 68:485–95. doi: 10.1002/hep.29848
76. Tsamalaidze, L, Stauffer, JA, Arasi, LC, Villacreses, DE, Franco, JSS, Bowers, S, et al. Laparoscopic sleeve gastrectomy for morbid obesity in patients after Orthotopic liver transplant: a matched case-control study. Obes Surg. (2018) 28:444–50. doi: 10.1007/s11695-017-2847-7
77. Jirapinyo, P, McCarty, TR, Dolan, RD, Shah, R, and Thompson, CC. Effect of endoscopic bariatric and metabolic therapies on NAFLD: A systematic review and Meta-analysis. Clin Gastroenterol Hepatol. (2022) 20:511–524.e1. doi: 10.1016/j.cgh.2021.03.017
78. El Haddad, A, Rammal, MO, Soweid, A, Sharara, AI, Daniel, F, Rahal, MA, et al. Intragastric balloon treatment of obesity: Long-term results and patient satisfaction. Turk J Gastroenterol. (2019) 30:461–6. doi: 10.5152/tjg.2019.17877
79. Chandan, S, Mohan, BP, Khan, SR, Facciorusso, A, Ramai, D, Kassab, LL, et al. Efficacy and safety of Intragastric balloon (IGB) in NAFLD: a comprehensive review and Meta-analysis. Obes Surg. (2021) 31:1271–9. doi: 10.1007/s11695-020-05084-0
80. Hajifathalian, K, Mehta, A, Ang, B, Skaf, D, Shah, SL, Saumoy, M, et al. Improvement in insulin resistance and estimated hepatic steatosis and fibrosis after endoscopic sleeve gastroplasty. Gastrointest Endosc. (2021) 93:1110–8. doi: 10.1016/j.gie.2020.08.023
81. Lavín-Alconero, L, Fernández-Lanas, T, Iruzubieta-Coz, P, Arias-Loste, MT, Rodriguez-Duque, JC, Rivas, C, et al. Efficacy and safety of endoscopic sleeve gastroplasty versus laparoscopic sleeve gastrectomy in obese subjects with NASH: study protocol for a randomized controlled trial (TESLA-NASH study). Trials. (2021) 22:756. doi: 10.1186/s13063-021-05695-7
82. Gollisch, KSC, Lindhorst, A, and Raddatz, D. EndoBarrier gastrointestinal liner in type 2 diabetic patients improves liver fibrosis as assessed by liver Elastography. Exp Clin Endocrinol Diabetes. (2017) 125:116–21. doi: 10.1055/s-0042-118961
83. Mingrone, G, van Baar, AC, Devière, J, Hopkins, D, Moura, E, Cercato, C, et al. Safety and efficacy of hydrothermal duodenal mucosal resurfacing in patients with type 2 diabetes: the randomised, double-blind, sham-controlled, multicentre REVITA-2 feasibility trial. Gut. (2022) 71:254–64. doi: 10.1136/gutjnl-2020-323608
84. Jastreboff, AM, Aronne, LJ, Ahmad, NN, Wharton, S, Connery, L, Alves, B, et al. Tirzepatide once weekly for the treatment of obesity. N Engl J Med. (2022) 387:205–16. doi: 10.1056/NEJMoa2206038
85. Yabut, JM, and Drucker, DJ. Glucagon-like Peptide-1 receptor-based therapeutics for metabolic liver disease. Endocr Rev. (2023) 44:14–32. doi: 10.1210/endrev/bnac018
86. Davies, MJ, Bergenstal, R, Bode, B, Kushner, RF, Lewin, A, Skjøth, TV, et al. Efficacy of Liraglutide for weight loss among patients with type 2 diabetes: the SCALE diabetes randomized clinical trial. JAMA. (2015) 314:687–99. doi: 10.1001/jama.2015.9676
87. Pi-Sunyer, X, Astrup, A, Fujioka, K, Greenway, F, Halpern, A, Krempf, M, et al. A randomized, controlled trial of 3.0 mg of Liraglutide in weight management. N Engl J Med. (2015) 373:11–22. doi: 10.1056/NEJMoa1411892
88. Armstrong, MJ, Gaunt, P, Aithal, GP, Barton, D, Hull, D, Parker, R, et al. Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet. (2016) 387:679–90. doi: 10.1016/S0140-6736(15)00803-X
89. Iqbal, J, Wu, HX, Hu, N, Zhou, YH, Li, L, Xiao, F, et al. Effect of glucagon-like peptide-1 receptor agonists on body weight in adults with obesity without diabetes mellitus-a systematic review and meta-analysis of randomized control trials. Obes Rev. (2022) 23:e13435. doi: 10.1111/obr.13435
90. Xie, Z, Yang, S, Deng, W, Li, J, and Chen, J. Efficacy and safety of Liraglutide and Semaglutide on weight loss in people with obesity or overweight: a systematic review. Clin Epidemiol. (2022) 14:1463–76. doi: 10.2147/CLEP.S391819
91. Wilding, JPH, Batterham, RL, Calanna, S, Davies, M, van Gaal, LF, Lingvay, I, et al. Once-weekly Semaglutide in adults with overweight or obesity. N Engl J Med. (2021) 384:989–1002. doi: 10.1056/NEJMoa2032183
92. Davies, M, Færch, L, Jeppesen, OK, Pakseresht, A, Pedersen, SD, Perreault, L, et al. Semaglutide 2·4 mg once a week in adults with overweight or obesity, and type 2 diabetes (STEP 2): a randomised, double-blind, double-dummy, placebo-controlled, phase 3 trial. Lancet. (2021) 397:971–84. doi: 10.1016/S0140-6736(21)00213-0
93. Rubino, D, Abrahamsson, N, Davies, M, Hesse, D, Greenway, FL, Jensen, C, et al. Effect of continued weekly subcutaneous semaglutide vs placebo on weight loss maintenance in adults with overweight or obesity: the STEP 4 randomized clinical trial. JAMA. (2021) 325:1414–25. doi: 10.1001/jama.2021.3224
94. Wharton, S, Batterham, RL, Bhatta, M, Buscemi, S, Christensen, LN, Frias, JP, et al. Two-year effect of semaglutide 2.4 mg on control of eating in adults with overweight/obesity: STEP 5. Obesity. (2023) 31:703–15. doi: 10.1002/oby.23673
95. Kadowaki, T, Isendahl, J, Khalid, U, Lee, SY, Nishida, T, Ogawa, W, et al. Semaglutide once a week in adults with overweight or obesity, with or without type 2 diabetes in an east Asian population (STEP 6): a randomised, double-blind, double-dummy, placebo-controlled, phase 3a trial. Lancet Diabetes Endocrinol. (2022) 10:193–206. doi: 10.1016/S2213-8587(22)00008-0
96. Kosiborod, MN, Bhatta, M, Davies, M, Deanfield, JE, Garvey, WT, Khalid, U, et al. Semaglutide improves cardiometabolic risk factors in adults with overweight or obesity: STEP 1 and 4 exploratory analyses. Diabetes Obes Metab. (2023) 25:468–78. doi: 10.1111/dom.14890
97. Husain, M, Bain, SC, Jeppesen, OK, Lingvay, I, Sørrig, R, Treppendahl, MB, et al. Semaglutide (SUSTAIN and PIONEER) reduces cardiovascular events in type 2 diabetes across varying cardiovascular risk. Diabetes Obes Metab. (2020) 22:442–51. doi: 10.1111/dom.13955
98. Marso, SP, Bain, SC, Consoli, A, Eliaschewitz, FG, Jódar, E, Leiter, LA, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. (2016) 375:1834–44. doi: 10.1056/NEJMoa1607141
99. Kristensen, SL, Rørth, R, Jhund, PS, Docherty, KF, Sattar, N, Preiss, D, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet Diabetes Endocrinol. (2019) 7:776–85. doi: 10.1016/S2213-8587(19)30249-9
100. Newsome, PN, Buchholtz, K, Cusi, K, Linder, M, Okanoue, T, Ratziu, V, et al. A placebo-controlled trial of subcutaneous Semaglutide in nonalcoholic steatohepatitis. N Engl J Med. (2021) 384:1113–24. doi: 10.1056/NEJMoa2028395
101. Loomba, R, Abdelmalek, MF, Armstrong, MJ, Jara, M, Kjær, MS, Krarup, N, et al. Semaglutide 2·4 mg once weekly in patients with non-alcoholic steatohepatitis-related cirrhosis: a randomised, placebo-controlled phase 2 trial. Lancet Gastroenterol Hepatol. (2023) 8:511–22. doi: 10.1016/S2468-1253(23)00068-7
102. Rosenstock, J, Wysham, C, Frías, JP, Kaneko, S, Lee, CJ, Fernández Landó, L, et al. Efficacy and safety of a novel dual GIP and GLP-1 receptor agonist tirzepatide in patients with type 2 diabetes (SURPASS-1): a double-blind, randomised, phase 3 trial. Lancet. (2021) 398:143–55. doi: 10.1016/S0140-6736(21)01324-6
103. Frías, JP, Davies, MJ, Rosenstock, J, Pérez Manghi, FC, Fernández Landó, L, Bergman, BK, et al. Tirzepatide versus Semaglutide once weekly in patients with type 2 diabetes. N Engl J Med. (2021) 385:503–15. doi: 10.1056/NEJMoa2107519
104. Ludvik, B, Giorgino, F, Jódar, E, Frias, JP, Fernández Landó, L, Brown, K, et al. Once-weekly tirzepatide versus once-daily insulin degludec as add-on to metformin with or without SGLT2 inhibitors in patients with type 2 diabetes (SURPASS-3): a randomised, open-label, parallel-group, phase 3 trial. Lancet. (2021) 398:583–98. doi: 10.1016/S0140-6736(21)01443-4
105. Del Prato, S, Kahn, SE, Pavo, I, Weerakkody, GJ, Yang, Z, Doupis, J, et al. Tirzepatide versus insulin glargine in type 2 diabetes and increased cardiovascular risk (SURPASS-4): a randomised, open-label, parallel-group, multicentre, phase 3 trial. Lancet. (2021) 398:1811–24. doi: 10.1016/S0140-6736(21)02188-7
106. Dahl, D, Onishi, Y, Norwood, P, Huh, R, Bray, R, Patel, H, et al. Effect of subcutaneous Tirzepatide vs placebo added to titrated insulin glargine on glycemic control in patients with type 2 diabetes: the SURPASS-5 randomized clinical trial. JAMA. (2022) 327:534–45. doi: 10.1001/jama.2022.0078
107. Gastaldelli, A, Cusi, K, Landó, LF, Bray, R, Brouwers, B, and Rodríguez, Á. Effect of tirzepatide versus insulin degludec on liver fat content and abdominal adipose tissue in people with type 2 diabetes (SURPASS-3 MRI): a substudy of the randomised, open-label, parallel-group, phase 3 SURPASS-3 trial. Lancet Diabetes Endocrinol. (2022) 10:393–406. doi: 10.1016/S2213-8587(22)00070-5
108. Hartman, ML, Sanyal, AJ, Loomba, R, Wilson, JM, Nikooienejad, A, Bray, R, et al. Effects of novel dual GIP and GLP-1 receptor agonist Tirzepatide on biomarkers of nonalcoholic steatohepatitis in patients with type 2 diabetes. Diabetes Care. (2020) 43:1352–5. doi: 10.2337/dc19-1892
109. Di Prospero, NA, Yee, J, Frustaci, ME, Samtani, MN, Alba, M, and Fleck, P. Efficacy and safety of glucagon-like peptide-1/glucagon receptor co-agonist JNJ-64565111 in individuals with type 2 diabetes mellitus and obesity: A randomized dose-ranging study. Clin Obes. (2021) 11:e12433. doi: 10.1111/cob.12433
110. Hope, DCD, Vincent, ML, and Tan, TMM. Striking the balance: GLP-1/glucagon co-Agonism as a treatment strategy for obesity. Front Endocrinol. (2021) 12:735019. doi: 10.3389/fendo.2021.735019
111. Nahra, R, Wang, T, Gadde, KM, Oscarsson, J, Stumvoll, M, Jermutus, L, et al. Effects of Cotadutide on metabolic and hepatic parameters in adults with overweight or obesity and type 2 diabetes: A 54-week randomized phase 2b study. Diabetes Care. (2021) 44:1433–42. doi: 10.2337/dc20-2151
112. Asano, M, Sekikawa, A, Sugeno, M, Matsuoka, O, Robertson, D, and Hansen, L. Safety/tolerability, efficacy and pharmacokinetics of 600-μg cotadutide in Japanese type 2 diabetes patients with a body mass index of 25 kg/m2 or higher: A phase I, randomized, double-blind, placebo-controlled study. Diabetes Obes Metab. (2023) 25:2290–9. doi: 10.1111/dom.15107
113. Romero-Gómez, M, Lawitz, E, Shankar, RR, Chaudhri, E, Liu, J, Lam, RL, et al. A phase IIa active-comparator-controlled study to evaluate the efficacy and safety of efinopegdutide in patients with non-alcoholic fatty liver disease. J Hepatol. (2023) 79:888–97. doi: 10.1016/j.jhep.2023.05.013
114. Alba, M, Yee, J, Frustaci, ME, Samtani, MN, and Fleck, P. Efficacy and safety of glucagon-like peptide-1/glucagon receptor co-agonist JNJ-64565111 in individuals with obesity without type 2 diabetes mellitus: a randomized dose-ranging study. Clin Obes. (2021) 11:e12432. doi: 10.1111/cob.12432
115. Nestor, JJ, Parkes, D, Feigh, M, Suschak, JJ, and Harris, MS. Effects of ALT-801, a GLP-1 and glucagon receptor dual agonist, in a translational mouse model of non-alcoholic steatohepatitis. Sci Rep. (2022) 12:6666. doi: 10.1038/s41598-022-10577-2
116. Harrison, SA, Tomah, S, Suschak, J, Roberts, S, Yang, J, He, L, et al. Pemvidutide, a GLP-1/glucagon dual receptor agonist significantly reduces liver fat, fibro-inflammation, and body weight in patients with non-alcoholic fatty liver disease: 1 24-week multicenter, randomized, double-blind, placebo-controlled trial. J Hepatol. (2023) 44:72–84. doi: 10.1007/s00261-018-1701-2
117. Rosenstock, J, Frias, J, Jastreboff, AM, du, Y, Lou, J, Gurbuz, S, et al. Retatrutide, a GIP, GLP-1 and glucagon receptor agonist, for people with type 2 diabetes: a randomised, double-blind, placebo and active-controlled, parallel-group, phase 2 trial conducted in the USA. Lancet. (2023) 402:529–44. doi: 10.1016/S0140-6736(23)01053-X
118. Jastreboff, AM, Kaplan, LM, Frías, JP, Wu, Q, du, Y, Gurbuz, S, et al. Triple-hormone-receptor agonist Retatrutide for obesity – a phase 2 trial. N Engl J Med. (2023) 389:514–26. doi: 10.1056/NEJMoa2301972
119. Sanyal, A, Frias, JP, Thomas, MK, et al. Triple hormone receptor agonist retatrutide resolves steatosis in >85% of subjects with MASLD and obesity in association with improved metabolic health. Hepatology. (2023) 78:S154–5.
120. Sanyal, A, Frias, JP, Thomas, MK, Mather, KJ, Wu, Q, Du, Y, et al. Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N Engl J Med. (2010) 362:1675–85. doi: 10.1056/NEJMoa0907929
121. O’Connor, EA, Evans, CV, Ivlev, I, Rushkin, MC, Thomas, RG, Martin, A, et al. Vitamin and mineral supplements for the primary prevention of cardiovascular disease and Cancer: updated evidence report and systematic review for the US preventive services task force. JAMA. (2022) 327:2334–47. doi: 10.1001/jama.2021.15650
122. Neuhouser, ML, Barnett, MJ, Kristal, AR, Ambrosone, CB, King, IB, Thornquist, M, et al. Dietary supplement use and prostate cancer risk in the carotene and retinol efficacy trial. Cancer Epidemiol Biomarkers Prev. (2009) 18:2202–6. doi: 10.1158/1055-9965.EPI-09-0013
123. Miller, ER 3rd, Pastor Barriuso, R, Dalal, D, Riemersma, RA, Appel, LJ, and Guallar, E. Meta-analysis: high-dosage vitamin E supplementation may increase all-cause mortality. Ann Intern Med. (2005) 142:37–46. doi: 10.7326/0003-4819-142-1-200501040-00110
124. Leppälä, JM, Virtamo, J, Fogelholm, R, Huttunen, JK, Albanes, D, Taylor, PR, et al. Controlled trial of alpha-tocopherol and beta-carotene supplements on stroke incidence and mortality in male smokers. Arterioscler Thromb Vasc Biol. (2000) 20:230–5. doi: 10.1161/01.ATV.20.1.230
125. Sato, K, Gosho, M, Yamamoto, T, Kobayashi, Y, Ishii, N, Ohashi, T, et al. Vitamin E has a beneficial effect on nonalcoholic fatty liver disease: a meta-analysis of randomized controlled trials. Nutrition. (2015) 31:923–30. doi: 10.1016/j.nut.2014.11.018
126. Xu, R, Tao, A, Zhang, S, Deng, Y, and Chen, G. Association between vitamin E and non-alcoholic steatohepatitis: a meta-analysis. Int J Clin Exp Med. (2015) 8:3024–6.
127. Wang, MY, Prabahar, K, Găman, MA, and Zhang, JL. Vitamin E supplementation in the treatment on NAFLD: evidence from an umbrella review of meta-analysis on randomized controlled trials. J Dig Dis. (2023) 24:380–9. doi: 10.1111/1751-2980.13210
128. Vilar Gomez, E, Vuppalanchi, R, Gawrieh, S, Ghabril, M, Saxena, R, Cummings, OW, et al. Vitamin E improves transplant-Free survival and hepatic decompensation among patients with NASH and advanced fibrosis. Hepatology. (2020) 71:495–509. doi: 10.1002/hep.30368
129. Cusi, K, Orsak, B, Bril, F, Lomonaco, R, Hecht, J, Ortiz-Lopez, C, et al. Long-term pioglitazone treatment for patients with nonalcoholic steatohepatitis and prediabetes or type 2 diabetes mellitus: A randomized trial. Ann Intern Med. (2016) 165:305–15. doi: 10.7326/M15-1774
130. Bril, F, Kalavalapalli, S, Clark, VC, Lomonaco, R, Soldevila-Pico, C, Liu, IC, et al. Response to pioglitazone in patients with nonalcoholic steatohepatitis with vs without type 2 diabetes. Clin Gastroenterol Hepatol. (2018) 16:558–566.e2. doi: 10.1016/j.cgh.2017.12.001
131. Musso, G, Cassader, M, Paschetta, E, and Gambino, R. Thiazolidinediones and advanced liver fibrosis in nonalcoholic steatohepatitis: a meta-analysis. JAMA. (2017) 177:633–40. doi: 10.1001/jamainternmed.2016.9607
132. Viscoli, CM, Inzucchi, SE, Young, LH, Insogna, KL, Conwit, R, Furie, KL, et al. Pioglitazone and risk for bone fracture: safety data from a randomized clinical trial. J Clin Endocrinol Metab. (2017) 102:914–22. doi: 10.1210/jc.2016-3237
133. Tang, H, Shi, W, Fu, S, Wang, T, Zhai, S, Song, Y, et al. Pioglitazone and bladder cancer risk: a systematic review and meta-analysis. Cancer Med. (2018) 7:1070–80. doi: 10.1002/cam4.1354
134. DeFronzo, RA, Inzucchi, S, Abdul-Ghani, M, and Nissen, SE. Pioglitazone: the forgotten, cost-effective cardioprotective drug for type 2 diabetes. Diab Vasc Disc Res. (2019) 16:133–43. doi: 10.1177/1479164118825376
135. Spence, JD, Viscoli, CM, Inzucchi, SE, Dearborn-Tomazos, J, Ford, GA, Gorman, M, et al. Pioglitazone therapy in patients with stroke and prediabetes: A post hoc analysis of the IRIS randomized clinical trial. JAMA Neurol. (2019) 76:526–35. doi: 10.1001/jamaneurol.2019.0079
136. Zhou, Y, Huang, Y, Ji, X, Wang, X, Shen, L, and Wang, Y. Pioglitazone for the primary and secondary prevention of cardiovascular and renal outcomes in patients with or at high risk of type 2 diabetes mellitus: a meta-analysis. J Clin Endocrinol Metab. (2020) 105:1670–81. doi: 10.1210/clinem/dgz252
137. Nesti, L, Tricò, D, Mengozzi, A, and Natali, A. Rethinking pioglitazone as a cardioprotective agent: a new perspective on an overlooked drug. Cardiovasc Diabetol. (2021) 20:109. doi: 10.1186/s12933-021-01294-7
138. Filipova, E, Uzunova, K, Kalinov, K, and Vekov, T. Pioglitazone and the risk of bladder cancer: a meta-analysis. Diabetes Ther. (2017) 8:705–26. doi: 10.1007/s13300-017-0273-4
139. Wong, VW, Zelber‐Sagi, S, Cusi, K, Carrieri, P, Wright, E, Crespo, J, et al. Management of NAFLD in primary care settings. Liver Int. (2022) 42:2377–89. doi: 10.1111/liv.15404
140. Jacques, V, Bolze, S, Hallakou‐Bozec, S, Czarnik, AW, Divakaruni, AS, Fouqueray, P, et al. Deuterium-stabilized (R)-pioglitazone (PXL065) is responsible for pioglitazone efficacy in NASH yet exhibits Little to no PPARγ activity. Hepatol Commun. (2021) 5:1412–25. doi: 10.1002/hep4.1723
141. Harrison, SA, Thang, C, Bolze, S, Dewitt, S, Hallakou-Bozec, S, Dubourg, J, et al. Evaluation of PXL065 – deuterium-stabilized (R)-pioglitazone in patients with NASH: A phase II randomized placebo-controlled trial (DESTINY-1). J Hepatol. (2023) 78:914–25. doi: 10.1016/j.jhep.2023.02.004
142. Sinha, B, Datta, D, and Ghosal, S. Meta-analysis of the effects of sodium glucose cotransporter 2 inhibitors in non-alcoholic fatty liver disease patients with type 2 diabetes. JGH Open. (2020) 5:219–27. doi: 10.1002/jgh3.12473
143. Jin, Z, Yuan, Y, Zheng, C, Liu, S, and Weng, H. Effects of sodium-glucose co-transporter 2 inhibitors on liver fibrosis in non-alcoholic fatty liver disease patients with type 2 diabetes mellitus: an updated meta-analysis of randomized controlled trials. J Diabetes Complications. (2023) 37:108558. doi: 10.1016/j.jdiacomp.2023.108558
144. Zinman, B, Wanner, C, Lachin, JM, Fitchett, D, Bluhmki, E, Hantel, S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. (2015) 373:2117–28. doi: 10.1056/NEJMoa1504720
145. Packer, M, Anker, SD, Butler, J, Filippatos, G, Pocock, SJ, Carson, P, et al. Cardiovascular and renal outcomes with Empagliflozin in heart failure. N Engl J Med. (2020) 383:1413–24. doi: 10.1056/NEJMoa2022190
146. Ghosal, S, and Sinha, B. Exploring the comparative cardiovascular death benefits of sodium-glucose cotransporter 2 inhibitors in type 2 diabetes: a frequentist and Bayesian network meta-analysis-based scoring. Front Endocrinol. (2023) 14:1168755. doi: 10.3389/fendo.2023.1168755
147. Riley, DR, Essa, H, Austin, P, Preston, F, Kargbo, I, Ibarburu, GH, et al. All-cause mortality and cardiovascular outcomes with sodium-glucose co-transporter 2 inhibitors, glucagon-like peptide-1 receptor agonists and with combination therapy in people with type 2 diabetes. Diabetes Obes Metab. (2023) 25:2897–909. doi: 10.1111/dom.15185
148. Rinella, ME, Tacke, F, Sanyal, AJ, and Anstee, QM, on behalf of the participants of the AASLD/EASL Workshop. Report on the AASLD/EASL joint workshop on clinical trial endpoints in NAFLD. Hepatology. (2019) 70:1424–36. doi: 10.1002/hep.30782
149. Cheung, A, Neuschwander‐Tetri, BA, Kleiner, DE, Schabel, E, Rinella, M, Harrison, S, et al. Defining improvement in nonalcoholic steatohepatitis for treatment trial endpoints: recommendations from the liver forum. Hepatology. (2019) 70:1841–55. doi: 10.1002/hep.30672
150. Ratziu, V, Harrison, SA, Francque, S, Bedossa, P, Lehert, P, Serfaty, L, et al. Elafibranor, an agonist of the peroxisome proliferator-activated receptor-α and -δ, induces resolution of nonalcoholic steatohepatitis without fibrosis worsening. Gastroenterology. (2016) 150:1147–1159.e5. doi: 10.1053/j.gastro.2016.01.038
151. Harrison, S, Ratziu, V, Dufour, JF, Kruger, C, Schattenberg, JM, Francque, S, et al. The dual PPARa/d agonist elafibranor did not achieve resolution of NASH without worsening of fibrosis in adult patients with non-alcoholic steato- hepatitis and significant fibrosis. Hepatology. (2020) 72 Abstract 1730. doi: 10.1002/hep.31579
152. Friedman, SL, Ratziu, V, Harrison, SA, Abdelmalek, MF, Aithal, GP, Caballeria, J, et al. A randomized, placebo-controlled trial of cenicriviroc for treatment of nonalcoholic steatohepatitis with fibrosis. Hepatology. (2018) 67:1754–67. doi: 10.1002/hep.29477
153. Ratziu, V, Sanyal, AJ, Harrison, SA, Wong, VWS, Francque, S, Goodman, Z, et al. Cenicriviroc treatment for adults with nonalcoholic steatohepatitis and fibrosis: final analysis of the phase 2b CENTAUR study. Hepatology. (2020) 72:892–905. doi: 10.1002/hep.31108
154. Harrison, SA, Wong, VWS, Okanoue, T, Bzowej, N, Vuppalanchi, R, Younes, Z, et al. Selonsertib for patients with bridging fibrosis or compensated cirrhosis due to NASH: results from randomized phase III STELLAR trials. J Hepatol. (2020) 73:26–39. doi: 10.1016/j.jhep.2020.02.027
155. Harrison, SA, Abdelmalek, MF, Caldwell, S, Shiffman, ML, Diehl, AM, Ghalib, R, et al. Simtuzumab is ineffective for patients with bridging fibrosis or compensated cirrhosis caused by nonalcoholic steatohepatitis. Gastroenterology. (2018) 155:1140–53. doi: 10.1053/j.gastro.2018.07.006
156. Charles, ED, Neuschwander‐Tetri, BA, Pablo Frias, J, Kundu, S, Luo, Y, Tirucherai, GS, et al. Pegbelfermin (BMS-986036), PEGylated FGF21, in patients with obesity and type 2 diabetes: results from a randomized phase 2 study. Obesity. (2019) 27:41–9. doi: 10.1002/oby.22344
157. Loomba, R, Sanyal, AJ, Kowdley, KV, Bhatt, DL, Alkhouri, N, Frias, JP, et al. Randomized, controlled trial of the FGF21 analogue Pegozafermin in NASH. N Engl J Med. (2023) 389:998–1008. doi: 10.1056/NEJMoa2304286
158. Siddiqui, MS, Parmar, D, Sheikh, F, Sarin, SK, Cisneros, L, Gawrieh, S, et al. Saroglitazar, a dual PPAR α/γ agonist, improves Atherogenic dyslipidemia in patients with non-cirrhotic NAFLD: A pooled analysis. Clin Gastroenterol Hepatol. (2023) 21:2597–2605.e2. doi: 10.1016/j.cgh.2023.01.018
159. Pellicciari, R, Fiorucci, S, Camaioni, E, Clerici, C, Costantino, G, Maloney, PR, et al. 6alpha-ethyl-chenodeoxycholic acid (6-ECDCA), a potent and selective FXR agonist endowed with anticholestatic activity. J Med Chem. (2002) 45:3569–72. doi: 10.1021/jm025529g
160. Krause, C, Grohs, M, El Gammal, AT, Wolter, S, Lehnert, H, Mann, O, et al. Reduced expression of thyroid hormone receptor β in human nonalcoholic steatohepatitis. Endocr Connect. (2018) 7:1448–56. doi: 10.1530/EC-18-0499
161. Pagadala, MR, Zein, CO, Dasarathy, S, Yerian, LM, Lopez, R, and McCullough, AJ. Prevalence of hypothyroidism in nonalcoholic fatty liver disease. Dig Dis Sci. (2012) 57:528–34. doi: 10.1007/s10620-011-2006-2
162. Kim, D, Kim, W, Joo, SK, Bae, JM, Kim, JH, and Ahmed, A. Subclinical hypothyroidism and low-Normal thyroid function are associated with nonalcoholic steatohepatitis and fibrosis. Clin Gastroenterol Hepatol. (2018) 16:123–131.e1. doi: 10.1016/j.cgh.2017.08.014
163. Abdelmalek, MF, Sanyal, AJ, Nakajima, A, Neuschwander-Tetri, BA, Goodman, ZD, Lawitz, EJ, et al. Pegbelfermin in patients with nonalcoholic steatohepatitis and compensated cirrhosis (FALCON 2): A randomized phase 2b study. Clin Gastroenterol Hepatol. (2023). doi: 10.1016/j.cgh.2023.04.012
164. Loomba, R, Lawitz, EJ, Frias, JP, Ortiz-Lasanta, G, Johansson, L, Franey, BB, et al. Safety, pharmacokinetics, and pharmacodynamics of pegozafermin in patients with non-alcoholic steatohepatitis: a randomised, double-blind, placebo-controlled, phase 1b/2a multiple-ascending-dose study. Lancet Gastroenterol Hepatol. (2023) 8:120–32. doi: 10.1016/S2468-1253(22)00347-8
165. Morrison, MC, Verschuren, L, Salic, K, Verheij, J, Menke, A, Wielinga, PY, et al. Obeticholic acid modulates serum metabolites and gene signatures characteristic of human NASH and attenuates inflammation and fibrosis progression in Ldlr−/−.Leiden mice. Hepatol Commun. (2018) 2:1513–32. doi: 10.1002/hep4.1270
166. Li, S, Zhuge, A, Wang, K, Xia, J, Wang, Q, Han, S, et al. Obeticholic acid and ferrostatin-1 differentially ameliorate non-alcoholic steatohepatitis in AMLN diet-fed Ob/Ob mice. Front Pharmacol. (2022) 13:1081553. doi: 10.3389/fphar.2022.1081553
167. Chaudhuri, S, Dutta, A, and Das Chakraborty, SB. Efficacy and safety of saroglitazar in real-world patients of non-alcoholic fatty liver disease with or without diabetes including compensated cirrhosis: A tertiary care center experience. JGH Open. (2023) 7:215–20. doi: 10.1002/jgh3.12878
168. Francque, S. Saroglitazar for the treatment of NASH: the peroxisome proliferator-activated receptor story Goes on! Hepatology. (2021) 74:1730–3. doi: 10.1002/hep.32024
169. Younossi, ZM, Ratziu, V, Loomba, R, Rinella, M, Anstee, QM, Goodman, Z, et al. Obeticholic acid for the treatment of non-alcoholic steatohepatitis: interim analysis from a multicentre, randomised, placebo-controlled phase 3 trial. Lancet. (2019) 394:2184–96. doi: 10.1016/S0140-6736(19)33041-7
170. Armstrong, LE, and Guo, GL. Role of FXR in liver inflammation during nonalcoholic steatohepatitis. Curr Pharmacol Rep. (2017) 3:92–100. doi: 10.1007/s40495-017-0085-2
171. Li, L, Zhang, Q, Peng, J, Jiang, C, Zhang, Y, Shen, L, et al. Activation of farnesoid X receptor downregulates monocyte chemoattractant protein-1 in murine macrophage. Biochem Biophys Res Commun. (2015) 467:841–6. doi: 10.1016/j.bbrc.2015.10.056
172. Sanyal, AJ, Ratziu, V, Loomba, R, Anstee, QM, Kowdley, KV, Rinella, ME, et al. Results from a new efficacy and safety analysis of the REGENERATE trial of obeticholic acid for treatment of pre-cirrhotic fibrosis due to nonalcoholic steatohepatitis. J Hepatol. (2023) 79:1110–20. doi: 10.1016/j.jhep.2023.07.014
173. Francque, SM, Bedossa, P, Ratziu, V, Anstee, QM, Bugianesi, E, Sanyal, AJ, et al. A randomized, controlled trial of the Pan-PPAR agonist Lanifibranor in NASH. N Engl J Med. (2021) 385:1. doi: 10.1056/NEJMoa2036205
174. Harrison, SA, Bashir, MR, Guy, CD, Zhou, R, Moylan, CA, Frias, JP, et al. Resmetirom (MGL-3196) for the treatment of non-alcoholic steatohepatitis: a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet. (2019) 394:2012–24. doi: 10.1016/S0140-6736(19)32517-6
175. Harrison, SA, Frias, JP, Neff, G, Abrams, GA, Lucas, KJ, Sanchez, W, et al. Safety and efficacy of once-weekly efruxifermin versus placebo in non-alcoholic steatohepatitis (HARMONY): a multicentre, randomised, double-blind, placebo-controlled, phase 2b trial. Lancet Gastroenterol Hepatol. (2023) 8:1080–93. doi: 10.1016/S2468-1253(23)00272-8
176. Ma, K, Saha, PK, Chan, L, and Moore, DD. Farnesoid X receptor is essential for normal glucose homeostasis. J Clin Invest. (2006) 116:1102–9. doi: 10.1172/JCI25604
177. Xu, W, Lu, C, Zhang, F, Shao, J, Yao, S, and Zheng, S. Dihydroartemisinin counteracts fibrotic portal hypertension via farnesoid X receptor-dependent inhibition of hepatic stellate cell contraction. FEBS J. (2017) 284:114–33. doi: 10.1111/febs.13956
178. Adorini, L, and Trauner, M. Miniseries: established pharmacological targets for NASHFXR agonists in NASH treatment. J Hepatol. (2023) 79:1317–31. doi: 10.1016/j.jhep.2023.07.034
179. Calkin, AC, and Tontonoz, P. Transcriptional integration of metabolism by the nuclear sterol-activated receptors LXR and FXR. Nat Rev Mol Cell Biol. (2012) 13:213–24. doi: 10.1038/nrm3312
180. Henriksson, E, and Andersen, B. FGF19 and FGF21 for the treatment of NASH-two sides of the same coin? Differential and overlapping effects of FGF19 and FGF21 from mice to human. Front Endocrinol. (2020) 11:601349. doi: 10.3389/fendo.2020.601349
181. Rodrigues, PM, Afonso, MB, Simão, AL, Carvalho, CC, Trindade, A, Duarte, A, et al. miR-21 ablation and obeticholic acid ameliorate nonalcoholic steatohepatitis in mice. Cell Death Dis. (2017) 8:e2748. doi: 10.1038/cddis.2017.172
182. Mudaliar, S, Henry, RR, Sanyal, AJ, Morrow, L, Marschall, H–U, Kipnes, M, et al. Efficacy and safety of the farnesoid X receptor agonist obeticholic acid in patients with type 2 diabetes and NAFLD. Gastroenterology. (2013) 145:574–582.e1. doi: 10.1053/j.gastro.2013.05.042
183. Neuschwander-Tetri, BA, Loomba, R, Sanyal, AJ, Lavine, JE, Van Natta, ML, Abdelmalek, MF, et al. Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): a multicentre, randomised, placebo-controlled trial. Lancet. (2015) 385:956–65. doi: 10.1016/S0140-6736(14)61933-4
184. Siddiqui, MS, Van Natta, ML, Connelly, MA, Vuppalanchi, R, Neuschwander-Tetri, BA, Tonascia, J, et al. Impact of obeticholic acid on the lipoprotein profile in patients with non-alcoholic steatohepatitis. J Hepatol. (2020) 72:25–33. doi: 10.1016/j.jhep.2019.10.006
185. Pockros, PJ, Fuchs, M, Freilich, B, Schiff, E, Kohli, A, Lawitz, EJ, et al. CONTROL: A randomized phase 2 study of obeticholic acid and atorvastatin on lipoproteins in nonalcoholic steatohepatitis patients. Liver Int. (2019) 39:2082–93. doi: 10.1111/liv.14209
186. John, BV, Schwartz, K, Levy, C, Dahman, B, Deng, Y, Martin, P, et al. Impact of Obeticholic acid exposure on decompensation and mortality in primary biliary cholangitis and cirrhosis. Hepatol Commun. (2021) 5:1426–36. doi: 10.1002/hep4.1720
187. Rinella, ME, Dufour, JF, Anstee, QM, Goodman, Z, Younossi, Z, Harrison, SA, et al. Non-invasive evaluation of response to obeticholic acid in patients with NASH: results from the REGENERATE study. J Hepatol. (2022) 76:536–48. doi: 10.1016/j.jhep.2021.10.029
188. Tran, CP, Kim, JJ, Feld, JJ, and Wong, WW. Cost-effectiveness of obeticholic acid for the treatment of non-alcoholic steatohepatitis: an early economic evaluation. Can Liver J. (2021) 4:360–9. doi: 10.3138/canlivj-2021-0011
189. Obeticholic acid. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. Bethesda, MD: National Institute of Diabetes and Digestive and Kidney Diseases (2019)
190. Ratziu, V, Rinella, ME, Neuschwander-Tetri, BA, Lawitz, E, Denham, D, Kayali, Z, et al. EDP-305 in patients with NASH: A phase II double-blind placebo-controlled dose-ranging study. J Hepatol. (2022) 76:506–17. doi: 10.1016/j.jhep.2021.10.018
191. Patel, K, Harrison, SA, Elkhashab, M, Trotter, JF, Herring, R, Rojter, SE, et al. Cilofexor, a nonsteroidal FXR agonist, in patients with noncirrhotic NASH: A phase 2 randomized controlled trial. Hepatology. (2020) 72:58–71. doi: 10.1002/hep.31205
192. Sanyal, AJ, Lopez, P, Lawitz, EJ, Lucas, KJ, Loeffler, J, Kim, W, et al. Tropifexor for nonalcoholic steatohepatitis: an adaptive, randomized, placebo-controlled phase 2a/b trial. Nat Med. (2023) 29:392–400. doi: 10.1038/s41591-022-02200-8
193. Naoumov, NV, Brees, D, Loeffler, J, Chng, E, Ren, Y, Lopez, P, et al. Digital pathology with artificial intelligence analyses provides greater insights into treatment-induced fibrosis regression in NASH. J Hepatol. (2022) 77:1399–409. doi: 10.1016/j.jhep.2022.06.018
194. Anstee, QM, Lucas, KJ, Francque, S, Abdelmalek, MF, Sanyal, AJ, Ratziu, V, et al. Tropifexor plus cenicriviroc combination versus monotherapy in non-alcoholic steatohepatitis: results from the phase 2b TANDEM study. Hepatology. (2023) 78:1223–39. doi: 10.1097/HEP.0000000000000439
195. Loomba, R, Noureddin, M, Kowdley, KV, Kohli, A, Sheikh, A, Neff, G, et al. Combination therapies including Cilofexor and Firsocostat for bridging fibrosis and cirrhosis attributable to NASH. Hepatology. (2021) 73:625–43. doi: 10.1002/hep.31622
196. Alkhouri, N, Herring, R, Kabler, H, Kayali, Z, Hassanein, T, Kohli, A, et al. Safety and efficacy of combination therapy with semaglutide, cilofexor and firsocostat in patients with NASH: A randomised, open-label phase II trial. J Hepatol. (2022) 77:607–18. doi: 10.1016/j.jhep.2022.04.003
197. Staels, B, Butruille, L, and Francque, S. Treating NASH by targeting peroxisome proliferator-activated receptors. J Hepatol. (2023) 79:1302–16. doi: 10.1016/j.jhep.2023.07.004
198. Wettstein, G, Luccarini, JM, Poekes, L, Faye, P, Kupkowski, F, Adarbes, V, et al. The new-generation pan-peroxisome proliferator-activated receptor agonist IVA337 protects the liver from metabolic disorders and fibrosis. Hepatol Commun. (2017) 1:524–37. doi: 10.1002/hep4.1057
199. Gawrieh, S, Noureddin, M, Loo, N, Mohseni, R, Awasty, V, Cusi, K, et al. Saroglitazar, a PPAR-α/γ agonist, for treatment of NAFLD: A randomized controlled double-blind phase 2 trial. Hepatology. (2021) 74:1809–24. doi: 10.1002/hep.31843
200. Siddiqui, MS, Idowu, MO, Parmar, D, Borg, BB, Denham, D, Loo, NM, et al. A phase 2 double blinded, randomized controlled trial of Saroglitazar in patients with nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol. (2021) 19:2670–2. doi: 10.1016/j.cgh.2020.10.051
201. Goyal, O, Nohria, S, Goyal, P, Kaur, J, Sharma, S, Sood, A, et al. Saroglitazar in patients with non-alcoholic fatty liver disease and diabetic dyslipidemia: a prospective, observational, real world study. Sci Rep. (2020) 10:21117. doi: 10.1038/s41598-020-78342-x
202. Bohinc, BN, Michelotti, G, Xie, G, Pang, H, Suzuki, A, Guy, CD, et al. Repair-related activation of hedgehog signaling in stromal cells promotes intrahepatic hypothyroidism. Endocrinology. (2014) 155:4591–601. doi: 10.1210/en.2014-1302
203. Kelly, MJ, Pietranico-Cole, S, Larigan, JD, Haynes, NE, Reynolds, CH, Scott, N, et al. Discovery of 2-[3,5-dichloro-4-(5-isopropyl-6-oxo-1,6-dihydropyridazin-3-yloxy)phenyl]-3,5-dioxo-2,3,4,5-tetrahydro[1,2,4]triazine-6-carbonitrile (MGL-3196), a highly selective thyroid hormone receptor β agonist in clinical trials for the treatment of dyslipidemia. J Med Chem. (2014) 57:3912–23. doi: 10.1021/jm4019299
204. Kannt, A, Wohlfart, P, Madsen, AN, Veidal, SS, Feigh, M, and Schmoll, D. Activation of thyroid hormone receptor-β improved disease activity and metabolism independent of body weight in a mouse model of non-alcoholic steatohepatitis and fibrosis. Br J Pharmacol. (2021) 178:2412–23. doi: 10.1111/bph.15427
205. Harrison, SA, Bashir, M, Moussa, SE, McCarty, K, Pablo Frias, J, Taub, R, et al. Effects of Resmetirom on noninvasive endpoints in a 36-week phase 2 active treatment extension study in patients with NASH. Hepatol Commun. (2021) 5:573–88. doi: 10.1002/hep4.1657
206. Harrison, SA, Bedossa, P, Guy, C, Schattenberg, J, Loomba, R, Taub, R, et al. Primary results from MAESTRO-NASH a pivotal phase 3 52-week serial liver biopsy study in 966 patients with NASH and fibrosis. J Hepatol. (2023) 78:401–6. doi: 10.1016/S0168-8278(23)00440-3
207. Tillman, EJ, and Rolph, T. FGF21: an emerging therapeutic target for non-alcoholic steatohepatitis and related metabolic diseases. Front Endocrinol. (2020) 11:601290. doi: 10.3389/fendo.2020.601290
208. Harrison, SA, Ruane, PJ, Freilich, BL, Neff, G, Patil, R, Behling, CA, et al. Efruxifermin in non-alcoholic steatohepatitis: a randomized, double-blind, placebo-controlled, phase 2a trial. Nat Med. (2021) 27:1262–71. doi: 10.1038/s41591-021-01425-3
209. Harrison, SA, Ruane, PJ, Freilich, B, Neff, G, Patil, R, Behling, C, et al. A randomized, double-blind, placebo-controlled phase IIa trial of efruxifermin for patients with compensated NASH cirrhosis. JHEP Rep. (2022) 5:100563. doi: 10.1016/j.jhepr.2022.100563
210. Loomba, R, Sanyal, AJ, Nakajima, A, Neuschwander-Tetri, BA, Goodman, ZD, Harrison, SA, et al. Pegbelfermin in patients with nonalcoholic steatohepatitis and stage 3 fibrosis (FALCON 1): A randomized phase 2b study. Clin Gastroenterol Hepatol. (2023). doi: 10.1016/j.cgh.2023.04.011
211. Bhatt, DL, Bays, HE, Miller, M, Cain, JE III, Wasilewska, K, Andrawis, NS, et al. The FGF21 analog pegozafermin in severe hypertriglyceridemia: a randomized phase 2 trial. Nat Med. (2023) 29:1782–92. doi: 10.1038/s41591-023-02427-z
212. Alisi, A, Ceccarelli, S, Panera, N, Prono, F, Petrini, S, de Stefanis, C, et al. Association between serum atypical fibroblast growth factors 21 and 19 and pediatric nonalcoholic fatty liver disease. PLoS One. (2013) 8:e67160. doi: 10.1371/journal.pone.0067160
213. Nicholes, K, Guillet, S, Tomlinson, E, Hillan, K, Wright, B, Frantz, GD, et al. A mouse model of hepatocellular carcinoma: ectopic expression of fibroblast growth factor 19 in skeletal muscle of transgenic mice. Am J Pathol. (2002) 160:2295–307. doi: 10.1016/S0002-9440(10)61177-7
214. Chen, Z, Jiang, L, Liang, L, Koral, K, Zhang, Q, Zhao, L, et al. The role of fibroblast growth factor 19 in hepatocellular carcinoma. Am J Pathol. (2021) 191:1180–92. doi: 10.1016/j.ajpath.2021.04.014
215. Zhou, M, Wang, X, Phung, V, Lindhout, DA, Mondal, K, Hsu, J-Y, et al. Separating Tumorigenicity from bile acid regulatory activity for endocrine hormone FGF19. Cancer Res. (2014) 74:3306–16. doi: 10.1158/0008-5472.CAN-14-0208
216. Zhou, M, Yang, H, Learned, RM, Tian, H, and Ling, L. Non-cell-autonomous activation of IL-6/STAT3 signaling mediates FGF19-driven hepatocarcinogenesis. Nat Commun. (2017) 8:15433. doi: 10.1038/ncomms15433
217. Zhou, M, Learned, RM, Rossi, SJ, DePaoli, AM, Tian, H, and Ling, L. Engineered FGF19 eliminates bile acid toxicity and lipotoxicity leading to resolution of steatohepatitis and fibrosis in mice. Hepatol Commun. (2017) 1:1024–42. doi: 10.1002/hep4.1108
218. Luo, J, Ko, B, Elliott, M, Zhou, M, Lindhout, DA, Phung, V, et al. A nontumorigenic variant of FGF19 treats cholestatic liver diseases. Sci Transl Med. (2014) 6:247ra100. doi: 10.1126/scitranslmed.3009098
219. Harrison, SA, Rossi, SJ, Paredes, AH, Trotter, JF, Bashir, MR, Guy, CD, et al. NGM282 improves liver fibrosis and histology in 12 weeks in patients with nonalcoholic steatohepatitis. Hepatology. (2020) 71:1198–212. doi: 10.1002/hep.30590
220. Harrison, SA, Neff, G, Guy, CD, Bashir, MR, Paredes, AH, Frias, JP, et al. Efficacy and safety of Aldafermin, an engineered FGF19 analog, in a randomized, double-blind, placebo-controlled trial of patients with nonalcoholic steatohepatitis. Gastroenterology. (2021) 160:219–231.e1. doi: 10.1053/j.gastro.2020.08.004
221. Harrison, SA, Abdelmalek, MF, Neff, G, Gunn, N, Guy, CD, Alkhouri, N, et al. Aldafermin in patients with non-alcoholic steatohepatitis (ALPINE 2/3): a randomised, double-blind, placebo-controlled, phase 2b trial. Lancet Gastroenterol Hepatol. (2022) 7:603–16. doi: 10.1016/S2468-1253(22)00017-6
222. Loomba, R, Kayali, Z, Noureddin, M, Ruane, P, Lawitz, EJ, Bennett, M, et al. GS-0976 reduces hepatic steatosis and fibrosis markers in patients with nonalcoholic fatty liver disease. Gastroenterology. (2018) 155:1463–1473.e6. doi: 10.1053/j.gastro.2018.07.027
223. Loomba, R, Mohseni, R, Lucas, KJ, Gutierrez, JA, Perry, RG, Trotter, JF, et al. TVB-2640 (FASN inhibitor) for the treatment of nonalcoholic steatohepatitis: FASCINATE-1, a randomized, placebo-controlled phase 2a trial. Gastroenterology. (2021) 161:1475–86. doi: 10.1053/j.gastro.2021.07.025
224. O’Farrell, M, Grimmer, K, Zetter, A, Tsai, WW, Kemble, G, Loomba, R, et al. Multicenter, randomized, double-blind, placebo-controlled trial of fatty acid synthase (FASN) inhibitor, denifanstat, versus placebo in the treatment of biopsy-proven NASH: A 26-week interim analysis of the FASCINATE-2 phase 2B trial. J Hepatol. (2023) 78:1475–86.
225. Safadi, R, Konikoff, FM, Mahamid, M, Zelber-Sagi, S, Halpern, M, Gilat, T, et al. The fatty acid-bile acid conjugate Aramchol reduces liver fat content in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. (2014) 12:2085–2091.e1. doi: 10.1016/j.cgh.2014.04.038
226. Ratziu, V, de Guevara, L, Safadi, R, Poordad, F, Fuster, F, Flores-Figueroa, J, et al. Aramchol in patients with nonalcoholic steatohepatitis: a randomized, double-blind, placebo-controlled phase 2b trial. Nat Med. (2021) 27:1825–35. doi: 10.1038/s41591-021-01495-3
227. Chalasani, N, Abdelmalek, MF, Garcia-Tsao, G, Vuppalanchi, R, Alkhouri, N, Rinella, M, et al. Effects of Belapectin, an inhibitor of Galectin-3, in patients with nonalcoholic steatohepatitis with cirrhosis and portal hypertension. Gastroenterology. (2020) 158:1334–1345.e5. doi: 10.1053/j.gastro.2019.11.296
228. Lindén, D, and Romeo, S. Therapeutic opportunities for the treatment of NASH with genetically validated targets. J Hepatol. (2023) 79:1056–64. doi: 10.1016/j.jhep.2023.05.007
Glossary
Keywords: MASLD, treatment, obesity, weight loss, liver disease-targeted drugs
Citation: Machado MV (2023) MASLD treatment—a shift in the paradigm is imminent. Front. Med. 10:1316284. doi: 10.3389/fmed.2023.1316284
Edited by:
Zheng Li, Jiangsu Normal University, ChinaReviewed by:
Sanal M. G., The Institute of Liver and Biliary Sciences (ILBS), IndiaValentina Cossiga, University of Naples Federico II, Italy
Stefano Ciardullo, University of Milano Bicocca, Italy
Copyright © 2023 Machado. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mariana Verdelho Machado, bXZlcmRlbGhvbWFjaGFkb0BnbWFpbC5jb20=
 Mariana Verdelho Machado
Mariana Verdelho Machado