
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 21 November 2023
Sec. Family Medicine and Primary Care
Volume 10 - 2023 | https://doi.org/10.3389/fmed.2023.1298778
Introduction: It is necessary to explore the evidence-based practice of perioperative management of elderly patients undergoing ambulatory surgery, to optimize the clinical workflow and improve the quality of nursing care.
Methods: Based on the best evidence obtained from the previous study, the perioperative management model and examination index of elderly patients undergoing day surgery were established, and the evidence of best practice was obtained by using the evidence-based methodology. Then, we integrated evidence into clinical practice and improved the process. We made a comparative analysis of the effect before and after the implementation of the evidence.
Results: This study summarized 26 pieces of evidence of perioperative management of elderly patients undergoing day surgery and transformed the evidence into 7 items and 11 items of examination index. After the application of the best evidence, knowledge, belief, and practice of perioperative management of nurses for elderly patients in the day operation ward reached 100%, and the rate of reaching the standard of most indicators increased after the application of evidence. The length of waiting for admission and waiting for operation and returning to the ward to discharge of elderly patients decreased significantly, and the difference was statistically significant (All p < 0.05).
Conclusion: Evidence-based perioperative management of elderly patients undergoing day surgery improves the nursing practice of clinical nurses and shortens the waiting time and hospitalization time of elderly patients undergoing day surgery, which should be promoted in clinical nursing care.
In recent years, with the shortage of medical resources and the rise of medical expenses, how to reduce medical expenses, speed up patient turnover, and make full and rational use of bed resources has become an important issue that the public is concerned about and the government urgently needs to solve (1, 2). The promotion of the day surgery ward has become one of the effective ways to solve this contradiction. The China Ambulatory Surgery Alliance (CASA) defines day surgery as “an operation or operation completed by a patient entering or leaving the hospital in 1 day (24 h)” (3). The longest hospitalization time of patients who need to be delayed due to their illness is not more than 48 h. At present, China is vigorously promoting the development of day surgery. From 2015 to 2017, China Government has issued many policy documents to promote the development of day surgery and expand the scope of day surgery (4). With the development of day surgery, it is very important to have standardized medical and nursing management processes to ensure the care quality and safety of patients (5). From the preparation of pre-admission examination and operation scheduling to the follow-up of hospitalization and discharge on the day of operation, nurses are important participants in all aspects that directly affect the smooth implementation and development of daytime surgery (6, 7). It is necessary to standardize management and care processes in order to ensure the quality of medical care and promote the development of high efficiency and quality of day surgery (8, 9).
Under the trend of the aging population and development of medical technology, more and more elderly patients can tolerate surgical treatment. For the elderly, shorter hospital stay can reduce the incidence of postoperative complications and readmission rates (10). At present, a large number of medical institutions have actively explored and practiced day surgery, but the perioperative management of day surgery in elderly patients is more complex because of their pathophysiological particularity (11). Compared with young patients, elderly patients need more medical management services (12). Therefore, the purpose of this study is to apply the best evidence of perioperative management of elderly patients undergoing day surgery through a systematic transformation of clinical evidence, to optimize the clinical workflow to improve the operational efficiency of the day operation ward and improve the quality of nursing care for elderly patients undergoing day surgery.
This study obtained approval from the ethical committee of our hospital with approval number: HD190026. This study was a before and after self-control study design. All the procedures were performed in accordance with the related regulations and guidelines.
We defined evidence-based problems and retrieval strategies according to the PIPOST principles. P (population): the target of evidence application was elderly patients undergoing day surgery; I (intervention): intervention, evidence-based practice based on the best evidence, including perioperative workflow management before admission, during hospital stay, and after discharge; P (professional): the implementer of clinical transformation of evidence, nurse, doctor, and anesthesiologist; O (outcome): including waiting time for surgery, preparation for discharge, patient satisfaction, practitioners’ knowledge, and belief and evidence-based compliance; S (setting): clinical scenario and day surgery ward of our hospital; T (type): including clinical practice guide, expert consensus, evidence summary, and systematic evaluation.
According to the “6s” evidence model, evidence retrieval was carried out. The English search strategies were (“old” OR “elderly” OR “aged” OR “geriatric”) AND (“peri-operation”) AND “day surgery” OR “short stay surgery” OR “ambulatory surg*.” We searched BMJ Best Practice, RNAO, NICE, NGC, SIGN, Association of Day Surgery (IAAS), China Alliance for Cooperation in Day Surgery, Cochrane, Joanna Briggs Institute (JBI), Medline, Embase, and CBM. The search time limit was from the establishment of the database to September 2021. The inclusion criteria of the literature were elderly patients (60 years old) who were treated in the day operation ward, and the content of the study was related to perioperative management. The study was designed for clinical decision-making, clinical practice guidelines, expert consensus, evidence summary, and systematic evaluation and was published in Chinese and English. The exclusion standard was that the full text could not be obtained, and the data of the research content report was incomplete.
A total of 11 articles were included in this project, including 2 guidelines (13, 14), 4 expert consensus (15–18), and 5 evidence summary (19–23). The quality of the two guidelines was evaluated using the Appraisal of Guidelines for Research and Evaluation (AGREE) (24).
The quality evaluation criteria of four expert consensus were used to evaluate the authenticity of the literature according to the evaluation tools of JBI evidence-based healthcare center expert opinions and professional consensus articles (25). Five pieces of evidence summarized the literature on which the evidence was based, and the corresponding evaluation criteria were selected according to the type of literature for quality evaluation. All the literature studies were scored by three researchers who had received evidence-based training according to the contents of the corresponding literature quality evaluation items, and the controversial items were discussed by the third-party researchers and finally reached an agreement. A total of 26 pieces of evidence of perioperative management of elderly patients undergoing day surgery were extracted.
The evidence evaluation team was composed of a head nurse in the day operation ward, 3 full-time nurses in the day operation ward, 2 general surgeons, and 1 nursing graduate student, all of whom have bachelor’s degree or above and had more than 2 years of working experience in the day operation ward. Based on the attributes of evidence FAME, the feasibility, suitability, clinical significance, and validity of 26 pieces of evidence were evaluated. The evidence level of the original guide or evidence summary was retained, and their sources were marked. When the included evidence comes from multiple articles, one with a higher level of evidence was selected. Finally, 7 pieces of best evidence were included. According to the principle of merging the same evidence and splitting the different evidence, 11 pieces of evidence for examination had been formulated, as shown in Table 1.
We established an evidence-based core group, including a professor engaged in nursing management and evidence-based practice methodology; two nursing backbones who were engaged in day surgery and trained in evidence-based methodology were responsible for team training, project implementation, evidence implementation process control, and data management; and three full-time day surgery nurses with bachelor’s degree were responsible for team coordination and communication, data collection, and follow-up maintenance. Two full-time nurses for day surgery were responsible for the application of evidence.
We collected data on the current nursing situation from September 2021 to December 2021. (1) On-site verification: As shown in Table 1, the review indicators 1–6, 9, and 10 were all judged by the members of the evidence-based core group on the spot of nurses and elderly patients in the day operation ward and truthfully recorded in the project data summary table according to the situation. (2) Questionnaire: As shown in Table 1, index 10 was investigated by the full-time nurses in the designated day operation ward using the Chinese version of the discharge readiness scale (26). Cronbach’s α of the internal consistency of the whole scale is 0.89 with good reliability and validity. (3) Review of the electronic medical record system: As shown in Table 1, review indicators 7 and 8 were extracted from the electronic medical record system, including waiting time for admission, operation, anesthesia start time, operation time, and time out of the operating room. (4) Nursing record sheet confirmation: As shown in Table 1, indicators 1 and 11 were reviewed, and the data collection and follow-up content forms were developed by the members of the evidence-based core group, and full-time nurses in the day operation ward were designated to collect information, including whether they could be admitted to the hospital as scheduled, preoperative fasting and intestinal preparation confirmation, and follow-up after discharge.
The main obstacles discussed and identified by the team included the following points: (1) There were differences in the process of admission preparation among different departments; (2) There was a lack of perioperative health education and materials; (3) The compliance of elderly patients with preoperative preparation was insufficient; (4) Doctor’s acceptance of the electronic day operation booking system was not high; (5) The turnover rate of daytime operation was high, and doctor’s order was not issued in time, which affected the progress of operation, discharge, and patient experience; (6) Medical staff did not have enough understanding of the best evidence-based practice in the perioperative period of day surgery; (7) Accurate evaluation of daytime surgery, there were deficiencies in the selection of appropriate anesthetic methods; and (8) The number of follow-up of patients undergoing daytime operation was large.
We introduced the best evidence to update the perioperative management process of elderly patients undergoing day surgery. The members of the evidence core group organized the management staff of the medical department, the doctors of the relevant clinical departments, and the nurses in the day operation ward for on-the-spot discussion to introduce the best evidence into the existing perioperative management process of elderly patients undergoing day surgery. The updated contents included unified coordination of preoperative preparation for daytime surgery before admission, evaluation of outpatient anesthesia, second confirmation of admission time, time of issuance of doctor’s orders, form, content, and time of health education, health education materials for different operations, evaluation and observation of postoperative complications, and postoperative follow-up. The updated perioperative management of elderly patients in the day operation ward was based on the best evidence content and defined the executor, execution time, and implementation standard in the whole process of day operation for elderly patients, which was operable.
In addition, we strengthened effective communication between doctors and nurses and introduced a daytime surgery information management system. We set up a WeChat working group for daytime surgery doctors and nurses. The doctor could book the operation date and bed at the same time in the outpatient clinic or complete the appointment after the consultation. Full-time nurses for daytime surgery confirmed the bed reservation information in the information management system and contacted the patients over the phone at least 1 day in advance to confirm the admission time of the patients and carry out preoperative preparation of health education. After the elderly patients were admitted to the hospital, the responsible nurse took the initiative to remind the bed doctor to issue surgical orders, nursing orders, and drug orders in time. The responsible doctor followed up the operation process in the operating room in time and contacted the ward nurse to prepare for the operation. After the operation, we correctly evaluated the patient’s postoperative condition, gave timely feedback to the doctor, and prepared for discharge. We organized and summarized the daily operation turnover every 2 weeks, communicated about the hindering factors, and improved the perioperative management process of elderly patients undergoing day surgery.
We also carried out perioperative management training for elderly patients undergoing day surgery. The perioperative management training of elderly patients undergoing day surgery was carried out through professional study and shift transfer, and the nurses were assessed. The contents included the confirmation of patient appointment information in the daytime operation information management system, the unification of health education content, updating the contents of preoperative preparation and the confirmation of preoperative evaluation results, postoperative nursing and discharge preparation evaluation, and other related knowledge.
At the same time, we have established a perioperative health education and discharge follow-up system for elderly patients undergoing day surgery. The content of perioperative health education for elderly patients undergoing day surgery consists of three parts. According to the best evidence, the appointment nurse and the responsible nurse completed the confirmation of the patient’s operation date and prepared the content of health education before admission to ensure that the operation was carried out normally. Intensive health education was carried out during the operation stage after admission. According to different anesthetic methods, surgical sites, surgical contents of health education, material distribution, and picture and text publicity, including TV rolling broadcast, corridor publicity wall posters, and video health education. After the completion of the operation, the patients were given postoperative health education, including observation of complications, time of intake, and type and usage of drugs. The elderly patients were followed up by the follow-up nurses in the ward within 1 week after discharge, including the incidence of complications, drug use compliance, pathological report review, and outpatient follow-up time.
In this evidence application, the day operation ward of a tertiary hospital in Shanghai was selected, and the subjects were the elderly patients and all the day surgery department nurses. The inclusion criteria for elderly patients were as follows: age ≥ 60 years old; the patients underwent day surgical treatment in our hospital; and the patients agreed to participate in this study.
A total of 10 nurses in the day operation ward were enrolled. The inclusion criteria were as follows: the nurses had the nurse qualification and registered nurse certificate; full-time nurse in the day operation ward, who was familiar with and knew most of the day operation types and nursing care; and the nurses had obtained the informed consent and agreed to participate in this study. The baseline review stage before the application of evidence was from September 2021 to December 2021 and the review stage after the application of evidence was from September 2022 to December 2022.
Practitioner level: Ten nurses in the day operation ward were investigated before and after evidence-based practice with self-made examination studies. The knowledge part included the process of perioperative management of day surgery for the elderly, assessment tools, health education, and postoperative follow-up, with a full score of 100. In addition, we used the Chinese version of the evidence-based practice questionnaire (EBPQ) on knowledge, belief, and practice to investigate clinical nurses (27). It had been reported that EBPQ’s Cronbach’s α was 0.94 and content validity was 0.83 with good reliability and validity (28). Process level: the implementation rate of each examination index of perioperative management of elderly patients undergoing day surgery. The data collection method included on-the-spot verification method, questionnaire method, consulting electronic medical record system, and form confirmation. Patient level: the change in waiting time in the perioperative period of elderly patients.
SPSS 21.0 statistical software was used for data analysis. The measurement data were expressed by mean and standard deviation using an independent sample t-test for group comparison. The counting data were expressed by the number of cases and percentage and compared by chi-square test. In this study, p < 0.05 was considered statistically significant.
This evidence-based practice included 10 full-time nurses in the day operation ward. All the above personnel were trained in evidence-based practice. The level of knowledge, belief, and practice of nurses on perioperative management of elderly patients undergoing day surgery before and after evidence-based practice is shown in Table 2.
Before evidence-based practice, the implementation rates of indicators 8 and 10 were 0, and the implementation rates of indicators 1, 3, 5, and 11 were all less than 30%. After evidence-based practice, the implementation rates of all indicators were significantly improved (p < 0.05). At the same time, the implementation rate of indicators 6 and 9 reached 100%, as shown in Table 3.
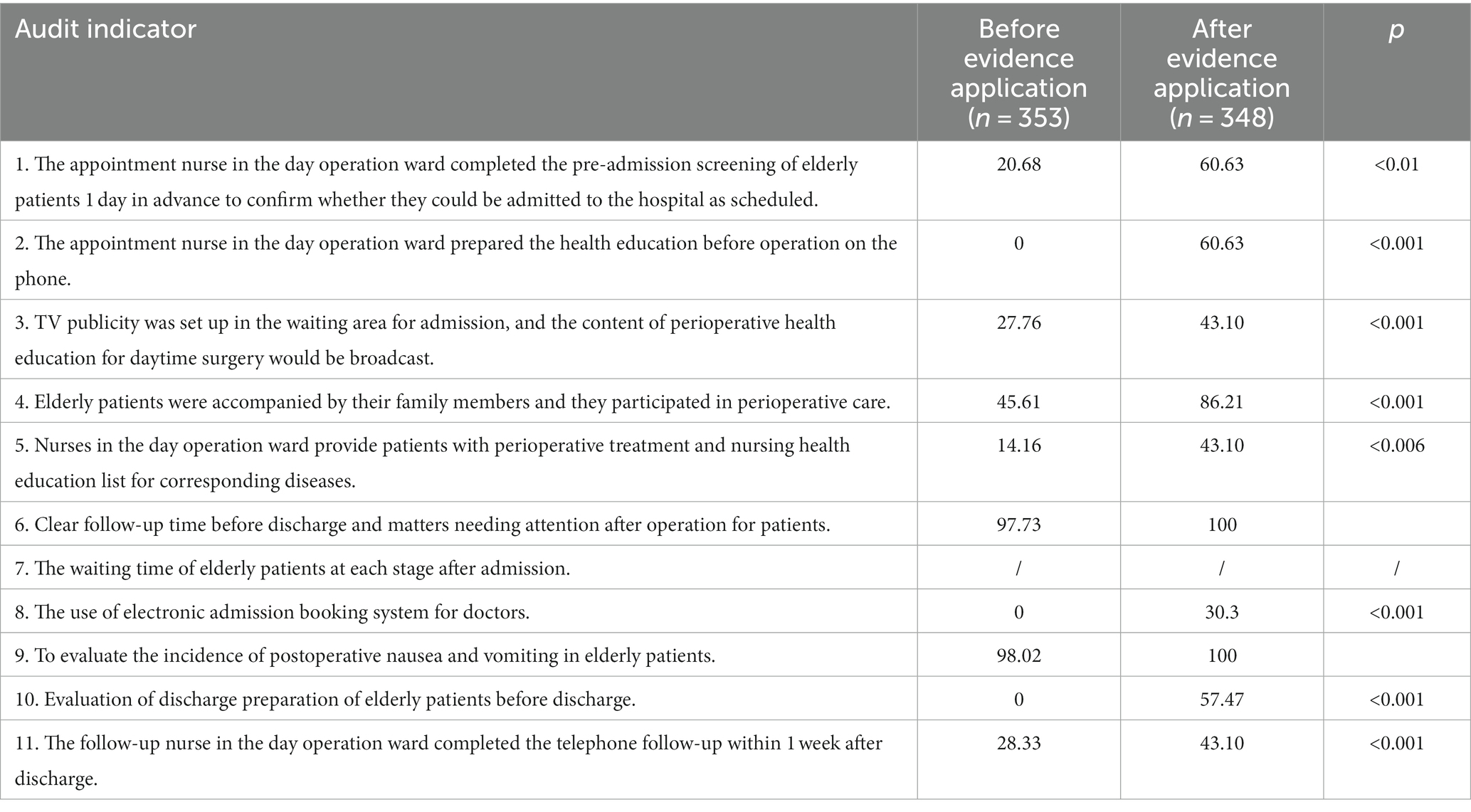
Table 3. Comparison of perioperative management audit indicators of elderly day surgery before and after evidence-based practice (%).
Before the evidence-based practice, there were 353 elderly patients, including 234 men and 119 women, and after the evidence-based practice, there were 348 elderly patients, including 247 men and 101 females. There was no significant difference in baseline before and after evidence-based practice (p > 0.05), as shown in Table 4. After evidence-based practice, the length of waiting for admission and waiting for operation and returning to the ward to discharge in elderly patients were shorter than those before practice, and the difference was statistically significant (all p < 0.05).
Under the premise of emphasizing the coexistence of efficiency and patient safety, daytime surgery can continuously improve the delay of perioperative management, shorten the operation waiting time of elderly patients, and improve the sense of medical experience of patients (29). The sense of experience of patients has a direct impact on their satisfaction and recommendation of hospital services (30). In this study, through evidence-based practice, the perioperative process of day surgery and medical satisfaction for elderly patients are further improved. During the outpatient visit, clinicians often evaluate the actual condition of elderly patients and judge whether it is suitable for daytime surgery. In this process, the time and channels for elderly patients and their families to receive information related to daytime surgery are insufficient, which can easily lead to many feelings of uncertainty and conflict about disease treatment, hospitalization environment, and medical process after admission. According to the evidence content of perioperative management of elderly patients undergoing day surgery, it combines preoperative health education and second confirmation of operation time of patients moving forward, prompting the admission time of patients in advance, improving the preoperative examination, estimating the length of stay in hospital, and suggesting reliable family members to accompany (31, 32). The results of this study show that after evidence-based practice, the implementation of indicators 1, 2, and 4 has been significantly improved. At the same time, the video of perioperative health education was played by rolling in the special waiting area of the daytime operation ward, and the individual perioperative health education was provided by responsible nurses; the result shows that the implementation of indicators 3 and 5 has improved in the review.
The perioperative management of day surgery for the elderly is the result of multi-disciplinary cooperation and multi-sector cooperation on the same public platform (33, 34). Under the policy guidance of the medical administration department, we jointly present the perioperative management mode and content of evidence-based day surgery. Through the introduction of evidence-based evidence, this study promotes the mastery and application of the latest evidence for perioperative management of day surgery in the elderly patients. Doctors and nurses gradually use the “daytime operation management system” to integrate electronic appointment information of patients and confirm the time of admission, the type of disease, the type of operation, and whether the preoperative anesthetic evaluation has been completed. At the management level, the latest best evidence content is strictly practiced in clinical practice, and the homogeneity of platform management is improved, which ensures the quality of day operation management for elderly patients and improves the homogeneity and standardization of day surgical service quality.
Day surgery has been paid more and more attention by researchers in the field of medical and healthcare year by year. The particularity of the elderly population is increasingly prominent in the day surgery medical group, which not only meets the needs of patients but also meets the requirements of the construction of a general hospital day operation platform, so there is an urgent need for the development and application of intelligent management platform (35–37). In order to further optimize the allocation of medical resources, daytime surgery management from extensive to fine transformation improves the level of medical services and advocates the creation of intelligent information on big data platforms (38, 39). Based on the background of the development of deep aging, the evidence of perioperative management in geriatric day operation ward is also the basic framework starting point for the development and construction of an intelligent management platform, in order to make patients get more convenient and effective medical experience and promote the development of high-quality daytime surgery.
Day operation is a type of operation mode that helps the patient to get out of the hospital in a short time. This model can not only reduce the total cost of patients but also improve the utilization rate and work efficiency of medical resources, and it is an efficient and convenient health service model. Although day surgery has been highly concerned and recognized by the medical community, and various medical institutions have made great efforts to carry out day surgery under the call of national policy in China, there are still some problems. It has been recognized by the vast majority of patients, but it is facing many challenges in developing countries, especially the limited coverage of medical insurance and the lack of follow-up services (40, 41). The mode of day operation ward is in the stage of development, and the speed of development is different in different areas (42). The nursing management of daytime surgery is quite different from that of the general ward, which needs to be adjusted according to the characteristics of daytime. This study has summarized the current findings of the literature, in order to provide a reference for our country to continuously improve the nursing management of daytime surgery, maximize the rational use and allocation of medical resources, deepen the concept of high-quality nursing service, and improve the satisfaction of the society, government, patients, and medical staff, to contribute to the reform of the medical and health system.
In conclusion, the best evidence of perioperative management of elderly day surgery patients was introduced into clinical practice in this study, and the standardized content of perioperative management was established by implementing the perioperative management process of day surgery. With relevant training for medical staff, promotion of daytime operation management system, and improvement of awareness and compliance of perioperative management evidence of medical staff for elderly patients, the nursing quality of daytime surgery has been improved greatly. However, due to the multi-team cooperation in this study, there is still insufficient use of electronic assessment tools and insufficient discharge readiness evaluation, which need to be solved through evidence-based practice in the later stage. In addition, this study is based on the clinical scenario, and the conclusions are limited; it is suggested that the validity of the evidence should be further verified by multicenter studies with a larger sample size in future investigations.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
This study had obtained the approval from the ethical committee of our hospital with approval number: 2021K010. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
MW: Investigation, Methodology, Writing – original draft. LX: Investigation, Writing – review & editing. LZ: Investigation, Writing – original draft, Writing – review & editing. YX: Investigation, Writing – original draft. YC: Investigation, Writing – original draft. XZ: Writing – original draft. LC: Investigation, Writing – original draft.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Fudan University-Fosun Nursing Research Project (No. FNF202116), Evidence Transformation and Clinical Application Program of evidence-based Nursing Center of Fudan University (No. Fudanebn202017), and Project established by Shanghai Science and Technology Commission (No. 16411951200).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
CASA, China Ambulatory Surgery Alliance; AGREE, Appraisal of Guidelines for Research and Evaluation; JBI, Joanna Briggs Institute.
1. Ellison, EC, Pawlik, TM, Way, DP, Satiani, B, and Williams, TE. The impact of the aging population and incidence of cancer on future projections of general surgical workforce needs. Surgery. (2018) 163:553–9. doi: 10.1016/j.surg.2017.09.035
2. Etzioni, DA, Liu, JH, Maggard, MA, and Ko, CY. The aging population and its impact on the surgery workforce. Ann Surg. (2003) 238:170–7. doi: 10.1097/01.SLA.0000081085.98792.3d
3. Xin, L, Buyue, Q, Rong, W, Lei, X, and Longfei, G. Practice of closed-loop remodeling of full procedure in daytime surgery. Chinese J Health Inform Manag. (2021) 56:530–5.
4. Liu, H. Current situation and related research progress of nursing safety management in daytime surgery. China Urban Rural Enterprise Health. (2021) 252:65–9.
5. Udo, IA, and Eyo, CS. Day surgery: are we transferring the burden of care? Niger J Clin Pract. (2014) 17:502–5. doi: 10.4103/1119-3077.134052
6. Zhuang, M, Cao, J, Cui, M, Yuan, S, Liu, Q, and Fan, W. Evaluation of day care versus inpatient cataract surgery performed at a Jiangsu public tertiary a hospital. BMC Ophthalmol. (2018) 18:134. doi: 10.1186/s12886-018-0800-8
7. Nivoche, Y, Leculee, R, Dahmani, S, Lucas, MM, Wodey, E, and Courreges, P. One day anaesthesia in children: a survey among the French speaking paediatric anaesthesiologists association (Adarpef). Ann Fr Anesth Reanim. (2010) 29:554–6. doi: 10.1016/j.annfar.2010.05.018
8. Dreuning, KM, Haverman, L, Bosschieter, PF, van Looij, MA, van Heurn, LE, and Derikx, JP. Age-specific and family-centered information modalities to prepare children at home for day-care surgery. J Pediatr Surg. (2023) 58:510–7. doi: 10.1016/j.jpedsurg.2022.08.023
9. de Luca, U, Mangia, G, Tesoro, S, Martino, A, Sammartino, M, and Calisti, A. Guidelines on pediatric day surgery of the Italian societies of pediatric surgery (SICP) and pediatric anesthesiology (SARNePI). Ital J Pediatr. (2018) 44:35. doi: 10.1186/s13052-018-0473-1
10. Maciejewski, D. Committee on ambulatory anaesthesia PSoA, intensive T: guidelines for system and anaesthesia organisation in short stay surgery (ambulatory anaesthesia, anaesthesia in day case surgery). Anaesthesiol Intensive Ther. (2013) 45:190–9. doi: 10.5603/AIT.2013.0038
11. Lu, X, Lin, J, and Feng, J. Research progress of nursing management in daytime surgery. Nurs Res. (2018) 32:5–7.
12. Jing, W, Zhennan, K, and Changyan, X. Related factors of early incision pain in elderly patients with inguinal hernia treated by day surgery in a hospital. Chin J Gerontol. (2017) 37:3–7.
13. Bailey, CR, Ahuja, M, Bartholomew, K, Bew, S, Forbes, L, Lipp, A, et al. Guidelines for day-case surgery 2019: guidelines from the association of anaesthetists and the British Association of day surgery. Anaesthesia. (2019) 74:778–92. doi: 10.1111/anae.14639
14. Liu, W. Diseases NCRCfG, cooperation CAfDs: clinical practice guide for rectoanal day surgery. Chin J Gastrointes Surg. (2019) 22:1001–11.
15. Ma, Z, Huang, Y, and Gu, X. Expert consensus on anesthesia management in adult day surgery for accelerated rehabilitation surgery. J Concord Med. (2019) 10:562–9.
16. Ouyang, W, Li, T, and Zhou, X. Consensus of anesthesia experts in daytime surgery. J Clin Anesthesiol. (2016) 32:1017–22.
17. Tang, Z, Dai, Y, and Huang, Y. Expert consensus on the standardized procedure of day surgery in biliary tract surgery. Chinese J Surgery. (2018) 56:321–7.
18. Zhang, Z, Chen, J, and Tang, J. Alliance CDsC, surgery CJohaaW, association haaWSCoSBoCP: expert consensus on standardized procedure for day operation of inguinal hernia. Chinese J Hernia Abdominal Wall Surgery. (2019) 13:193–7.
24. Brouwers, MC, Kho, ME, Browman, GP, Burgers, JS, Cluzeau, F, Feder, G, et al. AGREE II: advancing guideline development, reporting, and evaluation in health care. Prev Med. (2010) 51:421–4. doi: 10.1016/j.ypmed.2010.08.005
25. Hongli, C, Ge, Z, and Qing, Z. Evaluation and analysis of literature quality agreed by domestic nursing experts in recent 10 years. Nurs Manag China. (2020) 20:399–406.
26. Youyi, L, Jiachang, G, and Ami, L. Reliability and validity of Chinese version of hospital discharge readiness scale. J Nurs. (2014) 61:56–65.
27. Liu, J. Study on the practice level and influencing factors of evidence-based nursing of clinical nurses. Zhengzhou: Henan University (2014).
28. Li, Q, Hu, J, and Yu, L. Relationship between evidence-based practice ability of nurses and leadership in evidence transformation of head nurses. PLA J Nurs. (2019) 36:4–8.
29. Chaidas, K, and Winterborn, C. Oxford guidelines for adult day-case tonsillectomy. J Perioper Pract. (2023) 33:9–14. doi: 10.1177/17504589211031067
30. Yan, D, and Mingjun, H. Practice of nursing management in daytime surgery. Nurs Manag China. (2021) 21:6–9.
31. Berry, A, Houchen-Wolloff, L, Crane, N, Townshend, D, Clayton, R, and Mangwani, J. Perceived barriers and facilitators of day-case surgery for major foot and ankle procedures? A cross-sectional survey of United Kingdom surgeons. World J Orthop. (2023) 14:248–59. doi: 10.5312/wjo.v14.i4.248
32. Turner, M, Craighead, F, and MacKenzie, JD. Aujayeb a: day case local anaesthetic thoracoscopy: experience from 2 district general hospitals in the United Kingdom. Med Sci. (2023) 11:23. doi: 10.3390/medsci11010023
33. Mitchell, M. Guidance for the psychological care of day case surgery patients. Nurs Stand. (2002) 16:41–3; quiz 44. doi: 10.7748/ns.16.40.41.s3
34. Lawrence, D, Fedorowicz, Z, and van Zuuren, EJ. Day care versus in-patient surgery for age-related cataract. Cochrane Database Syst Rev. (2015) 2015:CD004242. doi: 10.1002/14651858.CD004242.pub5
35. Gottlieb, O. Anesthesia information management systems in the ambulatory setting: benefits and challenges. Anesthesiol Clin. (2014) 32:559–76. doi: 10.1016/j.anclin.2014.02.019
36. Jensen, CB, Troelsen, A, Foss, NB, Nielsen, CS, Lindberg-Larsen, M, and Gromov, K. 10-year evolution of day-case hip and knee arthroplasty: a Danish nationwide register study of 166,833 procedures from 2010 to 2020. Acta Orthop. (2023) 94:178–84. doi: 10.2340/17453674.2023.11961
37. Guihua, Z, Ning, P, and Yun, W. Centralized treatment of daytime surgery under decentralized management mode. China Health Standards Manag. (2017) 19:3–6.
38. Wei, N, Baldock, TE, Elamin-Ahmed, H, Walshaw, T, Walker, R, Trompeter, A, et al. ORthopaedic trauma hospital outcomes – patient operative delays (ORTHOPOD) study: the management of day-case orthopaedic trauma in the United Kingdom. Injury. (2023) 54:1588–94. doi: 10.1016/j.injury.2023.03.032
39. Cooper, DM, Bhuskute, N, Hepworth, C, and Walsh, G. The economic impact of a pilot digital day-case pathway for knee arthroplasty in a U.K. setting. JB JS Open Access. (2023) 8:e22.00051. doi: 10.2106/JBJS.OA.22.00051
40. Wu, S, Luo, M, and Chen, R. Hip and knee replacement day surgery center work efficiency improvement strategy and enlightenment. Chinese J Pract Nurs. (2022) 38:4–7.
41. Ying, Y, and Wei, D. Analysis and exploration of the effectiveness of day surgery. Modern Hosp Manag. (2022) 20:4–6.
Keywords: evidence, practice, elderly, day surgery, patients, care, nursing, management
Citation: Wu M, Xia L, Zhang L, Xu Y, Cheng Y, Zhang X and Chen L (2023) Perioperative management for elderly patients undergoing day surgery: evidence-based practice for nursing care and day surgery. Front. Med. 10:1298778. doi: 10.3389/fmed.2023.1298778
Received: 22 September 2023; Accepted: 30 October 2023;
Published: 21 November 2023.
Edited by:
Vahid Rashedi, University of Social Welfare and Rehabilitation Sciences, IranReviewed by:
Ana Corte-Real, University of Coimbra, PortugalCopyright © 2023 Wu, Xia, Zhang, Xu, Cheng, Zhang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Long Chen, aGVhdmVuX2xvbmdAMTI2LmNvbQ==; Xiaoju Zhang, c2hpcmx5enhqQDEyNi5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.