- 1Department of Health Sciences, University of Catanzaro "Magna Græcia", Catanzaro, Italy
- 2FAS@UMG Research Center, Department of Health Science, School of Medicine, University of Catanzaro, Catanzaro, Italy
Background: The aim of our study was to investigate the impact of the COVID-19 pandemic on the healthcare and the disease management of patients affected by non-communicable diseases (NCDs), by exploring, specifically, the obstacles encountered in the access to healthcare services during the latest phase of the pandemic.
Methods: This cross-sectional study was carried out among subjects attending the anti-SARS-CoV2 vaccination clinic in a Teaching Hospital of Southern Italy. To be included in the study, subjects had to be affected by at least one NCD, such as diabetes, hypertension, respiratory and heart diseases, renal and liver chronic conditions, immunodeficiency disorders due to cancer, or being kidney or liver transplant recipients.
Results: Among the 553 subjects who completed the questionnaire, the 39.4% (95% IC = 35.3–43.6) experienced obstacles in the access to healthcare services in the six months prior to the enrollment. The most frequent canceled/postponed healthcare services were the visits for routine checks for NCDs (60.6, 95% IC = 53.9–67), control visits of more complex diseases as cancer or transplantation (17.3, 95% IC = 12.6–22.8), and scheduled surgery (11.5, 95% IC = 7.7–16.4). The patients who experienced canceled/postponed healthcare services were significantly more likely to suffer from 3 or more NCDs (p = 0.042), to be diabetics (p = 0.038), to have immunodeficiency disorders (p = 0.028) and to have consulted GP at least once (p = 0.004).
Conclusion: Our results appear to be fundamental for guiding the choices of providers in order to concentrate organizational efforts to recover and reschedule missed appointments, where applicable, of the most fragile patients by virtue of age and chronic conditions.
1. Introduction
The sudden emergence of SARS-COV2, the cause of a pandemic that has led to more than 750 million confirmed cases and nearly 7 million deaths globally (1), has put a strain on the healthcare systems of countries around the world. In Italy, the law enforcement action was based on a complete lockdown during the first wave of the pandemic (March–June 2020) (2), followed by a series of more or less restrictive measures depending on the epidemiological trend of the infection, which characterized the second (November 2020–March 2021) and the third (March–April 2021) phase of the COVID-19 pandemic, up to the fourth phase characterized by a progressive easing of the restrictive measures which, starting from the end of April 2021 (3, 4), led to the end of the state of emergency in March 2022 (5).
To deal with the emergency, the reallocation of resources was required to strengthen the healthcare activities considered to be essential compared to the non-essential ones (6). Several studies have been performed to evaluate the remodulation of the access to healthcare services during the early phases of the pandemic, specifically since the start of the pandemic through December 2020. These studies have shown that, in 2020, there has been a relevant reduction of outpatient healthcare (7), primary care visits (8, 9), preventive interventions such as screening and vaccinations (7, 10, 11) and elective procedures (7, 12, 13) compared with the preceding years, and in most cases the comparison was with 2019. Instead, very poor evidence is available on the healthcare services utilization during the latest phase of the pandemic, characterized by a more sustainable management of the COVID-19, mostly attributable to the effectiveness of vaccinations, which completely changed the course of SARS-CoV2 infection in all categories of vaccinated subjects, including the frailest (14–16).
According to WHO’s 2020 Global Health Estimates (17), non-communicable diseases (NCDs) affect more people each year and are responsible for more than 70% of all deaths worldwide. The burden of NCDs will continue to grow over the coming decades, mainly due to cardiovascular diseases, with deaths rising by more than 2 million since 2000 to nearly 9 million in 2019, and to neoplastic diseases (18) with, in 2018, 18 million people in the world affected by cancer and more than 9 million deaths. Also, deaths from diabetes globally have more than double between 2000 and 2019 and account for the NCDs with the largest percentage increase of all WHO regions.
The management of NCDs, due to their chronic nature, often require repeated and prolonged interactions with the healthcare system in order to have access to pharmacological, surgical, rehabilitative therapies and regular monitoring, essential to determine if the treatment plan is on track and the patient is achieving results. Not getting the care needed often has devastating consequences for people living with NCDs. A recent meta-analysis (19) highlighted that the risk of death across the seven major cancer types (bladder, breast, colon, rectum, lung, cervix, and head and neck) would increase by 6–8% even with a delay of only 4-week in the curative treatment. Also, several studies showed an increase by up to 5-fold of the incidence of cardiovascular diseases complications as out-of-hospital cardiac arrest after the launch of emergency response measures against COVID-19 (20–22). Also, after the implementation of the lockdown, hospital admissions among diabetic patients decreased (23, 24) with a 92% increase in the average number of monthly deaths highlighted by Hernandez-Vasquez et al. (24) and a significantly higher plasma glucose and HbA1c levels than during pre-pandemic period (23).
Therefore, in the light of these considerations, the aim of our study was to investigate the impact of the COVID-19 pandemic on the healthcare and the disease management of patients affected by NCDs, by exploring, specifically, the obstacles encountered in the access to healthcare services during the latest phase of the pandemic.
2. Materials and methods
2.1. Study design and population
The survey took place from October 2021 to February 2022 in a Teaching Hospital of Southern Italy. To be included in the study, subjects had to be affected by at least one NCD, such as diabetes, hypertension, respiratory and heart diseases, renal and liver chronic conditions, immunodeficiency disorders due to cancer, or being kidney or liver transplant recipients. Patients affected by conditions managed by specific healthcare service areas, such as mental disorders, sexual, reproductive, maternal, child and adolescent health, were excluded.
All eligible subjects attending the anti-SARS-CoV2 vaccination clinic in the Teaching Hospital were asked to participate in our study. The proposal to participate in the study was made in the waiting room while the patients waited their turn. Prior to face-to-face interviews, the research team presented the aims of the study, emphasized that participation was voluntary and the anonymity of the responses and acquired written consent.
The sample size was estimated using the following equation: n = (z2 × p × q)/D2 (25) with the following assumptions: the probability of obstacles in healthcare accesses in NCDs patients was estimated to be equal to 25% (p), a value of 0.5 was chosen as the acceptable limit of precision (D) with a confidence interval of 99%(z). The value obtained was increased by 10% to take into account the non-response rate. Based on these assumptions the final sample size became 550 NCDs patients.
2.2. Survey instrument
Data were collected through a questionnaire administered to all subjects who gave their consent to participate in the study. The questionnaire consisted of three sections: in the first one, items on sociodemographic characteristics and lifestyle habits were included; in the second section, the health status was investigated and, to quantify the individual burden of disease, the age adjusted Charlson co-morbidity index was calculated for each subject. The perceived health status at the time of the interview was measured on a ten-point Likert scale for response, ranging from 0 (very poor) to 10 (excellent). In the third section the health status and the utilization of healthcare services during the six months prior to the subject’s enrollment in the study were investigated. In particular, information was collected about general practitioner (GP) and/or specialist consultations; hospital admissions; eventual obstacles in the access to healthcare services, including canceled/postponed medical consultations, follow-up visits, scheduled surgery and preventive activities. Finally, reasons for difficult access to healthcare services were investigated.
The study protocol was ratified by the Approval from the Regional Ethics Committee (ID N. 183).
2.3. Statistical analysis
Descriptive analyses were performed to illustrate demographic characteristics of participants and to determine the prevalence of the experienced obstacles in the access to healthcare services. Moreover, univariate analysis, by the appropriate test (t-test; chi-square test), and a multivariate stepwise logistic regression model were performed to determine the independent association of several characteristics with the experienced obstacles in the access to healthcare services, during the previous 6 months. The following explanatory variables were included in the model: gender (male = 0; female = 1), age (continuous), additional person in the household (none = 0; ≥1 = 1), marital status (married/cohabitant = 0; other = 1), education level (primary/secondary school = 0; high school = 1; university degree = 2), cardiovascular disease (no = 0; yes = 1), diabetes mellitus (no = 0; yes = 1), gastrointestinal diseases (no = 0; yes = 1), immunodeficiency disorders (no = 0; yes = 1), kidney disease (no = 0; yes = 1), neurological disease (no = 0; yes = 1), cancer (no = 0; yes = 1), respiratory diseases (no = 0; yes = 1), perceived health status (poor/fair/good = 0; very good/excellent = 1), number of chronic diseases (<3 = 0; ≥3 = 1), consultation to GP (none = 0; at least one = 1) and to the specialists (none = 0; at least one = 1) in the previous six months. Adjusted Odds Ratio (OR) and 95% Confidence Intervals (95% CI) were calculated. A p value ≤0.05 was considered statistically significant.
STATA version 16 statistical software package (2016, Stata Corp, LP, College Station, Tx, United States) was used to conduct all data analyses.
3. Results
A total of 553 subjects completed the questionnaire, with an 87% response rate. Selected characteristics of the sample are reported in Table 1. The mean age was 66.8 years (± 12.1 SD); 45.6% (95% CI 41.4–49.8) of respondents declared to suffer from three or more NCDs and the most prevalent were cardiovascular illness, including hypertension and heart diseases (77.4, 95% CI 73.7–80.8); cancer (28.2, 95% CI 24.5–32.2) and diabetes (25.5, 95% CI 21.9–29.3). Primary and secondary immunodeficiency disorders due to transplantation, asplenia and immunosuppressive medications were reported by 18.6% (95% CI 15.3–21.9) of respondents. Moreover, when patients were asked to indicate in a 10-point Likert-type scale their perceived health status, 39.2% (95% CI 34.4–42.7) evaluated their health in general as very good or excellent.
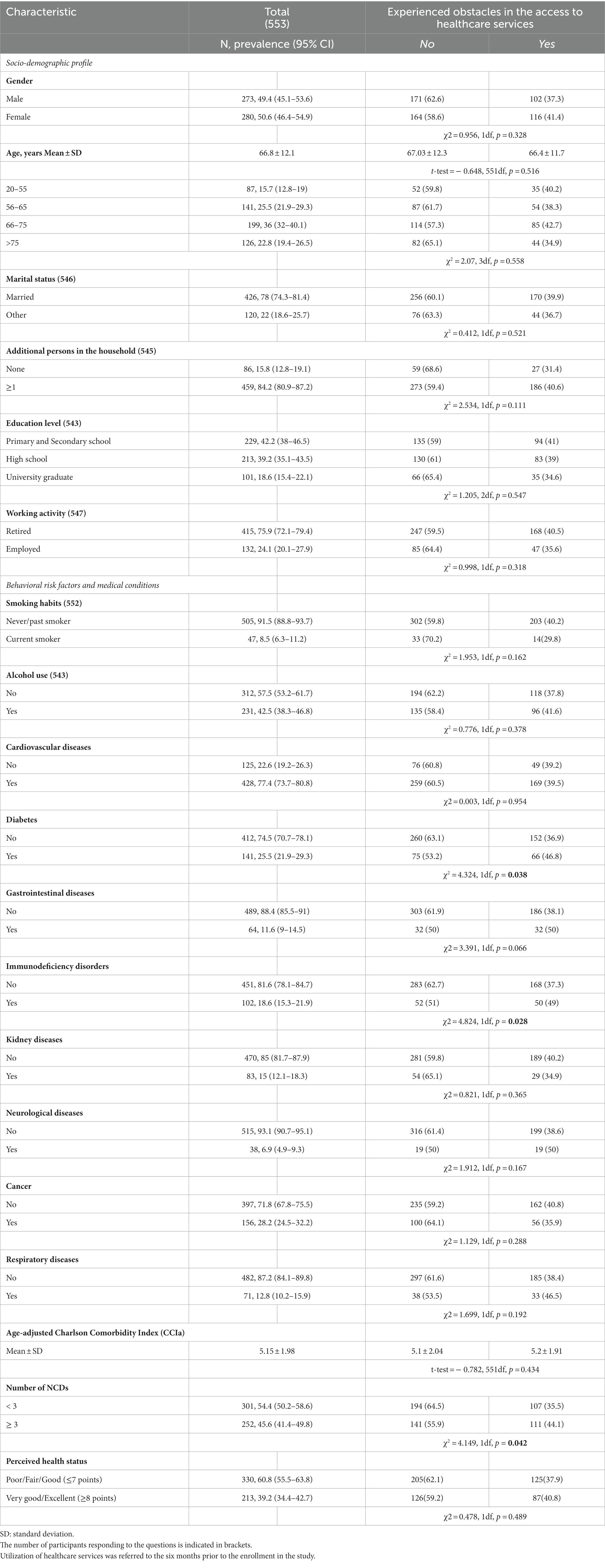
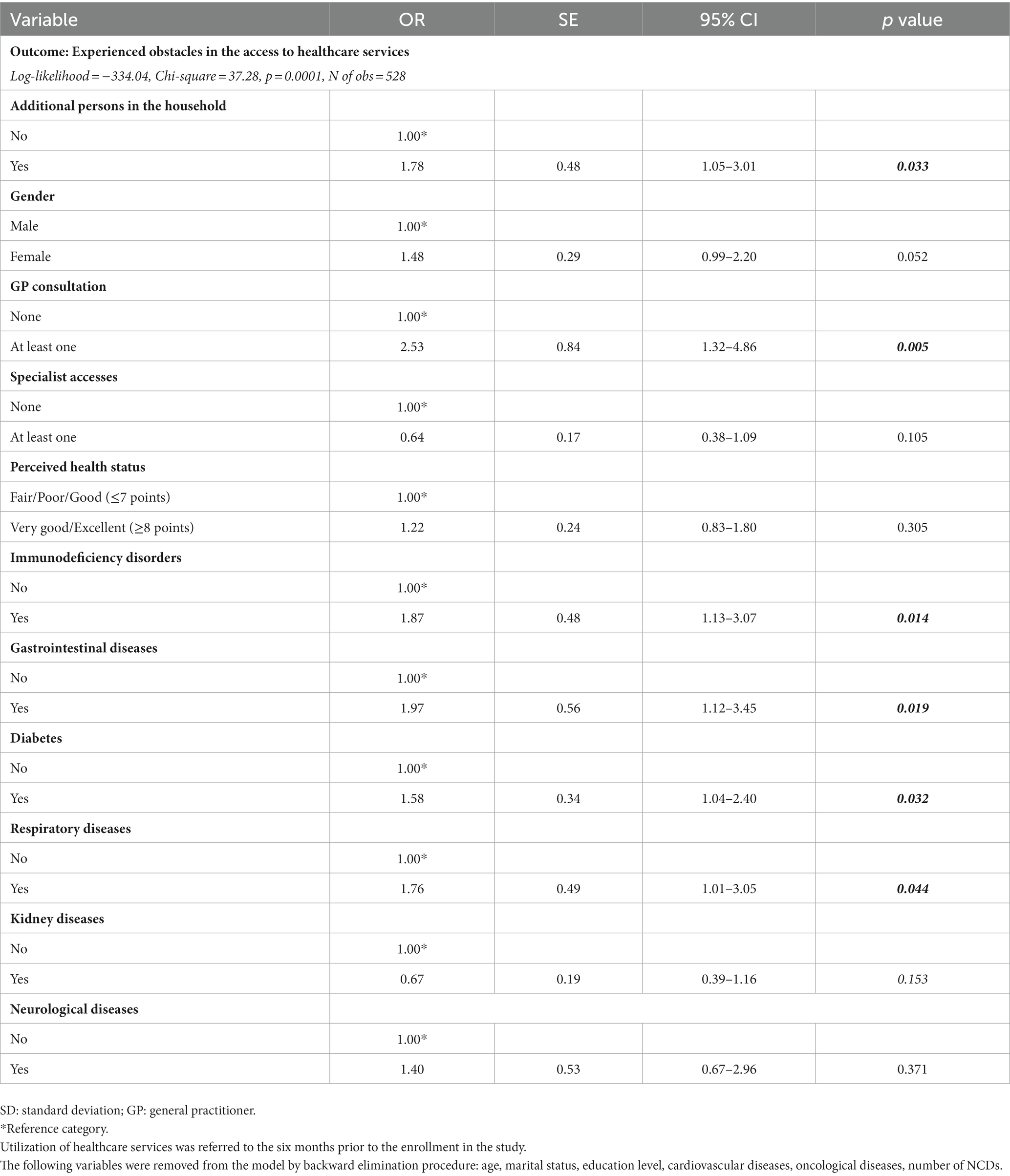
Table 1. Demographics and baseline characteristics of the study population and their association with prevalence of the experienced obstacles in the access to healthcare services during the latest phase of the COVID-19 pandemic.
The respondents’ pattern of utilization of healthcare services during the latest phase of the COVID-19 pandemic (Table 2) showed that, in the previous six months before enrollment in the study, almost 90% of the subjects had consulted GP at least once, and the mean reasons were medical prescriptions (77, 95% CI 73–80.6) and routine checks for NCDs (22%), while preventive interventions were required by only 1% of the subjects. Among the 85.5% (95% CI 82.3–88.4) of respondents that reported at least one specialist visit, routine checks for NCDs were the main declared reason (95.4, 95% CI 93–97.1). One third of respondents (33.1, 95% CI 29.2–37.2) were hospitalized, mainly for surgery (45.9, 95% CI 38.5–53.4) or for the occurrence of new symptoms (29.5, 95% CI 23–36.7). Slightly less than half (42.3, 95% CI 32.1–54.1) of the performed surgical interventions were severe/urgent, because they were carried out on cancer patients (54.5, 95% CI 38.1–72.1) or in patients in critical conditions (22.8, 95% CI 10.1–39.2) or because they were transplants (22.7, 95% CI 10.1–39.2) (data not shown).
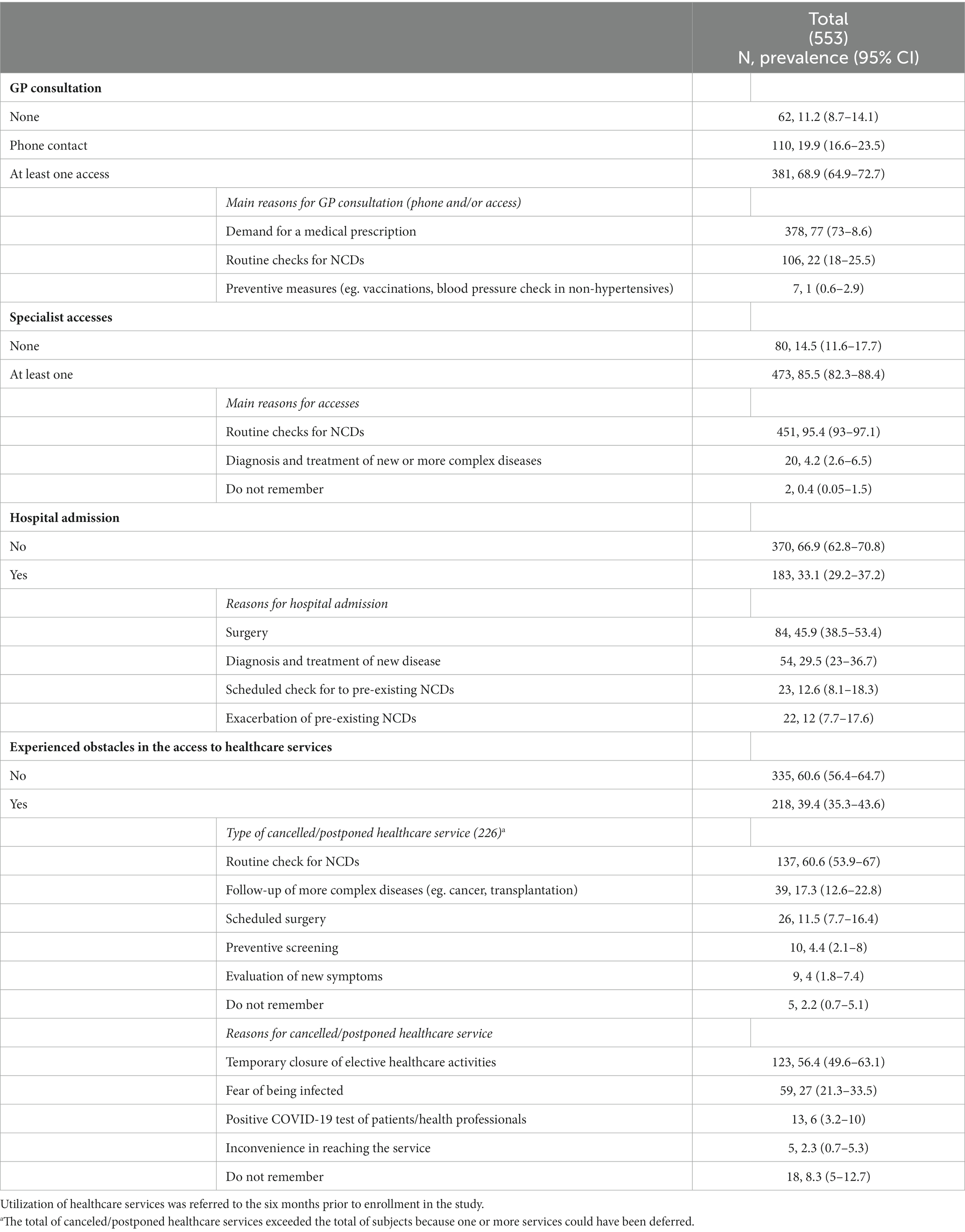
Table 2. Characteristics of the utilization of healthcare services during the latest phase of the COVID-19 pandemic by patients with NCDs.
Overall, 39.4% (95% CI 35.3–43.6) of the patients experienced obstacles in the access to healthcare services in the six months prior to the enrollment in the study. The most frequent canceled/postponed healthcare services were the visits for routine checks for NCDs (60.6, 95% CI 53.9–67), followed by control visits of more complex diseases as cancer or transplantation (17.3, 95% CI 12.6–22.8) and scheduled surgery (11.5, 95% CI 7.7–16.4) (Figure 1) and, of these, more than a quarter (26.5, 95% CI 11.6–47.8) were not performed (data not shown). Preventive interventions and the evaluation of the occurrence of new symptoms accounted for lower than 10% of the canceled healthcare services. The temporary closure of elective healthcare activities was the most common reason, reported by 56.4% (95% CI 49.6–63.1) of the patients that had experienced canceled or postponed healthcare services. In the Figure 2 were reported the percentages of patients who experienced obstacles in the access to healthcare services according to chronic disease suffered (Figure 2).
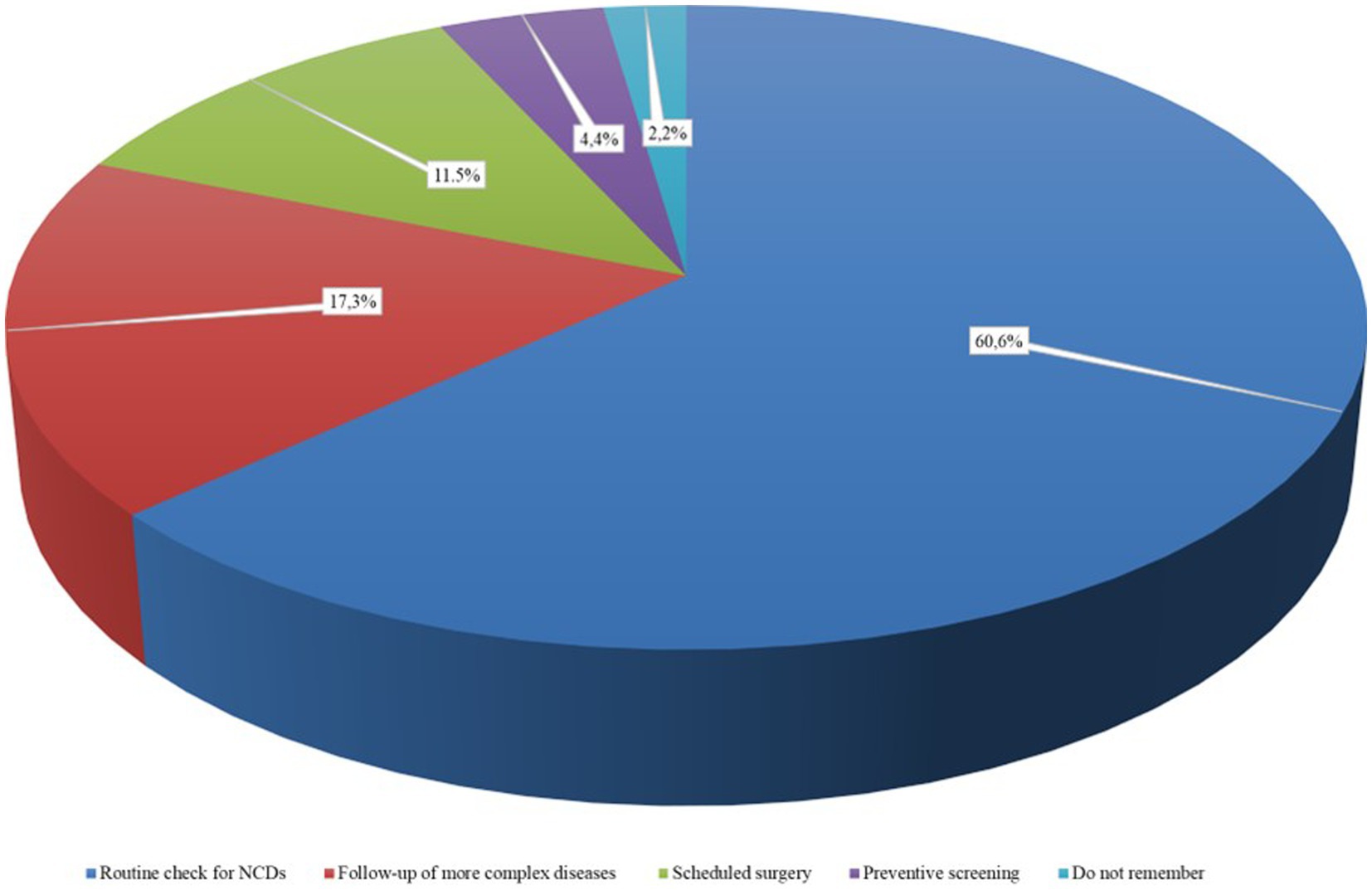
Figure 1. Types of canceled/posponed healthcare services during the latest phase of the COVID-19 pandemic.
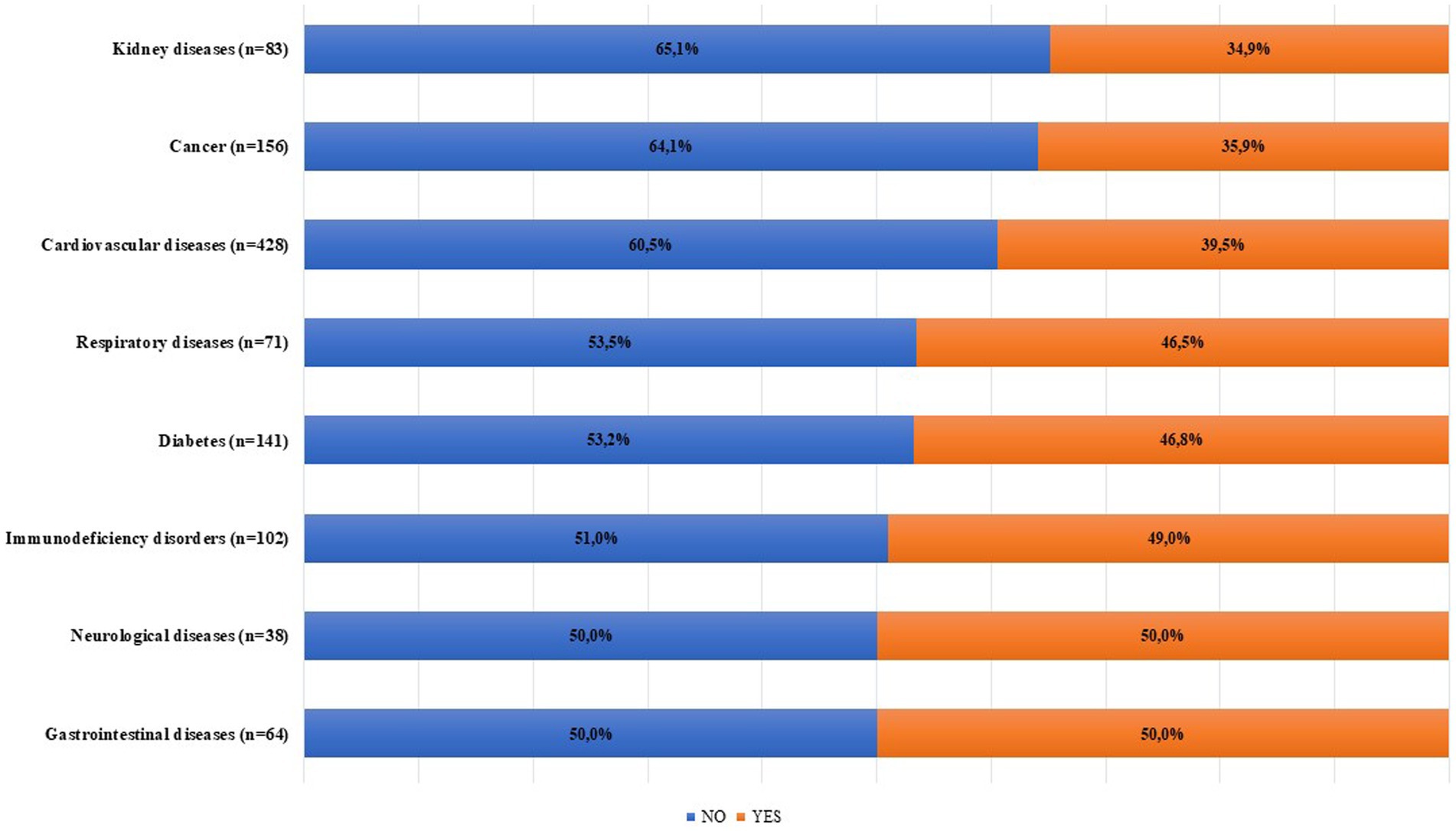
Figure 2. Experienced obstacles in the access to healthcare services according to NCDs during the latest phase of the COVID-19 pandemic.
Univariate analysis (Table 1) highlighted that patients who experienced canceled/postponed healthcare services in the latest phase of the COVID-19 pandemic were significantly more likely to suffer from 3 or more NCDs (χ2 = 4.149, p = 0.042), to be diabetics (χ2 = 4.324, p = 0.038), to have immunodeficiency disorders (χ2 = 4.824, p = 0.028) and to have consulted GP at least once (χ2 = 8.292, p = 0.004; data not shown), while no significant differences were found according to the socio-demographic profile or other NCDs.
When the multivariate analysis was performed, the results did not substantially change, with the exception of patients not living alone and those affected by respiratory diseases who had significantly higher odds of experiencing canceled/postponed healthcare services (Table 3).
4. Discussion
It is well known that severity and mortality associated to SARS-CoV2 infections increase dramatically with older age (>65 years), and in subjects suffering with pre-existing NCDs (26, 27). Many people, especially those in the above mentioned high-risks groups had experienced obstacles in the access to healthcare services to obtain treatment for ongoing conditions during the COVD-19 pandemic. Although this result is reasonable in the early phase of the pandemic, because of the prioritization of healthcare services against SARS-CoV2 infections, it is less acceptable in the latest phase of the pandemic. Indeed, the most remarkable result from this study revealed the persistent reduction of the elective healthcare activities, with almost 40% of patients with NCDs having experienced canceled/postponed healthcare services during this period.
To the best of our knowledge this investigation is the first offering an overview of how frail patients continued to experience obstacles in the access to healthcare services even when infection control measures, as mandatory use of protective masks, physical distancing, quarantine measures, had become less stringent and the effectiveness of the vaccination campaigns in the prevention of the most severe clinical outcomes had become clearly evident.
In this study, two main obstacles to access to healthcare services during the latest phase of the pandemic have emerged: the persistence of temporary closure of elective healthcare activities, and a specific patients’ choice due to the fear of being infected. Regarding the first aspect, as the more recent WHO interim report (28) has suggested, worldwide healthcare systems have not yet overcome the acute phase of the pandemic. Despite lower direct mortality and hospitalization than in the initial phase of the pandemic, the SARS-CoV2 infection continues to disrupt essential healthcare services in almost every country across the world (29). It is reasonable to hypothesize that the lack of resources, in terms of availability of health workers, drugs, vaccines, except for the anti-SARS-CoV2 ones, but also of facility infrastructure, space capabilities and diagnostic equipment could, at least in part, explain the persistent dearth of elective healthcare services.
The Italian National Healthcare System (NHS), as well as that of several other Organization for Economic Co-operation and Development (OECD) countries, has implemented the waiting list model, based on prioritization criteria according to clinical conditions and professional judgment, to manage the population healthcare requests (30). A non-secondary problem in the current healthcare landscape is represented by the need to make up for the delay accumulated in the management of waiting lists during the complete lockdown phase. Currently, indeed, the healthcare services requests add up to those planned but not carried out during the pandemic emergency phase and the subjects who most suffer to wait longer are those with worse health status, as recently reported by Brito Fernandes et al. (31). Therefore, obstacles experienced in the latest phase of the pandemic could be the consequences of pre-existing healthcare systems problems that have been exacerbated by the pandemic. Indeed, across all OECD countries in 2019, spending on prevention accounted for only 2.7% of the total health spending; healthcare systems were understaffed with an average of 12.4 of doctors and nurses per 1,000 people, and they suffered from underinvestment with insufficient physical infrastructure and occupancy rate over 90% for acute care beds or countries with less than half the mean expected number of adult intensive care beds (32, 33).
Similarly, to previous studies (34–36), almost 27% of NCDs patients avoided/delayed healthcare services due to the fear of being infected with SARS-CoV2, and this attitude was more frequent in patients with multiple medical conditions compared to those with a lower comorbidity burden (37). This is of particular concern, as timely interventions for these chronic conditions could reduce morbidity and mortality while, conversely, delay in healthcare access may adversely affect evolution of chronic conditions with potentially lasting consequences even after the pandemic.
During the earlier phases of the pandemic, self-management behaviors were encouraged among NCDs patients (38–40). Indeed, the self-management of interventions such as physical activity, diet, pharmacological treatment, monitoring of symptoms, is recognized as a promising measure, capable of improving the ability of NCDs patients in the control of their chronic disease, and resulting in the saving of healthcare resources and the improvement of clinical outcomes, however, despite a vast literature on this topic, there is a paucity of high-quality evidence showing improved outcomes for NCDs patients as a result of the implementation of self-management behaviors (40–42). It is plausible to hypothesize that NCDs patients continued to strictly adhere to self-management behaviors also in the latest phase of the pandemic, so delaying/avoiding healthcare services access. Indeed, as highlighted by the results of the study, diabetic patients, that represent the more routinely trained category in the self-management behaviors (43) and that during the pandemic have substantially increased self-management practices (38, 39, 44), had significantly higher odds of experiencing canceled/postponed healthcare services in respect to non-diabetics patients.
The finding that patients not living alone were more likely to experience canceled/postponed healthcare services is in line with previous studies, which have demonstrated that loneliness is an independent determinant of healthcare services utilization regardless of the subject’s health status (45), and that the physician-patient relationship could be a way to get not only medical care, but social support as well (46). According to Arreskov et al. (47), the role of the GP remains unique in terms of opportunities to establish a stable and close doctor-patient relationship and, above all, to ensure an individualized approach, especially in subjects with chronic and complex health problems. Therefore, it is not surprising our result that cancelation/postposition of the access to healthcare services were carried out more significantly by respondents which have consulted the GP at least one time in the study period.
It is essential to read the findings from this study considering the following possible limitations. First of all, the data were self-reported by patients and, due to the potential recall bias, it could represent a problem in terms of overestimates or underestimates of experienced obstacles in the access to healthcare services. Even though the period in question was limited to the previous 6 months only. Second, among the information collected, it was not asked whether the specialist visits were paid or carried out by public specialists, but this limit does not affect the results of the study which did not have among the objectives of evaluating the use, by patients, of paid visits to obtain healthcare services more quickly. Third, results must be interpreted under the cross-sectional point of view, taking into account its limitations in terms of capability to detect cause-effect relationship. Finally, our study involved only one Italian region, which might not represent all NCDs patients in Italy. However, we are confident the results of the study may be generalized at least to the Southern Italy regions.
5. Conclusion
Despite its limitations, this study provides important insights into how the COVID-19 pandemic continues to impact NCDs patients even in its latest and less aggressive phase. If patients with NCDs continue to be hindered in accessing health care services to manage chronic conditions, receive routine immunizations, or diagnose new conditions early, the consequences will be irreparable for the most frail patients (36). It therefore appears essential to provide chronic patients with correct information on the real risks associated with SARS-CoV2 infection with respect to those of non-treatment of the chronic pathologies presented or the onset of new symptoms. Finally, these results appear to be fundamental for guiding the choices of providers in order to concentrate organizational efforts to recover and reschedule missed appointments, where applicable, of the most fragile patients by virtue of age and chronic conditions.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Regional Ethics Committee (Calabria Region). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
CS: Conceptualization, Investigation, Supervision, Data curation, Formal analysis, Writing – original draft. RP: Data curation, Formal analysis, Investigation, Writing – original draft. MM: Data curation, Investigation, Writing – original draft, Software. CP: Investigation, Conceptualization, Methodology, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. WHO Health Emergency Coronavirus (COVID19) Dashboard . (n.d.). Available at https://covid19.who.int/ (Last access February 28, 2023).
2. Decreto-legge del . Misure urgenti per la graduale ripresa delle attività economiche e sociali nel rispetto delle esigenze di contenimento della diffusione dell'epidemia da COVID-19. Gazzetta Ufficiale n. 96 del 22 aprile 2021. (n.d.). Available at https://www.gazzettaufficiale.it/eli/id/2021/04/22/21G00064/sg (Last access February 28, 2023).
3. Decreto-legge del . (n.d.) 18 maggio 2021, n. 65 Misure urgenti relative all'emergenza epidemiologica da COVID-19. GU n.117 del 18-5-2021. Available at https://www.gazzettaufficiale.it/eli/gu/2021/05/18/117/sg/pdf (Last access February 28, 2023).
4. Decreto-legge del 23 luglio 2021, n. 105 Misure urgenti per fronteggiare l'emergenza epidemiologica da COVID-19 e per l'esercizio in sicurezza di attività sociali ed economiche. GU n.175 del 23-7-2021. Available at https://www.gazzettaufficiale.it/eli/gu/2021/07/23/175/sg/pdf (Last access February 28, 2023).
5. Decreto-legge del 24 marzo 2022, n. 24. Disposizioni urgenti per il superamento delle misure di contrasto alla diffusione dell'epidemia da COVID-19, in conseguenza della cessazione dello stato di emergenza. G.U. Serie Generale, n. 70 del 24 marzo 2022. Available at https://www.gazzettaufficiale.it/eli/gu/2022/03/24/70/sg/pdf (Last access February 28, 2023).
6. World Health Organization . Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, (2020). Available at https://apps.who.int/iris/handle/10665/334048 (Last access February 28, 2023).
7. Whaley, CM , Pera, MF , Cantor, J , Chang, J , Velasco, J , Hagg, HK, et al. Changes in health services use among commercially insured US populations during the COVID-19 pandemic. JAMA Netw Open. (2020) 3:e2024984. doi: 10.1001/jamanetworkopen.2020.24984
8. Alexander, GC , Tajanlangit, M , Heyward, J , Mansour, O , Qato, DM , and Stafford, RS . Use and content of primary care office-based vs telemedicine care visits during the COVID-19 pandemic in the US. JAMA Netw Open. (2020) 3:e2021476. doi: 10.1001/jamanetworkopen.2020.21476
9. Sato, K , Mano, T , Niimi, Y , Iwata, A , Toda, T , and Iwatsubo, T . The impact of COVID-19 pandemic on the utilization of ambulatory care for patients with chronic neurological diseases in Japan: evaluation of an administrative claims database. Biosci Trends. (2021) 15:219–30. doi: 10.5582/bst.2021.01194
10. Siedner, MJ , Kraemer, JD , Meyer, MJ , Harling, G , Mngomezulu, T , Gabela, P, et al. Access to primary healthcare during lockdown measures for COVID-19 in rural South Africa: an interrupted time series analysis. BMJ Open. (2020) 10:e043763. doi: 10.1136/bmjopen-2020-043763
11. Song, H , Bergman, A , Chen, AT , Ellis, D , David, G , Friedman, AB, et al. Disruptions in preventive care: mammograms during the COVID-19 pandemic. Health Serv Res. (2021) 56:95–101. doi: 10.1111/1475-6773.13596
12. Kute, VB , Gupta, A , Patel, HV , Engineer, DP , Banerjee, S , Rizvi, SJ, et al. The impact of COVID-19 pandemic on nephrology and transplant services and clinical training in India. Exp Clin Transplant. (2021) 19:651–8. doi: 10.6002/ect.2021.0018
13. Morris, EJA , Goldacre, R , Spata, E , Mafham, M , Finan, PJ , Shelton, J, et al. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: a population-based study. Lancet Gastroenterol Hepatol. (2021) 6:199–208. doi: 10.1016/S2468-1253(21)00005-4
14. Luxi, N , Giovanazzi, A , Capuano, A , Crisafulli, S , Cutroneo, PM , Fantini, MP, et al. COVID-19 vaccination in pregnancy, paediatrics, immunocompromised patients, and persons with history of allergy or prior SARS-CoV-2 infection: overview of current recommendations and pre- and post-marketing evidence for vaccine efficacy and safety. Drug Saf. (2021) 44:1247–69. doi: 10.1007/s40264-021-01131-6
15. Papadopoli, R , De Sarro, C , Palleria, C , Gallelli, L , Pileggi, C , and De Sarro, G . Serological response to SARS-CoV-2 messenger RNA vaccine: real-world evidence from Italian adult population. Vaccine. (2022) 9:1494. doi: 10.3390/vaccines9121494
16. Caglioti, A , Rania, V , Vocca, C , Marcianò, G , Arcidiacono, V , Catarisano, L, et al. Effectiveness and safety of anti SARS-CoV-2 vaccination in transplant patients treated with immunosuppressants: a real-world pilot study with a 1-year follow-up. Appl Sci. (2022) 12:6103. doi: 10.3390/app12126103
17. World Health Organization Global Health Estimates . (2020): Deaths by cause, age, sex, by country and by region, 2000-2019. Available at: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates/ghe-leading-causes-of-death. (Last access August 16, 2023)
18. WHO report on cancer: setting priorities, investing wisely and providing care for all. Geneva: World Health Organization ; (2020). Available at: https://apps.who.int/iris/rest/bitstreams/1267643/retrieve. (Last access August 16, 2023)
19. Hanna, TP , King, WD , Thibodeau, S , Jalink, M , Paulin, GA , Harvey-Jones, E, et al. Mortality due to cancer treatment delay: systematic review and metaanalysis. BMJ. (2020) 371:m4087. doi: 10.1136/bmj.m4087
20. Lai, PH , Lancet, EA , Weiden, MD , Webber, MP , Zeig-Owens, R , Hall, CB, et al. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in new York City. JAMA Cardiol. (2020) 5:1154–63. doi: 10.1001/jamacardio.2020.2488
21. Rashid Hons, M , Gale Hons, CP , Curzen Hons, N , Ludman Hons, P , De Belder, HM , Timmis Hons, A, et al. Impact of coronavirus disease 2019 pandemic on the incidence and management of out-of-hospital cardiac arrest in patients presenting with acute myocardial infarction in England. J Am Heart Assoc. (2020) 9:e018379. doi: 10.1161/JAHA.120.018379
22. Semeraro, F , Gamberini, L , Tartaglione, M , Iarussi, B , Descovich, C , Picoco, C, et al. Out-of-hospital cardiac arrest during the COVID-19 era in Bologna: system response to preserve performances. Resuscitation. (2020) 157:1–2. doi: 10.1016/j.resuscitation.2020.09.032
23. Lui, DTW , Lee, CH , Chow, WS , Fong, CHY , Woo, YC , Lam, KSL, et al. A territory-wide study on the impact of COVID-19 on diabetes-related acute care. J Diabetes Investig. (2020) 11:1303–6. doi: 10.1111/jdi.13368
24. Hernández-Vásquez, A , Barrenechea-Pulache, A , Portocarrero-Bonifaz, A , Rojas-Roque, C , and Gamboa-Unsihuay, JE . Multimorbidity analysis and hospitalizations for diabetes before and after lockdown due to the COVID-19 pandemic in Peru. Prev Med Rep. (2022) 28:101884. doi: 10.1016/j.pmedr.2022.101884
26. O’Driscoll, M , Ribeiro Dos Santos, G , Wang, L , Cummings, DA , Azman, AS , Paireau, J, et al. Age-specific mortality and immunity patterns of SARS-CoV-2. Nature. (2021) 590:140–5. doi: 10.1038/s41586-020-2918-0
27. COVID-19 information for specific groups of people . Available at https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/index.html.
28. World Health Organization . Third round of the global pulse survey on continuity of essential health services during the COVID-19 pandemic. (2022). Available at https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2022.1 (Last access March 2, 2023).
29. Steele, MK , Couture, A , Reed, C , Iuliano, D , Whitaker, M , Fast, H, et al. Estimated number of COVID-19 infections, hospitalizations, and deaths prevented among vaccinated persons in the US, December 2020 to September 2021. JAMA Netw Open. (2022) 5:e2220385. doi: 10.1001/jamanetworkopen.2022.20385
30. Siciliani, L , Borowitz, M , and Moran, V . Waiting time policies in the health sector: what works? OECD health policy studies. Paris, France: OECD (2013).
31. Brito Fernandes, Ó , Lucevic, A , Péntek, M , Kringos, D , Klazinga, N , Gulácsi, L, et al. Self-reported waiting times for outpatient health care services in Hungary: results of a cross-sectional survey on a national representative sample. Int J Environ Res Public Health. (2021) 18:2213. doi: 10.3390/ijerph18052213
33. OECD . Ready for the next crisis? Investing in Health System Resilience. Paris: OECD Health Policy Studies, OECD Publishing (2023).
34. Czeisler, MÉ , Marynak, K , Clarke, KE , Salah, Z , Shakya, I , Thierry, JM, et al. Delay or avoidance of medical care because of COVID-19 related concerns - United States, June 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:1250–7. doi: 10.15585/mmwr.mm6936a4
35. Soares, P , Leite, A , Esteves, S , Gama, A , Laires, PA , Moniz, M, et al. Factors associated with the patient's decision to avoid healthcare during the COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18:13239. doi: 10.3390/ijerph182413239
36. Park, C , Ng, BP , and Kim, K . Inability to access health care due to COVID-19 among Medicare beneficiaries. Am J Manag Care. (2022) 28:75–80. doi: 10.37765/ajmc.2022.88823
37. Centers for Disease Control and Prevention . People with certain medical conditions. (2023). Available at: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html (Last access April 6, 2023).
38. Czeisler, M &, Barrett, CE , Siegel, KR , Weaver, MD , Czeisler, CA , Rajaratnam, SMW, et al. Health care access and use among adults with Diabetes during the COVID-19 pandemic — United States, February–march 2021. MMWR Morb Mortal Wkly Rep (2021);70:1597–1602. doi: 10.15585/mmwr.mm7046a2
39. Olesen, K , Joensen, LE , Madsen, KP , and Willaing, I . How has the COVID-19 pandemic affected diabetes self-management in people with diabetes? A one-year follow-up study. Front Clin Diabetes Healthc. (2022) 3:867025. doi: 10.3389/fcdhc.2022.867025
40. Sakur, F , Ward, K , Khatri, N , and Lau, A . Self-care behaviors and technology used during COVID-19: systematic review. JMIR Hum Factors. (2022) 9:e35173. doi: 10.2196/35173
41. Rochfort, A , Beirne, S , Doran, G , Patton, P , Gensichen, J , Kunnamo, I, et al. Does patient self-management education of primary care professionals improve patient outcomes: a systematic review. BMC Fam Pract. (2018) 19:163. doi: 10.1186/s12875-018-0847-x
42. Sunol, R , González-González, AI , Valli, C , Ballester, M , Seils, L , Heijmans, M, et al. Self-management interventions for adults living with obesity to improve patient-relevant outcomes: an evidence map. Patient Educ Couns. (2023) 110:107647. doi: 10.1016/j.pec.2023.107647
43. Diabetes UK . Improving supported self-management for people with diabetes Available at: https://www.diabetes.org.uk/resources-s3/2017-09/Supported_self-management.pdf (2009).
44. Pardhan, S , Islam, MS , López-Sánchez, GF , Upadhyaya, T , and Sapkota, RP . Self-isolation negatively impacts self-management of diabetes during the coronavirus (COVID-19) pandemic. Diabetol Metab Syndr. (2021) 13:123. doi: 10.1186/s13098-021-00734-4
45. Burns, A , Leavey, G , Ward, M , and O’Sullivan, R . The impact of loneliness on healthcare use in older people: evidence from a nationally representative cohort. J Public Health. (2022) 30:675–84. doi: 10.1007/s10389-020-01338-4
46. Gerst-Emerson, K , and Jayawardhana, J . Loneliness as a public health issue: the impact of loneliness on health care utilization among older adults. Am J Public Health. (2015) 105:1013–9. doi: 10.2105/AJPH.2014.302427
Keywords: COVID-19 pandemics, frailty, health services accessibility, non-communicable, disease
Citation: De Sarro C, Papadopoli R, Morgante MC and Pileggi C (2023) A new emergency during the latest phase of the COVID-19 pandemic: access to healthcare services by patients with non-communicable diseases. Front. Med. 10:1261063. doi: 10.3389/fmed.2023.1261063
Edited by:
Afshin Ostovar, Tehran University of Medical Sciences, IranReviewed by:
Niloofar Peykari, Ministry of Health and Medical Education, IranMehdi Afkar, Islamic Azad University of Medical Sciences, Iran
Copyright © 2023 De Sarro, Papadopoli, Morgante and Pileggi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Claudia Pileggi, Y2xhdWRpYXBpbGVnZ2lAdW5pY3ouaXQ=
 Caterina De Sarro1
Caterina De Sarro1 Claudia Pileggi
Claudia Pileggi