
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Med., 28 September 2023
Sec. Gastroenterology
Volume 10 - 2023 | https://doi.org/10.3389/fmed.2023.1255545
This article is part of the Research TopicClinical Insights: Critical Bleeding in Different Clinical ScenariosView all 4 articles
Giant greater omental cysts with associated massive hemorrhage are rare. We encountered a 16-month-old boy with a four-day history of acute abdominal pain, distension, and paleness. Physical examination revealed a blood pressure of 74/27 mmHg. No well-defined masses were observed on abdominal palpation. The hemoglobin level on admission was 24 g/L. After initial resuscitation and blood transfusion, a computed tomography (CT) scan was performed, revealing a giant cystic mass with an intracystic hemorrhage. The diagnosis was confirmed via exploratory laparotomy, and the cyst, with the attached partial omentum was removed. Pathological findings revealed a simple cyst originating from the greater omentum. The patient recovered uneventfully and remained well during the two-year follow-up period. We reviewed the literature published over the last 27 years on cases of omental cysts to evaluate demographic characteristics, clinical presentations, complications, diagnostic tool options, and surgical approaches.
Intra-abdominal cysts, including mesenteric cysts, omental cysts, retroperitoneal lymphangiomas, and intestinal duplication cysts, are rare in the pediatric population. The estimated incidence is 1 in 20,000 admissions to a pediatric hospital (1–3) and among these, omental cysts are rare, representing 10%–30% of cystic lesions (4). The clinical manifestations of omental cysts include a painless mass incidentally found, moderate or marked abdominal distension, acute or chronic abdominal pain, fever, vomiting, and anemia (1, 5–10). Giant omental cysts may mimic ascites for years and may persist for several months after treatment for misdiagnosed abdominal tuberculosis (1, 7, 8, 10). Several cases have presented with severe anemia and shock, requiring fluid resuscitation and massive blood transfusion (5, 6, 11, 12). Herein, we describe a new case of giant omental cyst complicated by spontaneous massive hemorrhage that presented with profound anemia and shock, which was successfully treated, with a favorable outcome. The literature related to omental cysts from 1996 to date was reviewed and analyzed. As shown in Table 1, more than half of the patients were between one and seven years old. The main presentations were abdominal distension mimicking ascites (36.8%), abdominal masses (25%), anemia (13.2%), and acute abdominal pain (13.2%). Omental cysts should therefore be a diagnostic consideration in all children presenting with abdominal pain. We aimed to increase awareness of this rare disorder, explore its characteristics, and suggest strategies for diagnosis and management.
A previously healthy 16-month-old boy presented with a four-day history of acute abdominal distension and profound anemia. His parents denied any preceding trauma or bleeding disorders. Upon physical examination, he was pale and lethargic, with tachycardia of 162 beats per minute. His blood pressure was 74/27 mmHg, with cool extremities, prolonged capillary refill, and flat neck veins. His oxygen saturation was 98%–100% on room air; the patient was tachypneic. He presented with severe abdominal distension; however, no well-defined abdominal mass was palpated. Initial laboratory data showed profound anemia, with hemoglobin 24 g/L, red blood cell count 1.03 × 1012/L, and hematocrit 7.8%. The white blood cell count was 9.5 × 109/L and the platelet count was 304 × 109/L. Other laboratory parameters, including coagulation screening and serum chemistry, were within normal limits. The patient was immediately fluid resuscitated and received a massive blood transfusion, including 600 mL of concentrated red blood cells and 100 mL of fresh frozen plasma. The patient responded well to therapy and his hemoglobin level reached 92 g/L before surgical intervention. Point-of-care ultrasonography revealed a large anechoic mass with dense debris echoes, suggestive of hemorrhage into the cyst. A chest X-ray before surgery revealed no mass or hydrothorax. Abdominal computed tomography (CT) revealed a cystic unilocular hypodense lesion from the subdiaphragmatic space to the pelvis, measuring 18 × 17 × 10 cm (Figures 1A,B). Due to a suspicion of an intra-abdominal cyst associated with spontaneous massive bleeding, emergency surgical exploration was advised. Written informed consent for the surgical procedure was obtained from the guardian of the patient. Intraoperative findings revealed a large thin-walled and well-defined cyst that originated from the greater omentum and contained fresh hemorrhagic fluid (Figure 1C). Intraperitoneal bleeding was not observed. After controlled decompression using an aspirator, the cyst, with the attached greater omentum, was completely excised (Figure 1D). Hemostasis was achieved using bipolar electrocoagulation ligation of the feeder vessels. No abdominal drainage was required. Pathological examination of the excised specimen revealed a unilocular cyst lined by mesothelial cells and the absence of smooth muscle, confirming the diagnosis of a simple mesothelial cyst of the omentum. The postoperative recovery was uneventful, and the patient was discharged on the ninth postoperative day. An ultrasound scan was normal at the two-year follow-up after surgery.
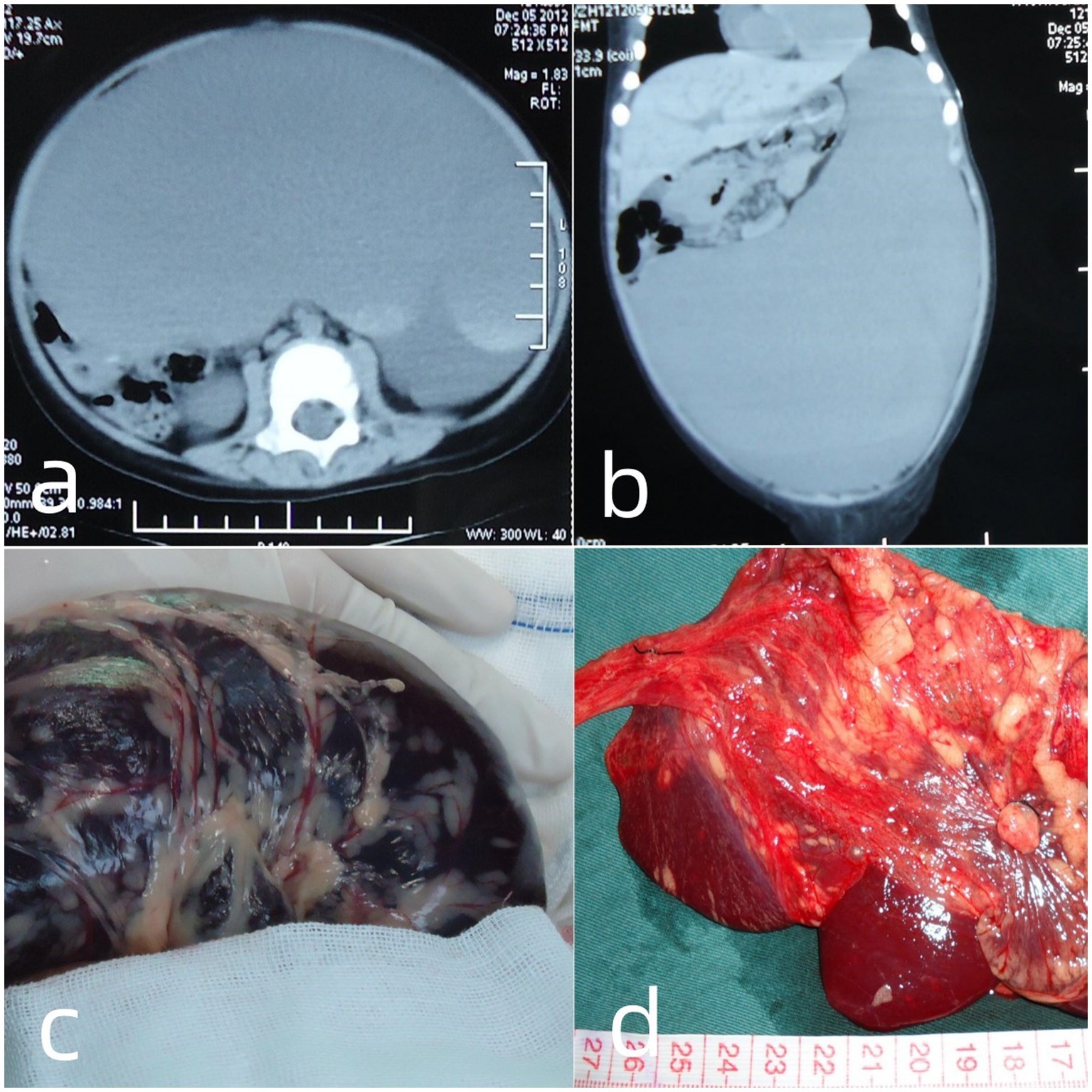
Figure 1. Abdominal and pelvic CT scans, revealing a large hypodense lesion that extended from the subdiaphragmatic space to the pelvis (A,B). Intraoperative findings showing a well-defined cyst containing a large volume of fresh hemorrhagic fluid (C). The surgically excised specimen showing a decompressed cyst, with attached partial greater omentum (D).
Omental cysts are uncommon congenital cystic lesions that rarely occur in children (1–4). A giant omental cyst complicated by spontaneous massive hemorrhage is an extremely rare but life-threatening condition (5, 6, 13, 14). Previously reported cases of giant omental cystic lymphangioma were associated with massive hemorrhage (5, 13, 14). In the present case, the patient had a progressively distended abdomen, profound anemia, and unstable hemodynamics. We reviewed the literature published over the last 27 years on cases of omental cysts by evaluating demographic characteristics, clinical presentations and complications, diagnostic tool options, differential diagnosis, and surgical approaches. Our analysis was conducted using the keywords “omental cyst,” “mesenteric cyst,” and “abdominal cystic lesions, pediatric” in the PubMed® database (Table 1) (1, 5, 6, 8–11, 13–40).
Based on the literature review, the results of the pathological diagnosis (41) revealed lymphangioma (n = 50, 73.2%), simple cysts (n = 17, 25%), and inflammatory melanotic cysts (n = 1, 2.8%). In the present case, the pathological findings revealed a simple unilocular cyst lined with mesothelial cells.
Clinically, an abdominal mass may mimic an ovarian cyst in female children (16%). Of the 68 reported cases, 27 (39.7%) patients experienced complications, including massive hemorrhage (26.5%), torsion (5.9%), infection, small bowel obstruction, and intestinal perforation. Profound acute anemia is usually associated with massive intracystic hemorrhage (5, 6).
In association with the absence of specific symptoms, the rarity of omental cysts, especially giant cysts, may complicate diagnosis. Greater omental cysts may mimic ascites (1, 7, 19, 22, 40), ovarian cysts (26, 27, 29, 42), acute abdomen (7, 25, 26, 42), and anemia (5, 6). Omental cysts should be considered as a diagnostic hypothesis in children with abdominal pain, with or without a mass (42). In the absence of trauma or hematologic disorders, a diagnosis of profound pediatric hemorrhagic anemia with severe abdominal distension and shock should rule out a giant omental cyst complicated by spontaneous major bleeding (14).
An accurate preoperative diagnosis may result in appropriate management options (24). Imaging is of paramount importance in the differential diagnosis of intra-abdominal cystic lesions (35). Regarding the imaging tool option, an initial ultrasonography scan, which reveals the cystic characteristics of the lesion in four-fifths of cases, was used as a diagnostic tool (18, 27, 43). CT and MRI scans were chosen in 54.4% and 16.2% of cases, respectively, which provided further and more accurate information, including the location, size, content, and relationship of the cyst with adjacent structures (8, 16, 21, 30). Although imaging studies, including point-of-care ultrasonography, CT scan, and magnetic resonance imaging, are vital for the diagnosis of intra-abdominal cysts, they may fail to differentiate giant omental cysts from other cystic lesions or ascites, such as mesenteric cysts (7), intestinal duplication cysts (17, 37), and abdominal tubercular ascites (8). It is necessary to do a chest CT and to detect tumor biomarkers to rule out other rare conditions, especially in patients with stable hemodynamic status (44, 45); however, increasing concern regarding radiation exposure and other potential risks from CT scan in babies should be considered (46, 47).
Regarding the management of patients with massive intracystic hemorrhage, treatment should focus on rapid crystalloid resuscitation followed by blood transfusion to restore blood volume. Emergent surgery is indicated due to high intra-abdominal pressure and the risk of continued bleeding or further major bleeding in a short timeframe, especially in toddlers (5, 6, 14).
Most authors agree with complete excision of the cyst without omentectomy or partial omentectomy to prevent the potential risk of complications due to the cyst (48). In selected cases, several approaches, including traditional open surgery (n = 45, 66.2%) (11, 22, 32), laparoscopic surgery (n = 22, 32.4%) (16, 18, 32, 39), and transumbilical minilaparotomy (30), have been described for the treatment of omental cysts. When technically available, laparoscopic surgery is usually preferred because of its minimal invasiveness, reduced blood loss and postoperative ileus, less postoperative pain, shorter hospitalization, and faster return to normal activity (8, 9, 15, 49).
It has been reported that the creation of a low-pressure pneumoperitoneum without compromising the cardiovascular physiology is possible for large intra-abdominal cystic lesions (50). Controlled decompression by aspiration of a large cyst can provide adequate space for manipulation (50–52). It is important to excise cystic lesions completely laparoscopically, especially large omental cysts. However, careful patient selection for the choice of laparoscopic approach is necessary and conversion to laparotomy is possible if required from a technical standpoint (49, 53).
In conclusion, omental cysts are rare. The diagnosis may be difficult because of nonspecific symptoms. Complete open or laparoscopic cyst removal is recommended to prevent potential complications and recurrence. We present the case of a toddler with a giant omental cyst complicated by a spontaneous massive hemorrhage leading to profound anemia and shock. Our case study reveals the importance of early recognition and proper management of this potentially fatal complication in patients with giant omental cysts.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical approval was not required for the study involving human samples in accordance with the local legislation and institutional requirements because (reason ethics approval was not required). Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article. Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
FC: Data curation, Methodology, Software, Validation, Writing – original draft, Writing – review & editing. XuX: Data curation, Supervision, Writing – original draft, Writing – review & editing. XL: Data curation, Methodology, Writing – original draft, Writing – review & editing. SS: Data curation, Methodology, Writing – original draft, Writing – review & editing. ZL: Data curation, Methodology, Writing – review & editing. XiX: Data curation, Methodology, Writing – original draft, Writing – review & editing. TF: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. LG: Data curation, Investigation, Methodology, Resources, Supervision, Validation, Writing – review & editing.
We thank the colleagues of the Department of Pediatric Surgery for their cooperation as well as the enthusiastic support from the operating room team.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Karhan, AN, Soyer, T, Gunes, A, Talim, B, Karnak, I, Oguz, B, et al. Giant omental cyst (lymphangioma) mimicking ascites and tuberculosis. Iran J Radiol. (2016) 13:e31943. doi: 10.5812/iranjradiol.31943
2. Hardin, WJ, and Hardy, JD. Mesenteric cysts. Am J Surg. (1970) 119:640–5. doi: 10.1016/0002-9610(70)90232-1
3. Hebra, A, Brown, MF, McGeehin, KM, and Ross, AJ 3rd. Mesenteric, omental, and retroperitoneal cysts in children: a clinical study of 22 cases. South Med J. (1993) 86:173–6. doi: 10.1097/00007611-199302000-00005
4. Giovanni, C, Riccardo, V, Grazia, EM, Umberto, B, Salvatore, C, and Antonio, L. Laparoscopic treatment of an omental cyst: a case report and review of the literature. Surg Laparosc Endosc Percutan Tech. (2005) 15:33–5. doi: 10.1097/01.sle.0000148472.97417.ca
5. Kokhanovsky, N, Nachtigal, A, Reindorp, N, Shinhar, D, and Zeina, AR. Giant omental hemorrhagic cyst presenting as acute hemorrhagic anemia in a 21-month-old infant. Pediatr Emerg Care. (2014) 30:188–90. doi: 10.1097/PEC.0000000000000092
6. Adikibi, BT, Wood, R, Pillay, K, and Millar, AJ. Omental cyst presenting with profound anaemia. Afr J Paediatr Surg. (2013) 10:180–4. doi: 10.4103/0189-6725.115050
7. Fitoz, S, Atasoy, C, Ekim, M, Yildiz, S, Erden, A, and Aktug, T. Torsion of a giant omental cyst mimicking ascites. J Clin Ultrasound. (2007) 35:85–7. doi: 10.1002/jcu.20248
8. Joshi, N, Yadav, S, Singh, B, and Gupta, A. Omental cyst presenting as tubercular ascites. J Infect Dev Ctries. (2010) 4:183–6. doi: 10.3855/jidc.314
9. Talukdar, S, Alagaratnam, S, Sinha, A, Thorn, CC, and Elton, C. Giant cystic lymphangioma in childhood: a rare differential for the acute abdomen. BMJ Case Rep. (2011) 2011:bcr0420114105. doi: 10.1136/bcr.04.2011.4105
10. Ravindranath, A, Wadhwa, RP, Sandeep, BS, and Srikrishna, KK. Infant with "ascites". J Pediatr. (2021) 237:314–5. doi: 10.1016/j.jpeds.2021.05.065
11. Safdar, A, Bakhsh, M, Ahmed, I, and Kibria, R. An unusual cause of haemoperitoneum in a child. J Pak Med Assoc. (2008) 58:458–60. PMID:18822648.
12. Olesen, T, Pilgaard, B, and Perrild, K. Svaer anaemi forårsaget af blødning i omentcyste [Severe anemia due to hemorrhage into an omental cyst]. Ugeskr Laeger. (1979) 141:2321–2. Danish.
13. Robbins, KJ, Antiel, RM, and Shakhsheer, BA. Omental cyst: a case report and review of the literature. Ann Pediatr Surg. (2021) 17:62. doi: 10.1186/s43159-021-00129-0
14. Mahmoudi, A, Rami, M, Khattala, K, El Madi, A, and Bouabdallah, Y. Huge omental lymphangioma with haemorrhage in children: case report. Pan Afr Med J. (2020) 35:20. doi: 10.11604/pamj.2020.35.20.8585
15. Bruloy, E, Haraux, E, Robert, B, Djeddi, D, and Buisson, P. Unusual presentation of Giant omental cystic lymphangioma mimicking Hemorrhagic ascites in a child. J Pediatr Gastroenterol Nutr. (2018) 66:e19. doi: 10.1097/MPG.0000000000001095
16. de Lagausie, P, Bonnard, A, Berrebi, D, Lepretre, O, Statopoulos, L, Delarue, A, et al. Abdominal lymphangiomas in children: interest of the laparoscopic approach. Surg Endosc. (2007) 21:1153–7. doi: 10.1007/s00464-006-9091-x
17. Henry, GM, Kern, IB, and Currie, BG. Omental cysts: an unusual cause of abdominal distension in children. Pediatr Surg Int. (1996) 11:387–9. doi: 10.1007/BF00497820
18. Yao, CC, Wu, TL, Wong, HH, Yang, CC, Liew, SC, and Lin, CS. Laparoscopic resection of an omental cyst with pedicle torsion. Surg Laparosc Endosc Percutan Tech. (1999) 9:372–4. doi: 10.1097/00129689-199910000-00012
19. Klin, B, Lotan, G, Efrati, Y, and Vinograd, I. Giant omental cyst in children presenting as pseudoascites. Surg Laparosc Endosc. (1997) 7:291–3. doi: 10.1097/00019509-199708000-00006
20. DeRusso, PA, Benson, J, and Lau, H. Intestinal malrotation and omental cyst presenting as fetal ascites. J Pediatr Gastroenterol Nutr. (2003) 36:283–6. doi: 10.1097/00005176-200302000-00023
21. Luo, CC, Huang, CS, Chao, HC, Chu, SM, and Hsueh, C. Intra-abdominal cystic lymphangiomas in infancy and childhood. Chang Gung Med J. (2004) 27:509–14. PMID:15508873.
22. Rattan, KN, Budhiraja, S, Pandit, SK, and Yadav, RK. Huge omental cyst mimicking ascites. Indian J Pediatr. (1996) 63:707–8. doi: 10.1007/BF02730829
23. Shafi, SM, Malla, MA, and Reshi, FA. Giant primary omental cyst mimicking a pseudoascites. Afr J Paediatr Surg. (2009) 6:58–60. doi: 10.4103/0189-6725.48581
24. Gupta, RK, Sah, S, Sah, PL, and Shah, BP. Congenital omental cyst. BMJ Case Rep. (2012) 2012:bcr2012006643. doi: 10.1136/bcr-2012-006643
25. Tsopozidi, M, Kepertis, C, Godosis, D, Mouravas, V, Demiri, C, and Spyridakis, I. Laparoscopic-assisted excision of a huge polycystic omental lymphangioma in a 3 year old patient presenting with acute abdomen: case report and review. Pan Afr Med J. (2021) 38:228. doi: 10.11604/pamj.2021.38.228.26607
26. Alemu, H, Alemu, S, and Berhane, M. Omental cyst presenting as an acute abdomen in a Pediatric patient: a case report. Int Med Case Rep J. (2022) 15:43–6. doi: 10.2147/IMCRJ.S351406
27. Kuga, T, Inoue, T, Taniguchi, S, Zempo, N, and Esato, K. Laparoscopic surgery in infants with intra-abdominal cysts: two case reports. JSLS. (2000) 4:243–6. PMID:10987403.
28. Mistry, KA, and Iyer, D. Torsion of the greater omentum secondary to omental lymphangioma in a child: a case report. Pol J Radiol. (2015) 80:111–4. doi: 10.12659/PJR.892873
29. Kumar, V, and Bedi, NK. Omental cyst, an uncommon entity, and the problems faced: the travails of a surgeon: a case report. IJSS Case Rep Rev. (2015) 2:13–5. doi: 10.17354/cr/2015/107
30. Odaka, A, and Hashimoto, D. Umbilical approach using the sliding-window method to avoid a large abdominal incision: report of two pediatric cases. Pediatr Surg Int. (2005) 21:928–31. doi: 10.1007/s00383-005-1519-1
31. Moralioğlu, S, Sönmez, K, Türkyilmaz, Z, Başaklar, AC, and Kale, N. A child with a giant omental cyst. Acta Chir Belg. (2007) 107:724–5. doi: 10.1080/00015458.2007.11680159
32. Méndez-Gallart, R, Bautista, A, Estévez, E, and Rodríguez-Barca, P. Abdominal cystic lymphangiomas in pediatrics: surgical approach and outcomes. Acta Chir Belg. (2011) 111:374–7. doi: 10.1080/00015458.2011.11680776
33. Nam, SH, Kim, DY, Kim, SC, and Kim, IK. The surgical experience for retroperitoneal, mesenteric and omental cyst in children. J Korean Surg Soc. (2012) 83:102–6. doi: 10.4174/jkss.2012.83.2.102
34. Tran, NS, and Nguyen, TL. Laparoscopic management of abdominal lymphatic cyst in children. J Laparoendosc Adv Surg Tech A. (2012) 22:505–7. doi: 10.1089/lap.2012.0003
35. Nett, MH, Vo, NJ, and Chapman, T. Large omental cyst. Radiol Case Rep. (2015) 5:388. doi: 10.2484/rcr.v5i2.388
36. Ishii, S, Hayashida, M, Nakatani, K, Shimozono, T, and Marutsuka, K. Omental lymphangioma presenting with acute abdomen due to hemorrhage. Pediatr Int. (2018) 60:896–8. doi: 10.1111/ped.13640
37. Chong, HC, Khalid, HM, Hanifah, NAM, Jaffrey, V, Thiyagaraja, N, and Hayati, F. Infected omental cyst complicated with subacute intestinal obstruction and ileal erosion in a 2-year-old boy: a case report. Pan Afr Med J. (2021) 40:257. doi: 10.11604/pamj.2021.40.257.30755
38. Tiwari, C, Shah, H, Waghmare, M, Makhija, D, and Khedkar, K. Cysts of gastrointestinal origin in children: varied presentation. Pediatr Gastroenterol Hepatol Nutr. (2017) 20:94–9. doi: 10.5223/pghn.2017.20.2.94
39. Tshilolo, L, Lukamba, R, Simbi, A, Kazadi, V, Mayemba, C, Lebwaze, B, et al. A giant omental cyst mimicking ascites in a three-year-old congolese child. Int J Case Rep Images. (2016) 7:471–5. doi: 10.5348/ijcri-201684-CR-10672
40. Salvador, A, Rosenberg, HK, Horrow, MM, and Kumar, SL. Abdominal lymphangioma in a preterm infant. J Perinatol. (1996) 16:305–8.8866304.
41. Ros, PR, Olmsted, WW, Moser, RP Jr, Dachman, AH, Hjermstad, BH, and Sobin, LH. Mesenteric and omental cysts: histologic classification with imaging correlation. Radiology. (1987) 164:327–32. doi: 10.1148/radiology.164.2.3299483
42. Sayeed, M, Benzamin, M, Akter, S, Mazumder, MW, Karim, ASMB, and Dey, BP. Omental cyst-rare cause of abdominal pain in a 7-year-old child: a case report. GE Port J Gastroenterol. (2021) 28:202–6. doi: 10.1159/000510022
43. Rahman, GA, and Johnson, AW. Giant omental cyst simulating ascites in a Nigerian child: case report and critique of clinical parameters and investigative modalities. Ann Trop Paediatr. (2001) 21:81–5. PMID:11284253. doi: 10.1080/02724930123762
44. Stabile, G, Zinicola, G, Romano, F, Laganà, AS, Pozzolo, CD, and Ricci, G. Pelvic mass, ascites, hydrothorax: a malignant or benign condition? Meigs syndrome with high levels of CA 125. Prz Menopauzalny. (2021) 20:103–7. doi: 10.5114/pm.2021.106100
45. Granja, C, and Mota, L. Paediatric neuroblastoma presenting as an asymptomatic abdominal mass: a report on the importance of a complete clinical examination with a view to a timely diagnosis and therapeutic guidance in paediatric oncology. BMJ Case Rep. (2022) 15:e247907. doi: 10.1136/bcr-2021-247907
46. Schultz, CH, Fairley, R, Murphy, LS, and Doss, M. The risk of cancer from CT scans and other sources of low-dose radiation: a critical appraisal of methodologic quality. Prehosp Disaster Med. (2020) 35:3–16. doi: 10.1017/S1049023X1900520X
47. Brody, AS, and Guillerman, RP. Ten rules for ordering chest CTs. Pediatr Pulmonol. (2021) 56:1868–71. doi: 10.1002/ppul.25399
48. Gagliardi, F, Lauro, A, Tripodi, D, Amabile, MI, Palumbo, P, Di Matteo, FM, et al. Mesenteric cyst with GI symptoms: a fluid approach to treatment-case report and literature review. Dig Dis Sci. (2022) 67:786–98. doi: 10.1007/s10620-021-07352-0
49. Lee, SW, Lee, SJ, Jang, DG, Yoon, JH, and Kim, JH. Comparison of laparoscopic and laparotomic surgery for the treatment of peritoneal inclusion cyst. Int J Med Sci. (2012) 9:14–9. doi: 10.7150/ijms.9.14
50. Deshpande, AA, and Dalvi, AN. Laparoscopic excision of a giant mesothelial omental cyst. J Minim Access Surg. (2012) 8:57–8. doi: 10.4103/0972-9941.95538
51. Bhandarkar, D, Ghuge, A, Kadakia, G, and Shah, R. Laparoscopic excision of an omental leiomyoma with a giant cystic component. JSLS. (2011) 15:409–12. doi: 10.4293/108680811X13125733357232
52. Kuriansky, J, Bar-Dayan, A, Shabtai, M, Barshach, I, Rosin, D, and Ayalon, A. Laparoscopic resection of huge omental cyst. J Laparoendosc Adv Surg Tech A. (2000) 10:283–5. doi: 10.1089/lap.2000.10.283
Keywords: omental cyst, hemorrhage, complication, shock, pediatric, case report
Citation: Cheng F, Xing X, Liu X, Sun S, Lv Z, Xu X, Fu T and Geng L (2023) Toddler with giant omental cyst, profound anemia, and shock: case report and review of the literature. Front. Med. 10:1255545. doi: 10.3389/fmed.2023.1255545
Received: 09 July 2023; Accepted: 06 September 2023;
Published: 28 September 2023.
Edited by:
Krisztian Tanczos, Semmelweis University, HungaryReviewed by:
Guglielmo Stabile, Institute for Maternal and Child Health Burlo Garofolo (IRCCS), ItalyCopyright © 2023 Cheng, Xing, Liu, Sun, Lv, Xu, Fu and Geng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tingliang Fu, ZHJmdXRsQHNpbmEuY29t; Lei Geng, MzgxODExNDFAcXEuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.