- 1Department of Human Genetics, School of Medicine, University of Texas Rio Grande Valley, Brownsville, TX, United States
- 2South Texas Diabetes and Obesity Institute, School of Medicine, University of Texas Rio Grande Valley, Brownsville, TX, United States
Background: Frailty is characterized by an accumulation of deficits that lead to vulnerability to adverse health outcomes. The Frailty Index (FI) quantifies frailty by measuring deficits that increase susceptibility to stressors. This study focused on a population of Mexican Americans living in vulnerable communities in the Rio Grande Valley of south Texas. We used a Frailty Index developed based on common health-related data--the Patient Health Questionnaire (PHQ-9) and a Health-related Quality of Life survey (Duke Health Profile). Quality of life, resilience, and frailty are interrelated and influenced by chronic illness, mental illness, poverty, cognitive impairment, and community support.
Methods: We used Logistic regression analysis, factor component analysis, receiver operating characteristic curves, and odds ratios to identify potential associations between clinical variables and candidate predictor variables and seven physiological health variables, and two survey instruments. We analyzed data obtained from participants (894) that live in two Colonias located on the Texas-Mexico border. We calculated the FI with seven physiological variables, PHQ-9 score, and the 11 domain-specific Duke Profile scores, for a total of 19 health deficits. We then dichotomized FI (>0.25) and determined ROC curves through model selection to determine best predictors of frailty.
Results: Females (n = 622) had a higher starting frailty, and males (n = 272) had a significantly greater change rate with age. Women score higher in anxiety, depression, anxiety/depression, and pain. The frailty index and quality of life markers are strongly inversely related; poorer quality of life leads to greater frailty independent physiological health variables, the PHQ 9, sex, and age.
Conclusion: The study highlights the importance of addressing modifiable mental health and social stressors to reduce frailty. Furthermore, it suggests that factors supporting resilience and well-being, such as physical and mental health, social support, and perceived health, play a crucial role in frailty development. The findings have implications for interventions targeting vulnerable populations and emphasize the need for further research on the relationship between health-related quality of life and frailty.
Introduction
Frailty is associated with psychosocial and biological mechanisms, including quality of life, physical decline, and overwhelmed resilience related to stressors (1–4). Frailty is a phenotype and is an accumulation of deficits characterized by vulnerability to adverse health outcomes (5, 6). The Frailty Index (FI) measures deficits that increase vulnerability to stressors and quantifies the level of frailty, focusing on the number and nature of deficits contributing to frailty (7, 8). The Frailty Index (FI) may incorporate social, physical, and psychological contributors and Frailty Index are consistently associated with frailty risk regardless of the specific factors measured (9–11). We calculate a FI as the number of deficits/total number of the deficits. Using data from Mexican American participants living in vulnerable communities (Rio Grande Valley Colonias) who sought healthcare from a mobile medical unit (UniMóvil), we developed a Frailty Index using 19 commonly measured health-related data (obesity hypertension, high triglycerides, low high-density lipoprotein, high low-density lipoprotein, high cholesterol), the Patient Health Questionnaire (9 domains), and a Health-related Quality of Life survey (Duke Health Profile) (1). We chose the 17-item self-report questionnaire HrQoL Duke Health Profile (reliability 0.30–0.78) (12) because of the inclusion of six health-function measures (physical, mental, social, general, perceived health, and self-esteem) and four health-dysfunction measures (anxiety, depression, pain, and disability). The Patient Health Questionnaire (PHQ-9; reliability 0.89, sensitivity 88%, and specificity 88%) is a commonly used screen for depression (13). We used the 19 measures because of the high prevalence in the Rio Grande Valley (RGV) of obesity (55.5%), hypertension (39%), diabetes (32.5%), and depression (19%) (14, 15). Initial data analysis supported our population’s high frailty prevalence, mirroring chronic illness’s prevalence. We found a higher prevalence of frailty in the older, more established Colonia (Cameron Park) within Brownsville, Texas, and in younger women. Frailty peaked at 40–60 years, and we found that although women had a higher FI earlier in life, men became more frail with age (most likely due to increased chronic illness and hard physical labor) (1).
HrQoL, resilience, and frailty are intimately interconnected (9, 16). Chronic illness, sarcopenia, mental illness, poverty, cognitive impairment, lower psychological well-being, and the degree of community support, affect HrQoL (17–24). Excessive treatment of chronic illness may also affect HrQoL and frailty (23). A study of community-dwelling older adults demonstrated statistically significant negative associations between physical frailty, psychological frailty, and all dimensions of HrQoL (25). Conversely, resilience is associated with protection from frailty (2, 4, 26–31).
We are conducting this study as an extension of our previous research, which highlighted the utility of a FI incorporating standard clinic and HrQoL measures in the healthcare of Mexican Americans in South Texas. Our current investigation aims to assess the influence of HrQoL and resilience on frailty among Mexican Americans facing vulnerable and at-risk living conditions (1). Our primary objective is to identify the specific measures that predict frailty in this population. Additionally, we aim to explore whether physical and psychological functions, as well as dysfunctions, serve as predictors of frailty. By analyzing the deficits measured, we can establish a reciprocal relationship between these factors, shedding light on their interplay with resilience, health-related quality of life, and frailty.
Materials and methods
The University of Texas Rio Grande Valley Institutional Review Board approved the protocol. All patients signed consent for care. The study adhered to the ethical guidelines of the Declaration of Helsinki. The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found at: Manusov (32).
Health-related quality-of-life questionnaires and depression surveys are routinely administered as part of the care provided by the mobile medical van clinic (UniMóvil) as part of an effort to address the community’s medical, mental health, and social needs. The clinical team travels to the Colonias bi-weekly and collects information such as body mass index, blood pressure, glycated hemoglobin, lipid levels, glucose level, the PHQ9, and the Duke Health Profile. Other services include diabetes education, nutrition counseling, counseling, health literacy, and preventive care education. The data collection methods are described in detail in our earlier publication (1). Information was collected on all participants who presented for care on the mobile medical van (UniMóvil); there were no exclusion criteria.
The community comprises families of Mexican descent who have poor healthcare access, low socioeconomic reserve, and poor transportation resources. The participants represented the general population of the Colonias of Cameron and Hidalgo counties. The Area Deprivation Index (ADI), created to share measures of neighborhood disadvantage for research, program planning, and policy development, ranks the region as the most disadvantaged block groups (33) and is significantly impacted by social determinants of health, health disparities, and poor healthcare access.
Statistical analysis
This report further analyzes the convenience sample of 894 patients evaluated on UniMovil between 2016 and 2018 using anonymized linked healthcare data. We calculated a Frailty Index described in an earlier publication (1). Following the literature, a dichotomous frailty variable, denoted as dFI, was constructed by scoring subjects with a frailty index of 0.25 or greater as 1 and 0 (20–22). Logistic regression analysis (yielding odds ratios) was used to determine associations between 19 possible variables and frailty. Backward stepwise model selection was used to determine the best models. Receiver operating characteristic (ROC) curve analysis was performed to compare the relative performance of the finalized models to classify frailty. All statistical analysis was conducted in the R statistical package version 4.2.0.
Results
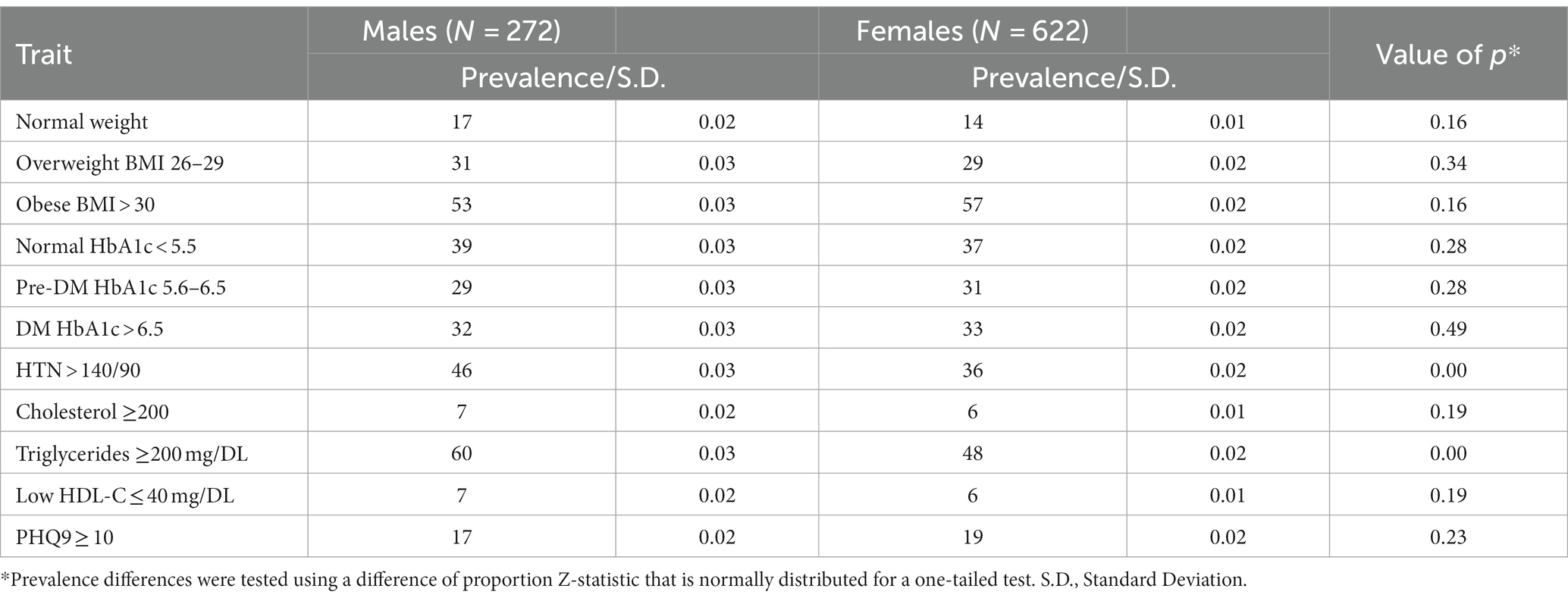
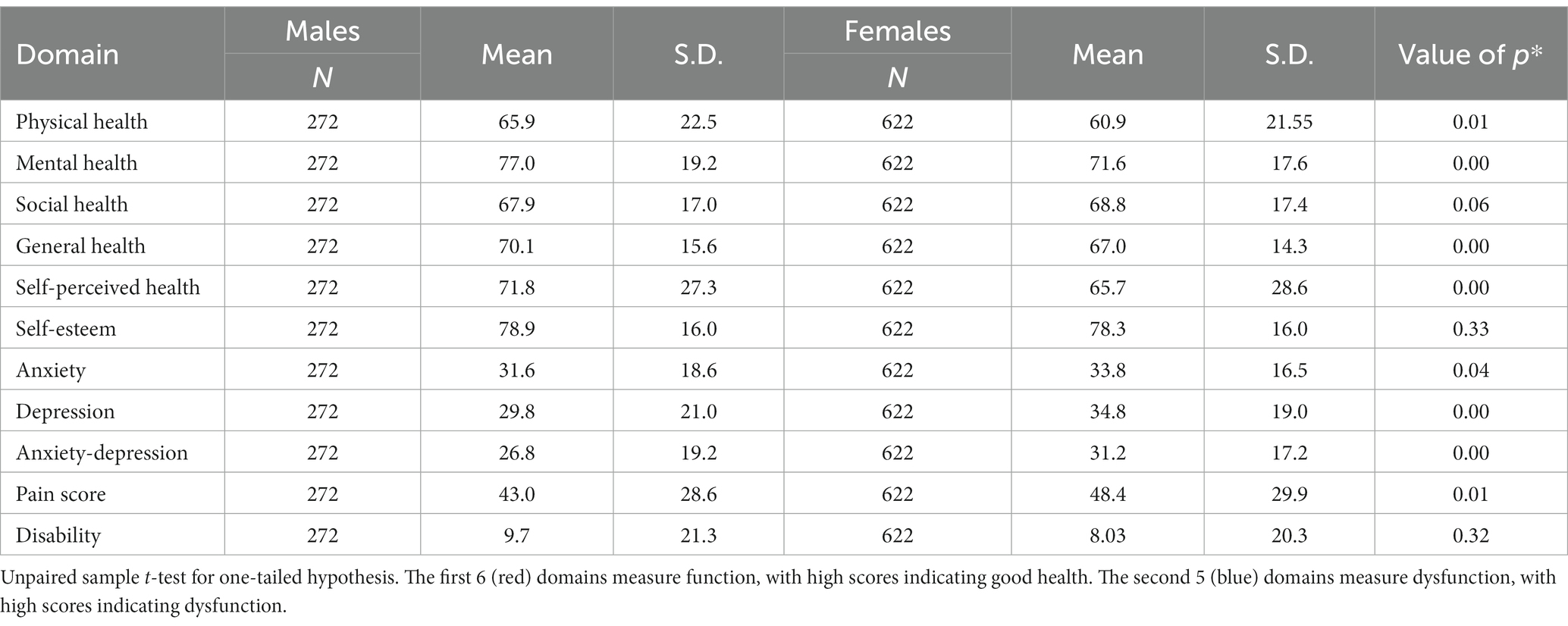
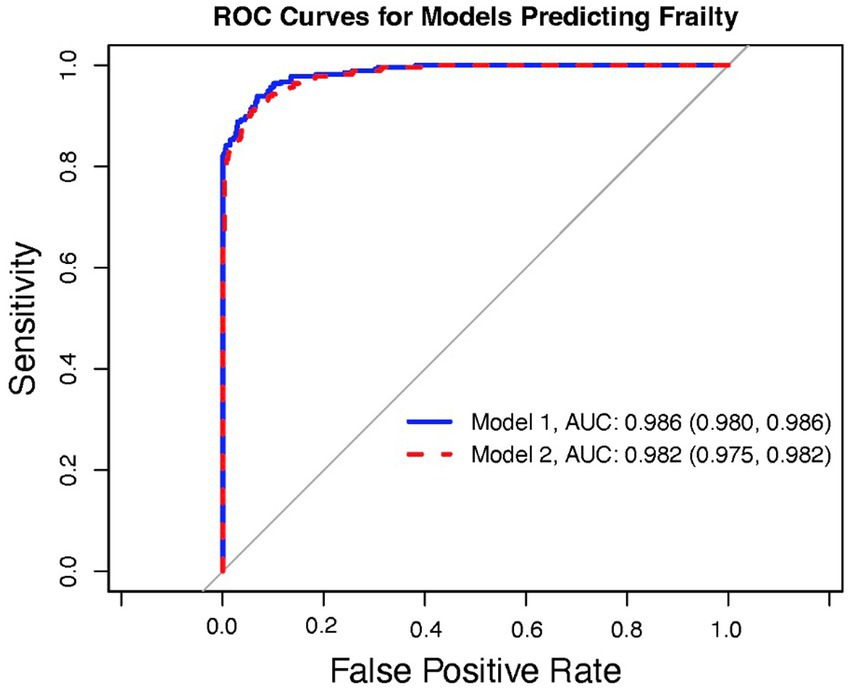
The total and sex-specific prevalence for clinical outcomes and the Duke Health Profile by total and sex-specific samples are shown in Tables 1 2. Model selection identified a model, Model 1, with the Duke Health Profile variables General, Self-esteem, Perceived, Anxiety, Depression, Anxiety-Depression, and Pain as significant independent predictors of dFI (Figure 1). However, because Anxiety, Depression, and Anxiety-Depression are highly intercorrelated, we formulated a reduced model, denoted as Model 2, where the predictors are the same as Model 1 but now exclude Anxiety and Depression (Figure 2). Figure 3 presents the ROC curves of the two models, which shows that they are statistically indistinguishable.
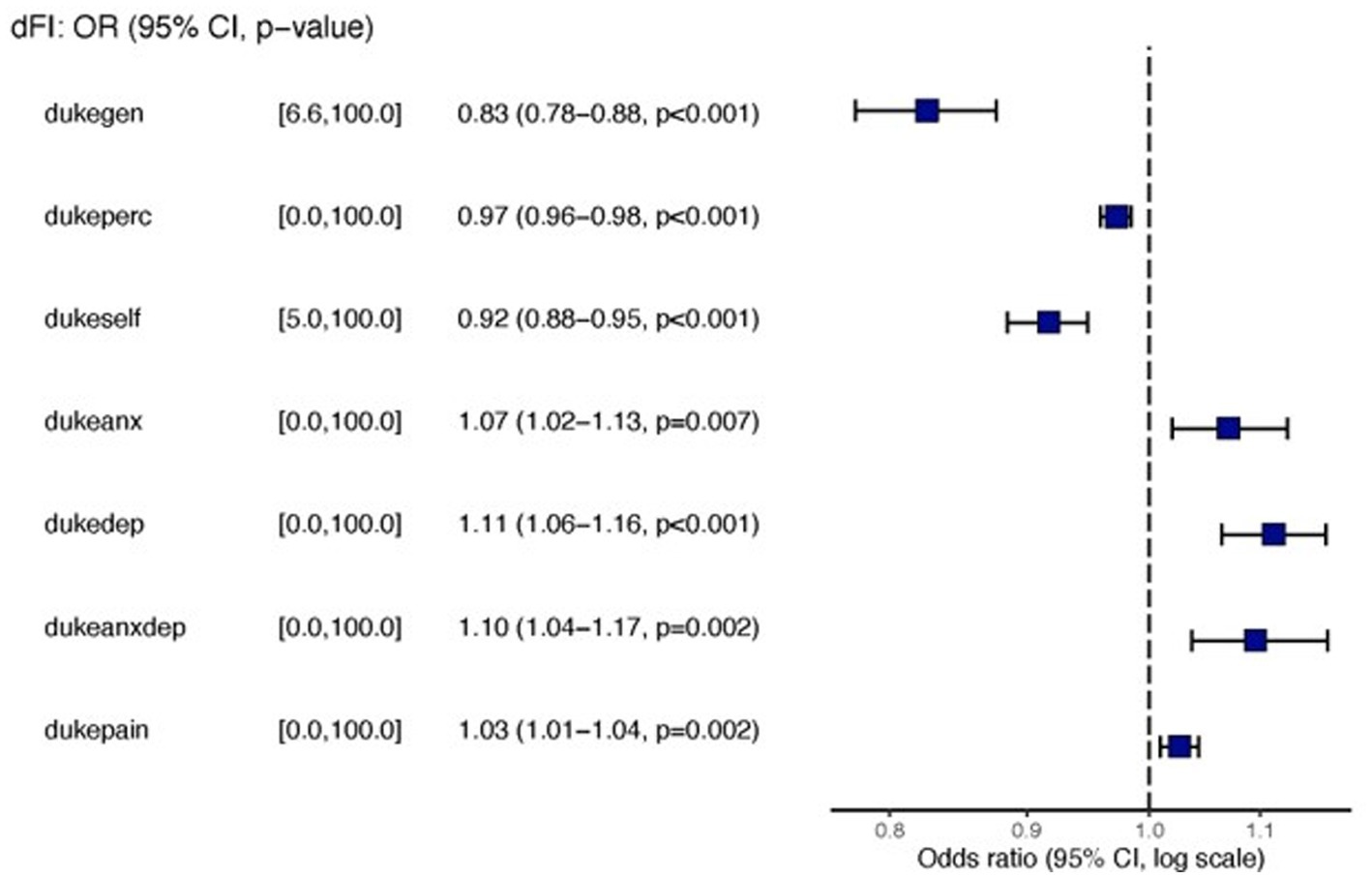
Figure 1. Forest plots for Model 1 with general, perceived, self-esteem, anxiety/depression and pain as independent predictors.
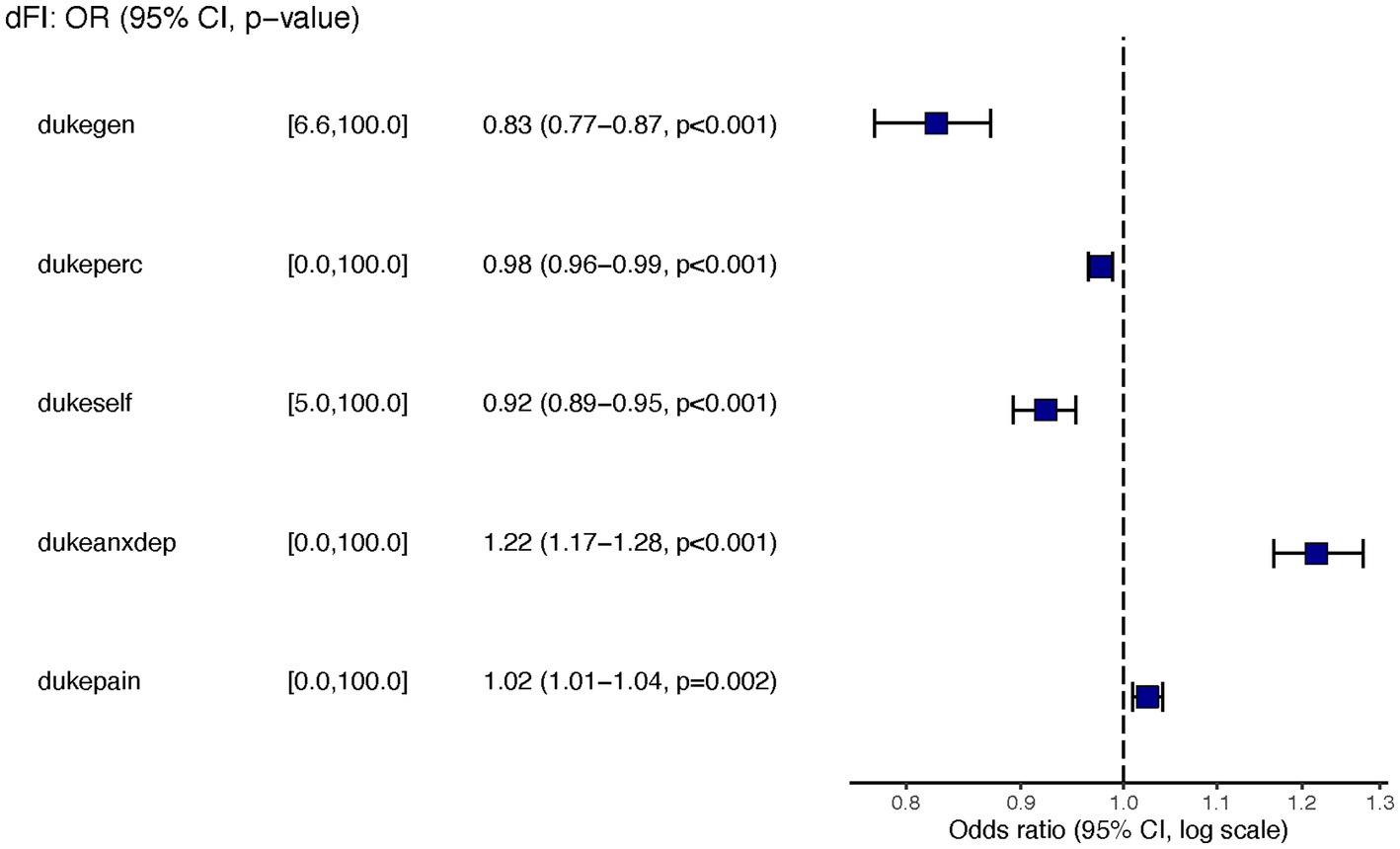
Figure 2. Forest plots for Model 2 with General, perceived health, self-esteem, anxiety/depression, and pain as independent predictors.
Similar to the findings of other researchers (34), we determined that frailty was more common in young women than men but increased exponentially as males aged. After logistic regression analysis (yielding odds ratios) to determine associations between 19 possible variables and frailty, we found the associations were present only for the HrQoL variables. The prevalence of hypertension and hypertriglyceridemia was higher in men than women (Table 1). Men scored better than women in all four domains of HrQoL function (physical health, mental health, social health, general health, self-perceived health, and self-esteem). Women scored worse in anxiety, depression, anxiety-depression, and pain (Table 2). Residents of the two Colonias scored similarly on 10 of the 11 domains of the Duke Profile other than perceived health. Males scored worse on five domains that measure function (i.e., physical, mental, social, general, and perceived health). For the five domains assessed by the Duke Profile (anxiety, depression, anxiety-depression, pain, and disability), women consistently scored worse than men in all domains except for the disability domain.
Discussion
Although we previously demonstrated that a Frailty Index that uses standard clinical and HrQoL measures is helpful in the South Texas population (1), what is novel is that the HrQoL measures, more than the biological measures of health, are the best predictors of frailty. Frailty is a state of increased vulnerability to disproportionate change in health due to the accumulation of small damages (35) and is linked to increased falls, hospitalizations, morbidity, mortality, and reduced quality of life (29). Resilience to frailty includes physical, genetic, social, and psychological moderators (2, 4, 26–28, 30, 31). Although not designed as a screen for resilience, HrQoL is moderated by social, physical, and mental health functions, and the Duke Profile HrQoL was created as a community-based screen for the same measures of the moderators of resilience (35–38). The Duke Profile HrQoL variables that best predict frailty include self-esteem, perceived health, anxiety, depression, and pain.
Whereas function (perceived health, general well-being, and self-esteem protect against frailty). Dysfunction differentially affects women, possibly due to the increased stress women living in Colonias endure (1, 39). Perception of health is also a significant predictor of frailty. Like other researchers, our findings support that psychosocial variables (depression, perceived social support, trauma account, and trauma severity) are associated with the risk of frailty (2). This is congruent with how older adults define aging (active participation, having good social and family support, thinking positively, active living, engagement, optimism and/or positive attitude, spirituality and/or religiosity, self-efficacy and/or self-esteem, gero-transcendence, spiritual well-being, and engagement with life) (26, 27, 31). The psychosocial variables, if present, increase resilience (28, 30, 40–43). Resilience is achieving, retaining, or regaining physical or emotional health after illness or loss (44). Our findings may reflect the associations between cultural stressors (acculturation and discrimination) and cultural values (family, respect, ethnic identity, and perseverance) that play a role in overcoming adversity and suggest that although biological determinants of health are essential to frailty development, HrQoL factors supporting resilience are as crucial for preventing frailty (45, 46).
Implications for research
We know that economic distress in Mexican American neighborhoods is strongly associated with the odds of being frail (47). Elderly immigrant populations affected by co-morbid chronic illness (18) and loneliness are more often frail. Interventions to improve frailty should focus on both mental and physical illness, as well as HrQoL (48, 49).
Further investigation into how the interaction between resilience and HrQoL affect frailty is needed. Chronic illness affects frailty, but if HrQoL has more predictive power, focusing on reducing mental health and social stressors that increase resilience may reduce frailty in vulnerable populations. The Health Belief Model may explain the importance of HrQoL in developing frailty. The model focuses on individual beliefs about health conditions (perception of severity, perceived susceptibility, perceived benefits, and self-efficacy), which predict individual health-related behaviors. If confidence and self-efficacy can alter behavior, these may protect against frailty through positive behaviors that support resilience, such as diet, reduction of at-risk alcohol/substance use, and sedentary lifestyle. The Resilience Activation Framework may serve as an implementation guide to mitigate adverse responses to biopsychosocial stressors (50).
Our study includes a comprehensive Frailty Index that employs validated measurement tools widely used by clinicians. The sample is a convenience sample; the data are cross-sectional, and the picture of frailty in the Colonias may not be generalizable to other populations. Further research is necessary to determine if other deficits, including cognitive decline, cancer, disease prognosis, and chronic illness complications, change the predictive value of deficits included in a FI.
Conclusion
This study is the first to determine the relative importance of HrQoL and subsequent resilience in the development of frailty in Mexican Americans on the U.S.-Mexican border. While FI consistently predicts frailty regardless of the number and type of variables used to calculate frailty, our findings suggest that HrQoL is more critical for predicting frailty in the Mexican American population of South Texas. Our results indicate we can decrease frailty by addressing modifiable mental health and social stressors.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found at: Manusov (32).
Ethics statement
The studies involving humans were approved by University of Texas Rio Grande Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
EM was the Principal Investigator on the United Health Foundation grant, collected data, analyzed data, wrote, and was substantially involved in editing the manuscript. VD analyzed the data, completed the statistical analysis, and was substantially involved in editing. SW-B was substantially involved in the development of the concept, manuscript development, and editing. All authors contributed to the article and approved the submitted version.
Funding
This research leverages instrumentation and capabilities established by Project THRIVE (Supported by the Valley Baptist Legacy Foundation) and a grant from the United Health Foundation funded the UniMovil project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Manusov, EG, Gomez De Ziegler, C, Diego, VP, Munoz-Monaco, G, and Williams-Blangero, S. Frailty index in the Colonias on the US-Mexico border: a special report. Front Med. (2021) 8:650259. doi: 10.3389/fmed.2021.650259
2. Freitag, S, and Schmidt, S. Psychosocial correlates of frailty in older adults. Geriatrics. (2016) 1:26. doi: 10.3390/geriatrics1040026
3. Cesari, M, Azzolino, D, LeBrasseur, NK, Whitson, H, Rooks, D, Sourdet, S, et al. Resilience: biological basis and clinical significance—a perspective report from the international conference on frailty and sarcopenia research (ICFSR) task force. J Frailty Aging. (2022) 11:342–7. doi: 10.14283/jfa.2022.62
4. Hale, M, Shah, S, and Clegg, A. Frailty, inequality and resilience. Clin Med. (2019) 19:219–23. doi: 10.7861/clinmedicine.19-3-219
5. Davinelli, S, Corbi, G, and Scapagnini, G. Frailty syndrome: a target for functional nutrients? Mech Ageing Dev. (2021) 195:111441. doi: 10.1016/j.mad.2021.111441
6. Church, S, Rogers, E, Rockwood, K, and Theou, O. A scoping review of the clinical frailty scale. BMC Geriatr. (2020) 20:393. doi: 10.1186/s12877-020-01801-7
7. Rockwood, K, Blodgett, JM, Theou, O, Sun, MH, Feridooni, HA, Mitnitski, A, et al. A frailty index based on deficit accumulation quantifies mortality risk in humans and in mice. Sci Rep. (2017) 7:43068. doi: 10.1038/srep43068
8. Dent, E, Kowal, P, and Hoogendijk, EO. Frailty measurement in research and clinical practice: a review. Eur J Intern Med. (2016) 31:3–10. doi: 10.1016/j.ejim.2016.03.007
9. Kojima, G, Iliffe, S, and Walters, K. Frailty index as a predictor of mortality: a systematic review and meta-analysis. Age Ageing. (2018) 47:193–200. doi: 10.1093/ageing/afx162
10. Rockwood, K, Hogan, DB, and MacKnight, C. Conceptualisation and measurement of frailty in elderly people. Drugs Aging. (2000) 17:295–302. doi: 10.2165/00002512-200017040-00005
11. Rockwood, K, and Mitnitski, A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. (2007) 62:722–7. doi: 10.1093/gerona/62.7.722
12. Parkerson, GR Jr, Willke, RJ, and Hays, RD. An international comparison of the reliability and responsiveness of the Duke health profile for measuring health-related quality of life of patients treated with alprostadil for erectile dysfunction. Med Care. (1999) 37:56–67. doi: 10.1097/00005650-199901000-00009
13. Kroenke, K, Spitzer, RL, and Williams, JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
14. Manusov, EG, Diego, VP, Smith, J, Garza, JR, Lowdermilk, J, Blangero, J, et al. UniMóvil: a Mobile health clinic providing primary care to the Colonias of the Rio Grande Valley, South Texas. Front Public Health. (2019) 7:215. doi: 10.3389/fpubh.2019.00215
15. Mitnitski, A, Howlett, SE, and Rockwood, K. Heterogeneity of human aging and its assessment. J Gerontol A Biol Sci Med Sci. (2017) 72:877–84. doi: 10.1093/gerona/glw089
16. Kojima, G, Iliffe, S, Jivraj, S, and Walters, K. Association between frailty and quality of life among community-dwelling older people: a systematic review and meta-analysis. J Epidemiol Community Health. (2016) 70:716–21. doi: 10.1136/jech-2015-206717
17. Souza Júnior, EV, Cruz, DP, Silva, CDS, Rosa, RS, Siqueira, LR, and Sawada, NO. Implications of self-reported fragility on the quality of life of older adults: a cross-sectional study. Rev Esc Enferm USP. (2021) 55:e20210040. doi: 10.1590/1980-220x-reeusp-2021-0040
18. Rivera-Almaraz, A, Manrique-Espinoza, B, Ávila-Funes, JA, Chatterji, S, Naidoo, N, Kowal, P, et al. Disability, quality of life and all-cause mortality in older Mexican adults: association with multimorbidity and frailty. BMC Geriatr. (2018) 18:236. doi: 10.1186/s12877-018-0928-7
19. O'Donovan, M, Sezgin, D, O'Caoimh, R, and Liew, A. The relationship between frailty and diabetes: an investigation of self-rated health, depression symptoms and quality of life in the study of health aging and retirement in Europe. Arch Gerontol Geriatr. (2021) 96:104448. doi: 10.1016/j.archger.2021.104448
20. Nguyen, AT, Nguyen, LH, Nguyen, TX, Nguyen, HTT, Nguyen, TN, Pham, HQ, et al. Frailty prevalence and association with health-related quality of life impairment among rural community-dwelling older adults in Vietnam. Int J Environ Res Public Health. (2019) 16:869. doi: 10.3390/ijerph16203869
21. Melo, LA, Jesus, ITM, Orlandi, FS, Gomes, GAO, Zazzetta, MS, Brito, TRP, et al. Frailty, depression, and quality of life: a study with elderly caregivers. Rev Bras Enferm. (2020) 73:947. doi: 10.1590/0034-7167-2018-0947
22. Liu, P, Zhang, Y, Li, Y, Li, S, Li, Y, Chen, Y, et al. Association of frailty with quality of life in older hypertensive adults: a cross-sectional study. Qual Life Res. (2021) 30:2245–53. doi: 10.1007/s11136-021-02816-2
23. Crocker, TF, Brown, L, Clegg, A, Farley, K, Franklin, M, Simpkins, S, et al. Quality of life is substantially worse for community-dwelling older people living with frailty: systematic review and meta-analysis. Qual Life Res. (2019) 28:2041–56. doi: 10.1007/s11136-019-02149-1
24. Chen, MZ, Wong, MWK, Lim, JY, and Merchant, RA. Frailty and quality of life in older adults with metabolic syndrome—findings from the healthy older people everyday (HOPE) study. J Nutr Health Aging. (2021) 25:637–44. doi: 10.1007/s12603-021-1609-3
25. Papathanasiou, IV, Rammogianni, A, Papagiannis, D, Malli, F, Mantzaris, DC, Tsaras, K, et al. Frailty and quality of life among community-dwelling older adults. Cureus. (2021) 13:e13049. doi: 10.7759/cureus.13049
26. Carver, LF, and Buchanan, D. Successful aging: considering non-biomedical constructs. Clin Interv Aging. (2016) 11:1623–30. doi: 10.2147/CIA.S117202
27. Douglas, H, Georgiou, A, and Westbrook, J. Social participation as an indicator of successful aging: an overview of concepts and their associations with health. Aust Health Rev. (2017) 41:455–62. doi: 10.1071/AH16038
28. Ma, L, Chhetri, JK, Zhang, Y, Liu, P, Chen, Y, Li, Y, et al. Integrated Care for Older People Screening Tool for measuring intrinsic capacity: preliminary findings from ICOPE pilot in China. Front Med. (2020) 7:576079. doi: 10.3389/fmed.2020.576079
29. Milman, S, Lerman, B, Ayers, E, Zhang, Z, Sathyan, S, Levine, M, et al. Frailty resilience score: a novel measure of frailty resilience associated with protection from frailty and survival. J Gerontol A Biol Sci Med Sci. (2023) 78:1771–7. doi: 10.1093/gerona/glad138
30. Pan, E, Bloomfield, K, and Boyd, M. Resilience, not frailty: a qualitative study of the perceptions of older adults towards "frailty". Int J Older People Nursing. (2019) 14:e12261. doi: 10.1111/opn.12261
31. Teater, B, and Chonody, JM. How do older adults define successful aging? A scoping review. Int J Aging Hum Dev. (2020) 91:599–625. doi: 10.1177/0091415019871207
32. Manusov, E. “Mobile Medical Van in the South Texas Colonias,” (2023). Mendeley Data, V2. Available at: http://dx.doi.org/10.17632/zz2b3wdf5r.2.
33. Kind, AJH, and Buckingham, WR. Making neighborhood-disadvantage metrics accessible—the neighborhood atlas. N Engl J Med. (2018) 378:2456–8. doi: 10.1056/NEJMp1802313
34. Mier, N, Ory, MG, Zhan, D, Conkling, M, Sharkey, JR, and Burdine, JN. Health-related quality of life among Mexican Americans living in colonias at the Texas-Mexico border. Soc Sci Med. (2008) 66:1760–71. doi: 10.1016/j.socscimed.2007.12.017
35. Brivio, P, Paladini, MS, Racagni, G, Riva, MA, Calabrese, F, and Molteni, R. From healthy aging to frailty: in search of the underlying mechanisms. Curr Med Chem. (2019) 26:3685–701. doi: 10.2174/0929867326666190717152739
36. Parkerson, GR Jr, Broadhead, WE, and Tse, CK. The Duke health profile. A 17-item measure of health and dysfunction. Med Care. (1990) 28:1056–72. doi: 10.1097/00005650-199011000-00007
37. Parkerson, GR Jr, Eisenson, HJ, and Campbell, C. Testing the Duke population health profile (Duke-PH) in a sample of community health center patients. Front Public Health. (2019) 7:248. doi: 10.3389/fpubh.2019.00248
38. Parkerson, GR Jr, Gehlbach, SH, Wagner, EH, James, SA, Clapp, NE, and Muhlbaier, LH. The Duke-UNC health profile: an adult health status instrument for primary care. Med Care. (1981) 19:806–28. doi: 10.1097/00005650-198108000-00002
39. Loecker, C, Schmaderer, M, and Zimmerman, L. Frailty in Young and middle-aged adults: an integrative review. J Frailty Aging. (2021) 10:1–7. doi: 10.14283/jfa.2021.14
40. Dury, S, Dierckx, E, van der Vorst, A, Van der Elst, M, Fret, B, Duppen, D, et al. Detecting frail, older adults and identifying their strengths: results of a mixed-methods study. BMC Public Health. (2018) 18:191. doi: 10.1186/s12889-018-5088-3
41. Henry, JD, Coundouris, SP, Mead, J, Thompson, B, Hubbard, RE, and Grainger, SA. Social frailty in late adulthood: social cognitive and psychological well-being correlates. J Gerontol B Psychol Sci Soc Sci. (2023) 78:87–96. doi: 10.1093/geronb/gbac157
42. Kalaitzaki, A, Koukouli, S, Panagiotakis, S, and Tziraki, C. Resilience in a Greek sample of informal dementia caregivers: Familism as a culture-specific factor. J Frailty Aging. (2022) 11:299–301. doi: 10.14283/jfa.2022.31
43. Petrinec, AB, Crowe, ML, Flanagan, SK, and Baker, J. Health-related quality of life of older women religious: negative influence of frailty. West J Nurs Res. (2020) 42:1088–96. doi: 10.1177/0193945920936171
44. Felten, BS, and Hall, JM. Conceptualizing resilience in women older than 85: overcoming adversity from illness or loss. J Gerontol Nurs. (2001) 27:46–53. doi: 10.3928/0098-9134-20011101-11
45. Morgan Consoli, ML, and Llamas, JD. The relationship between Mexican American cultural values and resilience among Mexican American college students: a mixed methods study. J Couns Psychol. (2013) 60:617–24. doi: 10.1037/a0033998
46. Corona, R, Rodríguez, VM, McDonald, SE, Velazquez, E, Rodríguez, A, and Fuentes, VE. Associations between cultural stressors, cultural values, and Latina/o college Students' mental health. J Youth Adolesc. (2017) 46:63–77. doi: 10.1007/s10964-016-0600-5
47. Espinoza, SE, and Hazuda, HP. Frailty prevalence and neighborhood residence in older Mexican Americans: the San Antonio longitudinal study of aging. J Am Geriatr Soc. (2015) 63:106–11. doi: 10.1111/jgs.13202
48. Verhagen, I, Ros, WJ, Steunenberg, B, and de Wit, NJ. Ethnicity does not account for differences in the health-related quality of life of Turkish, Moroccan, and Moluccan elderly in the Netherlands. Health Qual Life Outcomes. (2014) 12:138. doi: 10.1186/s12955-014-0138-8
49. Garcini, LM, Renzaho, AMN, Molina, M, and Ayala, GX. Health-related quality of life among Mexican-origin Latinos: the role of immigration legal status. Ethn Health. (2018) 23:566–81. doi: 10.1080/13557858.2017.1283392
50. Abramson, DM, Grattan, LM, Mayer, B, Colten, CE, Arosemena, FA, Bedimo-Rung, A, et al. The resilience activation framework: a conceptual model of how access to social resources promotes adaptation and rapid recovery in post-disaster settings. J Behav Health Serv Res. (2015) 42:42–57. doi: 10.1007/s11414-014-9410-2
Keywords: frailty, Mexican American, health-related quality of life, resilience, South Texas, Frailty Index
Citation: Manusov EG, Diego VP and Williams-Blangero S (2023) Frailty index in the Colonias of the Rio Grande Valley: health related quality of life and resilience. Front. Med. 10:1240494. doi: 10.3389/fmed.2023.1240494
Edited by:
Robbert Gobbens, Inholland University of Applied Sciences, NetherlandsReviewed by:
Fernando Gomez, University of Caldas, ColombiaHaider Abdul-Lateef Mousa, University of Basrah, Iraq
Copyright © 2023 Manusov, Diego and Williams-Blangero. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eron G. Manusov, ZXJvbi5tYW51c292QHV0cmd2LmVkdQ==
 Eron G. Manusov
Eron G. Manusov Vincent P. Diego
Vincent P. Diego Sarah Williams-Blangero
Sarah Williams-Blangero