- 1Carrera de Atención Prehospitalaria y en Emergencias, Universidad Central del Ecuador, Quito, Ecuador
- 2Facultad de Medicina, Carrera de Atención Prehospitalaria y en Emergencias, Universidad UTE, Quito, Ecuador
- 3Medignosis, Medical Research Department, Quito, Ecuador
- 4Escuela de Medicina, Universidad de las Américas (UDLA), Quito, Ecuador
Background: Emergency medical services (EMS) and critical care transport crews constantly face critically-ill patients who need ventilatory support in scenarios where correct interventions can be the difference between life and death; furthermore, challenges like limited staff working on the patient and restricted spaces are often present. Due to these, mechanical ventilation (MV) can be a support by liberating staff from managing the airway and allowing them to focus on other areas; however, these patients face many complications that personnel must be aware of.
Aims: To establish the main complications related to out-of-hospital MV and ventilatory support through a systematic review.
Methodology: PubMed, BVS and Scopus were searched from inception to July 2021, following the PRISMA guidelines; search strategy and protocol were registered in PROSPERO. Two authors carried out an independent analysis of the articles; any disagreement was solved by mutual consensus, and data was extracted on a pre-determined spreadsheet. Only original articles were included, and risk of bias was assessed with quality assessment tools from the National Institutes of Health.
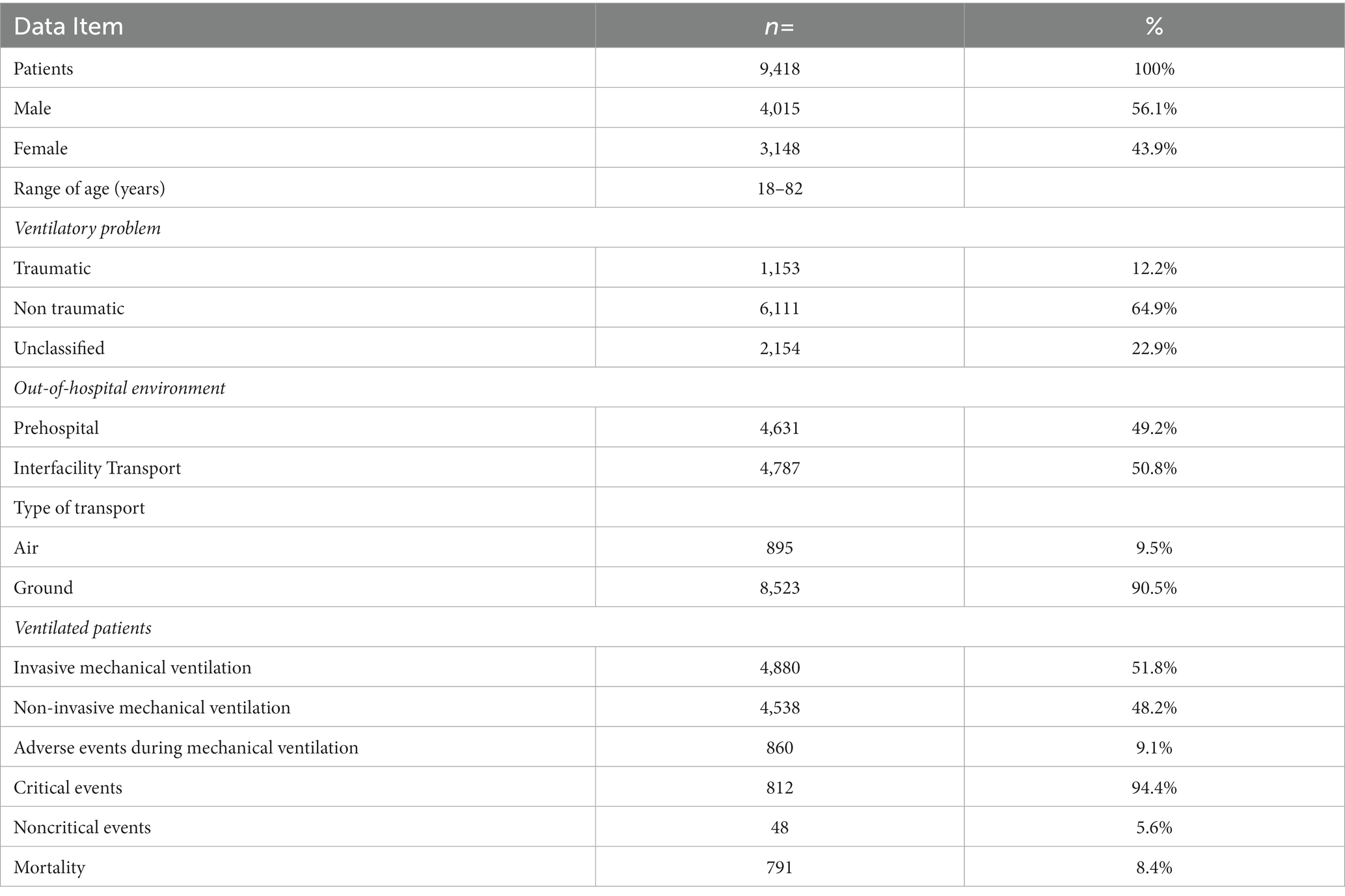
Results: The literature search yielded a total of 2,260 articles, of which 26 were included in the systematic review, with a total of 9,418 patients with out-of-hospital MV; 56.1% were male, and the age ranged from 18 to 82 years. In general terms of aetiology, 12.2% of ventilatory problems were traumatic in origin, and 64.8% were non-traumatic, with slight changes between out-of-hospital settings. Mechanical ventilation was performed 49.2% of the time in prehospital settings and 50.8% of the time in interfacility transport settings (IFTS). Invasive mechanical ventilation was used 98.8% of the time in IFTS while non-invasive ventilation was used 96.7% of the time in prehospital settings. Reporting of adverse events occurred in 9.1% of cases, of which 94.4% were critical events, mainly pneumothorax in 33.1% of cases and hypotension in 27.6% of cases, with important considerations between type of out-of-hospital setting and ventilatory mode; total mortality was 8.4%.
Conclusion: Reported adverse events of out-of-hospital mechanical ventilation vary between settings and ventilatory modes; this knowledge could aid EMS providers in promptly recognizing and resolving such clinical situations, depending on the type of scenario being faced.
Introduction
Emergency medical services and critical care transport crews are constantly facing critical patients who need ventilatory support for acute respiratory failure (ARF), airway protection in traumatic injuries, and high levels of sedation (1–3). The survival rate and favourable outcomes depend on the capacity to maintain physiologic end-tidal carbon dioxide (ETCO2) and oxygen levels and appropriate tidal volumes (1, 4, 5). The current methods used to achieve those goals in a prehospital setting include a bag-valve-mask device (BVM) and mechanical ventilation (MV).
Manual ventilation with a BVM is typically used for its dynamic and inexpensive applications; its use also requires less training when compared to MV – which can be complex and expensive (1). However, in an out-of-hospital setting (prehospital and interfacility), where limited staff, space, and equipment are common, MV can become a great ally, freeing the provider to attend to other urgent necessities (4). BVM and MV were considered equivalent for many years (6), but the reality is different; manual ventilation can maintain a physiologic ETCO2 only 16.7% of the time and provides inappropriate vital volumes – sometimes resulting in barotrauma (1, 7).
Mechanical ventilation through the means of either an instrument inside the trachea, named invasive mechanical ventilation (IMV), or without endotracheal devices, named non-invasive mechanical ventilation (NIMV), has demonstrated effective outcomes (8, 9). NIMV is useful in conscious patients who can maintain airway patency and is indicated mainly for chronic obstructive pulmonary disease (COPD), asthma exacerbations, and acute pulmonary oedema; it works by providing positive inspiratory pressure and maintaining end-expiratory pressure (PEEP), resulting in reduced inspiratory muscle work and fatigue (10). The main modalities used are continuous positive airway pressure (CPAP) or bilevel inspiratory positive airway pressure (BiPAP), which have shown reduced mortality and intubation rates in acute respiratory failure (11).
IMV is indicated when NIMV and other therapies have failed or when advanced airway management is needed to maintain patency and support severe injuries or illnesses (i.e., when controlled pulmonary pressures and specific parameters are needed) (1, 10). In contrast with NIMV, exact target parameters can be met by controlling pressure and/or volume and by using available pre-programmed modes (10). However, management of a mechanical ventilator requires specialized training and has a steep learning curve due to the high morbidity and mortality that ensue if the ventilatory settings are incorrect or monitoring is not done properly (1, 12). Patients can be exposed to iatrogenic ventilator-induced lung injury and disturbances in blood gases (i.e., hypocapnia, hypercapnia, hypoxia, and hyperoxia), especially when the aforementioned training is not done properly (10, 12).
Knowledge of these complications as well as the ventilatory modes used in an out-of-hospital setting can be helpful for EMS and critical care transport crews; such information can enable them to reduce mortality, identify the main ventilatory settings used in the field for mechanical ventilation, and anticipate the main adverse events that can arise during the procedure, reducing morbidity.
Methods
Protocol and registration
This study was made following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines. The research protocol as well as the full search criteria were uploaded and registered in PROSPERO (CRD42021279433).
Eligibility criteria
The language of the included studies was limited to English and Spanish. The eligibility criteria used can be found in Table 1.
All available studies, from the inception of the databases to July 28, 2021 were included.
Information sources
Studies were identified in PubMed, Scopus, and Biblioteca Virtual en Salud (BVS); the references of selected articles were also screened, and only one additional reference was extracted (13). No filters were used. BVS includes scientific literature from Latin America and the Caribbean, mainly written in Spanish; inclusion of such studies is limited in most systematic reviews that only consider the English language and therefore neglect literature from the Latin-American region, where traumatic events are highly prevalent.
Search
A search protocol was established, which can be found in the aforementioned PROSPERO registration. Search terms were tailored based on the PICO framework and the eligibility criteria; the following key terms, with variations, were used: mechanical ventilation, ventilation, out-of-hospital, mortality, safety, and adverse events.
Study selection
Two blinded reviewers conducted an independent and uniform evaluation of the chosen studies. Deduplication was performed automatically using Mendeley Reference Manager and two stages of screening were performed. The first stage involved the screening of titles and abstracts, while the second stage involved full-text review; after these, the data of the selected studies was extracted in a spreadsheet. Any discrepancies between the reviewers were resolved by discussion and mutual consensus.
Data items and collection process
For data extraction, we developed a spreadsheet with the following information: author, type of study, year of publication, number of ventilated patients, sex, age, type of out-of-hospital scenario (prehospital or interhospital as well as air or ground transport), ventilatory problem (traumatic, non-traumatic, and unclassified when the information provided in the study was not sufficient to classify the ventilatory problem), origin of the ventilatory problem (pulmonary, COVID-19, cardiovascular, neurologic, obstetric, septic, and other; unclassified was used when the author did not describe the origin of the problem), type of ventilation (invasive or non-invasive), mechanical ventilation mode (volume control, pressure control, pressure support, continuous airway pressure, CPAP+PS/BiPAP, and others), adverse events (divided in critical and non-critical), and mortality (divided in transport mortality and hospital mortality). If data was missing or inconsistent, we attempted to contact the authors; if they did not answer after repeated attempts, we considered it lost data. To note, due to the different illnesses of patients between out-of-hospital settings (prehospital and interfacility transport) and types of ventilation required (invasive or non-invasive) we decided to analyse them as different populations.
Risk of bias in individual studies
Both reviewers assessed the risk of bias independently using the Study Quality Assessment Tools from the National Institutes of Health (NIH). Studies were graded as either minimally low, moderately low, or high risk of bias. If answering yes in less than 50% of the questions, the study was graded as poor and hence had a high risk of bias; if between 50 and 79%, it was graded as fair and hence had a moderately low risk of bias; and if 80% or more, it was graded as good and hence had a minimally low risk of bias, as done in a previous review (14).
Results
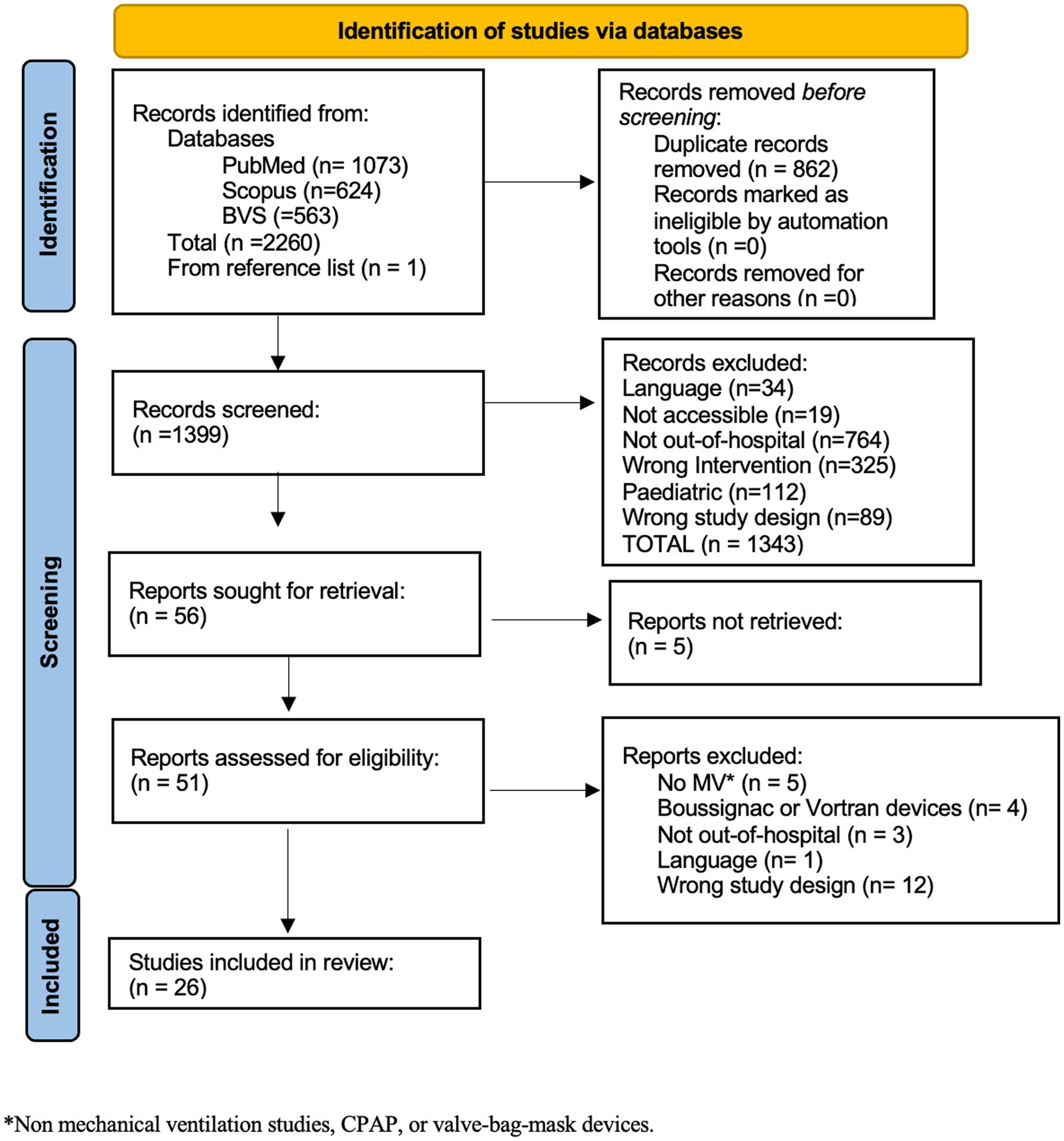
The searches from the inception of the databases to July 28, 2021 yielded a total of 2,260 results. Following the removal of duplicate entries, a subset of 1,399 articles remained for further evaluation during the screening phase. The complete process of article screening can be found in Figure 1.
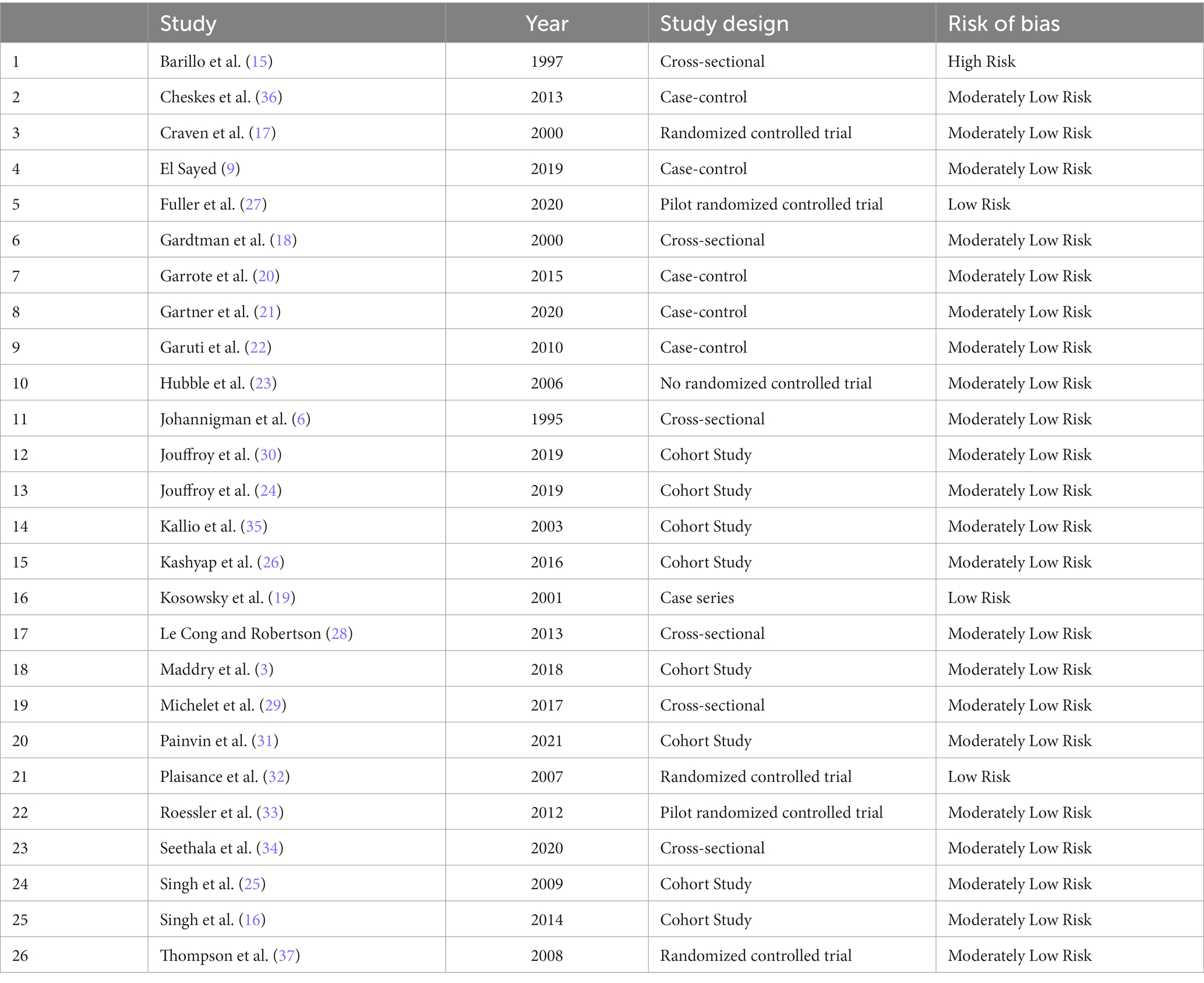
A total of 26 studies were finally included (3, 6, 9, 15-37); these studies, with their year of publication, design, and bias assessment, are shown in Table 2.
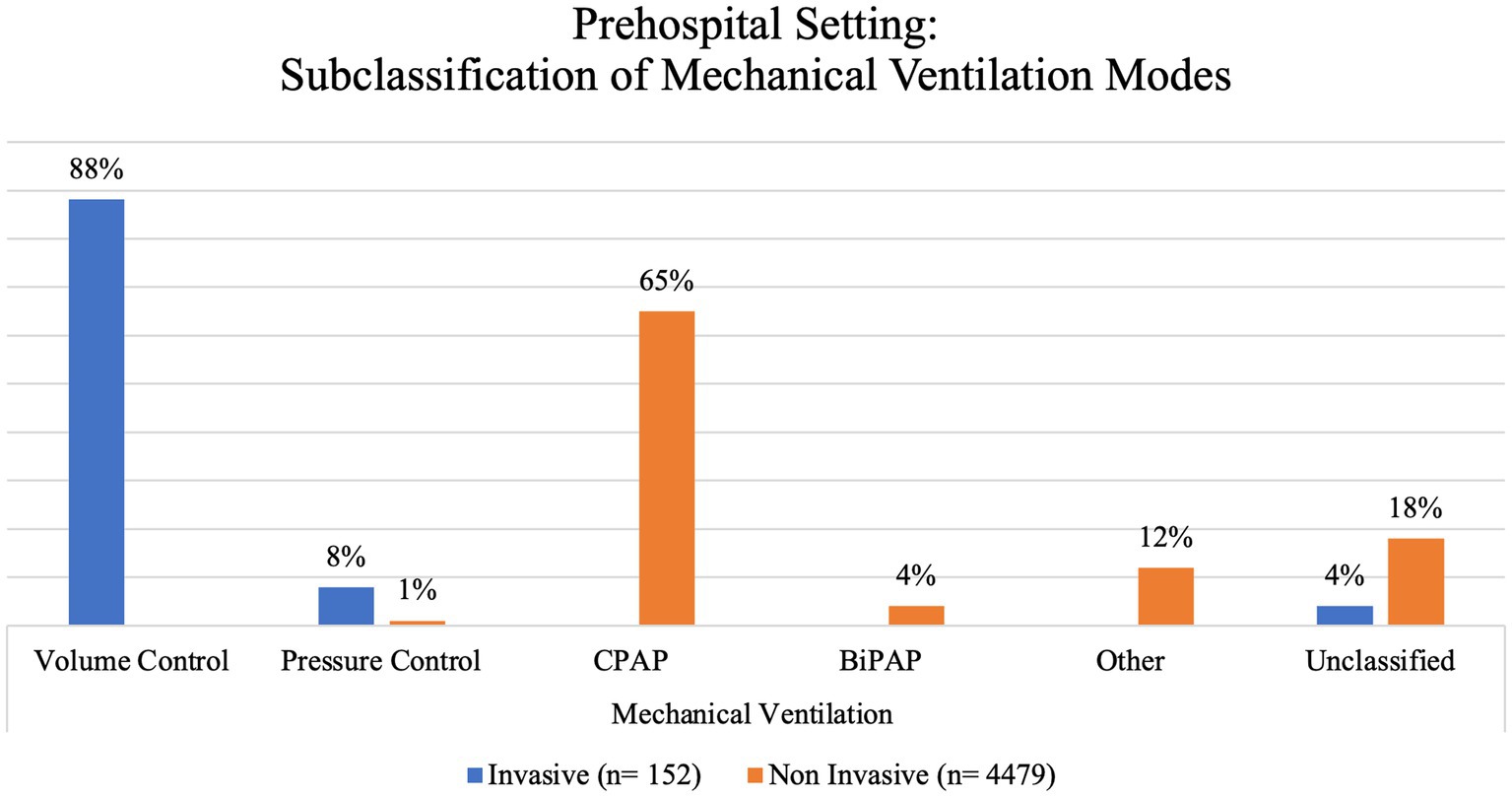
A total of 9,418 patients who received out-of-hospital mechanical ventilation were included in our research. Among these individuals, 56.1% were identified as male. The age range of all participants spanned from 18 to 82 years. In the context of the out-of-hospital setting, 49.2% of patients received MV in a prehospital setting, while the remaining received it in an IFTS. In the prehospital setting, the prevailing ventilatory mode was found to be CPAP (NIMV), administered to a total of 2,911 patients. In contrast, volume control (IMV) was administered to 1,702 patients in the IFTS. A general summary of all ventilated patients can be found in Table 3.
Mechanical ventilation in the prehospital setting
In prehospital settings, a total of 4,631 patients underwent mechanical ventilation. Among these patients, 49% were identified as female. Notably, NIMV was the primary method of ventilatory support in 96.7% of the instances, while just 3.3% of the cases used IMV. We further subclassified these based on the ventilatory mode used (Figure 2).
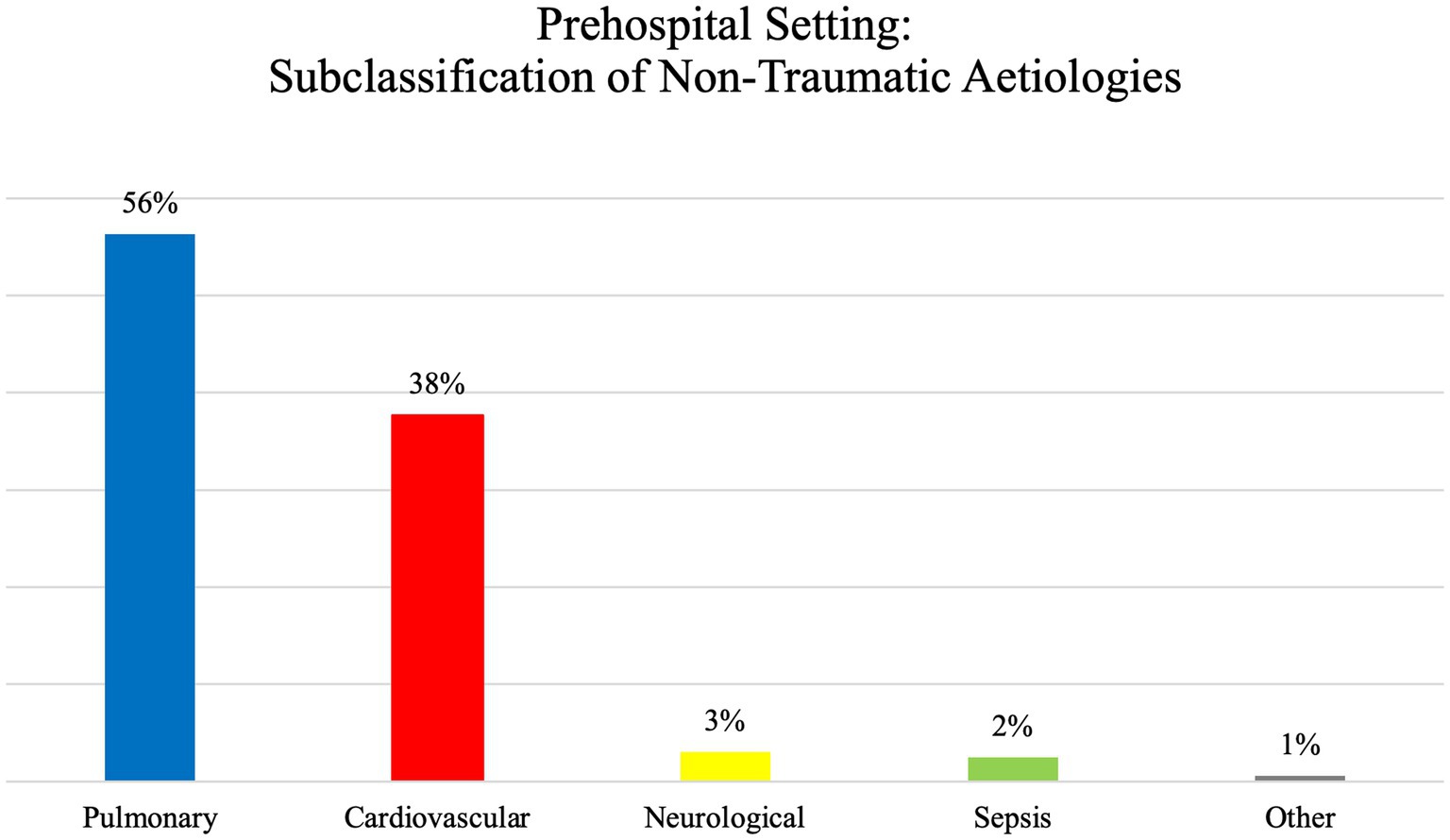
The analysis of the data indicates that non-traumatic ventilatory causes are more prevalent than traumatic ventilatory causes in the prehospital setting, accounting for 94.6 and 5.4%, respectively. Please see Figure 3 for the subclassification of non-traumatic aetiologies.
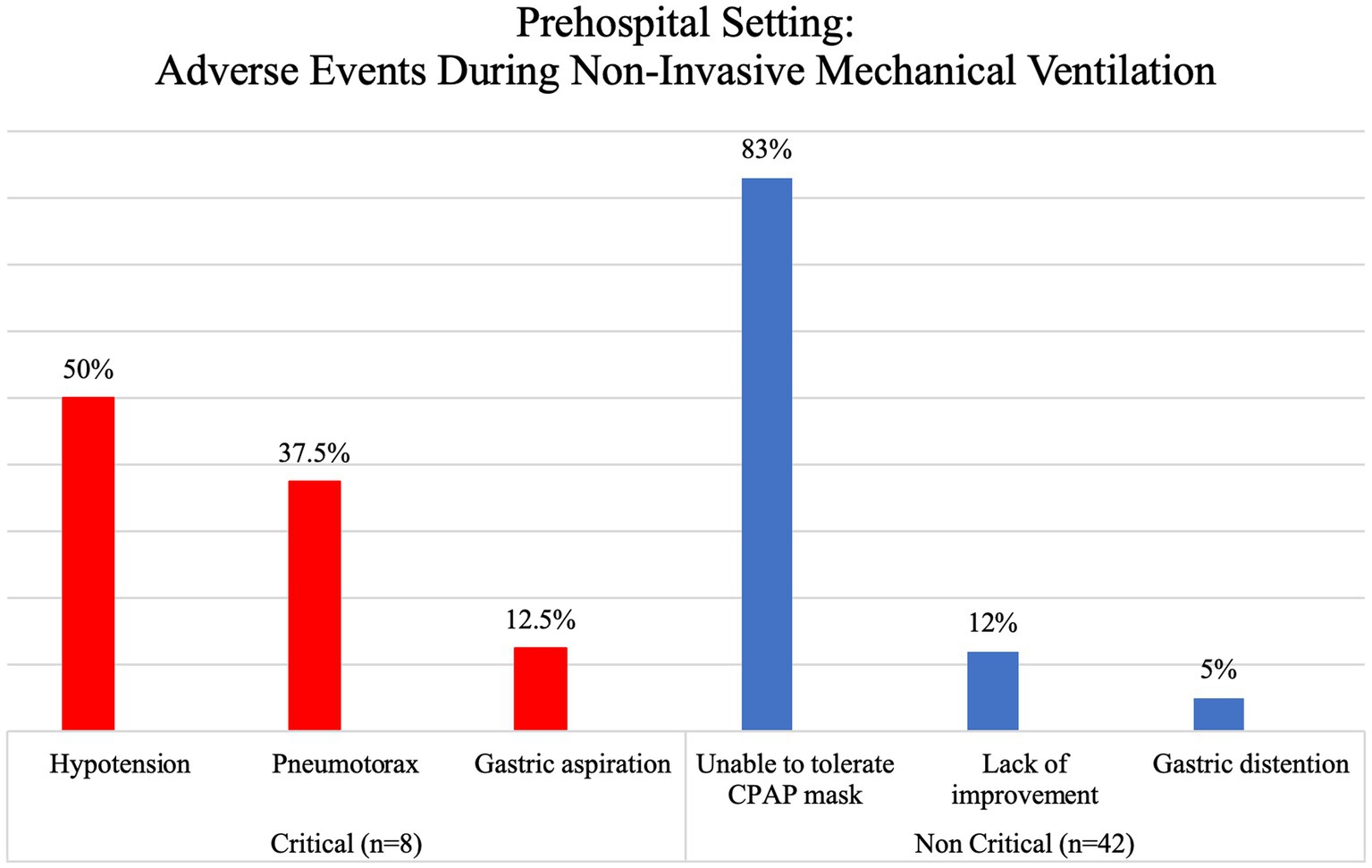
Adverse events that were seen during ventilation in the prehospital setting were documented in 1.8% of patients. These events were categorized based on their potential to cause life-threatening situations, with critical events accounting for 16% and non-critical events accounting for 84% of the reported cases. It is worth noting that adverse events were only recorded in relation to NIMV, as shown in Figure 4. The most critical events seen in this study were hypotension, which occurred in 50% of cases, and pneumothorax, which occurred in 37.5% of cases. These events were predominantly observed in patients with non-traumatic injuries, namely those with cardiovascular or pulmonary illnesses.
The vast majority of pre-hospital transfers, accounting for 99.6% of cases, were conducted by ground transportation. Among these cases, 661 patients, or 14.2% of the total, were reported to have died upon admission. Notably, no fatalities were recorded during the actual transport phase in the dataset under analysis.
Mechanical ventilation in the interfacility transport setting
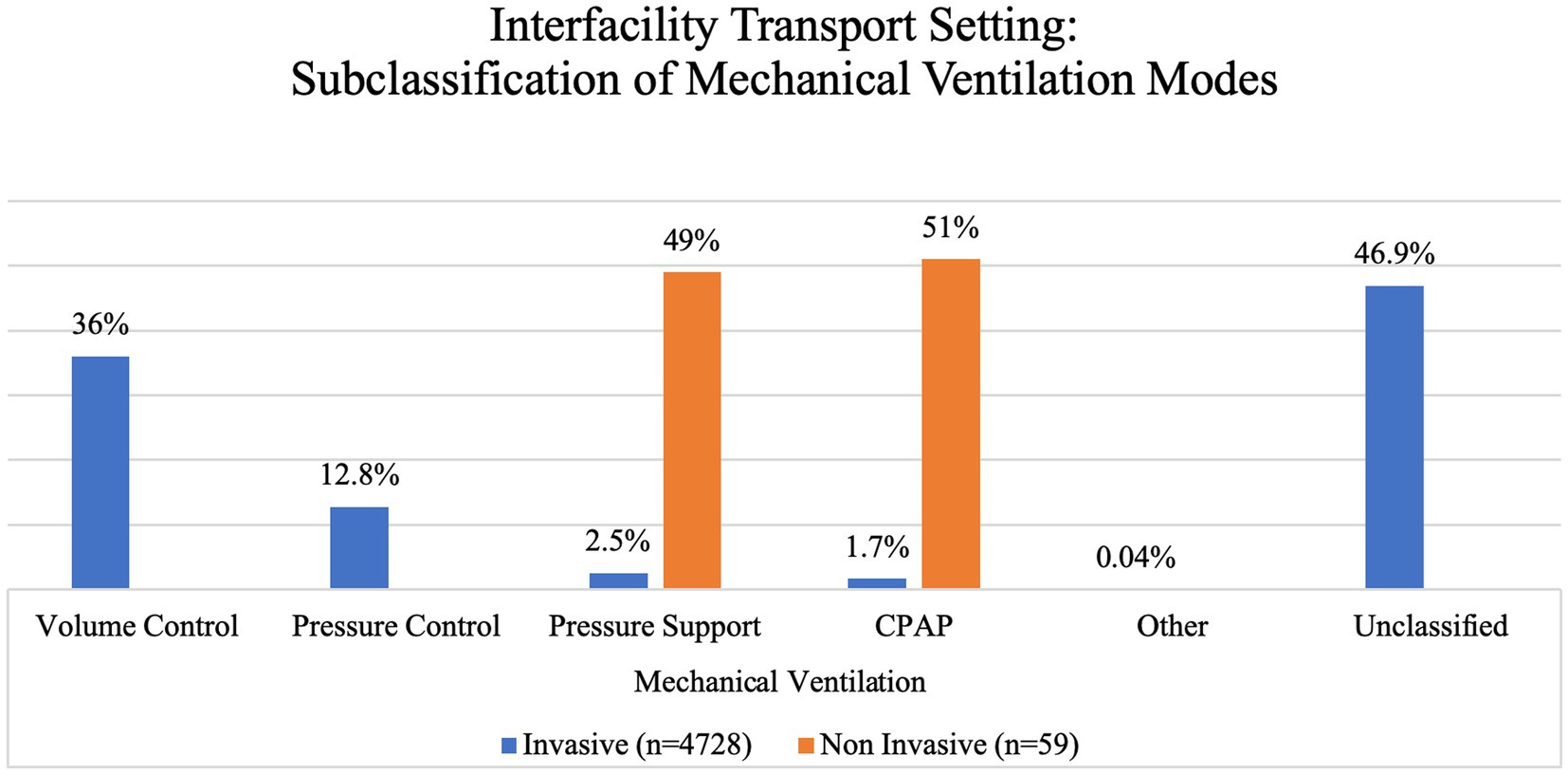
In the IFTS, a total of 4,787 individuals underwent mechanical ventilation. Among these, 68% were male and the majority (98.8%) got IMV as their primary form of ventilatory support, while a smaller proportion (1.2%) used NIMV. We further subclassified these based on the ventilatory mode used (Figure 5).
Similar to the prehospital setting, non-traumatic causes of ventilatory issues were more often seen than traumatic causes, with a prevalence of 36.1% compared to 20.8%. Please refer to Figure 6 for a breakdown of the subcategories of non-traumatic causes. Unfortunately, in this group, there was an important lack of data that prevented us from classifying the aetiology of the ventilatory problems (43.1% had to be categorized as unclassified).
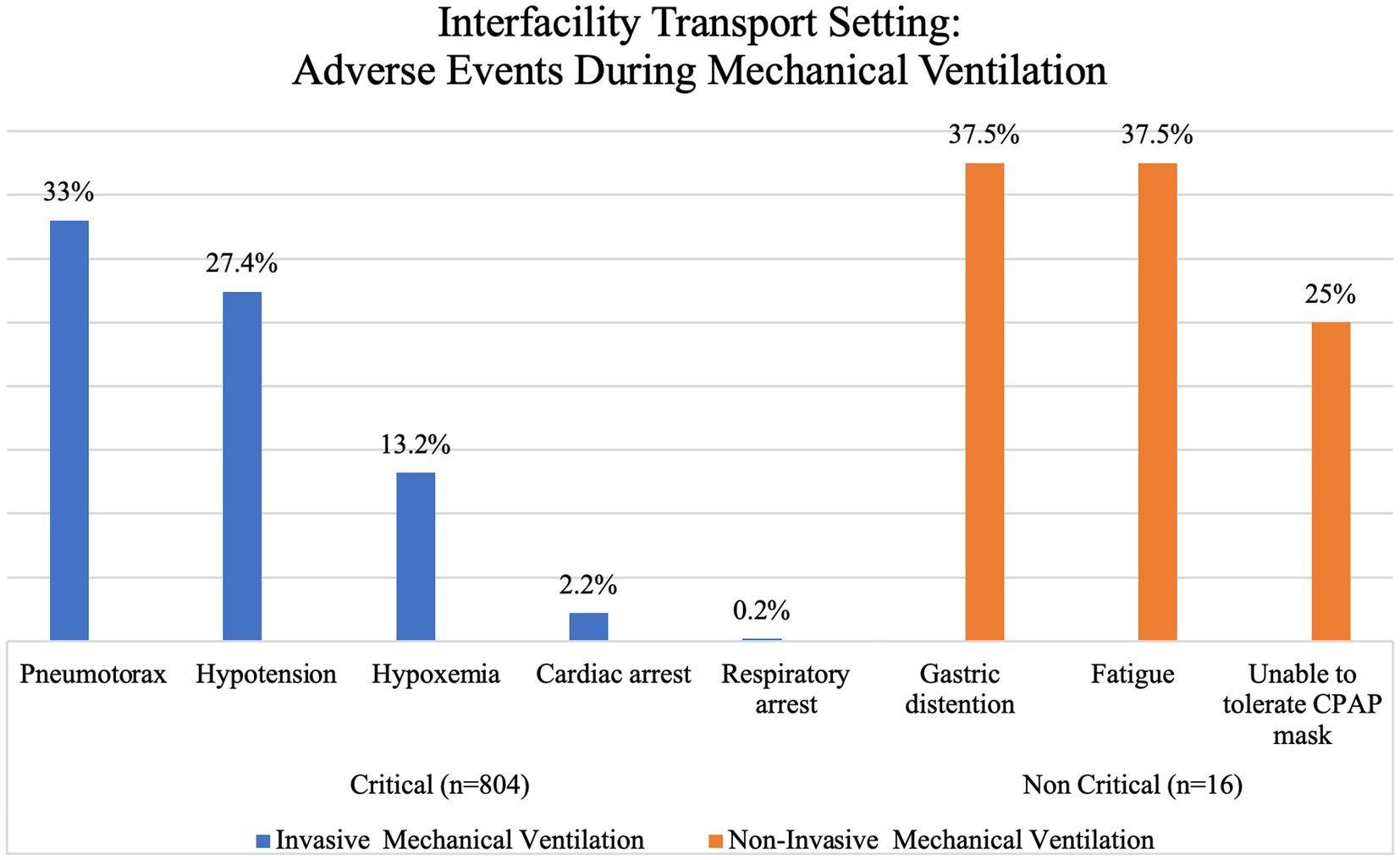
Reported adverse events during ventilation in the IFTS occurred in 16.9% of patients. Among these occurrences, 99.3% were classified as critical, while the remaining 0.7% were considered non-critical. The majority of adverse events were recorded in patients receiving IMV, accounting for 97.5% of cases, while only 2.5% of cases were associated with NIMV. Each of these categories was further divided into specific types of events and presented in Figure 7. The two main critical events reported in this group of patients were pneumothorax (33%), mainly in traumatic illnesses (i.e., blast or penetrating injuries), and hypotension (27.4%), mainly in non-traumatic injuries (i.e., cardiovascular or pulmonary illness). It is noteworthy that despite the relatively high occurrence of these events, overall mortality remained relatively low at 3%.
The majority of interfacility transports, around 82%, were conducted via land transportation, while the remaining proportion used air transport. Among the whole population of mechanically ventilated patients in the IFTS, a mortality rate of 3% was observed upon arrival. No instances of death were recorded during the transit phase in the data that was analysed.
Discussion
This systematic review was performed to assess the use of out-of-hospital mechanical ventilation, its features, reported adverse events, and mortality.
The attention of critically-ill patients in out-of-hospital settings is a challenge for EMS and critical care transport crews that need to expertly handle multiple complex procedures and therapies in a limited physical space with minimal equipment and staff – often following different protocols based on the institution or regulatory bodies of the country (16). The use of equipment in these instances, either at the location of attention or during transportation between centres, can help prolong life until definitive care in a hospital (16). In the course of these events, the EMS and critical care transport crews need to recognize all possible life-threatening conditions associated with the illness, as well as the adverse events that may arise from the use of devices, in order to prevent them from happening (16). However, it should be noted that our study does not establish a direct causal relationship between complications and mechanical ventilation, primarily due to limitations in the design and available information in the studies included. Nonetheless, our study does emphasize the frequency of adverse events in patients receiving mechanical ventilation. It underscores the importance of considering these complications when managing patients with traumatic or non-traumatic conditions, providing an opportunity to proactively address them based on the specific patient characteristics, the mode of mechanical ventilation employed, or the type of out-of-hospital setting.
Mechanical ventilation was typically used in hospitals, but over time this procedure became increasingly common in the prehospital setting – during transports and primary attention (6, 10, 38). In our study, we found an ample range of ages (18–82), which might be due to the fact that this procedure is being used more frequently in young people due to traumatic conditions such as burns, brain lesions, and combat injuries (3, 15), while still being beneficial for older adults that usually have chronic conditions or emergent conditions elicited by previous illnesses like acute cardiogenic pulmonary oedema or exacerbations of chronic obstructive pulmonary disease (COPD) (18, 19).
Mechanical ventilation during interfacility transport is more common than in the prehospital setting, especially during ground transport, which happens to be the most common modality due to higher availability and lower cost when compared to air ambulances (39); in our study, 90.5% were transported by ground using a variety of ventilatory modalities.
The means of mechanical ventilation were evenly distributed between invasive 51.8% (mainly in IFTS) and non-invasive 48.2% (mainly in prehospital settings). NIMV was represented primarily by CPAP (64.4%), which is not surprising given that previous studies have shown improvement on vital signs, reduction in short-term mortality, and less need for endotracheal intubation in patients with acute pulmonary oedema and chronic obstructive pulmonary disease (COPD) when using this ventilatory mode (40–42). In contrast, the main modality for IMV in out-of-hospital settings was volume control ventilation (37.6%), while the unclassified category represented 45.6% of all IMV patients. Showcasing that, studies assessing IMV in a prehospital setting often do not provide enough information to clearly determine the modality being used, leading to the loss of valuable information such as detecting common complications of each modality that might differ from those in a hospital setting. This is especially concerning when considering that the correct use of a ventilator with lung-protective parameters by properly trained prehospital professionals increases survival by improving the chances of accessing appropriate medical care (3, 24).
Adverse events
Hypotension and pneumothorax
Critically ill patients can face multiple adverse events during out-of-hospital care – evidence suggests an incidence of one in fifteen transports, with hypotension being a common complication in 4.4–11.9% of cases (16, 25, 43). This contrasts with our findings that show a higher incidence of pneumothorax than of hypotension (33% vs. 27.4%) in IFTS, possibly due to the underlying condition that required ventilation in the first place; however, in the pre-hospital setting, hypotension does show a higher incidence than pneumothorax (50% vs. 37.5%). However, we could not directly correlate hypotension or pneumothorax with the use of out-of-hospital mechanical ventilation due to the lack of complete data in the available evidence that would allow us to establish causality. Regardless of the aetiology, EMS and critical care transport personnel that use mechanical ventilation in out-of-hospital settings must be on high alert for such events and be prepared to solve them when they arise.
Oxygen levels
Hypoxia is a common condition in the prehospital setting, often requiring ventilatory support (44–46). Although this adverse event was less common than hypotension or pneumothorax in our analysis (13.1%), the EMS and critical care transport crews need to take it into account and monitor closely the oxygen availability and consumption along the transport; an ample supply of oxygen should be available in the vehicle, especially when expecting to travel long distances.
Although hypoxia is frequently discussed in the literature, hyperoxia – which can go unnoticed – is equally harmful to the patient; hence, prehospital responders must target SpO2 values above 94% and below 96% (30, 47).
Mortality
Although our reported mortality is relatively low – 8.4% overall for out-of-hospital mortality, 3% for the IFTS, and 14.3% for the prehospital setting – it correlates with epidemiological prehospital mortality studies in airlifted and ground patients (8.2 and 14.6%, respectively) (48). Continuing education and appropriate training of responders might help in improving the safety of this procedure. We performed a sub-analysis that revealed that most of the mortality occurred in airlifted patients; however, this is more likely explained by the severity of illness (requiring faster transport through the air) than by the direct effect of the type of transport or the use of mechanical ventilation. Therefore, we encourage out-of-hospital personnel to train in the proper use of all of their available devices, including the mechanical ventilator, in order to provide the best treatment possible until definitive care can be obtained.
Limitations
Our analysis was dependent on the quality of the data in the included studies, some of which lacked specific information that prevented an in-depth analysis of correlations or causality between mechanical ventilation and patient complications due to high heterogeneity. Regardless of comparators, when all patients who received the intervention are considered, less than 10% suffered an adverse event or manifestation of the underlying pathology associated with the condition that led to the intervention. Most of the studies analysed transported patients as a whole (i.e., including ventilated and non-ventilated), which precluded a subgroup exploration of aetiology, diagnosis, and complications or number of complications per patient of only those being mechanically ventilated; almost 22% of the patients included in this review had to be categorized as “unclassified” due to missing information. Additionally, there was little information regarding the ventilatory modes used and ventilatory settings, especially with IMV, which prevented us from properly assessing if the ventilatory modality was related to mortality or morbidity.
Conclusion
The mechanical ventilator can be a helpful device in an out-of-hospital setting given that it liberates EMS and critical care transport personnel to provide support for the patient’s condition during the transport in different areas other than ventilation. Additionally, achieving proper ventilatory parameters – while avoiding hypoxemia, low or high tidal volumes, and hypo or hypercapnia – becomes easier and significantly superior to using the BVM device.
Adverse events in out-of-hospital mechanical ventilation vary depending on the type of out-of-hospital setting and ventilatory mode. Although adverse events around mechanical ventilation are limited, the EMS and critical care transport crews must be trained and prepared to promptly recognize them or identify conditions that can lead to them; training and continuing education are paramount to achieving this.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
RP-V: conceptualization, data curation, formal analysis, investigation, visualization, writing – original draft preparation, and writing – review & editing. JL-R: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, and writing – review & editing. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the (Dirección General de Investigación y Vinculación, Universidad de Las Américas, Quito, Ecuador).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ARF, acute respiratory failure; BiPAP, bilevel inspiratory positive airway pressure; BVM, Bag-Valve-Mask-Device; BVS, Biblioteca Virtual en Salud; COPD, chronic obstructive pulmonary disease; CPAP, continuous positive airway pressure; ETCO2, end-tidal carbon dioxide; IFTS, interfacility transport settings; IMV, invasive mechanical ventilation; MV, mechanical ventilation; NIH, National Institutes of Health; NIMV, non-invasive mechanical ventilation; PEEP, end-expiratory pressure; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
References
1. McLachlan, B, Bilbrey, C, Mausner, K, and Lenz, TJ. Effectiveness of manual ventilation in intubated helicopter emergency services-transported trauma patients. Air Med J. (2019) 38:273–5. doi: 10.1016/j.amj.2019.03.013
2. Williams, TA, Finn, J, Perkins, GD, and Jacobs, IG. Prehospital continuous positive airway pressure for acute respiratory failure: a systematic review and meta-analysis. Prehosp Emerg Care. (2013) 17:261–73. doi: 10.3109/10903127.2012.749967
3. Maddry, JK, Mora, AG, Savell, SC, Perez, CA, Mason, PE, Aden, JK, et al. Impact of critical care air transport team (CCATT) ventilator management on combat mortality. J Trauma Acute Care Surg. (2018) 84:157–64. doi: 10.1097/TA.0000000000001607
4. Weiss, SJ, Ernst, AA, Jones, R, Ong, M, Filbrun, T, Augustin, C, et al. Automatic transport ventilator versus bag valve in the EMS setting: a prospective, randomized trial. South Med J. (2005) 98:970–6. doi: 10.1097/01.smj.0000182177.01436.70
5. COMACARE study groupJakkula, P, Reinikainen, M, Hästbacka, J, Pettilä, V, Loisa, P, et al. Targeting low- or high-normal carbon dioxide, oxygen, and mean arterial pressure after cardiac arrest and REsuscitation: study protocol for a randomized pilot trial. Trials. (2017) 18:507. doi: 10.1186/s13063-017-2257-0
6. Johannigman, JA, Branson, RD, Johnson, DJ, Davis, K, and Hurst, JM. Out-of-hospital ventilation: bag-valve device vs transport ventilator. Acad Emerg Med. (1995) 2:719–24. doi: 10.1111/j.1553-2712.1995.tb03624.x
7. Siegler, J, Kroll, M, Wojcik, S, and Moy, HP. Can EMS providers provide appropriate tidal volumes in a simulated adult-sized patient with a pediatric-sized bag-valve-mask? Prehosp Emerg Care. (2017) 21:74–8. doi: 10.1080/10903127.2016.1227003
8. Pandor, A, Thokala, P, Goodacre, S, Poku, E, Stevens, JW, Ren, S, et al. Pre-hospital non-invasive ventilation for acute respiratory failure: a systematic review and cost-effectiveness evaluation. Health Technol Assess. (2015) 19:1–102. doi: 10.3310/hta19420
9. El Sayed, MJ, Tamim, H, Mailhac, A, and Mann, NC. Impact of prehospital mechanical ventilation: a retrospective matched cohort study of 911 calls in the United States. Medicine. (2019) 98:e13990. doi: 10.1097/MD.0000000000013990
10. Rose, L. Management of critically ill patients receiving noninvasive and invasive mechanical ventilation in the emergency department. Open Access Emerg Med. (2012) 4:5–15. doi: 10.2147/OAEM.S25048
11. Goodacre, S, Stevens, JW, Pandor, A, Poku, E, Ren, S, Cantrell, A, et al. Prehospital noninvasive ventilation for acute respiratory failure: systematic review, network meta-analysis, and individual patient data meta-analysis. Acad Emerg Med. (2014) 21:960–70. doi: 10.1111/acem.12466
12. Stephens, RJ, Siegler, JE, and Fuller, BM. Mechanical ventilation in the prehospital and emergency department environment. Respir Care. (2019) 64:595–603. doi: 10.4187/respcare.06888
13. Sahu, AK, Timilsina, G, Mathew, R, Jamshed, N, and Aggarw, P. “Six-dial strategy”-mechanical ventilation during cardiopulmonary resuscitation. Indian J Crit Care Med. (2020) 24:487–9. doi: 10.5005/jp-journals-10071-23464
14. Ghaffari-Rafi, A, Peterson, C, Leon-Rojas, JE, Tadokoro, N, Lange, SF, Kaushal, M, et al. The role of magnetic resonance imaging to inform clinical decision-making in acute spinal cord injury: a systematic review and meta-analysis. J Clin Med. (2021) 10:4948. doi: 10.3390/jcm10214948
15. Barillo, DJ, Dickerson, EE, Cioffi, WG, Mozingo, DW, and Pruitt, BA. Pressure-controlled ventilation for the long-range aeromedical transport of patients with burns. J Burn Care Rehabil. (1997) 18:200–5. doi: 10.1097/00004630-199705000-00004
16. Singh, JM, MacDonald, RD, and Ahghari, M. Critical events during land-based interfacility transport. Ann Emerg Med. (2014) 64:9–15. doi: 10.1016/j.annemergmed.2013.12.009
17. Craven, RA, Singletary, N, Bosken, L, Sewell, E, Payne, M, and Lipsey, R. Use of bilevel positive airway pressure in out-of-hospital patients. Acad Emerg Med. (2000) 7:1065–8.
18. Gardtman, M, Waagstein, L, Karlsson, T, and Herlitz, J. Has an intensified treatment in the ambulance of patients with acute severe left heart failure improved the outcome? Eur J Emerg Med. (2000) 7:15–24.
19. Kosowsky, JM, Stephanides, SL, Branson, RD, and Sayre, MR. Prehospital use of continuous positive airway pressure (CPAP) for presumed pulmonary edema: a preliminary case series. Prehosp Emerg Care. (2001) 5:190–6.
20. Garrote, JI, Aylagas, D, Gutierrez, JM, Sinisterra, JA, Gowran, BM, Medina, A, et al. Noninvasive Mechanical Ventilation in Helicopter Emergency Medical Services Saves Time and Oxygen and Improves Patient and Mission Safety: A Pilot Study. Air Med J. (2015) 34:218–22.
21. Gartner, BA, Fehlmann, C, Suppan, L, Niquille, M, Rutschmann, OT, and Sarasin, F. Effect of noninvasive ventilation on intubation risk in prehospital patients with acute cardiogenic pulmonary edema: a retrospective study. Eur J Emerg Med. (2020) 27:54–8.
22. Garuti, G, Bandiera, G, Cattaruzza, MS, Gelati, L, Osborn, JF, Toscani, S, et al. Out-of-hospital helmet CPAP in acute respiratory failure reduces mortality: a study led by nurses. Monaldi Arch Chest Dis. (2010) 73:145–51.
23. Hubble, MW, Richards, ME, Jarvis, R, Millikan, T, and Young, D. Effectiveness of prehospital continuous positive airway pressure in the management of acute pulmonary edema. Prehosp Emerg Care. (2006) 10:430–9.
24. Jouffroy, R, Saade, A, Pegat-Toquet, A, Philippe, P, Carli, P, and Vivien, B. Pre-hospital mechanical ventilation in septic shock patients. Am J Emerg Med. (2019) 37:1860–3. doi: 10.1016/j.ajem.2018.12.047
25. Singh, JM, Ferguson, ND, MacDonald, RD, Stewart, TE, and Schull, MJ. Ventilation practices and critical events during transport of ventilated patients outside of hospital. Prehospital Emerg Care. (2009) 13:316–23. doi: 10.1080/10903120902935264
26. Kashyap, R, Anderson, PW, Vakil, A, Russi, CS, and Cartin-Ceba, R. A retrospective comparison of helicopter transport versus ground transport in patients with severe sepsis and septic shock. Int. J Emerg Med. (2016) 9.
27. Fuller, G, Keating, S, Goodacre, S, Herbert, E, Perkins, G, Rosser, A, et al. Is a definitive trial of prehospital continuous positive airway pressure versus standard oxygen therapy for acute respiratory failure indicated? The ACUTE pilot randomised controlled trial. BMJ Open. (2020) 10:e035915.
28. Le Cong, M, and Robertson, A. A 3-year retrospective audit of the use of noninvasive positive pressure ventilation via the Oxylog 3000 transport ventilator during air medical retrievals. Air Med J. (2013) 32:126–8.
29. Michelet, P, Bouzana, F, Charmensat, O, Tiger, F, Durand-Gasselin, J, Hraiech, S, et al. Acute respiratory failure after drowning: A retrospective multicenter survey. Eur J Emerg Med. (2017) 24:295–300.
30. Jouffroy, R, Saade, A, Saint Martin, LC, Philippe, P, Carli, P, and Vivien, B. Prognosis value of partial arterial oxygen pressure in patients with septic shock subjected to pre-hospital invasive ventilation. Am J Emerg Med. (2019) 37:56–60. doi: 10.1016/j.ajem.2018.04.050
31. Painvin, B, Messet, H, Rodriguez, M, Lebouvier, T, Chatellier, D, Soulat, L, et al. Inter-hospital transport of critically ill patients to manage the intensive care unit surge during the COVID-19 pandemic in France. Ann Intensive Care. (2021):11.
32. Plaisance, P, Pirracchio, R, Berton, C, Vicaut, E, and Payen, D. A randomized study of out-of-hospital continuous positive airway pressure for acute cardiogenic pulmonary oedema: physiological and clinical effects. Eur Heart J. (2007) 28:2895–901.
33. Roessler, MS, Schmid, DS, Michels, P, Schmid, O, Jung, K, Stöber, J, et al. Early out-of-hospital non-invasive ventilation is superior to standard medical treatment in patients with acute respiratory failure: A pilot study. Emer Med J. (2012) 29:409–14.
34. Seethala, RR, Frakes, MA, Cocchi, MN, Cohen, JE, Dargin, J, Friedman, F, et al. Feasibility and Safety of Prone Position Transport for Severe Hypoxemic Respiratory Failure Due to Coronavirus Disease 2019. Crit Care Explor. (2020) 2:e0293.
35. Kallio, T, Kuisma, M, Alaspää, A, and Rosenberg, PH. The use of prehospital continuous positive airway pressure treatment in presumed acute severe pulmonary edema. Prehosp Emerg Care. (2003) 7:209–13.
36. Cheskes, S, Turner, L, Thomson, S, and Aljerian, N. The impact of prehospital continuous positive airway pressure on the rate of intubation and mortality from acute out-of-hospital respiratory emergencies. Prehosp Emerg Care. (2013) 17:435–41.
37. Thompson, J, Petrie, DA, Ackroyd-Stolarz, S, and Bardua, DJ. Out-of-hospital continuous positive airway pressure ventilation versus usual care in acute respiratory failure: a randomized controlled trial. Ann Emerg Med. (2008) 52:241.e1.
38. Girotti, MJ, Pagliarello, G, Todd, TR, Demajo, W, Cain, J, Walker, P, et al. Physician- accompanied transport of surgical intensive care patients. Can J Anaesth. (1988) 35:303–8. doi: 10.1007/BF03010636
39. Taylor, CB, Stevenson, M, Jan, S, Middleton, PM, Fitzharris, M, and Myburgh, JA. A systematic review of the costs and benefits of helicopter emergency medical services. Injury. (2010) 41:10–20. doi: 10.1016/j.injury.2009.09.030
40. Simpson, PM, and Bendall, JC. Prehospital non-invasive ventilation for acute cardiogenic pulmonary oedema: an evidence-based review. Emerg Med J. (2011) 28:609–12. doi: 10.1136/emj.2010.092296
41. Masip, J. Noninvasive ventilation in acute heart failure. Curr Heart Fail Rep. (2019) 16:89–97. doi: 10.1007/s11897-019-00429-y
42. Williams, B, Boyle, M, Robertson, N, and Giddings, C. When pressure is positive: a literature review of the prehospital use of continuous positive airway pressure. Prehosp Disaster Med. (2013) 28:52–60. doi: 10.1017/S1049023X12001562
43. Nawrocki, PS, Poremba, M, and Lawner, BJ. Push dose epinephrine use in the management of hypotension during critical care transport. Prehospital Emerg Care. (2020) 24:188–95. doi: 10.1080/10903127.2019.1588443
44. L’Her, E, Duquesne, F, Paris, A, Mouline, J, Renault, A, Garo, B, et al. Spontaneous positive end-expiratory pressure ventilation in elderly patients with cardiogenic pulmonary edema. Assessment in an emergency admissions unit. Presse Med. (1998) 27:1089–94.
45. Britos, M, Smoot, E, Liu, KD, Thompson, BT, Checkley, W, and Brower, RG. The value of positive end-expiratory pressure and Fio2 criteria in the definition of the acute respiratory distress syndrome. Crit Care Med. (2011) 39:2025–30. doi: 10.1097/CCM.0b013e31821cb774
46. Roessler, M. Non-invasive ventilation in prehospital emergency medicine. Anasthesiol Intensivmed Notfallmed Schmerzther. (2008) 43:264–6. doi: 10.1055/s-2008-1076608
47. Cumpstey, AF, Oldman, AH, Martin, DS, Smith, A, and Grocott, MPW. Oxygen targets during mechanical ventilation in the ICU: a systematic review and meta-analysis. Crit Care Explor. (2022) 4:e0652. doi: 10.1097/CCE.0000000000000652
48. Alstrup, K, Petersen, JAK, Sollid, S, Johnsen, SP, and Rognås, L. Mortality and hospitalisation in the Danish helicopter emergency medical service (HEMS) population from 2014 to 2018: a national population-based study of HEMS triage. BMJ Open. 1228 (2020) 10:e038718. doi: 10.1136/bmjopen-2020-038718
Keywords: mechanical ventilation, EMS, critical care transport, complications, adverse event
Citation: Pinto-Villalba RS and Leon-Rojas JE (2023) Reported adverse events during out-of-hospital mechanical ventilation and ventilatory support in emergency medical services and critical care transport crews: a systematic review. Front. Med. 10:1229053. doi: 10.3389/fmed.2023.1229053
Edited by:
Jun Duan, First Affiliated Hospital of Chongqing Medical University, ChinaReviewed by:
Neeraj Srivastava, University of California, United StatesMeghan Bernier, Johns Hopkins Medicine, United States
Copyright © 2023 Pinto-Villalba and Leon-Rojas. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jose E. Leon-Rojas, am9zZS5sZW9uLnJvamFzQHVkbGEuZWR1LmVj
†ORCID: Ricardo Sabastian Pinto-Villalba, https://orcid.org/0000-0002-7745-6204
Jose E. Leon-Rojas, https://orcid.org/0000-0002-8130-6460
 Ricardo Sabastian Pinto-Villalba
Ricardo Sabastian Pinto-Villalba Jose E. Leon-Rojas
Jose E. Leon-Rojas