- 1School of Health Sciences, Polytechnic of Leiria, Morro do Lena, Alto do Vieiro, Leiria, Portugal
- 2Palliative Care Unit, Portuguese Institute of Oncology of Coimbra, Coimbra, Portugal
- 3Centre for Innovative Care and Health Technology (ciTechCare), Polytechnic of Leiria, Leiria, Portugal
- 4Comprehensive Health Research Centre (CHRC), University of Évora, Évora, Portugal
Introduction
Palliative Care (PC) can begin when a serious illness is diagnosed and continue during the entire continuum of care (1). According to the World Health Organization, PC “is a crucial part of integrated, people-centered health services. Relieving serious health-related suffering, be it physical, psychological, social, or spiritual, is a global ethical responsibility. Thus, whether the cause of suffering is cardiovascular disease, cancer, major organ failure, drug-resistant tuberculosis, severe burns, end-stage chronic illness, acute trauma, extreme birth prematurity, or extreme frailty of old age, palliative care may be needed and has to be available at all levels of care” [(2); p. 1].
Of the 234 nations in the globe, roughly 136 offer PC services and resources. While Europe, Australia, Canada, and the United States have the highest levels of PC integration, many regions of Africa and several regions of Asia and South America lack basic amenities (3). There are several aspects that contribute to the development of PC integration in health care systems: economic resources, cultural and religious aspects, education and training of health care teams (3–5).
The available evidence indicates an increasing need for PC (6–8). This represents a challenge in the definition of health policies (9–11), in the organization of health services and responses (12, 13), but also for health professionals (11, 14).
Recently, the COVID-19 pandemic resulted in many critically ill and dying patients requiring expert management of symptoms “such as dyspnea, pain, and delirium, as well as serious illness communication, including conversations about care goals and end-of-life issues” [(15); p. e22]. Given the increasing uncertainty of the disease's trajectory, high-quality PC must be offered and affordable for all people. However, COVID-19 did complicate matters. When patients deteriorated rapidly, time was of the essence, health workers were overburdened, seclusion was mandatory, and relatives were instructed not to touch or even be in the same room as loved ones (16). The pandemic is therefore considered to have significantly increased emerging PC needs. Likewise, the pandemic slowed and, in some instances, reversed advancements made in PC development (17, 18).
The literature has supported the idea that early referral to PC translates into increased quality of life (19, 20). Therefore, identifying the appropriate time to initiate the palliative approach to the patient is a challenge for formal as well as informal caregivers.
We aim to identify areas of assessment, auxiliary tools, as well as possible paradigm shifts toward a socio-ecological approach to the person with palliative needs, in order to provide differentiated PC adjusted to the person's condition as early as possible.
Benefits and implications of early palliative care
Several studies report that few people receive PC in their last year of life (21–23). However, earlier PC has been shown to improve quality of life and survival (20, 22, 24, 25). PC has several benefits, including improved quality of life and mood (25), decreased need for therapy at the end of life, and decreased healthcare costs (26). According to Mittmann et al. (22), early identification leads to an increase in access to PC services.
Timely PC is a systematic approach that identifies patients with high supportive care requirements and refers them to specialized PC as soon as possible based on defined referral criteria. According to Hui et al. (27), it needs four elements: routine assessment of patients' needs for supportive care; institution-specific consensual referral criteria; a system to initiate referrals when patients meet requirements; and availability of outpatient PC resources to provide individualized and timely patient-centered care, with the goal of improving patient and caregiver outcomes. That at least some aspects of PC begin earlier, while the patient is still able to communicate effectively and participate as fully as possible in their medical treatment, is crucial to patient-centered care (28). This may also minimize the burden of replacing decision-making by the patient's family or caregiver, thereby decreasing recurrent distress emotions and avoiding more complicated grieving in the future (28).
To provide effective and efficient patient-centered care at the palliative stage, we must attend to the complexity of care and the areas of specialized interventions (29), by clearly defining the core competencies of the multidisciplinary health team members, and prioritizing a holistic and interactive approach (30). Involvement of care teams reduces hospitalization rates for PC patients and enables them to spend more time at home (30), honoring patients' wish to be cared for at home (31).
When contemplating the start of PC, it is crucial to differentiate between the use of a palliative strategy to treatment (primary PC) and referral to specialist PC consulting services. Primary PC is appropriate at all stages of illness and can be delivered by any healthcare provider (21, 28). This palliative approach to care may be included in the care of every patient following diagnosis, as part of a personalized treatment plan. It provides patients, their relatives, and carers greater control, while also improving quality of life and wellbeing. It may include emotional, social, and spiritual components of care, in addition to physical components of care. Healthcare providers may collaborate with patients and their families to respect them as persons and honor their healthcare treatment choices by aligning care with the patient's goals and principles of PC (1, 28). In contrast, specialized consultation by a PC professional where the major focus of the consultation is comprehensive therapy, including advanced symptom management, psychological, social, and spiritual support, and dignity-preserving care. Specialist PC services are often required when symptoms—whether physical, psychological, or multifactorial—are refractory or difficult, and frequently include interdisciplinary therapy with the goal of fostering quality of life and preserving meaning in existence (28).
There is an urgent need to ensure quality and equality of treatment for all PC patients, from those who require a PC approach to those who require expert intense PC (29). Attention need be given to the areas of care requiring evaluation, the strategies to be implemented, the evaluation instruments that can be used, and the consequences resulting from this approach.
Current health-care models frequently rely on referral-based PC, which can lead to uneven access to treatments or patients receiving PC near the end of their illness progression (32). Early PC has been identified as one option for extending access to PC services for patients suffering from illnesses with an unpredictable course, such as organ failure (33). Early PC is a proactive technique for developing treatment goals, controlling symptoms, and improving quality of life in patients with any life-limiting chronic condition, thereby expanding the scope of traditional PC services (34). Clearly defining the early PC approach so that health professionals and patients understand what early PC is and what role it can play, as well as its potential benefits, could assist in overcoming patient- and family-related barriers rooted in the traditional portrayal of PC. Barriers include misinformation, reluctance to accept referral, or the belief that PC is synonymous with terminal care. Similarly, physicians are concerned that referring patients to PC may cause patients and their families to lose hope and experience suffering (35). Teaching physicians how to deliver “bad news” may aid in their ability to deal with the emotional concerns associated with sending patients to specialist PC (35).
Tuca et al. (36) propose an early PC model that includes a multidimensional assessment, allowing clinicians to classify patients as having low, medium, or high palliative complexity, based on the requirement for basic or specialist PC: “(a) Low complexity—capacity and training of a non-specialized PC team is sufficient; referral to a specialized team is not indicated; (b) Medium complexity—care requires more than capacity and training of a non-specialized PC team; a shared care with a specialized PC team is indicated; (c) High complexity—care entails far more than capacity and training of a non-specialized PC team; intensive shared care with specialized PC is required” (p. 242).
PC complexity is defined “as a clinical condition based on the interaction of emerging clinical characteristics according to a multidimensional evaluation, which confers a special tendency to clinical instability, uncertainty in the outcome of health care intervention, and the subsequent need to intensify specialized palliative support measures” [(36); p. 242].
The measurement of days for referral to specialist PC does not always imply that the team is not providing enough care based on the patient's needs (37). The number of persistent symptoms noted in each patient is a significant signal that specialized treatment may be required, since PC professionals may have better expertise treating refractory and chronic symptoms (37).
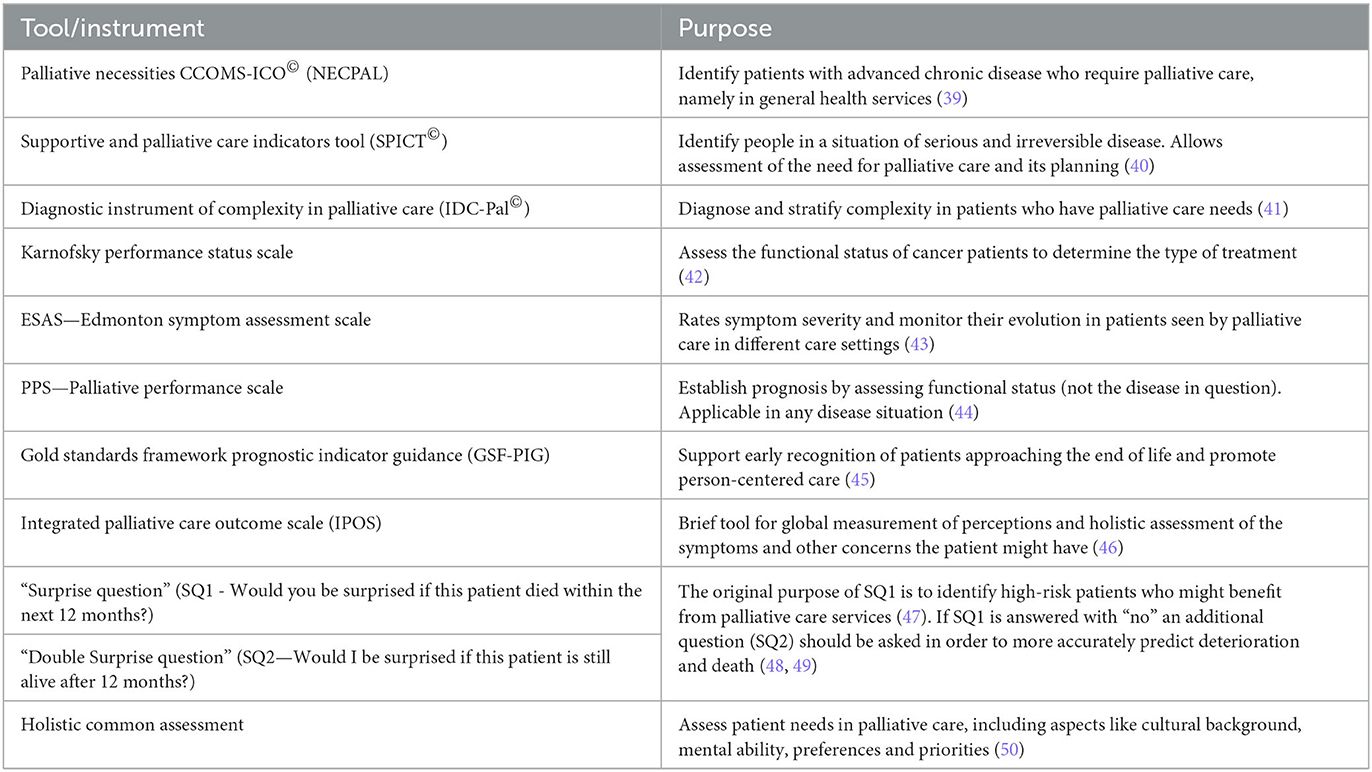
Support for a PC team, on the other hand, is often delayed or occurs when there is an excess of symptoms and functional dependency. The use of tools can be critical in the early identification of patients with palliative requirements, and they should ideally be accurate, dependable, low-cost, and smoothly integrated into the current workflow (38). Their usage may assist in indicating the appropriate palliative strategy and understanding the demands of the patient with advanced chronic illness. As demonstrated in Table 1, there is a series of instruments that guide the palliative approach via the assessment of prognosis and/or palliative requirements.
Despite efforts, there is still no consensus on when the palliative trajectory begins, and early integration of PC in clinical practice is still dependent on overcoming the numerous barriers associated with the disease, health professionals, and service organization (37).
Integrative approach: final remarks
Referral to PC tends to consider clinical aspects, such as the benefit of therapeutic intervention, as a dichotomous alternative to palliative intervention, considering them differentiated, separate approaches rather than attempting their integration in a holistic and complementary way.
Scientific knowledge suggests one should consider the palliative approach in an integrated manner, as a multidimensional and interdisciplinary intervention that views the person holistically. The fragmentation of health by professional area or by isolated clinical gain limits the potential for interventions addressing ecological and social aspects of health. Socio-ecological models have been used to contextualize the effect of many environmental variables on vulnerable people's lives. The person is at the heart of and immersed in a variety of environmental systems, ranging from proximate settings like the family to bigger contexts like culture (51). While PC has long acknowledged physical, psychological, social, and spiritual comprehensive worlds, we must go further. To comprehensively and effectively investigate and answer patients' requests, we must consider “pre-existing and cumulative complexity, the dynamic aspects of complexity, invisible complexity, service/system-level difficulties, and societal repercussions” [(52); p. 1078].
Illness as a condition of vulnerability, and therefore attending to a patient's specific needs, based on a client-centered care perspective, including all their dimensions (physical, psychosocial, and spiritual) is an ethical and moral imperative of health professionals. Thus, more than defining a chronological time to begin the palliative approach, it is important to consider the individual's time in meeting their real needs, incorporating PC in the practice of professionals, resorting to the expertise of differentiated professionals whenever they can contribute to the person's fulfillment in each moment of their experience of the processes of illness.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
This work was funded by national funds through FCT—Fundação para a Ciência e a Tecnologia, I.P. (UIDB/05704/2020 and UIDP/05704/2020) and under the Scientific Employment Stimulus—Institutional Call—[CEECINST/00051/2018].
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Cain CL, Surbone A, Elk R, Kagawa-Singer M. Culture and palliative care: preferences, communication, meaning, and mutual decision making. J Pain Symptom Manage. (2018) 55:1408–19. doi: 10.1016/j.jpainsymman.01007
2. World Health Organization (WHO). Palliative Care. Geneve: WHO. (2022). Available from: https://www.who.int/health-topics/palliative-care (accessed May 1, 2023).
3. Brant JM, Silbermann M. Global perspectives on palliative care for cancer patients: not all countries are the same. Curr Oncol Rep. (2021) 23:60. doi: 10.1007/s11912-021-01044-8
4. Migala S, Flick U. Cultural and individual barriers to palliative care from different angles: Data triangulation in practice. Qualit Inquiry. (2019) 25:786–98. doi: 10.1177/1077800418809475
5. Six S, Bilsen J, Deschepper R. Dealing with cultural diversity in palliative care. BMJ Support Palliat Care. (2023) 13:65–9. doi: 10.1136/bmjspcare-2020-002511
6. Dumanovsky T, Augustin R, Rogers M, Lettang K, Meier DE, Morrison RS, et al. The growth of palliative care in U.S. hospitals: a status report. J Palliat Med. (2015) 19:8–15. doi: 10.1089/jpm.2015.0351
7. Kamal AH, Wolf SP, Troy J, Leff V, Dahlin C, Rotella JD, et al. Policy changes key to promoting sustainability and growth of the specialty palliative care workforce. Health Aff. (2019) 38:910–8. doi: 10.1377/hlthaff.2019.00018
8. Kelley AS, Bollens-Lund E. Identifying the population with serious illness: the “denominator” challenge. J Palliat Med. (2017) 21(S2):S-7–16. doi: 10.1089./jpm.2017.0548
9. Chan HYL, Lee DTF, Woo J. Diagnosing gaps in the development of palliative and end-of-life care: a qualitative exploratory study. Int J Environ Res Public Health. (2019) 17:151. doi: 10.3390/ijerph17010151
10. Sleeman KE, Timms A, Gillam J, Anderson JE, Harding R, Sampson EL, et al. Priorities and opportunities for palliative and end of life care in United Kingdom health policies: a national documentary analysis. BMC Palliat Care. (2021) 20:108. doi: 10.1186/s12904-021-00802-6
11. Wong EL, Kiang N, Chung RY, Lau J, Chau PY, Wong SY, et al. Quality of palliative and end-of-life care in Hong Kong: perspectives of healthcare providers. Int J Environ Res Public Health. (2020) 17:5130. doi: 10.3390/ijerph17145130
12. Barasteh S, Rassouli M, Parandeh A, Vahedian-Azimi A, Zaboli R, Khaghanizadeh M. Palliative care in the health system of Iran: a review of the present status and the future challenges. Asian Pacific J Cancer Prevent APJCP. (2020) 21:845–51. doi: 10.31557/APJCP.213.845
13. Brock KE, Snaman JM, Kaye EC, Bower KA, Weaver MS, Baker JN, et al. Models of pediatric palliative oncology outpatient care—Benefits, challenges, and opportunities. J Oncol Pract. (2019) 15:476–87. doi: 10.1200/JOP.19.00100
14. Price DM, Strodtman LK, Montagnini M, Smith HM, Ghosh B. Health professionals perceived concerns and challenges in providing palliative and end-of-life care: a qualitative analysis. Am J Hosp Palliat Care. (2018) 36:308–15. doi: 10.1177/1049909118812193
15. Thomas JD, Leiter RE, Abrahm JL, Shameklis JC, Kiser SB, Gelfand SL, et al. Development of a palliative care toolkit for the cOVID-19 pandemic. J Pain Symptom Manage. (2020) 60:e22–5. doi: 10.1016/j.jpainsymman.05021
16. Lancet T. Palliative care and the COVID-19 pandemic. Lancet. (2020) 395:1168. doi: 10.1016/S0140-6736(20)30822-9
17. Tavares P, Rodrigues C, Neto IG. The impact of COVID-19 on palliative care: perspective of healthcare professionals. Cureus. (2021) 13:e19522. doi: 10.7759/cureus.19522
18. Fadul N, Elsayem AF, Bruera E. Integration of palliative care into COVID-19 pandemic planning. BMJ Support Palliat Care. (2021) 11:40. doi: 10.1136/bmjspcare-2020-002364
19. Cuviello A, Raisanen JC, Donohue PK, Wiener L, Boss RD. Initiating palliative care referrals in pediatric oncology. J Pain Symptom Manage. (2021) 61:81–9. doi: 10.1016/j.jpainsymman.07008
20. Hausner D, Tricou C, Mathews J, Wadhwa D, Pope A, Swami N, et al. Timing of palliative care referral before and after evidence from trials supporting early palliative care. Oncologist. (2021) 26:332–40. doi: 10.1002/onco.13625
21. Canadian Institute for Health Information. Access to Palliative Care in Canada. Ottawa, ON: CIHI (2018).
22. Mittmann N, Liu N, MacKinnon M, Seung SJ, Look Hong NJ, Earle CC, et al. Does early palliative identification improve the use of palliative care services? PLoS ONE. (2020) 15:e0226597. doi: 10.1371/journal.pone.0226597
23. Tanuseputro P, Budhwani S, Bai YQ, Wodchis WP. Palliative care delivery across health sectors: a population-level observational study. Palliat Med. (2016) 31:247–57. doi: 10.1177/0269216316653524
24. Shinall MC Jr, Karlekar M, Martin S, Gatto CL, Misra S, Chung CY, et al. COMPASS: a pilot trial of an early palliative care intervention for patients with end-stage liver disease. J. Pain Symptom Manag. (2019) 58:614–22. doi: 10.1016/j.jpainsymman.06023
25. Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. (2010) 363:733–42. doi: 10.1056/NEJMoa1000678
26. Schlick CJR, Bentrem DJ. Timing of palliative care: when to call for a palliative care consult. J Surg Oncol. (2019) 120:30–4. doi: 10.1002/jso.25499
27. Hui D, Heung Y, Bruera E. Timely palliative care: personalizing the process of referral. Cancers. (2022) 14:47. doi: 10.3390./cancers14041047
28. Dawson B, McConvey K, Gofton TE. When to initiate palliative care in neurology. Handb Clin Neurol. (2022) 190:105–25. doi: 10.1016/B978-0-323-85029-2.00011-7
29. Martin-Rosello ML, Sanz-Amores MR, Salvador-Comino MR. Instruments to evaluate complexity in end-of-life care. Curr Opin Support Palliat Care. (2018) 12:480–8. doi: 10.1097/SPC.0000000000000403
30. Fernando G, Hughes S. Team approaches in palliative care: a review of the literature. Int J Palliat Nurs 25(9). (2019) 444–51. doi: 10.12968/ijpn.259.444
31. Prado E, Marcon S, Kalinke L, da Silva M, Barreto M, Takemoto A, et al. Meanings and experiences of end-of-life patients and their family caregivers in hospital-to-home transitions: a constructivist grounded theory study. Int J Environ Res Public Health. (2022) 19:12987. doi: 10.3390/ijerph192012987
32. Szekendi MK, Vaughn J, Lal A, Ouchi K, Williams MV. The prevalence of inpatients at 33 U.S. hospitals appropriate for and receiving referral to palliative care. J Palliat Med. (2016) 19:360–72. doi: 10.1089/jpm.2015.0236
33. Watt CL, Downar J. Whither palliative care? Curr Oncol. (2019) 26:164–5. doi: 10.3747/co.26.4803
34. Kircher C, Hanna T, Tranmer J, Goldie C, Ross-White A, Goldie C, et al. Defining and implementing early palliative care for persons diagnosed with a life-limiting chronic illness: a scoping review protocol. JBI evidence synthesis. (2020) 18:2335–41. doi: 10.11124/JBISRIR-D-19-00377
35. Sarradon-Eck A, Besle S, Troian J, Capodano G, Mancini J. Understanding the barriers to introducing early palliative care for patients with advanced cancer: a qualitative study. J Palliat Med. (2019) 22:508–16. doi: 10.1089/jpm.2018.0338
36. Tuca A, Gómez-Martínez M, Prat A. Predictive model of complexity in early palliative care: a cohort of advanced cancer patients (PALCOM study). Supporte Care Cancer. (2018) 26:241–9. doi: 10.1007/s00520-017-3840-3
37. Santos EA, da Costa Lima NK, Freire ER. Palliative care for elderly non-oncology patients in an internal medicine service. OAJ Gerontol and Geriatric Med. (2020) 6:5676. doi: 10.19080/OAJGGM.05555676
38. Downar J, Wegier P, Tanuseputro P. Early identification of people who would benefit from a palliative approach—Moving from surprise to routine. JAMA Network Open. (2019) 2:e1911146. doi: 10.1001/jamanetworkopen.2019.11146
39. Gómez-Batiste X, Martínez-Muñoz M, Blay C, et al. Utility of the NECPAL CCOMS-ICO© tool and the surprise question as screening tools for early palliative care and to predict mortality in patients with advanced chronic conditions: a cohort study. Palliat Med. (2017) 31:754–63. doi: 10.1177/0269216316676647
40. Highet G, Crawford D, Murray SA. Development and evaluation of the supportive and palliative care indicators tool (SPICT): a mixed-methods study. BMJ Support Palliat Care. (2014) 4:285–90. doi: 10.1136/bmjspcare-2013-000488
41. Grant M, de Graaf E, Teunissen S. A systematic review of classifications systems to determine complexity of patient care needs in palliative care. Palliat Med. (2021) 35:636–50. doi: 10.1177/0269216321996983
42. Timmermann C. 'Just give me the best quality of life questionnaire': the Karnofsky scale and the history of quality of life measurements in cancer trials. Chronic Illn. (2013) 9:179–90. doi: 10.1177/1742395312466903
43. Hui D, Bruera E. The edmonton symptom assessment system 25 years later: past, present, and future developments. J Pain Symp Manag. (2017) 53:630–43. doi: 10.1016/j.jpainsymman.10370
44. Lee GJ, Gwak JH, Kim MS, Lee MY, Kim SR, Chun SH, et al. Changes in the palliative performance scale may be as important as the initial palliative performance scale for predicting survival in terminal cancer patients. Palliat Support Care. (2021) 19:547–51. doi: 10.1017/S1478951520001248
45. Gold Standard Framework. Proactive Identification Guidance (PIG), 7th ed. Shrewsbury: GSF (2022). Available online at: https://goldstandardsframework.org.uk/cd-content/uploads/files/PIG/Proactive%20Identification%20Guidance%20v7%20(2022).pdf (accessed July 20, 2023).
46. Murtagh FE, Ramsenthaler C, Firth A, Groeneveld EI, Lovell N, Simon ST, et al. A brief, patient- and proxy-reported outcome measure in advanced illness: validity, reliability and responsiveness of the integrated palliative care outcome scale (IPOS). Palliat Med. (2019) 33:1045–57. doi: 10.1177/0269216319854264
47. van Lummel EV, Ietswaard L, Zuithoff NP, Tjan DH, van Delden JJ. The utility of the surprise question: a useful tool for identifying patients nearing the last phase of life? A systematic review and meta-analysis. Palliat Med. (2022) 36:1023–46. doi: 10.1177/02692163221099116
48. Ermers DJ, Kuip EJ, Veldhoven C, Schers HJ, Perry M, Bronkhorst EM, et al. Timely identification of patients in need of palliative care using the double surprise question: a prospective study on outpatients with cancer. Palliat Med. (2021) 35:592–602. doi: 10.1177/0269216320986720
49. Veldhoven CM, Nutma N, De Graaf W, Schers H, Verhagen CA, Vissers KC, et al. Screening with the double surprise question to predict deterioration and death: an explorative study. BMC Palliat Care. (2019) 18:118. doi: 10.1186/s12904-019-0503-9
50. National Cancer Action Team NHS Improving Quality. (2010). Holistic Common Assessment of Supportive and Palliative Care Needs for Adults Requiring End of Life Care. (2010). Available online at: https://www.bl.uk/collection-items/holistic-common-assessment-of-the-supportive-and-palliative-care-needs-of-adults-requiring-end-of-life-care (accessed May 1, 2023).
51. Chandran D, Corbin JH, Shillam C. An ecological understanding of caregiver experiences in palliative care. J. Soc. Work End-of-Life Palliat. (2016) 12:162–82. doi: 10.1080/15520161156602
Keywords: palliative care, healthcare providers, assessment, patient-centered care, referral, resources, education, communication
Citation: Vitorino JV, Duarte BV and Laranjeira C (2023) When to initiate early palliative care? Challenges faced by healthcare providers. Front. Med. 10:1220370. doi: 10.3389/fmed.2023.1220370
Received: 10 May 2023; Accepted: 13 September 2023;
Published: 02 October 2023.
Edited by:
Jeremy M. Jacobs, Hadassah Medical Center, IsraelReviewed by:
Wojciech Leppert, Poznan University of Medical Sciences, PolandCopyright © 2023 Vitorino, Duarte and Laranjeira. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joel Vieira Vitorino, joelvieiravitorino@gmail.com; Carlos Laranjeira, carlos.laranjeira@ipleiria.pt
 Joel Vieira Vitorino
Joel Vieira Vitorino Beatriz Veiga Duarte
Beatriz Veiga Duarte Carlos Laranjeira
Carlos Laranjeira