- 1Institute of Medical Education, LMU University Hospital, LMU Munich, Munich, Germany
- 2Faculty of Health, University of Technology Sydney, Ultimo, NSW, Australia
- 3Chair of Education and Educational Psychology, Department of Psychology, LMU Munich, Munich, Germany
The health care system in Germany and in many other countries is facing fundamental challenges due to demographic change, which require new integrated care concepts and a revision of the collaboration between health care professions in everyday clinical practice. Internationally, several competency framework models have been proposed, but a framework that explicitly conceptualizes collaborative activities to improve interprofessional problem-solving competency in health care is still missing. Such a framework should define contextual, person-related, process-related, and outcome-related variables relevant to interprofessional problem solving in health care. Against this background, we present a conceptual framework to improve interprofessional collaboration in health education and care (FINCA) developed with scientific consideration of empirical data and various theoretical references. FINCA reflects an interprofessional learning and interaction process involving two persons from different health care professions and with different individual learning prerequisites. These two initially identify a problem that is likely to require interprofessional collaboration at some point. FINCA acknowledges the context of interprofessional learning, teaching, and working as well as its action-modifying context factors. We follow the reasoning that individual learning prerequisites interact with the teaching context during learning activities. At the heart of FINCA are observable collaborative activities (information sharing and grounding; negotiating; regulating; executing interprofessional activities; maintaining communication) that can be used to assess individuals’ cognitive and social skills. Eventually, the framework envisages an assessment of the outcomes of interprofessional education and collaboration. The proposed conceptual framework provides the basis for analysis and empirical testing of the components and variables it describes and their interactions across studies, educational interventions, and action-modifying contexts. FINCA further provides the basis for fostering the teaching and learning of interprofessional problem-solving skills in various health care settings. It can support faculty and curriculum developers to systematize the implementation and improvement of interprofessional teaching and learning opportunities. From a practical perspective, FINCA can help to better align curricula for different health professions in the future. In principle, we also see potential for transferability of the framework to other areas where different professions collaborate.
1. Introduction
The health care system in Germany, as well as in many other countries, is facing fundamental challenges due to demographic change. With the aging of the world’s population, on the one hand, the care of the elderly is gaining in importance – on the other hand, the associated need for treatment and management of complex chronic long-term conditions is becoming increasingly important (1, 2). These changes require new integrated care concepts and a revision of the cooperation between health care professions in everyday clinical practice. Numerous position papers and strategic plans have therefore been calling for an increased integration of interprofessional education in under-and postgraduate training in medicine as well as other health care professions (3–7).
Interprofessional collaboration (IPC) involves different health and social care professions meeting regularly to negotiate and agree on how to solve complex care problems or deliver services. Interprofessional teamwork is characterized by a high level of team identification and close networking and interdependence. The dimensions of IPC also include clear team goals, a shared team identity, shared team commitment, and clear role allocation (8). Interprofessional education (IPE), which is necessary to prepare for IPC, takes place whenever trainees, students, or professionals from two or more professions come together to learn with, from, and about each other in order to optimize collaboration in patient care (9). Both definitions reflect the need for IPE and IPC to include interactive problem-solving processes and related activities.
Similarily to other educational interventions, it remains challenging to demonstrate a causal relationship between IPE and general care system outcomes (such as improved clinical experience or improved patient experience). Multiple studies have demonstrated that IPE interventions can lead to improved patient care in specific contexts [(e.g., 10, 11)]. It must be noted, however, that due to the heterogeneous nature of these studies and the variety of IPE interventions, it is rather difficult to integrate and generalize results of these interventions to inform general theory-building (12).
Several competency framework models in IPE have been proposed internationally, primarily motivated by health policy makers [(e.g., 13–16)]. These framework models address both IPE and IPC and formulate overarching competency goals for successful interprofessional work. The frameworks include ethics and values, teamwork, leadership, conflict resolution, communication, mutual respect, role clarity and patient-centredness as important areas (17).
As the need for IPE and IPC increases due to the demands brought about by demographic change, we believe there is also a growing need for a framework that explicitly conceptualizes collaborative activities to improve interprofessional problem-solving skills in health care. Such a framework should define contextual, person-related, process-related, and outcome-related variables relevant for interprofessional problem-solving in health care. At the same time, it should be based on observable activities that allow for an operationalization of interprofessional problem-solving skills.
In this paper, we propose a framework based on a combination of three theoretical strands from educational psychology research on collaborative learning: (1) fostering of diagnostic competencies (18), (2) collaboration scripts (19), and (3) collaborative problem-solving skills (20). These theoretical strands have proven useful in different contexts and domains such as teacher and medical education (see Section 2.2). To our knowledge, these generalizable educational frameworks and theories have not yet been utilized to inform and enrich the development and design of competency framework models for improved IPE and IPC.
On this basis, we offer definitions and operationalizations that will enable empirical research studies to assess and subsequently foster collaborative problem-solving skills, as well as the integration of results across diverse IPE and IPC contexts. Quantitative methods could thus be increasingly employed in the study of IPC, which to date has been primarily of a qualitative nature (21). Moreover, such a framework could serve as an educational tool by providing the foundation for fostering the teaching and learning of interprofessional problem-solving skills in various health care settings.
2. Developing a conceptual framework for analyzing and fostering interprofessional problem-solving skills
2.1. Development context
The conceptual Framework to Improve iNterprofessional Collaboration in health education and cAre (FINCA) presented in this article was developed by the authors in the context of the Graduate School “Interprofessional Teaching in the Health Professions” (ILEGRA) which was funded by the Robert Bosch Stiftung from 2018 until 2022. ILEGRA served to promote young scientists and was conducted in cooperation between the University of Osnabrück and LMU Munich. ILEGRA research fellows came from a variety of health care professions and worked on dissertation topics related to teaching, assessing and evaluating in the context of IPE or health care practice. ILEGRA brought together researchers from different disciplines to serve as scientific supervisors or advisory board members, some of whom work outside the health professions. This allowed for a broad exchange of experts from the health professions with experts from educational psychology, adult education, work and organizational psychology, and sociology. The approach resembled focus group discussions (22) and took into account existing framework concepts and the variables they contain. The iterative discussion rounds with all experts and with the ILEGRA fellows informed the development and conceptual design of the present framework, offering new perspectives beyond the health professions.
2.2. Theoretical sources beyond IPE and IPC to inform the development process
The proposed framework addresses all educational scientists and curriculum developers in the field of IPE to contribute to better IPC processes and outcomes. The development of FINCA was guided by three theoretical strands beyond the aforeementioned competency framework models for IPE and IPC:
(1) The first strand is an interdisciplinary framework on the acquisition and fostering of diagnostic competencies by Heitzmann et al. (18) with its basic assumption that one’s own cognitive activities are an important prerequisite for the acquisition of competencies. Disciplines are defined as broad academic fields, such as anthropology, economics and geography (8). We propose to conceptualize collaborative activities for interprofessional problem-solving on the basis of this framework which also considers a wide range of individual prerequisites (cognitive professional abilities as well as motivational and affective factors) and also context factors that could potentially moderate collaborative activities. FINCA was further inspired by Biggs’ 3P model (Presage, Process, and Product) of teaching that shows how learner prerequisites interact with the teaching context during learning activities and relates them with learning outcomes (23).
(2) The second strand assumes that the extent to which IPC takes place in specific situations depends on the thought processes and activities of the individuals involved, drawing on cognitive structures like illness scripts and collaboration scripts. Illness scripts were first used to explain the diagnostic behavior of physicians. However, their usefulness is also being advocated in the nursing context [(e.g., 24)]. In short, medical or nursing knowledge is organized into illness scripts which consist of patterns for diseases or clinical dysfunctions, their underlying pathophysiological processes and symptoms, as well as their care courses including therapeutic interventions (25). With clinical experience, these illness scripts develop further as increasingly efficient ways of thinking and work organization of physicians, nurses, and allied health professionals to solve and manage clinical problems. Thus, the continuous development of illness scripts enable health professionals to speed up and improve the quality of their decisions based on recurrent patterns.
Particularly in the educational context, collaboration scripts are also described in the literature (19). Internal collaboration scripts can be understood as a person’s current knowledge of implicit and explicit rules for effective and efficient collaboration. External collaboration scripts can, in turn, be understood as sets of scaffolds that help to structure collaborative learning processes. They may gradually become internalized as learners act in accordance with the script content (26). While only few empirical studies are available to date regarding the use of collaboration scripts in a medical context [(e.g., 27, 28)], the consideration of internal collaboration scripts of health professionals in the context of IPE and IPC is promising to support the development and application of collaboration knowledge.
(3) The third strand encompasses collaborative problem-solving skills that are crucial when two or more health professionals interact and orchestrate knowledge and skills to solve a shared problem. Interprofessional interactions are characterized by a diversity of professional backgrounds, distribution of responsibilities, and different approaches and values with regard to the provision of care. Interprofessional collaborative practice is dependent on the competencies of each professional group to ensure optimal care for patients, families and communities. In such situations, competencies must be integrated and a common level of information must be established, which requires a high degree of collaborative problem-solving competence from all professionals involved. Liu et al. (20) studied collaborative problem-solving in groups, describing social skills such as sharing ideas, negotiating ideas, regulating problem-solving activities, and maintaining communication. Following these considerations, we consider collaborative problem-solving skills as indispensable prerequisites for a person to participate effectively in a process in which two or more participants attempt to solve a problem together.
3. Structural components of FINCA
FINCA (see Figure 1) reflects an interprofessional learning and interaction process that involves two different health care professionals (i.e., person in profession A and person in profession B) with different individual learning prerequisites (18). These two persons recognize a problem that presumably requires interprofessional collaboration at one point – we term this noticing, which involves recognition and identification, but can be explicit or implicit/tacit (29, 30). FINCA further acknowledges the context of interprofessional learning, teaching, and working and its action-modifying context factors. We follow the reasoning that individual learning prerequisites interact with the teaching context during learning activities (18, 23). At the core of FINCA are observable collaborative activities [cf. (20)]. At the same time, the framework envisages an assessment of the outcomes of IPE and IPC. In the following sections, the core content aspects of the framework are explained and pragmatic research approaches will be outlined.
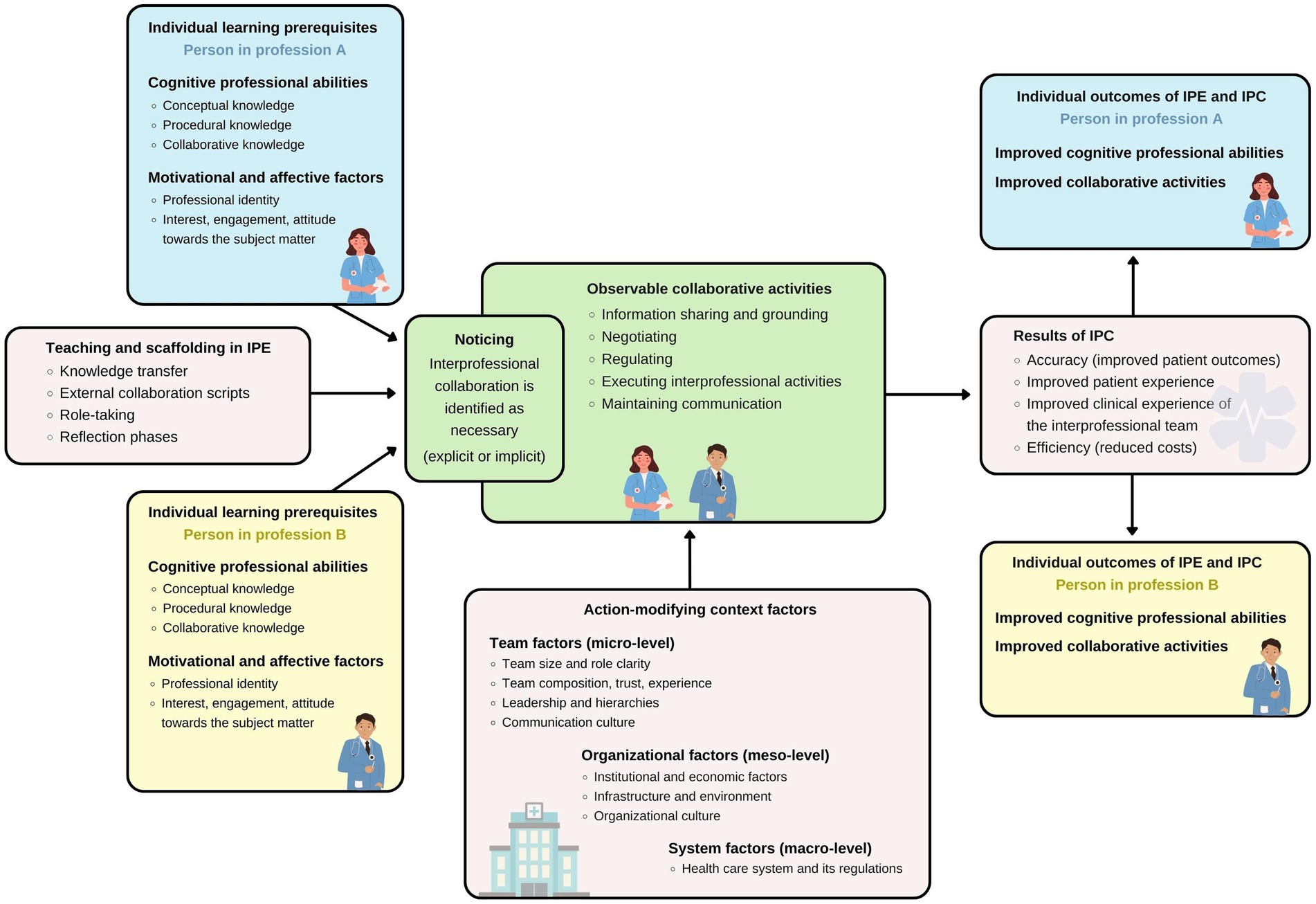
Figure 1. The conceptual framework to improve interprofessional collaboration in health education and care (FINCA). Arrows visualize the influence of the respective activities and factors. For instance, teaching and scaffolding in interprofessional education (IPE) affects noticing and the partially overlapping observable collaborative activities. Both individual learning prerequisites of the persons from different professions involved in the interprofessional collaboration (IPC) and action-modifying context factors influence these collaborative activities. Eventually, results of IPC arise from the collaboration and individual outcomes of IPE and IPC can be assessed for the persons involved.
3.1. Teaching and scaffolding in IPE
Learners and practitioners across all health professions collect and evaluate multiple pieces of clinical information to make decisions about patient care. In doing so, both learners and practitioners use an analytical approach called clinical reasoning. Clinical reasoning refers to all cognitive processes underlying these decisions (31) and includes medical problem-solving and medical decision-making.
In an interprofessional context, collaborative clinical reasoning can lead to a shared mental model about patient problems and further care (32, 33). This includes an interprofessional comparison of different diagnoses or dysfunctions and the process of care, patient monitoring, explanation of treatment options, and team communication. Visser et al. (34) conclude that learners from different health professions discussing treatment plans together would benefit more in their learning process. This is because learners would have to (a) structure their thoughts (cognitive level) and (b) have to provide explanations for learners from other professions, answer their questions, and give feedback to them (metacognitive level) in order to create a common knowledge base.
Both educational research in general and research in health professionals’ education in particular have shown that additional instructional support is needed for learning from challenging problems in complex learning scenarios (18, 28, 35, 36). FINCA therefore suggests various support measures in the context of teaching and learning as important variables that may influence or moderate the observable collaborative activities.
Central to scaffolding is supporting learners by directing attention while they work on a task. This can, for instance, be done by providing cues, case illustrations, or prompts. Numerous empirical studies have demonstrated the effectiveness of scaffolding for knowledge transfer [(see 35)]. A wide variety of types of socio-cognitive scaffolding have been developed for collaborative problem-solving scenarios, e.g., in the form of external collaboration scripts (19). Instructional support with external collaboration scripts can foster learning processes by introducing a sequence for collaborative activities. External collaboration scripts can (a) specify certain activities to be performed by learners, (b) predetermine the timing of activities, or (c) specify collaboration roles and interaction activities (37). External collaboration scripts have been developed for both face-to-face and computer-mediated settings and have been largely successful in improving collaboration processes as well as individual learning outcomes (38). In addition, scripts promote collaborative activities such as exchanging new ideas, asking questions, or negotiating between learning partners. Furthermore, collaboration scripts support deeper cognitive elaboration in individual learners. The use of collaboration scripts such as the handover tool SBAR (Situation, Background, Assessement, Recommendation) and its derivatives has shown promising results in mono-and interprofessional patient care [(e.g., 39, 40)]. The SBAR tool is a scheme for structuring communication processes for the exchange of patient information (41) that organizes this information, reminds of important content and details that may otherwise be lost, and reduces leaps of thought and omissions which is critical to patient safety in a complex system (42, 43). The use of SBAR has even been recommended by the WHO (44).
Another promising type of scaffolding for IPE could be provided by assigning specific roles to learners to reduce the full complexity of a task. Through role-taking, the perspective on the full task can be focused on key learning points. In interprofessional encounters, the roles of the collaborating health professionals and the role of the patient are typical. Systematic role change allows for new perspectives and learning. Additionally, learners can be assigned the role of an observer. Results on acquiring diagnostic competences in the role of an observer are still lacking, but Stegmann et al. (45) showed that communication skills can be acquired effectively in this role.
Reflection phases are another scaffolding approach that holds potential to foster IPE. Nguyen et al. (46) provided a comprehensive definition of reflection as “the process of engaging the self in attentive, critical, exploratory and iterative interactions with one’s thoughts and actions, and their underlying conceptual frame, with a view to changing them and with a view on the change itself” (p. 1182). Guided reflection can take place before, during, or after an event that requires IPC. Different types of guided reflection have been reported to efficiently foster the acquisition of diagnostic competences in medicine (47, 48). There are three main reasons why reflection could be beneficial for learning: (1) Reflection phases add a pause that learners might use to better retrieve and apply conceptual knowledge with less time pressure. Learners might also use such a pause to evaluate the selected strategy and think about alternatives. (2) Learners may generate self-feedback to advance their learning during guided reflection. (3) Reflection phases may also support the planning of subsequent steps in the collaboration process.
To date, there has been little systematic research on what forms of scaffolding are suitable in IPE to foster interprofessional problem-solving skills (49). However, learning with simulations has been shown to have great potential in this regard (50, 51). Against this background, the following support measures have been included by way of example in FINCA, but this list can of course be extended: knowledge transfer, external collaboration scripts, role-taking, and reflection phases.
3.2. Individual learning prerequisites
In any interprofessional interaction, at least two persons from different professions learn and work together (52). Therefore, FINCA takes the individual learning prerequisites of two or more persons from health care professions A and B into account. IPE is about mutual recognition of roles and responsibilities. These vary from profession to profession as well as within professions that specialize. When collaborating interprofessionally, it is important to understand who you are working with and how best to use the skills of each profession and individual for successful collaborative problem-solving. Less optimal practice results from not having this understanding (1).
In the context of teaching and learning, knowledge is understood as the mental representation of information (53). Under cognitive professional abilities, FINCA includes conceptual and procedural knowledge as well as collaborative knowledge (54). Under motivational and affective factors, FINCA includes professional identity as well as interest, engagement, and attitude toward the subject matter.
A comprehensive research program on IPE and its instructional facilitation must address the question of how and to what extent individual learning prerequisites affect the outcomes of IPE and IPC. The benefit of clarifying the relationship between instructional effects and pre-existing individual differences among learners is obvious. Systematically incorporating individual learning prerequisites addresses the question for whom particular instructional designs are likely to be effective. Scientific insights into the moderating effects of individual learning prerequisites can help make interprofessional learning environments more effective and could serve as the basis for individualized and adaptive facilitator support measures that address the learning needs of each professional. This could involve the aforementioned use of simulations that address learning outcomes relevant to learners of all health professions involved (55, 56).
In the following, we propose cognitive, affective, and personality related moderators which can serve as a starting point for more systematic research on how learning prerequisites affect the processes and outcomes of interprofessional patient care and learning with and without additional instructional support.
3.2.1. Cognitive professional abilities
The basis of knowledge acquisition lies in the formation of concepts and contexts in a specific learning area, such as medicine or care. In contrast to this conceptual knowledge, which can also be referred to as factual knowledge, procedural knowledge focuses on the procedure and steps to be followed in clinical problem-solving. Procedural knowledge includes both strategic knowledge (about typical problem-solving strategies) and conditional knowledge (about conditions of application of conceptual and strategic knowledge) (54, 57). Besides individual cognitive structures of learners, collaborative knowledge is an essential element of cognitive professional abilities in FINCA. Collaborative knowledge comprises cognitive activities (e.g., explaining, questioning, summarizing), metacognitive activities (e.g., observing, regulating, formulating arguments), as well as social activities (e.g., taking turns, listening) (19). Although collaborative practice is commonplace in clinical settings, there has been little empirical research on how to analyze and promote the skills required for it (12).
Another view on the professional knowledge base in health care differentiates between biomedical and clinical knowledge (58, 59). Biomedical knowledge includes knowledge about physiological, pathological, as well as psychosocial elements. Clinical knowledge, on the other hand, includes symptoms, symptom patterns and clinical pictures, typical disease courses, as well as suitable therapeutic procedures. While the biopsychosocial model of medicine by Engel (60) is still relevant, there are calls for expanding this model toward a health care system perspective (61). From an interprofessional perspective, such an expansion should comprise perspectives and values of all professions contributing to health and patient care. One outcome of IPE could be, for instance, that health professionals better understand the importance of social and cultural factors for health and illness from diverse professional perspectives and recognise their significance in the care process [cf. (62)].
3.2.2. Motivational and affective factors
FINCA systematically addresses individual learning prerequisites. This includes motivational and affective factors such as interest, engagement, and attitude toward the subject matter. The framework also considers the influence of the development of professional identity in the respective professions involved in IPC. At this point, however, it should be pointed out that there is currently no uniform definition of professional identity within an interprofessional context (63, 64). To our knowledge, there has been no systematic research examining potential moderating effects of motivational and affective factors on the development of interprofessional activities in IPE.
3.3. Noticing
In teacher education research, noticing has been described as a process that lets teachers’ pay attention to significant events within teaching and learning in the classroom (29, 30). Applied to the clinical context, we suggest that noticing can analogously be understood as a psychological process leading to interprofessional interaction and the corresponding collaborative activities.
We propose that noticing occurs at the beginning of any interprofessional interaction or collaboration when there is a realization that collaboration with other health care professions must be initiated to jointly address specific needs of a patient. A distinction can be made between spontaneous noticing, when an unexpected situation requires IPC (e.g., decision to treat a wound with a vacuum pump), and ritualized IPC where noticing happens implicitly (e.g., interprofessional surgical ward rounding). In FINCA, noticing marks the transition to observable collaborative activities (see Figure 1). The communicative part of noticing itself might already be observable and thus amenable to an assessment.
Linking the theoretical elements described earlier, one could hypothesize that noticing leads to an activation of illness scripts and the complementary internal collaboration scripts among the individuals involved. The interaction of individual participants in a given situation thus depends on their memory structures related to their respective memories of a specific social situation (e.g., patient handover). In our view, these memory structures can be conceptualized as internal collaboration scripts that individuals can draw on depending on the situation (19, 25).
3.4. Observable collaborative activities
At the heart of FINCA are observable collaborative activities that can be used to assess individuals’ cognitive and social skills. Liu et al. (20) postulate that collaborative learning scenarios can promote greater integration of knowledge and thus lead to better learner performance. To this end, they propose a conceptual model that includes a matrix of individual cognitive and social skills involved in collaborative problem-solving. This model can also serve as a basis for assessing an individual’s collaborative problem-solving skills. Liu’s assumptions are based on research in computer-supported collaborative learning (65) and also draw on the PISA 2015 Collaborative Problem Solving Framework (66). The conceptual model by Liu and colleagues also considers individual cognitive prerequisites and assigns the following key social skills to them: information sharing, negotiating, regulating, and maintaining communication. In order to incorporate clinical practice, FINCA further adds the more practice-oriented activity executing interprofessional activities.
3.4.1. Information sharing and grounding
The activity information sharing captures how individual group members contribute different ideas to a common conversation (20) or point to relevant resources that help to solve a problem that requires IPC. However, it is important that not only information is shared, but that communication partners also strive for mutual understanding. Clark and Brennan (67) refer to this process as grounding.
3.4.2. Negotiating
In the context of IPC, the term negotiating is often used in the sense of negotiated order theory [(e.g., 21, 68)]. In FINCA, negotiating refers specifically to conversations about the team’s collaborative knowledge construction by comparing alternative ideas and information resources, presenting evidence, and justifying an argument. Subcategories of this activity include asking for clarification, elaborating/reformulating a collaboration partners’ ideas, identifying knowledge gaps, and revising/reformulating one’s own ideas (20).
3.4.3. Regulating
Regulating problem-solving activities refers to conversations about clarifying objectives, monitoring, evaluating, and confirming team understanding of problem-solving. This category focuses on the collaborative regulation aspect of team conversations. It includes subcategories such as identifying aims, evaluating teamwork, and checking mutual understanding regarding aims that were jointly agreed upon (20). In clinical practice, this would occur, for example, when an interprofessional team agrees on a joint management plan for a patient.
3.4.4. Executing interprofessional activities
The observable collaborative activities mentioned previously refer to cognitive and communicative skills. They prepare for executing interprofessional activities that can be assessed on the grounds of clinical standards, guidelines, and patient safety requirements. Instruments for the assessment of interprofessional team collaboration have recently been developed and evaluated [(e.g., 69–71)].
3.4.5. Maintaining communication
Maintaining communication includes all activities related to the conversational climate. This encompasses all conducive activities that enable efficient and effective dyadic communication between a person A and a person B (see Figure 1) or within interprofessional teams. This also includes avoiding professionally irrelevant social communication (20).
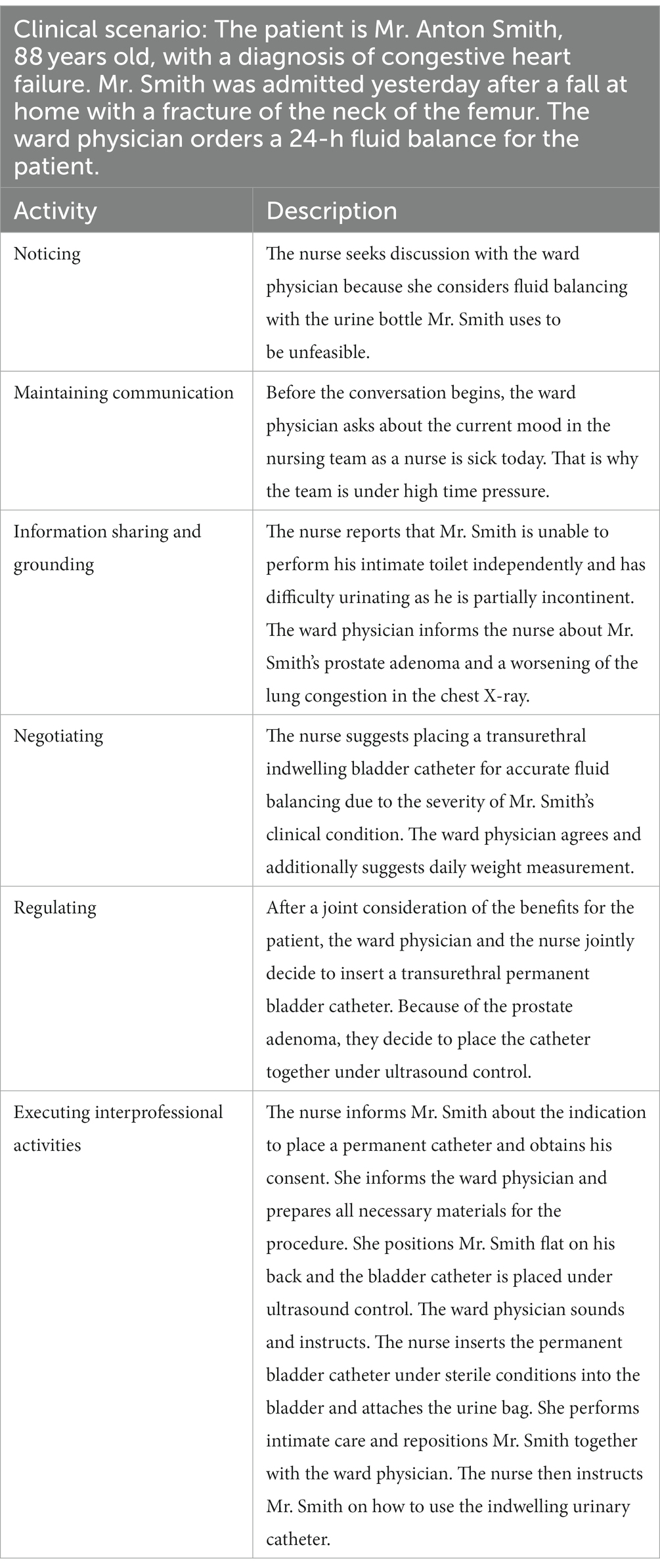
To exemplify the proposed observable collaborative activities we describe a realistic clinical scenario in Table 1. It is important to note that the procedures can be repeated several times and are by no means a linear process. In our example, a nurse and a physician on a ward must jointly decide whether to place a permanent bladder catheter in a patient based on clinical data and observations.
3.5. Action-modifying context factors
FINCA acknowledges action-modifying context factors as potentially significant moderators of interprofessional collaborative activities. The literature suggests a variety of such factors that may influence the effectiveness and efficiency of interprofessional collaborative practice [(e.g., 5, 72, 73)]. However, the evidence base regarding their impact is not sufficient (74). Mulvale et al. (75) identified a number of studies that measured correlations between collaborative processes in interprofessional practice and structural and process factors. Thus, FINCA includes action-modifying context factors which can be divided into team factors (micro-level), organizational factors (meso-level), and system factors (macro-level). At each level, we focus on the contextual and process-related factors that we propose to be associated with interprofessional collaborative activities. While not all of the relevant factors on the respective levels can be influenced to the same extent, we believe they are important to a framework that aims to comprehensively address IPC in health education and care.
3.5.1. Micro-level
Under the micro-level, we subsume formal and informal factors that can influence a team, such as team size and role clarity, team composition, trust between team members, as well as the team’s experience with IPC. We also consider leadership and hierarchies, as well as communication culture within teams as important (76, 77).
3.5.2. Meso-level
The meso-level comprises institutional and economic factors, infrastructure and environment, and organizational culture. It should be noted that context factors on the meso-level are typically beyond the control of individual health professionals.
3.5.3. Macro-level
The macro-level includes the health care system and its regulations, which should be considered on both the educational planning and the organizational side. The context factors on the macro-level are even harder to change in order to improve IPE and IPC.
3.6. Outcomes of IPE and IPC
Following Heitzmann et al. (18) and Liu et al. (20), FINCA aims to capture and assess outcomes of IPE and IPC, both of which are complex and multifaceted constructs. In addition to assessing entire teams and their performance, there is an urgent need in research to develop stable and robust outcome criteria to demonstrate a causal relationship between IPE, IPC, and overall health care system outcomes.
3.6.1. Results of IPC
Bodenheimer and Sinsky’s (78) Quadruple Aim concept is now widely recognized as a compass for optimizing health care delivery and is being further developed as a standard assessment criterion for IPC [(e.g., 79)]. Following this concept, we have included the following promising criteria for assessing results of IPC in FINCA: (1) Accuracy (improved patient outcomes); (2) Improved patient experience; (3) Improved clinical experience of the interprofessional team; (4) Efficiency (reduced costs).
3.6.2. Individual outcomes of IPE and IPC
On top of the prevalent profession-specific assessment instruments for conceptual and procedural knowledge (improved cognitive professional abilities), instruments are needed that allow for the assessment of interprofessional collaborative activities [(e.g., 71)]. According to the current IPE literature (80), individual performance should be assessed separately from team performance when evaluating collaboration in health care (improved collaborative activities). One possibility in this respect is offered by the concept of entrustable professional activities (EPAs). Simply put, this is about detailed authentic descriptions of clinical activities that health care trainees can be entrusted with (81). Recently, transdisciplinary EPAs have been conceptualized to be used for multiple professions (82).
4. Discussion
The present conceptual framework has been developed with scientific consideration of empirical data under various theoretical references. In our view, FINCA adequately reflects the process of IPC in a clinical context building on established theoretical foundations – it operationalizes contextual, person-related, process-related, and outcome-related variables (23) to capture what we postulate to be the observable part of IPC. In this way, the framework provides the basis for analysis and empirical testing of the components and variables described, as well as their interactions across different studies, educational interventions, and action-modifying contexts (micro-, meso-, and macro-level). FINCA further provides the basis for fostering the teaching and learning of interprofessional problem-solving skills across different health care settings.
In addition, FINCA may support faculty and curriculum developers to systematize the implementation and improvement of interprofessional teaching and learning opportunities [cf. (83)]. From a practical perspective, FINCA can help to better align curricula for different health professions in the future.
The proposed framework does not claim to be a theory or model yet – as yet, this is a qualitative synthesis of published literature, the empirical confirmation of which is pending. We invite readers to discuss modifications, additions, innovations, or other perspectives with us. Perspectives from all professional groups involved in health care are explicitly welcome. In principle, we also see potential for transferability of the framework to other domains where different professions collaborate.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
MW, JZ, BW, FF and MF jointly developed the first version of the framework model. MW and JZ wrote the first draft of the manuscript with support from BW. This draft was commented on and expanded by FF, JT and MF. The manuscript was eventually revised by MW, JZ, JT and MF. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Robert Bosch Stiftung (Graduiertenkolleg ILEGRA “Interprofessionelle Lehre in den Gesundheitsberufen – Vermittlung, Evaluation, Prüfung”, grant no. 32.5.A381.0058.0).
Acknowledgments
The authors would like to thank the ILEGRA research fellows, the team of scientists involved in the ILEGRA Graduate School (Birgit Babitsch, Anne Frenzel, Kai-Christoph Hamborg, Swen Malte John, Georg Marckmann, Hartmut Remmers, Ursula Walkenhorst), the members of the ILEGRA International Advisory Board (Simon Kitto, Peter Musaeus, Annette Nauerth, Rudolf Tippelt, Christoff Zalpour), as well as further associated research colleagues who accompanied the development of FINCA (Riikka Hofmann, Anika Mitzkat, Ansgar Opitz, Anika Radkowitsch). Finally, the authors would like to express their special thanks to Simon Kitto for his detailed and most helpful feedback on an early version of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Thistlethwaite, JE. Interprofessional education: a review of context, learning and the research agenda. Med Educ. (2012) 46:58–70. doi: 10.1111/j.1365-2923.2011.04143.x
2. Tsakitzidis, G, Timmermans, O, Callewaert, N, Verhoeven, V, Lopez-Hartmann, M, Truijen, S, et al. Outcome indicators on Interprofessional collaboration interventions for elderly. Int J Integr Care. (2016) 16:5. doi: 10.5334/ijic.2017
3. Dauven, S, and Cobbers, B. Koordination und Integration: Gesundheitsversorgung in einer Gesellschaft des längeren Lebens. Gesundheits-und Sozialpolitik. (2009) 63:15–21. doi: 10.5771/1611-5821-2009-6-15
4. Robert Bosch Stiftung (2011). Memorandum Kooperation der Gesundheitsberufe: Qualität und Sicherstellung der zukünftigen Gesundheitsversorgung. Available at: https://www.bosch-stiftung.de/sites/default/files/publications/pdf_import/Memorandum_Kooperation_der_Gesundheitsberufe.pdf
5. Walkenhorst, U, Mahler, C, Aistleithner, R, Hahn, EG, Kaap-Fröhlich, S, Karstens, S, et al. Position statement GMA committee – "Interprofessional education for the health care professions". GMS Z Med Ausbild. (2015) 32:Doc22. doi: 10.3205/zma000964
6. Wissenschaftsrat (2018). Neustrukturierung des Medizinstudiums und Änderung der Approbationsordnung für Ärzte–Empfehlungen der Expertenkommission zum Masterplan Medizinstudium. Available at: https://www.wissenschaftsrat.de/download/archiv/7271-18.pdf
7. World Health Organization (2010). Framework for action on Interprofessional Education & Collaborative Practice. Available at: https://www.who.int/publications/i/item/framework-for-action-on-interprofessional-education-collaborative-practice
8. Reeves, S, Lewin, S, Espin, S, and Zwarenstein, M. Interprofessional teamwork for health and social care. Oxford: Blackwell (2010).
9. Barr, H, Koppel, I, Reeves, S, Hammick, M, and Freeth, DS. Effective interprofessional education. Oxford: Blackwell (2005).
10. Cox, M, Cuff, P, Brandt, B, Reeves, S, and Zierler, B. Measuring the impact of interprofessional education on collaborative practice and patient outcomes. J Interprof Care. (2016) 30:1–3. doi: 10.3109/13561820.2015.1111052
11. Reeves, S, Perrier, L, Goldman, J, Freeth, D, and Zwarenstein, M. Interprofessional education: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. (2013) 2013:CD002213. doi: 10.1002/14651858.CD002213.pub3
12. Spaulding, EM, Marvel, FA, Jacob, E, Rahman, A, Hansen, BR, Hanyok, LA, et al. Interprofessional education and collaboration among healthcare students and professionals: a systematic review and call for action. J Interprof Care. (2021) 35:612–1. doi: 10.1080/13561820.2019.1697214
13. Brewer, ML, and Jones, S. An interprofessional practice capability framework focusing on safe, high-quality, client-centred health service. J Allied Health. (2013) 42:e45–9.
14. Canadian Interprofessional Health Collaborative (2010). A national Interprofessional competency framework. https://phabc.org/wp-content/uploads/2015/07/CIHC-National-Interprofessional-Competency-Framework.pdf
15. Interprofessional Education Collaborative Expert Panel (2011). Core competencies for interprofessional collaborative practice: Report of an expert panel. Interprofessional Education Collaborative.
16. Walsh, CL, Gordon, MF, Marshall, M, Wilson, F, and Hunt, T. Interprofessional capability: a developing framework for interprofessional education. Nurse Educ Pract. (2005) 5:230–7. doi: 10.1016/j.nepr.2004.12.004
17. Thistlethwaite, JE, Forman, D, Matthews, LR, Rogers, GD, Steketee, C, and Yassine, T. Competencies and frameworks in interprofessional education: a comparative analysis. Acad Med. (2014) 89:869–5. doi: 10.1097/ACM.0000000000000249
18. Heitzmann, N, Seidel, T, Opitz, A, Hetmanek, A, Wecker, C, Fischer, MR, et al. Facilitating diagnostic competences in simulations: a conceptual framework and a research agenda for medical and teacher education. Frontline Learn Res. (2019) 7:1–24. doi: 10.14786/flr.v7i4.384
19. Fischer, F, Kollar, I, Stegmann, K, and Wecker, C. Toward a script theory of guidance in computer-supported collaborative learning. Educ Psychol. (2013) 48:56–66. doi: 10.1080/00461520.2012.748005
20. Liu, L, Hao, J, von Davier, A, Kyllonen, P, and Zapata-Rivera, J-D. A tough nut to crack: measuring collaborative problem solving In: Y Rosen, S Ferrara, and M Mosharraf, editors. Handbook of research on technology tools for real-world skill development. Pennsylvania: IGI Global (2016)
21. Schot, E, Tummers, L, and Noordegraaf, M. Working on working together. A systematic review on how healthcare professionals contribute to interprofessional collaboration. J Interprof Care. (2020) 34:332–2. doi: 10.1080/13561820.2019.1636007
22. Kitzinger, J. Focus groups In: C Pope and N Mays, editors. Qualitative research in health care. Hoboken: Blackwell Publishing (2006)
23. Biggs, J, Kember, D, and Leung, DY. The revised two-factor study process questionnaire: R-SPQ-2F. Br J Educ Psychol. (2001) 71:133–9. doi: 10.1348/000709901158433
24. Vreugdenhil, J, Döpp, D, Custers, EJ, Reinders, ME, Dobber, J, and Kusukar, RA. Illness scripts in nursing: directed content analysis. J Adv Nurs. (2022) 78:201–10. doi: 10.1111/jan.15011
25. Kiesewetter, J, Kollar, I, Fernandez, N, Lubarsky, S, Kiessling, C, Fischer, MR, et al. Crossing boundaries in interprofessional education: a call for instructional integration of two script concepts. J Interprof Care. (2016) 30:689–2. doi: 10.1080/13561820.2016.1184238
26. Kiesewetter, J, Gluza, M, Holzer, M, Saravo, B, Hammitzsch, L, and Fischer, MR. Towards a measurement of internalization of collaboration scripts in the medical context – results of a pilot study. GMS Z Med Ausbild. (2015) 32:974. doi: 10.3205/zma000974
27. Tremblay, ML, Lafleur, A, Dieckmann, P, Rethans, JJ, and Dolmans, D. Collaboration scripts or checklists to engage novice observers in immersive simulation? Simul Healthcare. (2023). doi: 10.1097/sih.0000000000000713
28. Zottmann, JM, Dieckmann, P, Taraszow, T, Rall, M, and Fischer, F. Just watching is not enough: fostering simulation-based learning with collaboration scripts. GMS J Med Educ. (2018) 35:Doc35. doi: 10.3205/zma001181
29. Rainio, AP, and Hofmann, R. Teacher professional dialogues during a school intervention: from stabilization to possibility discourse through reflexive noticing. J Learn Sci. (2021) 30:707–6. doi: 10.1080/10508406.2021.1936532
30. Seidel, T, and Stürmer, K. Modeling and measuring the structure of professional vision in preservice teachers. Am Educ Res J. (2014) 51:739–1. doi: 10.3102/0002831214531321
31. Elstein, AS, and Schwartz, A. Clinical problem solving and diagnostic decision making: selective review of the cognitive literature. BMJ. (2002) 324:729–2. doi: 10.1136/bmj.324.7339.729
32. Hanum, C, Findyartini, A, and Soemantri, D. Collaborative clinical reasoning learning using an integrated care pathway in undergraduate interprofessional education: an explorative study. J Interprof Care. (2023) 37:438–7. doi: 10.1080/13561820.2022.2086221
33. Kiesewetter, J, Fischer, F, and Fischer, MR. Collaborative clinical reasoning – a systematic review of empirical studies. J Contin Educ Health Prof. (2017) 37:123–8. doi: 10.1097/CEH.0000000000000158
34. Visser, CL, Wouters, A, Croiset, G, and Kusurkar, RA. Scaffolding clinical reasoning of health care students: a qualitative exploration of Clinicians' perceptions on an Interprofessional obstetric Ward. J Med Educ Curric Dev. (2020) 7:90791. doi: 10.1177/2382120520907915
35. Chernikova, O, Heitzmann, N, Fink, MC, Timothy, V, Seidel, T, Fischer, F, et al. Facilitating diagnostic competences in higher education – a Meta-analysis in medical and teacher education. Educ Psychol Rev. (2020) 32:157–6. doi: 10.1007/s10648-019-09492-2
36. Kerres, A, Hausen, A, Wissing, C, and Kemser, J. Studiengangsübergreifendes Lernen im Sim Lab. PADUA. (2019) 14:244–8. doi: 10.1024/1861-6186/a000509
37. Kollar, I, Fischer, F, and Slotta, JD. Internal and external scripts in computer-supported collaborative inquiry learning. Learn Instr. (2007) 17:708–1. doi: 10.1016/j.learninstruc.2007.09.021
38. Radkowitsch, A, Vogel, F, and Fischer, F. Good for learning, bad for motivation? A meta-analysis on the effects of computer-supported collaboration scripts. Int J Comput-Support Collab Learn. (2020) 15:5–47. doi: 10.1007/s11412-020-09316-4
39. De Meester, K, Verspuy, M, Monsieurs, KG, and Van Bogaert, P. SBAR improves nurse–physician communication and reduces unexpected death: a pre and post intervention study. Resuscitation. (2013) 84:1192–6. doi: 10.1016/j.resuscitation.2013.03.016
40. Gross, B, Rusin, L, Kiesewetter, J, Zottmann, JM, Fischer, MR, Prückner, S, et al. Microlearning for patient safety: crew resource management training in 15-minutes. PLoS One. (2019) 14:e0213178. doi: 10.1371/journal.pone.0213178
41. Haig, KM, Sutton, S, and Whittington, J. SBAR: a shared mental model for improving communication between clinicians. Jt Comm J Qual Patient Saf. (2006) 32:167–5. doi: 10.1016/S1553-7250(06)32022-3
42. von Dossow, V, and Zwißler, B. Empfehlung der DGAI zur strukturierten Patientenübergabe in der perioperativen Phase–Das SBAR-Konzept. AINS. (2016) 51:136–7. doi: 10.1055/s-0042-101190
43. Foster, S, and Manser, T. The effects of patient handoff characteristics on subsequent care: a systematic review and areas for future research. Acad Med. (2012) 87:1105–24. doi: 10.1097/ACM.0b013e31825cfa69
44. World Health Organization (2007). Lösungskonzepte zur Patientensicherheit. Available at: https://www.plattformpatientensicherheit.at/download/publikationen/PatientSolutionsGERMAN.pdf
45. Stegmann, K, Pilz, F, Siebeck, M, and Fischer, F. Vicarious learning during simulations: is it more effective than hands-on training? Med Educ. (2012) 46:1001–8. doi: 10.1111/j.1365-2923.2012.04344.x
46. Nguyen, QD, Fernandez, N, Karsenti, T, and Charlin, B. What is reflection? A conceptual analysis of major definitions and a proposal of a five-component model. Med Educ. (2014) 48:1176–89. doi: 10.1111/medu.12583
47. Mamede, S, van Gog, T, Sampaio, AM, de Faria, RM, Maria, JP, and Schmidt, HG. How can students’ diagnostic competence benefit most from practice with clinical cases? The effects of structured reflection on future diagnosis of the same and novel diseases. Acad Med. (2014) 89:121–7. doi: 10.1097/ACM.0000000000000076
48. Sandars, J. The use of reflection in medical education: AMEE guide no. 44. Med Teach. (2009) 31:685–5. doi: 10.1080/01421590903050374
49. Visser, CL, Ket, JC, Croiset, G, and Kusurkar, RA. Perceptions of residents, medical and nursing students about Interprofessional education: a systematic review of the quantitative and qualitative literature. BMC Med Educ. (2017) 17:77. doi: 10.1186/s12909-017-0909-0
50. Lunde, L, Moen, A, Jakobsen, RB, Rosvold, EO, and Brænd, AM. Exploring healthcare students’ interprofessional teamwork in primary care simulation scenarios: collaboration to create a shared treatment plan. BMC Med Educ. (2021) 21:416. doi: 10.1186/s12909-021-02852-z
51. Motola, I, Devine, LA, Chung, HS, Sullivan, JE, and Issenberg, SB. Simulation in healthcare education: a best evidence practical guide. AMEE guide no. 82. Med Teach. (2013) 35:e1511–30. doi: 10.3109/0142159X.2013.818632
52. Barr, H, Gray, R, Helme, M, Low, H, and Reeves, S. CAIPE Interprofessional education guidelines 2016. Fareham: Centre for the Advancement of Interprofessional Education (2016).
54. Förtsch, C, Sommerhoff, D, Fischer, F, Fischer, MR, Girwidz, R, Obersteiner, A, et al. Systematizing professional knowledge of medical doctors and teachers: development of an interdisciplinary framework in the context of diagnostic competences. Educ Sci. (2018) 8:207. doi: 10.3390/educsci8040207
55. Saragih, ID, Tarihoran, DE, Sharma, S, and Chou, F-H. A systematic review and meta-analysis of outcomes of interprofessional education for healthcare students from seven countries. Nurse Educ Pract. (2023) 71:103683. doi: 10.1016/j.nepr.2023.103683
56. Zendejas, B, Brydges, R, Wang, AT, and Cook, DA. Patient outcomes in simulation-based medical education: a systematic review. J Gen Intern Med. (2013) 28:1078–89. doi: 10.1007/s11606-012-2264-5
57. Schmidmaier, R, Eiber, S, Ebersbach, R, Schiller, S, Hege, I, Holzer, M, et al. Learning the facts in medical school is not enough: which factors predict successful application of procedural knowledge in a laboratory setting? BMC Med Educ. (2013) 13:28. doi: 10.1186/1472-6920-13-28
58. Boshuizen, H. On the role of biomedical knowledge in clinical reasoning by experts, intermediates and novices. Cogn Sci. (1992) 16:153–4. doi: 10.1016/0364-0213(92)90022-M
59. van de Wiel, MW, Boshuizen, HP, and Schmidt, HG. Knowledge restructuring in expertise development: evidence from pathophysiological representations of clinical cases by students and physicians. Eur J Cogn Psychol. (2000) 12:323–6. doi: 10.1080/09541440050114543
60. Engel, GL. The clinical application of the biopsychosocial model. Am J Psychiatr. (1980) 137:535–4. doi: 10.1176/ajp.137.5.535
61. Wade, DT, and Halligan, PW. The biopsychosocial model of illness: a model whose time has come. Clin Rehabil. (2017) 31:995–04. doi: 10.1177/0269215517709890
62. Richter, M, and Hurrelmann, K. Soziologie von Gesundheit und Krankheit. London: Springer (2016).
63. Thistlethwaite, JE, Kumar, K, and Roberts, C. Becoming interprofessional: professional identity formation in the health professions In: RL Cruess, SR Cruess, and Y Steinert, editors. Teaching medical professionalism: Supporting the development of a professional identity. 2nd ed. Cambridge: Cambridge University Press (2016)
64. Tong, R, Brewer, M, Flavell, H, and Roberts, LD. Professional and interprofessional identities: a scoping review. J Interprofess Care. (2020):1–9. doi: 10.1080/13561820.2020.1713063
65. Cress, U, Rosé, C, Wise, A, and Oshima, J. International handbook of computer-supported collaborative learning. Cham: Springer (2021).
66. Hao, J, Liu, L, von Davier, A, Kyllonen, P, and Kitchen, C Collaborative problem solving skills versus collaboration outcomes: findings from statistical analysis and data mining. In T. Barnes, M. Chi, and M. Feng (Eds.), Proceedings of the 9th International Conference on Educational Data Mining (2016). IEDMS.
67. Clark, HH, and Brennan, SE. Grounding in communication In: LB Resnick, J Levine, and SD Teasley, editors. Perspectives on socially shared cognition. Washington: American Psychological Association (1991)
68. Goldman, J, Reeves, S, Wu, R, Silver, I, Mac Millan, K, and Kitto, S. Medical residents and interprofessional interactions in discharge: an ethnographic exploration of factors that affect negotiation. J Gen Intern Med. (2015) 30:1454–60. doi: 10.1007/s11606-015-3306-6
69. Bain, L, Kennedy, C, Archibald, D, LePage, J, and Thorne, C. A training program designed to improve interprofessional knowledge, skills and attitudes in chronic disease settings. J Interprof Care. (2014) 28:419–5. doi: 10.3109/13561820.2014.898622
70. Havyer, RD, Nelson, DR, Wingo, MT, Comfere, NI, Halvorsen, AJ, McDonald, FS, et al. Addressing the Interprofessional collaboration competencies of the Association of American Medical Colleges: a systematic review of assessment instruments in undergraduate medical education. Acad Med. (2016) 91:865–8. doi: 10.1097/ACM.0000000000001053
71. Sicks, S, Umland, E, Koch, A, Hass, RW, and Tenpa, J. Measuring interprofessional education and collaborative practice competencies: a content validity study of the Jefferson teamwork observation guide®. J Interprof Care. (2022) 36:691–7. doi: 10.1080/13561820.2021.1972946
72. Atzeni, G, Schmitz, C, and Berchtold, P. Die Praxis gelingender interprofessioneller Zusammenarbeit: studie im Auftrag der SAMW. Swiss Academies Reports. (2017) 12:5–58.
73. Oandasan, I, and Reeves, S. Key elements for interprofessional education. Part 1: the learner, the educator and the learning context. J Interprof Care. (2005) 19:21–38. doi: 10.1080/13561820500083550
74. Zwarenstein, M, Goldman, J, and Reeves, S. Interprofessional collaboration: effects of practice-based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. (2009) 3:CD000072. doi: 10.1002/14651858.CD000072.pub2
75. Mulvale, G, Embrett, M, and Razavi, SD. 'Gearing Up' to improve interprofessional collaboration in primary care: a systematic review and conceptual framework. BMC Fam Pract. (2016) 17:83. doi: 10.1186/s12875-016-0492-1
76. Reeves, S, Pelone, F, Harrison, R, Goldman, J, and Zwarenstein, M. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst Rev. (2017) 6:CD000072. doi: 10.1002/14651858.CD000072.pub3
77. Sheffer-Hilel, G, Drach-Zahavy, A, and Endevelt, R. The paradoxical effects of professional stereotypes on the quality of care by interprofessional teams: the contingent effects of team faultlines, team stereotypes, and championship behaviors. Front Psychol. (2023) 14:1135071. doi: 10.3389/fpsyg.2023.1135071
78. Bodenheimer, T, and Sinsky, C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. (2014) 12:573–6. doi: 10.1370/afm.1713
79. Guck, TP, Walters, RW, Abdul-Greene, C, Doll, J, Greene, MA, and McGaha, AL. Sustainable and replicable clinical and financial outcomes in an interprofessional education and collaborative practice nexus. J Interprofess Care. (2021):1–8. doi: 10.1080/13561820.2021.1932776
80. ten Cate, O, and Pool, IA. The viability of interprofessional entrustable professional activities. Adv Health Sci Educ. (2020) 25:1255–62. doi: 10.1007/s10459-019-09950-0
81. ten Cate, O, and Taylor, DR. The recommended description of an entrustable professional activity: AMEE guide no. 140. Med Teach. (2021) 43:1106–14. doi: 10.1080/0142159X.2020.1838465
82. Pool, I, Hofstra, S, van der Horst, M, and ten Cate, O. Transdisciplinary entrustable professional activities. Med Teach. (2023) 45:1019–24. doi: 10.1080/0142159X.2023.2170778
Keywords: interprofessional education, interprofessional collaboration, collaborative problem-solving skills, observable collaborative activities, learning, teaching, scaffolding
Citation: Witti MJ, Zottmann JM, Wershofen B, Thistlethwaite JE, Fischer F and Fischer MR (2023) FINCA – a conceptual framework to improve interprofessional collaboration in health education and care. Front. Med. 10:1213300. doi: 10.3389/fmed.2023.1213300
Edited by:
Juliane E. Kämmer, University of Bern, SwitzerlandReviewed by:
Shaista S. Guraya, Royal College of Surgeons in Ireland (Bahrain), BahrainReimer Riessen, University of Tübingen, Germany
Copyright © 2023 Witti, Zottmann, Wershofen, Thistlethwaite, Fischer and Fischer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jan M. Zottmann, amFuLnpvdHRtYW5uQG1lZC51bmktbXVlbmNoZW4uZGU=
†These authors have contributed equally to this work
 Matthias J. Witti1†
Matthias J. Witti1† Jan M. Zottmann
Jan M. Zottmann Jill E. Thistlethwaite
Jill E. Thistlethwaite Martin R. Fischer
Martin R. Fischer