- 1Department of Basic Medical Sciences, Faculty of Medicine, Al-Balqa Applied University, Al-Salt, Jordan
- 2Applied Science Research Center, Applied Science Private University, Amman, Jordan
- 3Department of Pharmacy, Faculty of Pharmacy, Al-Zaytoonah University of Jordan, Amman, Jordan
- 4Laboratory for Molecular Modeling, Division of Chemical Biology and Medicinal Chemistry, Eshelman School of Pharmacy, The University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 5Jordan CDC, Amman, Jordan
- 6Department of Curriculum and Methods of Instruction, United Arab Emirates University, Al Ain, United Arab Emirates
- 7Faculty of Educational Sciences, Hashemite University, Zarqa, Jordan
- 8Department of Clinical Laboratory Sciences, University of Jordan, Amman, Jordan
Background: COVID-19 vaccines continue to save people’s lives around the world; however, some vaccine adverse events have been a major concern which slowed down vaccination campaigns. Anecdotal evidence pointed to the vaccine effect on menstruation but evidence from the adverse event reporting systems and the biomedical literature was lacking. This study aimed to investigate the physiological changes in women during menstruation amid the COVID-19 vaccination.
Methods: A cross-sectional online survey was distributed to COVID-19 vaccinated women from Nov 2021 to Jan 2022. The results were analyzed using the SPSS software.
Results: Among the 564 vaccinated women, 52% experienced significant menstrual irregularities post-vaccination compared to before regardless of the vaccine type. The kind of menstrual irregularity varied among the vaccinated women, for example, 33% had earlier menstruation, while 35% reported delayed menstruation. About 31% experienced heavier menstruation, whereas 24% had lighter menstrual flow. About 29% had menstruation last longer, but 13% had it shorter than usual. Noteworthy, the menstrual irregularities were more frequent after the second vaccine shot, and they disappeared within 3 months on average. Interestingly, 24% of the vaccinated women reported these irregularities to their gynecologist.
Conclusion: The COVID-19 vaccine may cause physiological disturbances during menstruation. Luckily, these irregularities were short-termed and should not be a reason for vaccine hesitancy in women. Further studies are encouraged to unravel the COVID-19 vaccine adverse effect on women’s health.
Introduction
COVID-19 vaccines have decreased the burden of SARS-CoV-2 infections worldwide by averting 80–90% of hospitalized individuals from getting reinfected and attenuating 40–65% of signs and symptoms (1, 2). The availability of various vaccine platforms has saved people’s lives and reduced hospital care and death toll, distinctly through the first 6 months of being fully vaccinated with two doses (3–6). Vaccines have circumvented the prevalence of COVID-19, prevented severe pandemic waves in vaccinated communities, and decreased lockdown protocols and governmental inspection measures (7, 8). The widely distributed vaccines platforms that were approved by either the US Food and Drug Administration (FDA) or the World Health Organization (WHO) were: messenger RNA (mRNA) vaccines, viral vector (adenovirus) vaccines, and inactivated (killed SARS-CoV-2 virus) vaccines.
While COVID-19 vaccines were important tools in the fight against SARS-CoV-2, they were associated with adverse events like any other pharmaceutical drugs. Some adverse events were common or frequent, and others were rare or uncommon. For example, the most frequently reported COVID-19 vaccine adverse events were headache, fever, fatigue and muscle pain. BioNTech/Pfizer vaccine triggered diverse adverse effects within 27% of vaccinated people (9) including arrhythmia, fatigue, headache, lymphadenopathy, right leg paresthesia, and vaccination site injury (5, 10, 11). Moderna’s vaccine resulted in chills, fatigue, headache, joint and muscle pain, rashes, and pain or swelling at the injection site (12). Johnson & Johnson’s vaccine led to blood clots in vaccinated people (13). Sinopharm’s vaccine was accompanied with fatigue, lethargy, headache, and tenderness especially after the second vaccine shot, and in higher frequency in females compared to males (14).
Adverse event databases as the vaccine adverse event reporting system (VAERS) and the Eudra Vigilance European database, highlighted serious cardiovascular adverse events after receiving COVID-19 vaccines including myocarditis, pericarditis, venous thromboembolism, hemorrhage, myocardial infarction, and stroke (15). In fact, many published articles reported on the development of acute myocarditis and pericarditis following COVID19 vaccination (16–18) and derived mechanistic hypotheses to explain these events (16, 17, 19).
Fears that COVID-19 vaccines could affect the female reproductive system escalated both on social media and in the scientific literature. Menstrual adverse events including menstrual cycle irregularity were reported after receiving COVID-19 vaccines (20). Studies reported that 50–60% of reproductive age women, who received the first dose of COVID-19 vaccine, have menstrual cycle disturbances regardless of the administered vaccine platforms (21). Changes in periodicity of the succeeding menstrual cycles were reported after the first vaccination dose of the different vaccine types; 66.7% of AstraZeneca (Vaxzevria), 57.1% of Pfizer-BioNTech (Comirnaty), 47.4% of Moderna (Spikevax), and 33.3% of Johnson & Johnson (Janssen) vaccinated females (21). The prevalent menstrual changes were longer and heavier menstrual cycles than normal (21) in addition to a minor change in the cycle length (22). It should be noted that COVID-19 infection itself affected women’s reproductive system and led to menstrual cycle changes. A clinical study on women of reproductive age showed that 25% of COVID-19 infected females had menstrual disturbances (23) and they experienced changes in mensural volume and/or cycle duration after being diagnosed with COVID-19 infection (23). In addition to SARS-CoV-2 infection itself and COVID-19 vaccines, stress was suggested as a plausible reason for menstrual cycle changes during the pandemic (24, 25).
Although, the UK’s Medicines and Healthcare products Regulatory Agency (MHRA) (20) did not confirm a potential link between menstrual changes and COVID-19 vaccines (26, 27). The agency recommended further probing of post-COVID-19-vaccine menstrual disturbances (26, 28, 29). However, post-vaccine menstrual changes were not frequently reported in vaccine adverse effects reporting systems including VAERS database of the United States (26, 27) and local healthcare records from Jordan. We attributed this to that fact that women do not often perceive menstrual changes as an immediate threat to their lives and therefore may not seek medical attention or report it to healthcare authorities. Additionally, the vaccine effect on menstruation was understudied in Jordan and the Middle East, despite an increasing number of reports circulating on social media regarding post-vaccine adverse effects on the menstrual cycle and fertility, leading to more vaccine-hesitancy among Jordanian women. Thus, we opted to investigate the association between COVID-19 vaccines and menstrual changes and study the physiological changes in women during menstruation amid after receiving COVID-19 vaccine.
The rationale for conducting this study relied on increasing number of reports in the biomedical literature pointing to a possible relationship between COVID-19 vaccines and menstrual changes. These reports were exploited by anti-vaxxers who claimed that vaccine-induced menstrual changes could cause infertility. This led to increased rates of vaccine hesitancy among women world-wide including women in Middle Eastern countries like Jordan where people prefer large families and put more emphasis on fertility issues.
The main questions that this study aimed to answer were the following:
1. Are COVID-19 vaccines associated with menstrual cycle irregularities among Jordanian women?
2. Do post-vaccine menstrual cycle irregularities depend on the type of vaccine?
3. Does the COVID-19 vaccine type affect the duration of menstrual cycle irregularities?
Methods
Study design
This was an anonymous observational cross-sectional study. Quantitative data methodology was used to collect data. A specifically designed questionnaire was used to collect data from participants who were COVID-19 vaccinated women.
Data collection and data processing
The vaccinated women questionnaire was prepared and edited by the research team which includes physiologists, medical pharmacists, and a professor in the Department of Biology Education. The development of the questionnaire was guided by the one that Phelan et al. (30) used in their study.
Study validation
For validation, initial drafts of the questionnaire were submitted to a group of experts to comment on the items’ relevance, clarity, and language accuracy. The reviewers were asked to suggest any additions, deletions, or replacements of any unsuitable items in the questionnaires. Based on the experts’ feedback, some modifications were introduced to the questionnaire to make it ready for the administration stage. The study was conducted and reported according to published best practice guidelines for reporting observational studies (STROBE) (31).
The validated version of the questionnaire consisted of three parts: Part 1: discussed the socio-demographic information of the vaccinated women including (age, marital status, functional status, educational level, and place of living). Part 2: collected COVID-19 vaccine information from the vaccinated women (the type of vaccine and the number of vaccine shots). Part 3: discussed the period status of the vaccinated women, it included two sections, 3-A: included factors that may cause menstrual cycle irregularities among the vaccinated females such as using contraceptives, and the presence of any of the common female reproductive problems including; ovarian cysts, pelvic inflammatory diseases, uterine fibroids, thyroid disorders, and osteoporosis. 3-B: evaluated the menstrual cycle irregularities details like the first incidence, quality, and duration.
The study’s questionnaire was included into an online survey which had an introductory paragraph describing the aim of the study. Additionally, it was mentioned in the survey that the participation in this study is voluntary and optional, and that the participants’ information is highly confidential. Filling the survey was estimated to take 3–5 min to finish. The survey was prepared in English, then translated to Arabic and was distributed in Arabic language. Survey responses were translated back to English. All translations were made using the forward-backward translation techniques (32). A full list of survey questions can be found in Supplementary Tables 1, 2.
The survey was published from November 2021 through January 2022 using Google application forms, and the survey link was distributed via email as well as social media channels including Facebook and WhatsApp applications. Ethical approval was granted for the study by the Al-Zaytoonah University Ethics Unit. Written consent was not required as all data was collected anonymously.
The survey was distributed by the research team to eligible individuals who were females with ages 16 and above, i.e., all women who were eligible to take the COVID-19 vaccine according to the Ministry of Health in Jordan.1 Eligibility criteria included the following: healthy, non-pregnant, non-lactating women, with no restrictions on the demographic information. The required sample size was calculated using the online Raosoft sample size calculator.2 The target study population consisted of the fully vaccinated population in Jordan as of November 1st, 2021 was 3,534,187 (see text footnote 1). Ideally, the percentage of vaccinated women should have been considered as the target population, but this information was not publicly available. That said, the calculated minimum sample size was 385, at a confidence level of 95%. A sample size calculation was performed. The actual sample size was 564 considering all vaccinated women who answered the survey questions, with a margin of error of 4.13%.
Statistical analysis
Raw data were coded and analyzed using IBM’s SPSS software (2020) (SPSS Inc., Chicago, IL, United States). Parametric data is reported as mean and standard deviation (SD). Chi-Square test was used to analyze non-Parametric data. Descriptive and analytical statistical measures and indices were calculated to answer the proposed research questions. Pearson correlation coefficients were used to assess the strength of associations between vaccines and several menstrual cycle irregularities among the vaccinated women. A p-value ≤ 0.05 was considered statistically significant.
Searching the vaccine adverse event reporting system (VAERS)
The vaccine adverse event reporting system (VAERS) (33) database was searched for “menstrual irregularity” adverse events in response to COVID-19 vaccines. Our query consisted of searching “all symptoms” for “COVID-19 vaccines” included in the database. Filtering was later done on “irregularity menstrual,” and manually inspecting all terms linked to menstruation.
Results
The sociodemographic information of the vaccinated women
The sociodemographic information of the 564 vaccinated women was summarized in Figure 1. Eighty-five percent of the vaccinated women were between 18 and 45 years old, 62% of them were married. Regarding the employment status, 48% were employed, 12.9% of them were employed in health care sectors. Concerning the educational level, about 70% had either Diploma or Bachelor’s degree. A large share (87.9%) of the surveyors were living in urban areas.

Figure 1. The sociodemographic information of the vaccinated women. (A) A bar chart represents the vaccinated women’ age categories in years. (B) A doughnut chart represents the vaccinated women marital status. (C) A doughnut chart represents vaccinated women functional status. (D) A doughnut chart represents the vaccinated women educational level. (E) A doughnut chart represents the vaccinated women place of living.
The COVID-19 information of the vaccinated women
The vaccine information for participating women was shown in Figure 2. About 55% of the surveyed women had Pfizer–BioNTech, 12.0% Oxford–AstraZeneca, 32.0% Sinopharm BBIBP, and only 1.0% had Moderna vaccine (Figure 2A). Most of the vaccinated women (90.6%) had two vaccine shots of the same vaccine type (Figure 2B). Noteworthy, the third vaccine shot that was given to people in Jordan was only Pfizer–BioNTech vaccine.
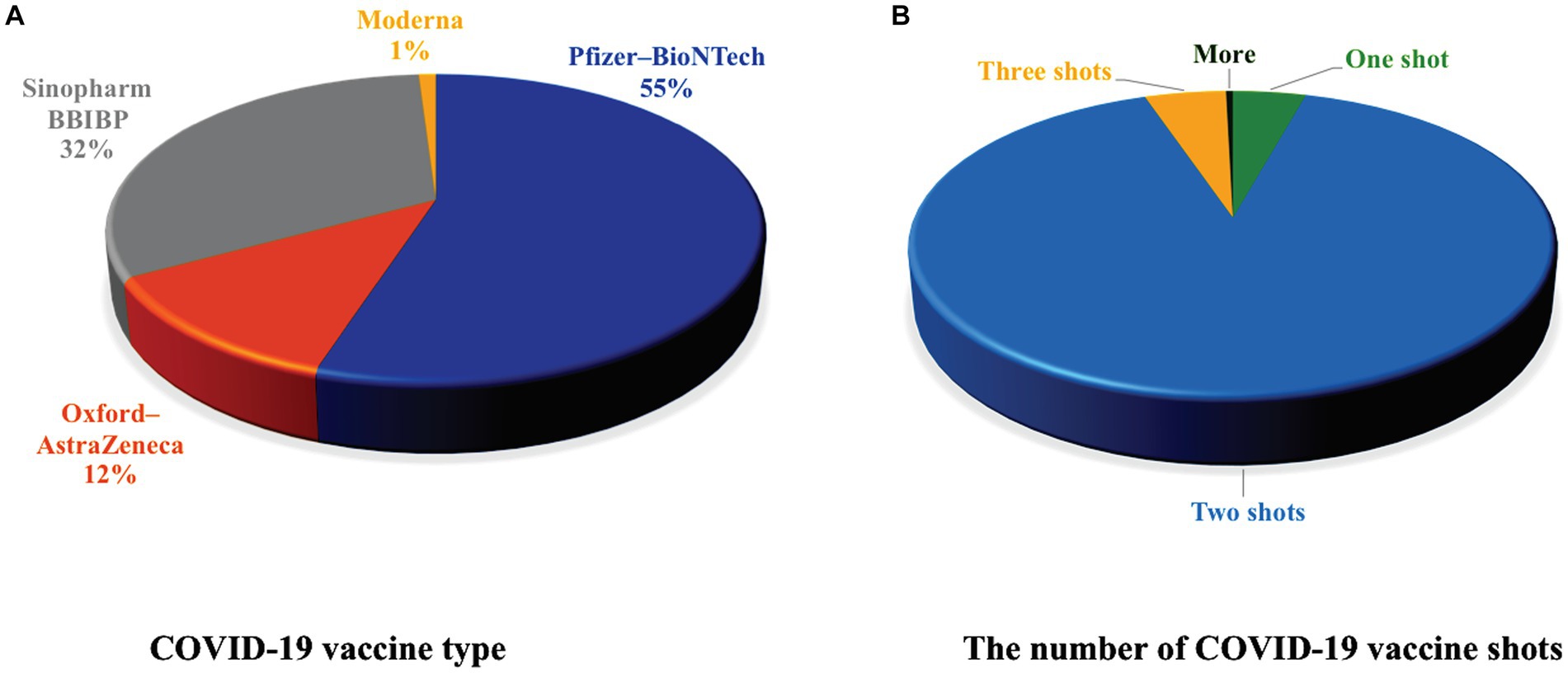
Figure 2. The COVID-19 information for the vaccinated women. (A) A pie chart showing the percentage of the different types of COVID-19 vaccines used by the vaccinated women. 55% had Pfizer–BioNTech, 12.0% Oxford–AstraZeneca, 32.0% Sinopharm BBIBP, and 1.0% had Moderna. (B) A pie chart representing the number of vaccine shots received by the vaccinated women. Most of the women received 2 shots of the COVID-19 vaccine.
The vaccinated women health baseline characteristics before and after COVID-19 vaccination
To assess the effects of the COVID-19 vaccines on women’s menstrual cycles, the surveyed women answered questions about their menstruation status before and after vaccination (Table 1). About 18% of the study participants had menstrual cycle irregularities before vaccination, whereas 52% reported post-vaccine menstrual irregularities. Of note, less than 20% of the participants were using contraceptives before and after vaccination (Table 1). The vaccinated women also reported any health issues they had that may affect menstruation. Results in Table 1 showed that 10.5% of vaccinated women had ovarian cysts, 3.2% had pelvic inflammatory disease, 3.7% had uterine fibroids, 8.3% had thyroid disorders, and only 2% had osteoporosis (Table 1).
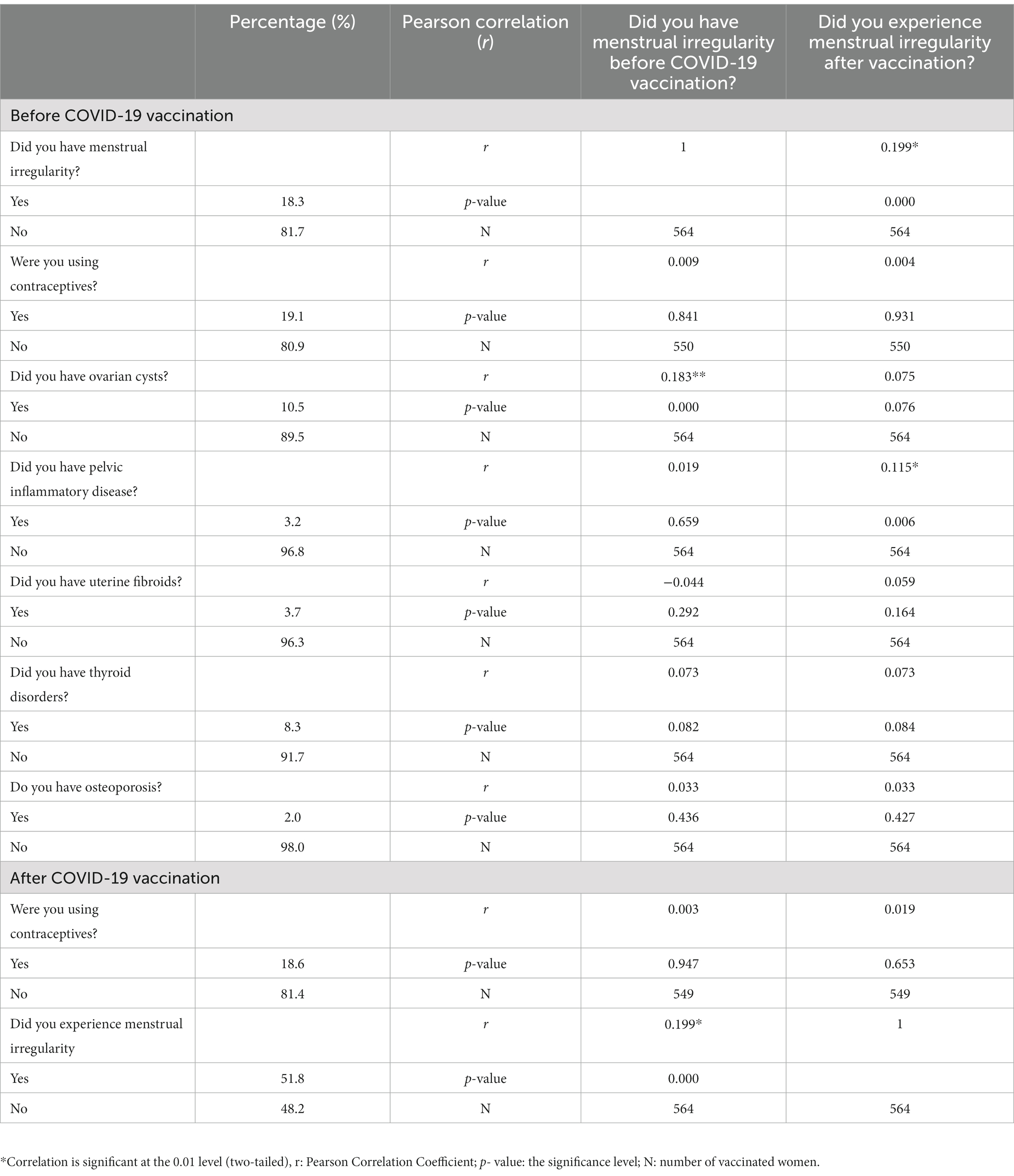
Table 1. The vaccinated women health baseline characteristics before and after COVID-19 vaccination.
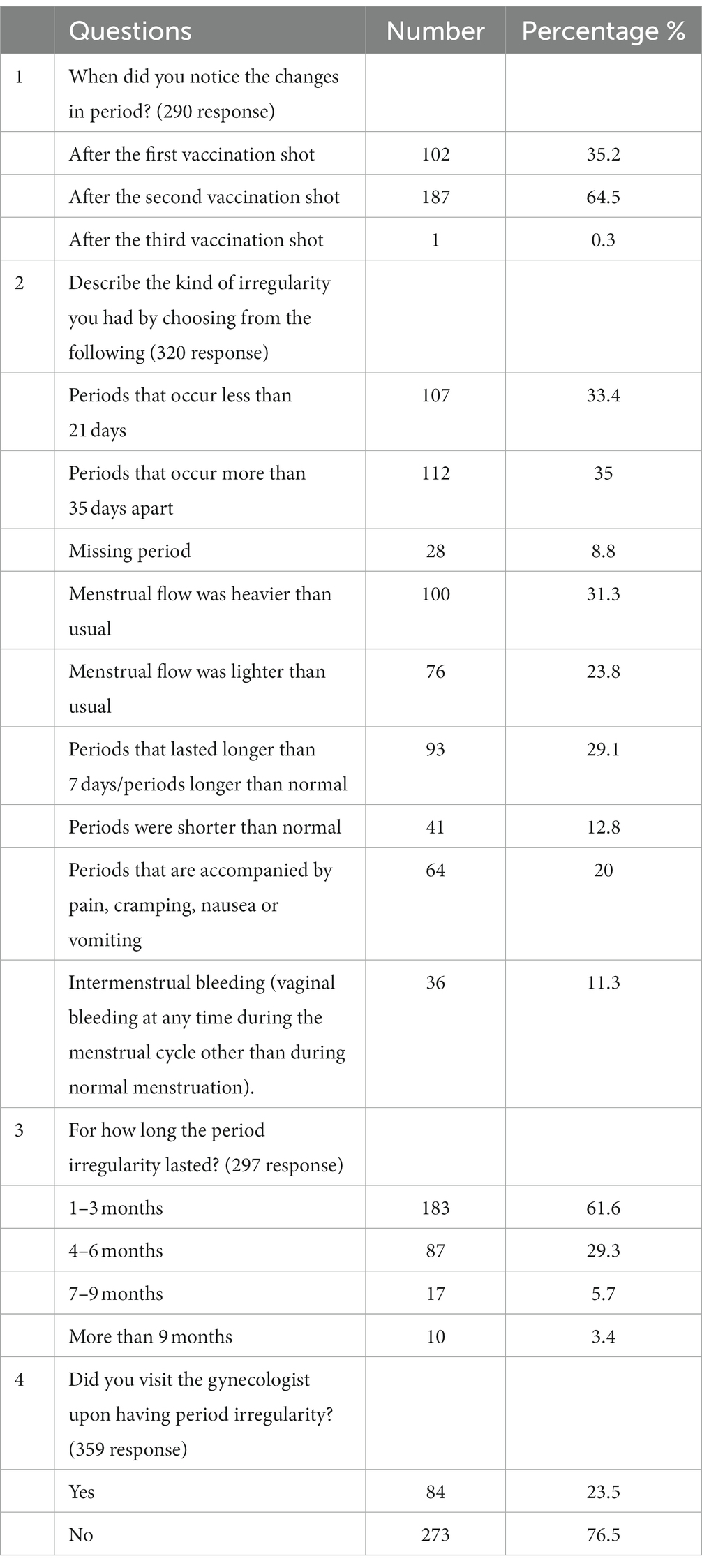
Menstrual cycle irregularity description
Most of the vaccinated women (65%) noticed menstrual irregularities after the second vaccine shot (Table 2). Women had distinct responses describing the nature of menstrual irregularities. About 33% of women reported shorter menstrual cycle than usual (less than 21 days), whereas 35% experienced longer menstruation than usual (more than 35 days). 8.8% of women missed at least one period. About 31% of women had heavier menstrual flow than normal, while 23.8% had it lighter. 29% of the vaccinated women had menstruation lasted longer than usual, but 12.8% had it shorter. 20% of women reported a menstruation accompanied with pain, cramping, and nausea or vomiting. About 11% had intermenstrual bleeding.
The duration of menstrual irregularities varied among the vaccinated women, results in Table 2 showed that more than 60% of women had menstrual irregularities lasted from 1 to 3 months, while 29% had it from 4 to 6 months. The menstrual irregularities were a concern for about 24% of the vaccinated women, which made them visiting the gynecologist in this regard (Table 2).
The COVID-19 vaccine’s effect on the menstrual cycle
To underscore the COVID-19 vaccine effect on menstruation, Pearson correlation analysis was performed to test for the correlation between the menstrual cycle irregularities pre and post vaccination. Results in Table 1 showed that the menstrual irregularities were significantly higher post-vaccination compared to pre-vaccination in women (r = 0.199; p < 0.001).
Since contraceptives affect the menstrual flow and regularity (34), their correlation with vaccination was assessed and revealed no significant correlation (r = 0.009, 0.003) respectively. Remarkably, none of the following health issues (uterine fibroids, thyroid disorders, and osteoporosis) showed a correlation with menstruation pre and post-vaccination (Table 1). Of note, a positive correlation was detected between having ovarian cysts and menstrual irregularities only before vaccination (r = 0.183). Whereas the pelvic inflammatory diseases showed a positive correlation only during the vaccination period but not before (r = 0.115).
The effect of the COVID-19 vaccine type on menstrual cycle
The effect of vaccine type on menstrual cycle was assessed. Results in Table 3 showed that 52.6, 51.5, 50.3, and 66.7% of women who received Pfizer–BioNTech, Oxford–AstraZeneca, Sinopharm BBIBP, and Moderna vaccine, respectively, experienced menstrual cycle irregularities during the vaccination period. Further analysis for a possible association between the type of vaccine and the menstrual irregularities using Chi-square test revealed no significant association (Table 3).
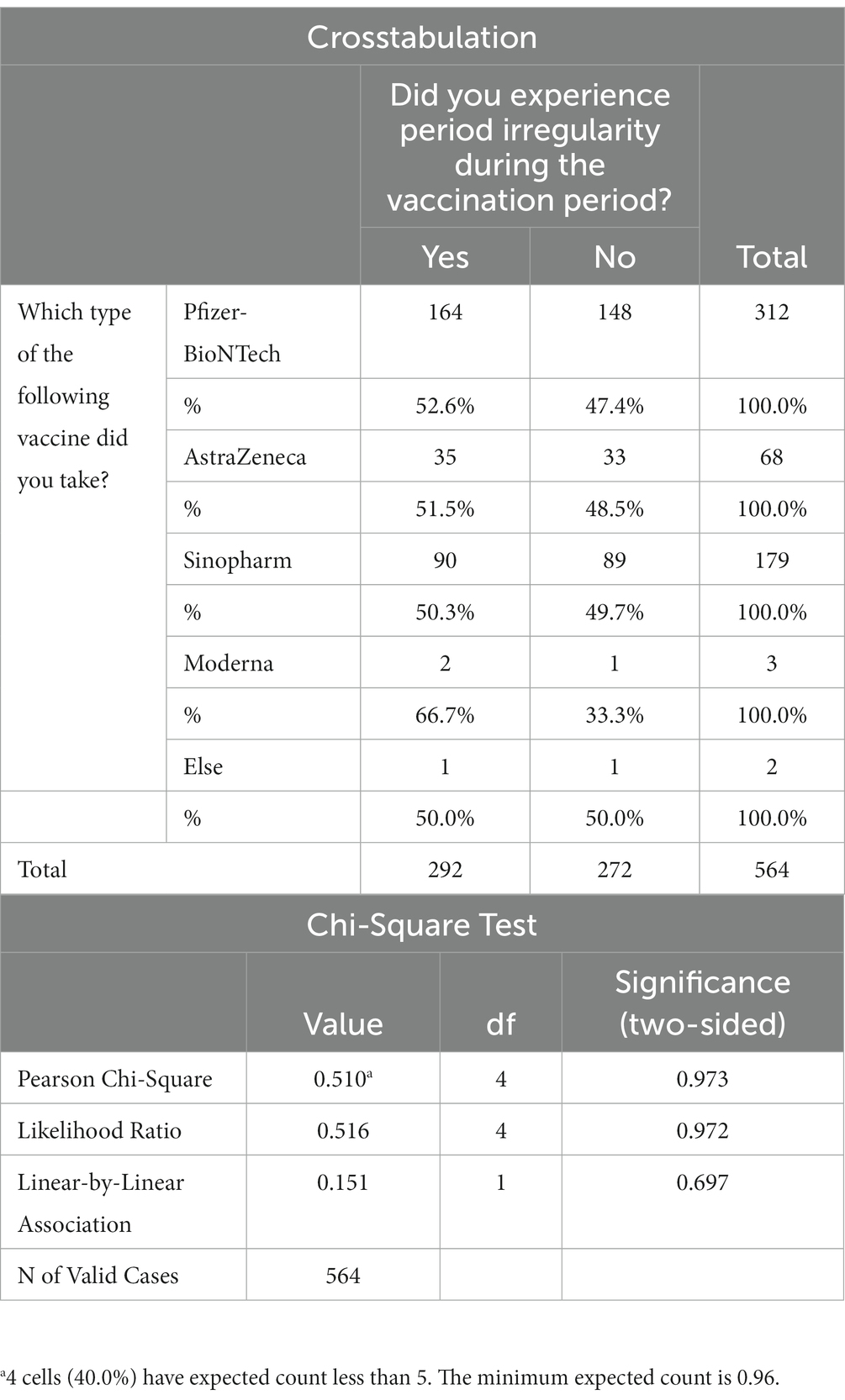
Table 3. The correlation analysis between the type of COVID-19 vaccine and the menstrual cycle during the vaccination period.
The effect of vaccine type on the duration of menstrual cycle
Results in Table 4 showed that about 30–34% of vaccines caused menstrual irregularities during the first 3 months of vaccination. The vaccine effect on menstruation declined with time (Table 4). Chi-squared test revealed a significant correlation between the vaccine type and menstrual irregularities duration (p-value = 0.004), indicating that Pfizer-BioNTech, AstraZeneca, and Sinopharm vaccines changed the regularity of the menstrual cycle from one to 3 months, whereas Moderna vaccine changed it from one to 6 months (Table 4).
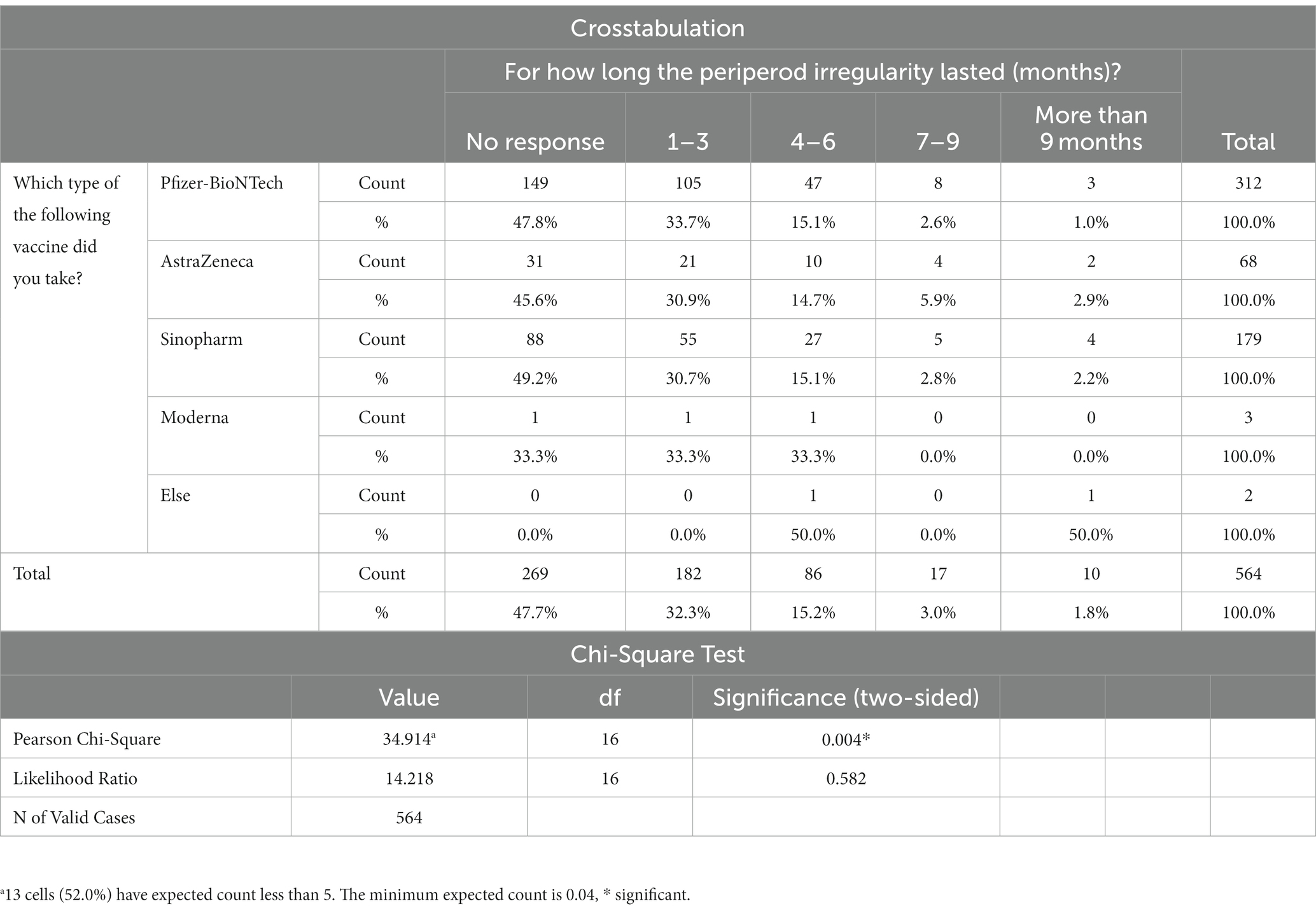
Table 4. The correlation analysis between the type of COVID-19 vaccine and the menstrual cycle duration.
Comparison with the VAERS data
Mining the VAERS database for “irregularity menstrual” in response to COVID-19 vaccines indicated that menstruation irregularity constituted 0.75% of all reported adverse events for the COVID-19 vaccines. Other menstrual cycle disturbances were annotated individually and were captured by the manual inspection of all reported adverse event symptoms. Remarkably, the manual search for menstruation-related adverse events such as “heavy menstrual bleeding,” “menstrual disorder” “dysmenorrhoea” (painful period), “intermenstrual bleeding” (bleeding during the menstruation), “amenorrhoea” (absence of menstruation) and “postmenopausal hemorrhage” showed the prevalence of 1.11%, 0.60, 0.52, 0.33, and 0.24%, respectively (Figure 3). Other menstrual cycle related symptoms such as “premenstrual syndrome,” “premenstrual pain,” “menstrual discomfort,” and “ovulation pain” were of lower frequency (i.e., < 0.10%) as shown in Figure 3. This indicates that the database did not really capture the magnanimity of the menstrual irregularities in vaccinated women.
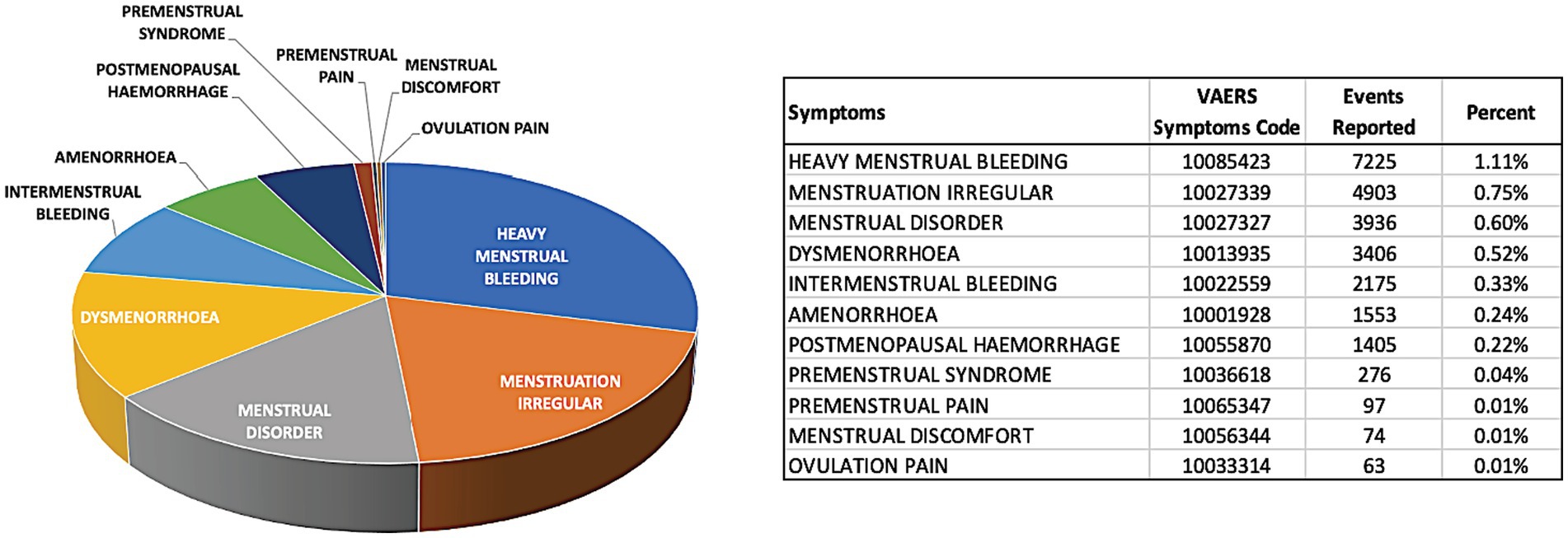
Figure 3. The most frequent menstrual adverse events reported in the VAERS database for COVID-19 vaccines. The pie chart represents visually the share of each of the adverse events related to menstruation-only adverse events. The summary table shows the exact number of reported adverse events and the percent from all adverse event reported for COVID-19 vaccines. VAERS reports processed as of 7th of September 2022 were considered.
Discussion
This study was designed to investigate the latest report about COVID-19 vaccine adverse effect on women’s menstruation. Anecdotal reports appeared in the UK Medicine and Healthcare Products Regulatory Agency (MHRA) which indicated that many women were experiencing post-vaccine changes in their menstrual cycles (20, 26). However, these changes were short-lived and are not expected to affect fertility in the vaccinated women (2, 20, 26).
Our results showed that 52% of the vaccinated women experienced post-vaccine menstrual irregularities compared to before. This result was in agreement with other cross-sectional studies, which reported that 50–66% of the vaccinated women experienced menstrual cycle irregularities (21, 26, 35).
Our results are in line with the previous studies showing that the menstrual cycle irregularities were independent of the vaccine type, confirming that all the COVID-19 vaccines may cause menstrual cycle irregularities (21, 26, 35).
About 65% of women in this study reported that the menstrual cycle irregularities were more often after the second vaccine shot. This is in agreement with the previous finding indicating that the menstrual cycle irregularities were slightly higher after the second dose (21). Suggesting additive effect of the vaccine on women. However, another publication reported that the menstrual cycle irregularities were mainly after the first vaccine shot (35). The difference in effect could be attributed to the type of vaccine (mRNA or adenovirus vaccines), or to the immune response of the vaccinated women (20).
Fortunately, the reported menstrual cycle irregularities did not last for a long period of time; most changes were observed and resolved within 3 months following full vaccination regimens. This result is in agreement with previous findings indicating that menstrual cycle changes occurred during the first 2 months after vaccination and totally resolved on their own after that (21, 26, 35).
Vaccinated women reported more than one form of menstrual cycle irregularities. Most of them had more frequent menstrual cycle, while another group reported less frequent menstrual cycle than usual. Additionally, a heavier menstruation than usual was also reported by the vaccinated women. A group of the vaccinated women claimed having menstruation that lasted longer than usual (more than 7 days). This is in agreement with other reports which showed that vaccinated women had longer menstruation with a heavier flow and a wider menstrual frequency than normal periods (21, 35). Taken together, women had distinct responses regarding the nature of the menstrual cycle irregularities, this could be attributed to the time when the woman received the vaccine, which could matches with different phases of woman’s menstrual cycle (follicular or luteal phase), hence the vaccine effect differ from woman to another (21, 26).
Finally, about 52% of the surveyed women claimed menstrual cycle irregularity amid the COVID-19 vaccination, about half of them visited the gynecologist upon having changes in menstruation. Comparing our results to the VAERS data that showed “menstruation irregular” adverse event in only 0.75%. We infer that the menstrual-related adverse events were under reported in the VAERS database for the COVID-19 vaccines compared to other vaccine-induced issues such as myocarditis and pericarditis (16). This could be attributed to many factors; Personal factors, few women tends to seek for medical help upon having problems in menstruation due to lack of awareness or carelessness (36). Social factors, women feel shy to report any health issues related to menstruation, mainly in the low-income and conservative countries (37), a study from Cambodia showed that many young females express fear, shyness, and discomfort during menstruation (37). In addition, there is a lack of studies about menstrual health research in the developing countries (38).
Additionally, such menstrual changes aren’t unique to COVID-19 vaccines; the human papillomavirus (HPV) vaccination was associated with menstrual irregularities (39). This indicates that immune response to viral infections, rather than the viral particle itself, is responsible for inducing this change. However, the exact mechanistic processes linking COVID-19 vaccines to menstrual cycle changes remain elusive. However, some studies tried to link these changes to the nature of the immune response to vaccination indicating some differences between women and women. One study indicated that women developed a higher antibody response and reported various adverse effects in response to COVID-19 vaccination compared to males (40). Other studies reported that COVID-19 vaccination may induce thrombocytopenia which could influence the women’s menstrual cycles (35, 41), leading to loss of endometrial hemostasis and causing heavy bleeding (42). Moreover, the vaccine could affect the production of the female sex hormones, which eventually affect the menstrual cycle stages (23, 43). It should be noted that menstrual cycle irregularities could be attributed to many other factors including viral infection itself (40, 44). In fact, bout 25% of the SARS-CoV-2 infected women had menstrual cycle irregularities upon the pandemic (23).
Strength and limitations
The strength of this research lies in the flow of the well-structured questionnaire that comprehensively covers the vaccinated women’s demographics, vaccine information, and menstrual cycle status. Additionally, timing of the study reduced the risks of recall bias by conducting the study right after the COVID-19 vaccination process was started in Jordan. This reduced the risk of obtaining inaccurate information provided by the vaccinated women. Furthermore, this study is one of the first studies in Jordan and in the Middle East that discussed menstrual cycle irregularities upon starting the COVID-19 vaccination campaigns. Taken together, the study outcomes enforced the previous findings in the biomedical literature regarding a possible link between COVID-19 vaccines and menstrual cycle changes (21, 26, 45).
However, our research had some limitations. One of the limitations was the women’s willingness to participate in the study and to share their private information regarding their periods, even though the women were informed at the beginning of the study that their information was confidential and the data were collected anonymously. As a result, the sample size was small but it exceeded the minimal statistically-acceptable sample size. This might have created a selection bias preventing the generalizability of the research results. However, this is not uncommon in cross-sectional studies which are often susceptible to the different types of bias according to the nature of the conducted cross-sectional studies. The information bias arises from the women’s knowledge about the different factors that may cause menstrual cycle irregularities including vaccines, and their updated medical records. Further, women’s emotions could be affected by the vaccination or the period changes. Fortunately, our study is free of potential bias since the vaccinated women were approached randomly, and their participation was not subjected to any benefits. Although the research team worked hard to cover all aspects of the research topic, some important information was not covered in the survey like COVID-19 infection information, and some details about menstrual cycle irregularities.
Implications for practice
The study results advocated the generalizability of the COVID-19 vaccine effect on women’s period regardless of vaccine type. Even though the vaccine effect is temporary, it may affect women’s daily activities and future pregnancy plans. Women need to be informed about the possible changes in the menstrual cycle upon vaccination. It is strongly recommended to investigate the causal effects of vaccines on women’s menstrual cycles at the molecular level. Further investigation on the mechanism of vaccine action on females’ and males’ reproductive systems is highly encouraged. We suggest to address the menstrual cycle irregularities with the COVID-19 vaccine’s possible side effects.
Conclusion
This study provides evidence that post-COVID-19-vaccine physiological adverse effects during the menstrual cycle were frequently observed in vaccinated women. Fortunately, all studied post-vaccine adverse events concerning menstrual cycle irregularities during menstruations were short-terms and subsided within 3 months on average. Therefore, these adverse events should not be a reason for vaccine hesitancy in young women based on these results.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study was approved by the Institutional Review Board (IRB) Committee of the Al-Zaytoonah University with no need for writing consent for women’s participation which was optional. Women were informed earlier that all their information are confidential and will be used only for research purposes.
Author contributions
EA: project administration, conceptualization, investigation, supervision, writing original draft, review, and editing. RH: idea and conceptualization, investigation, writing original draft, review, and editing. AQ: methodology, validation, and writing—review and editing. DS and AA-m: conceptualization, writing original draft, review, and editing. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors would like to thank all the vaccinated women who agreed to provide us with their private information regarding their menstruation and psychological symptoms.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1211283/full#supplementary-material
Footnotes
References
1. Sabbah, DA, Hajjo, R, Bardaweel, SK, and Zhong, HA. An updated review on SARS-CoV-2 main proteinase (MPro): protein structure and small-molecule inhibitors. Curr Top Med Chem. (2021) 21:442–60. doi: 10.2174/1568026620666201207095117
2. Hajjo, R, Sabbah, DA, and Tropsha, A. Analyzing the systems biology effects of COVID-19 mRNA vaccines to assess their safety and putative side effects. Pathogens. (2022) 11:743. doi: 10.3390/pathogens11070743
3. Bok, K, Sitar, S, Graham, BS, and Mascola, JR. Accelerated COVID-19 vaccine development: milestones, lessons, and prospects. Immunity. (2021) 54:1636–51. doi: 10.1016/j.immuni.2021.07.017
4. Pascual-Iglesias, A, Canton, J, Ortega-Prieto, AM, Jimenez-Guardeño, JM, and Regla-Nava, JA. An overview of vaccines against SARS-CoV-2 in the COVID-19 pandemic era. Pathogens. (2021) 10:1030. doi: 10.3390/pathogens10081030
5. Chung, JY, Thone, MN, and Kwon, YJ. COVID-19 vaccines: the status and perspectives in delivery points of view. Adv Drug Deliv Rev. (2021) 170:1–25. doi: 10.1016/j.addr.2020.12.011
6. Francis, AI, Ghany, S, Gilkes, T, and Umakanthan, S. Review of COVID-19 vaccine subtypes, efficacy and geographical distributions. Postgraduate Med J. (2022) 98:389–94. doi: 10.1136/postgradmedj-2021-140654
7. Al-Qerem, WA, and Jarab, AS. COVID-19 vaccination acceptance and its associated factors among a middle eastern population. Front Public Health. (2021) 9:632914. doi: 10.3389/fpubh.2021.632914
8. Almomani, EY, Qablan, AM, Atrooz, FY, Almomany, AM, Hajjo, RM, and Almomani, HY. The influence of coronavirus diseases 2019 (COVID-19) pandemic and the quarantine practices on university students’ beliefs about the online learning experience in Jordan. Front Public Health. (2021) 8:595874. doi: 10.3389/fpubh.2020.595874
9. Baden, LR, El Sahly, HM, Essink, B, Kotloff, K, Frey, S, Novak, R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. (2021) 384:403–16. doi: 10.1056/NEJMoa2035389
10. Lee, GM. The importance of context in COVID-19 vaccine safety. N Engl J Med. (2021) 385:1138–40. doi: 10.1056/NEJMe2112543
11. Oliver, SE, Gargano, JW, Marin, M, Wallace, M, Curran, KG, Chamberland, M, et al. The advisory committee on immunization practices’ interim recommendation for use of Pfizer-BioNTech COVID-19 vaccine - United States, December 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:1922–4. doi: 10.15585/mmwr.mm6950e2
12. Chu, L, McPhee, R, Huang, W, Bennett, H, Pajon, R, Nestorova, B, et al. A preliminary report of a randomized controlled phase 2 trial of the safety and immunogenicity of mRNA-1273 SARS-CoV-2 vaccine. Vaccine. (2021) 39:2791–9. doi: 10.1016/j.vaccine.2021.02.007
13. Macneil, JR. Updated recommendations from the advisory committee on immunization practices for use of the Janssen (Johnson & Johnson) COVID-19 vaccine after reports of thrombosis with thrombocytopenia syndrome among vaccine recipients — United States, 2021. MMWR Morb Mortal Wkly Rep. (2021) 70:651–656. doi: 10.15585/mmwr.mm7017e4
14. Meo, AS, Masood, A, Shabbir, U, Ali, H, Nadeem, Z, Meo, SA, et al. Adverse effects of sinopharm COVID-19 vaccine among vaccinated medical students and health care workers. Vaccines. (2023) 11:105. doi: 10.3390/vaccines11010105
15. Cari, L, Alhosseini, MN, Fiore, P, Pierno, S, Pacor, S, Bergamo, A, et al. Cardiovascular, neurological, and pulmonary events following vaccination with the BNT162b2, ChAdOx1 nCoV-19, and Ad26.COV2.S vaccines: an analysis of European data. J Autoimmun. (2021) 125:102742. doi: 10.1016/j.jaut.2021.102742
16. Hajjo, R, Sabbah, DA, Bardaweel, SK, and Tropsha, A. Shedding the light on post-vaccine myocarditis and pericarditis in COVID-19 and non-COVID-19 vaccine recipients. Vaccines. (2021) 9:1186. doi: 10.3390/vaccines9101186
17. Abou Hassan, OK, Sheng, CC, Wang, TKM, and Cremer, PC. SARS-CoV-2 myocarditis: insights into incidence, prognosis, and therapeutic implications. Curr Cardiol Rep. (2021) 23:129. doi: 10.1007/s11886-021-01551-x
18. Bautista García, J, Peña Ortega, P, Bonilla Fernández, JA, Cárdenes León, A, Ramírez Burgos, L, and Caballero, DE. Acute myocarditis after administration of the BNT162b2 vaccine against COVID-19. Rev Esp Cardiol. (2021) 74:812–4. doi: 10.1016/j.recesp.2021.03.009
19. Soraci, L, Lattanzio, F, Soraci, G, Gambuzza, ME, Pulvirenti, C, Cozza, A, et al. COVID-19 vaccines: current and future perspectives. Vaccine. (2022) 10:608. doi: 10.3390/vaccines10040608
20. GOV.UK. Medicines and healthcare products regulatory agency. (2022). Available at: https://www.gov.uk/government/organisations/medicines-and-healthcare-products-regulatory-agency
21. Laganà, AS, Veronesi, G, Ghezzi, F, Ferrario, MM, Cromi, A, Bizzarri, M, et al. Evaluation of menstrual irregularities after COVID-19 vaccination: results of the MECOVAC survey. Open Med. (2022) 17:475–84. doi: 10.1515/med-2022-0452
22. Edelman, A, Boniface, ER, Benhar, E, Han, L, Matteson, KA, Favaro, C, et al. Association between menstrual cycle length and coronavirus disease 2019 (COVID-19) vaccination: a U.S. Cohort Obstet Gynecol. (2022) 139:481–9. doi: 10.1097/AOG.0000000000004695
23. Li, K, Chen, G, Hou, H, Liao, Q, Chen, J, Bai, H, et al. Analysis of sex hormones and menstruation in COVID-19 women of child-bearing age. Reprod Biomed. (2021) 42:260–7. doi: 10.1016/j.rbmo.2020.09.020
24. Demir, O, Sal, H, and Comba, C. Triangle of COVID, anxiety and menstrual cycle. J Obstetr Gynaecol. (2021) 41:1257–61. doi: 10.1080/01443615.2021.1907562
25. Jing, Y, Run-Qian, L, Hao-Ran, W, Hao-Ran, C, Ya-Bin, L, Yang, G, et al. Potential influence of COVID-19/ACE2 on the female reproductive system. Mol Hum Reprod. (2020):26:367–73. doi: 10.1093/molehr/gaaa030
26. Male, V. Menstrual changes after covid-19 vaccination. BMJ. (2021) 374:n2211. doi: 10.1136/bmj.n2211
28. Kurdoğlu, Z. Do the COVID-19 vaccines cause menstrual irregularities? Int J Women’s Health Reprod Sci. (2021) 9:158–9. doi: 10.15296/ijwhr.2021.29
29. Prado, RCR, Silveira, R, and Asano, RY. SARS-CoV-2 (COVID-19) pandemic and a possible impact in the future of menstrual cycle research. Health Sci Rep. (2021) 4:e276:e276. doi: 10.1002/hsr2.276
30. Phelan, N, Behan, LA, and Owens, L. The impact of the COVID-19 pandemic on women’s reproductive health. Front Endocrinol. (2021) 12:642755. doi: 10.3389/fendo.2021.642755
31. von Elm, E, Altman, DG, Egger, M, Pocock, SJ, Gøtzsche, PC, and Vandenbroucke, JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. (2007) 335:806–8. doi: 10.1136/bmj.39335.541782
32. Sperber, A, DeVellis, R, and Boehlecke, B. Cross-cultural translation. J Cross-Cult Psychol. (1994) 25:501–24. doi: 10.1177/0022022194254006
33. Vaccine Adverse Event Reporting System (VAERS) (2022). Available at: https://vaers.hhs.gov/
34. Stubblefield, PG. Menstrual impact of contraception. Am J Obstetr Gynecol. (1994) 170:1513–22. doi: 10.1016/S0002-9378(94)05013-1
35. Muhaidat, N, Alshrouf, MA, Azzam, MI, Karam, AM, Al-Nazer, MW, and Al-Ani, A. Menstrual symptoms after COVID-19 vaccine: a cross-sectional investigation in the MENA region. IJWH. (2022) 14:395–404. doi: 10.2147/IJWH.S352167
36. White, PA, and Wildman, BG. Factors related to medical help-seeking in women with menstrual discomfort. Behav Res Ther. (1986) 24:471–4. doi: 10.1016/0005-7967(86)90012-4
37. Daniels, G, MacLeod, M, Cantwell, RE, Keene, D, and Humprhies, D. Navigating fear, shyness, and discomfort during menstruation in Cambodia. PLoS Global Public Health. (2022) 2:e0000405. doi: 10.1371/journal.pgph.0000405
38. Hennegan, J, Shannon, AK, Rubli, J, Schwab, KJ, and Melendez-Torres, GJ. Women’s and girls’ experiences of menstruation in low- and middle-income countries: a systematic review and qualitative metasynthesis. PLoS Med. (2019) 16:e1002803. doi: 10.1371/journal.pmed.1002803
39. Suzuki, S, and Hosono, A. No association between HPV vaccine and reported post-vaccination symptoms in Japanese young women: results of the Nagoya study. Papillomavirus Res. (2018) 5:96–103. doi: 10.1016/j.pvr.2018.02.002
40. Flanagan, KL, Fink, AL, Plebanski, M, and Klein, SL. Sex and gender differences in the outcomes of vaccination over the life course. Annu Rev Cell Dev Biol. (2017) 33:577–99. doi: 10.1146/annurev-cellbio-100616-060718
42. Saleem, A, Javed, SO, and Malik, F. COVID-19 vaccine related menstrual irregularities: a cause of vaccine hesitation? J Pak Med Assoc. (2022) 72:1683–4. doi: 10.47391/JPMA.5415
43. Karagiannis, A, and Harsoulis, F. Gonadal dysfunction in systemic diseases. Eur J Endocrinol. (2005) 152:501–13. doi: 10.1530/eje.1.01886
44. Saxena, R, Basavaraju, M, and Meghana, T. Effect of COVID-19 infection on menstruation: a retrospective study. J South Asian Federation Obstetr Gynaecol. (2022) 14:161–5. doi: 10.5005/jp-journals-10006-2025
Keywords: COVID-19 vaccine, adverse events, menstrual cycle irregularity, vaccinated women, Jordan
Citation: Almomani EY, Hajjo R, Qablan A, Sabbah DA and Al-Momany A (2023) A cross-sectional study confirms temporary post-COVID-19 vaccine menstrual irregularity and the associated physiological changes among vaccinated women in Jordan. Front. Med. 10:1211283. doi: 10.3389/fmed.2023.1211283
Edited by:
Gerardo Cazzato, University of Bari Aldo Moro, ItalyReviewed by:
Astawus Alemayehu, Harar Health Science College (HHSC), EthiopiaLuca Soraci, Unit of Geriatric Medicine, IRCCS INRCA, Italy
Copyright © 2023 Almomani, Hajjo, Qablan, Sabbah and Al-Momany. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ensaf Y. Almomani, ZW5zYWYubW9tYW5pQGJhdS5lZHUuam8=; Rima Hajjo, ci5oYWpqb0B6dWouZWR1Lmpv
†ORCID: Ensaf Y. Almomani, https://orcid.org/0000-0002-1032-627X
Rima Hajjo, https://orcid.org/0000-0002-7090-5425
 Ensaf Y. Almomani
Ensaf Y. Almomani Rima Hajjo
Rima Hajjo Ahmad Qablan6,7
Ahmad Qablan6,7 Dima A. Sabbah
Dima A. Sabbah Abass Al-Momany
Abass Al-Momany