
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 05 September 2023
Sec. Pulmonary Medicine
Volume 10 - 2023 | https://doi.org/10.3389/fmed.2023.1206419
 Po-Chang Chiang1†
Po-Chang Chiang1† Chia-Ying Lin1†
Chia-Ying Lin1† Ya-Chun Hsu1
Ya-Chun Hsu1 Li-Ting Huang1
Li-Ting Huang1 Ta-Jung Chung1
Ta-Jung Chung1 Yi-Sheng Liu1
Yi-Sheng Liu1 Chao-Chun Chang2*
Chao-Chun Chang2*Background: Although percutaneous transthoracic catheter drainage (PCD) has been proven effective in lung abscesses, the optimal timing of PCD is still unclear. The study aimed to evaluate the safety and efficacy of early versus delayed drainage in patients with lung abscesses.
Methods: This retrospective study included 103 consecutive patients with liquefied lung abscesses more than 3 cm confirmed by a CT scan received CT-guided PCD over 16 years, from July 2005 to September 2021, in a single institution were reviewed. Early drainage was defined as PCD within one week after a lung abscess was diagnosed. The primary outcome was 90-day mortality. The secondary outcomes included perioperative complications and patients’ length of hospital stay (LoS). Factors associated with 90-day mortality and LoS were also analyzed. The key statistical methods were Chi-square test, Fisher’s exact test, Student t-test, and Pearson correlation.
Results: Amount the 103 patients, there were 64 patients who received early PCD, and 39 patients received delayed PCD. Between the two groups, there were no significant differences in clinical characteristics, 90-day mortality, or perioperative complications. The LoS was significantly shortened in early PCD group (28.6 ± 25.5 vs. 39.3 ± 26.8 (days), p = 0.045). Higher Charlson comorbidity index, secondary lung abscess, and liver cirrhosis were associated with higher mortality (all p < 0.05). Positive sputum culture significantly increased the LoS (coefficient 19.35 (10.19, 28.50), p < 0.001).
Conclusion: The 90-day mortality and complications were similar for early PCD and delayed PCD patients, but LoS was significantly shortened in early PCD patient.
Lung abscess was once a life-threatening disease, with a mortality rate of up to 75% (1). The outcomes of lung abscesses have improved over past decades due to timely diagnosis, effective antimicrobial therapy, application of drainage, or surgery. Currently, about 80%–90% of pyogenic lung abscesses are treated successfully with antibiotics. However, 10%–20% of patients with lung abscesses need invasive treatment, such as surgical intervention or percutaneous transthoracic catheter drainage (PCD), due to conservative treatment failure. In the past, PCD for lung abscesses was usually reserved for patients who fail to improve after antibiotic treatment (2–7). Because of the concerns about major complications, such as bronchopleural fistula (BPF), pneumothorax, hemoptysis, and empyema (8). With technological improvement, image-guided PCD is considered less invasive and safer than surgical intervention (9, 10). It can also bridge the gap between medical and operative management (11). The role of early PCD remains unclear. Current evidence, comprising a single or a few case series, show a high success rate without major complication or mortality in early PCD with concurrent antibiotics (12–14). Given the paucity of data in this field, we aim to compare the safety and efficacy of early versus delayed drainage in patients with lung abscesses. We hypothesize that early PCD results in better outcomes compared with delayed PCD.
This retrospective study was approved by the Institutional Review Board of the National Cheng Kung University Hospital (A-ER-111-325), and informed consent was waived. Between July 2005 and September 2021, all patients who underwent CT-guided PCD for lung abscesses at National Cheng Kung University were reviewed. The diagnosis of lung abscess was based on CT imaging findings and clinical presentation. Criteria for CT-guided drainage included liquefied abscess greater than 3 cm (Figure 1) with ongoing sepsis. Exclusion criteria included incomplete clinical or radiological data.
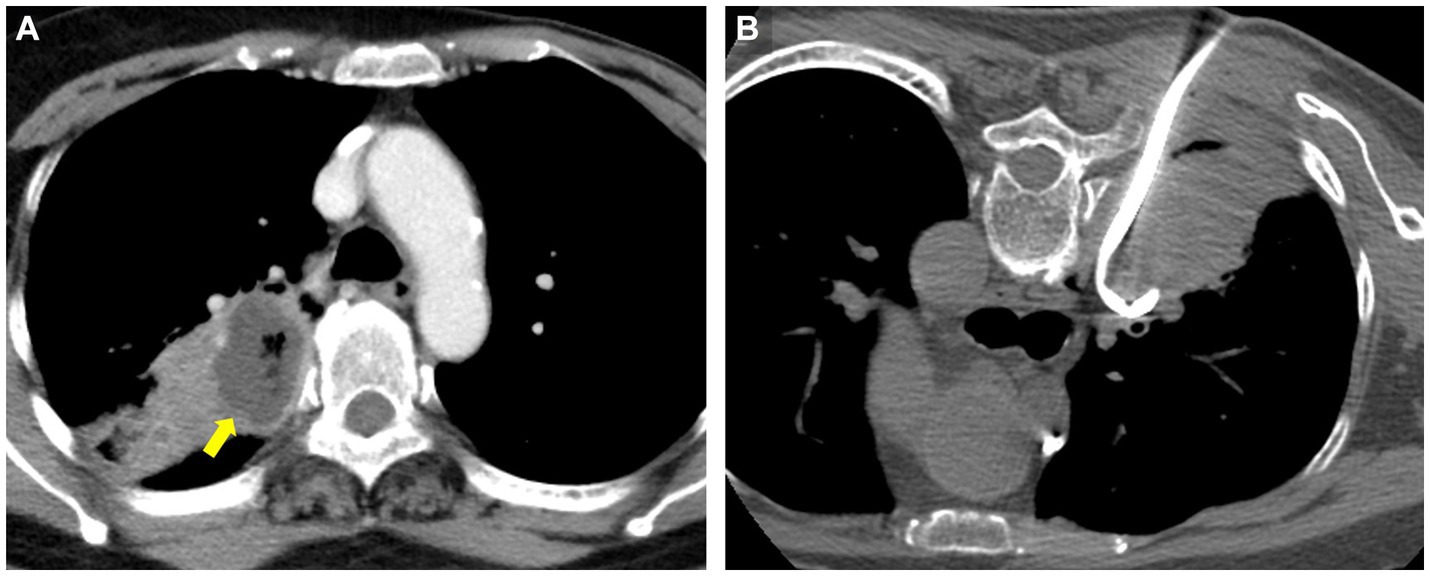
Figure 1. Representative contrast-enhanced CT (CECT) images with liquefied lung abscess in a 69 years-old woman who presented with fever and cough for 2 weeks. (A) CECT shows a 3.7 cm low-attenuation necrotic region (arrow) with gas formation. (B) CT-guided PCD was performed after CECT at the same day.
Age, sex, size of the abscess, white blood cell (WBC) count, C-reactive protein (CRP), cause of lung abscesses, Charlson comorbidity index, underlying diseases or malignancy, presence of preprocedural emphysema or pulmonary embolism, duration of pre-drainage antibiotics, the size of the drainage tube, whether trans-aerated lung parenchyma or not, drainage tube indwelling time, microbiological results, rationales of antibiotic use, subsequent surgery were recorded. The abscess size was determined by measuring the maximum diameter of the largest abscess identified. The duration of pre-drainage antibiotics was defined as the time interval between the first dose of intravenous antibiotics and the day of CT-guided PCD. There were primary and secondary causes of lung abscesses. Primary abscesses were infectious in origin, caused by aspiration or pneumonia in the healthy host. Secondary abscesses were caused by a preexisting condition (e.g., obstruction), spread from an extrapulmonary site, or bronchiectasis. The rationales for antibiotic use included empirical and culture-based. The subsequent surgery included lung resection and decortication.
Early PCDs were defined as PCDs performed within 1 week (≦7 days) after a lung abscess was diagnosed. Delayed PCDs meant PCDs were performed more than 1 week (>7 days) after a lung abscess was diagnosed. In general, PCDs were kept in place for at least 2 weeks before removal. If there were persistent air leaks from the drainage tube, the drainage tube was kept in place for 3 weeks to form a bronchopleurocutaneous fistula. The wound was compressed by sterile gauze after drainage tube removal. Reasons for drainage removal included recovery, dislodgement, subsequent surgery, or death.
The drainage procedures were performed by a total of 19 board-certificated radiologists during the study period, with or without assistance from a resident. Drainage was performed using standard sterile technique with CT guidance (Optima 660, General Electric) using the Seldinger technique and local anesthesia. The size of the catheter and the route of placement were determined based on the cavity size and clinical experience of the attending radiologists. The abscess contents were aspirated, and the pus was sent for microbiologic culture. In general, empiric antibiotics were prescribed before PCD, and specific antibiotics were given once the culture results were available. Post-procedure imaging was performed to ensure the proper positioning of the drainage catheter. Abnormal coagulation profiles, including INR above 1.5 or platelets below 50,000/mL, were corrected before the procedure. If there were pre-procedure empyema, another pleural drainage tube was inserted.
The primary outcome was postoperative mortality within 90 days. Secondary outcomes included perioperative complications and patients’ length of hospital stay (LoS). Perioperative complications included BPF, empyema, hemoptysis, and pneumothorax.
Patient demographics and lesion characteristics were summarized using descriptive statistics (mean ± standard deviation for continuous variables and proportions for categorical variables). Differences between categorical and continuous variables between the two groups were compared using the chi-square test or Fisher’s exact test and student t-test, respectively. Correlations between continuous variables were analyzed using Pearson correlation. A p < 0.05 was set to indicate statistical significance. SPSS system (IBM SPSS Statistics, Version 22.0, Armonk, NY) was used for statistical analysis.
The study flowchart is presented in Figure 2. Among 109 patients who received PCD between July 2005 and September 2021, 6 were excluded due to missing clinical or radiographic data. The final study consisted of 103 patients: 64 received early PCD (mean age 59.2 years ±20.7), and 39 received delayed PCD (mean age 65.3 years ±14.6). Demographic characteristics are summarized in Table 1 and detailed in Supplementary Table S1. The patient demographics and clinical characteristics, including age, sex, size of the abscess, WBC, CRP, cause, Charlson comorbidity index, underlying disease, pre-procedure empyema, pulmonary embolism, drainage tube size, the distance of trans-aerated lung parenchyma, drainage tube indwelling time, culture positivity, the rationale of antibiotics use, were similar between the two groups. The overall positivity rates were 77.7% (80/103) from abscess culture, 45.6% (47/103) from sputum culture, and 3.9% (4/103) from blood culture. A total of 15 patients received subsequent surgery after PCD treatment failure, including 6 lung resections, 6 decortications, and 3 with both lung resection and decortication.
The primary and secondary outcomes are presented in Table 2. There was no significant difference in 90 days mortality between the two groups [early PCD group: 11 of 64 patients (17.2%), delayed PCD group: 10 of 39 patients (25.6%); p = 0.302]. The total complication was 8.7% (9/103). The two groups had a similar complication rate, included BPF [early PCD group: 1 of 64 patients (1.6%), delayed PCD group: 0 of 39 patients (0%); p = 1], empyema [early PCD group: 1 of 64 patients (1.6%), delayed PCD group: 3 of 39 patients (7.7%); p = 0.151], hemoptysis [early PCD group: 1 of 64 patients (1.6%), delayed PCD group: 0 of 39 patients (0%); p = 1], and pneumothorax [early PCD group: 2 of 64 patients (3.1%), delayed PCD group: 1 of 39 patients (2.6%); p = 0.1]. Patients with post-PCD empyema and pneumothorax were treated with another drainage tube, except one patient who underwent lung resection due to persistent BPF. The LoS was significantly shortened in the early PCD group (28.6 ± 25.5 vs. 39.3 ± 26.8 days, p = 0.045).
Demographic characteristics and factors associated with 90 days mortality are summarized in Supplementary Table S2. Among 103 patients who received PCD for lung abscesses more than 3 cm in diameter, 82 (79.6%) recovered, and 21 (20.4%) had 90 days mortality. These two groups were similar in age, sex, and tube size. The 90 days mortality rate significantly increased with higher Charlson scores (7.8 ± 3.4 vs. 5.4 ± 3.2 in death and recovery group respectively, p = 0.006), secondary lung abscess (34.7% vs. 7.4% p = 0.001), and liver cirrhosis (50.0% vs. 17.2%, p = 0.014). The drainage duration (18.9 ± 29.6 vs.16.3 ± 12.9 days in recovery and death group respectively, p = 0.541), LoS (31.8 ± 27.4 vs. 35.8 ± 22.3 days in recovery and death group respectively, p = 0.497), complications (including BPF, empyema, hemoptysis, or pneumothorax), rationales of antibiotic use were similar between the two groups. There was a similar recovery rate between patients treated with empirical antibiotics and those treated with culture-based antibiotics (75.0% vs. 80.5%, respectively, p = 0.736).
Possible factors for the LoS are shown in Table 3. There was no significant difference in age, sex, and cause of lung abscess (primary or secondary). The patients with esophageal cancer (48.9 ± 42.8 vs. 30.7 ± 23.3 days respectively, p = 0.03), liver cirrhosis (48.8 ± 35.8 vs. 30.9 ± 24.8 days respectively, p = 0.041), longer duration of pre-drainage antibiotics (p < 0.001), positive sputum culture group (44.7 ± 33.4 vs. 22.5 ± 11.3 days respectively, p < 0.001), underwent subsequent surgery (50.9 ± 48.8 vs. 29.5 ± 19.1 days respectively, p = 0.003) had significant longer LoS. A mixed-effect model for the LoS is presented in Table 4. Early PCD significantly reduced the LoS in patients with lung abscesses [coefficient −10.52 (−19.69, −1.34), p = 0.025]. Positive sputum culture significantly increased the LoS [coefficient 19.35 (10.19, 28.50), p < 0.001].
Our results show that early PCD has a similar 90 days mortality and complication rate, but shorter LoS compared with delayed PCD. Our study’s overall recovery rate of patients who received PCD was 79.6%. Prior systemic review studies showed that malignancy-related abscesses and the occurrence of major complications were predictors of treatment failure (10). Our study had a similar finding: patients with secondary lung abscesses had a lower recovery rate than patients with primary lung abscesses (65.3% vs. 92.6%), which may relate to underlying disease. Besides, liver cirrhosis is associated with an increased mortality rate and prolonged LoS. Our drainage tubes ranged from 8 to 12 Fr., averaging 10 Fr.. There was no statistically significant difference between tube size and LoS (p = 0.221), possibly due to the small difference in tube diameter.
Although the traditional dogma that PCD for lung abscess was reserved for patients unresponsive to medical treatment, there is a paucity of data specifically comparing the timing of PCD and the outcome. Recent systematic review and meta-analysis showed no difference in outcomes or major complications between pre-PCD antibiotics in groups of more than 14 days and less than 14 days (10). Literature review of prior studies about PCD for lung abscess is summarized in Table 5. The drainage duration was longer in our study, which could be explained by our drainage management strategy. Prolonged drainage tube placement leads to adjacent pleural adhesions, thus lower the incidence of empyema or persistent BPF. Our study is the largest to date and is concordant with previous smaller studies that found that early PCD provides an equivalent outcome to delayed PCD.
Our relatively low overall complication rate of 8.7% in both groups may be explained by our procedure technique and imaging guidance method. We use the Seldinger method instead of the Trocar technique, and the procedure is performed using CT guidance. The Seldinger technique is considered safer because the puncture is made with a small-caliber needle, and thus the risk of adjacent structure injury in erroneous puncture is reduced. In addition, CT-guided puncture allows the clear visualization of the thorax during the procedure, free from overshadowing, compared with ultrasound guidance (24). A prior study suggested that traversal of normal lung parenchyma was a risk factor for complications like pneumothorax or hemothorax (10), but we could not confirm this in our study cohort.
Adequate adhesion around the abscess and drainage tube promotes spontaneous healing of bronchopleural fistula (BPF) without surgical intervention. Persistent BPF is the most dangerous and lethal complication of PCD. The treatment for BPF is difficult; surgical or bronchoscopic interventions was often required (25). In our studies, the majority of BPFs are sealed by early drainage and anti-infective treatment. Two reasons may explain our relatively low persistent BPF rate. First, in cases of empyema adjacent to an abscess, early placement of a pleural drainage tube is actively pursued to minimize the residual pleural space (26), and adequate adhesion around the abscess and drainage tube promotes the formation of a bronchopleurocutaneous fistula after 2 weeks of catheter placement and spontaneous healing of BPF without surgical intervention. Besides, the average size of the catheter was 10 Fr., which is smaller than the large bore chest tube. However, in a particular case with prolonged ventilator use, persistent severe air leakage under positive pressure breathing prevented effective adhesion in the surrounding costal cavity. Consequently, the patient necessitated a lobectomy to seal the BPF effectively.
Our patients received pre-drainage antibiotics with a mean duration of 7.9 ± 8.7 days. There is a tendency for patients in the recovery groups to have a lesser duration of pre-drainage antibiotics compared with the mortality group. Besides, the duration of pre-drainage antibiotics correlates with the LoS. Early PCD is beneficial for antibiotic stewardship. Our studies show that the positive rate of sputum culture was 45.6%, and blood culture was 3.9%. On the contrary, the positive rate from abscess culture is 77.7%. Although our results show similar mortality in patients who receive culture-based antibiotics and continued empirical broad-spectrum antibiotics, earlier pathogen detection allows antibiotics to be optimized. De-escalation of antibiotics can be performed earlier if a responsible pathogen is identified to avoid drug resistance.
The patients who received subsequent surgery have a comparable recovery rate to the overall recovery rate. Surgical treatment still plays an important role in lung abscesses. Of note, these patients are often operated on by open thoracotomy due to severe adhesion and unstable vital signs. The disadvantages of surgery include reduction of lung functional reserve after lung resection and intraoperative bleeding. Besides, residual dirty pleural space may be an infectious focus, and prolonged postoperative ventilator support may increase the risk of BPF (1, 27). Our results show that the timing of PCD placement (early vs. delayed) does not affect the risk of subsequent lung resection or decortication, nor influence the mortality rate. We suggest that for a lung abscess larger than 3 cm at initial diagnostic CT confirmed by radiological examination, the patient should receive early PCD to shorten recovery time.
Our surgical group utilizes both traditional thoracotomy and video-assisted thoracoscopic surgery (VATS). In our review of 15 surgical cases, 10 underwent VATS while 5 underwent open surgery. Thoracoscopy was introduced in our hospital in 2008. As VATS techniques matured, most surgeries gradually transitioned to VATS. The majority of VATS procedures involved mini-thoracotomy, which still required rib incision and the use of a rib spreader. True “complete” VATS remained relatively uncommon. In cases where patient condition was unstable, operators aimed to minimize operation time, but adhesive and undesirable lung deflation significantly prolonged the VATS completion time.
Our study has limitations. First, patients are not randomized to the early PCD and delayed PCD groups. The clinical physician made the decision on the timing of PCD insertion, which could lead to selection bias. However, the two groups have no significant difference in basic demographics or clinical characteristics. Second, this was a single-center retrospective study with a limited case number. However, it is the largest study to date. Third, our study does not compare with other treatment methods, such as direct surgery or medical treatment alone. However, medical treatment alone was less likely to cure lung abscesses more than 4 cm in diameter (15, 17). Fourth, our study had a long study period, the clinical management strategies might be different among physicians.
In conclusion, this cohort study demonstrates that early PCD within 1 week of diagnosis is associated with a shorter LoS for patients with liquefied lung abscesses larger than 3 cm. The 90 days mortality and complications were comparable between the early PCD and delayed PCD groups. These findings suggest the importance of emphasizing early drainage for lung abscesses exceeding 3 cm in clinical care paradigms and treatment guidelines.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by National Cheng Kung University Hospital Institutional Review Board. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
P-CC and C-CC have full access to all the data in the study and take responsibility for the content of the manuscript. C-YL conceived and designed the study. P-CC, C-YL, and C-CC integrated data, analyzed the data, and wrote the manuscript. C-CC provided methodological and statistical support. C-YL and C-CC participated in editing of the manuscript. Y-CH, L-TH, T-JC, and Y-SL contributed to investigation and clinical inputs. All authors contributed to the article and approved the submitted version.
This work is funded by the National Cheng Kung University Hospital of Taiwan (NCKUH-11201007 and NCKUH-11203049) and the Ministry of Science and Technology of Taiwan (MOST 111-2314-B-006-106).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1206419/full#supplementary-material
1. Schweigert, M, Dubecz, A, Stadlhuber, RJ, and Stein, HJ. Modern history of surgical management of lung abscess: from Harold Neuhof to current concepts. Ann Thorac Surg. (2011) 92:2293–7. doi: 10.1016/j.athoracsur.2011.09.035
2. Kuhajda, I, Zarogoulidis, K, Tsirgogianni, K, Tsavlis, D, Kioumis, I, Kosmidis, C, et al. Lung abscess-etiology, diagnostic and treatment options. Ann Transl Med. (2015) 3:183. doi: 10.3978/j.issn.2305-5839.2015.07.08
3. Wali, SO. An update on the drainage of pyogenic lung abscesses. Ann Thorac Med. (2012) 7:3–7. doi: 10.4103/1817-1737.91552
4. Vainrub, B, Musher, DM, Guinn, GA, Young, EJ, Septimus, EJ, and Travis, LL. Percutaneous drainage of lung abscess. Am Rev Respir Dis. (1978) 117:153–60. doi: 10.1164/arrd.1978.117.1.153
5. Weissberg, D. Percutaneous drainage of lung abscess. J Thorac Cardiovasc Surg. (1984) 87:308–12. doi: 10.1016/S0022-5223(19)37427-6
6. Mengoli, L. Giant lung abscess treated by tube thoracostomy. J Thorac Cardiovasc Surg. (1985) 90:186–94. doi: 10.1016/S0022-5223(19)38618-0
7. Schmitt, GS, Ohar, JM, Kanter, KR, and Naunheim, KS. Indwelling transbronchial catheter drainage of pulmonary abscess. Ann Thorac Surg. (1988) 45:43–7. doi: 10.1016/s0003-4975(10)62394-6
8. Yazbeck, MF, Dahdel, M, Kalra, A, Browne, AS, and Pratter, MR. Lung abscess: update on microbiology and management. Am J Ther. (2014) 21:217–21. doi: 10.1097/MJT.0b013e3182383c9b
9. Matarese, A, Tamburrini, M, Desai, U, and Zuccon, U. Percutaneous lung abscess drainage: revisiting the old gold standard. Monaldi Arch Chest Dis. (2020) 90:90. doi: 10.4081/monaldi.2020.1214
10. Lee, JH, Hong, H, Tamburrini, M, and Park, CM. Percutaneous transthoracic catheter drainage for lung abscess: a systematic review and meta-analysis. Eur Radiol. (2022) 32:1184–94. doi: 10.1007/s00330-021-08149-5
11. Harclerode, TP, and Gnugnoli, DM. Percutaneous abscess drainage. Treasure Island, FL: StatPearls (2022).
12. Rami-Porta, R, Bravo-Bravo, JL, Alix-Trueba, A, and Serrano-Munoz, F. Percutaneous drainage of lung abscess. J Thorac Cardiovasc Surg. (1985) 89:314. doi: 10.1016/S0022-5223(19)38833-6
13. Carvalho, JS, Marques, DP, Oliveira, I, and Vieira, AC. Unusual case of a giant lung abscess initially misdiagnosed and treated as an empyema. BMJ Case Rep. (2019) 12:e228849. doi: 10.1136/bcr-2018-228849
14. Gaballah, A, Elgazzar, AE, Elshahat, H, Yusuf, A, and Takwa, H. The role of ultrasound-guided nephrostomy catheter drainage in the management of peripheral pyogenic lung abscess. Egypt J Chest Dis Tuberc. (2018) 67:38. doi: 10.4103/ejcdt.ejcdt_17_17
15. Rice, TW, Ginsberg, RJ, and Todd, TR. Tube drainage of lung abscesses. Ann Thorac Surg. (1987) 44:356–9. doi: 10.1016/s0003-4975(10)63790-3
16. Shim, C, Santos, GH, and Zelefsky, M. Percutaneous drainage of lung abscess. Lung. (1990) 168:201–7. doi: 10.1007/BF02719693
17. vanSonnenberg, E, D’Agostino, HB, Casola, G, Wittich, GR, Varney, RR, and Harker, C. Lung abscess: CT-guided drainage. Radiology. (1991) 178:347–51. doi: 10.1148/radiology.178.2.1987590
18. Ri, JM, Kim, YJ, and Kang, DS. Percutaneous drainage of lung abscess. J Korean Radiol Soc. (1992) 28:373–81. doi: 10.3348/jkrs.1992.28.3.373
19. Kim, GH, Hwang, YS, and Kim, HJ. Percutaneous drainage of lung abscess and infected Bulla. Tuberc Respir Dis. (1994) 41:120–6. doi: 10.4046/trd.1994.41.2.120
20. Prasad, B, Shashirekha, TSC, and Kasthuri, AS. Management of lung abscess with percutaneous catheter drainage. Med J Armed Forces India. (1998) 54:134–6. doi: 10.1016/S0377-1237(17)30503-8
21. Jabłoński, S, Modrzewski, W, Rysz, J, Machała, W, Jabłonowski, Z, and Kordiak, J. Pulmonary abscesses-aetiology and treatment. Ten-year experience of the Department of General and Thoracic Surgery in Lodz, Poland. Arch Med Sci. (2006) 2:47–54.
22. Yunus, M. CT guided transthoracic catheter drainage of intrapulmonary abscess. J Pak Med Assoc. (2009) 59:703–9.
23. Kelogrigoris, M, Tsagouli, P, Stathopoulos, K, Tsagaridou, I, and Thanos, L. CT-guided percutaneous drainage of lung abscesses: review of 40 cases. JBR-BTR. (2011) 94:191–5. doi: 10.5334/jbr-btr.583
24. Noldge, G, Richter, GM, Grenacher, L, Brado, M, and Kauffmann, GW. CT-guided puncture. Radiologe. (1996) 36:683–91. doi: 10.1007/s001170050128
25. Salik, I, Vashisht, R, and Abramowicz, AE. Bronchopleural fistula. Treasure Island, FL: StatPearls (2022).
26. Li, X, Wang, S, Yin, M, Li, X, Qi, Y, Ma, Y, et al. Treatment of peripheral bronchopleural fistula with interventional negative pressure drainage. Ther Adv Respir Dis. (2022) 16:175346662211118. doi: 10.1177/17534666221111877
Keywords: lung abscess, drainage, interventional radiology (IR), length of stay, treatment outcome
Citation: Chiang P-C, Lin C-Y, Hsu Y-C, Huang L-T, Chung T-J, Liu Y-S and Chang C-C (2023) Early drainage reduces the length of hospital stay in patients with lung abscess. Front. Med. 10:1206419. doi: 10.3389/fmed.2023.1206419
Received: 15 April 2023; Accepted: 22 August 2023;
Published: 05 September 2023.
Edited by:
Dawei Yang, Fudan University, ChinaReviewed by:
Patrick Zardo, Hannover Medical School, GermanyCopyright © 2023 Chiang, Lin, Hsu, Huang, Chung, Liu and Chang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chao-Chun Chang, aTU0OTMxNDlAZ21haWwuY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.