
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 25 May 2023
Sec. Intensive Care Medicine and Anesthesiology
Volume 10 - 2023 | https://doi.org/10.3389/fmed.2023.1199750
A correction has been applied to this article in:
Corrigendum: Association of airway obstruction with first-pass success and intubation-related adverse events in the emergency department: multicenter prospective observational studies
 Jin Takahashi1,2*
Jin Takahashi1,2* Tadahiro Goto3
Tadahiro Goto3 Shigeki Fujitani2
Shigeki Fujitani2 Hiroshi Okamoto4
Hiroshi Okamoto4 Yusuke Hagiwara5
Yusuke Hagiwara5 Hiroko Watase6
Hiroko Watase6 Kohei Hasegawa7 and the Japanese Emergency Medicine Network Investigators
Kohei Hasegawa7 and the Japanese Emergency Medicine Network Investigators Background: Airway obstruction is a relatively rare but critical condition that requires urgent intervention in the emergency department (ED). The present study aimed to investigate the association of airway obstruction with first-pass success and intubation-related adverse events in the ED.
Methods: We analyzed data from two prospective multicenter observational studies of ED airway management. We included adults (aged ≥18 years) who underwent tracheal intubation for non-trauma indications from 2012 through 2021 (113-month period). Outcome measures were first-pass success and intubation-related adverse events. We constructed a multivariable logistic regression model adjusting for age, sex, modified LEMON score (without airway obstruction), intubation methods, intubation devices, bougie use, intubator’s specialty, and ED visit year with accounting for patients clustering within the ED.
Results: Of 7,349 eligible patients, 272 (4%) underwent tracheal intubation for airway obstruction. Overall, 74% of patients had first-pass success and 16% had intubation-related adverse events. The airway obstruction group had a lower first-pass success rate (63% vs. 74%; unadjusted odds ratio [OR], 0.63; 95% CI, 0.49–0.80), compared to the non-airway obstruction group. This association remained significant in the multivariable analysis (adjusted OR 0.60, 95%CI 0.46–0.80). The airway obstruction group also had a significantly higher risk of adverse events (28% vs. 16%; unadjusted OR, 1.93; 95% CI, 1.48–2.56, adjusted OR, 1.70; 95% CI, 1.27–2.29). In the sensitivity analysis using multiple imputation, the results remained consistent with the main results: the airway obstruction group had a significantly lower first-pass success rate (adjusted OR, 0.60; 95% CI, 0.48–0.76).
Conclusion: Based on these multicenter prospective data, airway obstruction was associated with a significantly lower first-pass success rate and a higher intubation-related adverse event rate in the ED.
Tracheal intubation is a critical resuscitation procedure in the emergency department (ED). As multiple intubation attempts are associated with an increased risk of intubation-related adverse events (1–3), the early identification of patients at risk of intubation failure is essential. Airway obstruction is a relatively rare indication for airway management in EDs, with a reported incidence of 2–3% (1, 4, 5). Airway obstruction may lead to intubation failure—e.g., as “cannot intubate, cannot oxygenate” (CICO) situations, and cardiac arrest. Emergency physicians should aim to achieve first-pass success even in the challenging condition (6).
Despite the significance of airway obstruction in the EDs, little is known about the relationship between airway obstruction and intubation outcomes in the ED. Two small, single-center studies (n 366) evaluating factors associated with difficult intubation (i.e., the LEMON score) have found no association between airway obstruction and difficult intubation (7, 8). Further understanding of airway management in cases of airway obstruction and its relationship with intubation outcomes will facilitate the development of optimal strategies for ED airway management.
To address the major knowledge gap in the literature, we aimed to examine the association of airway obstruction with first-pass success and intubation-related adverse events by analyzing data of two multicenter prospective studies of ED patients.
The present study a post hoc analysis data obtained from multicenter prospective observational studies of consecutive patients who underwent emergency airway management in EDs; the second and fifth Japanese Emergency Airway Network (JEAN-2 and -5) studies. The study design, setting, data collection methods, and measured variables of JEAN have been reported previously (1, 9–16). In summary, JEAN-2 comprised 15 academic and community EDs in various geographic regions across Japan and was conducted between February 2012 and March 2020. JEAN-5 is a subsequent study using standardized procedures that are similar to JEAN-2. JEAN-5 consisted of 14 EDs (accordingly, JEAN-2 and JEAN-5 comprised a total of 21 EDs) was conducted between April 2020 and July 2021. All EDs have emergency medicine residency programs and are staffed by emergency medicine attending physicians. Each ED has individual protocols for airway management. At the discretion of the attending physician, intubations are performed by attending physicians, resident physicians, or transitional-year residents (postgraduate years 1 and 2) rotating through EDs. The institutional review board of each participating institution approved the protocol with a waiver of informed consent before data collection.
A standardized data collection form was completed by the intubator performing tracheal intubation immediately after each procedure. These data included patient demographics (age, sex, and estimated height and weight), the primary indication for intubation, intubation methods, administered medications, intubation devices, level of training and specialty of the intubator, number of intubation attempts, pre- and post-intubation vital signs, intubation success or failure, and intubation-related adverse events (14). The JEMNet (Japanese Emergency Medicine Network) Coordinating Centre and site investigator at each participating institution monitored compliance with data form completion. If there was any data missing from the data form, the data was returned to the intubator for completion. If there was any inconsistency in the data form, the intubator was contacted for clarification by the site investigator. We defined an intubation “attempt” as the insertion of a laryngoscope blade (or other devices) past the teeth (4, 14). An intubation attempt was defined as a success if a tracheal tube was passed through the vocal cord with placement confirmed by quantitative or colorimetric end-tidal carbon dioxide monitoring.
The present analysis used data from adult (aged ≥18 years) patients who underwent tracheal intubation for non-trauma indications including cardiac arrest in EDs during a consecutive 113-month period (from February 2012 through July 2021). We excluded patients who underwent tracheal intubation for trauma and those with missing data, such as age, height, weight, intubation methods, intubation devices, or intubator’s specialty.
The primary exposure was airway obstruction as the primary indication (including airway obstruction caused by anaphylaxis but excluding that caused primarily by altered mental status). Other non-trauma indications for tracheal intubation (e.g., respiratory failure, shock, altered mental status, and cardiac arrest) were defined as no airway obstruction.
The primary outcome of interest was first-pass success (2, 9, 13, 16, 17). The secondary outcome was overall intubation-related adverse events measured in EDs. Intubation-related adverse events were categorized into major (i.e., hypotension [systolic blood pressure < 90 mmHg], hypoxemia [pulse oximetry saturation < 90%], esophageal intubation with delayed recognition, cardiac arrest, and dysrhythmia) and minor (i.e., esophageal intubation with early recognition, endobronchial intubation, dental or lip trauma, regurgitation, and airway trauma) adverse events (1, 9, 15).
First, we compared patient demographics, airway management characteristics, and intubation outcomes between the airway obstruction and the non-airway obstruction groups by using Mann–Whitney U test, Fisher’s exact, or the chi-square test as appropriate. Next, to determine the association between airway obstruction and each of the intubation outcomes, we constructed logistic regression models with generalized estimating equations to account for potential patients clustering within the ED. We also adjusted for potential confounders, including age (9, 15), sex, body mass index (BMI; <25.0, 25.0–29.9, and ≥30.0 kg/m2) (16), modified LEMON score (without airway obstruction), intubation methods (rapid sequence intubation, sedation without paralysis, no medication, and others), intubation devices (direct laryngoscopy, video laryngoscopy, fiberscope, and others) (13), bougie use (17), intubator’s specialty (transitional-year resident, emergency medicine resident, emergency attending physician, and other specialties), and ED visit year. As the modified LEMON criteria include airway obstruction, a score of 1 was given to modified LEMON if any criteria except airway obstruction were met. We selected these confounders based on clinical plausibility and a priori knowledge (10, 13, 15–17).
To determine the robustness of our inference, we conducted a series of sensitivity analyses. First, we calculated E-values and their lower 95% confidence interval (CI) limit. The E-value gauges the evidence for causality (18). The E-value indicates how strong an unmeasured confounder would have to be associated with both the exposure and outcome in order for the observed association not to be causal (18). For example, an E-value of 2.0 means that the OR for the associations of unmeasured confounders with both the exposure and outcome would have to be >2.0 to fully explain away the observed exposure-outcome association of interest. Second, there were because there were missing values for age, BMI, modified LEMON score, intubation devices, and intubator’s specialty, we imputed missing data using the multiple imputation method based on the assumption that missing was at random. All these variables and sex, intubation methods, bougie use, ED visit year, primary exposure (airway obstruction or no airway obstruction), and outcomes (first-pass success, overall, major, or minor adverse events) were used to predict imputation. We applied 20 imputed datasets using multivariable imputation using the chained equations (MICE) algorithm and then estimated odds ratios with 95% CI based on Rubin’s rules (19, 20). Third, we repeated the model using two additional outcomes: intubation success within two attempts, and rescue surgical airway attempts. p-values of <0.05 were considered statistically significant. Statistical analyses were performed using STATA 16.1 (StataCorp, College Station, TX) and JMP 14.0.0 (SAS Institute, Inc., Cary, NC).
During the 113-month study period, the JEAN-2 and JEAN-5 studies recorded a total of 14,312 patients who underwent emergency airway management in 21 EDs (capture rate, 97%; Supplementary Figure S1). Of these, the present study excluded 397 pediatric patients, 1,910 patients who underwent intubation for trauma, and 4,656 patients with missing data (age [n = 19], BMI [n = 844], modified LEMON score [n = 3,773], intubation devices [n = 6], and intubator’s specialty [n = 14]), leaving 7,349 patients with complete covariate data. Of these, 272 patients (4%) underwent tracheal intubation for airway obstruction.
Clinical and airway management characteristics are summarized in Table 1. Overall, the median age of study participants was 72 years (interquartile range [IQR], 60–81 years) and 62% of them were male. The airway obstruction group, compared to the non-airway obstruction group, comprised a greater proportion of obesity and modified LEMON score of ≥1 (both p < 0.05). In addition, patients with airway obstruction were less likely to have been intubated using a direct laryngoscope and more likely to have been intubated using a fiberscope or by an attending physician (all p < 0.05).

Table 1. Clinical and airway management characteristics of patients who underwent tracheal intubation in the emergency department according to airway obstruction.
Overall, the first-pass success rate was 74%. The airway obstruction group had a significantly lower first-pass success rate than the non-airway obstruction group (63% vs. 74%; unadjusted odds ratio [OR], 0.63; 95% CI, 0.49–0.80; p < 0.001; Table 2 and Figure 1). With adjusting for potential confounders, the association remained significant (adjusted OR, 0.60; 95%CI, 0.46–0.80; p < 0.001; E-value = 1.90). The overall rate of adverse events was 16% (major adverse events, 9%; minor adverse events, 9%) (Table 2). The airway obstruction group had significantly higher rates of overall (28% vs. 16%; p < 0.001), major (13% vs. 8%; p < 0.01), and minor (16% vs. 8%; p < 0.001) adverse events, compared to the non-airway obstruction group (Figure 1). Likewise, in the multivariable models, airway obstruction was associated with significantly higher rates of overall (adjusted OR, 1.70; 95% CI, 1.27–2.29; p < 0.001; E-value = 1.93) and minor (adjusted OR, 2.07; 95% CI, 1.43–3.00; p < 0.001; E-value = 3.56) adverse events.
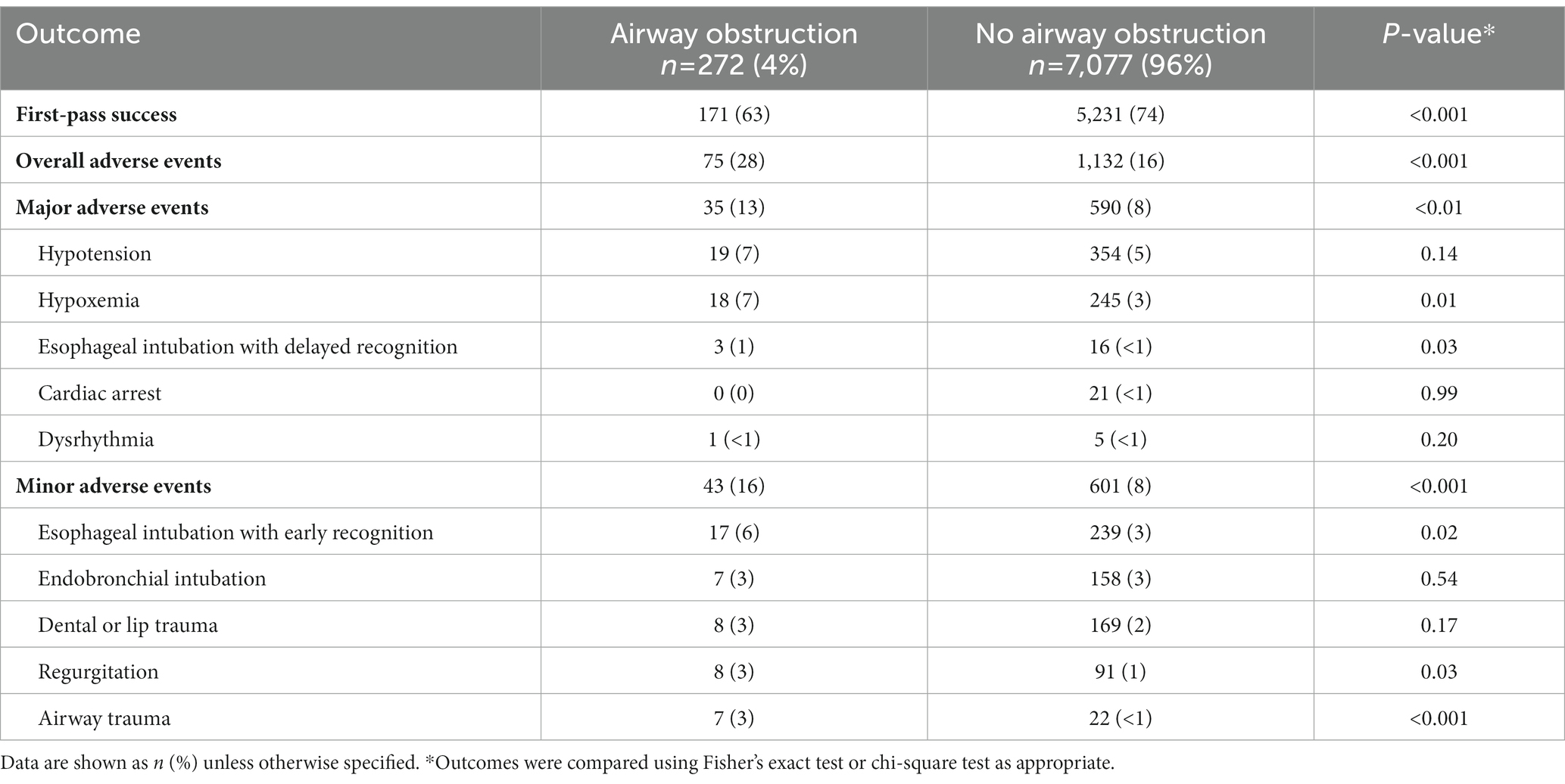
Table 2. First intubation success and intubation-related adverse events according to airway obstruction.
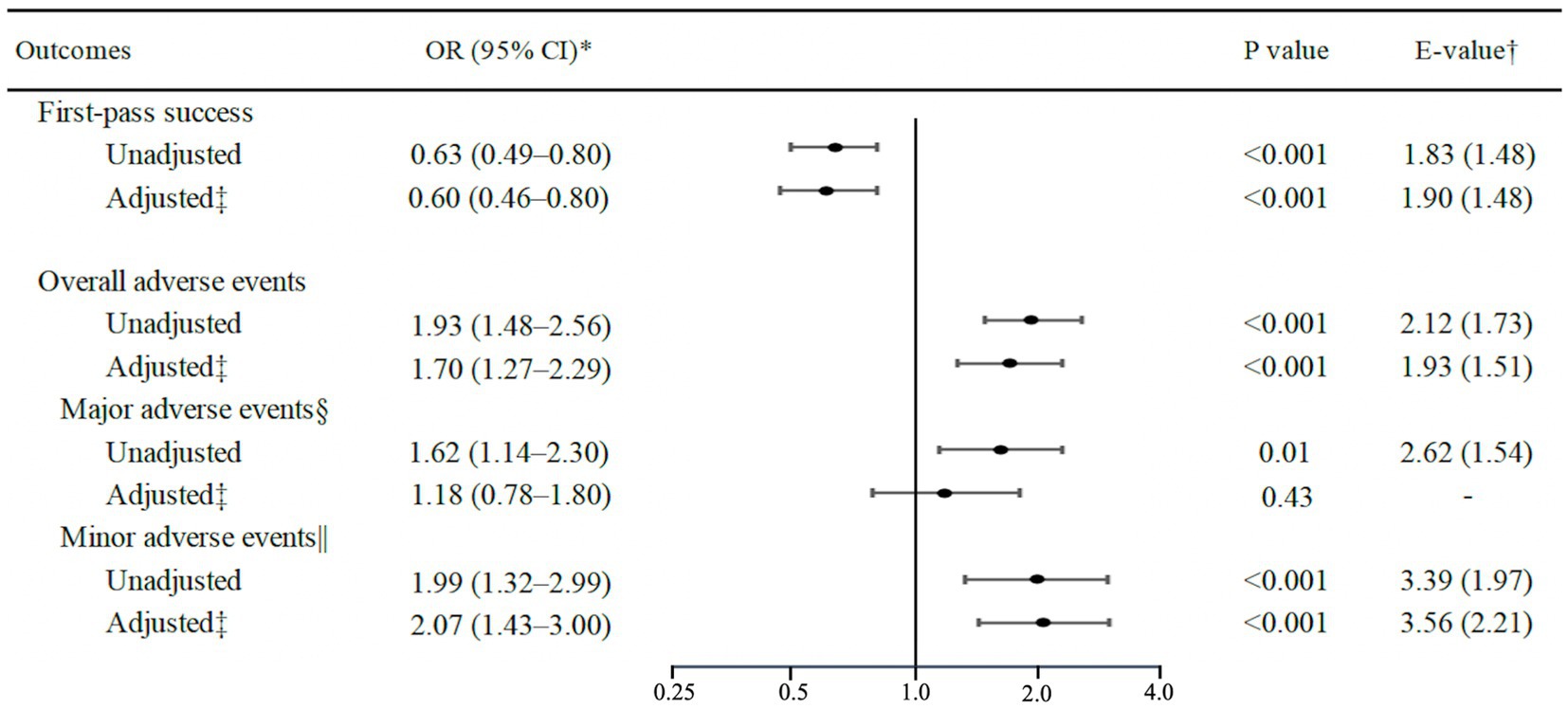
Figure 1. Unadjusted and adjusted associations of airway obstruction with first-pass success and intubation-related adverse events. *Logistic regression models with generalized estimating equations were used to account for potential patients clustering within the emergency department. †E-value (and its lower 95% CI limit) indicates the strength of the association between an unmeasured confounder(s) and both the exposure and outcome required to fully explain the observed association. ‡Adjusted for age, sex, body mass index, modified LEMON score, intubation methods, intubation devices, bougie use, intubator’s specialty, and ED visit year. §Major adverse events included hypotension, hypoxemia, esophageal intubation with delayed recognition, cardiac arrest, and dysrhythmia. ||Minor adverse events included esophageal intubation with early recognition, endobronchial intubation, dental or lip trauma, regurgitation, and airway trauma. CI, confidence interval; OR, odds ratio.
In the sensitivity analyses, first, in the analysis using multiple imputation, the results remained consistent with the main results — e.g., patients with airway obstruction had a significantly lower first-pass success rate (adjusted OR, 0.60; 95% CI, 0.48–0.76; p < 0.001; E-value = 1.90; Figure 2). Second, airway obstruction was significantly associated with a lower rate of intubation success within two attempts (OR, 0.58; 95% CI, 0.40–0.85; p < 0.01; E-value = 1.95) and higher rate of rescue surgical airway attempt (unadjusted OR, 8.91; 95% CI, 3.35–23.74; p < 0.001; Table 3).
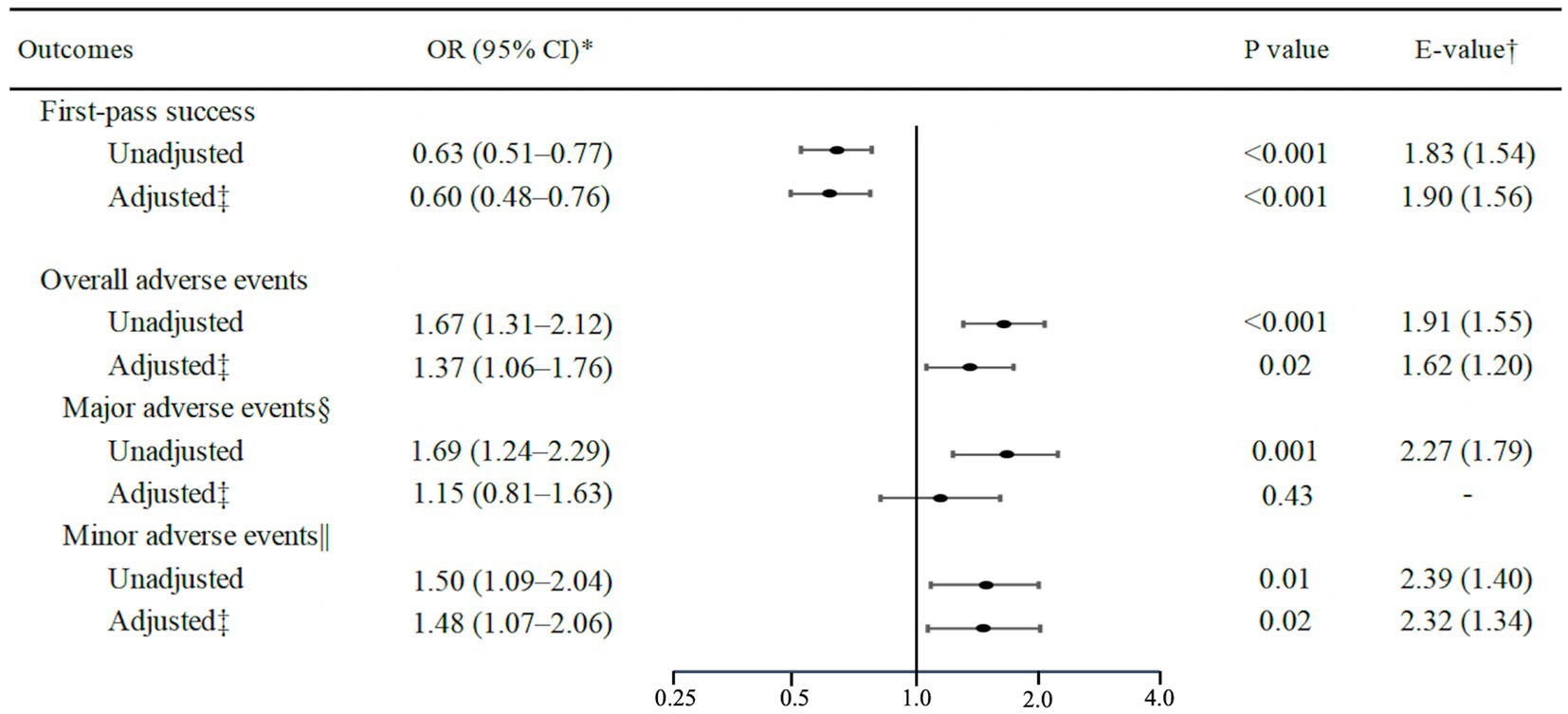
Figure 2. Unadjusted and adjusted associations of airway obstruction with first-pass success and intubation-related adverse events using multiple imputation. *Logistic regression models with generalized estimating equations were used to account for potential patients clustering within the emergency department. †E-value (and its lower 95% CI limit) indicates the strength of the associations between an unmeasured confounder(s) and both the exposure and outcome required to fully explain the observed associations. ‡Adjusted for age, sex, body mass index, modified LEMON score, intubation methods, intubation devices, bougie use, intubator’s specialty, and ED visit year. §Major adverse events included hypotension, hypoxemia, esophageal intubation with delayed recognition, cardiac arrest, and dysrhythmia. ||Minor adverse events included esophageal intubation with early recognition, endobronchial intubation, dental or lip trauma, regurgitation, and airway trauma. OR, odds ratio; CI, confidence interval.
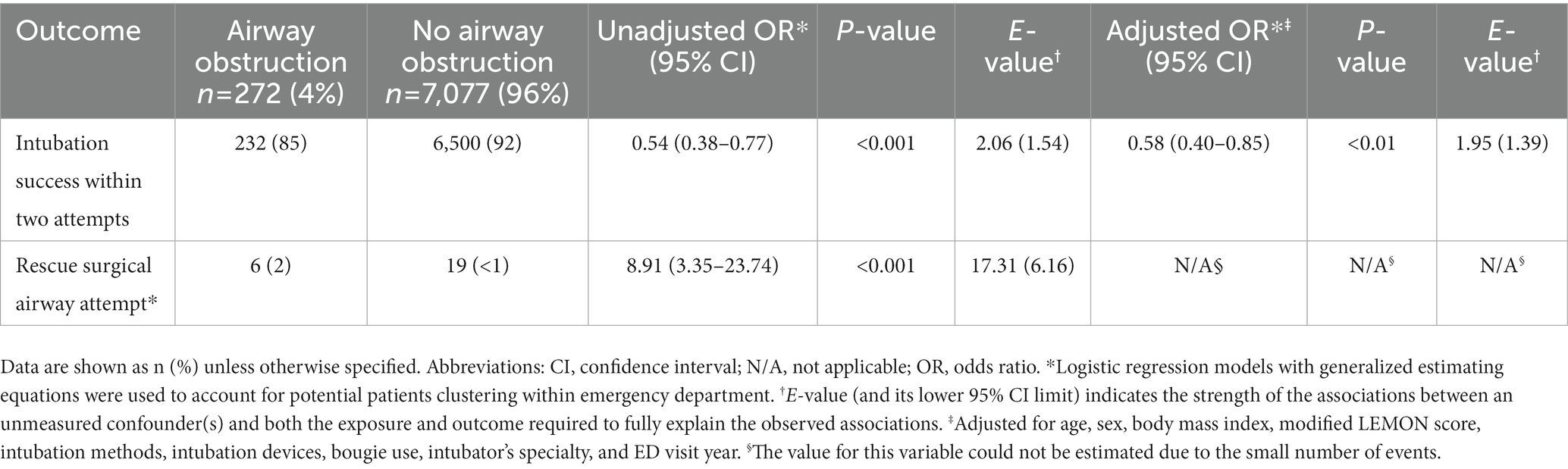
Table 3. Unadjusted and adjusted associations of airway obstruction with intubation success within two attempts and rescue surgical airway attempt.
In the present analysis of data from two multicenter prospective studies of 7,349 ED intubations, airway obstruction was associated with a significantly lower first-pass success rate and a significantly higher risk of intubation-related adverse events. The observed associations were consistent across the different analytical assumptions. Patients with airway obstruction also had a significantly lower rate of intubation success within two attempts and a higher rate of rescue surgical airway attempts. To the best of our knowledge, this is the first investigation that has demonstrated the relationship of airway obstruction with worse intubation outcomes in the ED.
The sparse ED literature on this research topic makes direct comparison with our observations difficult. In the field of anesthesiology, 40% of major intubation-related adverse events (e.g., death) in the operation room were due to airway abnormalities involving the head, neck, and trachea, and 70% of those were due to airway obstruction (21). In the ED setting, a descriptive study of intubation for angioedema reported a first-pass success rate of 81% (22). Potential reasons for the high first-pass success rate include the more-frequent use of the fiberscope (49%) and potential underestimation of intubation attempt frequency (22). In contrast to our findings, two smaller single-center studies (n 366) investigating predictors of intubation difficulty found no significant association between airway obstruction and intubation difficulty (7, 8). The discrepancy between the findings may be attributable to the difference in the study design, sample, data collection measures, study sample size, or any combination of these factors. Regardless, our study—with a sample size many times larger—build on these earlier reports and extend them by demonstrating the relationship between airway obstruction and intubation outcomes in the ED.
The underlying mechanisms of the observed association are likely multifactorial. First, the underlying cause(s) of airway obstruction may further hinder visualization of the vocal cords and tracheal intubation. Poor visualization of the vocal cord is known to increase the technical difficulty of intubation (23). Indeed, in the present study, esophageal intubation (with early or delayed recognition), airway trauma, and hypoxemia were more frequently observed in the airway obstruction group, supporting this mechanism (23). Second, as each patient has a different (partial or complete) level of airway obstruction, the optimal intubation methods and devices are different between patients (6, 24). This complexity and cognitive load might have led to intubation failure and adverse events (24). Lastly, these mechanisms are not mutually exclusive. Regardless of the complexity of these potential mechanisms, emergency physicians should develop optimal airway management strategies and technical skills (e.g., fiberscope, bougie, and surgical airway procedures) for patients with airway obstruction. In addition to these technical improvements, individual or team simulation training and in-situ supervision by attending physicians may increase the effectiveness of airway management (25, 26).
The present study has several potential limitations. First, airway obstruction was primarily determined by the judgment of the intubator as the study does not have data on the actual causes of airway obstruction. This might have introduced information bias. Second, we excluded traumatic airway obstruction because medical and traumatic airway obstruction cannot be dealt with as the same due to their differences in physiological and anatomical factors. In addition, JEAN registries did not collect information on whether pharyngeal foreign bodies were removed with Magill forceps. In cases where intubation was necessary due to airway obstruction caused by a foreign body, we assumed that the removal of the foreign body and intubation was considered a single event. Regardless, the rate of airway obstruction observed in the current study was 2.9%, which was consistent with that of earlier reports (i.e., 1.7–3.2%) (4, 5). Third, the exclusion of patients with a missing value may have introduced selection bias. To address this issue, we performed a subsequent analysis using multiple imputation, which demonstrated consistent inference. Fourth, self-reporting bias may have overestimated the first-pass success rate and underestimated the rate of adverse events. However, the study was based on a previously defined self-reporting system with standardized data forms and a high capture rate (97%). Fifth, the causal inference may be confounded by unmeasurable confounders, such as patient demographics (e.g., underlying diseases) and factors related to airway obstruction (e.g., malformation or obstruction severity). Nevertheless, the E-values supported the robustness of our inference. Finally, the generalizability of our findings may be limited in other ED settings. Nevertheless, the observed relationships are plausible.
On the basis of data from two multicenter prospective studies of 7,349 patients who underwent tracheal intubation, patients with airway obstruction had a significantly lower first-pass success rate and a significantly higher rate of intubation-related adverse events. For clinicians, our data underscore the importance of identifying these high-risk patients and the systematic use of rescue intubation techniques in emergency airway management. Furthermore, our observations should facilitate further investigation into the optimal airway management practice in the ED, which will, in turn, lead to better outcomes in critically-ill patients.
IRB does not allow data sharing.
The protocols for the studies were approved by the Ethics Committees of Tokyo Bay Urayasu Ichikawa Medical Center (approval number of JEAN-2 873, approval number of JEAN-5 533). Written informed consent for participation was not required for these studies in accordance with the institutional requirements.
JT took responsibility for the manuscript as a whole. JT, TG, SF, and KH conceived the study. HO, YH, HW, and KH supervised the conduct of the study. TG, SF, and KH provided the statistical advice. JT and TG performed the data analyses. JT drafted the manuscript. All authors contributed substantially to manuscript revision.
The present study was supported by grants from St. Luke’s Science Institute (H26, H27) (Tokyo, Japan). The study sponsor had no involvement in the study design, data collection, data analysis and interpretation, manuscript preparation, or in the decision to submit the manuscript for publication.
The authors acknowledge the Japanese Emergency Medicine Network Investigators for their contributions to this project: (1) Hiroshi Morita; Takahisa Kawano; Yohei Kamikawa (Fukui University Hospital); (2) Hideya Nagai; Takashi Matsumoto; Suguru Nonami; Yusuke Miyoshi (Fukui Prefectural Hospital); (3) Sho Segawa; Yuya Kitai; Kenzo Tanaka; Saburo Minami (Kameda Medical Center); (4) Hiromasa Yakushiji (Kishiwada Tokushukai Hospital); (5) Hiroshi Okamoto; Naoto Miyauchi; Yudai Yano (Kurashiki Central Hospital); (6) Yukari Goto (Nagoya Ekisaikai Hospital); (7) Nobuhiro Sato (Nigata City General Hospital); (8) Koichiro Gibo; Masashi Okubo; Shojiro Oka; Yukiko Nakayama (Okinawa Chubu Prefectural Hospital); (9) Nobuhiro Miyamae (Otowa Hospital); (10) Hirose Kaoru; Taichi Imamura; Azusa Uendan; Ami Horiike (Shonan Kamakura General Hospital); (11) Yasuaki Koyama (St. Marianna University School of Medicine Hospital); (12) Hiroshi Kamura; Nakashima Yoshiyuki; Jin Takahashi (Tokyo Bay Urayasu Ichikawa Medical Center); (13) Jin Irie; Nobunaga Okada (University Hospital, Kyoto Prefectural University of Medicine); (14) Seiro Oya (Yokohama Rosai Hospital); and (15) Akihiko Inoue (Hyogo Emergency Medical Center). (16) Daiki Shiba (St.Luke’s International Hospital); (17) Hidenori Higashi (Japanese Red Cross Wakayama Medical Center); (18) Osamu Nomura (Hirosaki University Hospital); (19) Mikio Nakajima (Tokyo Metropolitan Hiroo Hospital); (20) Hiromichi Naito (Okayama University Hospital); (21) Masakazu Obayashi (Chutoen General Medical Center); Michihito Kyo (Hiroshima University Hospital). We also thank our many emergency physicians and residents for their perseverance in pursuing new knowledge about this vital resuscitative procedure.
TG was employed by TXP Medical Co., Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1199750/full#supplementary-material
1. Hasegawa, K, Shigemitsu, K, Hagiwara, Y, Chiba, T, Watase, H, Brown, CA 3rd, et al. Association between repeated intubation attempts and adverse events in emergency departments: an analysis of a multicenter prospective observational study. Ann Emerg Med. (2012) 60:749–754.e2. doi: 10.1016/j.annemergmed.2012.04.005
2. Sakles, JC, Chiu, S, Mosier, J, Walker, C, and Stolz, U. The importance of first pass success when performing orotracheal intubation in the emergency department. Acad Emerg Med. (2013) 20:71–8. doi: 10.1111/acem.12055
3. Mort, TC . Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg. (2004) 99:607–13. doi: 10.1213/01.ANE.0000122825.04923.15
4. Brown, CA, Bair, AE, Pallin, DJ, and Walls, RM. Techniques, success, and adverse events of emergency department adult intubations. Ann Emerg Med. (2015) 65:363–370.e1. doi: 10.1016/j.annemergmed.2014.10.036
5. Cho, J, Cho, YS, You, JS, Lee, HS, Kim, H, Chung, HS, et al. Current status of emergency airway management for elderly patients in Korea: multicentre study using the Korean emergency airway management registry. Emerg Med Australas. (2013) 25:439–44. doi: 10.1111/1742-6723.12122
6. Eskander, A, de Almeida, JR, and Irish, JC. Acute upper airway obstruction. N Engl J Med. (2019) 381:1940–9. doi: 10.1056/NEJMra1811697
7. Reed, MJ, Dunn, MJ, and McKeown, DW. Can an airway assessment score predict difficulty at intubation in the emergency department? Emerg Med J. (2005) 22:99–102. doi: 10.1136/emj.2003.008771
8. Soyuncu, S, Eken, C, Cete, Y, Bektas, F, and Akcimen, M. Determination of difficult intubation in the ED. Am J Emerg Med. (2009) 27:905–10. doi: 10.1016/j.ajem.2008.07.003
9. Imamura, T, Brown, CA 3rd, Ofuchi, H, Yamagami, H, Branch, J, Hagiwara, Y, et al. Emergency airway management in geriatric and younger patients: analysis of a multicenter prospective observational study. Am J Emerg Med. (2013) 31:190–6. doi: 10.1016/j.ajem.2012.07.008
10. Hagiwara, Y, Watase, H, Okamoto, H, Goto, T, and Hasegawa, K, Japanese Emergency Medicine Network I. Prospective validation of the modified LEMON criteria to predict difficult intubation in the ED. Am J Emerg Med. (2015) 33:1492–6. doi: 10.1016/j.ajem.2015.06.038
11. Goto, T, Gibo, K, Hagiwara, Y, Morita, H, Brown, DF, Brown, CA 3rd, et al. Multiple failed intubation attempts are associated with decreased success rates on the first rescue intubation in the emergency department: a retrospective analysis of multicentre observational data. Scand J Trauma Resusc Emerg Med. (2015) 23:5. doi: 10.1186/s13049-014-0085-8
12. Takahashi, J, Goto, T, Okamoto, H, Hagiwara, Y, Watase, H, Shiga, T, et al. Association of fentanyl use in rapid sequence intubation with post-intubation hypotension. Am J Emerg Med. (2018) 36:2044–9. doi: 10.1016/j.ajem.2018.03.026
13. Okamoto, H, Goto, T, Wong, ZSY, Hagiwara, Y, Watase, H, Hasegawa, K, et al. Comparison of video laryngoscopy versus direct laryngoscopy for intubation in emergency department patients with cardiac arrest: a multicentre study. Resuscitation. (2019) 136:70–7. doi: 10.1016/j.resuscitation.2018.10.005
14. Goto, Y, Goto, T, Hagiwara, Y, Tsugawa, Y, Watase, H, Okamoto, H, et al. Techniques and outcomes of emergency airway management in Japan: an analysis of two multicentre prospective observational studies, 2010-2016. Resuscitation. (2017) 114:14–20. doi: 10.1016/j.resuscitation.2017.02.009
15. Takahashi, J, Goto, T, Funakoshi, H, Okamoto, H, Hagiwara, Y, Watase, H, et al. Association of advanced age with intubation-related adverse events in the emergency department: a multicentre prospective observational study. Emerg Med J. (2021) 38:874–81. doi: 10.1136/emermed-2020-209801
16. Yakushiji, H, Goto, T, Shirasaka, W, Hagiwara, Y, Watase, H, Okamoto, H, et al. Associations of obesity with tracheal intubation success on first attempt and adverse events in the emergency department: an analysis of the multicenter prospective observational study in Japan. PLoS One. (2018) 13:e0195938. doi: 10.1371/journal.pone.0195938
17. Driver, BE, Prekker, ME, Klein, LR, Reardon, RF, Miner, JR, Fagerstrom, ET, et al. Effect of use of a bougie vs endotracheal tube and stylet on first-attempt intubation success among patients with difficult airways undergoing emergency intubation: a randomized clinical trial. JAMA. (2018) 319:2179–89. doi: 10.1001/jama.2018.6496
18. VanderWeele, TJ, and Ding, P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. (2017) 167:268–74. doi: 10.7326/M16-2607
19. Royston, P, and White, I. Multiple imputation by chained equations (MICE): implementation in Stata. J Stat Softw. (2011) 45:1–20. doi: 10.18637/jss.v045.i04
20. Rubin, DB, and Schenker, N. Multiple imputation in health-care databases: an overview and some applications. Stat Med. (1991) 10:585–98. doi: 10.1002/sim.4780100410
21. Cook, TM, Woodall, N, and Frerk, C, Fourth National Audit Project. Major complications of airway management in the UK: results of the fourth National Audit Project of the Royal College of Anaesthetists and the difficult airway society. Part 1: anaesthesia. Br J Anaesth. (2011) 106:617–31. doi: 10.1093/bja/aer058
22. Sandefur, BJ, Liu, XW, Kaji, AH, Campbell, RL, Driver, BE, Walls, RM, et al. Emergency department intubations in patients with angioedema: a report from the National Emergency Airway Registry. J Emerg Med. (2021) 61:481–8. doi: 10.1016/j.jemermed.2021.07.012
23. Taboada, M, Soto-Jove, R, Miron, P, Martinez, S, Rey, R, Ferreiroa, E, et al. Evaluation of the laryngoscopy view using the modified Cormack-Lehane scale during tracheal intubation in an intensive care unit. A prospective observational study. Rev Esp Anestesiol Reanim (Engl Ed). (2019) 66:250–8. doi: 10.1016/j.redar.2019.01.004
24. Lynch, J, and Crawley, SM. Management of airway obstruction. BJA Educ. (2018) 18:46–51. doi: 10.1016/j.bjae.2017.11.006
25. Thomas, F, Carpenter, J, Rhoades, C, Holleran, R, and Snow, G. The usefulness of design of experimentation in defining the effect difficult airway factors and training have on simulator oral-tracheal intubation success rates in novice intubators. Acad Emerg Med. (2010) 17:460–3. doi: 10.1111/j.1553-2712.2010.00706.x
Keywords: airway obstruction, first-pass success, intubation-related adverse events, emergency department, adults
Citation: Takahashi J, Goto T, Fujitani S, Okamoto H, Hagiwara Y, Watase H, Hasegawa K and the Japanese Emergency Medicine Network Investigators (2023) Association of airway obstruction with first-pass success and intubation-related adverse events in the emergency department: multicenter prospective observational studies. Front. Med. 10:1199750. doi: 10.3389/fmed.2023.1199750
Received: 03 April 2023; Accepted: 02 May 2023;
Published: 25 May 2023.
Edited by:
Shu-Chien Huang, National Taiwan University Hospital, TaiwanReviewed by:
Masahiro Kashiura, Jichi Medical University Saitama Medical Center, JapanCopyright © 2023 Takahashi, Goto, Fujitani, Okamoto, Hagiwara, Watase, Hasegawa and the Japanese Emergency Medicine Network Investigators. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jin Takahashi, amludEBqYWRlY29tLmpw
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.