- 1Department of Andrology, The Seventh Affiliated Hospital, Sun Yat-sen University, Shenzhen, China
- 2National Research Center for Assisted Reproductive Technology and Reproductive Genetics, Cheeloo College of Medicine, Shandong University, Jinan, China
Purpose: Pregnancy outcomes (overall patency rate, overall pregnancy rate, natural pregnancy rate, and the ratio of patients with pregnancy by assisted reproductive technology) after microsurgical vasoepididymostomy (MVE) in patients with epididymal obstructive azoospermia (EOA) were assessed through meta-analysis.
Method: We searched PubMed, Embase, Web of Science, and the Cochrane Library databases up to 28 September 2022 for published literature related to retrospective or prospective clinical studies of obstructive azoospermia after apparent microsurgical vasoepididymostomy. Our search terms included obstructive azoospermia, epididymis obstruction, epididymal obstruction and vasoepididymostomy, and epididymovasostomy. Two researchers independently performed the literature search and assessed the eligibility of selected studies according to established inclusion criteria. The meta-analysis was performed using RevMan 5.4 software.
Result: A total of 504 patients with EOA were included in 10 studies (including 2 prospective clinical studies and 8 retrospective clinical studies). The mean patency rate after MVE was 72% (95% CI 68–76%). The overall pregnancy rate was 34% (95% CI 30–38%). The natural pregnancy rate is 21% (95% CI 17–24%). The ratio of patients with pregnancy by assisted reproductive technology (ART) was 34.9%. For the factors affecting pregnancy outcomes after MVE, the overall pregnancy rates in patients receiving bilateral MVE were significantly higher than those receiving unilateral MVE (75.4 vs. 24.6%). The mean best sperm count and sperm motility in patients with overall pregnancy were significantly higher than those with failing pregnancies. For the subgroup meta-analysis of microsurgical vasoepididymostomy, there were no statistically significant differences in the overall patency rate (68 vs. 70%), the overall pregnancy rate (33 vs. 37%), the natural pregnancy rate (20 vs. 23%), the ratio of ART (30 vs. 28%) in end-to-side or end-to-end anastomosis, and longitudinal or triangular intussusception MVE.
Conclusion: Vasectomy patency rates are higher, but natural pregnancy rates are lower in EOA male infertility patients after MVE. Altering the MVE procedures alone does not significantly improve pregnancy outcomes, but ART after MVE could improve the chance of pregnancy regardless of sperm parameters. We recommended that human sperms from EOA male infertility patients should be cryopreserved during intraoperative MVE for application in the subsequent ICSI treatment procedure.
1. Introduction
Obstructive azoospermia (OA) is the primary cause of male infertility, accounting for ~40% of male patients with azoospermia (1). Congenital or acquired OA is usually caused by the obstruction of the reproductive tract, including the vas deferens, epididymis, and ejaculatory duct. Among them, epididymal obstruction is the most common etiology of OA, and the prevalence of epididymal obstructive azoospermia (EOA) is 42.4–48% (2).
With the continuous improvement of assisted reproductive technologies (ART), reproductive tract reconstruction procedures and micro-testicular sperm extraction combined with intracytoplasmic sperm injection (ICSI) have become the main procedures of OA (3). However, as the previous gold standard for the treatment of male reproductive tract obstruction, microsurgical vasoepididymostomy (MVE) is also considered to be the procedure of choice for patients with EOA who are willing to achieve natural pregnancy (4). Although MVE can achieve natural pregnancy for patients with EOA, there are still some abnormal intraoperative complications, such as difficult genital tract separation or reconstruction (5), which are dependent on ART to achieve pregnancy (6). Therefore, the assessment of pregnancy outcomes is clinically important, including the overall patency rate, the overall pregnancy rate, the natural pregnancy rate, and the ratio of patients with pregnancy by ART.
The natural pregnancy rate of the MVE procedure is significantly lower than that of ICSI (7). However, the remediable treatment or secondary surgery after a failed MVE procedure increases the risk of surgical trauma and economic burden (8). Therefore, the purpose of this meta-analysis was to evaluate pregnancy outcomes in order to provide the best preoperative strategy for ART in patients with EOA after MVE.
2. Methods
2.1. Study retrieval
A literature search was performed following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Guidelines. We searched PubMed, EMBASE, Web of Science, and the Cochrane Library for English-language articles to collect prospective or retrospective clinical studies of apparent microsurgical vasoepididymostomy in patients with epididymal obstructive azoospermia from the start of the database to 28 September 2022. Search terms included “obstructive azoospermia,” “epididymis obstruction,” “epididymal obstruction” and “vasoepididymostomy,” and “epididymovasostomy.” In addition, all references of included studies were manually scanned to search for relevant articles in our study. The PRISMA flow diagram of the literature search and screening is shown in Figure 1.
2.2. Inclusion criterion
Study selection and eligibility screening were conducted according to the patient population, intervention or exposure, comparator, outcome, and study design (PICOS). All patients had a clinical examination and biopsy histopathological analysis confirming obstructive azoospermia (P). All of these patients received surgical treatment with microsurgical vasoepididymostomy (I). We compared two surgical procedures of microsurgical vasoepididymostomy, that is, end-to-side or end-to-end anastomosis and longitudinal or triangular intussusception for subgroup analysis (C). All clinical studies included pregnancy outcomes (the overall patency rate, the overall pregnancy rate, the natural pregnancy rate, and the ratio of assisted reproductive technology) (O). We included only retrospective or prospective cohort studies (S). The review articles and case reports were excluded from our study.
2.3. Data extraction
Two investigators (ZW and XW) independently conducted the screening and data extraction for the literature search. Articles were first screened based on titles and abstracts and then selected by full-text articles according to eligibility criteria. The following data were extracted for our study: authors, year, country, study type, quality assessment level, total numbers of cases, surgical procedures, and pregnancy outcomes (the overall patency rate, the overall pregnancy rate, the natural pregnancy rate, and the ratio of assisted reproductive technology).
2.4. Quality assessment
Two investigators (ZW and XW) independently completed the quality assessment and risk of bias for all included studies. We assessed the quality of single-group studies using the “Quality Assessment Tool for Before-After (Pre-Post) Studies with No Control Group Scale.” Publication bias was assessed by funnel plots and Begg's test.
2.5. Statistical analysis
Meta-analysis was performed in Review Manager (RevMan) version 5.4 to calculate the corresponding probabilities, standard errors, risk difference (RD), and 95% credible intervals (95% CI) as an effective index. After initial fixed-effects model analysis revealed a high degree of heterogeneity between studies (I2>50%) for subgroup analysis, a meta-analysis was performed using a fixed-effects model with a random-effects model. Publication bias was assessed using a funnel plot and Begg's test. The grouped analyses were performed in R language (3.6.1) software and statistical significance was determined with the t-test. A P-value of < 0.05 was considered to be statistically significant.
3. Results
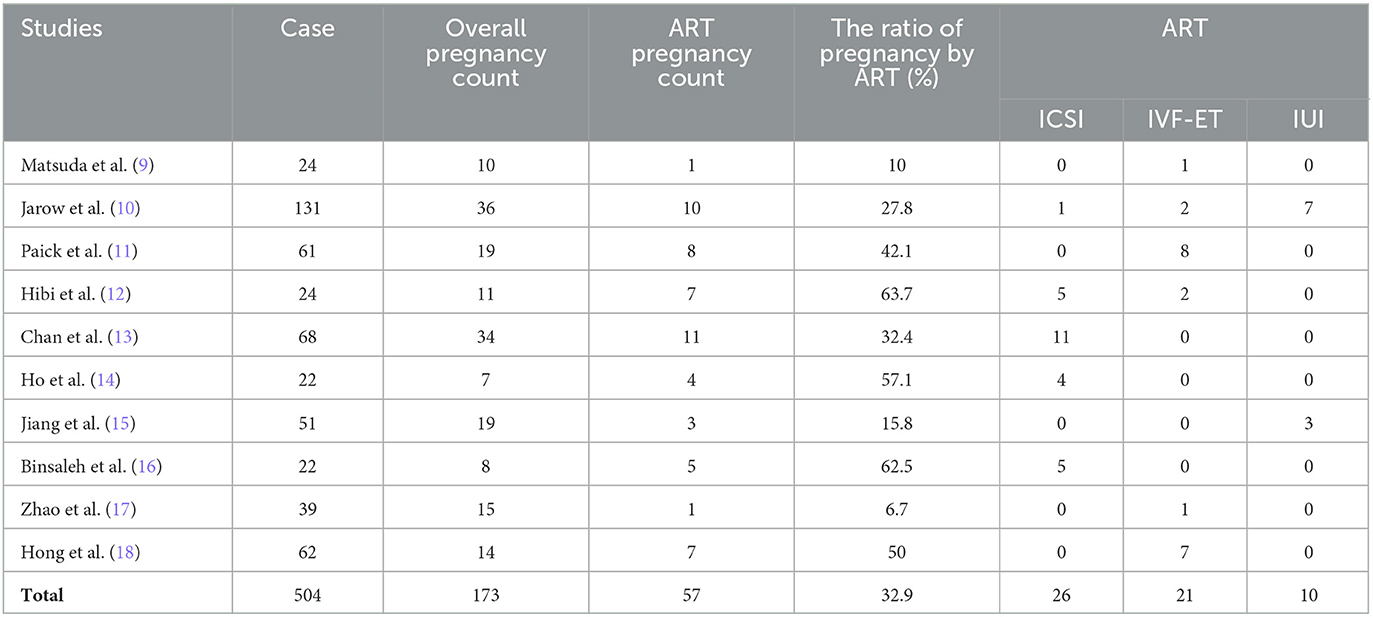
3.1. Literature search process and results
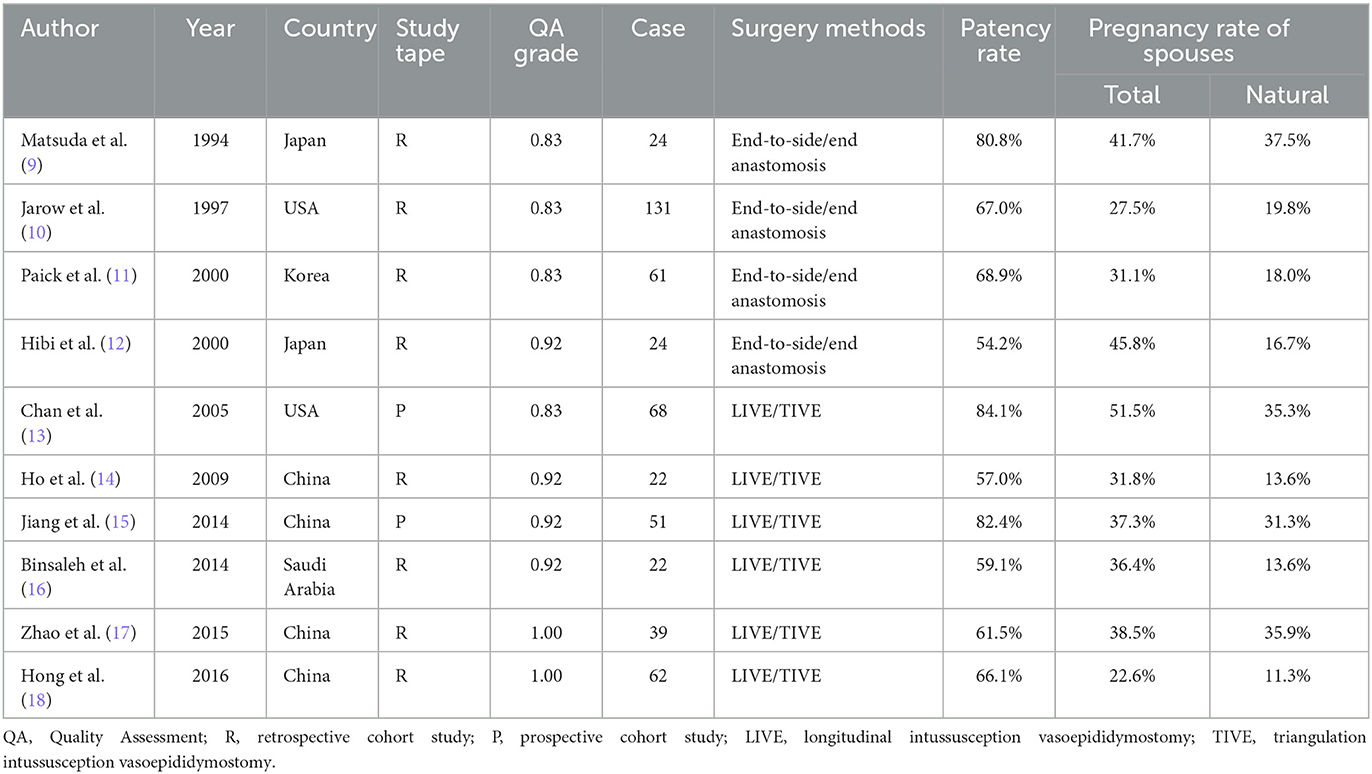
The literature search yielded 319 potentially relevant articles, from which 10 relevant studies met the inclusion criteria (9–18), including eight prospective cohort studies (9–12, 14, 16–18) and two retrospective cohort studies (13, 15). The PRISMA flow diagram in Figure 1 shows the literature search process. These 10 relevant studies included a total of 504 patients who received MVE, of whom 348 achieved vasectomy patency. A total of 173 patients achieved pregnancies, of which 116 achieved natural pregnancy and 57 achieved pregnancy by ART (Table 1).
3.2. The results of the meta-analysis
3.2.1. The overall patency rate of the vas deferens after MVE
A total of 10 clinical studies, including 504 patients were reviewed (9–18). In this analysis, a random-effect model was proposed for the high inter-study heterogeneity (P = 0.006, I2 = 61%). The results showed that the overall patency rate of the vas deferens after MVE was 72% (95% CI 68–76%, P < 0.0001, Figure 2A).
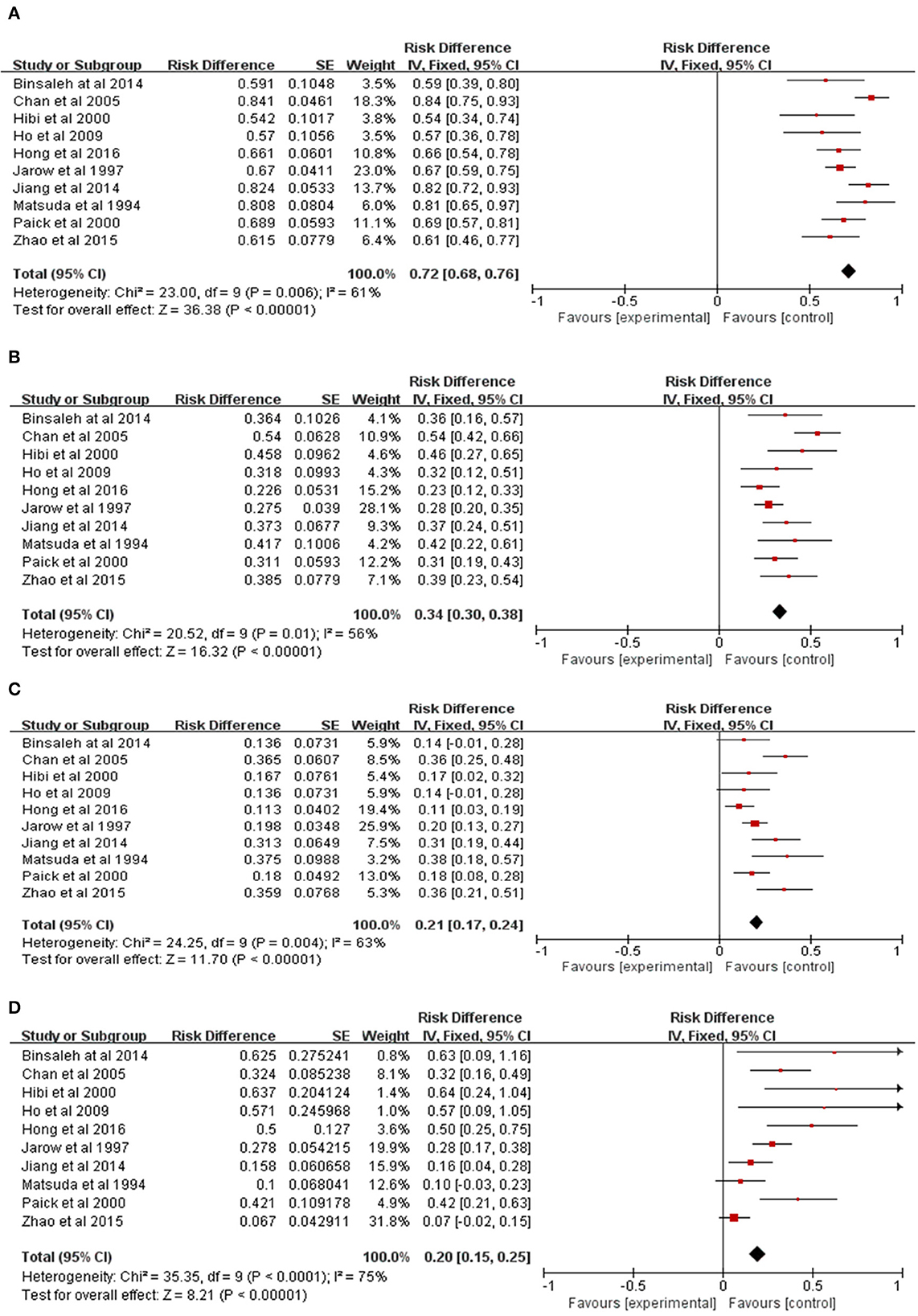
Figure 2. Meta-analysis of pregnancy outcomes in patients with EOA after MVE. (A) Meta-analysis of patency rate. (B) Meta-analysis of overall pregnancy rate. (C) Meta-analysis of natural pregnancy rate. (D) Meta-analysis of the ratio of pregnancy by ART.
3.2.2. The overall pregnancy rate after MVE
A total of 10 clinical studies, including 504 patients were reviewed (9–18). In this analysis, a random-effect model was presented for the high inter-study heterogeneity (P = 0.01, I2 = 56%). The results showed the overall pregnancy rate of 34% after MVE (95% CI 30–38%, P < 0.0001, Figure 2B).
3.2.3. The natural pregnancy rate after MVE
A total of 10 clinical studies were reviewed for inclusion, including 504 patients (9–18). In this analysis, a random-effect model was presented for the high inter-study heterogeneity (P = 0.004, I2 = 63%). The results showed the natural pregnancy rate after MVE was 21% (95% CI 17–24%, P < 0.0001, Figure 2C).
3.2.4. The ratio of pregnancy by ART after MVE
A total of 10 clinical studies were reviewed for inclusion, in which 173 patients' spouses achieved pregnancy (9–18). In this analysis, a random-effect model was presented for the high inter-study heterogeneity (P = 0.0002, I2 = 72%). There were 57 patients who achieved pregnancy by ART, including 26 ICSI cases, 21 in vitro fertilization and embryo transfer (IVF-ET) cases, and 10 intrauterine insemination (IUI) cases (Table 2). The results showed that the ratio of pregnancy by ART after MVE was 32.9% (Table 2; Figure 2D).
3.3. The factors affecting pregnancy outcomes after MVE
The factors affecting pregnancy outcomes after MVE includes the age of patients and their spouses, the etiology of obstruction, unilateral or bilateral operation, and postoperative sperm parameters.
3.3.1. The ages of patients and their spouses
A total of 10 clinical studies reviewed for the ages of patients, including 504 patients, with a mean age of 35.12 (20–57) years (9–18). However, for the lack of statistical data on the ages of spouses in three studies (9, 10, 18), there are only seven clinical studies reviewed, including 287 patients, with a mean age of 28.89 (21–41) years (11–17) (Table 3). However, there is only one study showing the effect of a spouse's gestational age on pregnancy outcomes (17). The result showed that the mean age of the pregnant and non-pregnant spouses was 26.5 ± 4.5 (ranging from 21 to 34 years) and 32.7 ± 3.3 years old (ranging from 29 to 38 years) (P < 0.05).
3.3.2. The etiology and duration of obstruction
The etiologies of obstruction mainly contain infection or epididymitis, vasectomy or inguinal herniorrhaphy, congenital anomalies, trauma, and idiopathic anomalies. A total of 10 clinical studies reviewed for these etiologies, including 504 patients (9–18). Overall, 159 (31.6%) patients suffered from infection or epididymitis, with 112 (22.2%) from vasectomy or inguinal herniorrhaphy, 27 (5.3%) from congenital anomalies, 5 (1%) from trauma, and 201 (39.9%) from idiopathic anomalies (Table 3).
Only five studies include the duration of obstruction (9, 10, 12, 13, 17) and only two above studies compared the duration between pregnancy and non-pregnancy (9, 17). However, for the lack of these patients' data from adolescence, the results showed no significant difference between pregnancy and the duration of obstruction (Table 3).
3.3.3. Meta-analysis of unilateral or bilateral MVE
A total of seven clinical studies, including 244 patients were reviewed (9, 12, 14–18). The overall pregnancy rates in patients receiving bilateral MVE were significantly higher than those receiving unilateral MVE (184 vs. 60, 75.4 vs. 24.6%, P = 0.03, Figure 3A; Table 4).
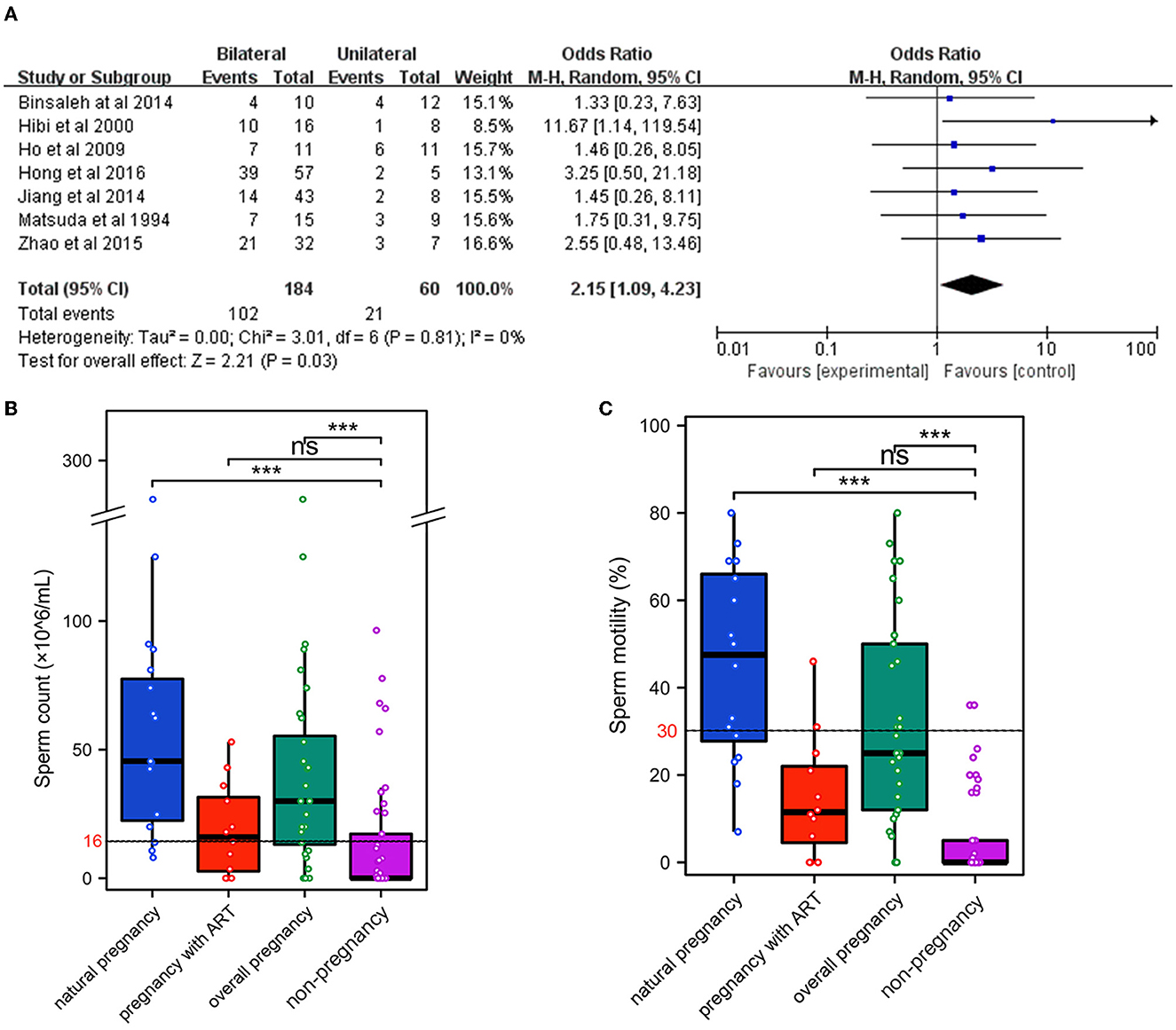
Figure 3. Factors affecting pregnancy outcomes after MVE. (A) Meta-analysis of unilateral or bilateral MVE. Grouped analyses of sperm parameters after MVE, including sperm count (B) and sperm motility (C). ***P < 0.001.
3.3.4. Grouped analyses and meta-analysis of sperm parameters after MVE
A total of six clinical studies contain sperm parameters after MVE (9, 12, 13, 16–18). These studies include 239 patients and the follow-up data containing sperm parameters were 219 patients (Table 5). The mean best sperm count was 21.8 × 106/ml (normal range ≥ 16 × 106/mL), and the mean best sperm motility (progressive motility rate, PR) was 19.4% (normal range ≥30%). The lower PR levels after MVE in semen samples could be the reason for the lower natural pregnancy rate.
There are three clinical studies including all sperm parameters of every patient (9, 12, 16). We performed grouped analyses for sperm count and sperm motility of these 70 patients. The mean best sperm count in patients with natural pregnancy and overall pregnancy were significantly higher than those failing pregnancy, respectively (66.5 × 106/ml vs. 22.3 × 106/ml, 46.8 × 106/ml vs. 22.3 × 106/ml, P < 0.001, Figure 3B). The same results showed the mean best PR levels in these patients (45.5 vs. 6.2%, 36.3 vs. 6.2%, P < 0.001, Figure 3C). However, the mean best sperm count and PR levels in patients with pregnancy by ART were not significantly higher (Figures 3B, C). The mean best sperm count in these patients (18.9 × 106/mL) was slightly higher than the normal ranges, and the PR levels (14.8%) were even lower than the normal ranges (Table 5).
We also performed continuous meta-analysis for sperm count and motility in these three clinical studies (9, 12, 16). The sperm count and motility in patients with overall pregnancy were significantly higher than those failing to achieve pregnancy, respectively (Supplementary Figures 1A, B), but those in natural pregnancy were not significantly higher (Supplementary Figures 1C, D). Furthermore, there were no significant differences between the sperm count or motility and successful pregnancy by ART after MVE (Supplementary Figures 1E, F). Therefore, combined with the data on the overall pregnancy rate and the ratio of patients with pregnancy by ART, ART after MVE could improve the chance of pregnancy regardless of sperm parameters.
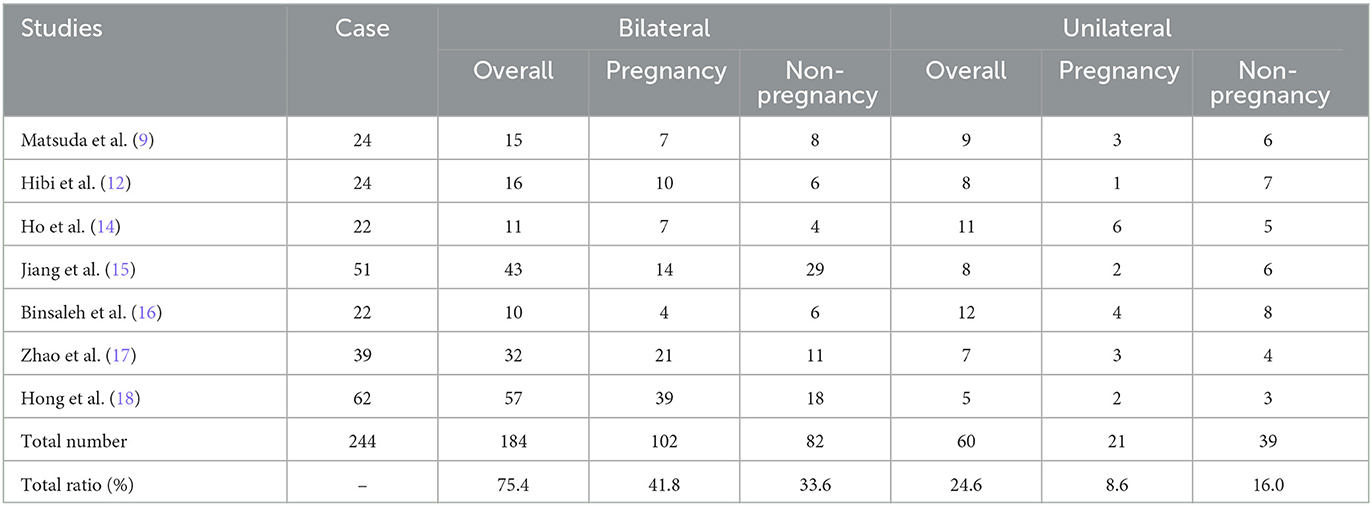
3.4. The results of the subgroup analysis
3.4.1. The overall patency rate of the vas deferens in different surgical procedures
A total of four clinical studies with end-to-side or end-to-end anastomosis (9–12) and six clinical studies with longitudinal or triangular intussusception (13–18) were included in the subgroup analysis. In this subgroup analysis, the random-effect models were uniformly presented as a high inter-study heterogeneity (P = 0.22 vs. 0.006, I2 = 33 vs. 69%, respectively). The results showed that the overall patency rates of the vas deferens after end-to-side or end-to-end anastomosis and longitudinal or triangular intussusception were 68% and 70% (95% CI 61–76 vs. 61–80%, P < 0.0001 vs. P < 0.0001, Figure 4A), respectively.
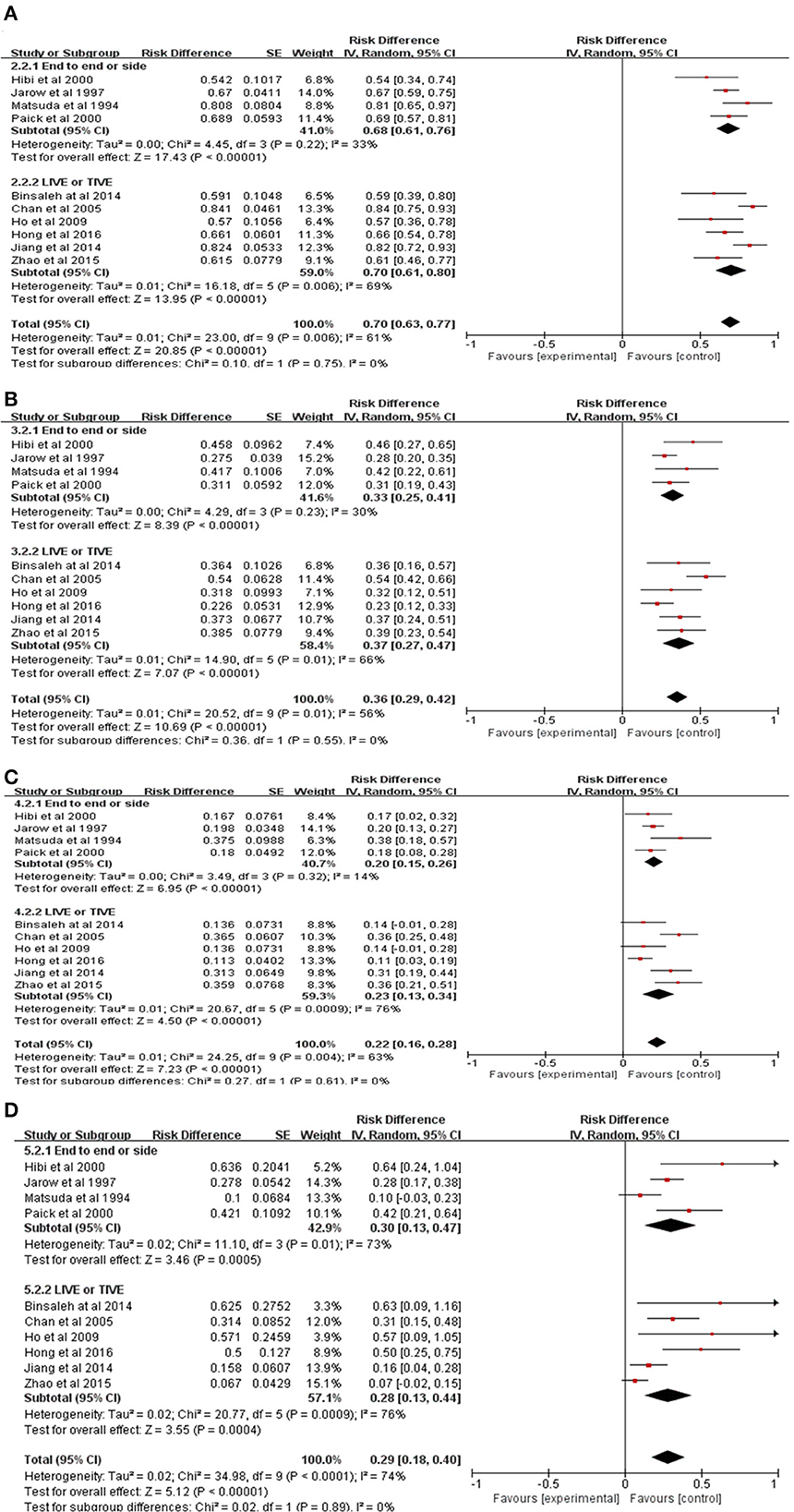
Figure 4. Subgroup meta-analysis of pregnancy outcomes in patients with EOA after MVE. (A) Subgroup meta-analysis of patency rate. (B) Subgroup meta-analysis of overall pregnancy rate. (C) Subgroup meta-analysis of natural pregnancy rate. (D) Subgroup meta-analysis of the ratio of pregnancy by ART.
3.4.2. The overall pregnancy rate in different surgical procedures
A total of four clinical studies with end-to-side or end-to-end anastomosis (9–12) and six clinical studies with longitudinal or triangular intussusception (13–18) were included in the subgroup analysis. In this subgroup analysis, the random-effect models were uniformly presented as a high inter-study heterogeneity (P = 0.23 vs. 0.01, I2 = 30 vs. 66%, respectively). The results showed that the overall pregnancy rates for the vas deferens after end-to-side or end-to-end anastomosis and longitudinal or triangular intussusception were 33% and 37% (95% CI 25–41 vs. 27–47%, P < 0.0001 vs. P < 0.0001, Figure 4B), respectively.
3.4.3. The natural pregnancy rate in different surgical procedures
A total of four clinical studies with end-to-side or end-to-end anastomosis (9–12) and six clinical studies with longitudinal or triangular intussusception (13–18) were included in the subgroup analysis. In this subgroup analysis, the random-effect models were uniformly presented as a high inter-study heterogeneity (P = 0.32 vs. 0.0009, I2 = 14 vs. 76%, respectively). The results showed that the natural pregnancy rates for the vas deferens after end-to-side or end-to-end anastomosis and longitudinal or triangular intussusception were 20% and 23% (95% CI 15–26 vs. 13–34%, P < 0.0001 vs. P < 0.0001, Figure 4C), respectively.
3.4.4. The ratio of pregnancy by ART in different surgical procedures
A total of four clinical studies with end-to-side or end-to-end anastomosis (9–12) and six clinical studies with longitudinal or triangular intussusception (13–18) were included in the subgroup analysis. In this subgroup analysis, the random-effect models were uniformly presented as a high inter-study heterogeneity (P = 0.01 vs. 0.0009, I2 = 73 vs. 76%), respectively. The results showed that the ratio of ART for the vas deferens after end-to-side or end-to-end anastomosis and longitudinal or triangular intussusception were 30% and 28% (95% CI 13–47 vs. 13–44%, P = 0.0005 vs. P = 0.0004, Figure 4D), respectively.
3.5. Publication bias test
The funnel plots analysis of publication bias revealed general symmetry, and Begg's test results indicated that there was no strong evidence of publication bias (Figures 5A–D).
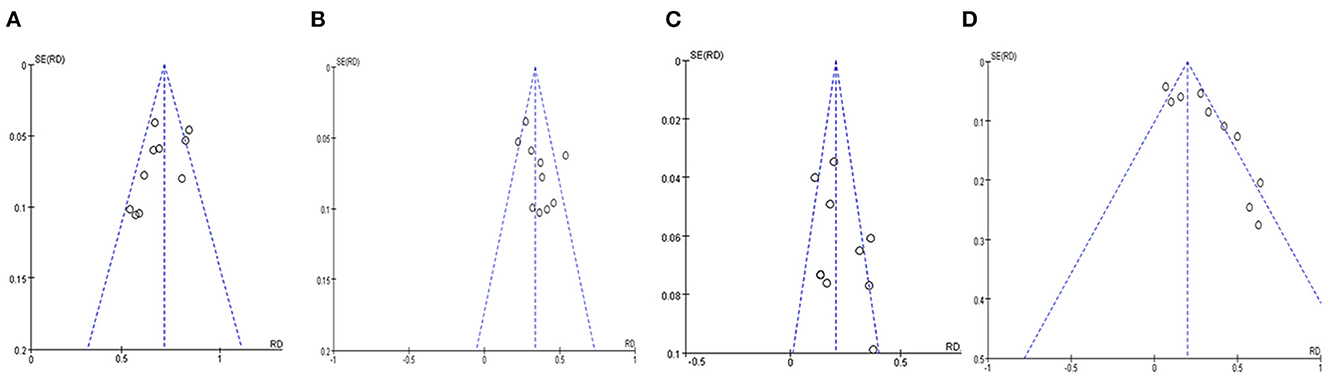
Figure 5. Funnel plots analysis for publication bias of pregnancy outcomes in patients with EOA after MVE. (A) Funnel plot of patency rate. (B) Funnel plot of overall pregnancy rate. (C) Funnel plot of natural pregnancy rate. (D) Funnel plot of the ratio of pregnancy by ART.
4. Discussion
Epididymal obstruction is the most common etiology of male infertility in patients with obstructive azoospermia (OA). Currently, assisted reproductive technology (ART), such as intracervical insemination (ICI), intrauterine insemination (IUI), in vitro fertilization and embryo transfer (IVF-ET), micro-testicular sperm extraction, and intracytoplasmic sperm injection (ICSI), has an obvious therapeutic effect on male infertility. However, there is still part of patients with epididymal obstructive azoospermia (EOA) (4) performing microsurgical vasoepididymostomy (MVE) to achieve natural pregnancy (19) and avoid ICSI complications, including ovarian hyperstimulation syndrome (OHSS) and multiple pregnancies (20). Single-center studies (21, 22) found a higher patency rate in male infertility patients with EOA after MVE (48.0%-71.7%), which is consistent with our meta-analysis (72%, 95% CI 68–76%). Therefore, the MVE procedure could obviously improve the overall patency rate of the vas deferens in male infertility patients with EOA.
However, the natural pregnancy rate in male infertility patients with EOA after MVE did not significantly improve. The results of our meta-analysis showed that the natural pregnancy rate is 21%, but the pregnancy success rate of ICSI is ~45–65% (6). Therefore, many male infertility patients with EOA require ART, including ICSI, to improve the pregnancy success rate of the spouse after the MVE procedure (8). Our meta-analysis included 54 patients who received ART after MVE to achieve a successful pregnancy in their spouses. The ratio of ART after MVE was 32.9%, and the pregnancy success rate of their spouses improved to 34%. Meanwhile, the application of ART could improve the chance of pregnancy regardless of postoperative sperm parameters. Therefore, we recommended that male infertility patients with EOA should receive ART after MVE to improve the rate of successful pregnancy in their spouses, including ICSI.
For patients with EOA after MVE, ICSI has become the preferred ART treatment strategy to improve fertilization rates (23), identify sperm morphology, and make up for the defect of lower sperm quality which failed to satisfy the demand for IUI and IVF-ET (24). Microsurgical epididymal sperm aspiration (MESA) has a higher rate of mate pregnancy than testicular sperm extraction (TESE). Therefore, MESA is the preferred epididymal sperm extraction procedure for male infertility patients with EOA after MVE (25).
Several abnormal complications during MVE, failure of vasectomy patency, and sperm dysfunction due to surgical trauma (5) have led EOA patients to receive micro-testicular sperm extraction and ICSI to achieve pregnancy after MVE, increasing the financial burden and secondary surgical trauma (24). The fertilization rates, spousal pregnancy rates, and abortion rates of cryopreserved sperms after ICSI were not significantly different compared with testicular fresh sperms (26, 27). The sperm motility after MVE was lower than the normal range according to World Health Organization (WHO) 6th guidelines in our systematic review. Therefore, we recommended that sperms from EOA male infertility patients should be cryopreserved in intraoperative MVE for application in the subsequent ICSI treatment procedure.
Previous studies found that the mean patency rate and mean pregnancy rates for end-to-side or end-to-end anastomosis were 61.1% and 29.9%, respectively. In contrast, the data on longitudinal or triangular intussusception developed to 69.1% and 36.9%, respectively (19). However, our meta-analysis found no significant differences in the overall patency rate (68 vs. 70%), the overall pregnancy rate (33 vs. 37%), the natural pregnancy rate (20 vs. 23%), and the ratio of ART (30 vs. 28%) among the different MVE procedures for end-to-side or end-to-end anastomosis and longitudinal or triangular intussusception. Therefore, changing the MVE procedure alone did not improve the pregnancy outcomes.
According to Binsaleh et al. (16), the average cost of MVE for patients in Western countries is more than $6000–9000. While the average cost of MVE in the Guangdong-Hong Kong-Macao Greater Bay Area of China is nearly ¥12000, and the financial burden of secondary micro-testicular sperm extraction combined with ICSI is similar to intraoperative cryopreserved sperm (¥43000–50000 vs. ¥42000–48000), with the same pregnancy rate of the spouse (55.2%). Therefore, there is no additional financial burden for patients with MESA cryopreserved human sperms in intraoperative MVE.
This study has the following limitations: first, for a lack of adequate data in these 10 clinical studies, we did not evaluate the effect of a spouse's gestational age on pregnancy outcomes. Previous studies have revealed that the optimal gestational age was lower than 39 years, and the overall pregnancy rate decreased with the age of the spouse (28), while there are significant differences between the average gestational age and non-pregnant age (26.5 vs. 32.7) (17). Therefore, further extensive searches are needed to investigate the gestational age of the spouses. Second, we did not evaluate the pregnancy rate of those who received ART after MVE. Since the included literature did not contain all the information on ART after MVE, we performed a meta-analysis only on the ratio of patients with pregnancy by ART after MVE for these patients who achieved the final outcome of pregnancy. Therefore, more extensive systematic studies are needed to evaluate the pregnancy rate of ART after MVE. Next, for the lack of these patients' data from adolescence, we cannot evaluate the correlation between the duration of obstruction and pregnancy outcomes. Finally, due to the lack of a randomized controlled study (RCT), we conducted only single-group studies on pregnancy outcomes. Therefore, we planned to continue prospective or retrospective randomized controlled clinical studies on this topic.
5. Conclusion
Vasectomy patency rates are higher, but natural pregnancy rates are lower in EOA male infertility patients after MVE. Altering the MVE procedures alone does not significantly improve pregnancy outcomes, but ART after MVE could improve the chance of pregnancy regardless of sperm parameters. We recommended that human sperms from EOA male infertility patients should be cryopreserved during intraoperative MVE for application in the subsequent ICSI treatment procedure.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
XX and ZW contributed to the design and conception of the study, and the acquisition of data was performed by XW, CS, FL, and JZ. Analysis and interpretation of data were performed by ZW, XW, NL, and BJ. The manuscript was drafted by ZW, XW, and ST. The critical revision of the manuscript was performed by CS, FL, and ST. All authors approved the submitted and final versions.
Funding
This research was supported by the Seventh Affiliated Hospital project of Sun Yat-sen University (No. zsqylckyjj202020).
Acknowledgments
We thank Hongwei Wu and Wenyang Xiao for their help during the research and preparation of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1186729/full#supplementary-material
References
1. Minhas S, Bettocchi C, Boeri L, Capogrosso P, Carvalho J, Cilesiz NC, et al. European association of urology guidelines on male sexual and reproductive health: 2021 update on male infertility. Eur Urol. (2021) 80:603–20. doi: 10.1016/j.eururo.2021.08.014
2. Li P, Liu N, Zhi E, Yao C, Chen H, Tian R, et al. Vasal vessel-sparing microsurgical single-armed vasoepididymostomy to epididymal obstructive azoospermia: A retrospective control study. Andrologia. (2021) 53:e14133. doi: 10.1111/and.14133
3. Morin SJ, Hanson BM, Juneau CR, Neal SA, Landis JN, Scott RT, et al. A comparison of the relative efficiency of ICSI and extended culture with epididymal sperm versus testicular sperm in patients with obstructive azoospermia. Asian J Androl. (2020) 22:222–6. doi: 10.4103/aja.aja_58_19
4. Kumar R, Mukherjee S, Gupta NP. Intussusception vasoepididymostomy with longitudinal suture placement for idiopathic obstructive azoospermia. J Urol. (2010) 183:1489–92. doi: 10.1016/j.juro.2009.12.027
5. Shiraishi K, Matsuyama H. Outcomes of partial intussusception and endo-to-side vasoepididymostomy in men with epididymal obstructive azoospermia. Int J Urol. (2020) 27:1124–9. doi: 10.1111/iju.14368
7. Alharbi M, Almarzouq A, Zini A. Sperm retrieval and intracytoplasmic sperm injection outcomes with testicular sperm aspiration in men with severe oligozoospermia and cryptozoospermia. Can Urol Assoc J. (2021) 15:E272–5. doi: 10.5489/cuaj.6798
8. Namekawa T, Imamoto T, Kato M, Komiya A, Ichikawa T. Vasovasostomy and vasoepididymostomy: review of the procedures, outcomes, and predictors of patency and pregnancy over the last decade. Reprod Med Biol. (2018) 17:343–55. doi: 10.1002/rmb2.12207
9. Matsuda T, Horii Y, Muguruma K, Komatz Y, Yoshida O. Microsurgical epididymovasostomy for obstructive azoospermia: factors affecting postoperative fertility. Eur Urol. (1994) 26:322–6. doi: 10.1159/000475408
10. Jarow JP, Oates RD, Buch JP, Shaban SF, Sigman M. Effect of level of anastomosis and quality of intraepididymal sperm on the outcome of end-to-side epididymovasostomy. Urology. (1997) 49:590–5. doi: 10.1016/S0090-4295(97)80001-5
11. Paick JS, Hong SK, Yun JM, Kim SW. Microsurgical single tubular epididymovasostomy: assessment in the era of intracytoplasmic sperm injection. Fertil Steril. (2000) 74:920–4. doi: 10.1016/S0015-0282(00)01534-X
12. Hibi H, Yamada Y, Honda N, Fukatsu H, Katsuno S, Ohshima S, et al. Microsurgical vasoepididymostomy with sperm cryopreservation for future assisted reproduction. Int J Urol. (2000) 7:435–9. doi: 10.1046/j.1442-2042.2000.00226.x
13. Chan PT, Brandell RA, Goldstein M. Prospective analysis of outcomes after microsurgical intussusception vasoepididymostomy. Bju Int. (2005) 96:598–601. doi: 10.1111/j.1464-410X.2005.05691.x
14. Ho KL, Wong MH, Tam PC. Microsurgical vasoepididymostomy for obstructive azoospermia. Hong Kong Med J. (2009) 15:452–7.
15. Jiang HT, Yuan Q, Liu Y, Liu ZQ, Zhou ZY, Xiao KF, et al. Multiple advanced surgical techniques to treat acquired seminal duct obstruction. Asian J Androl. (2014) 16:912–6. doi: 10.4103/1008-682X.139256
16. Binsaleh S. Two-suture single-armed longitudinal intussusception vasoepididymostomy for obstructive azoospermia: report of patients characteristics and outcome. Int Urol Nephrol. (2014) 46:2271–7. doi: 10.1007/s11255-014-0835-6
17. Zhao L, Tu XA, Zhuang JT, Chen Y, Wang WW, Zeng LY, et al. Retrospective analysis of early outcomes after a single-armed suture technique for microsurgical intussusception vasoepididymostomy. Andrology-Us. (2015) 3:1150–3. doi: 10.1111/andr.12111
18. Hong K, Zhao LM, Xu SX, Tang WH, Mao JM, Liu DF, et al. Multiple factors affecting surgical outcomes and patency rates in use of single-armed two-suture microsurgical vasoepididymostomy: a single surgeon's experience with 81 patients. Asian J Androl. (2016) 18:129–33. doi: 10.1016/S1569-9056(16)60181-1
19. Yoon YE, Lee HH, Park SY, Moon HS, Kim DS, Song SH, et al. The role of vasoepididymostomy for treatment of obstructive azoospermia in the era of in vitro fertilization: a systematic review and meta-analysis. Asian J Androl.(2018)
20. Peng J, Yuan Y, Zhang Z, Cui W, Song W, Gao B. Microsurgical vasoepididymostomy is an effective treatment for azoospermic patients with epididymal obstruction and prior failure to achieve pregnancy by sperm retrieval with intracytoplasmic sperm injection. Hum Reprod. (2014) 29:1–7. doi: 10.1093/humrep/det385
21. Peng J, Yuan Y, Zhang Z, Gao B, Song W, Xin Z, et al. Patency rates of microsurgical vasoepididymostomy for patients with idiopathic obstructive azoospermia: a prospective analysis of factors associated with patency–single-center experience. Urology. (2012) 79:119–22. doi: 10.1016/j.urology.2011.09.034
22. Zhao L, Deng CH, Sun XZ, Chen Y, Wang WW, Zhao LY, et al. A modified single-armed technique for microsurgical vasoepididymostomy. Asian J Androl. (2013) 15:79–82. doi: 10.1038/aja.2012.100
23. Isikoglu M, Avci A, Kendirci CA, Aydinuraz B, Ata B. Conventional IVF revisited: Is ICSI better for non-male factor infertility? randomized controlled double blind study. J Gynecol Obstet Hum Reprod. (2021) 50:101990. doi: 10.1016/j.jogoh.2020.101990
24. Dubin JM, White J, Ory J, Ramasamy R. Vasectomy reversal vs. sperm retrieval with in vitro fertilization: a contemporary, comparative analysis. Fertil Steril. (2021) 115:1377–83. doi: 10.1016/j.fertnstert.2021.03.050
25. van Wely M, Barbey N, Meissner A, Repping S, Silber SJ. Live birth rates after MESA or TESE in men with obstructive azoospermia: is there a difference? Hum Reprod. (2015) 30:761–6. doi: 10.1093/humrep/dev032
26. Vernaeve V, Krikilion A, Verheyen G, Van Steirteghem A, Devroey P, Tournaye H. Outcome of testicular sperm recovery and ICSI in patients with non-obstructive azoospermia with a history of orchidopexy. Hum Reprod. (2004) 19:2307–12. doi: 10.1093/humrep/deh394
27. Verheyen G, Vernaeve V, Van Landuyt L, Tournaye H, Devroey P, Van Steirteghem A. Should diagnostic testicular sperm retrieval followed by cryopreservation for later ICSI be the procedure of choice for all patients with non-obstructive azoospermia? Hum Reprod. (2004) 19:2822–30. doi: 10.1093/humrep/deh490
Keywords: microsurgical vasoepididymostomy, epididymal obstructive azoospermia, assisted reproductive technology, patency rate, natural pregnancy, pregnancy outcome
Citation: Wang Z, Wang X, Song C, Lu F, Zhai J, Li N, Jiang B, Tan S and Xuan X (2023) The pregnancy outcomes in patients with epididymal obstructive azoospermia after microsurgical vasoepididymostomy: a systematic review and meta-analysis. Front. Med. 10:1186729. doi: 10.3389/fmed.2023.1186729
Received: 15 March 2023; Accepted: 24 April 2023;
Published: 18 May 2023.
Edited by:
Abraham A. Pouliakis, National and Kapodistrian University of Athens, GreeceReviewed by:
Dong Soo Park, CHA University, Republic of KoreaFrancesco Sessa, Careggi University Hospital, Italy
Yiming Yuan, Peking University, China
Copyright © 2023 Wang, Wang, Song, Lu, Zhai, Li, Jiang, Tan and Xuan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xujun Xuan, eHVhbnhqNUBtYWlsLnN5c3UuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
 Zilong Wang
Zilong Wang Xinkun Wang1†
Xinkun Wang1† Changze Song
Changze Song