
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Med., 11 December 2023
Sec. Gastroenterology
Volume 10 - 2023 | https://doi.org/10.3389/fmed.2023.1185482
This article is part of the Research TopicCurrent Trends of Minimally Invasive Therapy for CholecystocholedocholithiasisView all 5 articles
Background: Although the past decade has witnessed unprecedented medical progress, no consensus has been reached on the optimal approach for patients with acute cholecystitis. Herein, we conducted a systematic review and meta-analysis to assess the differences in patient outcomes between Early Laparoscopic Cholecystectomy (ELC) and Delayed Laparoscopic Cholecystectomy (DLC) in the treatment of acute cholecystitis. Our protocol was registered in the PROSPERO database (registration number: CRD42023389238).
Objectives: We sought to investigate the differences in efficacy, safety, and potential benefits between ELC and DLC in acute cholecystitis patients by conducting a systematic review and meta-analysis.
Methods: The online databases PubMed, Springer, and the Cochrane Library were searched for randomized controlled trials (RCTs) and retrospective studies published between Jan 1, 1999 and Jan 1, 2022.
Results: 21 RCTs and 13 retrospective studies with a total of 7,601 cases were included in this research. After a fixed-effects model was applied, the pooled analysis showed that DLC was associated with a significantly high conversion rate (OR: 0.6247; 95%CI: 0.5115–0.7630; z = −4.61, p < 0.0001) and incidence of postoperative complications (OR: 0.7548; 95%CI: 0.6197–0.9192; z = −2.80, p = 0.0051). However, after applying a random-effects model, ELC was associated with significantly shorter total hospitalization duration than DLC (MD: −4.0657; 95%CI: −5.0747 to −3.0566; z = −7.90, p < 0.0001).
Conclusion: ELC represents a safe and feasible approach for acute cholecystitis patients since it shortens hospitalization duration and decreases the incidence of postoperative complications of laparoscopic cholecystectomy.
Systematic review registration: https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=389238, identifier (CRD42023389238).
Laparoscopic Cholecystectomy (LC) represents the standard of care treatment for patients requiring a cholecystectomy (1, 2). Acute cholecystitis has long been considered unsuitable for immediate surgical treatment. However, with the significant progress achieved in minimally invasive technology, the number of patients undergoing early laparoscopic surgery has significantly escalated (3, 4). Nevertheless, no consensus has been reached on the optimal timing for surgery. It has long been thought that the risk of intraoperative conversion to laparotomy and intraoperative or postoperative complications was increased with early laparoscopic cholecystectomy (ELC) due to gallbladder congestion and edema, severe peripheral inflammatory reaction, and undefined anatomy of the Calot triangle (5–8). However, in recent years, with an improved knowledge of the etiology of the abovementioned complications and surgical method improvements, the incidence of intraoperative and postoperative complications has markedly decreased (9, 10). Compared to delayed laparoscopic cholecystectomy (DLC), ELC for acute cholecystitis reportedly decreases the operative complications and conversion rate and shortens the hospitalization duration (11–13). Nonetheless, the optimal timing for surgery remains subject to debate, emphasizing the need for further research.
Even though the superiority of ELC over DLC has been increasingly documented in the literature, most studies were based on relatively small populations (14–17). Accordingly, we comprehensively studied the current literature to determine the efficiency, safety profile, and potential benefits of ELC in contrast to DLC.
Literature was included in strict compliance with the PICOS principle. The target population consisted of “patients with acute cholecystitis,” the intervention was “LC,” the comparison was conducted between “ELC” and “DLC,” the outcomes consisted of “primary (conversion rate, intraoperative and postoperative complications) and secondary outcomes (Operation time, postoperative hospitalization duration and total hospitalization duration)” and the study design included “RCTs and retrospective studies.” The reporting principle of this meta-analysis complied with the Preferred Reporting Items for Systematic Review and meta-analysis (PRISMA) 2020 protocol and Meta-analysis of Observational Studies in Epidemiology (MOOSE) declaration (18, 19).
Our literature search was carried out in July of 2022 with no restriction to countries, type of publication or language utilized in the following electronic databases: PubMed and the Cochrane Library. The following MeSH terms and combinations were utilized to search the title, abstract and keyword sections: Early Laparoscopic Cholecystectomy OR Delay Laparoscopic Cholecystectomy AND acute cholecystitis AND complication AND timing.
All reports included in our study were randomized controlled trials (RCTs) or retrospective comparative studies (cohort or case–control studies) contrasted ELC to DLC irrespective of age, and analyzed at least one of our primary outcomes. During literature screening, the following were excluded: Animal experimental studies, case reports, letters to the editor and review articles.
The primary outcomes included intraoperative complication rate, postoperative complication rate and conversion rate. Intraoperative complications were common complications encountered during surgery, such as intraoperative bleeding, bile duct injury, and gallbladder perforation. In contrast, postoperative complications were defined as bleeding, wound infection, bile leakage, and so on (20, 21). Conversion was defined as open cholecystectomy performed when the anatomical structure around the gallbladder was unclear, pericholecystic inflammation was severe or intraoperative bleeding could not be controlled. The secondary outcomes were operative time (min), postoperative hospitalization duration (d) and total hospitalization duration (d). Comparative indicators included at least one primary outcome and one secondary outcome.
The Cochrane Collaboration’s tool was used for assessing the risk of bias of RCTs graded as “low,” “unclear” or “high risk” (22). The Newcastle-Ottawa Scale (NOS) was employed for the quality assessment of retrospective research based on criteria categorized into three dimensions: selection, comparability, and outcomes. A total score > 5 was associated with a low risk of bias (23).
R software Version 4.1.3 was used to perform the meta-analysis of included studies. For continuous data, “metacont” from “meta” package was used to pool the data, and “metabin” was used for binary data. The pooled results of continuous and binary data were compared using weighted mean difference (WMD) and Odds Ratio (OR), respectively. When I2 < 50%, we used a fixed-effects model for pooling WMD or OR and its 95% confidence interval. Otherwise, a random-effects model was selected. Heterogeneity among the studies was explored by using subgroup analysis and meta-regression. To assess the pooled results’ stability, the “metainf” function was utilized for sensitivity analysis. Finally, Egger’s test and funnel plots were used to indicate the publication bias. When Egger’s value of p<0.05, the trim-and-fill approach was used for funnel plot asymmetry adjustment.
861 studies were retrieved for a preliminary search in online databases PubMed, Springer, and Cochrane Library, according to the PRISMA2020 statement. After 827 non-eligible studies were excluded, ultimately, 34 studies were analyzed in this meta-analysis. The literature screening process is shown in Figure 1.
The risk of bias in the included retrospective studies was evaluated using the Newcastle-Ottawa Scale based on the following domains subject selection, comparability and outcomes. The total scoring of each retrospective study was more than 5 points (Table 1). The Cochrane bias risk assessment system was employed to assess the included RCTs (Figure 2). Overall, the literature quality assessment found a low risk of bias for all included studies.
After literature screening and quality assessment, 34 studies were included in this meta-analysis, including RCTs (n = 21) (12, 14, 34–52) and retrospective studies (n = 13) (4, 13, 15, 24–33). The definition of ELC and DLC in the included studies was different. For ELC cases, laparoscopic cholecystectomy timing after acute cholecystitis onset was less than 24 h (n = 6) (12, 25, 35, 40, 46, 48), 48 h (n = 3) (24, 29, 51), 72 h (n = 15) (15, 26, 30–33, 36, 39, 42, 43, 45, 47, 49, 50, 52), 4 days (n = 3) (4, 37, 41), 5 days (n = 1) (34), and 7 days (n = 3) (13, 28, 38). For the 3 remaining studies (14, 27, 44), the specific timing for ELC was not mentioned, and the authors just proposed performing laparoscopic cholecystectomy as early as possible. Regarding the definition of DLC, laparoscopic cholecystectomy timing after acute cholecystitis onset was set to more than 24 h (n = 1) (25), 48 h (n = 2) (24, 29), 72 h (n = 7) (15, 26, 30–32, 39, 42), 6 weeks (n = 14) (12, 27, 35, 36, 38, 40, 41, 44, 45, 47–50, 52), 12 weeks (n = 1) (43) and 15 weeks (n = 1) (34). In 7 studies (4, 13, 14, 28, 33, 46, 51), the timing ranged from 72 h to 6 weeks, while no mention of the specific timing for DLC was found in 1 study (37). The details of the studies included in our report are shown in Table 2.
I2 values less than 50% were obtained for the pooling conversion rate (I2 = 43%, τ2 = 0.2548, p = 0.01), intraoperative complications (I2 = 18.0%, τ2 = 0.2977, p = 0.28) and postoperative complications (I2 = 19.0%, τ2 < 0.0001, p = 0.17). Accordingly, we utilized a fixed-effects model to conduct the meta-analysis of primary outcomes. No significant differences in intraoperative complications were found between ELC and DLC (OR: 1.2616; 95%CI: 0.8998–1.7689; z = 1.35, p = 0.1778) (Figure 3B). However, compared with ELC, DLC associated with a high conversion rate (OR: 0.6247; 95%CI: 0.5115–0.7630; z = −4.61, p < 0.0001) (Figure 3A) and postoperative complication incidence (OR: 0.7548; 95%CI: 0.6197–0.9192; z = −2.80, p = 0.0051) (Figure 3C).
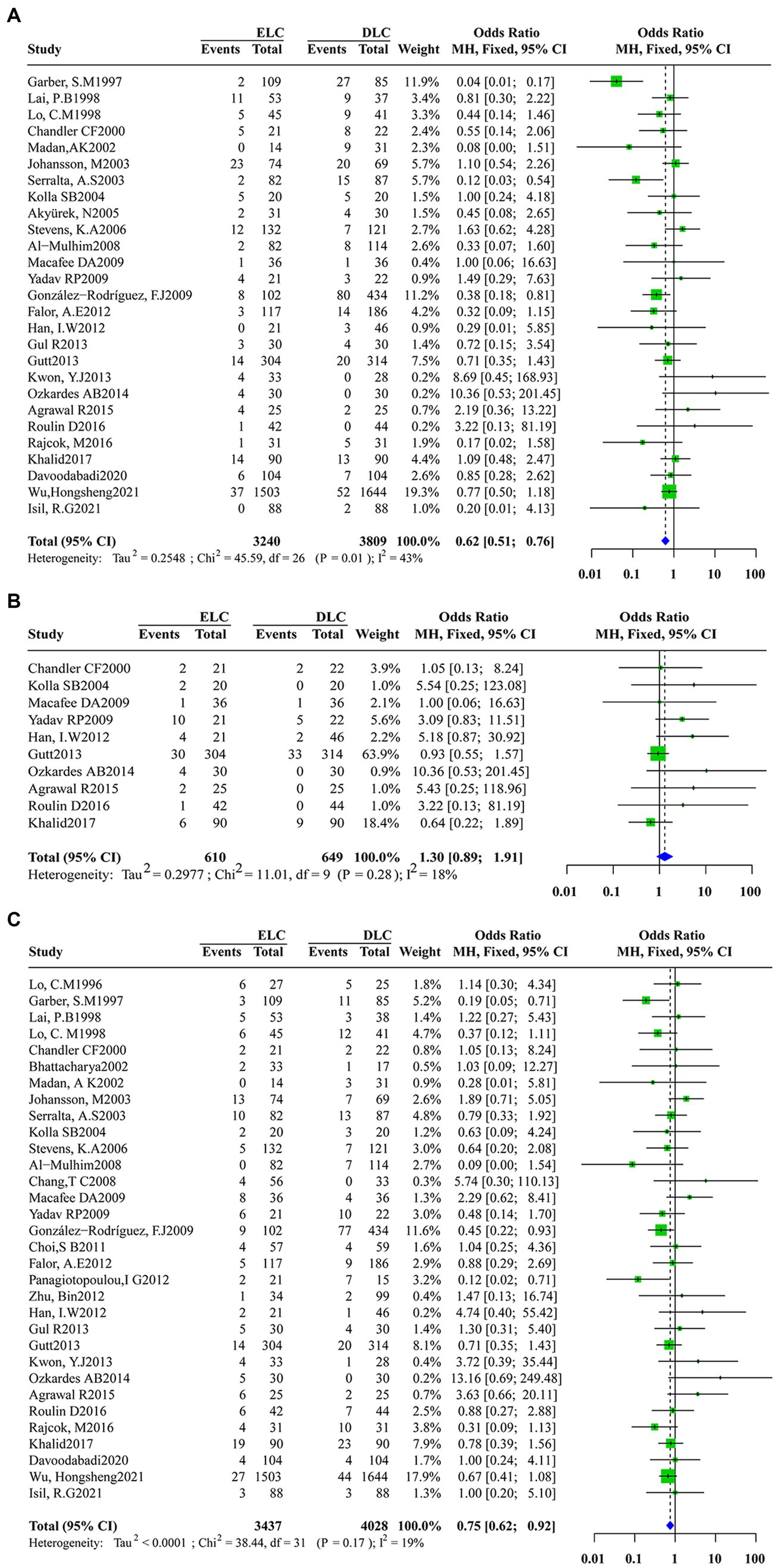
Figure 3. Forest plot of primary outcomes between ELC and DLC. (A).Conversion rate; (B).Intraoperative complications; (C).Postoperative complications. Green squares represent the point estimates of the treatment effect OR, with 95% CI indicated by horizontal bars. Blue diamonds represent the summary estimate from the pooled studies with 95% CI using common fixed models.
Significant heterogeneity was found among studies that assessed the secondary outcomes with I2 values above 50% obtained for the operation time (I2 = 96%, τ2 = 202.6737, p < 0.01), postoperative hospitalization duration (I2 = 98%, τ2 = 2.4357, p < 0.01) and total hospitalization duration (I2 = 98%,τ2 = 7.6196, p < 0.01). Accordingly, a random-effects model was applied for data synthesis. The pooled estimates revealed no marked differences in operation time (MD: 0.4594; 95%CI: −5.3527 to 6.2716; z = 0.16, p = 0.8769) (Figure 4A) and postoperative hospitalization duration (MD: -0.1088; 95%CI: −8.332 to 0.6157; z = −0.29, p = 0.7685) (Figure 4B) between ELC and DLC. In contrast, ELC was associated with significantly shorter total hospitalization duration than with DLC (MD: -4.0657; 95%CI:-5.0747 to −3.0566; z = −7.90, p < 0.0001) (Figure 4C).
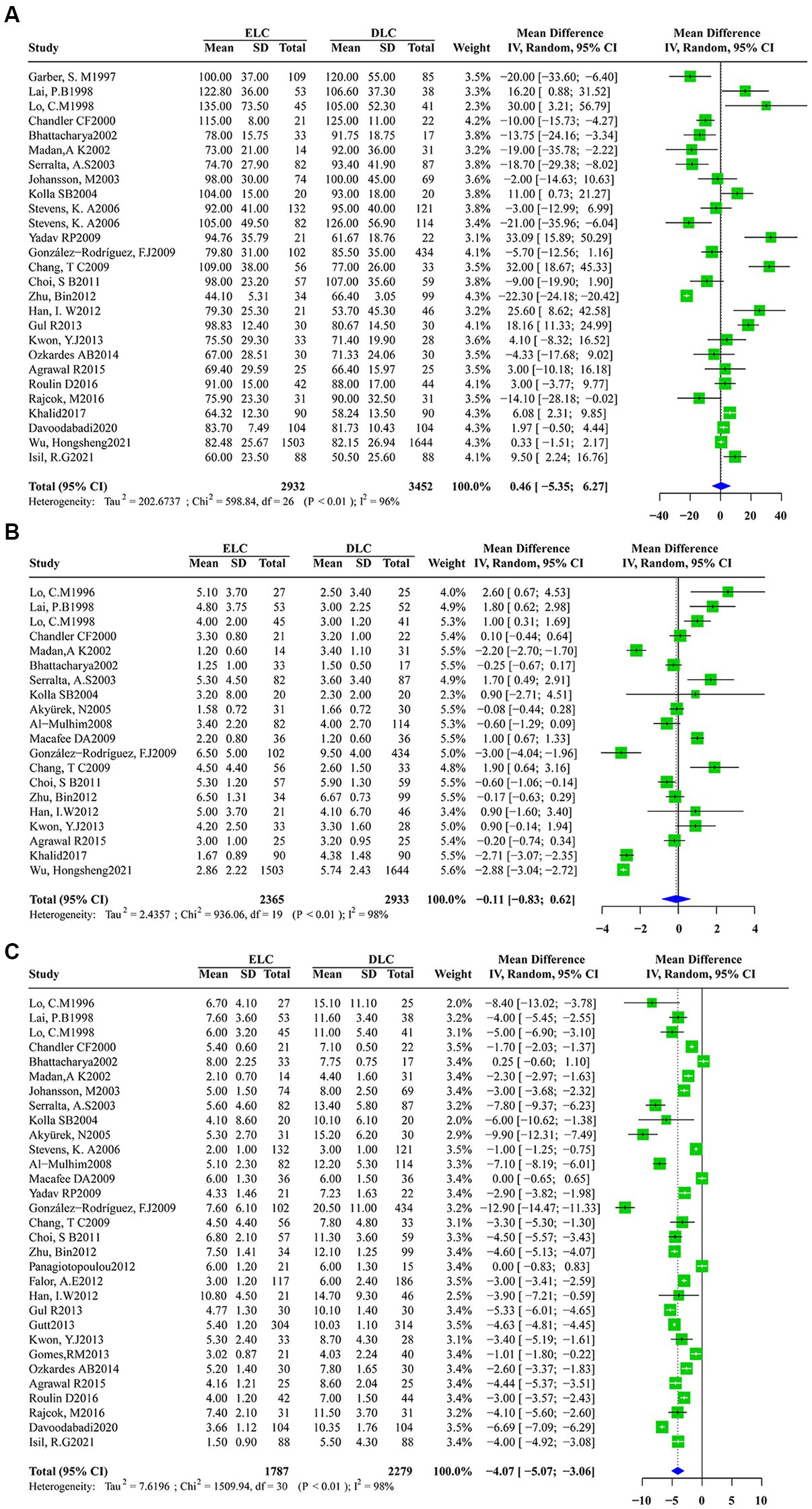
Figure 4. Forest plots of secondary outcomes between ELC and DLC. (A) Operation time; (B) Postoperative hospital stay duration; (C) Total hospital stay duration. Green squares represent the point estimates of the treatment effect OR, with 95% CI indicated by horizontal bars. Blue diamonds represent the summary estimate from the pooled studies with 95% CI using random effected models.
Given that significant heterogeneity was found in operation time, postoperative hospitalization duration and total hospitalization duration, subgroup analysis was conducted according to the study design (e.g., RCT or Retrospective research), location (e.g., Asia, America or Europe), ELC definition (e.g., Timing of laparoscopic cholecystectomy after the onset of acute cholecystitis less than 72 h or other definitions) and year of study (e.g., Studies before 2013 or since and after 2013). Subgroup analysis according to operation time indicated no significant significance between the subgroups in the study design (heterogeneity test: I2 = 96%,τ2 = 202.674, p < 0.01, random effect model: χ2 = 0.97, df = 1, p = 0.33) (Appendix 1), ELC definition (heterogeneity test: I2 = 96%,τ2 = 202.674, p < 0.01, random effect model: χ2 = 0.01, df = 1, p = 0.92) (Appendix 2) and year of study (heterogeneity test: I2 = 96%,τ2 = 202.674, p < 0.01, random effect model: χ2 = 0.80, df = 1, p = 0.37) (Appendix 3). However, after subgroup analysis according to location, compared with America and Europe, ELC was associated with longer operation time than DLC in Asia (heterogeneity test: I2 = 96%,τ2 = 202.674, p < 0.01, random effect model: χ2 = 18.65, df = 2, p < 0.01) (Figure 5). Subgroup analysis according to the total hospitalization duration revealed no significant differences between subgroups for the study design (heterogeneity test: I2 = 98%,τ2 = 7.6196, p < 0.01, random effect model: χ2 = 0.38, df = 1, p = 0.54) (Appendix 4), ELC definition (heterogeneity test: I2 = 98%,τ2 = 7.6196, p < 0.01, random effect model: χ2 = 0.96, df = 1, p = 0.33) (Appendix 5) and year of study (heterogeneity test: I2 = 98%,τ2 = 7.6196, p < 0.01, random effect model: χ2 = 0.07, df = 1, p = 0.79) (Appendix 6). However, ELC was associated with longer total hospitalization duration than DLC in Asia compared with America and Europe (heterogeneity test: I2 = 98%,τ2 = 7.6196, p < 0.01, random effect model: χ2 = 16.60, df = 2, p < 0.01) (Figure 6).
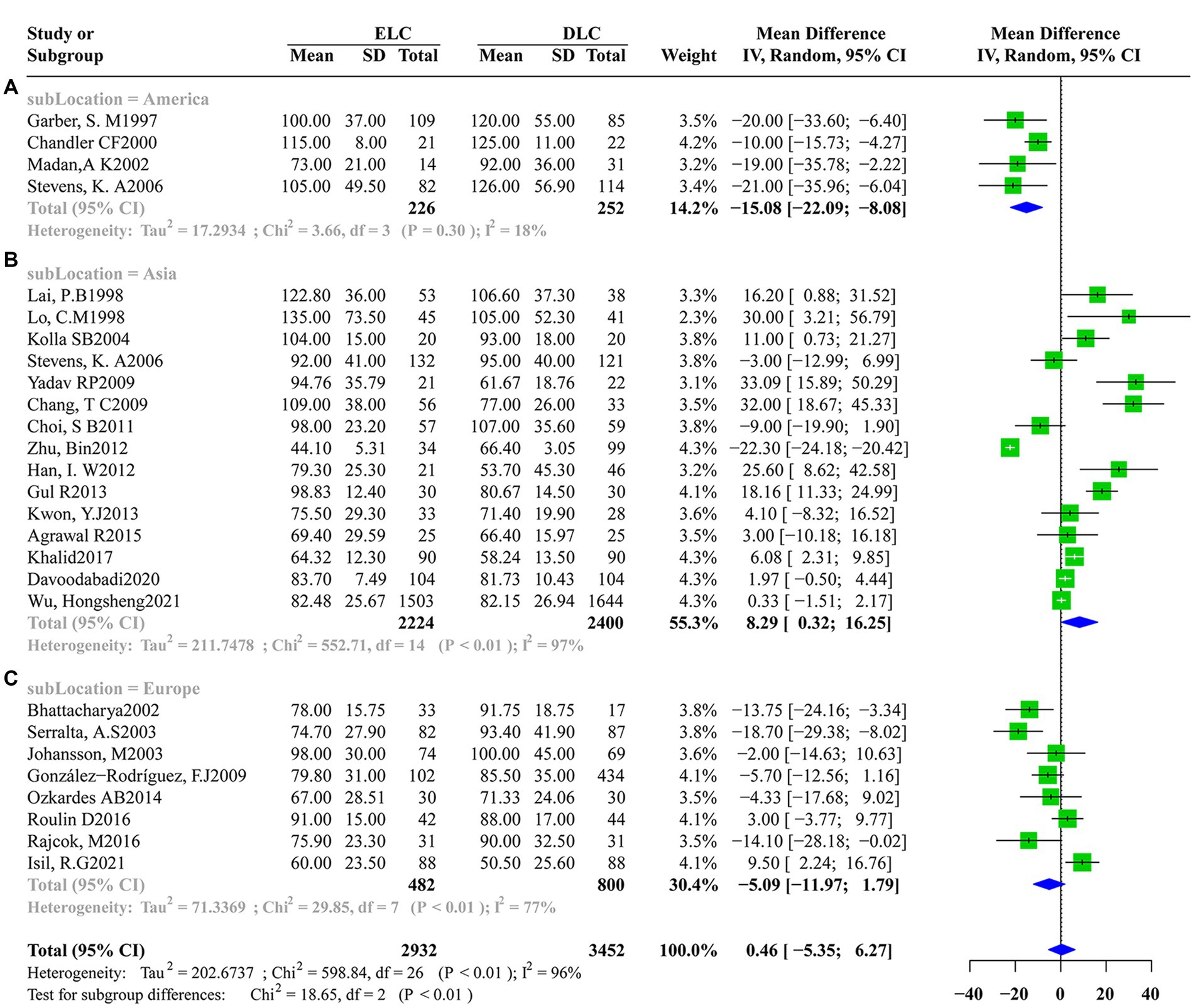
Figure 5. Subgroup analysis of location factors for operation time between ELC and DLC. (A) Subgroup for American population; (B) Subgroup for Asian population; (C) Subgroup for European population.
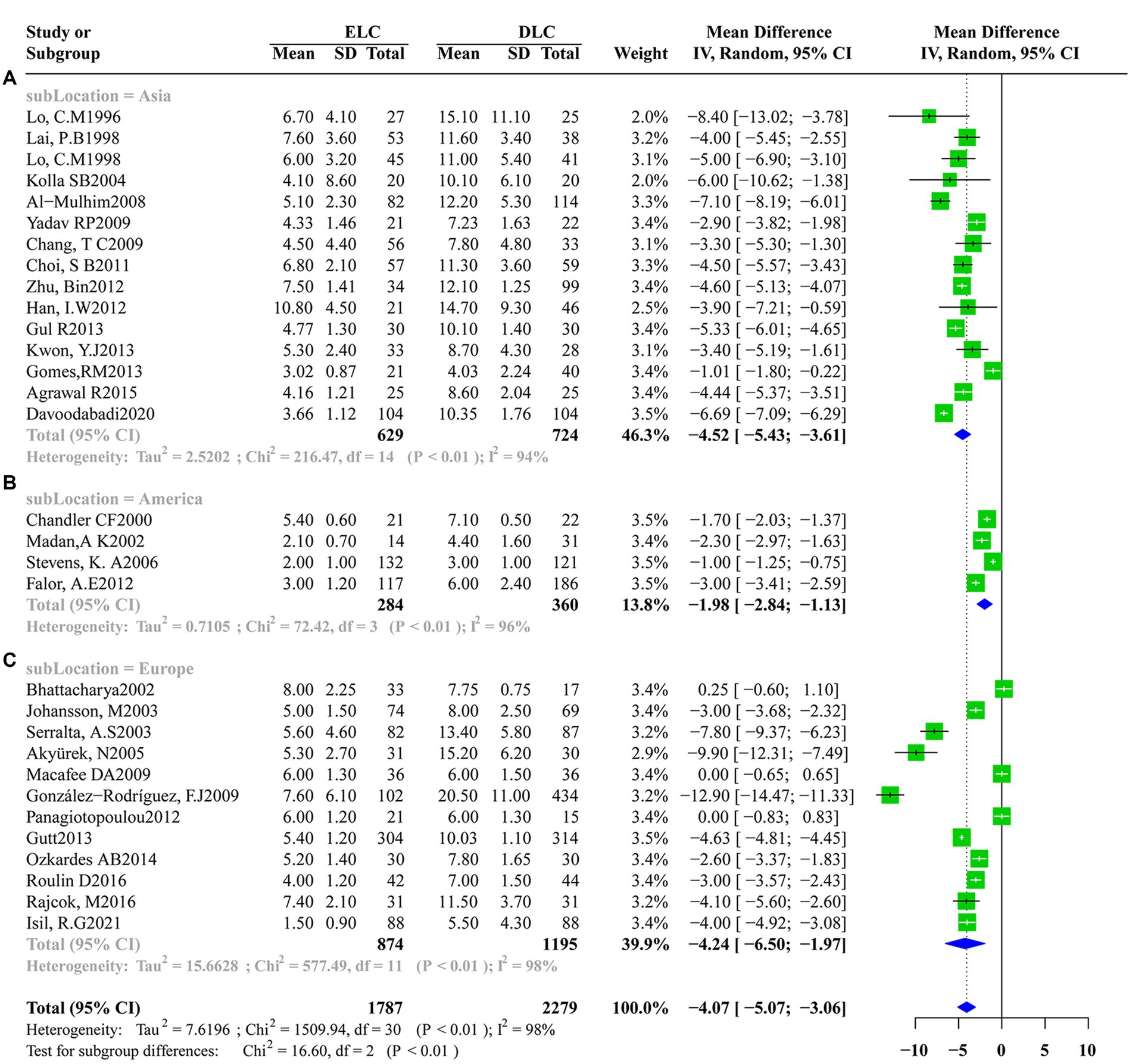
Figure 6. Subgroup analysis of location factors for total hospital stay duration between ELC and DLC. (A) Subgroup for Asian population; (B) Subgroup for American population; (C) Subgroup for European population.
Furthermore, we analyzed the heterogeneity source using a Meta-regression analysis, revealing that the operation time and location accounted for the heterogeneity among studies (z = 2.5294, 95%CI: 4.9790–39.2566, p = 0.0114), consistent with the results of subgroup analysis (Figure 7).
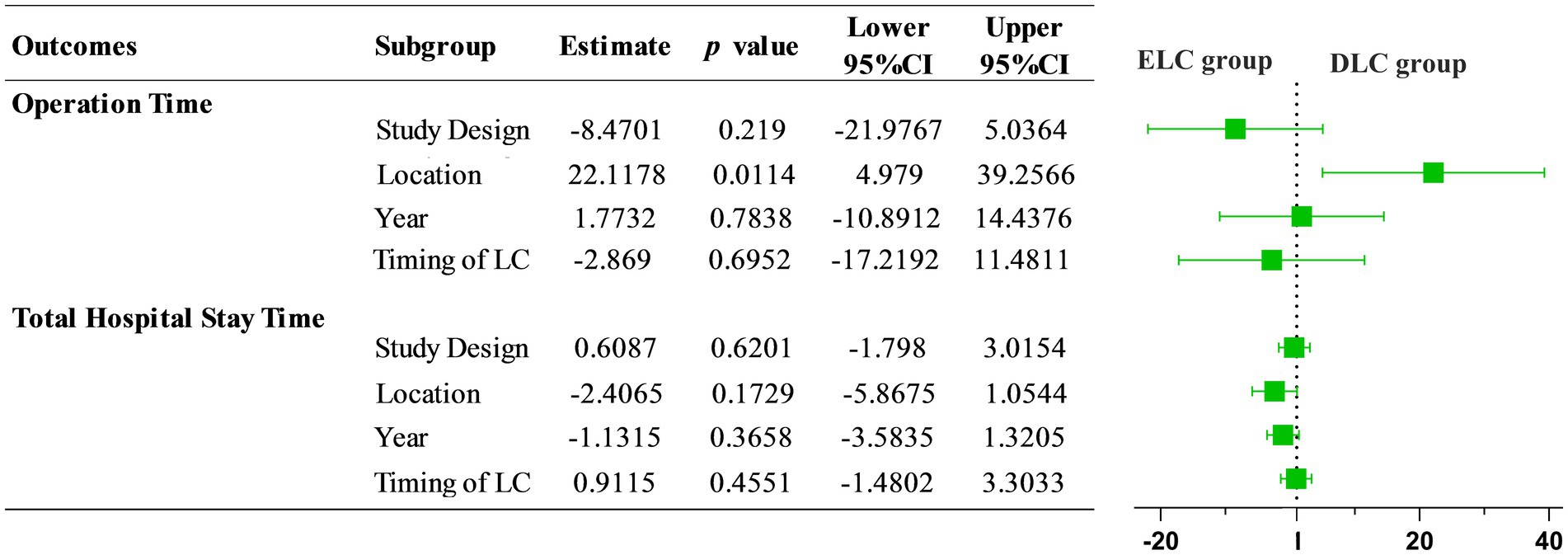
Figure 7. Meta regression of operation time and total hospital stay time between ELC and DLC. The results indicated that location factor was responsible for the source of heterogeneity with statistical significance (OR = 22.1178, 95%CI: 4.979–39.2566).
Since the first laparoscopic cholecystectomy was successfully performed in the late 1980s, minimally invasive surgery has been increasingly used to treat biliary tract diseases. Nowadays, LC has become the most common surgical approach for cholecystectomy. Due to the limitations of this new technology in the early days, laparoscopic cholecystectomy was not recommended for patients who suffered from acute cholecystitis due to the severe edema, the unclear anatomic structure of the Calot triangle, the uncontrollable bleeding around the gallbladder and the degree of surgeon’s experience (53–55). However, with the rapid development of laparoscopic technology and the refined understanding of intraoperative and postoperative complications of laparoscopic cholecystectomy, performing laparoscopic cholecystectomy for acute cholecystitis in the early period is no longer regarded as a contraindication (56, 57). Nevertheless, little is currently known about the optimal timing. Indeed, during the initial stages of acute cholecystitis, acute inflammatory reaction and edematous connective tissues impede the dissection of Calot’s triangle, contributing to reactive hyperemia and increase bleeding and bile duct injury during ELC. Accordingly, this may increase the operative time due to the severe inflammatory response in the early period of acute cholecystitis patients. Indeed, a longer operative time may increase the open surgery conversion rate and risk of biliary damage. On the other hand, patients that undergo DLC may benefit from a decreased conversion rate and risk of complications while prolonging hospitalization and increasing medical expenses (24, 58, 59).
Although several meta-analysis studies have compared ELC and DLC, they have some limitations. In this respect, Siddiqui et al. (60) and Gurusamy et al. (61) conducted studies based on a limited number of research and patients, suggesting significant bias in their studies. Complications of LC consist of intraoperative and postoperative complications. The most common intraoperative complications are bile duct injury, intraoperative bleeding, and conversion to open surgery. Bile duct injury is more serious and can be treated via T-tube placement. In cases of delayed diagnosis, ERCP may be performed after LC, but biliary stricture and recurrent biliary tract infection may occur. The most common postoperative complications are bile leak, wound site infection, and fluid collection around the gallbladder fossa. Bile leak may be the most serious among these, leading to acute peritonitis and septic shock. Current strategies to solve bile leakage include (1). Evaluation of the anatomical structure of the biliary tract; (2). For relatively small leaks, an indwelling abdominal tube should be placed for adequate drainage; (3). For relatively large leaks, a biliary stent may be inserted by ERCP (62, 63). Indeed, during the early stages of acute cholecystitis, gallbladder congestion, edema, brittle tissue bleeding and other factors may make laparoscopic dissection more challenging and constitute the main reason for conversion to laparotomy.
Our meta-analysis found that compared with ELC, DLC was associated with a high conversion rate and high postoperative complications with a fixed-effects model. However, the total hospitalization time in ELC was significantly shorter than in DLC when a random-effects model was utilized. In order to assess the heterogeneity in this meta-analysis, subgroup analysis and meta-regression were also employed, and both approaches indicated that regional factors accounted for the heterogeneity of this study. Subgroup analysis according to the operation time indicated that compared with Europe and America, a significantly longer operation time was observed for ELC patients in Asia, which suggested that acute inflammation and other factors during the early stage of acute cholecystitis were inclined to prolong the operation time in Asia (35, 36). During the subgroup analysis of hospitalization duration, we found that patients that underwent DLC in America correlated with shorter hospitalization than in Asia or Europe. The longest hospitalization duration was 7.10 ± 0.50 days (14) in America, which was shorter than in Asia (15.1 ± 11.1 days) (34) and Europe (20.5 ± 11.0 days) (26). This finding may account for the heterogeneity in our meta-analysis.
To investigate the stability and reliability of our findings, a sensitivity analysis was performed by removing one study each time. No study interfered with the results of this meta-analysis, substantiating the stability and reliability of our pooled estimates (Appendix 7). To analyze the possible presence of publication bias in this meta-analysis, we conducted an Egger’s test and generated funnel plots. Egger’s test showed that the funnel plots of intraoperative complications and postoperative hospital stay time were asymmetric. Next, we evaluated the impact of publication bias on the results by using the trim-and-fill method. It was found that with 4 added studies on intraoperative complications and 10 on postoperative hospitalization duration, there was no significant change in OR, WMD and their corresponding p values. Our funnel plot with filled-in data which was based on the trim-and-fill approach exhibited a symmetrical distribution (Figure 8).
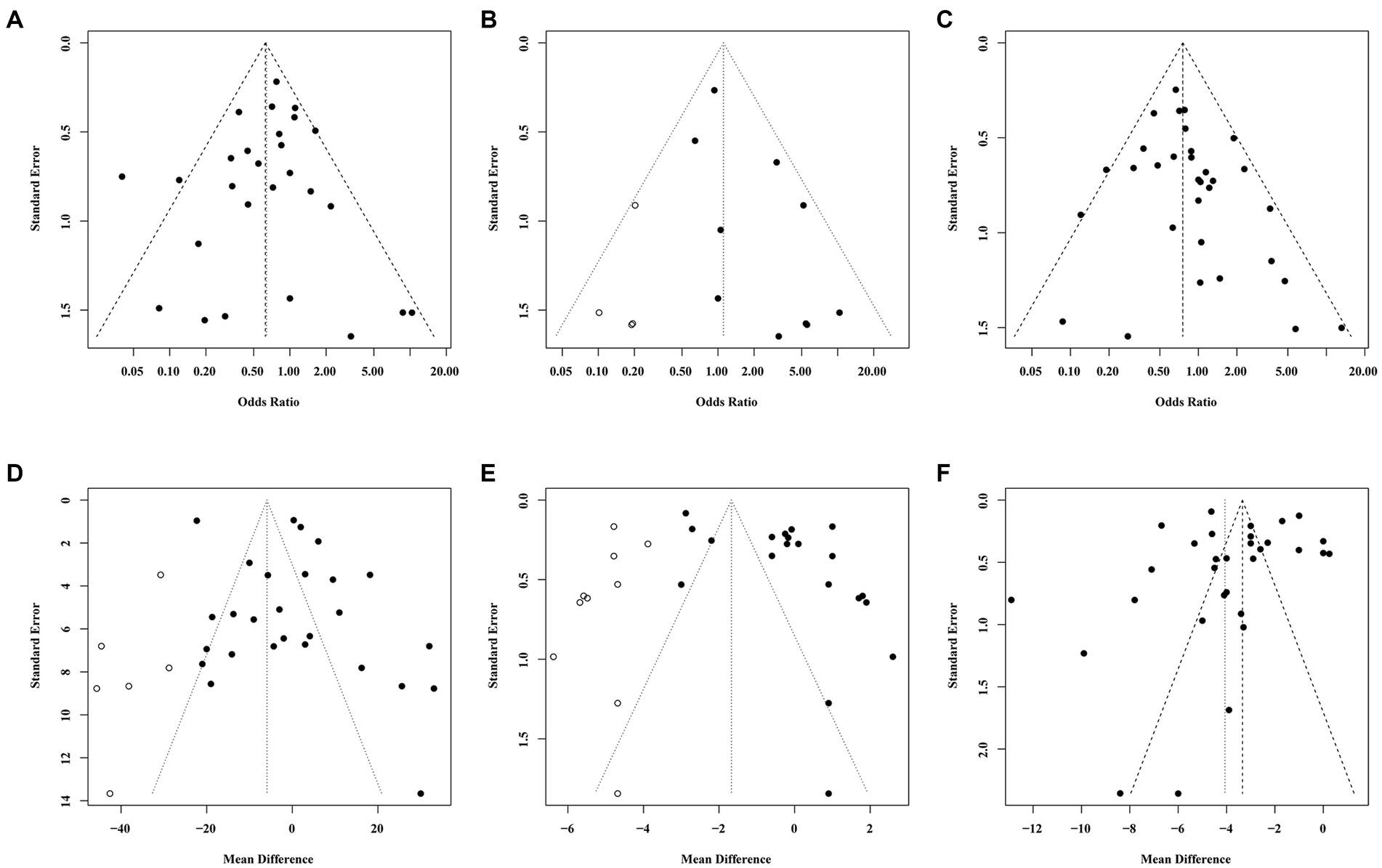
Figure 8. Funnel plots illustrated meta-analysis of primary and secondary outcomes. (A–C) represented the funnel plots of primary outcomes (A: Conversion rate; B: Intraoperative complications; C:Postoperative complications), the x-axis stood for odds ratio, while y-axis stood for standard error. (D–F) represented the funnel plots of secondary outcomes (D: Operation time; E: Postoperative hospital stay time; F: Total hospital stay time), the x-axis stood for mean difference while y-axis stood for standard error. Both funnel plots of B,D,E using trim-and-fill method, after filling studies indicated as hollow circle dots in the funnel plots, the funnel plot is basically symmetrical.
Several limitations found in this meta-analysis should be acknowledged. First, about one-third of the studies were retrospective studies, and the blinding method was not mentioned, which impacted the quality of included studies. Besides, studies from different locations accounted for the heterogeneity in this meta-analysis. Selecting uniform RCTs might reduce the heterogeneity, but it would increase the risk of bias. Moreover, for publication bias on intraoperative complications and postoperative hospital stay time, although the funnel plot with filled-in data based on the trim-and-fill approach exhibited a symmetrical distribution, other factors such as study design, exceeding positive results and greater weight mean difference may account for publication bias. Accordingly, more large-scale, high-quality RCTs are required in the future.
This meta-analysis revealed that compared with DLC, ELC was associated with a lower conversion rate and incidence of postoperative complications and shorter hospitalization duration for acute cholecystitis. ELC brings significant advantages in terms of safety profile and cost-effectiveness. Nevertheless, despite our rigorous methodology, some limitations were still unavoidable. Large-scale and high-quality RCTs with long follow-ups are warranted to validate the findings of this meta-analysis.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
HW and KM: study concept and design. TJ and JH: acquisition of data. HW and BL: statistical analysis and manuscript writing. TC and YL: generation of statistical figures. HW, BL, TC, TJ, JH, YL, and KM: final approval of manuscript. All authors contributed to the article and approved the submitted version.
This research was supported by the Internal Medicine Research Fund (Grant no 2020A01) and the Construction of Major Subject [Grant no (YNZDXK202201, 2022-2025)] of Affiliated Huadu Hospital, Southern Medical University.
We would like to thank the Internal Medicine Research Fund of Affiliated Huadu Hospital, Southern Medical University for their support.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1185482/full#supplementary-material
1. Campanile, FC, Pisano, M, Coccolini, F, Catena, F, Agresta, F, and Ansaloni, L. Acute cholecystitis: WSES position statement. World J Emerg Surg. (2014) 9:58. doi: 10.1186/1749-7922-9-58
2. Popkharitov, AI. Laparoscopic cholecystectomy for acute cholecystitis. Langenbeck's Arch Surg. (2008) 393:935–41. doi: 10.1007/s00423-008-0313-7
3. Wakabayashi, G, Iwashita, Y, Hibi, T, Takada, T, Strasberg, SM, Asbun, HJ, et al. Tokyo guidelines 2018: surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. (2018) 25:73–86. doi: 10.1002/jhbp.517
4. Garber, SM, Korman, J, Cosgrove, JM, and Cohen, JR. Early laparoscopic cholecystectomy for acute cholecystitis. Surg Endosc. (1997) 11:347–50. doi: 10.1007/s004649900360
5. Lee, W, and Kwon, J. Delayed laparoscopic cholecystectomy after more than 6 weeks on easily controlled cholecystitis patients. Korean. J Hepato-Biliary-Pancreat Surg. (2013) 17:60–5. doi: 10.14701/kjhbps.2013.17.2.60
6. Graves, HA, Ballinger, JF, and Anderson, WJ. Appraisal of laparoscopic cholecystectomy. Ann Surg. (1991) 213:655–64. doi: 10.1097/00000658-199106000-00017
7. Wilson, RG, Macintyre, IM, Nixon, SJ, Saunders, JH, Varma, JS, and King, PM. Laparoscopic cholecystectomy as a safe and effective treatment for severe acute cholecystitis. BMJ. (1992) 305:394–6. doi: 10.1136/bmj.305.6850.394
8. Kum, CK, Goh, PM, Isaac, JR, Tekant, Y, and Ngoi, SS. Laparoscopic cholecystectomy for acute cholecystitis. Br J Surg. (1994) 81:1651–4. doi: 10.1002/bjs.1800811130
9. Aziret, M, Karaman, K, Ercan, M, Vargol, E, Toka, B, Arslan, Y, et al. Early laparoscopic cholecystectomy is associated with less risk of complications after the removal of common bile duct stones by endoscopic retrograde cholangiopancreatography. Turk J Gastroenterol. (2019) 30:336–44. doi: 10.5152/tjg.2018.18272
10. Lo, HC, Wang, YC, Su, LT, and Hsieh, CH. Can early laparoscopic cholecystectomy be the optimal management of cholecystitis with gallbladder perforation? A single institute experience of 74 cases. Surg Endosc. (2012) 26:3301–6. doi: 10.1007/s00464-012-2344-y
11. Strobel, O, and Büchler, MW. Early laparoscopic cholecystectomy as therapy of choice for acute cholecystitis. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen. (2013) 84:999. doi: 10.1007/s00104-013-2633-6
12. Khalid, S, Iqbal, Z, and Bhatti, AA. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis. J Ayub Med Coll Abbottabad. (2017) 29:570–3.
13. Panagiotopoulou, IG, Carter, N, Lewis, MC, and Rao, S. Early laparoscopic cholecystectomy in a district general hospital: is it safe and feasible? Int J Evid Based Healthc. (2012) 10:112–6. doi: 10.1111/j.1744-1609.2012.00260.x
14. Chandler, CF, Lane, JS, Ferguson, P, Thompson, JE, and Ashley, SW. Prospective evaluation of early versus delayed laparoscopic cholecystectomy for treatment of acute cholecystitis. Am Surg. (2000) 66:896–900. doi: 10.1177/000313480006600921
15. Han, IW, Jang, JY, Kang, MJ, Lee, KB, Lee, SE, and Kim, SW. Early versus delayed laparoscopic cholecystectomy after percutaneous transhepatic gallbladder drainage. J Hepatobiliary Pancreat Sci. (2012) 19:187–93. doi: 10.1007/s00534-011-0458-6
16. Skouras, C, Jarral, O, Deshpande, R, Zografos, G, Habib, N, and Zacharakis, E. Is early laparoscopic cholecystectomy for acute cholecystitis preferable to delayed surgery?: best evidence topic (BET). International journal of surgery (London, England). (2012) 10:250–8. doi: 10.1016/j.ijsu.2012.04.012
17. Pisano, M, Ceresoli, M, Allegri, A, Belotti, E, Coccolini, F, Colombi, R, et al. Single center retrospective analysis of early vs. delayed treatment in acute calculous cholecystitis: application of a clinical pathway and an economic analysis. Ulusal travma ve acil cerrahi dergisi = Turkish journal of trauma & emergency surgery: TJTES. (2015) 21:373–9. doi: 10.5505/tjtes.2015.62679
18. Stroup, DF, Berlin, JA, Morton, SC, Olkin, I, Williamson, GD, Rennie, D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
19. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
20. Fletcher, E, Seabold, E, Herzing, K, Markert, R, Gans, A, and Ekeh, AP. Laparoscopic cholecystectomy in the acute care surgery model: risk factors for complications. Trauma Surg Acute Care Open. (2019) 4:e000312. doi: 10.1136/tsaco-2019-000312
21. Konstadoulakis, MM, Antonakis, PT, Karatzikos, G, Alexakis, N, and Leandros, E. Intraoperative findings and postoperative complications in laparoscopic cholecystectomy_ the Greek experience with 5,539 patients in a single center. J Laparoendosc Adv Surg Tech A. (2004) 14:31–6. doi: 10.1089/109264204322862333
22. DeMets, DL. Methods for combining randomized clinical trials_ strengths and limitations. Stats in Medicine. (1987) 6:341–8. doi: 10.1002/sim.4780060325
23. Lo, CK-L, Mertz, D, and Loeb, M. Newcastle-Ottawa scale: comparing reviewers' to authors' assessments. BMC Med Res Methodol. (2014) 14:45. doi: 10.1186/1471-2288-14-45
24. Madan, AK, Aliabadi-Wahle, S, Tesi, D, Flint, LM, and Steinberg, SM. How early is early laparoscopic treatment of acute cholecystitis. Am J Surg. (2002) 183:232–6. doi: 10.1016/S0002-9610(02)00789-4
25. Stevens, KA, Chi, A, Lucas, LC, Porter, JM, and Williams, MD. Immediate laparoscopic cholecystectomy for acute cholecystitis: no need to wait. Am J Surg. (2006) 192:756–61. doi: 10.1016/j.amjsurg.2006.08.040
26. González-Rodríguez, FJ, Paredes-Cotoré, JP, Pontón, C, Rojo, Y, Flores, E, Luis-Calo, ES, et al. Early or delayed laparoscopic cholecystectomy in acute cholecystitis conclusions of a controlled trial. Hepato-Gastroenterology. (2009) 56:11–6.
27. Chang, T-C, Lin, M-T, Wu, M-H, Wang, M-Y, and Lee, P-H. Evaluation of early versus delayed laparoscopic cholecystectomy in the treatment of acute cholecystitis. Hepato-Gastroenterology. (2009) 56:26–8.
28. Choi, SB, Han, HJ, Kim, CY, Kim, WB, Song, T-J, Suh, SO, et al. Early laparoscopic cholecystectomy is the appropriate management for acute gangrenous cholecystitis. Am Surg. (2011) 77:401–6. doi: 10.1177/000313481107700412
29. Falor, AE, de Virgilio, C, Stabile, BE, Kaji, AH, Caton, A, Kokubun, BA, et al. Early laparoscopic cholecystectomy for mild gallstone pancreatitis: time for a paradigm shift. Arch Surg. (2012) 147:1031–5. doi: 10.1001/archsurg.2012.1473
30. Zhu, B, Zhang, Z, Wang, Y, Gong, K, Lu, Y, and Zhang, N. Comparison of laparoscopic cholecystectomy for acute cholecystitis within and beyond 72 h of symptom onset during emergency admissions. World J Surg. (2012) 36:2654–8. doi: 10.1007/s00268-012-1709-7
31. Kwon, YJ, Ahn, BK, Park, HK, Lee, KS, and Lee, KG. What is the optimal time for laparoscopic cholecystectomy in gallbladder empyema? Surg Endosc. (2013) 27:3776–80. doi: 10.1007/s00464-013-2968-6
32. Gomes, RM, Mehta, NT, Varik, V, and Doctor, NH. No 72-hour pathological boundary for safe early laparoscopic cholecystectomy in acute cholecystitis: a clinicopathological study. Ann Gastroenterol. (2013) 26:340–5.
33. Wu, H, Ma, K, Yu, L, Gu, W, Yan, Y, Wang, B, et al. The timing of laparoscopic cholecystectomy and nano-ligation clip for acute calculous cholecystitis under guidance of Tokyo guidelines 2018 (multi-center retrospective analysis). Mater Express. (2021) 11:1681–90. doi: 10.1166/mex.2021.2085
34. Lo, CM, Liu, CL, Lai, EC, Fan, ST, and Wong, J. Early versus delayed laparoscopic cholecystectomy for treatment of acute cholecystitis. Ann Surg. (1996) 223:37–42. doi: 10.1097/00000658-199601000-00006
35. Lai, PB, Kwong, KH, Leung, KL, Kwok, SP, Chan, AC, Chung, SC, et al. Randomized trial of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg. (1998) 85:764–7. doi: 10.1046/j.1365-2168.1998.00708.x
36. Lo, CM, Liu, CL, Fan, ST, Lai, EC, and Wong, J. Prospective randomized study of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Ann Surg. (1998) 227:461–7. doi: 10.1097/00000658-199804000-00001
37. Bhattacharya, D, Senapati, PSP, Hurle, R, and Ammori, BJ. Urgent versus interval laparoscopic cholecystectomy for acute cholecystitis: a comparative study. J Hepato-Biliary-Pancreat Surg. (2002) 9:538–42. doi: 10.1007/s005340200070
38. Johansson, M, Thune, A, Blomqvist, A, Nelvin, L, and Lundell, L. Management of acute cholecystitis in the laparoscopic era_ results of a prospective, randomized clinical trial. J gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract. (2003) 7:642–5. doi: 10.1016/S1091-255X(03)00065-9
39. Serralta, AS, Bueno, JL, Planells, MR, and Rodero, DR. Prospective evaluation of emergency versus delayed laparoscopic cholecystectomy for early cholecystitis. Surg Laparosc Endosc Percutan Tech. (2003) 13:71–5. doi: 10.1097/00129689-200304000-00002
40. Kolla, SB, Aggarwal, S, Kumar, A, Kumar, R, Chumber, S, Parshad, R, et al. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a prospective randomized trial. Surg Endosc. (2004) 18:1323–7. doi: 10.1007/s00464-003-9230-6
41. Akyürek, N, Salman, B, Yüksel, O, Tezcaner, T, Irkörücü, O, Yücel, C, et al. Management of acute calculous cholecystitis in high-risk patients_ percutaneous cholecystotomy followed by early laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. (2005) 15:315–20. doi: 10.1097/01.sle.0000191619.02145.c0
42. Al-Mulhim, AA. Timing of early laparoscopic cholecystectomy for acute cholecystitis. JSLS: Journal of the Society of Laparoendoscopic Surgeons. (2008) 12:282–7.
43. Macafee, DA, Humes, DJ, Bouliotis, G, Beckingham, IJ, Whynes, DK, and Lobo, DN. Prospective randomized trial using cost-utility analysis of early versus delayed laparoscopic cholecystectomy for acute gallbladder disease. Br J Surg. (2009) 96:1031–40. doi: 10.1002/bjs.6685
44. Yadav, RP, Adhikary, S, Agrawal, CS, Bhattarai, B, Gupta, RK, and Ghimire, A. A comparative study of early vs. delayed laparoscopic cholecystectomy in acute cholecystitis. Kathmandu University medical journal (KUMJ). (2009) 7:16–20.
45. Gul, R, Dar, RA, Sheikh, RA, Salroo, NA, Matoo, AR, and Wani, SH. Comparison of early and delayed laparoscopic cholecystectomy for acute cholecystitis: experience from a single center. N Am J Med Sci. (2013) 5:414–8. doi: 10.4103/1947-2714.115783
46. Gutt, CN, Encke, J, Köninger, J, Harnoss, JC, Weigand, K, Kipfmüller, K, et al. Acute cholecystitis: early versus delayed cholecystectomy, a multicenter randomized trial (ACDC study, NCT00447304). Ann Surg. (2013) 258:385–93. doi: 10.1097/SLA.0b013e3182a1599b
47. Ozkardeş, AB, Tokaç, M, Dumlu, EG, Bozkurt, B, Ciftçi, AB, Yetişir, F, et al. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a prospective, randomized study. Int Surg. (2014) 99:56–61. doi: 10.9738/INTSURG-D-13-00068.1
48. Agrawal, R, Sood, KC, and Agarwal, B. Evaluation of early versus delayed laparoscopic cholecystectomy in acute cholecystitis. Surgery research and practice. (2015) 2015:349801:1–7. doi: 10.1155/2015/349801
49. Rajcok, M, Bak, V, Danihel, L, Kukucka, M, and Schnorrer, M. Early versus delayed laparoscopic cholecystectomy in treatment of acute cholecystitis. Bratislavske lekarske listy. (2016) 117:328–31. doi: 10.4149/BLL_2016_065
50. Roulin, D, Saadi, A, Di Mare, L, Demartines, N, and Halkic, N. Early versus delayed cholecystectomy for acute cholecystitis, are the 72 hours still the rule?: a randomized trial. Ann Surg. (2016) 264:717–22. doi: 10.1097/SLA.0000000000001886
51. Davoodabadi, A, Beigmohammadi, E, Gilasi, H, Arj, A, and Taheri, NH. Optimizing cholecystectomy time in moderate acute biliary pancreatitis: a randomized clinical trial study. Heliyon. (2020) 6:e03388. doi: 10.1016/j.heliyon.2020.e03388
52. Isil, RG, Yazici, P, Isil, CT, and Mihmanli, M. Does surgical experience really matter on the treatment approach to acute cholecystitis. A randomised clinical trial. Ann Ital Chir. (2021) 92:38–5.
53. Strasberg, SM, Sanabria, JR, and Clavien, PA. Complications of laparoscopic cholecystectomy. Can J Surg. (1992) 35:275–80.
55. Delaitre, B, Testas, P, Dubois, F, Mouret, P, Nouaille, JM, Suc, B, et al. Complications of cholecystectomy by laparoscopic approach. Apropos of 6512 cases. Chirurgie. (1992) 118
56. Kiviluoto, T, Sirén, J, Luukkonen, P, and Kivilaakso, E. Randomised trial of laparoscopic versus open cholecystectomy for acute and gangrenous cholecystitis. Lancet. (1998) 351:321–5. doi: 10.1016/S0140-6736(97)08447-X
57. Eldar, S, Sabo, E, Nash, E, Abrahamson, J, and Matter, I. Laparoscopic cholecystectomy for the various types of gallbladder inflammation: a prospective trial. Surg Laparosc Endosc. (1998) 8:200–7. doi: 10.1097/00019509-199806000-00008
58. Cameron, IC, Chadwick, C, Phillips, J, and Johnson, AG. Acute cholecystitis--room for improvement? Ann R Coll Surg Engl. (2002) 84:10–3.
59. Rattner, DW, Ferguson, C, and Warshaw, AL. Factors associated with successful laparoscopic cholecystectomy for acute cholecystitis. Ann Surg. (1993) 217:233–6. doi: 10.1097/00000658-199303000-00003
60. Siddiqui, T, MacDonald, A, Chong, PS, and Jenkins, JT. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a meta-analysis of randomized clinical trials. Am J Surg. (2008) 195:40–7. doi: 10.1016/j.amjsurg.2007.03.004
61. Gurusamy, K, Samraj, K, Gluud, C, Wilson, E, and Davidson, BR. Meta-analysis of randomized controlled trials on the safety and effectiveness of early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Br J Surg. (2010) 97:141–50. doi: 10.1002/bjs.6870
62. Karvonen, J, Gullichsen, R, Laine, S, Salminen, P, and Grönroos, JM. Bile duct injuries during laparoscopic cholecystectomy: primary and long-term results from a single institution. Surg Endosc. (2007) 21:1069–73. doi: 10.1007/s00464-007-9316-7
Keywords: ELC, DLC, acute cholecystitis, review, meta-analysis
Citation: Wu H, Liao B, Cao T, Ji T, Huang J, Luo Y and Ma K (2023) Comparison of the safety profile, conversion rate and hospitalization duration between early and delayed laparoscopic cholecystectomy for acute cholecystitis: a systematic review and meta-analysis. Front. Med. 10:1185482. doi: 10.3389/fmed.2023.1185482
Received: 13 March 2023; Accepted: 13 November 2023;
Published: 11 December 2023.
Edited by:
Riccardo Inchingolo, Ospedale Generale Regionale F. Miulli, ItalyReviewed by:
Maria Conticchio, Ospedale Generale Regionale Francesco Miulli, ItalyCopyright © 2023 Wu, Liao, Cao, Ji, Huang, Luo and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongsheng Wu, Y3Jhenl3dTIwMDdAMTI2LmNvbQ==; Keqiang Ma, bWtxOTkyOEBob3RtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.