- 1The First School of Clinical Medicine, Zhejiang Chinese Medical University, Hangzhou, China
- 2Department of Oncology, Guang' Anmen Hospital, China Academy of Chinese Medical Sciences, Beijing, China
- 3Department of Traditional Chinese Medicine, The Second People’s Hospital of Xiaoshan District, Hangzhou, China
- 4The First Affiliated Hospital of Zhejiang Chinese Medical University (Zhejiang Provincial Hospital of Chinese Medicine), Hangzhou, China
Aim: The objective of this study is to examine the correlation between patient serum cholinesterase (SCHE) concentration and weaning failure in the context of invasive mechanical ventilation (IMV), as well as to identify predictors of ventilator weaning failure. Additionally, this study investigates the potential relationship between SCHE and nutritional risk for developing more effective weaning strategies.
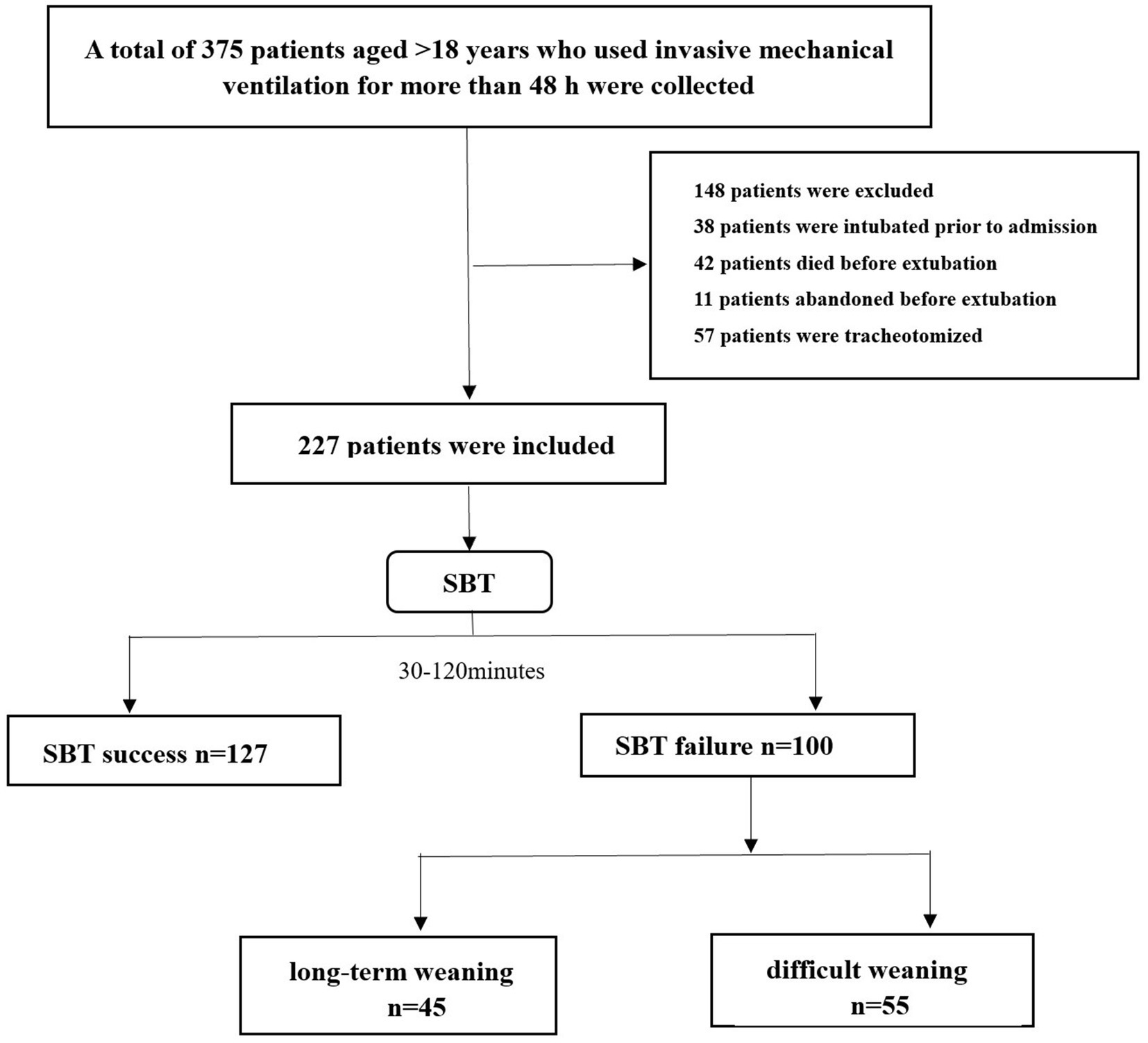
Method: A retrospective observational study was conducted. The sample was collected from 227 patients with IMV over 48 h who underwent SBT before weaning. Relevant experimental samples and data collection were analyzed at the time of patient admission and before the initiation of the SBT. The correlation between SCHE and weaning failure was determined by multifactorial logistic regression and propensity matching scores.
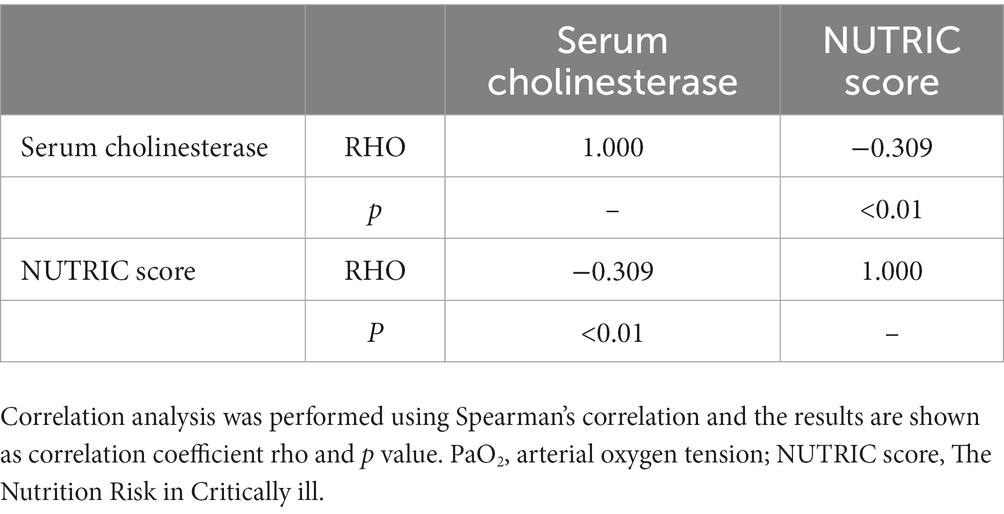
Results: Weaning was successful in 127 patients and failed in 100 patients. Depending on the difficulty of weaning, 55 of these patients had difficulty in weaning and 45 had long-term weaning. In the crude cohort, experimental data collected on the day of SBT showed that SCHE concentrations were higher in patients with successful weaning than in those with failed weaning (4,514 u/l vs. 3,190 u/l p < 0.01). The critical value for predicting weaning failure was SCHE 3,228 u/l (p < 0.01). Ventilator weaning failure was predicted by multifactorial logistic regression analysis of SCHE, heart rate, and PaO2 before SBT, with SCHE predicting ventilator weaning failure (AUC 0.714; 95% CI 0.647–0.782) better than heart rate (AUC 0.618; 95% CI 0.545–0.690), PaO2 (AUC 0.59; 95% CI 0.515–0.664). After propensity-matched scores, SCHE remained an independent predictor of weaning failure (p = 0.05). And the SCHE concentration was strongly correlated with the patient’s weaning difficulties (p < 0.01). The Nutrition Risk in Critically Ill (NUTRIC) score was also significantly correlated with SCHE according to Spearman’s correlation analysis (p < 0.01).
Conclusion: Our study revealed that the patients who experienced weaning failure exhibited lower SCHE values compared to those who successfully underwent weaning. Before spontaneous breathing trial (SBT), SCHE, heart rate, and PaO2 were identified as independent predictors of weaning failure. Following propensity score matching (PSM), SCHE and heart rate remained independent predictors. Patients with SCHE levels below 3,228 u/l should undergo careful evaluation before weaning. Our findings suggest that malnutrition may be a contributing factor to weaning failure in patients.
Introduction
In recent times, the utilization of Invasive Mechanical Ventilation(IMV) has become more prevalent, resulting in enhancing life safety for patients with acute and critical illnesses. Reports indicate that over one-third of patients admitted to the Intensive Care Unit (ICU) necessitate IMV for life-sustaining purposes (1). The weaning process is a crucial stage for mechanically ventilated patients, comprising two steps: discontinuing the ventilator and removing the tracheal intubation from the oral or nasal cavity. Therefore, it is imperative to establish an appropriate decannulation plan that involves the collaboration of all healthcare professionals. The SBT technique serves as a tool to aid clinicians in evaluating the potential risk of patient failure during the deconditioning process. This technique involves observing patients for a period of 0.5–2 h in a low-level supported spontaneous breathing mode or T-tube to determine their ability to breathe independently (2).
Several factors impact the outcomes of patient weaning, with respiratory muscle dysfunction (3), cardiac insufficiency (4), and malnutrition being the primary contributors (5). The nutritional status of patients is a significant determinant of successful weaning from mechanical ventilation. Patients receiving mechanical ventilation experience compromised nutrient absorption due to eating difficulties and disease management that disrupts gastrointestinal function. Additionally, chronic pain, inflammation, immobilization, and high catabolism render patients more susceptible to malnutrition (6). Malnourishment in patients results in heightened protein catabolism, insufficient energy provision, and unfavorable nitrogen balance, culminating in diminished respiratory muscle mass, potency, and stamina, as well as compromised ventilation. Furthermore, malnourishment impairs patients’ immune function and resistance, rendering mechanically ventilated patients more vulnerable to pulmonary infections and escalating weaning failure (7).
Given the negative impact of weaning failure on patients, the selection of an optimal time to initiate the weaning process and enhance the success rate of weaning has emerged as a critical research focus in the management of clinical use and therapeutic application of ventilators for ICU patients. The identification of appropriate weaning prediction parameters can assist clinicians in determining the appropriate timing for weaning, reducing the incidence of weaning failure, and improving patient outcomes. However, the conventional parameters utilized for weaning, such as blood oxygen saturation, brain natriuretic peptide, and shallow rapid breathing, may not provide adequate precision for predicting successful weaning due to their inherent limitations in clinical practice (8–10). Therefore, there is an urgent clinical need for predictors of offline success.
The human body generates two distinct types of cholinesterases, namely acetylcholinesterase, which is present in the brain, nerves, and red blood cells, and butyrylcholinesterase, a nonspecific cholinesterase which is present in the liver, pancreas, central nervous system, and blood. The measurement of serum butyrycholinesterase concentration is being utilized as a marker for cholinesterase levels. Prior research has established that a decreased concentration of this enzyme is linked to liver damage, inflammation, and malnourishment (11). During our regular clinical practice, we observed a potential correlation between abnormal SCHE concentrations and weaning outcomes in patients. As a result, the objective of this study was to identify predictive factors for ventilator weaning failure and to examine the relationship between low SCHE concentrations and weaning failure, while also evaluating the potential impact of low SCHE concentrations on weaning failure due to organismal malnutrition. This was accomplished by assessing the nutritional status of patients using the NUTRIC score.
Materials and methods
Patients and data collected
The study was conducted from January 2021 to September 2022 in the intensive care unit (ICU) of Zhejiang Hospital of Traditional Chinese Medicine, affiliated with Zhejiang University of Traditional Chinese Medicine, and retrospectively enrolled 227 adult patients treated with IMV for more than 48 h. Based on the sample content estimation formula for diagnostic tests, the minimum sample size was 90 cases. A sample size of 227 cases was included in this study, which met the minimum sample size inclusion requirement. Patients younger than 18 years of age; pregnancy; tracheotomy or other upper airway diseases; mechanical ventilation for less than 48 h; intubation before admission; abandonment before extubation; neuromuscular disease; lack of cooperation; the decision to limit active treatment and incomplete data were excluded for 148 individuals. Patients were considered ready to undergo an SBT when they fulfilled the criteria listed in the electronic Supplementary material. Demographic data, causes of IMV, the severity of illness scores, and nutritional scores were recorded at the time of ICU admission. Parameters related to blood gas analysis and ventilator mode on admission were also recorded. The duration of mechanical ventilation from the start of ventilator-assisted ventilation to the first SBT was recorded. As well as the results of vital signs, blood gas analysis, and SCHE before the start of the first SBT, and the score of the patient’s disease severity before the first SBT test.
Study protocol
This protocol has been approved by our institutional ethics committee to waive informed consent. Clinical and laboratory data were obtained for all patients at admission and before the first SBT trial (Figure 1, flowchart). SBT was performed with the patient in a semi-recumbent position, and oxygen was administered at concentrations prescribed by the attending physician through modalities such as reduced ventilator support or direct decompression. SBT lasted 30–120 min, depending on the patient’s tolerance or the physician’s decision. If the criteria for weaning failure were met, the patient was reconnected to mechanical ventilation; weaning was also considered a failure if reintubation was required within 48 h after SBT (12). According to the S2K guidelines published by the German Respiratory Society, we have divided the types of weaning into three categories (Table 1). Simple weaning group includes patients who successfully pass the first SBT and are extubated at the first attempt. Difficult weaning is defined as patients who require three SBT or up to 7 days from the first SBT to successfully wean. Prolonged weaning refers to patients with more than three SBT or >7 days of weaning after the first SBT (13, 14).
Sample collection and biomarker assays
All arterial and central venous blood gases were measured using a blood gas analyzer (ABL800, Radiometer, Copenhagen, Denmark). All arterial blood indices were measured using a fully automated five-classification blood count analyzer (BC-5180CRP, mindray, Shenzhen, China). SCHE concentrations were measured using a fully automated biochemical analyzer (AU5800, Beckman, Brea, United States).
Statistical analysis
For the comparison of categorical data described by frequencies and percentages, Chi-square (χ2) tests were performed. For continuous variables, the Kolmogorov–Smirnov test was used to test the normal distribution. For normally distributed data, the t-test was used and expressed as mean ± standard deviation. For non-normally distributed data the Mann–Whitney U test was used, expressed as the median (25th–75th percentile). To identify significant predictive markers of weaning failure, factors with p-values less than 0.05 in the univariate analysis were included in a multifactorial logistic regression model for analysis to obtain adjusted odds ratios (OR, 95% CI). Considering the differences in baseline characteristics between the successful and failed weaning groups, propensity score (PS) matching was used to identify cohorts of patients with similar baseline characteristics. Propensity scores were estimated using a non-parsimonious multivariable logistic-regression model with the weaning outcome as the independent variable and all baseline characteristics outlined in Tables 1, 2 as covariates. A propensity score (PS) was generated for each patient based on these variables. Patients with successful weaning and those with failed weaning were matched in a 1:1 ratio without replacement, using a caliper width of 0.02. A logistic regression model was rebuilt applying the matched patients to test the effect of each factor on weaning outcome. All analyses were two-tailed, and probability values (p values) less than 0.05 were considered statistically significant. We used receiver operating characteristic (ROC) analysis and diagnostic calibration curves to assess the predictive power of logistic regression models, as well as to observe the sensitivity and specificity of indicators such as SCHE in predicting weaning failure and to determine the optimal cut-off values for the diagnostic markers studied. Finally, Spearman’s correlation was used for correlation analysis of the SCHE and nutritional scores, with results expressed as rho and p values. Statistical analysis was performed using SPSS (Statistical Package for the Social Science; SPSS Inc., Chicago, IL, United States) version 25 from Microsoft Windows or R software (version 4.2.1).
Results
Baseline characteristics and weaning outcome
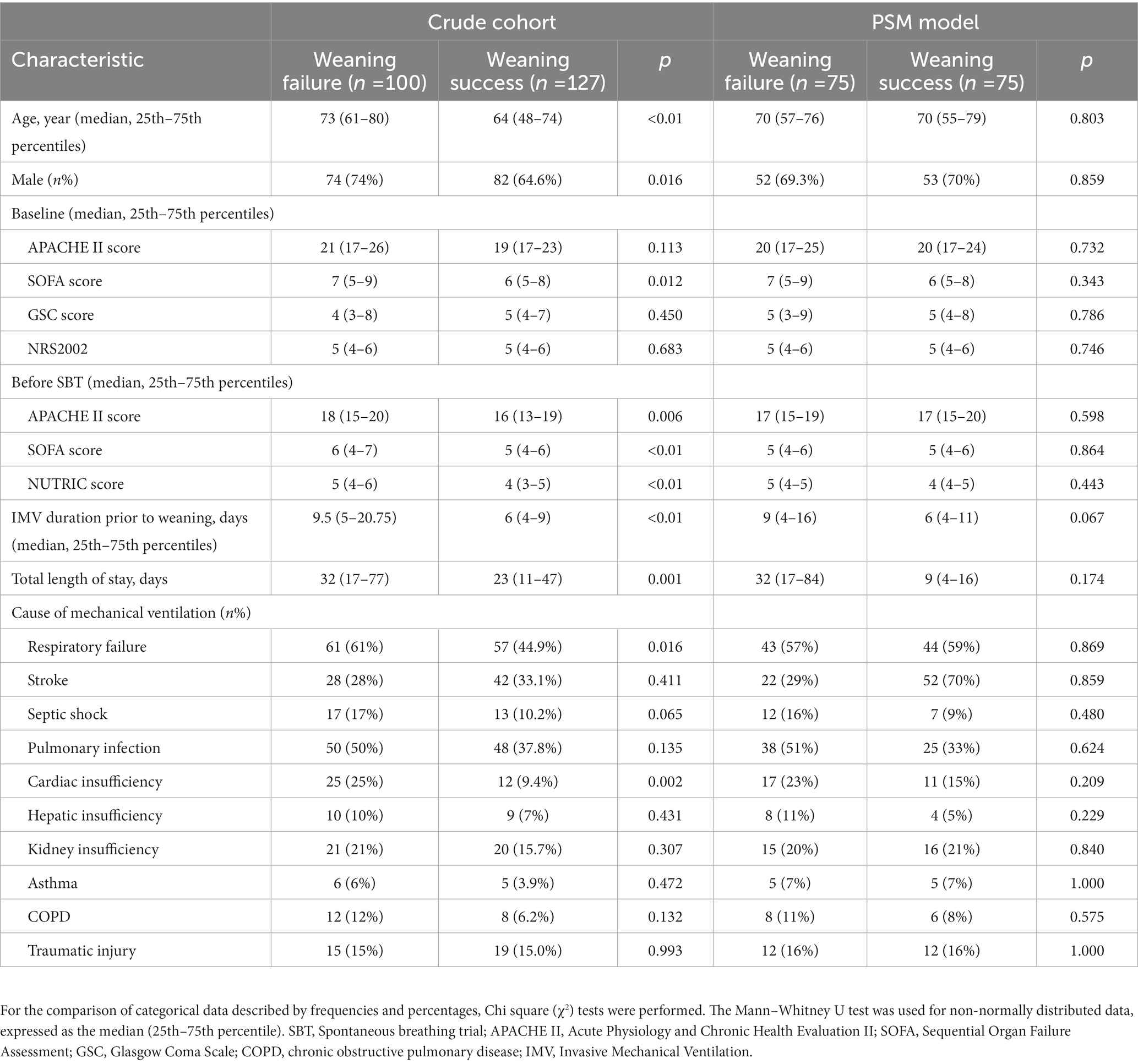
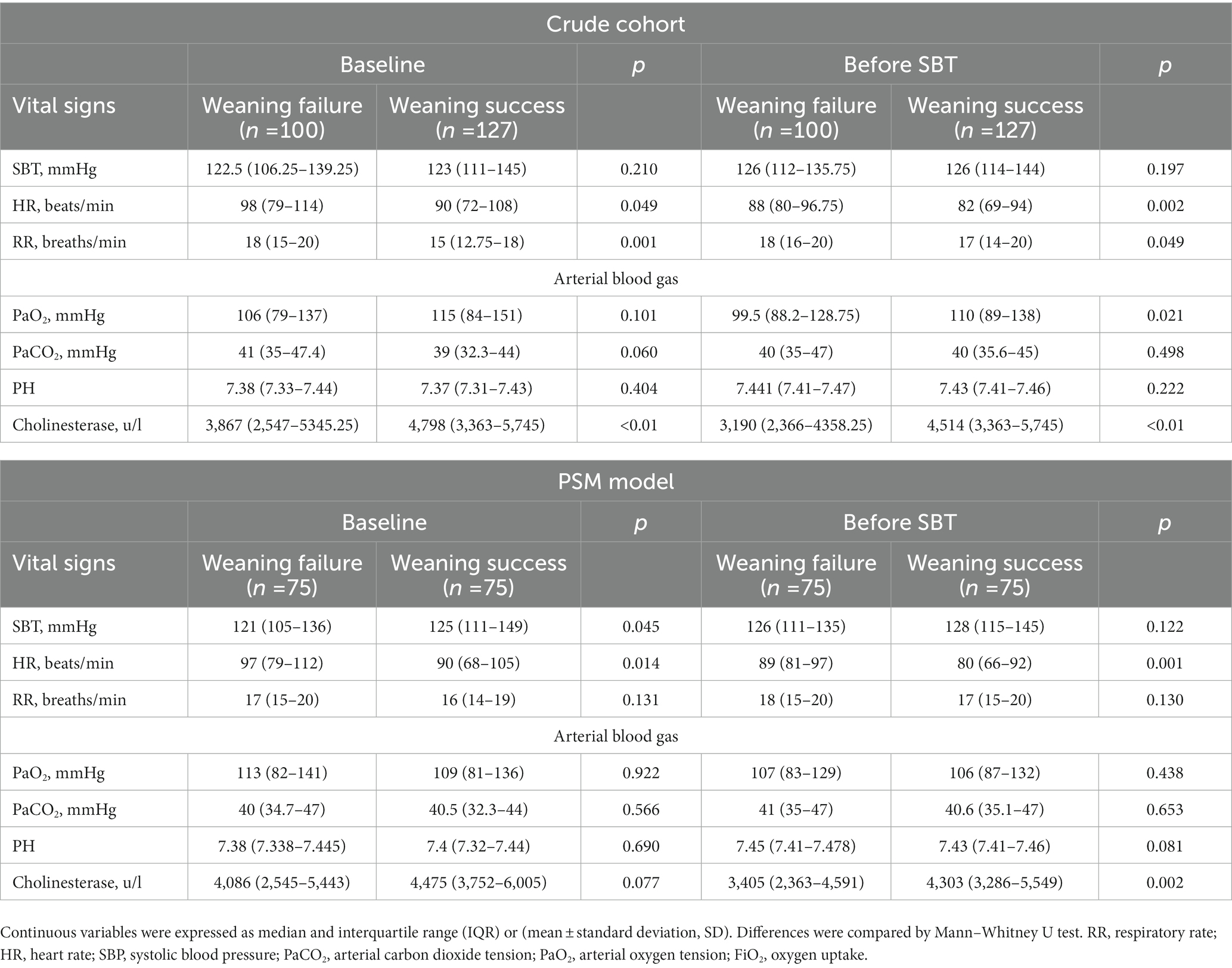
As shown in Figure 1, a total of 227 patients participated in this study. Of this total, 100 failed during weaning (94 failed SBT and 6 failed extubation after successful SBT) and 127 were eventually weaned successfully. The main causes of tracheal intubation are respiratory failure and stroke. Table 1 shows the baseline characteristics of all patients. Prior to propensity score matching, the failure group had a longer total length of stay and higher APACHE II and SOFA scores compared with those who successfully weaned; and lower GCS scores. There was a longer duration of IMV before weaning, higher APACHE II, SOFA scores, and nutrition scores, and significant differences in RR, PaO2, and FiO2 between the two groups. By using one-to-one propensity score matching (PSM), 150 patients with successful weaning were matched with 150 patients with failed weaning. After matching, there were no significant differences in p-values for most variables between the two groups indicating good propensity score matching. That is, there was only a small difference in baseline characteristics between the successful weaning and failure groups (Tables 1, 2).
Multifactorial logistic regression predicts indicators of weaning failure
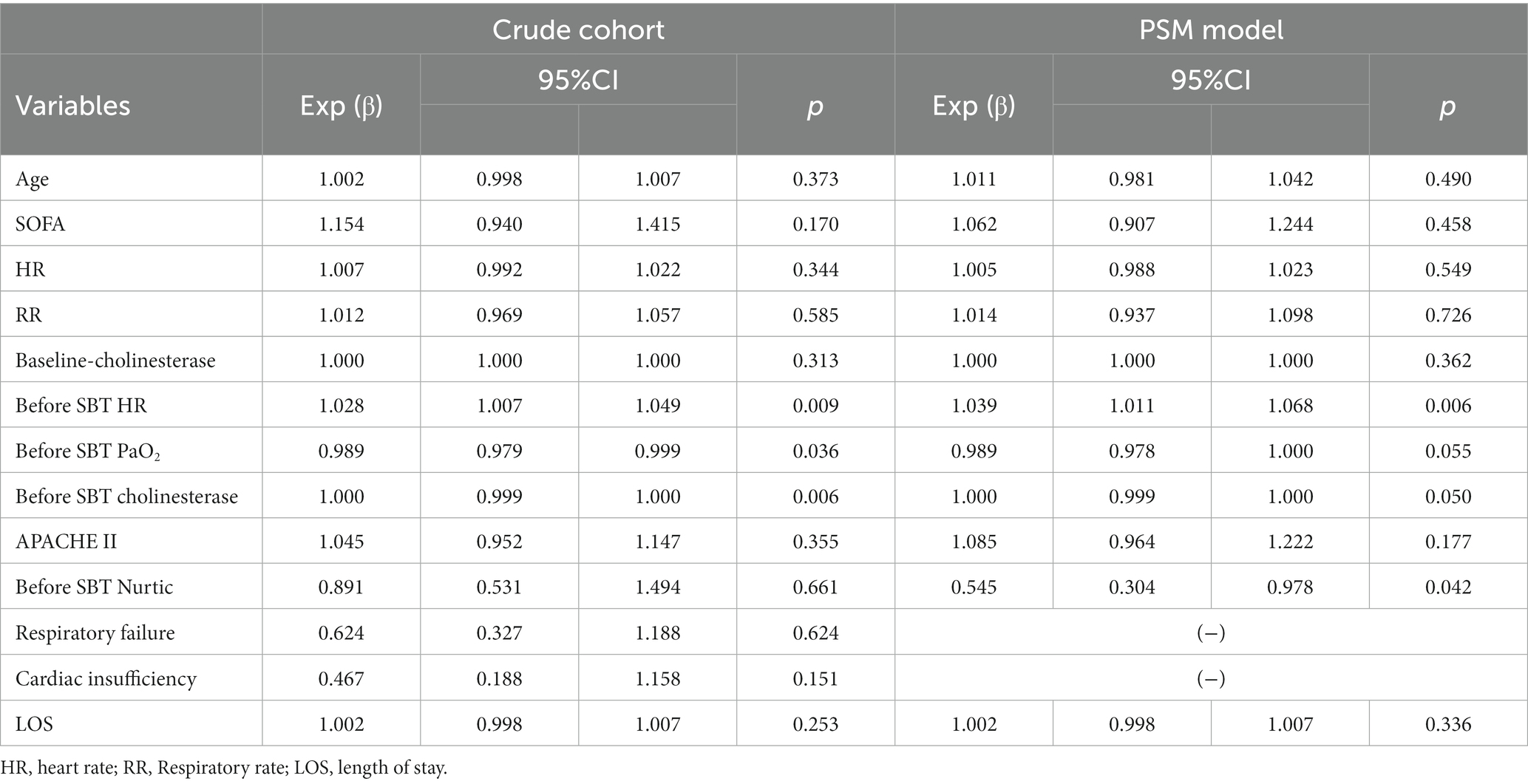
We used a multifactorial logistic regression model to assess the correlation between various factors and weaning events in the crude cohort and PSM model.
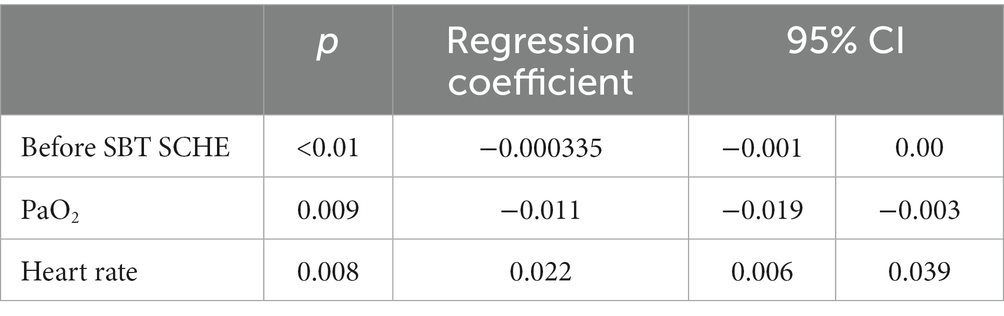
The findings of both the crude cohorts and the PSM model are shown in Table 3. In the crude model, before-SBT heart rate, PaO2, and SCHE were found to be independent predictors of weaning failure by multifactorial analysis (p = 0.009; p = 0.036; p = 0.006). In the propensity score model, before-SBT SCHE and heart rate remained independent predictors (p = 0.05; p = 0.006).
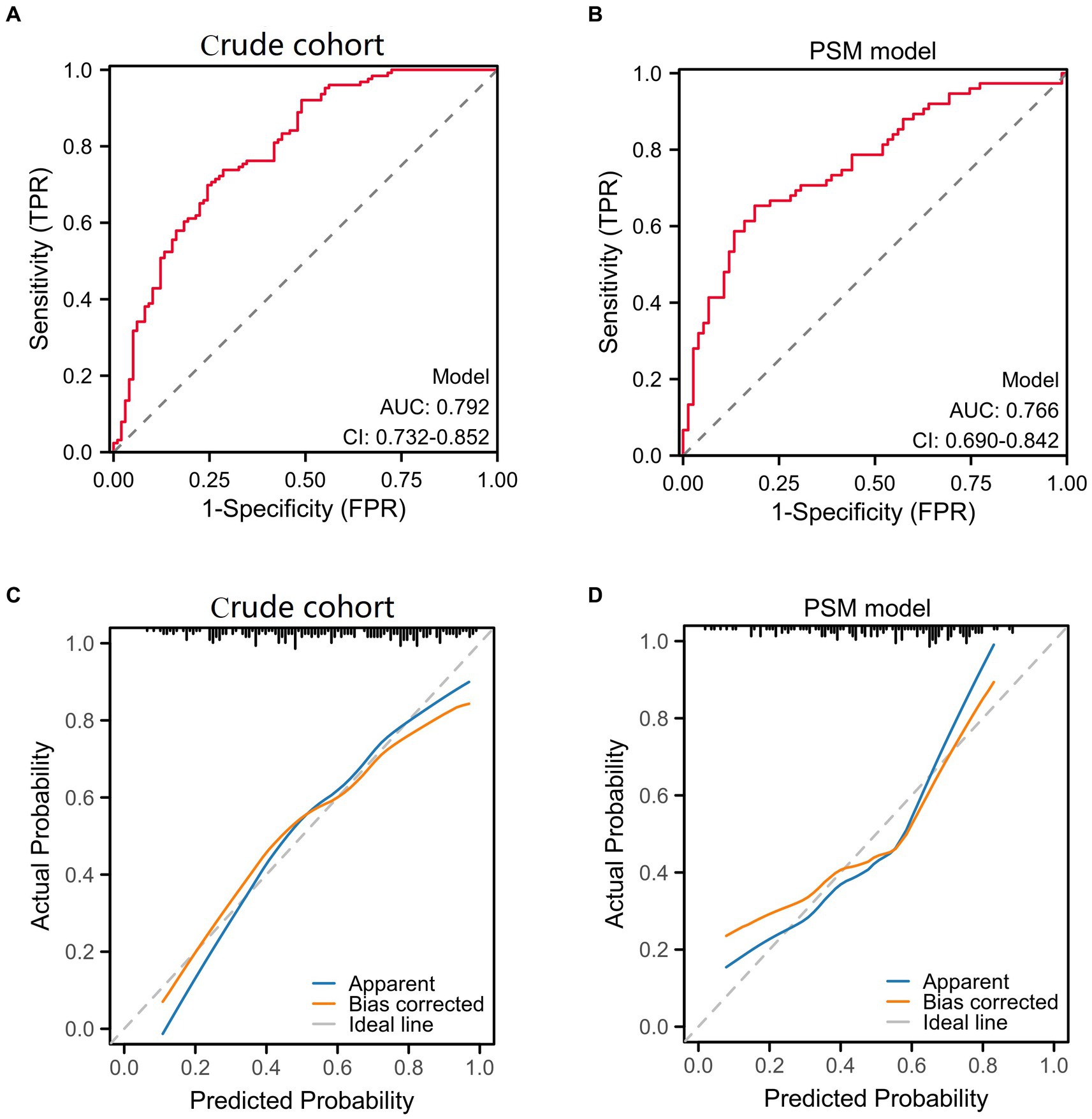
We used receiver operating characteristic (ROC) analysis and diagnostic calibration curves to assess the predictive power of logistic regression models. Figure 2 shows that the AUC for crude cohort (0.792; 95% CI 0.732–0.852) was higher than that for PSM model (0.766; 95% CI 0.690–0.842). The calibration curves for the crude cohort and PSM model showed no significant deviation from the reference line, The C-indexes were 0.792 and 0.766 for the crude cohort and PSM model indicating a relatively fair agreement between the PSM model predictions and crude cohort (Figure 2).
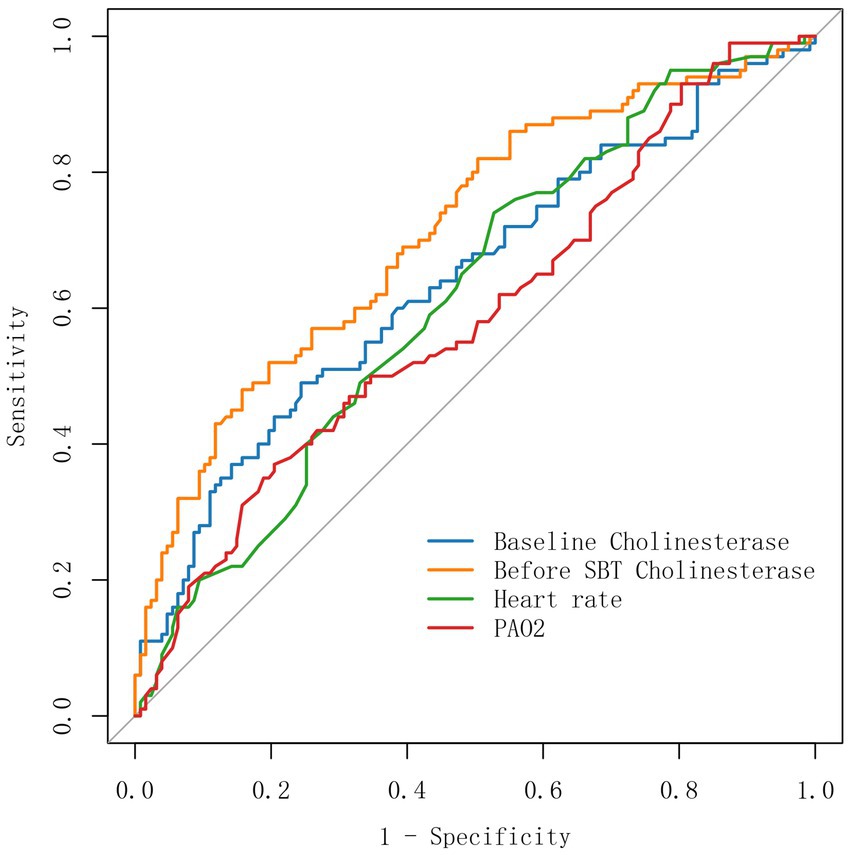
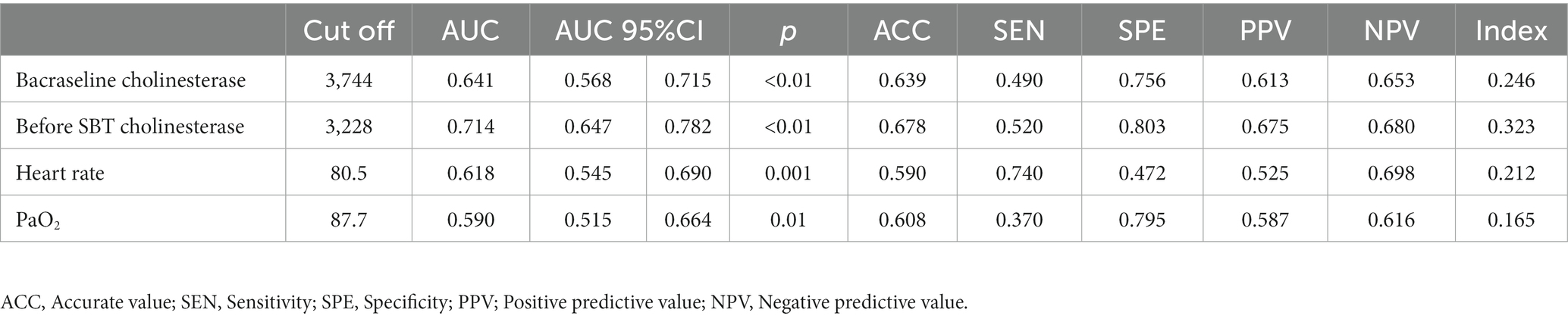
The performance of baseline SCHE, SCHE before SBT, heart rate, and PaO2 in predicting weaning failure was evaluated by calculating the area under the subject’s working characteristic curve (Figure 3 and Table 4). The optimal thresholds for predicting weaning failure were before SBT SCHE <3,228 u/l, baseline SCHE <3,744 u/l, heart rate >80.5 beats, and PaO2 <87.7 mmHg. Table 4 shows that the AUC for before-SBT SCHE (0.714; 95% CI 0.647–0.782) was higher than that for baseline SCHE (0.641; 95% CI 0.568–0.715) and heart rate (0.618; 95% CI 0.545). The diagnostic accuracy before SBT SCHE was the highest.
Weaning difficulty and SCHE concentration
According to the patients’ weaning condition, they were divided into two types: difficult weaning and long-term weaning, and long-term weaning was more difficult and severer than difficult weaning. Therefore, we performed a subgroup analysis to explore the correlation between SCHE concentration and patients’ weaning difficulty by ordered logistic regression (Table 5). The results showed that SCHE before SBT was strongly correlated with patients’ weaning difficulty (p < 0.01), and so does the heart rate and PaO2 before SBT (p = 0.009, p = 0.008). According to the regression coefficients, SCHE and PaO2 were negatively correlated with weaning difficulties, and heart rate was positively correlated with weaning difficulties.
SCHE and nutrition
Patients’ nutrition was assessed before weaning and on the day of SBT according to the NUTRIC score. Spearman correlation analysis was performed between the SCHE concentration and the NUTRIC score of patients before SBT, and the results showed that SCHE was negatively correlated with NUTRIC scores (p < 0.01, Table 6). Therefore, patients with lower SCHE were found to be at higher nutritional risk.
Discussion
This research aimed to investigate the relationship between SCHE and other indicators with weaning outcomes. A cohort study with a one-to-one propensity score-matching approach revealed that low SCHE was significantly associated with weaning failure following invasive mechanical ventilation. Further analysis of subgroups with varying degrees of weaning difficulty facilitated a more comprehensive understanding of the relationship between SCHE and different levels of weaning failure. Additionally, our findings indicated that low SCHE is correlated to a high nutritional risk. The crude cohort exhibited a negative correlation, which was also observed in the logistic regression model established through the PSM approach.
The state of critical illness is characterized by a significant catabolic effect, and in the event of insufficient nutritional interventions, patients are at risk of malnutrition, which can result in unfavorable clinical outcomes (15). Additionally, energy expenditure and nitrogen loss exhibit temporal variability, underscoring the importance of appropriate nutritional therapy and optimal dosing (5, 16). Malnutrition may contribute to respiratory muscle weakness and heighten the likelihood of aspiration due to dysphagia, while also impacting the patient’s cardiopulmonary exercise and weaning (17, 18).
According to previous research, SCHE levels have demonstrated efficacy as a biomarker for identifying older adults who are susceptible to muscle loss (19). Furthermore, SCHE has been shown to play a significant role in lipid metabolism (20). Consequently, SCHE levels are considered to be a comprehensive biomarker for malnutrition in theory. Reduced serum SCHE levels have been observed in various clinical contexts, including malnutrition, inflammation, and liver damage. In the current investigation, patients with low SCHE levels exhibited higher NUTRIC scores, indicating a greater nutritional risk. Prospective clinical studies have reported that nutritional support can be beneficial for patients at high nutritional risk (21, 22). Furthermore, SCHE levels have demonstrated moderate correlation with albumin levels, body mass index (BMI), and other nutritional indicators, while exhibiting weak or no correlation with liver function test results and C-gamma reactive protein levels. These findings suggest that SCHE levels are primarily influenced by malnutrition rather than inflammation or liver function (23, 24). Notably, both serum SCHE and albumin are synthesized in the liver and possess serum half-lives of 8–11 days and 12–17 days, respectively. Compared to albumin, the half-life of SCHE is shorter and more responsive, so SCHE starts to decrease earlier than albumin Consequently, SCHE may be more appropriate for dynamic nutritional status testing (25). Furthermore, In patients receiving albumin supplementation, the level of hepatic synthesis of albumin is difficult to detect, but can be replaced by monitoring the SCHE (26). The literature has also documented that SCHE stands out as the most robust prognostic indicator among various nutritional parameters (27).
This study presents an investigation into the potential utility of serum cholinesterase (SCHE) levels as a predictor of successful ventilator weaning (<3,228 u/l). The study found a negative correlation between SCHE concentration and nutritional risk, which sheds light on the role of SCHE in the occurrence of ventilator weaning failure. The findings of this study highlight the significance of SCHE levels in guiding the timing of weaning and evaluating the nutritional status of patients.
Limitations
This study has several limitations. First, this was a single-center retrospective study with a relatively small sample and short duration, and the results of this study should be considered with caution. Second, we did not study medications that may affect SCHE, such as drugs that may impair liver function such as antibiotics. Second, certain complications, nutritional status, and anti-inflammation may affect withdrawal outcomes, but data are lacking because of the difficulty of obtaining all data in the ICU. Third, due to a lack of data, we did not assess the relevance of other more classical parameters associated with deconditioning, such as rapid shallow respiratory index or negative inspiratory force, or grip strength.
Conclusion
In conclusion, the presence of lower serum cholinesterase (SCHE) concentrations may have a negative impact on the withdrawal of mechanical ventilation, and this decrease in SCHE levels is linked to malnutrition. It is recommended that SCHE assessment be correlated with other prognostic indicators. Additionally, tachycardia or lower arterial partial pressure of oxygen prior to weaning are positive predictors of weaning failure. Therefore, SCHE concentrations hold significant clinical value, and further large-scale prospective studies are necessary.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The Ethics Committee of Zhejiang Hospital of Traditional Chinese Medicine, affiliated with Zhejiang University of Traditional Chinese Medicine, approved the study (NO.2023-KLS-003-01). Due to the retrospective study, the Ethics Committee of Zhejiang Hospital of Traditional Chinese Medicine Affiliated with Zhejiang University of Traditional Chinese Medicine agreed to waive written informed consent and we kept the clinical data of the patients confidential. All procedures were by the Declaration of Helsinki. All personal information was encrypted in the database and was anonymous, so there was no invasion of privacy.
Author contributions
JL and TS designed the study and completed the first draft. CM provided technical support for statistical analysis. HC, XL, and XY collected and analyzed the data. KS participated in the revision of the manuscript. DW, LW, and SL provided financial support. JL,TS, HC, CM, XL, XY, KS, LW, SL, and DW wrote the paper. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by 2022 Supported Discipline of Zhejiang Provincial Hospital of Chinese Medicine(No.2022-65); 2022 University-level Basic Scientific Research Ability Improvement Project of Zhejiang Chinese Medical University(No.2022JKJNTZ24); the National Natural Science Foundation of China (No.82104587); 2022 National Traditional Chinese Medicine Administration Project For the Traditional Chinese Medicine Rehabilitation Service Capability Improvement (No. 2021-242); Zhejiang Provincial Medical and Health Technology Program(No. 2019ZD044).
Acknowledgments
We thank all the researchers and members of the Department of Critical Care Medicine, Pulmonary and Critical Care Medicine for their efforts.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1175089/full#supplementary-material
Abbreviations
SCHE, Serum Cholinesterase; IMV, invasive mechanical ventilation; SBT, autonomic breathing test; ICU, Intensive Care Unit; APACHE II, Acute Physiology and Chronic Health Evaluation II; SOFA, Sequential Organ Failure Assessment; GSC, Glasgow Coma Scale; COPD, chronic obstructive pulmonary disease; RR, respiratory rate; HR, heart rate; SBP, systolic blood pressure; PaCO2, arterial carbon dioxide tension; PaO2, arterial oxygen tension; FiO2, oxygen uptake; LOS, length of stay.
References
1. Roberts, KJ . Year in review: adult invasive mechanical ventilation. Respir Care. (2018) 64:604–9. doi: 10.4187/respcare.06927
2. Schmidt, GA, Girard, TD, Kress, JP, Morris, PE, Ouellette, DR, Alhazzani, W, et al. Liberation from mechanical ventilation in critically ill adults: executive summary of an official American College of Chest Physicians/American Thoracic Society clinical practice guideline. Chest. (2017) 151:160–5. doi: 10.1016/j.chest.2016.10.037
3. Magalhães, PAF, Camillo, CA, Langer, D, Andrade, LB, Duarte, M, and Gosselink, R. Weaning failure and respiratory muscle function: what has been done and what can be improved? Respir Med. (2018) 134:54–61. doi: 10.1016/j.rmed.2017.11.023
4. Voga, G . Hemodynamic changes during weaning: can we assess and predict cardiac-related weaning failure by transthoracic echocardiography? Crit Care. (2010) 14:174. doi: 10.1186/cc9085
5. Huang, SW, Lin, HC, Chou, YF, Lin, TY, Lo, CY, Huang, HY, et al. The impact of higher protein intake in patients with prolonged mechanical ventilation. Nutrients. (2022) 14. doi: 10.3390/nu14204395
6. Lampón, N, Hermida-Cadahia, EF, Riveiro, A, and Tutor, JC. Association between butyrylcholinesterase activity and low-grade systemic inflammation. Ann Hepatol. (2012) 11:356–63. doi: 10.1016/S1665-2681(19)30932-9
7. Xu, X, Zhang, G, Hu, M, Ji, C, Meng, J, Lai, Z, et al. Influence of clinical nutritional support on the effects of mechanical ventilation. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. (2018) 30:262–5. doi: 10.3760/cma.j.issn.2095-4352.2018.03.014
8. Woo, HY, Oh, SY, Lee, H, and Ryu, HG. Evaluation of the association between decreased skeletal muscle mass and extubation failure after long-term mechanical ventilation. Clin Nutr. (2020) 39:2764–70. doi: 10.1016/j.clnu.2019.12.002
9. Wang, YL, Dong, Q, Wei, YH, Hu, LW, and Li, SJ. Value of weaning parameters from mechanical ventilation in ischemic stroke patient. Chinese J Geriatr Heart Brain Vessel Dis. (2015) 17:369–71. doi: 10.1186/s13054-016-1208-6
10. Liu, J, Wang, CJ, Ran, JH, Lin, SH, Deng, D, Ma, Y, et al. The predictive value of brain natriuretic peptide or N-terminal pro-brain natriuretic peptide for weaning outcome in mechanical ventilation patients: evidence from SROC. J Renin-Angiotensin-Aldosterone Syst. (2021) 22:1470320321999497. doi: 10.1177/1470320321999497
11. Yamamoto, M, Saito, H, Uejima, C, Tanio, A, Tada, Y, Matsunaga, T, et al. Combination of serum albumin and cholinesterase levels as prognostic indicator in patients ith colorectal cancer. Anticancer Res. (2019) 39:1085–90. doi: 10.21873/anticanres.13217
12. Esteban, A, Frutos, F, Tobin, MJ, Alía, I, Solsona, JF, Valverdú, I, et al. A comparison of four methods of weaning patients from mechanical ventilation. Spanish lung failure collaborative group. N Engl J Med. (1995) 332:345–50. doi: 10.1056/NEJM199502093320601
13. Boles, JM, Bion, J, Connors, A, Herridge, M, Marsh, B, Melot, C, et al. Weaning from mechanical ventilation. Eur Respir J. (2007) 29:1033–56. doi: 10.1183/09031936.00010206
14. Schönhofer, B, Geiseler, J, Dellweg, D, Moerer, O, Barchfeld, T, Fuchs, H, et al. S2k-guideline “prolonged weaning”. Pneumologie. (2015) 69:595–607. doi: 10.1055/s-0034-1392809
15. Sharma, K, Mogensen, KM, and Robinson, MK. Pathophysiology of critical illness and role of nutrition. Nutr Clin Pract. (2019) 34:12–22. doi: 10.1002/ncp.10232
16. van Zanten, ARH, De Waele, E, and Wischmeyer, PE. Nutrition therapy and critical illness: practical guidance for the ICU, post-ICU, and long-term convalescence phases. Crit Care. (2019) 23:368. doi: 10.1186/s13054-019-2657-5
17. Carbone, S, Billingsley, HE, Rodriguez-Miguelez, P, Kirkman, DL, Garten, R, Franco, RL, et al. Lean mass abnormalities in heart failure: the role of sarcopenia, Sarcopenic obesity, and cachexia. Curr Probl Cardiol. (2020) 45:100417. doi: 10.1016/j.cpcardiol.2019.03.006
18. Emami, A, Saitoh, M, Valentova, M, Sandek, A, Evertz, R, Ebner, N, et al. Comparison of sarcopenia and cachexia in men with chronic heart failure: results from the studies investigating co-morbidities aggravating heart failure (SICA-HF). Eur J Heart Fail. (2018) 20:1580–7. doi: 10.1002/ejhf.1304
19. Cacciatore, F, Della-Morte, D, Basile, C, Curcio, F, Liguori, I, Roselli, M, et al. Butyryl-cholinesterase is related to muscle mass and strength. A new biomarker to identify elderly subjects at risk of sarcopenia. Biomark Med. (2015) 9:669–78. doi: 10.2217/bmm.15.28
20. Santarpia, L, Grandone, I, Contaldo, F, and Pasanisi, F. Butyrylcholinesterase as a prognostic marker: a review of the literature. J Cachexia Sarcopenia Muscle. (2013) 4:31–9. doi: 10.1007/s13539-012-0083-5
21. Jie, B, Jiang, ZM, Nolan, MT, Zhu, SN, Yu, K, and Kondrup, J. Impact of preoperative nutritional support on clinical outcome in abdominal surgical patients at nutritional risk. Nutrition. (2012) 28:1022–7. doi: 10.1016/j.nut.2012.01.017
22. Heyland, DK, Dhaliwal, R, Jiang, X, and Day, AG. Identifying critically ill patients who benefit the most from nutrition therapy: the development and initial validation of a novel risk assessment tool. Crit Care. (2011) 15:R268. doi: 10.1186/cc10546
23. Seo, M, Yamada, T, Tamaki, S, Hikoso, S, Yasumura, Y, Higuchi, Y, et al. Prognostic significance of serum cholinesterase level in patients with acute decompensated heart failure with preserved ejection fraction: insights from the PURSUIT-HFpEF registry. J Am Heart Assoc. (2020) 9:e014100. doi: 10.1161/JAHA.119.014100
24. Ramachandran, J, Sajith, KG, Priya, S, Dutta, AK, and Balasubramanian, KA. Serum cholinesterase is an excellent biomarker of liver cirrhosis. Trop Gastroenterol. (2014) 35:15–20. doi: 10.7869/tg.158
25. Gamsjäger, T, Brenner, L, Sitzwohl, C, and Weinstabl, C. Half-lives of albumin and cholinesterase in critically ill patients. Clin Chem Lab Med. (2008) 46:1140–2. doi: 10.1515/CCLM.2008.220
26. Yue, C, Zhang, C, Ying, C, and Jiang, H. Reduced serum cholinesterase is an independent risk factor for all-cause mortality in the pediatric intensive care unit. Front Nutr. (2022) 9:809449. doi: 10.3389/fnut.2022.809449
27. Mitsunaga, S, Kinoshita, T, Hasebe, T, Nakagohri, T, Konishi, M, Takahashi, S, et al. Low serum level of cholinesterase at recurrence of pancreatic cancer is a poor prognostic factor and relates to systemic disorder and nerve plexus invasion. Pancreas. (2008) 36:241–8. doi: 10.1097/MPA.0b013e31815b6b2b
Keywords: serum cholinesterase, weaning, invasive mechanical ventilation, nutrition, autonomic breathing test
Citation: Liu J, Shao T, Chen H, Ma C, Lu X, Yang X, Song K, Wang L, Lei S and Wang D (2023) Serum cholinesterase as a new nutritional indicator for predicting weaning failure in patients. Front. Med. 10:1175089. doi: 10.3389/fmed.2023.1175089
Edited by:
Luigi Vetrugno, University of Studies G. d'Annunzio Chieti and Pescara, ItalyReviewed by:
Federico Barbariol, Azienda Sanitaria Universitaria Friuli Centrale (ASU FC), ItalyPasquale Raimondo, Azienda Ospedaliero Universitaria Consorziale Policlinico di Bari, Italy
I-Shiang Tzeng, National Taipei University, Taiwan
Copyright © 2023 Liu, Shao, Chen, Ma, Lu, Yang, Song, Wang, Lei and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dafen Wang, VzE4MjU4ODkxNjk5QDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
 Jiaping Liu1†
Jiaping Liu1† Xiaohui Lu
Xiaohui Lu Xiaoming Yang
Xiaoming Yang Dafen Wang
Dafen Wang