- 1Department of Anesthesiology, Third Affiliated Hospital of Zhengzhou University, Zhengzhou, China
- 2Department of Obstetrics and Gynecology, Third Affiliated Hospital of Zhengzhou University, Zhengzhou, China
Introduction: Compared with traditional open surgery, laparoscopic surgery is widely used in surgery, with the advantages of being minimally invasive, having good cosmetic effects, and having short hospital stays, but in laparoscopic surgery, pneumoperitoneum and the Trendelenburg position can cause complications, such as atelectasis. Recently, several studies have shown that protective lung ventilation strategies are protective for abdominal surgery, reducing the incidence of postoperative pulmonary complications (PPCs). Ventilator-associated lung injury can be reduced by protective lung ventilation, which includes microtidal volume (4–8 mL/kg) ventilation and positive end-expiratory pressure (PEEP). Therefore, we used randomized, controlled trials (RCTs) to assess the results on this topic, and RCTs were used for meta-analysis to further evaluate the effect of protective lung ventilation on pulmonary complications in patients undergoing laparoscopic surgery.
Methods: In this meta-analysis, we searched the relevant literature contained in six major databases—CNKI, CBM, Wanfang Medical, Cochrane, PubMed, and Web of Science—from their inception to October 15, 2022. After screening the eligible literature, a randomized, controlled method was used to compare the occurrence of postoperative pulmonary complications when a protective lung ventilation strategy and conventional lung ventilation strategy were applied to laparoscopic surgery. After statistical analysis, the results were verified to be statistically significant.
Results: Twenty-three trials were included. Patients receiving protective lung ventilation were 1.17 times less likely to develop pulmonary complications after surgery than those receiving conventional lung ventilation (hazard ratio [RR] 0.18, 95% confidence interval [CI] 1.13–1.22; I2 = 0%). When tested for bias (P = 0.36), the result was statistically significant. Patients with protective lung ventilation were less likely to develop pulmonary complications after laparoscopic surgery.
Conclusion: Compared with conventional mechanical ventilation, protective lung ventilation reduces the incidence of postoperative pulmonary complications. For patients undergoing laparoscopic surgery, we suggest the use of protective lung ventilation, which is effective in reducing the incidence of lung injury and pulmonary infection. Implementation of a low tidal volume plus moderate positive end-expiratory pressure strategy reduces the risk of postoperative pulmonary complications.
Introduction
Laparoscopic surgery is a technique that uses a laparoscope in the abdominal cavity to monitor and guide surgery from outside the abdomen to complete the exploration of diseased tissue, haemostasis, electrocoagulation, suturing and other operations. Laparoscopic surgery is widely used because of its low rate of bleeding, low postoperative pain (1), fast recovery, and short hospital stays. Compared with traditional open surgery, laparoscopy is widely used in surgery with the advantages of minimal invasiveness, good cosmetic effects and short hospital stays. However, during laparoscopic surgery, pneumoperitoneum and Trendelenburg positions can cause postoperative pulmonary complications (PPCs), such as atelectasis (2), resulting in severe perioperative respiratory dysfunction. Studies have shown that the incidence of PPCs after general surgery is 5%, while the incidence of PPCs after abdominal surgery is between 12% and 58% (1).
Mechanical ventilation is a routine surgical form of ventilation that used to use high tidal volume ventilation (10 to 15 mL/kg) to prevent hypoxaemia and atelectasis. However, experiments have shown that mechanical ventilation under high tidal volume ventilation conditions can cause alveolar hyperexpansion, worsen lung injury, and cause ventilator-related lung injury (3). Recently, several studies have shown that certain lung ventilation strategies are protective for abdominal surgery, reducing the incidence of PPCs (4, 5).
Protective lung ventilation minimizes lung injury and circulatory suppression due to mechanical ventilation while improving hypoxaemia. Intraoperative protective ventilation strategies can maintain alveolar dilation, reduce alveolar collapse or over dilation, and decrease the incidence of atelectasis. The core components of protective pulmonary ventilation include small tidal volume ventilation [Vt 6–8 mL/kg (6, 7)], moderate positive end-expiratory pressure [PEEP 5–10 cm H2O (6, 8)], and pulmonary recruitment.
A high tidal volume can be used to reopen an area of the lung where the end of the expiratory has collapsed and repair arterial oxygenation injury, but it is considered safe only for short periods of mechanical ventilation. Appropriate positive end-expiratory pressure can be effective in preventing PPCs. High PEEP can promote alveolar hyperexpansion, pulmonary vascular resistance can increase accordingly (1), and ventilatory blood flow ratio imbalance can impair haemodynamics, causing postoperative pulmonary complications, and the ideal PEEP value is currently unclear. However, all relevant studies have recommended small tidal volumes, and there is clear evidence that protective lung ventilation in patients with acute lung injury and acute respiratory distress syndrome is effective in reducing morbidity and mortality (8). Nevertheless, the effect is not obvious in the general patient population, and there is a lack of strong evidence and clear mechanisms to prove that protective lung ventilation can be effective in reducing the occurrence of pulmonary complications when applied to laparoscopic surgery.
Therefore, we used randomized, controlled trials (RCTs) to assess the results on this topic and for meta-analysis to further assess the effects of protective lung ventilation (low tidal volume ventilation and PEEP) on pulmonary complications in laparoscopic surgery patients.
Methods
Search strategy
In this systematic review and meta-analysis, we submitted a registration for this study on the PROSPERO website and is currently being assessed. We followed the PRISMA (9) guidelines (PRISMA Checklist can be seen in Appendix 1) and collected articles from six Chinese and English literature databases—CNKI, Medical Wanfang, CBM, Cochrane, PubMed, and Web of Science—as well as relevant subject literature from the China Clinical Trial Registry through a literature search, without language restrictions. Randomized, controlled trials were searched for according to the corresponding keywords and extended terms in Chinese and English, and all relevant articles from the establishment of the database up to November 2022 were retrieved.
The complete detailed search string for PubMed was as follows: ((“Laparoscopes”[Mesh]) OR ((((((((((Peritoneoscope[Title/Abstract]) OR (Celioscope[Title/Abstract])) OR (Laparoscope[Title/Abstract])) OR (Laparoscopic surgery[Title/Abstract])) OR (Porous laparoscopy[Title/Abstract])) OR (Single-port laparoscopy[Title/Abstract])) OR (Transumbilical laparoscopy[Title/Abstract])) OR (Transumbilical single-port laparoscopy[Title/Abstract]))) AND ((“Pulmonary Ventilation”[Mesh]) OR (((((((((((((Ventilation, Pulmonary[Title/Abstract]) OR (Airflow, Respiratory[Title/Abstract])) OR (Airflow, Expiratory[Title/Abstract])) OR (Protective pulmonary ventilation[Title/Abstract])) OR (Protective ventilation[Title/Abstract])) OR (Pulmonary protective ventilation[Title/Abstract])) OR (Lung protective ventilation[Title/Abstract])) OR (Lung protective strategies[Title/Abstract])) OR (Lung-protective ventilation therapy[Title/Abstract])) OR (Pulmonary protective ventilation mode[Title/Abstract])) mechanical ventilation[Title/Abstract]))))AND(((randomized controlled Trial[Publication Type] OR (randomized[Title/Abstract])) OR (placebo[Title/Abstract])). The search strategies of other search engines can be seen in Appendix 2.
Inclusion criteria and exclusion criteria
After completing the initial search of the literature, preliminary screening was performed by removing duplicate literature; excluding reviews, meta-analyses, systematic reviews, and literature with inconsistent research content by reading titles and abstracts; and selecting the literature that needed to be obtained in the original language by formulating inclusion and exclusion criteria and final evaluation indicators. The inclusion criteria were the following: (1) Study subjects: patients undergoing laparoscopic surgery; (2) Interventions: conventional lung ventilation strategies were in the control group and protective lung ventilation strategies used in the experimental group; (3) Outcome measures: at least one of the following: pulmonary complications: atelectasis, hypoxia, and hypoxaemia; (4) Study design: randomized, controlled trials (RCTs). Patients were randomly assigned to two groups, and the results of the two groups were compared. One group (experimental group) received an intervention with a protective lung ventilation strategy, while the other group (control group) received a conventional ventilation strategy. The two groups were compared for postoperative outcomes to determine the effectiveness of the intervention in the experimental group.
The exclusion criteria were: (1) repeatedly reported studies; (2) valid outcome measures not being obtained, e.g. atelectasis, hypoxia, and hypoxaemia; (3) additional measures added to the experimental group intervention; (4) the experimental design not matching in that protective lung ventilation strategies were used in the intervention group, and conventional pulmonary ventilation was used in the control group. Finally, by reading the original texts, the final relevant documents were obtained by eliminating the documents that did not meet the requirements.
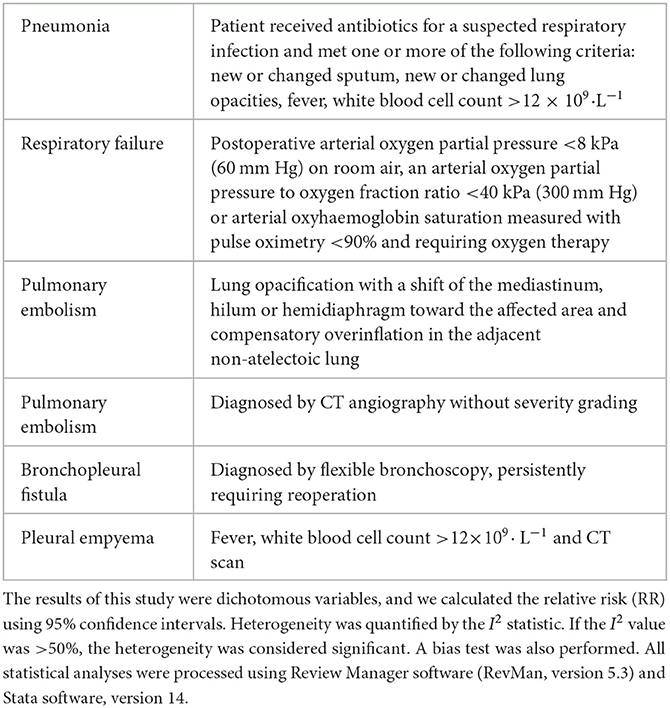
In this review, we define:P as a patient who requires laparoscopic surgery; I means: the use of protective lung ventilation strategy as an intervention; C means: the control group uses the conventional lung ventilation strategy; O means: The outcomes of this meta-analysis are pulmonary complications; S means: the experimental design protocol is a fully randomized controlled trial. Pulmonary complications include: Pneumonia, Respiratory failure, Pulmonary embolism, Pulmonary embolism, Bronchopleural fistula, Pleural empyema. To investigate the effects of protective lung ventilation on pulmonary complications after laparoscopic surgery. Primary outcomes are: pulmonary infection, atelectasis; Secondary outcomes are: cough, lung injury, etc.
Data extraction and quality analysis
We read the extracted data and further confirmed the relevant data extracted. The following data were extracted from each entry: first author, year of publication, group and number of participants, population characteristics (weight, sex, age), tidal volume and PEEP value in the experimental group (protective lung ventilation group) and control group (conventional lung ventilation group). The main evaluation indicators were pulmonary complications, such as lung infection and atelectasis, and the secondary indicators were cough, lung injury, etc. [PPCs are defined in Table 1 (10)].
RCT methods were used in this study. The studies were assessed for complete random allocation, allocation concealment, blinding of participants and staffs, data integrity, selective reporting of study results, and other sources of bias (small sample size, conflict of interest, unbalanced baseline), completed literature quality assessment, heterogeneity testing, and bias testing.
Results
Literatures search
After a well-developed literature screening strategy, 646 articles were obtained. Two students read the titles and abstracts of these 646 articles alone, screened according to the inclusion and exclusion criteria formulated in advance, and summarized the articles screened by the two students together. By reading the title and summary, we excluded 173 duplicate articles. Then 574 articles were excluded due to non-compliance (Figure 1). The last 23 RCTs met the inclusion criteria for this meta-analysis.
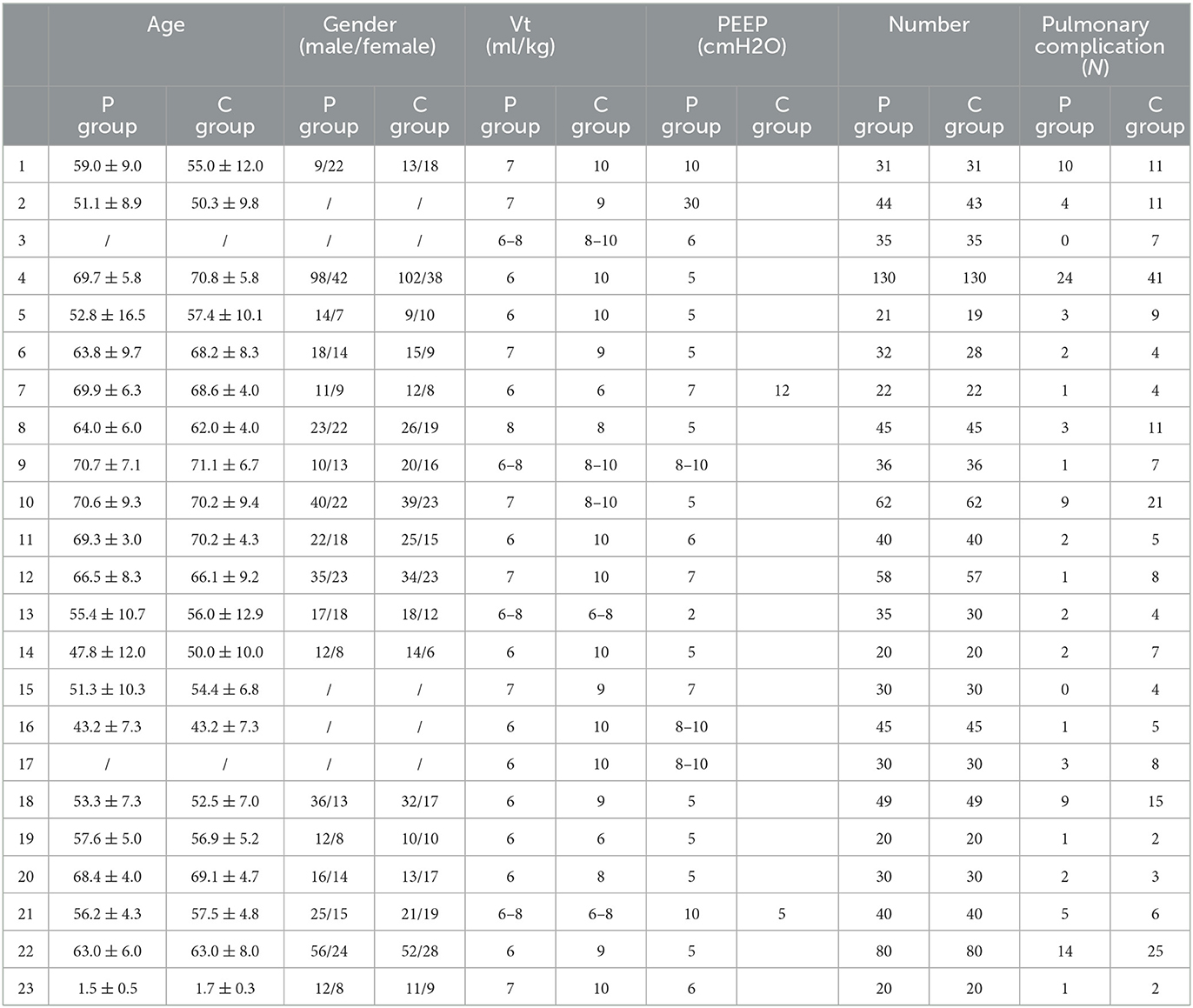
The main characteristics of the 23 articles (1, 9, 11–31) of this study are shown in Table 2.
Data analysis
Of the 23 articles included in this meta-analysis, 1 described pediatric laparoscopic surgery, and 22 described laparoscopic surgery in adult patients, of whom 2 underwent gynecological laparoscopic surgery, and 3 described laparoscopic surgery in overweight patients. The summary data in Table 1 were processed in Review Manager (version 5.3) software to complete the data bias assessment. We assessed the certainty of the evidence using the GRADE approach, which is presented in Appendix 2. Figure 2 summarizes the details of the risk of bias assessment. Two trials were judged to be at low risk of bias, 18 were at unclear risk, and three were at high risk of bias. All trials produced appropriate random sequences, and nine trials reported appropriate allocation concealment.

Figure 2. Risk of bias of included trials was assessed using the Cochrane risk of bias tool. Low risk = bias, if present, unlikely to significantly change results; unclear risk = bias raises some doubt about results; high risk = bias might significantly change results.
After the heterogeneity test (I2 = 0% and P = 0.86 > 0.1), the Q test indicated that there was no heterogeneity between the selected literature in this study (the heterogeneity was not statistically significant), and the fixed effect was selected for pooled effect size. Twenty-three studies used a fixed-effect pooled RR = 1.17 (95% CI 1.13 to 1.22) and were statistically significant (Z = 7.95 and P = 0.00001 < 0.05), suggesting that protective lung ventilation is less likely to have pulmonary complications when applied to laparoscopic surgery than conventional lung ventilation and that protective lung ventilation is 1.17 times less like to cause complications than conventional lung ventilation. Figure 3 provides for details.

Figure 3. Effect of protective lung ventilation on pulmonary complications after laparoscopic surgery. A risk ratio >1.0 indicates a favorable effect on postoperative lung recovery. CI, confidence interval; event, number of people without pulmonary complications. I2 = 0%, P = 0.86.
By plotting funnel plots to investigate whether there was publication bias in the 23 articles of this study, visual findings showed that the funnel plots were symmetrical (Figure 4) and that there was no publication bias. The funnel plots were then evaluated in Stata software, version 14.0 to obtain P = 0.36 > 0.1, further confirming that the data were unbiased, and the conclusions of this study were accurate and reliable, as shown in Figure 5 with details.
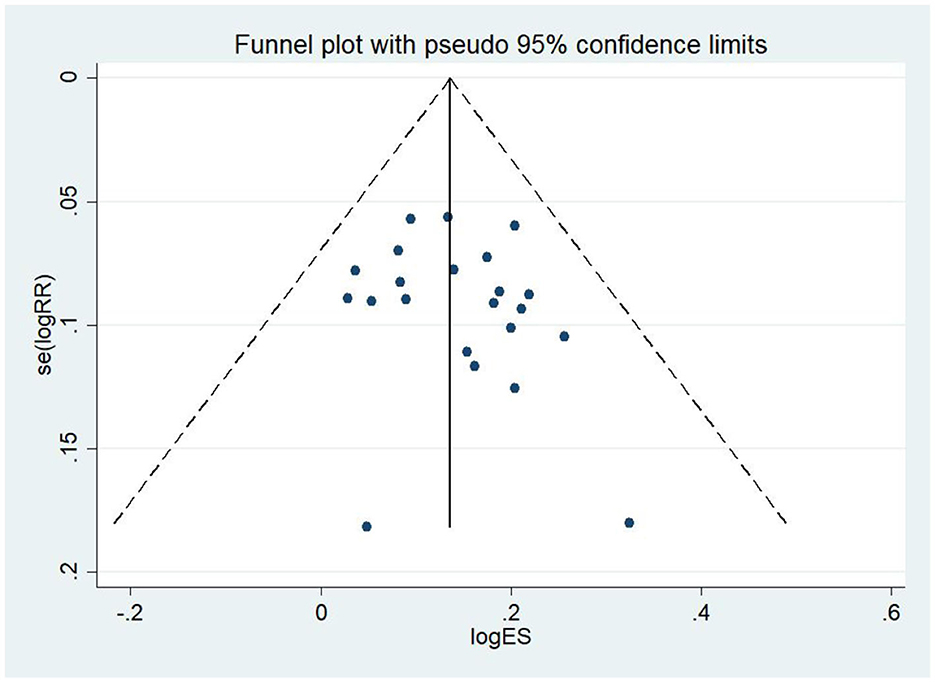
Figure 4. Test for bias (funnel plot). Preliminary judgement of bias was determined by whether it was symmetrical.
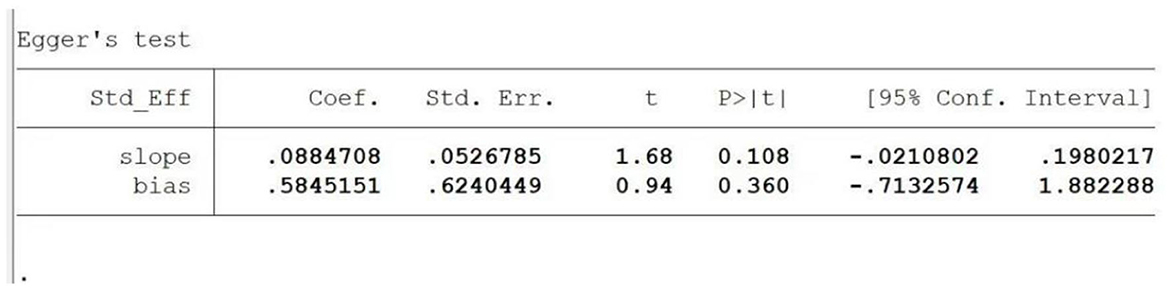
Figure 5. Protective lung ventilation test for bias of pulmonary complications after laparoscopic surgery. P > 0.1, the included data were unbiased and statistically significant.
Then, we further studied the subgroup analysis of the effects of different PEEP plus small tidal volume ventilation on pulmonary complications (Figure 6), and the results showed that when PEEP was in 6 cm H2O, RR = 2.71, I2 = 0%, P = 0.84, when PEEP was in 7 cm H2O, RR = 2.81, I2 = 0%, P = 0.56, there was no heterogeneity between the literature in the above two groups. We can conclude that different levels of PEEP plus small tidal volume ventilation reduce the incidence of pulmonary complications after laparoscopic surgery. The results of the between-group comparison were I2 = 0%, P = 0.91, which indicated that there was no heterogeneity between the groups.

Figure 6. Subgroup analysis of different PEEP plus small tidal volume on the pulmonary complications. A risk ratio >1.0 indicates a favorable effect on postoperative lung recovery. CI, confidence interval; event, number of people without pulmonary complications.
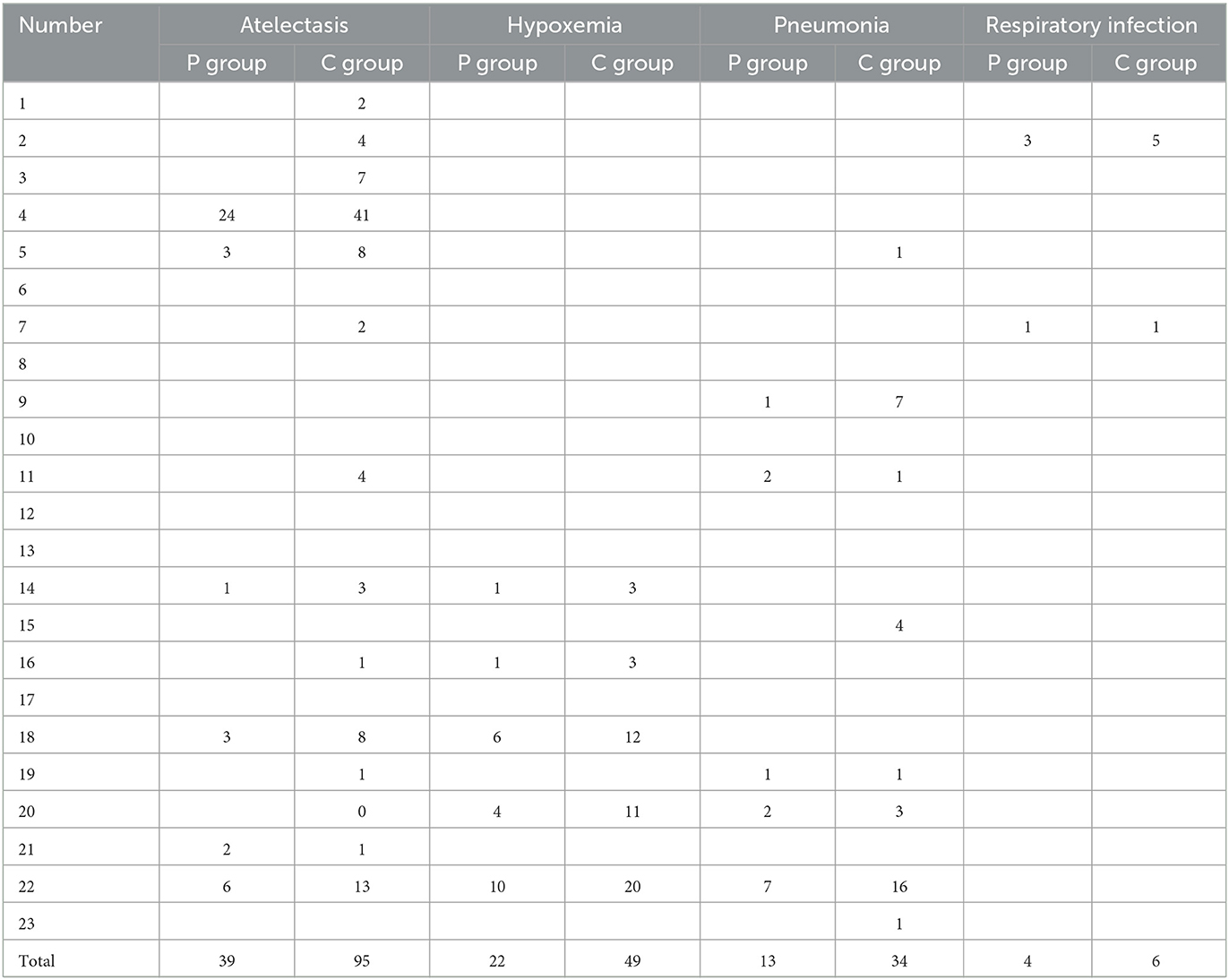
We summarized specific pulmonary complications: atelectasis, hypoxemia, pneumonia, respiratory infections, as shown in Table 3. We found that the experimental groups with protective lung ventilation had significantly fewer PPCs than the control groups with conventional ventilation. Patients with PPCs are mainly characterized by atelectasis, hypoxemia, and pneumonia. And a few number of patients had respiratory infection, diffuse infiltrate, localized infiltrate, pleural effusion, increased thickness of interstitium, etc. Therefore, we can conclude that, when protective pulmonary ventilation is used in laparoscopic surgery, the probability of no pulmonary complications is 1.17 times that with conventional pulmonary ventilation, so laparoscopic surgery patients can have a better ventilation effect, with a reduced incidence of postoperative pulmonary complications, and protective ventilation can promote patient prognosis by adopting a protective lung ventilation strategy (small tidal volume + PEEP).
Discussion
For patients who require laparoscopic surgery under general anesthesia, there might not be a variety of serious lung diseases, but various factors, such as anesthetic drugs, mechanical ventilation, pneumoperitoneal pressure, special positioning, and surgical trauma used during surgery, can cause damage to the patient's lung tissue. Studies have found that when pneumoperitoneum pressure is at the level of 11–13 mm Hg it can lead to an average increase of 66% in atelectasis, greatly increasing the incidence of postoperative pulmonary complications.
Mechanical ventilation is one of the important conditions for the successful completion of laparoscopic surgery, but it can also cause ventilator-induced lung injury (VILI) while providing life support to patients. In the past, it was believed that the length of mechanical ventilation was directly proportional to the incidence of pulmonary complications. However, the latest research shows that even a short period of mechanical ventilation can cause VIIL and even ARDS in healthy lungs.
Protective lung ventilation strategies include small tidal volume ventilation and continuous positive airway pressure (PEEP). Relevant studies have shown that excessive tidal volume, blood transfusion, infection, and extracorporeal bypass during mechanical ventilation can lead to damage to healthy lungs (32). In animal experiments, it was found that, if healthy animals were subjected to mechanical ventilation with a large tidal volume for several hours, it caused deformation, necrosis, and exfoliation of alveolar epithelial cells and vascular endothelial cells, increased the level of inflammatory mediators in bronchoalveolar lavage, and significantly increased the expression of various cytokines (such as TNF). In this study, it was found that the use of small tidal volume protective pulmonary ventilation during mechanical ventilation could indeed reduce the incidence of pulmonary complications (33, 34), providing definitive evidence for clinical work.
Continuous positive airway pressure (PEEP) and the use of appropriate PEEP during mechanical ventilation can assist in collapsed alveolar remanoeuvres (35). Studies have shown that alveolar remanation can increase the functional residual gas volume and lung compliance of the lungs from a physiological point of view, improve the ventilation status and oxygenation status of patients, and reduce functional shunts in the lungs. The study found that, comparing small tidal volumes plus lower level PEEP and low tidal volumes plus high level PEEP, the former had a relatively large area of alveolar collapse and atelectasis during surgery and basically no tensile lung tissue. In the latter, there was hypertense lung tissue (36). Therefore, although small tidal volumes plus low-level PEEP cannot adequately maintain alveolar remanoestasis, it will not cause alveolar hypertension. However, small tidal volumes plus high-level PEEP can satisfactorily achieve the purpose of alveolar remanoeuvres, but at the same time, there is alveolar hypertonic damage, which has an impact on circulatory function. Therefore, too low or too high a level of PEEP has certain adverse effects. Choosing an appropriate PEEP is particularly important for mechanical ventilation and preventing postoperative pulmonary complications.
Protective lung ventilation strategies have received a lot of attention in recent years as a new approach to mechanical ventilation-related lung injury. Many studies have shown that protective lung ventilation has high clinical value for the treatment of patients with acute respiratory lung injury (ALI) and acute respiratory distress syndrome (ARDS), while there is a lack of clear clinical evidence in relevant studies in patients with better physical condition. In this study, we concluded that the use of protective lung ventilation strategies in general patients can effectively reduce the incidence of postoperative pulmonary complications by including patients of different ages and physical conditions. This demonstrates that the protective ventilation strategy with a small tidal volume plus moderate PEEP is also suitable for mechanical ventilation in general patients. The evidence shows that a target tidal volume of 6 mL/kg causes mild hypercapnia in patients with relatively normal lung function and gas exchange. Studies have shown that mild hypercapnia is permissible during ventilation because respiratory acidosis due to hypercapnia can increase respiratory motility, although this is based on the absence of craniocerebral lesions or cardiovascular diseases. In addition, in this study, we also analyzed the effect of small tidal volume plus different levels of PEEP on postoperative pulmonary complications in patients. Through subgroup analysis, we found that when PEEP was set to 6 or 7 cm H2O, compared with conventional ventilation group, it can effectively reduce the occurrence of postoperative pulmonary complications in patients, which provides the effective evidence for subsequent clinical work.
In summary, a protective lung ventilation strategy with a small tidal volume plus moderate levels of PEEP can be used to minimize ventilator-associated lung injury when mechanical ventilation is performed during laparoscopic surgery (3). Postoperative pulmonary complications, including atelectasis, pneumonia, and lung injury, are the most common complications and the main causes of morbidity and mortality, affecting the prognosis and prolonging the hospital stay. Therefore, we recommend the use of protective lung ventilation strategies during mechanical ventilation, which can effectively reduce the incidences of lung injury and lung infection. A strategy of low tidal volume + moderate positive end-expiratory airway pressure reduces the risk of lung injury and infection. In addition, the occurrence of VILI is also related to various factors, such as inspired oxygen concentration, ventilation mode, and pulmonary recruitment maneuvers, so we still require further research to optimize the protective lung ventilation strategy by adjusting the inspired oxygen concentration, improving the ventilation mode, and selecting a reasonable lung recruitment method.
Limitations
This study has certain limitations. Firstly, in the process of screening the literatures, two people completed the process separately and summarized them, and there was a degree of subjectivity. Secondly, the 23 articles included patients of different ages, including children, adults, and the elderly, and the outcome indicators were inevitably affected by age, physical condition, lung function and other factors, which had an impact in our conclusion that the protective lung ventilation strategy used in laparoscopic surgery can effectively reduce the incidence of PPCs. In addition, we used pulmonary complications as an independent and complete indicator to demonstrate that protective lung ventilation strategies used in laparoscopic surgery are effective in reducing the incidence of PPCs after surgery. However, there was no detailed comparison of interventions for pneumonia, atelectasis, etc.
Conclusion
Compared with conventional mechanical ventilation, protective lung ventilation reduces the incidence of postoperative pulmonary complications. For patients undergoing laparoscopic surgery, we suggest the use of protective lung ventilation, which is effective in reducing the incidence of lung injury and pulmonary infection. Implementation of a low tidal volume plus moderate positive end-expiratory pressure strategy reduces the risk of postoperative pulmonary complications. Postoperative pulmonary complications, including atelectasis, pneumonia, and lung injury, are the most common complications and the main causes of morbidity and mortality, affecting the prognosis and prolonging the hospital stay. Therefore, the use of protective lung ventilation strategy can facilitate the patient's recovery more quickly.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
YW and LJ proposed and designed this study. MS and BY retrieved and selected the data and responsible for the extraction of the data and the quality assessment of all study data. MS performed a statistical analysis and summarized the data and drafted the manuscript. YW, BY, and TW revised it. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to thank the authors of the primary studies included in this systematic review and meta-analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1171760/full#supplementary-material
References
1. Nguyen TK, Nguyen VL, Nguyen TG, Mai DH, Nguyen NQ, Vu TA, et al. Lung-protective mechanical ventilation for patients undergoing abdominal laparoscopic surgeries: a randomized controlled trial. BMC Anesthesiol. (2021) 21:95. doi: 10.1186/s12871-021-01318-5
2. Zhou ZF, Fang JB, Wang HF, He Y, Yu YJ, Xu Q, et al. Effects of intraoperative PEEP on postoperative pulmonary complications in high-risk patients undergoing laparoscopic abdominal surgery: study protocol for a randomized controlled trial. BMJ Open. (2019) 9:e028464. doi: 10.1136/bmjopen-2018-028464
3. Gu WJ, Wang F, Liu JC. Effect of lung-protective ventilation with lower tidal volumes on clinical outcomes among patients undergoing surgery: a meta-analysis of randomized controlled trials. CMAJ. (2015) 187:E101–9. doi: 10.1503/cmaj.141005
4. Deng QW, Tan WC, Zhao BC, Wen SH, Shen JT, Xu M. Intraoperative ventilation strategies to prevent postoperative pulmonary complications: a network meta-analysis of randomized controlled trials. Br J Anaesth. (2020) 124:324–35. doi: 10.1016/j.bja.2019.10.024
5. Park JH, Park IK, Choi SH, Eum D, Kim MS. Volume-controlled vs. dual-controlled ventilation during robot-assisted laparoscopic prostatectomy with steep trendelenburg position: a randomized-controlled trial. J Clin Med. (2019) 8:2032. doi: 10.3390/jcm8122032
6. Futier E, Constantin JM, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. (2013) 369:428–37. doi: 10.1056/NEJMoa1301082
7. Beitler JR, Malhotra A, Thompson BT. Ventilator-induced Lung Injury. Clin Chest Med. (2016) 37:633–46. doi: 10.1016/j.ccm.2016.07.004
8. Severgnini P, Selmo G, Lanza C, Chiesa A, Frigerio A, Bacuzzi A, et al. Protective mechanical ventilation during general anesthesia for open abdominal surgery improves postoperative pulmonary function. Anesthesiology. (2013) 118:1307–21. doi: 10.1097/ALN.0b013e31829102de
9. Liu J, Huang X, Hu S, Meng Z, He H. Individualized lung protective ventilation vs. conventional ventilation during general anesthesia in laparoscopic total hysterectomy. Exp Ther Med. (2020) 19:3051–9. doi: 10.3892/etm.2020.8549
10. Hulzebos EH, Helders PJ, Favié NJ, De Bie RA, Brutel de la Riviere A, Van Meeteren NL. Preoperative intensive inspiratory muscle training to prevent postoperative pulmonary complications in high-risk patients undergoing CABG surgery: a randomized clinical trial. JAMA. (2006) 296:1851–7. doi: 10.1001/jama.296.15.1851
11. Park SJ, Kim BG, Oh AH, Han SH, Han HS, Ryu JH. Effects of intraoperative protective lung ventilation on postoperative pulmonary complications in patients with laparoscopic surgery: prospective, randomized and controlled trial. Surg Endosc. (2016) 30:4598–606. doi: 10.1007/s00464-016-4797-x
12. Li H, Zheng ZN, Zhang NR, Guo J, Wang K, Wang W, et al. Intra-operative open-lung ventilatory strategy reduces postoperative complications after laparoscopic colorectal cancer resection: a randomized controlled trial. Eur J Anaesthesiol. (2021) 38:1042–51. doi: 10.1097/EJA.0000000000001580
13. Koritarova V, Georgiev S. The Impact of Protective Ventilation Strategy, Applied in Patients During Prolonged Gynecological Surgery, on Postoperative Oxygenation. Proceed Bulg Acad Sci. (2022) 75:129–35. doi: 10.7546/CRABS.2022.01.15
14. Bai J. Application of the Lung-Protective Ventilation Strategy in patients Undergoing Laparoscopic Colorectal Cancer Surgery. Master's Thesis. [China (Chin)]: Dalian Medical University (2018).
15. Fang YX. Effects of Different PEEP Lung-Protective Ventilation on Respiratory Mechanics and Oxygenation in Elderly Patients Undergoing Laparoscopic Colorectal Cancer Surgery. [Master's Thesis]. [China (Chin)]: Guangzhou Medical University (2021).
16. Hao LY. Effects of Lung-Protective Ventilation Strategies Under Different Ventilation Modes on Respiratory Mechanics and Postoperative Pulmonary Complications in Laparoscopic Gastric Cancer in Elderly Patients. [Master's Thesis]. [China (Chin)]: Hebei Medical University (2020).
17. Li R, Li Y, Li BB. Effect of lung-protective ventilation strategies on respiratory function in elderly patients undergoing prolonged laparoscopic surgery. Guizhou Med J. (2017) 41:483–5. doi: 10.1097/eja.0000000000001580
18. Yang CJ, Wei L, Yan SF, Wang XS, Yang F, Ni YP. Pulmonary protective effect of transpulmonary drive pressure-directed ventilation strategy in elderly patients undergoing radical bowel cancer resection. J Reg Anat Operative Surg. (2022) 31:799–803.
19. Liu J, Meng ZP, Yan W, Yao HQ, Qiu P. Effects of lung-protective ventilation strategies on pulmonary oxygenation function and postoperative pulmonary complications in elderly patients undergoing laparoscopic radical gastric cancer surgery. J Clin Anesthesiol. (2019) 35:344–7.
20. He MJ. Effect of Deep Muscle Loose Lung-Protective Ventilation on Pulmonary Complications in Patients Undergoing Laparoscopic Radical Colorectal Resection. [Master's Thesis]. [China (Chin)]: Southern Medical University (2019).
21. Zhao L, Chen XG, Wang P. Effects of lung-protective ventilation strategies on respiratory mechanics and lung function in patients undergoing laparoscopic surgery in Trendelenburg position. J Qiqihar Med Univ. (2022) 43:745–9.
22. Li WJ, Hu YF, Zhang LB, Zhou YL, Shen WH, Zhu MM, et al. Application of small tidal volume lung protective ventilation strategy in laparoscopic gastrointestinal surgery in elderly patients with pulmonary insufficiency. Geriatr Health Care. (2020) 26:648–51.
23. Wang H, Huang XH, Liu J. Effect of lung-protective ventilation strategies on lung function in obese patients undergoing laparoscopic gynaecological surgery. Clinl Edu Gen Pract. (2020) 18:415–8. doi: 10.13558/j.cnki.issn1672-3686.2020.005.009
24. Luo YH, Su JY, Liu HZ, Yan GS, Yang ZJ. Effect of protective lung ventilation on perioperative lung function in obese patients undergoing laparoscopic radical gastrectomy for gastric cancer. Pract J Cancer. (2018) 33:1326–9.
25. Wang L, Li LD, Cui YN, Zhou YJ. Application of lung-protective ventilation strategies in laparoscopic surgery. J Changzhi Med Coll. (2016) 30:366–9.
26. Deng XY, Xian LN. Effect of lung-protective ventilation on postoperative pulmonary complications in patients with esophageal cancer. Chin J Endoscopy. (2018) 24:64–70.
27. Xu MX. Application of the Positive End-Expiratory Pressure Pulmonary Protective Ventilation Strategy in Laparoscopic Surgery in Overweight Patients. [Master's Thesis]. [China (Chin)]: China Medical University (2019).
28. Yin XX, Li J. Effect of positive end-expiratory pressure level on intraoperative respiratory function in obese laparoscopic radical colon cancer resection patients. Chin J Obes Metabol Dis. (2021) 7:250–4.
29. Yang LX, Quan RX, Yu CJ, Hu JJ, Lv HB. Clinical value of lung-protective ventilation strategies in thoracic laparoscopic radical esophageal resection. Chinese Journal Of Digestive Surgery. (2016) 11:1100–5.
30. Wang ZL. Application of Lung-Protective Ventilation Strategies During General Anesthesia for Pediatric Laparoscopic Surgery. [Master's Thesis]. [China (Chin)]: Chongqing Medical University (2016).
31. Xie YY, Chen HZ, Wang J. Effect of protective pulmonary ventilation on postoperative lung oxygenation function in elderly patients undergoing laparoscopic colorectal cancer surgery. J Dalian Med Univ. (2018) 40:102–7.
32. Li Q, Liu SQ, Chen H, Zhang XW, Pan C, Liu L, et al. A meta-analysis of the prognostic effect of small tidal volume ventilation in patients with non-acute respiratory distress syndrome. Chin J Int Med. (2016) 10:784–90.
33. Serpa Neto A, Cardoso SO, Manetta JA, Pereira VG, Espósito DC, Pasqualucci Mde O, et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. JAMA. (2012) 30:1651–9. doi: 10.1001/jama.2012.13730
34. Sutherasan Y, Vargas M, Pelosi P. Protective mechanical ventilation in the non-injured lung: review and meta-analysis. Crit Care. (2014) 18:211. doi: 10.1186/cc13778
35. Peng XR, Yang L, Zhu T. Comparison of the effects of positive end-expiratory pressure pulmonary protective ventilation strategies at high and low levels: a meta-analysis. Chin J Anesthesiol. (2020) 06:716–9.
Keywords: protective lung ventilation, small tidal volume, moderate PEEP, laparoscopic surgery, pulmonary complications, meta-analysis
Citation: Sun M, Jia R, Wang L, Sun D, Wei M, Wang T, Jiang L, Wang Y and Yang B (2023) Effect of protective lung ventilation on pulmonary complications after laparoscopic surgery: a meta-analysis of randomized controlled trials. Front. Med. 10:1171760. doi: 10.3389/fmed.2023.1171760
Received: 22 February 2023; Accepted: 05 May 2023;
Published: 25 May 2023.
Edited by:
Savino Spadaro, University of Ferrara, ItalyReviewed by:
Ming Zhong, Fudan University, ChinaMichela Rauseo, University of Foggia, Italy
Amiya Kumar Barik, Post Graduate Institute of Medical Education and Research (PGIMER), India
Marco Milone, Federico II University Hospital, Italy
Copyright © 2023 Sun, Jia, Wang, Sun, Wei, Wang, Jiang, Wang and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuxia Wang, d3l4d2xAenp1LmVkdS5jbg==; Bo Yang, eWFuZ2JveXNAMTI2LmNvbQ==
 Menglin Sun
Menglin Sun Ruolin Jia
Ruolin Jia Lijuan Wang1
Lijuan Wang1 Tao Wang
Tao Wang Yuxia Wang
Yuxia Wang