- Intensive Care Unit (ICU), Department of Cardiac Surgery, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, Shandong, China
Objectives: This review aimed to summarize the recent literature on positive-pressure extubation.
Design: A scoping review was conducted under the framework of the Joanna Briggs Institute.
Data sources: Web of Science, PubMed, Ovid, Cumulative Index to Nursing & Allied Health, EBSCO, Cochrane Library, Wan Fang Data, China National Knowledge Infrastructure, and China Biology Medicine databases were searched for studies on adults and children.
Study selection: All articles describing the use of positive-pressure extubation were considered eligible for inclusion. The exclusion criteria were articles not available in English or Chinese, and those without full text available.
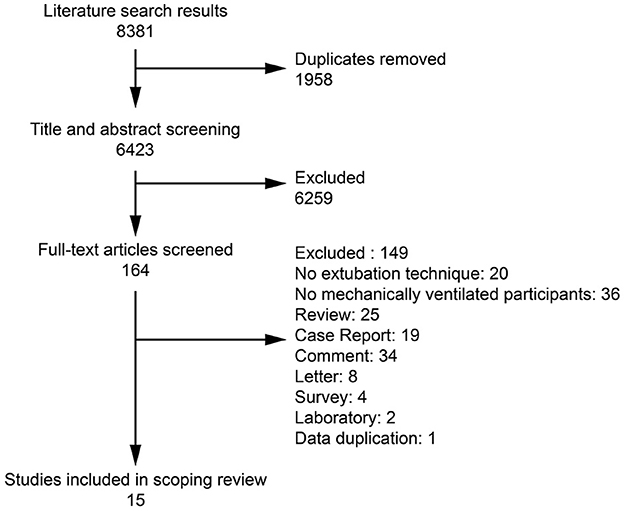
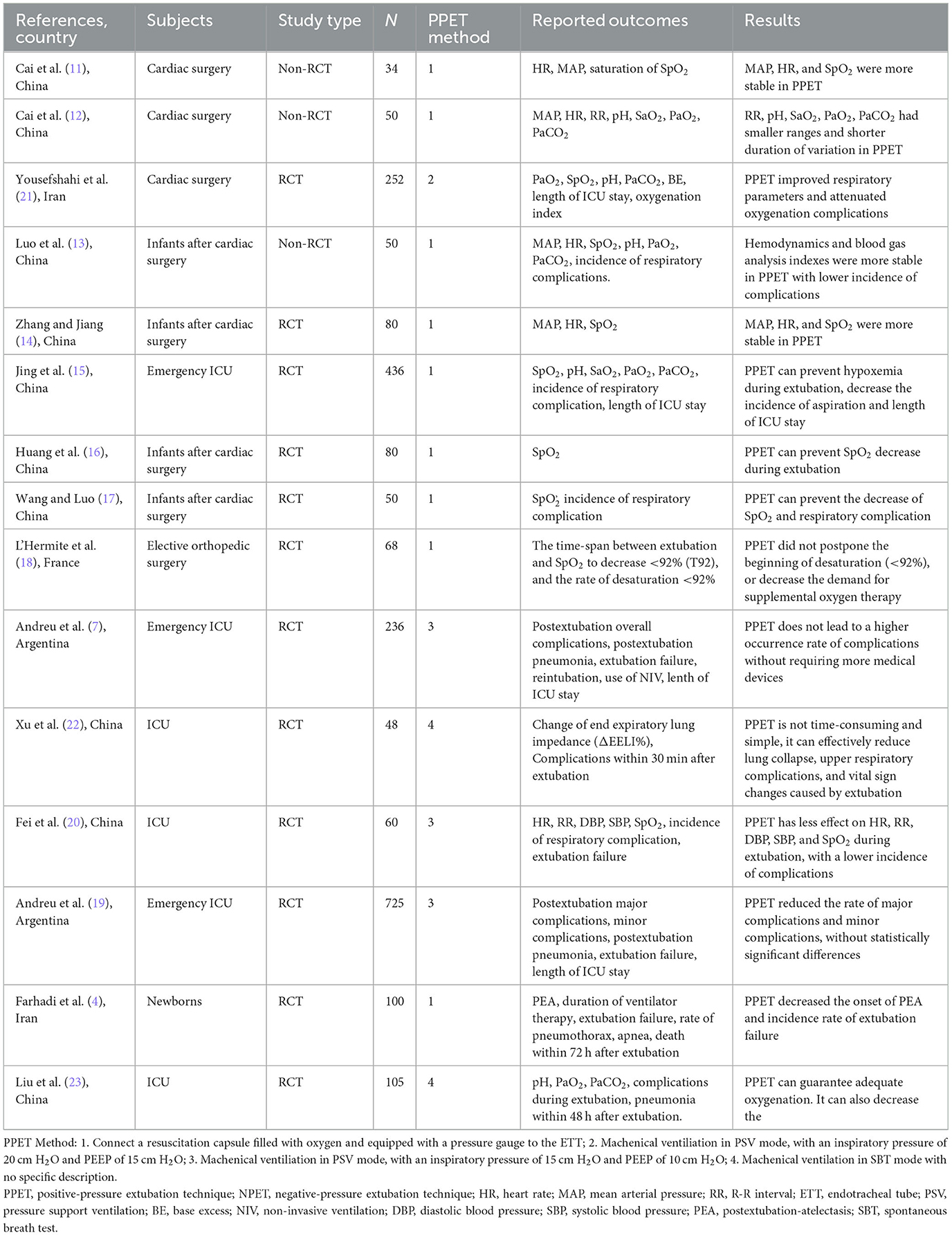
Data extraction and synthesis: The database searches identified 8,381 articles, 15 of which could be included in this review, with an aggregated patient number of 1,544. Vital signs, including mean arterial pressure, heart rate, R-R interval, and SpO2 before and after extubation; blood gas analysis indexes, including pH, oxygen saturation, PaO2, and PaCO2 before and after extubation; and incidence of respiratory complications, including bronchospasm, laryngeal edema, aspiration atelectasis, hypoxemia, and hypercapnia, were reported in the included studies.
Results: The majority of these studies reported that the positive-pressure extubation technique can maintain stable vital signs and blood gas analysis indices as well as prevent complications during the peri-extubation period.
Conclusions: The positive-pressure extubation technique has a safety performance similar to that of the traditional negative-pressure extubation technique and may lead to better clinical outcomes, including stable vital signs, arterial blood gas analysis, and a lower incidence of respiratory complications.
Introduction
Extubation is defined as removing the endotracheal tube (ETT), which is the last step in releasing a patient from mechanical ventilation. Extubation can have physiological effects, which may be broadly categorized into cardiovascular and respiratory complications, including hypertension, tachycardia, coughing or bucking, and increases in intracranial and intraocular pressure. It has been reported that the most common complications associated with extubation are laryngospasm (25%), desaturation (22%), and coughing (18%) (1), whereas in ICU patients, the most common complications are hypertension (28.4%), desaturation (24. 1%), and tachycardia (23.7%) (2). These effects may be more significant in young children because of their weak functional residual capacity and high oxygen consumption (3). For example, atelectasis is a common complication after the removal of an ETT in neonates, which increases the extubation failure rate (4).
An operational definition for extubation procedures is lacking, according to previous clinical guidelines (5, 6); however, two techniques are described in the literature. One of these is the conventional extubation technique, which involves placing a suction catheter into the ETT and trachea, emptying the cuff, and removing the ETT with continuous suctioning during the entire procedure [so-called negative-pressure extubation technique (NPET)]. The other is the positive-pressure extubation (PPET) technique, which involves applying positive-pressure through the trachea during cuff emptying and extubation. Theoretically, the airflow passing between the ETT and the larynx during PPET pushes the accumulated subglottic secretions upward so that they can be discharged through the oral cavity.
PPET was proposed based on the concept of improving lung opening and reducing aspiration. Prior studies reported better clinical outcomes with PPET, including but not limited to less desaturation, atelectasis, and coughing (4, 7). However, another investigation showed that more than 80% of practitioners simply applied suction trachea techniques, and that <5% of practitioners adjusted positive end-expiratory pressure settings during extubation in the UK (8). Similarly, 93.5% of participants in Argentina performed endotracheal suctioning and only 12.5% used positive-pressure during extubation (9). Therefore, there is a gap between experiments and clinical practice.
The objective of this scoping review was to identify the body of existing published research that explicitly mentions PPET vs. NPET.
Review of the literature
Methods
This study followed the methodology for scoping reviews described by Arksey and O'Malley (10) and the Preferred Reporting Items for Systematic reviews and Meta-Analyses Extension for Scoping Reviews guidelines. We searched for relevant publications in the PubMed, Web of Science, Ovid, Cumulative Index to Nursing & Allied Health, EBSCO, Cochrane Library, China Biology Medicine, China National Knowledge Infrastructure, and WanFang Data databases. Literature was searched from the respective database inception dates until July 31, 2022. The key search terms were “airway tube,” “tracheal tube,” “endotracheal tube,” “tracheal catheter,” “orotracheal tube,” “tracheostomy,” “decannulation,” “airway extubation,” “extubation technique,” “extubation,” “positive-pressure extubation,” and “negative-pressure extubation.” urthermore, a manual search of the references of all included articles and previous review articles was performed to identify additional studies.
All published randomized controlled trials, cluster randomized trials, crossover trials, non-randomized trials, quasi-randomized trials, and observational studies with controls were included. Studies in English and Chinese were accepted. Conference abstracts and review articles were excluded.
Study selection
Studies were selected independently by two researchers (Liu and Li). The two researchers compared their lists, and any differences in opinion were resolved by discussion to consensus, or through arbitration by a third researcher (Cui), if necessary.
Data extraction and synthesis were conducted by one researcher (Qi), using standard data-extraction forms. Data extracted included the first author, publication year, country, objects, design, sample size, interventions, reported outcomes, results, and conclusions. Another researcher (Liu) verified the extracted data. We organized the extracted data described above for a qualitative synthesis.
Patient and public involvement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Results
In total, 8,381 records were initially identified, of which 1,873 studies were searched in Chinese databases, and 6,508 studies were searched in English databases. After removing duplicates, 6,423 records remained. After reading the titles and abstracts, 164 records that did not meet the inclusion criteria were excluded, and the full texts of eligible articles were further evaluated. Ultimately, 15 publications were included (Figure 1). These articles were all controlled trials, published between April 2008 and March 2022 and are summarized in Table 1.
Positive-pressure extubation technique
In the 15 included studies, PPET was used in 1,032 adults in the ICU, 444 infants, and 68 adults emerging from anesthesia. All the included studies reported the effects of PPET vs. NPET. PPET and NPET were implemented in the same way, using three different methods. One of the three PPET methods was reported in nine studies (4, 11–18); it involved connecting a resuscitation capsule filled with oxygen and equipped with a pressure gauge to the ETT during the inspiration phase. Seven studies published between 2008 and 2016 were conducted on patients after cardiac surgery in China (11–17). One study was conducted on patients emerging from anesthesia in France (18). The remaining study was conducted on newborns undergoing mechanical ventilation in Iran (4). Another method involved removing the ETT at the end of the inspiratory period, with a higher PEEP, and ventilator parameters were set to pressure support ventilation mode, which was reported in four studies and all of them were conducted on ICU patients [two in Argentina (7, 19), one in China (20), and one in Iran (21)]. The last method involved removing the ETT at the end of the inspiratory period under the original ventilation mode, which was reported in two studies (22, 23), all of which were conducted on ICU patients in China.
Clinical performance indicators
Vital signs, including mean arterial pressure, heart rate, respiratory rate, and SpO2 before and after extubation; blood gas analysis indexes including pH, oxygen saturation, PaO2, and PaCO2 before and after extubation. The incidence of respiratory complications, including bronchospasm, laryngeal edema, aspiration atelectasis, hypoxemia, and hypercapnia were reported in the included studies. The majority of these studies reported that PPET can maintain stable vital signs and blood gas analysis indices, as well as prevent complications during the peri-extubation period. Nevertheless, one study (18) showed that PPET did not appear to delay the onset of hyposaturation or reduce the need for oxygen therapy during the first 10 min after extubation, but its patients underwent short-term ventilation. In addition, the most significant differences between the two groups came from small- sample studies, and the largest multicenter study (19) showed no significant differences between NPET and PPET groups. Four studies reported extubation failure of the two techniques. Two (4, 7) reported a significant decrease in extubation failure, and the other two (19, 20) reported no significant differences.
Discussion
In theory, PPET has potential advantages over NPET, based on the concept of lung opening and reducing aspiration to maximize alveolar recruitment. A study on newborns has confirmed that compared to NPET, PPET reduces the rate of post-extubation atelectasis (24), and positive-pressure ventilation with oxygen can be provided with a bag-valve device during endotracheal extubation.
However, because secretions accumulate in the subglottic space during invasive mechanical ventilation, they can be aspirated into the airways during cuff deflation and tracheal extubation. This may not be associated with clinical manifestations at the time but may lead to pneumonitis or pneumonia. In laboratory research (25), negative suctioning during cuff deflation and extubation was shown to result in increased leakage into the lower respiratory tract. This could be addressed by mechanical ventilation using the pressure support mode at a level of 15/10 cm H2O or 20/5 cm H2O, resulting in minimal leakage. In another laboratory study (26), three extubation methods were designed to measure the leakage of water or artificial sputum (with different viscosities): negative-pressure suction, positive-pressure by a resuscitator, and ventilation following a continuous positive airway pressure mode with the pressure level set at 5, 10, and 20 cm H2O. The results showed that continuous positive airway pressure extubation resulted in less secretion leakage than the other methods. In terms of the different positive pressure levels, the optimal pressure at 5 cm H2O resulted in a smaller amount of secretion leakage, even when viscosity was higher.
In this first scoping review of positive vs. NPETs, we found that PPET was not inferior to NPET, based on the current literature, which may maintain stable vital signs and blood gas analysis indexes, as well as prevent complications during the peri-extubation period in both adults and infants undergoing mechanical ventilation. However, because the settings, patients, and methods of PPET in different studies are inconsistent, and there is a relative risk of publication bias. Furthermore, the use of PPET by adjusting the PEEP level on the ventilator has been shown to save manpower during the extubation process, without increasing safety risks (7). However, this has not been investigated in infants in the literature, and it is important to determine the appropriate ventilator parameters. Extubation failure is an important indicator related to the clinical outcome of patients. Considering that the extubation failure rate is related to many factors, such as disease status, implementation of spontaneous breathing tests and extubation procedures, further clinical trials are needed to verify the effect of PPET on extubation failure.
Moreover, all the outcomes reported in the literature to date reflect short-term effects, with no longer than 72 h of follow-up. Long-term indicators, such as length of hospital stay and cost, did not differ between PPET and NPET.
This study had some limitations. Owing to our review method, we may have missed publications written in languages other than English or Chinese. Considering the heterogeneity of the present PPET articles on subjects, settings, different ways of extubation, differences in follow-up and reporting of results based on the present literature; it is difficult to draw definitive conclusions about the efficacy of PPET. Thus, this article is written as a scoping review to describe the current evidence to identify directions for future research. Given this, randomized controlled trials and cohort studies that compare different methods and pressure levels of PPET, particularly in infants and pediatric patients are needed to answer all clinical questions and verify its safety.
Conclusion
The current literature suggests that PPET is as safe as NPET and may lead to better clinical outcomes, including stable vital signs, improved arterial blood gas analysis results, and a reduced incidence of respiratory complications during extubation. Clinical trials and cohort series with uniform operating standards are required to explore the safety and efficacy of PPET further.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
JL and ZC contributed to study design and conceptualization. FL and JL contributed to databases searching. XQ and XZ contributed to data screening and data extraction. JL and XZ contributed to data synthesis, interpretation, and manuscript drafting. ZC and FL contributed to critical revision. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rassam S, Sandbythomas M, Vaughan RS, Hall JE. Airway management before, during and after extubation: a survey of practice in the United Kingdom and Ireland. Anaesthesia. (2005) 60:995–1001. doi: 10.1111/j.1365-2044.2005.04235.x
2. Andreu MF, Bezzi MG, Dotta ME. Incidence of immediate postextubation complications in critically Ill adult patients. Heart Lung. (2020) 49:774–8. doi: 10.1016/j.hrtlng.2020.09.016
3. Guglielminotti J, Constant I, Murat I. Evaluation of routine tracheal extubation in children: inflating or suctioning technique? Br J Anaesth. (1998) 81:692–5. doi: 10.1093/bja/81.5.692
4. Farhadi R, Nakhshab M, Hojjati A, Khademloo M. Positive versus negative-pressure during removal of endotracheal-tube on prevention of post-extubation atelectasis in ventilated neonates: a randomized controlled trial. Ann Med Surg. (2022) 76:103573. doi: 10.1016/j.amsu.2022.103573
5. AARC Clinical Practice Guideline. Removal of the endotracheal tube-−2007 revision & update. Resp Care. (2007) 52:81–93.
6. Girard TD, Alhazzani W, Kress JP, Ouellette DR, Schmidt GA, Truwit JD, et al. An official American thoracic society/american college of chest physicians clinical practice guideline: liberation from mechanical ventilation in critically ill adults. Rehabilitation protocols, ventilator liberation protocols, and cuff leak tests. Am J Respir Crit Care Med. (2017) 195:120–33. doi: 10.1164/rccm.201610-2075ST
7. Andreu MF, Dotta ME, Bezzi MG, Borello S, Cardoso GP, Dip PC, et al. Safety of positive-pressure extubation technique. Respir Care. (2019) 64:899–907. doi: 10.4187/respcare.06541
8. Hodd J, Doyle A, Carter J, Albarran J, Young P. Extubation in intensive care units in the UK: an online survey. Nurs Crit Care. (2010) 15:281–4. doi: 10.1111/j.1478-5153.2010.00424.x
9. Andreu MF, Bezzi M, Pedace P, Fredes M, Salvati I, Leoz A, et al. Survey on the extubation procedure in intensive care units in Buenos Aires, Argentina. Rev Bras Ter Intensiva. (2019) 31:180–5. doi: 10.5935/0103-507X.20190027
10. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
11. Cai RM, Song YY, Zhou WH. The effect of positive pressure ventilation extubation on cardiovascular indexes of patients with orotracheal intubation after intracardiac opening operation under direct vision. J Nurs. (2008) 15:1–3. doi: 10.3969/j.issn.1008-9969.2008.04.001
12. Cai RM, Song YY, Zhou WH. Effect of positive-pressure ventilation extubation on arterial blood gas indexes on patients undergoing cardiac surgery. Chin J Pract Nurs. (2011) 27:14–7. doi: 10.3760/cma.j.issn.1672-7088.2011.11.043
13. Luo FX, Sheng D, Huang JC, et al. Comparison of two methods of extubation of nasal tracheal intubation in infants after cardiac surgery. Chin J Mod Nurs. (2013) 19:3282–5. doi: 10.3760/cma.j.issn.1672-7088.2013.23.007
14. Zhang Y, Jiang WL. Effect of positive pressure ventilation and laryngeal spray on the removal of tracheal intubation in infants after cardiac surgery. J Nurs. (2014) 21:58–60.
15. Jing K, Yanping G, Xianghuan Q, Haixia W, Hongli Z. The effect of a modified endotracheal extubation method. J Nurs Sci. (2015) 11:12–4. doi: 10.3870/hlxzz.2015.11.012
16. Huang JC, Jiang WL, Luo FX, Deng S, Tang H. Effect of positive-pressure ventilation and laryngeal spray on oxygen saturation of tracheal intubation in infants after cardiac surgery. Today Nurse. (2016) 4:63–4.
17. Wang XL, Luo FX. Effect of positive pressure ventilation extubation on respiratory function in infants after cardiac surgery. Today Nurse. (2016) 1:49–50.
18. L'Hermite J, Wira O, Castelli C, Coussaye J-Ed, Ripart J, Cuvillon P. Tracheal extubation with suction vs. positive pressure during emergence from general anaesthesia in adults: a randomised controlled trial. Anaesth Crit Care Pain Med. (2018) 37:147–53. doi: 10.1016/j.accpm.2017.07.005
19. Andreu M, Bertozzi M, Bezzi M, Borello S, Castro D, Di Giorgio V, et al. Comparison of two extubation techniques in critically ill adult subjects: the ExtubAR randomized clinical trial. Respir Care. (2021) 2021:respcare.09276. doi: 10.4187/respcare.09276
20. Fei L, Chen LF, Huan D, Qin S. Effect of positive pressure extubation in ICU patients with ortracheal intubation. J Qiqihar Med Univ. (2020) 41:2083–6. doi: 10.3969/j.issn.1002-1256.2020.16.042
21. Yousefshahi F, Barkhordari K, Movafegh A, Tavakoli V, Paknejad O, Bina P, et al. A new method for extubation: comparison between conventional and new methods. J Tehran Heart Cent. (2012) 7:121–7.
22. Xu PF, Li XD, Ge HQ. The impact of two methods of extubation on the occurrence of extubation complications. Chin J Emerg Crit Care Nurs. (2020) 1:512–5. doi: 10.3761/j.issn.2096-7446.2020.06.007
23. Liu S, Ye Z, Zou H, Mei C, Hu Z, Xu W, et al. [Comparison of positive and negative pressure extubation after mechanical ventilation in intensive care unit patients]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. (2022). 34:265–8. doi: 10.3760/cma.j.cn121430-20211022-01545
24. Ortega R, Connor C, Rodriguez G. Endotracheal extubation. N Engl J Med. (2014) 370:1267–8. doi: 10.1056/NEJMc1401725
25. Andreu MF, Salvati IG, Donnianni MC, Ibañez B, Cotignola M, Bezzi M. Effect of applying positive pressure with or without endotracheal suctioning during extubation: a laboratory study. Respir Care. (2014) 59:1905–11. doi: 10.4187/respcare.03121
Keywords: airway extubation, extubation complications, extubation methods, positive-pressure extubation, positive-pressure respiration, ventilator weaning
Citation: Liu J, Li F, Qi X, Zhuang X and Cui Z (2023) Positive- vs. negative-pressure extubation technique: a scoping review. Front. Med. 10:1169879. doi: 10.3389/fmed.2023.1169879
Received: 20 February 2023; Accepted: 19 April 2023;
Published: 12 May 2023.
Edited by:
Ramadan A. Mahmoud, Sohag University, EgyptReviewed by:
Steve Frost, University of Wollongong, AustraliaCarmen Silvia Valente Barbas, University of São Paulo, Brazil
Copyright © 2023 Liu, Li, Qi, Zhuang and Cui. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhaomei Cui, Y3Vpemhhb21laTE5ODFAMTYzLmNvbQ==
 Jing Liu
Jing Liu Fang Li
Fang Li