- 1Department of Hematology, Colentina Clinical Hospital, Bucharest, Romania
- 2Titu Maiorescu University, Bucharest, Romania
The tolerance of the immune system for the semi-allogeneic embryo is promoted by several factors and the cells involved in the immune system and factors in the mother during pregnancy. The dysregulation of the immune responses between the mother and fetus is a risk factor that raises the likelihood of rejection of the embryo and reproductive failure. To safeguard embryos and prevent immunological attacks, it is critical to suppress immunological rejection and encourage immunological tolerance. Based on current medical literature, it seems that immune cell management through immunosuppressive therapies can address reproductive failures. Immunosuppressive treatment has demonstrated encouraging results in terms of enhancing outcomes related to pregnancy and rates of live birth by regulating the immune responses of mothers and positively impacting the reproductive processes of humans. Currently, there is scarcity of high-quality data regarding the safety and efficacy of immunosuppressive therapies for children and mothers. Therefore, it is important to exercise caution while selecting use of any immunosuppressive therapy in pregnancy. This mini review provides a comprehensive overview of the existing literature regarding the impact of Calcineurin Inhibitors and anti-TNF treatment on improving the live birth rate following embryo transfer.
Introduction
While having a child is a momentous occasion in life, the ability to conceive without assistance is frequently uncertain. Around 15 % of couples in the global reproductive population experience infertility (1). In recent strides made in scientific research, assisted reproductive technology (ART) has been a major breakthrough for couples who were previously not able to conceive and has also helped in the detection of early miscarriages. However, with the advancement of ART, a new hurdle has come to light, known as recurrent implantation failure (RIF) (2), which poses a challenge for couples trying to achieve a successful pregnancy. Implantation is the process in which the embryo attaches to the luminal surface of the endometrium (3). Successful implantation is indicated by the detection of an intrauterine gestational sac through ultrasonography (4). Negative pregnancy tests and the absence of a visible gestational sac can result from implantation failure during the initial phases of embryo migration or attachment (5). Implantation failure may also occur at a later stage after the embryo has successfully migrated through the endometrial luminal surface and started producing hCG, which can be identified in blood or urine. However, if gestational sac formation is impaired before it can occur, the implantation process will be hindered (5). The implantation rate can be described as the proportion of embryos that result in the production of gestational sacs to the total number of embryos that are transported into the uterine cavity (4).
Studies have shown that the implantation rate during the IVF process is higher when embryos are transferred on day 5 or 6 (40%) compared to day 2 or 3 (25%) (5). Repeated implantation failure (RIF) is a condition that occurs in patients utilizing assisted reproductive techniques where multiple cycles of in vitro fertilization and transfer of several high-quality embryos fail to result in a clinical pregnancy (6). Coughlan et al. (5, 7) proposed a commonly accepted definition of RIF which states that the absence of a successful clinical pregnancy in women who are younger than 40 years of age despite a minimum of four good-quality embryos have been transferred in at least three fresh or frozen cycles. The process of implantation is complex and RIF can be influenced by several factors of maternal or embryonic origin. Successful implantation of the embryo, which is considered a homozygous hemizygous antigen, is dependent on various factors (6, 7). For successful embryo synchronization following transfer into the uterine cavity, it is essential that the endometrium is receptive, and that the maternal immune system is able to tolerate the presence of the paternal alloantigen throughout the pregnancy (8). There are several potential factors that may contribute to impaired endometrium receptivity and defective maternal-fetal immunotolerance, including uterine abnormalities, infections, metabolic or hormonal disorders, immunological factors, severe male factors, thrombophilias, or an abnormal immune response. Furthermore, inflammation is believed to have a significant influence on pregnancy and can profoundly affect its outcome (8). While thrombophilia was previously considered as a cause for recurrent abortions when no genetic, local, or infectious causes were identified, recent attention has shifted towards the immunological aspect of pregnancy. Due to this, the need for balancing and immunomodulation has emerged to improve rate of successful pregnancy. Various immunosuppressive drugs have been studied for their potential in this regard. However, ethical considerations limit the scope of such studies to a small patient population. Previously immunosuppressive treatments such as corticosteroids, intravenous immunoglobulin (IVIG), and hydroxychloroquine has shown improved outcomes in some studies (9–11). However, the use of these treatments after an embryo transfer to increase the rate of live birth remains controversial (12). Furthermore, the use of these drugs has been incorporated into IVF protocols in many European Union countries. The recommendations for the utilization of immunosuppressive treatment in clinical practice are based on a relatively low level of evidence which necessitates careful consideration for their use in pregnancy. Methotrexate, mycophenolate, teriflunomide, and mitoxantrone are contraindicated in pregnancy due to their known teratogenic effects. When considering the use of anti-TNF-alpha agents and mTOR inhibitors in the context of pregnancy, it is important to exercise caution as there is limited experience with these drugs in pregnant patients (13). Currently, almost all immunosuppressive and immunomodulatory therapies carry little evidence regarding safety and efficacy for children and mothers. However, these agents have been used in pregnancy for other reasons such as atopic dermatitis which can impart significant clinical benefits (14). Thus, it is essential to gain a deeper understanding of the scientific basis of their use. This mini review aims to provide a comprehensive overview of the current evidence concerning the role of Calcineurin Inhibitors and anti-TNF treatment in enhancing live birth rates.
Recurrent implantation failure and immune system
The immunological response in pregnancy is a highly intricate and multifaceted process, characterized by the co-existence of both inflammatory and anti-inflammatory mechanisms. The successful outcome of pregnancy hinges on the intricate interplay between these processes. It has been well-established that implantation is marked by a restrained inflammatory state, while mid-pregnancy is marked by a predominance of anti-inflammatory processes. However, as parturition approaches, there is renewed activation of inflammatory pathways (8, 15). Immune cells such as natural killer (NK) cells, dendritic cells, macrophages, and T cells are present in the endometrium and have different functions in regulating endometrial receptivity and facilitating embryo implantation (16). The success of embryo implantation and development is also influenced by immune-related cytokines such as interleukin (IL)-6, IL-10, IL-15, IL-17, interferon gamma (IFN-γ), tumor necrosis factor alpha (TNF-α), and nuclear factor kappa B (NF-κB), which are present in the intima (16, 17). The failure of embryo implantation may be attributed to a decrease in endometrial receptivity, which can result from dysregulation of the endometrial immune profile (2, 5, 18). Studies have reported that a majority of RIF patients, specifically 81.7%, exhibit dysregulation in their endometrial immune profiles. Furthermore, among RIF patients, overactivation of the immune system has been observed in 56.6% of cases while low activation has been observed in 25% (2). Therefore, addressing this mechanism could potentially enhance the chances of successful pregnancies in patients with RIF.
Maternal immune tolerance is induced during the window of implantation (WOI) through a substantial influx of immune cells to shelter the embryo from refusal (19). Maternal immune tolerance during pregnancy is maintained by the delicate interplay of cytokine signals, which is facilitated by immune cells such as T-helper cells (Th1, Th2, and Th17) and regulatory T-cells (Treg) (20). T-helper cells (Th1) play a role in cell-mediated immunity by producing cytokines such as interleukin-2 (IL-2), tumor necrosis factor-alpha (TNF-α), and interferon gamma (IFN-γ), which can trigger inflammation and there is a dominance of Th1 in peri-implantation phase and the regulated TH1 immunity is advantageous for the invading trophoblasts rather than causing harm. On the other hand, Th2 cells are responsible for humoral responses and produce anti-inflammatory cytokines like IL-4 and IL-10. Following successful implantation, the immune response of the endometrial lining transitions from a cell-mediated to a humoral response. At the site of placental implantation, the prevailing TH2 immunity supersedes TH1 immunity and helps to safeguard the fetus by maintaining a balance between the two immune responses and supporting the growth and development of the placenta. However, if there is an unequal distribution of Th1 and Th2 cells and their cytokines, it can lead to implantation failure (18).
Recent studies have brought to light the crucial role of natural killer (NK) cells in pregnancy (8). The functionality of NK cells is governed by a balance between activating and inhibiting signals, which not only confer direct cytotoxic properties but also exert protective effects via cytokine production. NK cells are categorized into three different groups based on their receptor families, namely, killer immunoglobulin-like receptors, C-type lectin family (CD94/NKGs), and immunoglobulin-like transcripts (ILTs or LIRs), and their receptor repertoires vary between individuals. During the pre-ovulatory stage of the menstrual cycle, the number of NK cells is minimal, but it increases during the secretory phase as progesterone levels rise (21). In the event of pregnancy, NK cells comprise approximately 70% of all mononuclear cells in the decidua and exhibit their full range of activating receptors, including NKp44, which is frequently observed post-NK cell activation (22). Reduced levels of NKp44 have been linked to reproductive failure. It is worth noting that uterine NK cells are distinct from peripheral blood cells since they are primarily CD56brightCD16−, whereas blood NK cells are CD56dimCD16+. Uterine NK cells perform a critical function in establishing a normal pregnancy by communicating directly with invading trophoblasts (23). They exhibit cytotoxic activity to regulate trophoblast invasion and modulate the immune response locally via TH2- and TH3-type cytokines. However, they can also express classical NK cytotoxicity and alloimmune reactions, leading to the recognition of the fetus as “non-self (22).” The involvement of natural killer (NK) cell cytotoxicity in adverse pregnancy outcomes is well-established. In a study by Hadinedoushan et al. (24), NK cytotoxicity was significantly higher in recurrent spontaneous abortion patients compared to healthy controls. Similar observations were reported by Yamada et al. (25) who identified preconception NK abnormalities as a significant cause of recurrent abortions in females. Thum et al. (26) investigated predictors of successful in vitro fertilization outcomes and found that serum tumor necrotic factor (TNF)-alpha and interferon (IFN)-gamma levels had no relation with recurrent abortion. However, high levels of TNF-alpha and IFN-gamma were associated with elevated levels of activated NK cells, which could be a risk factor for subsequent abortion. Perricone et al. (27) suggested immunotherapy to reduce the high levels of NK cells in such patients.
For a pregnancy to be successful, it is crucial that the mother’s immune system does not attack and refuse the fetus. One of the crucial mechanisms for the success of pregnancy involves the suppression of T helper (Th) 1 cells and the upregulation of Th2 cells. This is known to be an essential process for down-regulating the cellular immune response (28, 29). Earlier studies on Th1/Th2 immune responses during pregnancy have demonstrated that both in murine models as well as human pregnancy, there is a significant inclination towards Th2-type reactions at both systemic sites (30, 31) and the fetomaternal interface (28).Treatment with immunoregulatory therapy might be able to show beneficial effects in addressing immune imbalances. The use of medications such as prednisone (PDN), cyclosporine (CsA), or hydroxychloroquine (HCQ), has been shown to suppress the secretion of Th1 cytokines, enhance the regulatory T cells’ number, and promote the development of maternal-fetal acceptance (32). Immunosuppressants such as tacrolimus have been found to be effective in the case of implantation refusal or recurrent loss of pregnancy (33, 34). Since the prevalence of in vitro process of fertilization (IVF) and embryo transfer (ET) has increased significantly in current times on a global scale (35) which has been accompanied by a rise in the number of women who have undergone multiple unsuccessful attempts of IVF including repeated implantation failures (RIFs), the importance of immunosuppressants cannot be ignored.
Successful embryo implantation and immunosuppressants
Between 2 and 5 days after conception, an embryo is transplanted to the uterus through in vitro process of fertilization (IVF) and embryo transfer (ET). Successful implantation of the embryo into the maternal decidua, which involves building up the immunological tolerance of mother to the semi-allograft embryo, is necessary for pregnancy to occur (36). Successful implantation depends on establishing appropriate immune responses during the implantation process, which suggests that immune factors may contribute to repeated implantation failures (RIFs) following IVF/ET. The immune response involves the interplay of Th1 and Th2 cells, which are responsible for promoting either immune tolerance or rejection (37). There is a consensus that during pregnancy, there is a prevalence of immune response of T helper 2 (Th2), while an immune response of T helper 1 (Th1) is associated with refusal of the embryo (8, 38, 39). Therefore, the Th1/Th2 equilibrium model has been suggested to account for maternal-fetal immune interactions during pregnancy because critical roles in immunological responses are played by T helper cells (Th1 and Th2), which are responsible for either increasing immune acceptance or refusal (40). In general, pregnancy is characterized by a prevalence of immune response of T helper 2 (Th2), except during parturition and implantation. Conversely, an excessive immune response of T helper 1 (Th1; including TNF-α and IFN-γ) at the time of implantation is connected with miscarried implantation, early loss of pregnancy, and recurrent pregnancy loss (8, 38, 39). Women who experience RIF following assisted reproductive technology (ART) treatment have been found to have increased proportions of Th1/Th2 cell. However, treatment with immunosuppressants has been shown to enable approximately half of the women with elevated ratios of Th1/Th2 and RIF to achieve pregnancy (18). T helper subtype interactions have been suggested as one of the contributing factors to the success of in IVF pregnancy. However, it is important to note that the local and systemic roles of these interactions vary. Their clinical assessment in IVF units is subpar and so, this tends to affect which and how immunotherapy agents are used.
Tacrolimus as immunosuppressant therapy for reproductive failures
The use of new immunosuppressive agents has significantly improved the survival rate of transplanted grafts, as demonstrated by the notable success achieved in this area (40). One of the primary immunosuppressive agents used to minimize the alloreactivity of the immune system of recipient and lessen the chance of organ refusal following allogeneic organ transplantation is tacrolimus (41). According to studies, tacrolimus can successfully reduce the allograft’s immunological rejection and enhance its longevity. This is accomplished by limiting the formation of cytotoxic T cells, the expression of IL-2 receptors, the proliferation of lymphocytes brought on by alloantigens, and the release of soluble mediators produced by T cells, such as IL2 and IFN-c (42). Although many subsets of T cells are linked to graft-versus-host disease and other immunological disorders including rheumatoid arthritis, tacrolimus has been demonstrated to successfully regulate these conditions (43, 44). Increased Th1 immune response and an elevated ratio of Th1/Th2 cell have been observed in women suffering from RIF (38), indicating the potential for an immune-suppressive agent like tacrolimus to enhance rates of implantation and outcomes of pregnancy in such individuals, particularly those with heightened Th1 immunity.
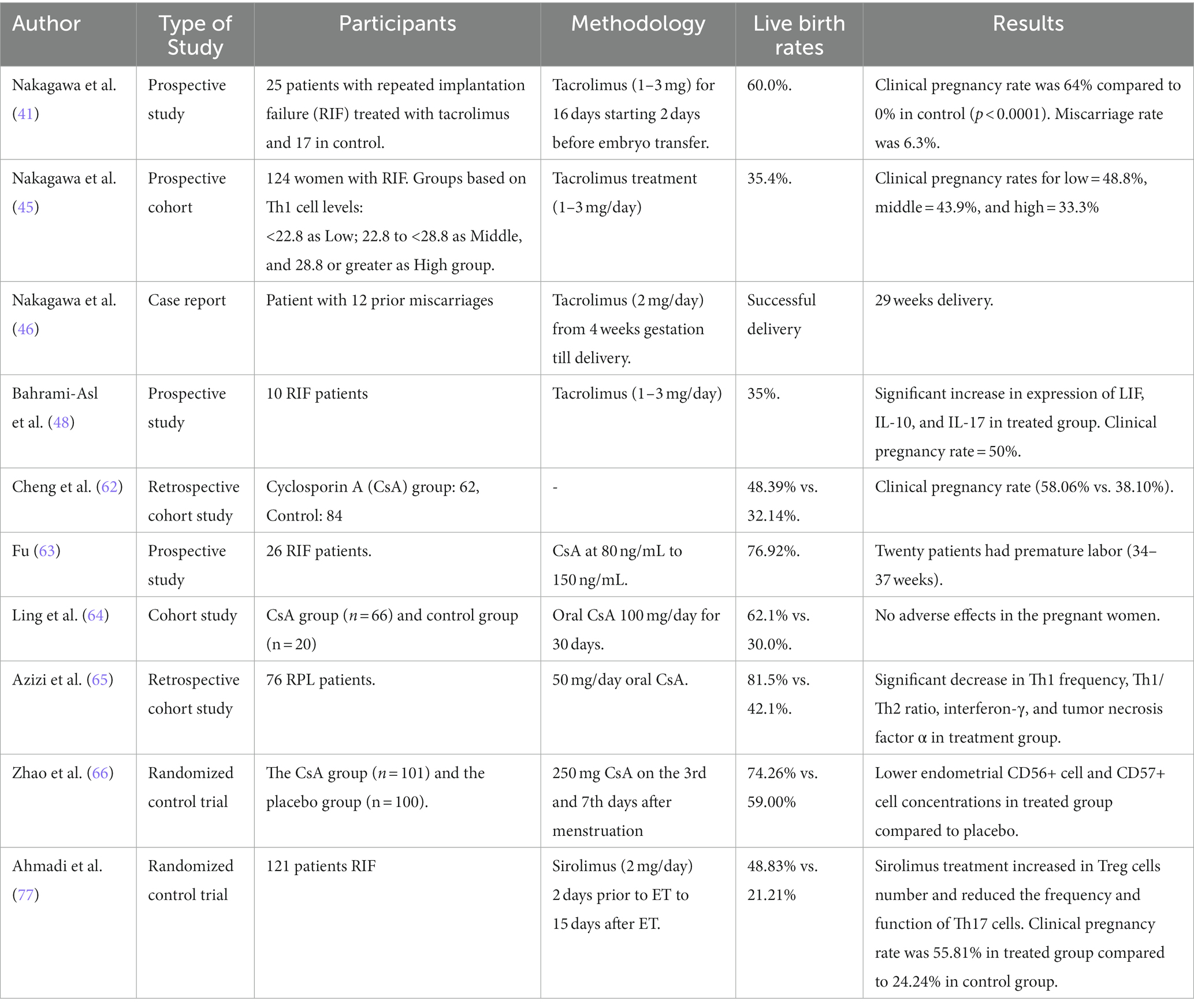
The efficacy of tacrolimus has been tested through years of research. A prospective cohort research was conducted in 2014 evaluating the clinical significance of treatment with tacrolimus in women suffering from RIF. The results were compared between a group who were treated with tacrolimus and who did not receive any treatment. Tacrolimus was administered to the treatment group beginning 2 days before the transfer of embryo and continued until the day pregnancy test was taken. Altogether, it was a period of 16 days. The findings of the research observed that the group who did not receive any treatment had 0 % rate of clinical pregnancy while the group treated with tacrolimus showed 64 % pregnancy rate. The miscarriage rate in the treatment group was found to be 6.3% while percentage of live births was 60 % (18). A 2017 study investigated whether the level of T helper 1 (Th1) cells in peripheral blood could forecast the pregnancy outcome in patients with a past of RIF following ART cycles. The patients who received the treatment were separated into three groups based on the level of Th1 cell. The findings of the research established that a negative connection exists between outcome of pregnancy and Th1 cells in peripheral blood and the proportion of Th1/Th2 cells is a prognostic pointer for the outcome of ART in patients suffering from RIF who received tacrolimus treatment (45).
A case study also reported despite prior treatments with unfractionated heparin, low-dose aspirin, intravenous immunoglobulin, and prednisolone, a patient who was treated with tacrolimus achieved a successful pregnancy after experiencing 12 consecutive miscarriages. The number of Th2 cells were reportedly increase with tacrolimus treatment and the ratio of Th1/Th2 was decreased demonstrating that miscarriage can be avoided with dominance of Th2 cells (46). By securing to the immunophilin FKBP12 (FK506 binding protein), tacrolimus creates a new complex that reduces the activity of peptidyl-prolyl isomerase. This complex, known as FKBP12-FK506, not only interacts with and inhibits calcineurin but also blocks the signal transduction of T-lymphocytes and transcription of IL-2 (47). Another 2020 clinical study determined if tacrolimus treatment for women who had experienced RIF was effective on their endometrium. The study observed that tacrolimus upregulated IL-10, LIF, and IL-17 while down regulates the proportion of IFN-γ/IL-10, IFN-γ, and IL-4 in RIF patients. In RIF patients with high ratios of Th1/Th2 cells, who had previously undergone at least three embryo transfers without success, treatment with tacrolimus resulted in a 40 % rate of implantation, 50 % rate of clinical pregnancy, and thirsty-5 % rate of live births. The study also established a noteworthy association between the intensities of IL-10 and the implantation rate, which showed a positive correlation (48).
A 2022 study investigated the alterations in the populations of Th1 and 2 cells in the peripheral blood of RIF patients who were treated with tacrolimus, delivered a live born baby, and were in the course of pregnancy. Two groups were made based whether the patients have suffered recurrent pregnancy loss (RPL). The study found that in both the groups, tacrolimus treatment suppressed the Th1 immunity, however, in the group with RIF-plus-RPL, it was observed that the percentage of Th1 cells decreased slowly after the start of the treatment (49). In RIF patients, tacrolimus was established to pointedly enhance the expression of IL-10, LIF, and IL-17 while reducing the expression of the proportion of IFN-γ/IL-10, IFN-γ, and IL-4. Moreover, the treatment resulted in a gradual decrease in the numbers of Th1 cells. Given that the group with high concentration of Th1 displayed a markedly lower ongoing rate of pregnancy and higher rate of miscarriage, it is possible that an increase in Th1 cells can cause pregnancy losses and implantation failures. As a result, it is recommended that tacrolimus treatment should not be stopped after the setting up of implantation of embryo in the mother. The safety of tacrolimus has been demonstrated during pregnancy. Furthermore, the use of tacrolimus has also been associated with inhibited fetal malformation rates, restored morphology of spiral arterial modification, and improved uterine arterial and umbilical blood flow (50, 51). Currently, topical tacrolimus is used off-label in young children, however, data on long-term safety is relatively scarce. A study by Salava et al. (52) reported a comparable safety and efficacy of topical tacrolimus (0.03 and 0.1%) and topical corticosteroids in children with AD. Similarly, a review found no evidence of increased infection risk or cancer after a 4-year follow-up in patients who used tacrolimus ointment (53). More comprehensive and randomized controlled studies with double-blind methodology are needed to establish the efficacy of tacrolimus in resolving pregnancy issues caused by immune system anomalies.
Cyclosporin as immunosuppressant therapy for reproductive failures
Cyclosporine (CsA) was first identified as an immunosuppressant in 1976 (54). Both cell-mediated and humoral immune responses are suppressed by it (55). In order to avoid organ refusal or other autoimmune diseases including systemic lupus erythematosus and rheumatoid arthritis, it is frequently administered as an immunosuppressant (56–59). A complex is formed by cyclosporine with cyclophilin to amplify its effect and this complex in turn binds to calcineurin and hinders with the production of lymphokines including IFN-ɣ, TNF-α, and interleukin 2 as well as lymphocyte proliferation (IL-2). These are carried out by inhibiting serine–threonine protein phosphatase activity, which causes the immune system to be downregulated (60). Studies on the effectiveness of cyclosporine in enhancing RIF patients’ outcomes are few. A 2021 study examined the effects of cyclosporine on the outcomes of clinical pregnancy in women who have suffered inexplicable transfer refusal in cycles of frozen–thawed embryo transfer (FET). However, the study was not able to obtain any beneficial results for outcomes of clinical pregnancy (61).
A recent study by Cheng et al. looked at the impact of cyclosporine on outcomes of pregnancy in RIF patients. The study found that the use of cyclosporine after embryo transfer led to a significant improvement in rate of implantation, rate of clinical pregnancy, and rate of live birth among RIF patients, with no increase in the chances of pediatric or obstetric complications (62). Moreover, patients with refractory immune recurrent spontaneous abortion (RSA) who failed to respond to prior therapies with prednisone, aspirin, heparin, IVIG, and lymphocyte immunotherapy, and who were also suffering from antiphospholipid syndrome (APS) were treated with cyclosporine. Cyclosporine was effective in reducing the levels of autoantibodies, resulting in a 76.92% success rate in achieving pregnancy (63). The safety, impact and mode of action of low-dose cyclosporine in RSA patients were evaluated by Ling et al. When pregnancy test came out positive, the treatment group started taking oral cyclosporine at a dose of 100 mg/day for 30 days while the progesterone was used in the control group. Assessments of immunologic parameters were made before and after the treatment. After therapy, maternal blood’s CD3 level increased while its CD8 level decreased. Additionally, the cyclosporine group had a considerably greater live birth rate. There were no negative pregnancy outcomes or side effects (64).
Furthermore, in their trial, Azizi et al. enrolled 76 women with RPL (38 women each group treated with cyclosporine and the control group), and they investigated immunologic parameter changes in addition to pregnancy outcomes before and after the treatment. The results exhibited that after receiving cyclosporine, there was a momentous decrease in the Th1 cells’ frequency, the proportion of Th1/Th2, the expression of T-bet (a Th1-related transcription factor), and the secretion of TNF-α and IFN-ɣ, compared to pre-treatment. No significant changes were observed in the control group. Additionally, cyclosporine significantly increased the Th2 cells’ frequency, the expression of GATA-3, and the IL-10’s release. There was also a significant increase in the rate of successful childbirth in the cyclosporine group (65). Recently, Zhao et al. conducted a randomized controlled trial to scrutinize the intrauterine perfusion efficacy of cyclosporine in women with RSA who were also suffering from endometrial alloimmune dysfunction. The results showed a significantly higher rate of live births in group treated with cyclosporine in contrast to the control group. Additionally, in the second menstrual cycle, the frequency of CD57+ cells and CD56+ cells during the luteal phase o was lower in the cyclosporine group (66). So far, very little evidence is available regarding the safety of CsA, however, it is generally considered safe. Some studies have shown that CsA use can lead to increased risk of preterm birth and low birth weight, however, no congenital defects have been reported (67). CsA can cross placenta and the concentration in fetus has been shown to vary between 37 and 64% compared to maternal concentration (68). Various studies have addressed the use of Cyclosporine among patients with acute myocardial infarction. A systemic review of 6 RCTs reported no serious adverse events in all the studies (69). Similarly, in another study, the safety and efficacy of cyclosporine were shown in children treated for vernal keratoconjunctivitis (70). A case series by Leonardi et al. (71) also concluded that cyclosporine is safe in patients treated with AD. Despite ongoing research, the usefulness of cyclosporine for patients with persistent spontaneous abortion and persistent implantation refusal is currently only partially supported by high-quality data. Given the lack of robust evidence, the use of cyclosporine for these patients is not recommended and should only be used within the context of clinical trials.
Sirolimus as immunosuppressant therapy for reproductive failures
Sirolimus, commonly called rapamycin, is an immunomodulatory agent that has been approved by the FDA for the inhibition of refusal in solid organ transplants. In addition, sirolimus has been shown to have anti-tumor effects. The immunosuppressive action of sirolimus is achieved through its inhibitory effect on the mammalian target of rapamycin (mTOR) kinase pathway, which blocks downstream co-stimulatory signals (72). The T regulatory cells’ expansion, the interception of differentiation of Th17 cell, the bocking of proliferation of T and B lymphocytes by stopping the IL-2 and IL-4’s development, and the reduction of responses due to inflammation are some of the proposed mechanisms through which sirolimus exerts its action in moderating the immune system (73, 74). Sirolimus is not a contraindication for pregnancy, according to the national transplantation pregnancy registry (NTPR), which noted that over 14,000 female transplant patients globally had previous successful pregnancies (75).
Furthermore, animal studies also supported sirolimus’ beneficial effect on gestation. A study on a mouse model of RIF showed that sirolimus was capable to increase the number of Treg cells and improve implantation rates in mice short of regulatory T cells (DEREG) (76). In a Phase II randomized clinical trial conducted by Ahmadi et al., the sirolimus’ impact on immunological abnormalities in women with RIF and a history of at least three implantation failures was evaluated. The trial found that patients with an eminent proportion of Th17/Treg who received sirolimus as treatment experienced a surge in Treg cells and a decrease in Th17 cells and the of Th17/Treg. This was connected with a higher rate of clinical pregnancy and the outcome of live birth in the treatment group in comparison to the control group that were not treated with sirolimus (77). So far, no study has evaluated the effectiveness of sirolimus in enhancing outcomes of pregnancy in women suffering from RPL. As of right now, sirolimus has been utilized in animal models of RIF and for improving the outcomes of pregnancy of women suffering from RIF in the research by Ahamdi et al. The safety of sirolimus has been reported in several small studies; however, no large study is available (78, 79). Furthermore, adverse outcome such as miscarriage low birth weight and preterm delivery but no malformities defected has been reported. Some case studies have reported that placental transfer in sirolimus takes place, however, it is in very low concentrations (80, 81). Sirolimus has been confirmed to be effective in various diseases. A study by Adams et al. reported the safety and efficacy of sirolimus in patients with complicated vascular anomalies. The most common grade 3 or more toxicities in their study were bone marrow toxicity, gastrointestinal toxicity, and metabolic toxicity (82). Similarly, another study reported mild adverse events in lymphangioleiomyomatosis patients treated with sirolimus (83). Even, in the pediatric population, sirolimus has shown safety in childhood diseases (84). Despite the lack of sufficient evidence on the efficacy of sirolimus in cases of reproductive failure, its demonstrated ability to modulate the immune system suggests that it has the prospective to be an encouraging treatment option for reproductive and fertility problems with an immunologic origin (Table 1).
Anti-TNF-α therapy for reproductive failures
Anti-tumor necrosis factor-α (anti-TNF-α) drugs were first introduced in the United States in 1998 to suppress inflammation. These drugs have proven effective in treating autoimmune diseases such as rheumatoid arthritis (85). Elevated levels of TNF-α have been implicated in recurrent miscarriages. Increased TNF-α concentrations can stimulate Th1 cell-mediated immune responses, promote the production of prostaglandin E2, leading to uterine muscle contraction, trigger the activation of the blood coagulation system, and induce upregulation of oxidative stress (86). These effects can result in placental vascular thrombosis and ultimately lead to poor pregnancy outcomes. Adalimumab and Etanercept are FDA-approved anti-TNF-α agents used to treat infertility and miscarriage (85). Adalimumab is a type of recombinant immunoglobulin G1 (IgG1) while Etanercept is a dimeric fusion protein that consists of the soluble form of TNF receptor 2 and the Fc portion of human IgG1 antibody (87). A study has demonstrated that TNF-α inhibitors can be efficacious in enhancing the rates of embryo implantation and improving pregnancy outcomes in women who experience RSA (88).
According a randomized control trial, a total of 95 patients with refractory innate immune RSA received etanercept at a dose of 25 mg per week (89). The results showed that 89.47% of the patients who received etanercept delivered a healthy baby, whereas the corresponding number was only 72.04% in the placebo group. There were also significantly lower levels of TNF-α and NK cell activity during week 4 of gestation (89). Furthermore, administering Etanercept during endometrial preparation has been shown to enhance IVF outcomes in individuals with RIF (90). Furthermore, investigations into Adalimumab have uncovered a rise in the rates of successful pregnancy among women undergoing IVF. This effect is primarily attributed to a decrease in the TNF-α/IL-10 ratio, particularly during the implantation stage (91). Anti-TNF-α therapies such as Etanercept and Adalimumab may be specific and effective strategies to reduce serum TNF-α levels (an inflammatory mediator) and improve pregnancy outcomes in women with RSA or RIF. Several studies have shown that anti-TNF-α does cause negative impacts on maternal and fetal health (92, 93). However, further studies are necessary to fully evaluate the safety of anti-TNF-α during pregnancy.
Conclusion
Many couples have to face the fetal immunological rejection. To avoid this semi-allograft rejection, maternal tolerance to fetal alloantigens is necessary. Numerous investigations on the use of immunosuppressive agents have been conducted in this area to date. While immunosuppressive treatments like tacrolimus, cyclosporine, anti-TNF-α therapy, and sirolimus have shown promise in managing complications related to reproduction and fertility, including RPL and RIF, and have already been used in clinical settings to control reproductive problems but further research is needed to identify the best candidates in addition to negative effects. By manipulating immune cells, these immunosuppressive agents have the power to regulate infertility. Despite conducting extensive research on the subject matter, we encountered a dearth of high-quality studies that could provide robust evidence to support our findings. To protect the fetus from immune responses, there is presently no single treatment strategy with high safety and effectiveness. Therefore, additional evaluation of treatment modalities in the field of reproductive failures need more rigorous clinical trials and experiments.
Author contributions
The author confirms being the sole contributor of this work and has approved it for publication.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Agarwal, A, Mulgund, A, Hamada, A, and Chyatte, MR. A unique view on male infertility around the globe. Reprod Biol Endocrinol. (2015) 13:37. doi: 10.1186/s12958-015-0032-1
2. Lédée, N, Petitbarat, M, Chevrier, L, Vitoux, D, Vezmar, K, Rahmati, M, et al. The uterine immune profile may help women with repeated unexplained embryo implantation failure after in vitro fertilization. Am J Reprod Immunol. (2016) 75:388–401. doi: 10.1111/aji.12483
3. Benkhalifa, M, Demirol, A, Sari, T, Balashova, E, Tsouroupaki, M, Giakoumakis, Y, et al. Autologous embryo-cumulus cells co-culture and blastocyst transfer in repeated implantation failures: a collaborative prospective randomized study. Zygote. (2012) 20:173–80. doi: 10.1017/s0967199411000062
4. Zegers-Hochschild, F, Adamson, GD, De Mouzon, J, Ishihara, O, Mansour, R, Nygren, K, et al. The international committee for monitoring assisted reproductive technology (ICMART) and the world health organization (WHO) revised glossary on ART terminology, 2009. Hum Reprod. (2009) 24:2683–7. doi: 10.1093/humrep/dep343
5. Coughlan, C, Ledger, W, Wang, Q, Liu, F, Demirol, A, Gurgan, T, et al. Recurrent implantation failure: definition and management. Reprod Biomed Online. (2014) 28:14–38. doi: 10.1016/j.rbmo.2013.08.011
6. Bashiri, A, Halper, KI, and Orvieto, R. Recurrent implantation failure-update overview on etiology, diagnosis, treatment and future directions. Reprod Biol Endocrinol. (2018) 16:1–18. doi: 10.1186/s12958-018-0414-2
7. Cakiroglu, Y, and Tiras, B. Determining diagnostic criteria and cause of recurrent implantation failure. Curr Opin Obstet Gynecol. (2020) 32:198–204. doi: 10.1097/GCO.0000000000000620
8. Andreescu, M, Frîncu, F, Plotogea, M, and Mehedințu, C. Recurrent abortion and the involvement of killer-cell immunoglobulin-like receptor (KIR) genes, activated T cells, NK abnormalities, and cytokine profiles. J Clin Med. (2023) 12:1355. doi: 10.3390/jcm12041355
9. Abdolmohammadi-Vahid, S, Pashazadeh, F, Pourmoghaddam, Z, Aghebati-Maleki, L, Abdollahi-Fard, S, and Yousefi, M. The effectiveness of IVIG therapy in pregnancy and live birth rate of women with recurrent implantation failure (RIF): a systematic review and meta-analysis. J Reprod Immunol. (2019) 134-135:28–33. doi: 10.1016/j.jri.2019.07.006
10. Nørgård, BM, Larsen, MD, Friedman, S, and Fedder, J. Corticosteroids prior to embryo transfer in assisted reproduction in women with Crohn's disease and ulcerative colitis—a Nationwide cohort study. Clin Epidemiol. (2020) 12:317–26. doi: 10.2147/clep.S234996
11. Mirzaei, M, Amirajam, S, Moghimi, ES, Behzadi, S, Rohani, A, Zerangian, N, et al. The effects of hydroxychloroquine on pregnancy outcomes in infertile women: a systematic review and meta-analysis. J Med Life. (2023) 16:189–94. doi: 10.25122/jml-2022-0095
12. Lee, KA, Koo, JJ, Yoon, TK, Do, BR, Ko, JJ, and Cha, KY. Immunosuppression by corticosteroid has no effect on the pregnancy rate in routine in-vitro fertilization/embryo transfer patients. Hum Reprod. (1994) 9:1832–5. doi: 10.1093/oxfordjournals.humrep.a138343
13. Leroy, C, Rigot, J-M, Leroy, M, Decanter, C, Le Mapihan, K, Parent, A-S, et al. Immunosuppressive drugs and fertility. Orphanet J Rare Dis. (2015) 10:136. doi: 10.1186/s13023-015-0332-8
14. Heilskov, S, Deleuran, MS, and Vestergaard, C. Immunosuppressive and Immunomodulating therapy for atopic dermatitis in pregnancy: an appraisal of the literature. Dermatol Ther (Heidelb). (2020) 10:1215–28. doi: 10.1007/s13555-020-00457-w
15. Mor, G, Cardenas, I, Abrahams, V, and Guller, S. Inflammation and pregnancy: the role of the immune system at the implantation site. Ann N Y Acad Sci. (2011) 1221:80–7. doi: 10.1111/j.1749-6632.2010.05938.x
16. Bidarimath, M, Khalaj, K, Wessels, JM, and Tayade, C. MicroRNAs, immune cells and pregnancy. Cell Mol Immunol. (2014) 11:538–47. doi: 10.1038/cmi.2014.45
17. Kany, S, Vollrath, JT, and Relja, B. Cytokines in inflammatory disease. Int J Mol Sci. (2019) 20:6008. doi: 10.3390/ijms20236008
18. Nakagawa, K, Kwak-Kim, J, Ota, K, Kuroda, K, Hisano, M, Sugiyama, R, et al. Immunosuppression with tacrolimus improved reproductive outcome of women with repeated implantation failure and elevated peripheral blood TH1/TH2 cell ratios. Am J Reprod Immunol. (2015) 73:353–61. doi: 10.1111/aji.12338
19. Piccinni, M-P, Lombardelli, L, Logiodice, F, Kullolli, O, Romagnani, S, and Le Bouteiller, P. T helper cell mediated-tolerance towards fetal allograft in successful pregnancy. Clin Mol Allergy. (2015) 13:1–5. doi: 10.1186/s12948-015-0015-y
20. Feyaerts, D, Benner, M, van Cranenbroek, B, van der Heijden, OW, Joosten, I, and van der Molen, RG. Human uterine lymphocytes acquire a more experienced and tolerogenic phenotype during pregnancy. Sci Rep. (2017) 7:2884. doi: 10.1038/s41598-017-03191-0
21. Jabrane-Ferrat, N, and Siewiera, J. The up side of decidual natural killer cells: new developments in immunology of pregnancy. Immunology. (2014) 141:490–7. doi: 10.1111/imm.12218
22. Faas, MM, and De Vos, P. Uterine NK cells and macrophages in pregnancy. Placenta. (2017) 56:44–52. doi: 10.1016/j.placenta.2017.03.001
23. Sharma, S. Natural killer cells and regulatory T cells in early pregnancy loss. Int J Dev Biol. (2014) 58:219–29. doi: 10.1387/ijdb.140109ss
24. Hadinedoushan, H, Mirahmadian, M, and Aflatounian, A. Increased natural killer cell cytotoxicity and IL-2 production in recurrent spontaneous abortion. Am J Reprod Immunol. (2007) 58:409–14. doi: 10.1111/j.1600-0897.2007.00524.x
25. Yamada, H, Morikawa, M, Kato, EH, Shimada, S, Kobashi, G, and Minakami, H. Pre-conceptional natural killer cell activity and percentage as predictors of biochemical pregnancy and spontaneous abortion with Normal chromosome karyotype. Am J Reprod Immunol. (2003) 50:351–4. doi: 10.1034/j.1600-0897.2003.00095.x
26. Thum, MY, Abdalla, HI, Bhaskaran, S, Harden, EL, Ford, B, Sumar, N, et al. The relationship of systemic TNF-alpha and IFN-gamma with IVF treatment outcome and peripheral blood NK cells. Am J Reprod Immunol. (2007) 57:210–7. doi: 10.1111/j.1600-0897.2006.00465.x
27. Perricone, R, Di Muzio, G, Perricone, C, Giacomelli, R, De Nardo, D, Fontana, L, et al. High levels of peripheral blood NK cells in women suffering from recurrent spontaneous abortion are reverted from high-dose intravenous immunoglobulins. Am J Reprod Immunol. (2006) 55:232–9. doi: 10.1111/j.1600-0897.2005.00356.x
28. Wegmann, TG, Lin, H, Guilbert, L, and Mosmann, TR. Bidirectional cytokine interactions in the maternal-fetal relationship: is successful pregnancy a TH2 phenomenon? Immunol Today. (1993) 14:353–6. doi: 10.1016/0167-5699(93)90235-D
29. Lin, H, Mosmann, TR, Guilbert, L, Tuntipopipat, S, and Wegmann, TG. Synthesis of T helper 2-type cytokines at the maternal-fetal interface. J Immunol (Baltimore, Md: 1950). (1993) 151:4562–73.
30. Dudley, DJ, Chen, C-L, Mitchell, MD, Daynes, RA, and Araneo, BA. Adaptive immune responses during murine pregnancy: pregnancy-induced regulation of lymphokine production by activated T lymphocytes. Am J Obstet Gynecol. (1993) 168:1155–63. doi: 10.1016/0002-9378(93)90361-L
31. Hill, JA, Polgar, K, and Anderson, DJ. T-helper 1-type immunity to trophoblast in women with recurrent spontaneous abortion. JAMA. (1995) 273:1933–6. doi: 10.1001/jama.1995.03520480053039
32. Ghasemnejad-Berenji, H, Novin, MG, Hajshafiha, M, Nazarian, H, Hashemi, S, Ilkhanizadeh, B, et al. Immunomodulatory effects of hydroxychloroquine on Th1/Th2 balance in women with repeated implantation failure. Biomed Pharmacother. (2018) 107:1277–85. doi: 10.1016/j.biopha.2018.08.027
33. Zand, MS. Immunosuppression and immune monitoring after renal transplantation. Sem in Dial. (2005). 18:511–9. doi: 10.1111/j.1525-139X.2005.00098.x
34. Brogan, P, and Dillon, M. The use of immunosuppressive and cytotoxic drugs in non-malignant disease. Arch Dis Child. (2000) 83:259–64. doi: 10.1136/adc.83.3.259
35. Sunderam, S, Kissin, DM, Zhang, Y, Folger, SG, Boulet, SL, Warner, L, et al. Assisted reproductive technology surveillance—United States, 2016. MMWR Surveill Summ. (2019) 68:1–23. doi: 10.15585/mmwr.ss6804a1
36. Schjenken, JE, Tolosa, JM, Paul, JW, Clifton, VL, and Smith, R. Mechanisms of maternal immune tolerance during pregnancy In: Recent Advances in Research on the Human Placenta, eds Jing Zheng, Intech Open (2012). 211–42.
37. Saito, S, Nakashima, A, Shima, T, and Ito, M. Th1/Th2/Th17 and regulatory T-cell paradigm in pregnancy. Am J Reprod Immunol. (2010) 63:601–10. doi: 10.1111/j.1600-0897.2010.00852.x
38. Kwak-Kim, J, Chung-Bang, H, Ng, S, Ntrivalas, E, Mangubat, C, Beaman, K, et al. Increased T helper 1 cytokine responses by circulating T cells are present in women with recurrent pregnancy losses and in infertile women with multiple implantation failures after IVF. Hum Reprod. (2003) 18:767–73. doi: 10.1093/humrep/deg156
39. Ng, SC, Gilman-Sachs, A, Thaker, P, Beaman, KD, Beer, AE, and Kwak-Kim, J. Expression of intracellular Th1 and Th2 cytokines in women with recurrent spontaneous abortion, implantation failures after IVF/ET or normal pregnancy. Am J Reprod Immunol. (2002) 48:77–86. doi: 10.1034/j.1600-0897.2002.01105.x
40. Goring, SM, Levy, AR, Ghement, I, Kalsekar, A, Eyawo, O, L'Italien, GJ, et al. A network meta-analysis of the efficacy of belatacept, cyclosporine and tacrolimus for immunosuppression therapy in adult renal transplant recipients. Curr Med Res Opin. (2014) 30:1473–87. doi: 10.1185/03007995.2014.898140
41. Morales, JM, Andrés, A, Dominguez-Gil, B, Arriola, M, Gutiérrez, MJ, Hernández, E, et al. Ten years of treatment with tacrolimus is related to an excellent renal function, allowing monotherapy in a large proportion of cases: unicentric results of the tacrolimus versus cyclosporine a European multicentric study in kidney transplant patients. Transplant Proc. (2005) 37:3738–42. doi: 10.1016/j.transproceed.2005.09.178
42. Kino, T, Hatanaka, H, Hashimoto, M, Nishiyama, M, Goto, T, Okuhara, M, et al. FK-506, a novel immunosuppressant isolated from a Streptomyces. I. Fermentation, isolation, and physico-chemical and biological characteristics. J Antibiot (Tokyo). (1987) 40:1249–55. doi: 10.7164/antibiotics.40.1249
43. Ramiro, S, Gaujoux-Viala, C, Nam, JL, Smolen, JS, Buch, M, Gossec, L, et al. Safety of synthetic and biological DMARDs: a systematic literature review informing the 2013 update of the EULAR recommendations for management of rheumatoid arthritis. Ann Rheum Dis. (2014) 73:529–35. doi: 10.1136/annrheumdis-2013-204575
44. Ram, R, Gafter-Gvili, A, Yeshurun, M, Paul, M, Raanani, P, and Shpilberg, O. Prophylaxis regimens for GVHD: systematic review and meta-analysis. Bone Marrow Transplant. (2009) 43:643–53. doi: 10.1038/bmt.2008.373
45. Nakagawa, K, Kwak-Kim, J, Kuroda, K, Sugiyama, R, and Yamaguchi, K. Immunosuppressive treatment using tacrolimus promotes pregnancy outcome in infertile women with repeated implantation failures. Am J Reprod Immunol. (2017) 78. doi: 10.1111/aji.12682
46. Nakagawa, K, Kuroda, K, Sugiyama, R, and Yamaguchi, K. After 12 consecutive miscarriages, a patient received immunosuppressive treatment and delivered an intact baby. Reprod Med Biol. (2017) 16:297–301. doi: 10.1002/rmb2.12040
47. Liu, J, Farmer, JD Jr, Lane, WS, Friedman, J, Weissman, I, and Schreiber, SL. Calcineurin Is a Common Target of Cyclophilin-Cyclosporin a and Fkbp-Fk506 Complexes. Cells (1991). 66:807–815. doi: 10.1016/0092-8674(91)90124-h
48. Bahrami-Asl, Z, Farzadi, L, Fattahi, A, Yousefi, M, Quinonero, A, Hakimi, P, et al. Tacrolimus improves the implantation rate in patients with elevated Th1/2 helper cell ratio and repeated implantation failure (RIF). Geburtshilfe Frauenheilkd. (2020) 80:851–62. doi: 10.1055/a-1056-3148
49. Hisano, M, Nakagawa, K, Kwak-Kim, J, Sugiyama, R, Sago, H, and Yamaguchi, K. Changes in the T-helper 1 and 2 cell populations during pregnancy in tacrolimus-treated women with repeated implantation failure and recurrent pregnancy loss. Hum Fertil (Camb). (2022) 25:975–82. doi: 10.1080/14647273.2021.1955415
50. Albaghdadi, AJH, Hewitt, MA, Putos, SM, Wells, M, Ozolinš, TRS, and Kan, FWK. Tacrolimus in the prevention of adverse pregnancy outcomes and diabetes-associated embryopathies in obese and diabetic mice. J Transl Med. (2017) 15:32. doi: 10.1186/s12967-017-1137-4
51. Boulay, H, Mazaud-Guittot, S, Supervielle, J, Chemouny, JM, Dardier, V, Lacroix, A, et al. Maternal, foetal and child consequences of immunosuppressive drugs during pregnancy in women with organ transplant: a review. Clin Kidney J. (2021) 14:1871–8. doi: 10.1093/ckj/sfab049
52. Salava, A, Perälä, M, Pelkonen, A, Mäkelä, M, and Remitz, A. Safety of tacrolimus 0.03 and 0.1% ointments in young children with atopic dermatitis: a 36-month follow-up study. Clin Exp Dermatol. (2022) 47:889–902. doi: 10.1111/ced.15024
53. Remitz, A, and Reitamo, S. Long-term safety of tacrolimus ointment in atopic dermatitis. Expert Opin Drug Saf. (2009) 8:501–6. doi: 10.1517/14740330902969441
54. Borel, JF. History of the discovery of cyclosporin and of its early pharmacological development. Wien Klin Wochenschr. (2002) 114:433–7. Available at: https://pubmed.ncbi.nlm.nih.gov/12422576/
55. Atreya, R, Weigmann, B, Bartsch, B, Galle, P, and Neurath, M. W1151 a mechanism of action for cyclosporine a in ulcerative colitis: the role of the Tec kinase Itk in disease pathogenesis. Gastroenterology. (2008) 134:A–644. doi: 10.1016/S0016-5085(08)63005-X
56. Sketris, I, Yatscoff, R, Keown, P, Canafax, DM, First, MR, Holt, DW, et al. Optimizing the use of cyclosporine in renal transplantation. Clin Biochem. (1995) 28:195–211. doi: 10.1016/0009-9120(95)91341-y
57. Germano, V, Picchianti Diamanti, A, Ferlito, C, Podestà, E, Salemi, S, Migliore, A, et al. Cyclosporine a in the long-term management of systemic lupus erythematosus. J Biol Regul Homeost Agents. (2011) 25:397–403. Available at: https://pubmed.ncbi.nlm.nih.gov/22023764/
58. Hetland, ML. Modern treatment strategies in rheumatoid arthritis. Dan Med Bull. (2011) 58:B4320. Available at: https://ugeskriftet.dk/dmj/modern-treatment-strategies-rheumatoid-arthritis
59. Tang, C, Chen, L, Gu, W, Du, M, Li, M, Chen, Q, et al. Cyclosporin a enhances the ability of trophoblasts to displace the activated human umbilical vein endothelial cell monolayers. Int J Clin Exp Pathol. (2013) 6:2441–50. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3816813/
60. Archer, TM, Stokes, JV, Kummari, E, Fellman, C, Thomason, J, Haraschak, J, et al. In vivo effects of aspirin and cyclosporine on regulatory T cells and T-cell cytokine production in healthy dogs. Vet Immunol Immunopathol. (2018) 197:63–8. doi: 10.1016/j.vetimm.2018.01.003
61. Qu, D, Tian, X, Ding, L, Li, Y, and Zhou, W. Impacts of Cyclosporin a on clinical pregnancy outcomes of patients with a history of unexplained transfer failure: a retrospective cohort study. Reprod Biol Endocrinol. (2021) 19:44. doi: 10.1186/s12958-021-00728-x
62. Cheng, W, Wu, Y, Wu, H, Zou, Q, Meng, Q, Wang, F, et al. Improved pregnancy outcomes of cyclosporine a on patients with unexplained repeated implantation failure in IVF/ICSI cycles: a retrospective cohort study. Am J Reprod Immunol. (2022) 87:e13525. doi: 10.1111/aji.13525
63. Fu, JH. Analysis of the use of cyclosporin a to treat refractory immune recurrent spontaneous abortion. Clin Exp Obstet Gynecol. (2015) 42:739–42. doi: 10.12891/ceog2006.2015
64. Ling, Y, Huang, Y, Chen, C, Mao, J, and Zhang, H. Low dose Cyclosporin a treatment increases live birth rate of unexplained recurrent abortion—initial cohort study. Clin Exp Obstet Gynecol. (2017) 44:230–5. doi: 10.12891/ceog3375.2017
65. Azizi, R, Ahmadi, M, Danaii, S, Abdollahi-Fard, S, Mosapour, P, Eghbal-Fard, S, et al. Cyclosporine a improves pregnancy outcomes in women with recurrent pregnancy loss and elevated Th1/Th2 ratio. J Cell Physiol. (2019) 234:19039–47. doi: 10.1002/jcp.28543
66. Zhao, L, Qi, L, Fu, J, Bi, S, Li, L, and Fu, Y. Efficacy of intrauterine perfusion of Cyclosporin a for intractable recurrent spontaneous abortion patients with endometrial alloimmune disorders: a randomized controlled trial. Front Physiol. (2021) 12:737878. doi: 10.3389/fphys.2021.737878
67. Paziana, K, Del Monaco, M, Cardonick, E, Moritz, M, Keller, M, Smith, B, et al. Ciclosporin use during pregnancy. Drug Saf. (2013) 36:279–94. doi: 10.1007/s40264-013-0034-x
68. Bar Oz, B, Hackman, R, Einarson, T, and Koren, G. Pregnancy outcome after cyclosporine therapy during pregnancy: a meta-analysis. Transplantation. (2001) 71:1051–5. doi: 10.1097/00007890-200104270-00006
69. Rahman, FA, Abdullah, SS, Manan, WZWA, Tan, LT-H, Neoh, C-F, Ming, LC, et al. Efficacy and safety of cyclosporine in acute myocardial infarction: a systematic review and Meta-analysis. Front Pharmacol. (2018) 9:9. doi: 10.3389/fphar.2018.00238
70. Bourcier, T, Dory, A, Dormegny, L, Alcazar, J, Gaucher, D, and Sauer, A. Efficacy and safety of 0.1% cyclosporine versus 2% cyclosporine in the treatment of severe vernal Keratoconjunctivitis in children. Clin Ophthalmol. (2022) 16:3589–96. doi: 10.2147/OPTH.S370414
71. Leonardi, S, Marchese, G, Rotolo, N, Miraglia Del Giudice, M, and La Rosa, M. Cyclosporin is safe and effective in severe atopic dermatitis of childhood. Rep Three Cases Minerva Pediatr. (2004) 56:231–7. Available at: https://pubmed.ncbi.nlm.nih.gov/15249910/
72. Law, BK. Rapamycin: an anti-cancer immunosuppressant? Crit Rev Oncol Hematol. (2005) 56:47–60. doi: 10.1016/j.critrevonc.2004.09.009
73. Mehrabi, A, Fonouni, H, Kashfi, A, Schmied, BM, Morath, C, Sadeghi, M, et al. The role and value of sirolimus administration in kidney and liver transplantation. Clin Transpl. (2006) 20:30–43. doi: 10.1111/j.1399-0012.2006.00598.x
74. Kopf, H, de la Rosa, GM, Howard, OM, and Chen, X. Rapamycin inhibits differentiation of Th17 cells and promotes generation of FoxP3+ T regulatory cells. Int Immunopharmacol. (2007) 7:1819–24. doi: 10.1016/j.intimp.2007.08.027
75. Coscia, LA, Constantinescu, S, Moritz, MJ, Frank, AM, Ramirez, CB, Maley, WR, et al. Report from the National Transplantation Pregnancy Registry (NTPR): outcomes of pregnancy after transplantation. Clin Transpl. (2010) 105730:65–85. Available at: https://terasaki.org/store/CH7-Coscia_2010
76. Royster, GD, Harris, JC, Nelson, A, Castro, Y, Weitzel, RP, Tisdale, J, et al. Rapamycin corrects T regulatory cell depletion and improves embryo implantation and live birth rates in a murine model. Reprod Sci. (2019) 26:1545–56. doi: 10.1177/1933719119828110
77. Ahmadi, M, Abdolmohamadi-Vahid, S, Ghaebi, M, Dolati, S, Abbaspour-Aghdam, S, Danaii, S, et al. Sirolimus as a new drug to treat RIF patients with elevated Th17/Treg ratio: a double-blind, phase II randomized clinical trial. Int Immunopharmacol. (2019) 74:105730. doi: 10.1016/j.intimp.2019.105730
78. Framarino-dei-Malatesta, M, Derme, M, Napoli, A, Iaria, G, Manzia, TM, Orlando, G, et al. Placental, lipid, and glucidic effects of mammalian target of rapamycin inhibitors: impact on fetal growth and metabolic disorders during pregnancy after solid organ transplantation. Transplant Proc. (2014) 46:2254–8. doi: 10.1016/j.transproceed.2014.07.047
79. Sifontis, NM, Coscia, LA, Constantinescu, S, Lavelanet, AF, Moritz, MJ, and Armenti, VT. Pregnancy outcomes in solid organ transplant recipients with exposure to mycophenolate mofetil or sirolimus. Transplantation. (2006) 82:1698–702. doi: 10.1097/01.tp.0000252683.74584.29
80. Pluym, ID, Sklansky, M, Wu, JY, Afshar, Y, Holliman, K, Devore, GR, et al. Fetal cardiac rhabdomyomas treated with maternal sirolimus. Prenat Diagn. (2020) 40:358–64. doi: 10.1002/pd.5613
81. Park, H, Chang, CS, Choi, SJ, Oh, SY, and Roh, CR. Sirolimus therapy for fetal cardiac rhabdomyoma in a pregnant woman with tuberous sclerosis. Obstet Gynecol Sci. (2019) 62:280–4. doi: 10.5468/ogs.2019.62.4.280
82. Adams, DM, Trenor, CC 3rd, Hammill, AM, Vinks, AA, Patel, MN, Chaudry, G, et al. Efficacy and safety of Sirolimus in the treatment of complicated vascular anomalies. Pediatrics. (2016) 137:e20153257. doi: 10.1542/peds.2015-3257
83. Hu, S, Wu, X, Xu, W, Tian, X, Yang, Y, Wang, S-T, et al. Long-term efficacy and safety of sirolimus therapy in patients with lymphangioleiomyomatosis. Orphanet J Rare Dis. (2019) 14:206. doi: 10.1186/s13023-019-1178-2
84. Zhang, Z, Li, Y, Zhang, G, Yang, K, Qiu, T, Zhou, J, et al. Safety evaluation of Oral Sirolimus in the treatment of childhood diseases: a systematic review. Children. (2022) 9:1295. doi: 10.3390/children9091295
85. Eworuke, E, Panucci, G, Goulding, M, Neuner, R, and Toh, S. Use of tumor necrosis factor-alpha inhibitors during pregnancy among women who delivered live born infants. Pharmacoepidemiol Drug Saf. (2019) 28:296–304. doi: 10.1002/pds.4695
86. Zhang, C, Deng, X, Zhang, X, Pan, Z, Zhao, W, Zhang, Y, et al. Association between serum TNF-α levels and recurrent spontaneous miscarriage: a Meta-analysis. Am J Reprod Immunol. (2016) 75:86–93. doi: 10.1111/aji.12447
87. Peppel, K, Crawford, D, and Beutler, B. A tumor necrosis factor (TNF) receptor-IgG heavy chain chimeric protein as a bivalent antagonist of TNF activity. J Exp Med. (1991) 174:1483–9. doi: 10.1084/jem.174.6.1483
88. Winger, EE, and Reed, JL. ORIGINAL ARTICLE: treatment with tumor necrosis factor inhibitors and intravenous immunoglobulin improves live birth rates in women with recurrent spontaneous abortion. Am J Reprod Immunol. (2008) 60:8–16. doi: 10.1111/j.1600-0897.2008.00585.x
89. Fu, J, Li, L, Qi, L, and Zhao, L. A randomized controlled trial of etanercept in the treatment of refractory recurrent spontaneous abortion with innate immune disorders. Taiwan J Obstet Gynecol. (2019) 58:621–5. doi: 10.1016/j.tjog.2019.07.007
90. Santiago, KY, Porchia, LM, and López-Bayghen, E. Endometrial preparation with etanercept increased embryo implantation and live birth rates in women suffering from recurrent implantation failure during IVF. Reprod Biol. (2021) 21:100480. doi: 10.1016/j.repbio.2021.100480
91. Winger, EE, Reed, JL, Ashoush, S, Ahuja, S, El-Toukhy, T, and Taranissi, M. Treatment with adalimumab (Humira®) and intravenous immunoglobulin improves pregnancy rates in women undergoing IVF. Am J Reprod Immunol. (2009) 61:113–20. doi: 10.1111/j.1600-0897.2008.00669.x
92. Romanowska-Próchnicka, K, Felis-Giemza, A, Olesińska, M, Wojdasiewicz, P, Paradowska-Gorycka, A, and Szukiewicz, D. The role of TNF-α and anti-TNF-α agents during preconception, pregnancy, and breastfeeding. Int J Mol Sci. (2021) 22. doi: 10.3390/ijms22062922
Keywords: reproductive immunology, Immunosuppressants, recurrent pregnancy loss, immunotherapy, repeated implantation failure
Citation: Andreescu M (2023) The impact of the use of immunosuppressive treatment after an embryo transfer in increasing the rate of live birth. Front. Med. 10:1167876. doi: 10.3389/fmed.2023.1167876
Edited by:
Yanlin Ma, Hainan Medical University, ChinaReviewed by:
Fatemeh Rezaei-Tazangi, Fasa University of Medical Sciences, IranNishel Mohan Shah, Imperial College London, United Kingdom
Copyright © 2023 Andreescu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mihaela Andreescu, dGV2ZXRtaWhhZWxhQGdtYWlsLmNvbQ==
 Mihaela Andreescu
Mihaela Andreescu