- 1Division of Liver Surgery, Department of General Surgery, West China Hospital, West China School of Nursing, Sichuan University, Chengdu, China
- 2West China School of Medicine, West China Hospital, Sichuan University, Chengdu, Sichuan, China
- 3Nursing Key Laboratory of Sichuan Province, West China Medical Center, Sichuan Medical University, Chengdu, China
Purpose: This study aimed to conduct a systematic review of the literature to identify and summarize the existing evidence regarding ERAS failure and related risk factors after hepatic surgery. The objective was to provide physicians with a better understanding of these factors so that they can take appropriate action to minimize ERAS failure and improve patient outcomes.
Method: A literature search of the PubMed MEDLINE, OVID, EMBASE, Cochrane Library, and Web of Science was performed. The search strategy involved terms related to ERAS, failure, and hepatectomy.
Result: A meta-analysis was conducted on four studies encompassing a total of 1,535 patients, resulting in the identification of 20 risk factors associated with ERAS failure after hepatic surgery. Four of these risk factors were selected for pooling, including major resection, ASA classification of ≥3, advanced age, and male gender. Major resection and ASA ≥ 3 were identified as statistically significant factors of ERAS failure.
Conclusion: The comprehensive literature review results indicated that the frequently identified risk factors for ERAS failure after hepatic surgery are linked to operative and anesthesia factors, including substantial resection and an American Society of Anesthesiologists score of 3 or higher. These insights will assist healthcare practitioners in taking prompt remedial measures. Nevertheless, there is a requirement for future high-quality randomized controlled trials with standardized evaluation frameworks for ERAS programs.
Introduction
The utilization of liver resection as a definitive surgical intervention for a variety of malignant and benign conditions has been traditionally associated with high postoperative mortality and morbidity rates (1). However, with the technical progress of surgical personnel and standardization of surgical procedures, the mortality rate has decreased to an acceptable level of less than 5% (2). Despite this improvement, the rate of morbidity and complication remain high(30–40%), which not only delays discharge, causes suffering for the patient, and increases the risk of mortality, but also is associated with decreased overall long-term survival following surgery for malignant diseases (3–5). As such, the minimization of morbidity is crucial for improving outcomes.
There has been a shift in traditional postoperative treatments, with a focus on earlier mobilization and faster recovery after surgery over the past two decades (6). This has led to the development and implementation of Enhanced Recovery After Surgery (ERAS) programs, which have been extensively studied and shown to be safe and effective (7–9). In 2011, the ERAS Society published guidelines, further promoting the widespread adoption of these programs across various surgical fields (10, 11). Despite the demonstrated benefits of ERAS programs in reducing postoperative morbidity and length of hospital stay in patients undergoing hepatic surgery, several studies have reported that a subset of patients fail to fully adhere to or benefit from these protocols (12–14). To address this issue, it is crucial to identify and understand the risk factors associated with ERAS failure, and to develop strategies for early identification and intervention in those patients who are at risk of deviation from the established protocols. However, the literature on this topic is currently limited, as there is a lack of consensus on the definition of ERAS failure and the specific risk factors associated with it, particularly in the context of liver surgery.
The present study aimed to conduct a systematic review of the literature in order to identify and summarize existing evidence pertaining to the failure of ERAS protocols and associated risk factors among patients undergoing hepatic surgery. The utilization of this evidence would enable physicians to identify patients at risk of ERAS failure and subsequently implement timely interventions to address this issue.
Materials and methods
Search strategies
Original articles were searched for in databases including PubMed MEDLINE, OVID, EMBASE, Cochrane Library, and Web of Science until November 1, 2022. We used following terms for the literature search: (“enhanced recovery after surgery” OR ERAS OR “enhanced recovery program” OR ERP OR “enhanced recovery” OR fast-track) AND (failure OR fail) AND (hepatectomy OR “liver resection” OR “liver surgery”). The citation language was restricted to English.
Inclusion and exclusion criteria
Articles were included if they evaluated any risk factor of ERAS failure in whether open or laparoscopic hepatectomy. Articles were excluded if they were: (1) prospective or retrospective studies but there were no control groups; (2) reviews, comments, conference abstracts, letters, and case reports; (3) animal experiments; and (4) only citations available, full texts not retrievable.
Data extraction
Two reviewers independently reviewed all included articles, and extracted necessary data: author, publication year, country, research type, study population, definition of ERAS failure, and risk factors. Two reviewers independently evaluated the quality of evidence of included studies using the Newcastle-Ottawa Scale. If any disagreement was present, another reviewer was assigned to re-evaluate the study.
Statistical analysis
Categorical data were synthesized as odds ratio (OR) with its 95% confidence interval (CI); continuous data measured with the same scale were synthesized using the weighted mean difference (WMD). If continuous data were demonstrated as medians and interquartile ranges (IQRs), the means and standard deviations (SDs) were estimated using an estimation method (15, 16). I-square (I2) was calculated to estimate heterogeneity. If I2 > 50%, the random effect model was used to integrate data, otherwise the fixed effect model was used. Begg’s test was used to evaluate publication bias. Signification level (α) was set to 0.05 for statistical tests.
Results
Study selection
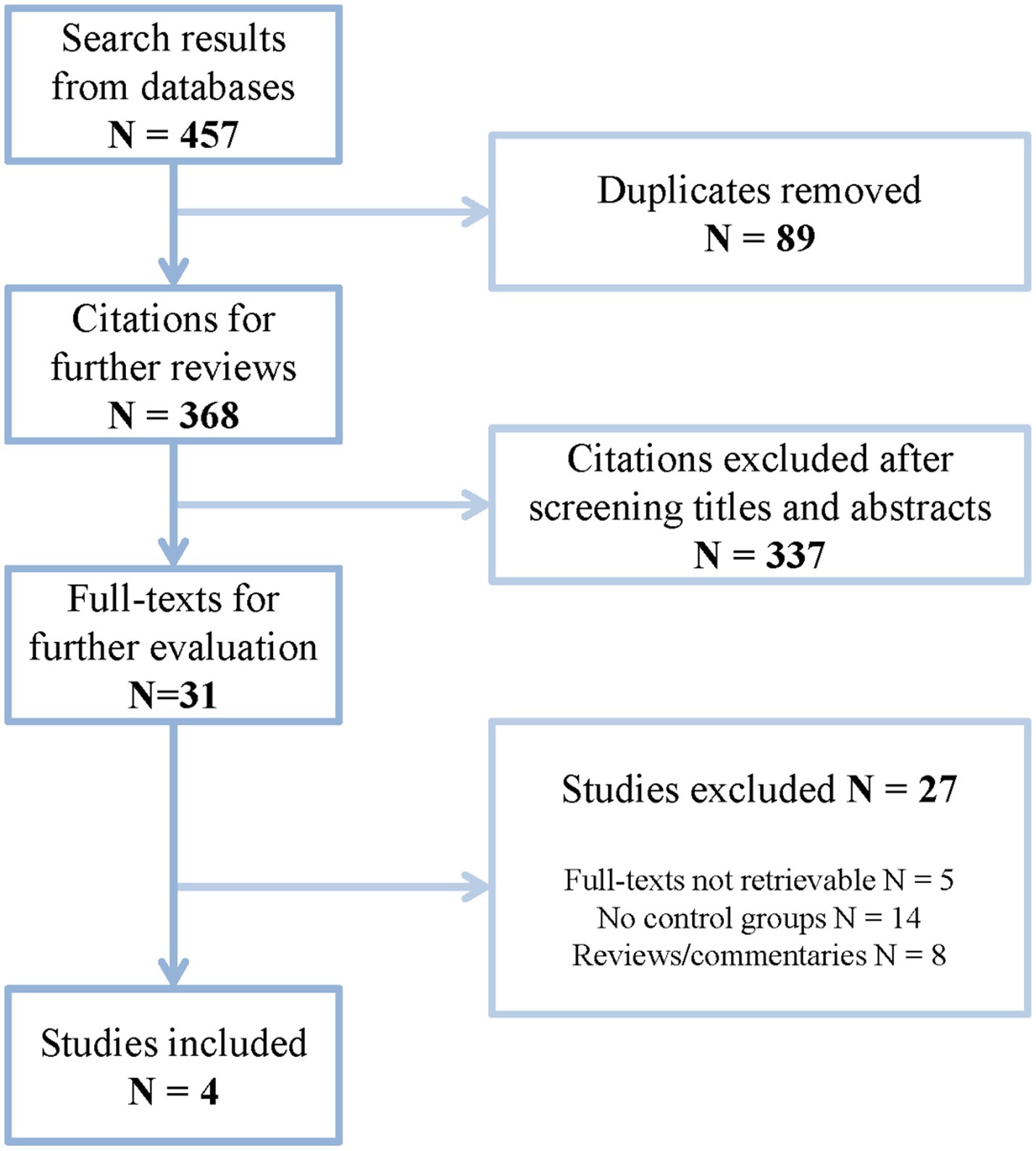
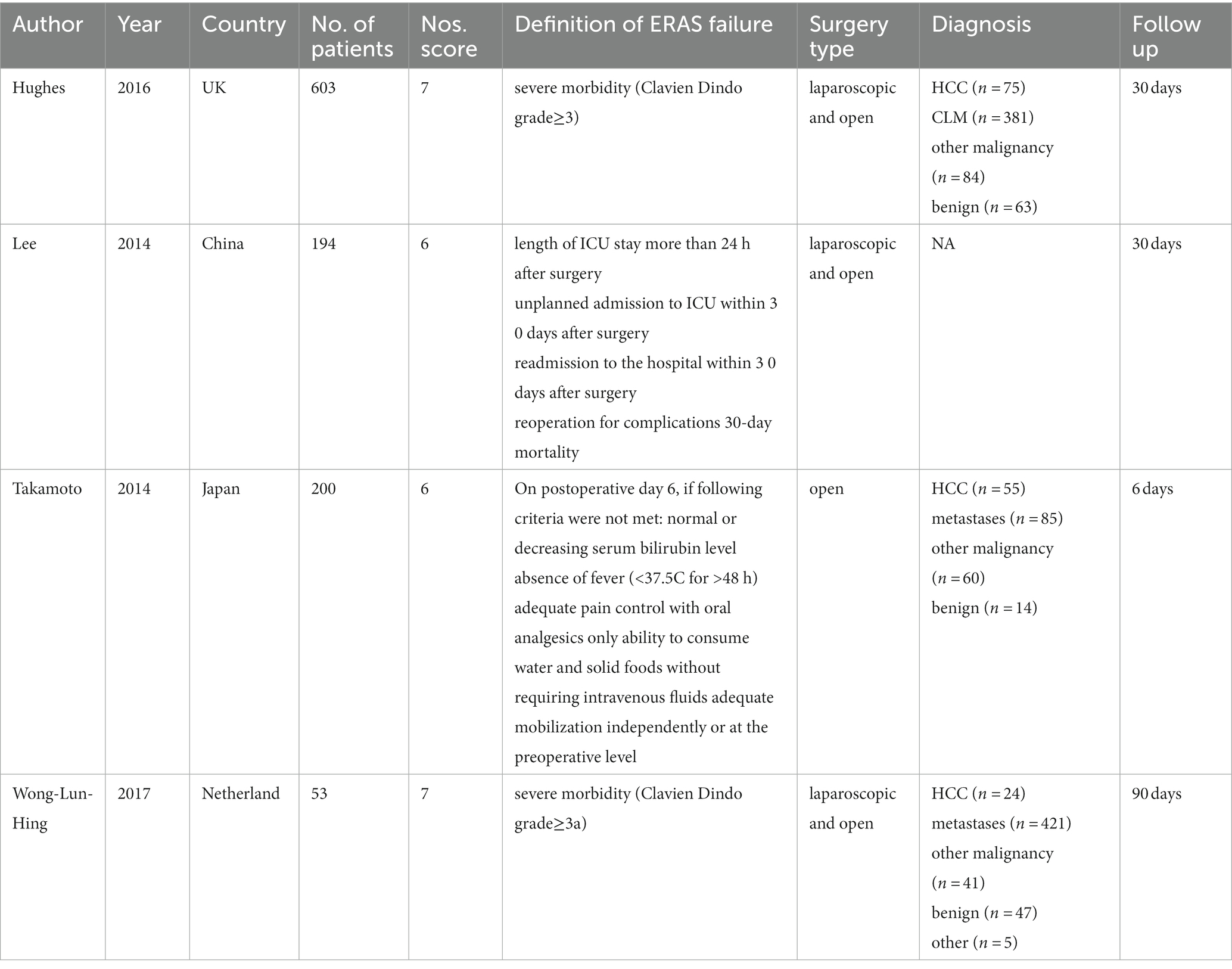
A flow chart shows the process of study inclusion in Figure 1. A total of 457 citations were found after initial literature search. After removing duplicates, there were 368 citations remaining for further review. After screening titles and abstracts, there were 31 articles remaining for further review. Finally, four studies were included in this systematic review and meta-analysis after reviewing full texts. The baseline information of these studies is shown in Table 1. All of them are retrospective studies and a total of 1,535 cases were involved in them.
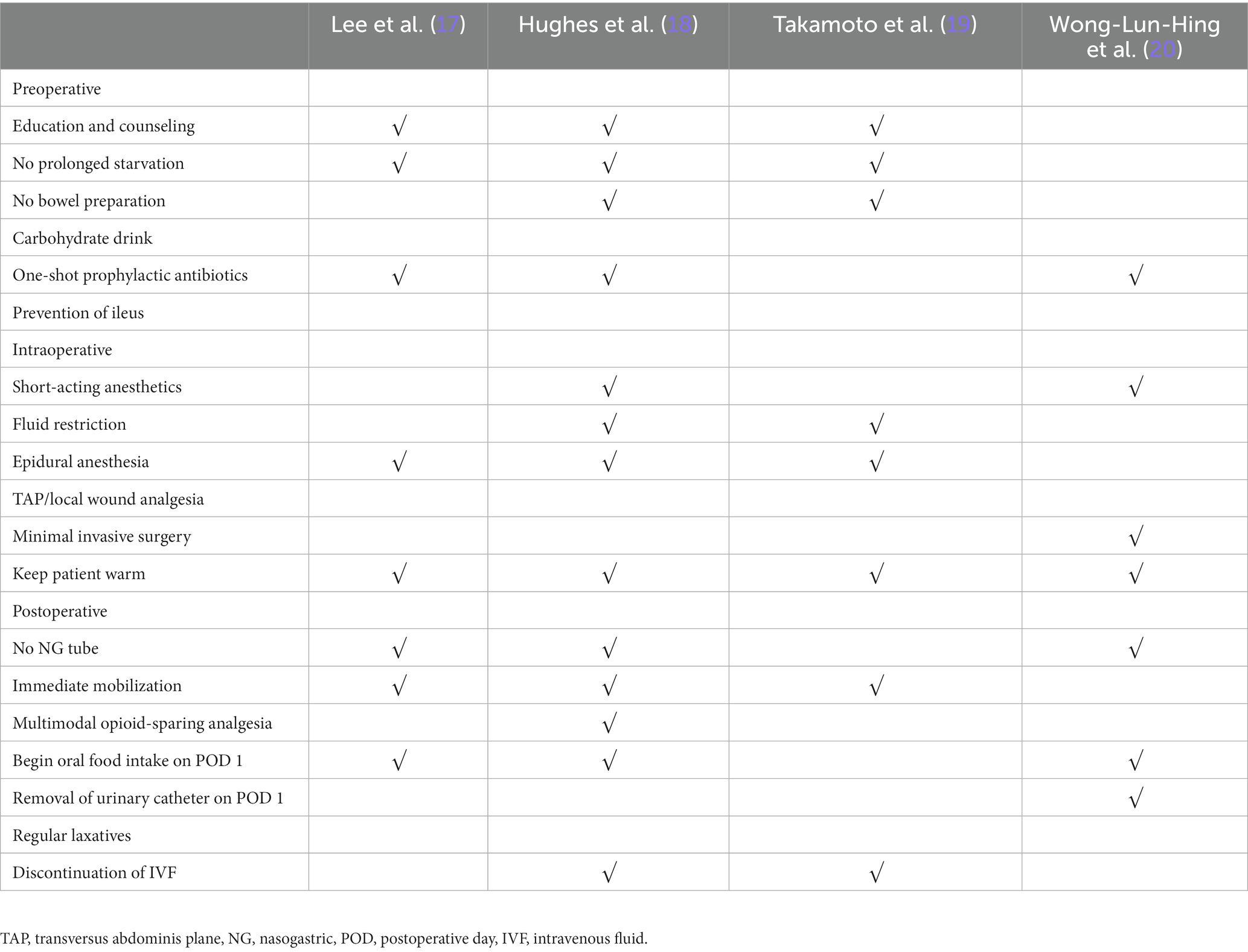
ERAS elements
The ERAS protocol is summarized in Table 2. The ERAS items applied at least four times included education and intake of liquid carbohydrates in the preoperative period, minimal invasive surgery in the intraoperative period, and no nasogastric tube use and oral food intake within 24 h after surgery in the postoperative period. Immediate mobilization and removal of the urinary catheter within 24 h after surgery were reported in all included studies.
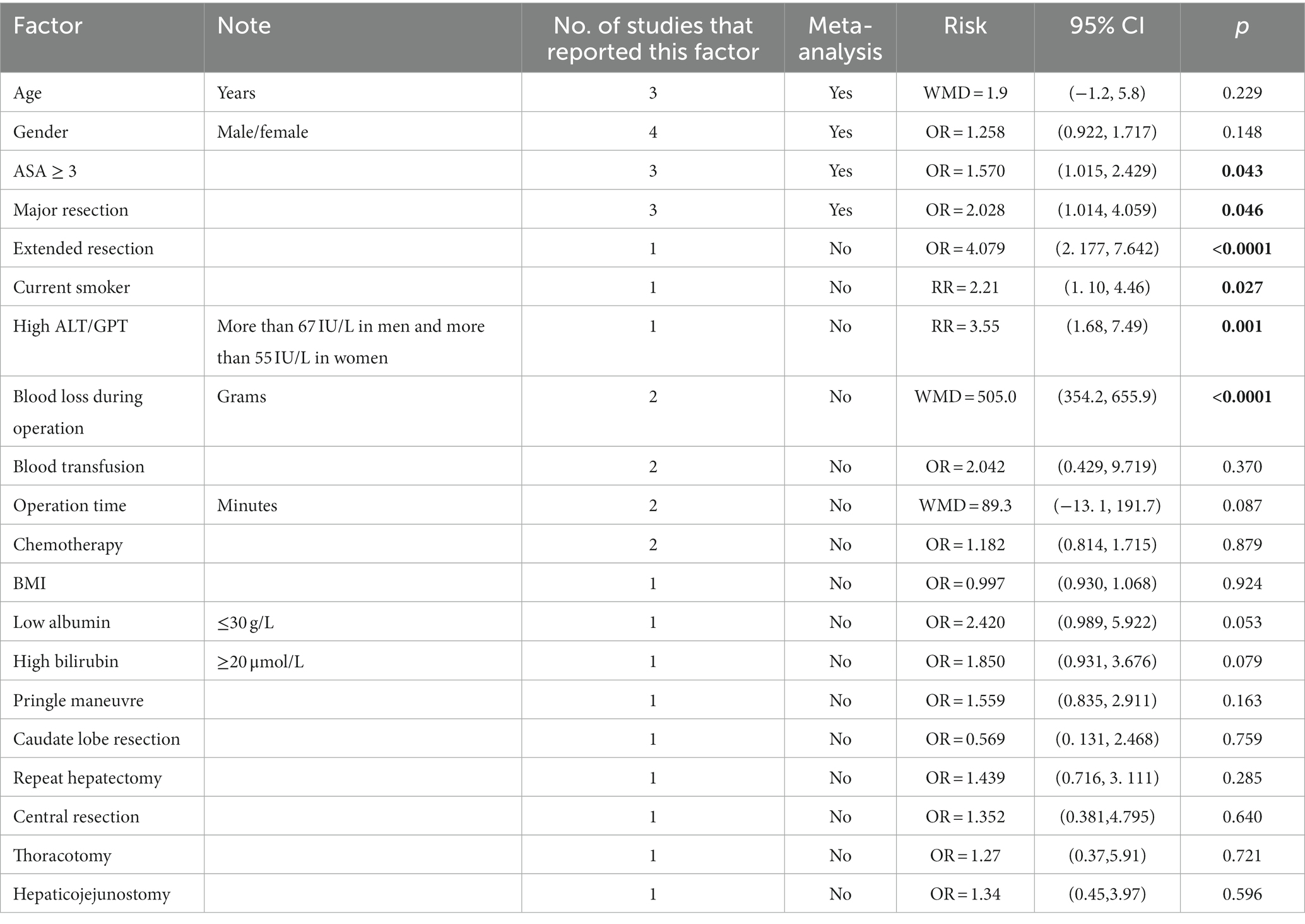
Risk factors
A total of 20 factors were involved in these four studies (Table 3). Among them, four risk factors could be pooled for the meta-analysis. Major resection and ASA ≥ 3 were identified as statistically significant factors of ERAS failure (p = 0.048 and p = 0.043 respectively; Figure 2). A funnel plot shows there is no obvious publication bias for both factors (Begg’s p = 0.602 and Begg’s p = 0.117; Figure 3). Older age and male gender were risk factors of ERAS failure but were not significant (Supplementary Figure 1).
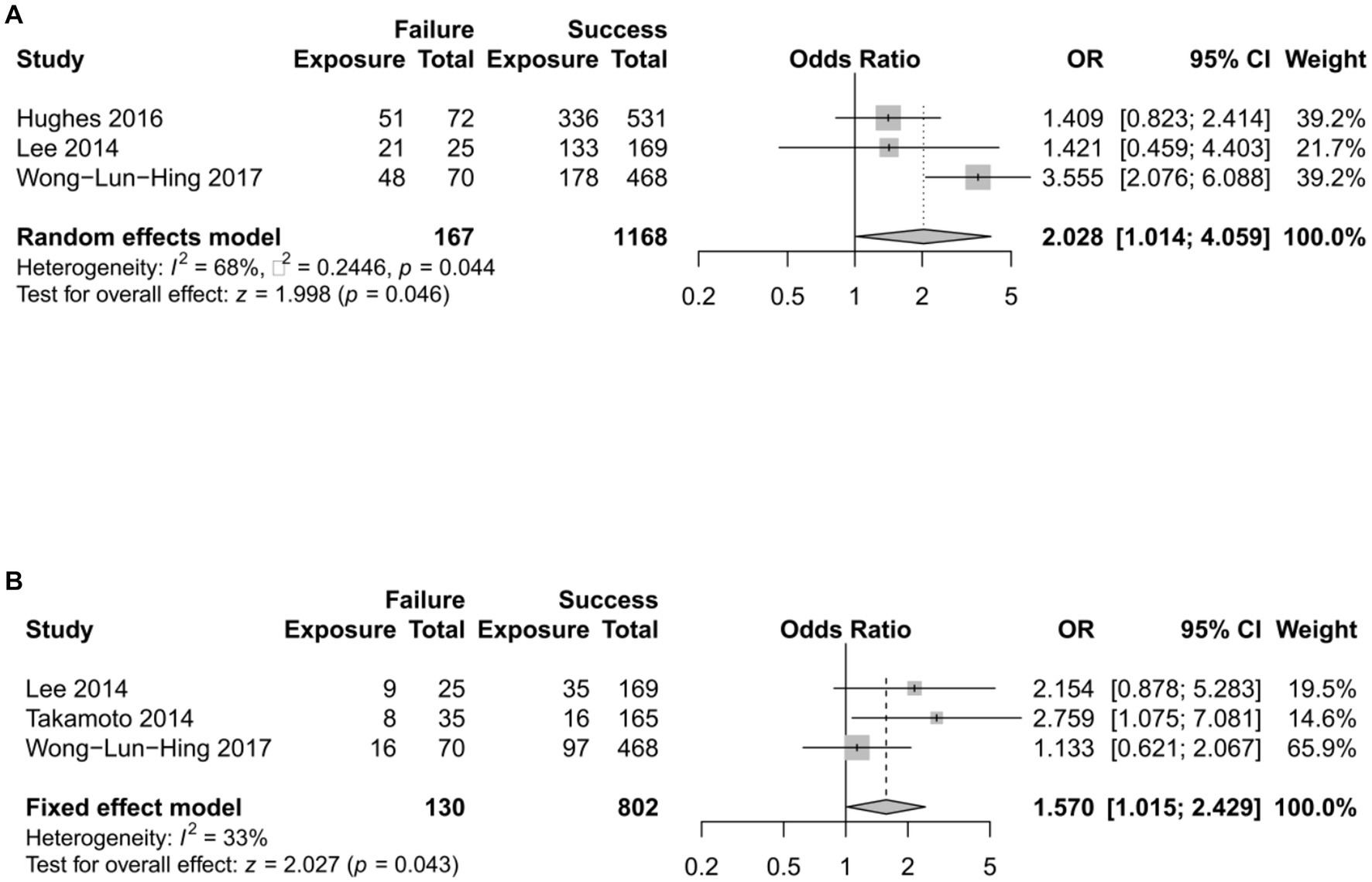
Figure 2. The effects of significant factors on ERAS failure. The horizontal lines with centered points and shaded squares stand for each study, while the diamond stand for pooled effects. (A) The effect of major resection. (B) The effect of ASA ≥3. OR, odds ratio; CI, confidence interval.
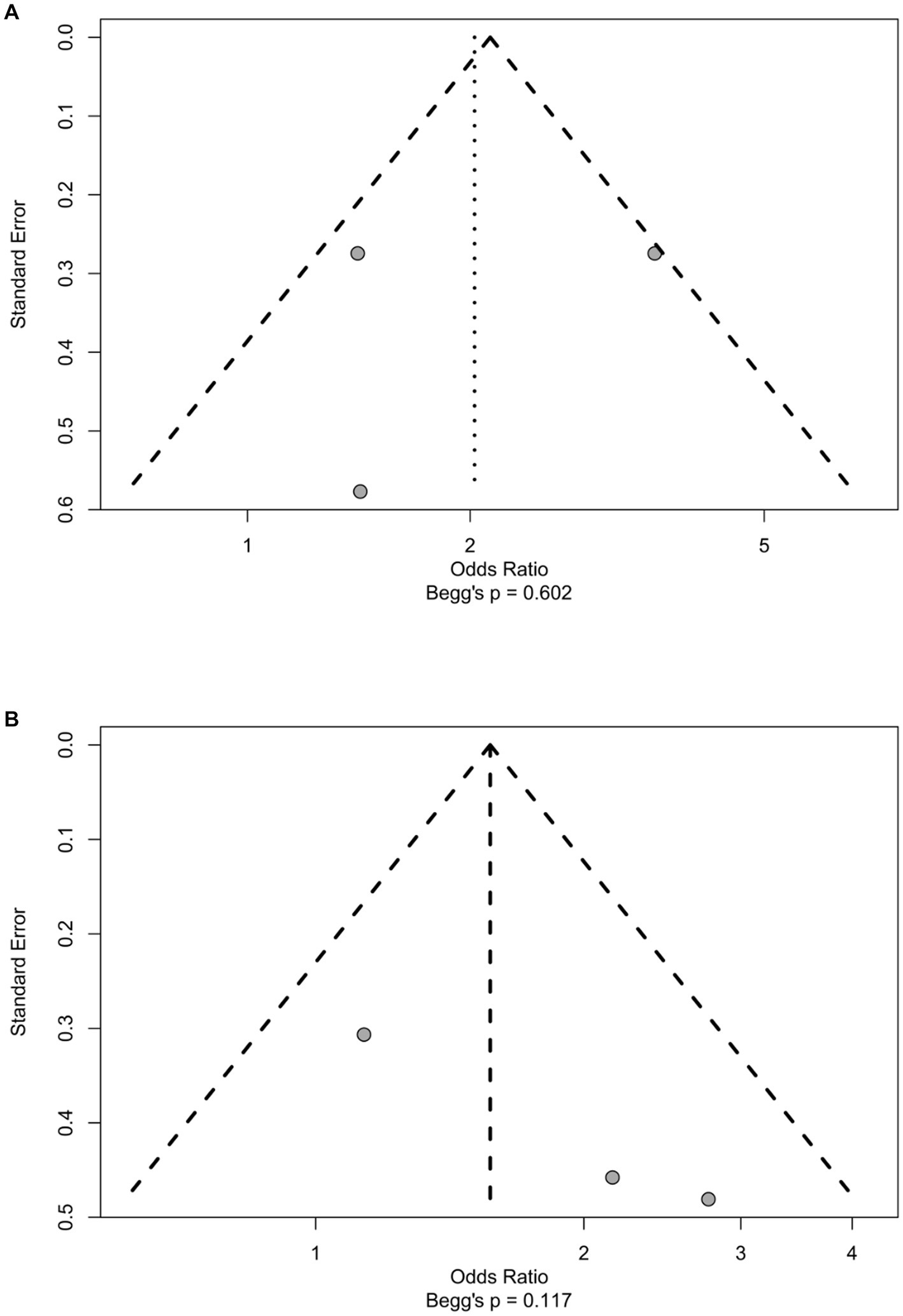
Figure 3. The funnel plot of significant factors. The distribution of the points and Begg’s p value suggest that there were no obvious sign of publicayion bias. (A) Major resection. (B) ASA ≥3.
More blood loss during operation was a statistically significant risk factor whether pooled or not (Supplementary Figure 1). However, only two studies reported this variable, therefore it was not eligible for the meta-analysis and was considered as a factor identified from individual studies. The effects of peration time, blood loss during surgery, blood transfusion and the use of chemotherapy were also pooled, but their effects were not significant either (Supplementary Figure 1).
Other factors identified from individual studies were mostly not significant. Nevertheless, there were two factors reported in individual studies. Lee et al. (17) reported that high ALT/GPT and smoking were independent risk factors of ERAS failure (RR = 3.55, p = 0.001 and RR = 2.21, p = 0.027, respectively), where high ALT/GPT was defined as more than 67 IU/L in men and more than 55 IU/L in women. Hughes et al. (18) reported that extended resection was an independent risk factor of ERAS failure (OR = 4.079, p < 0.0001).
Discussion
The present investigation conducted a systematic review of the literature to identify four articles that pertained to the failure of ERAS protocols and associated risk factors in patients who underwent hepatic surgery. The results of this study may be useful in identifying patients who are at a higher risk of ERAS failure, thereby allowing for timely implementation of corrective measures. Due to the substantial heterogeneity in study design and variations in ERAS protocols among the included studies, the meta-analysis was only performed for four risk factors. As far as we are aware, this is the initial systematic review and meta-analysis that specifically examines the risk factors for ERAS failure in the context of hepatic surgery.
The utilization of ERAS protocols has gained significant traction in the field of surgical operations, with numerous studies demonstrating the effectiveness of these protocols in reducing hospital admission times, morbidity rates and overall improving patient outcomes. This has led to the widespread acceptance of ERAS as a standard of care in surgeries (12, 13, 17, 18). Similarly, there has been a growing interest in the application of ERAS protocols in the field of liver resectional surgery. Recent studies, including several randomized controlled trials, have demonstrated the safety and feasibility of ERAS in liver surgery, as well as a reduction in morbidity rates following liver resections (19, 20). Systematic reviews of observational studies have demonstrated the safety and feasibility of ERAS programs in hepatobiliary surgery (18, 21, 22). Such programs, when compared to traditional clinical pathways, have been found to have similar risks of readmission, morbidity, and mortality, and have been associated with reduced duration of postoperative length of stay and overall hospital costs. However, the degree of compliance with core components of enhanced recovery after liver surgery programs among high-volume European centers has been found to vary (23).
In past few years, a number of high-volume medical centers have reported achieving approximately a zero-mortality rate after liver resection, suggesting that the surgical procedure and perioperative care for patients undergoing this procedure have a high rate of successful completion (23). However, it is important to note that the maintenance of a low rate of mortality for liver resection protocols cannot be guaranteed, even with significant improvements in perioperative care. Although the standard ERAS protocol guidelines recommend 26 perioperative care interventions, not all of those past interventions were implemented in the studies that were included in the review (24). The implementation of an ERAS for an invasive hepatectomy procedure should be carefully evaluated, taking into consideration not only reductions in length of hospital stay and medical expenses, but also potential risks to the patient. The literature has reported a wide range of morbidity rates following liver surgery, with estimates ranging from 22 to 45% (1, 22, 25). When comparing these rates to those of liver resection performed under ERAS protocols, the reported morbidity ranges from 11 to 46% (14). Overall, it appears that the use of ERAS principles in the management of liver resection may result in a reduction in morbidity compared to traditional practices. However, it should be noted that the literature does not indicate any significant impact of ERAS care on specific surgical morbidity.
Recent studies have demonstrated a trend towards increasingly favorable long-term outcomes following major resection for advanced disease (2–4, 25, 26). This trend serves as justification for an aggressive surgical approach in these cases. However, our study suggested that major resection was identified as statistically significant factors of ERAS failure. The current study observed significantly elevated rates of liver impairment following extended resections in comparison to major and minor hepatic resections (27). Despite the utilization of advanced techniques, such as Partial Volume Resection (PVE), tumor volume reduction, and two-stage procedures, to mitigate the risk of liver failure, this complication remains a concern in the context of major resections. Furthermore, the study observed significantly higher rates of bile leak and abscess formation after extended resections compared to non-extended resections (27, 28). Despite the implementation of these techniques, hepatic insufficiency remains a complication that requires ongoing attention.
In addition to surgical challenges, major resections also present difficulties in addressing non-surgical complications and management. The analgesic regimens after surgery are still complex, and the metabolism of different analgesic drugs is currently not well understood following major resection (29). The American Society of Anesthesiologists (ASA) guidelines from 2016 stipulate that ERAS is an integral component of the Perioperative Surgical Home (PSH) and recommends the implementation of a multimodal, opioid-sparing approach for the management of postoperative pain (30–32). In line with this recommendation, dexmedetomidine is increasingly being utilized as part of ERAS protocols in conjunction with regional nerve blocks and other medications, in order to achieve satisfactory postoperative outcomes while minimizing opioid consumption (33, 34). Furthermore, postoperative nutrition is of paramount importance in the context of liver resection due to the increased surgical insult and risk of sepsis. As such, further research is necessary to investigate the effects of small liver remnant volume on outcomes following liver resection and to determine how ERAS protocols should be adapted to account for the unique aspects of liver surgery that cannot directly draw lessons from other general abdominal surgery.
Our review had several limitations that should be acknowledged. Firstly, all of the studies included in the review employed a retrospective cohort design, which is prone to information bias and publication bias, as authors are more likely to submit studies with positive results for publication. Secondly, the heterogeneity of the ERAS protocols utilized in the included studies precluded a comprehensive assessment of all 26 elements recommended in the guidelines, and the level of compliance with these elements was not reported. To address this limitation, future studies with standardized ERAS protocols and detailed information on compliance with all recommended elements would be beneficial. Additionally, the scope of the review was limited to studies that reported on ERAS failure, which resulted in a small sample size and precluded an examination of other outcomes such as delayed discharge and high-quality randomized controlled trials (RCTs) that follow a standardized framework for evaluating ERAS programs should be conducted in the future might address this limitation.
Conclusion
The results of a comprehensive literature review indicated that the most commonly reported risk factors for ERAS failure after hepatic surgery include operative and anesthetic factors such as major resection and ASA ≥ 3. These findings will aid healthcare providers in taking corrective actions promptly. However, there is a need for high-quality randomized controlled trials with standardized evaluation frameworks for ERAS programs in the future.
Author contributions
QR and JL had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. QR, MW, HL, JL, and ZZ: concept and design and drafting of the manuscript. QR, HL, JL, and ZZ: acquisition, analysis, or interpretation of data. QR, MW, HL, and JL: critical revision of the manuscript for important intellectual content. QR, MW, and JL: supervision. All authors contributed to the article and approved the submitted version.
Funding
The name of granting agencies: West China Nursing Discipline Development Special fund, Sichuan University grant number: HXHL20043. A short description: analysis of the elements that lead to failure and development of a model for predicting the likelihood of quick rehabilitation surgery following partial hepatectomy.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1159960/full#supplementary-material
References
1. Virani, S, Michaelson, JS, Hutter, MM, Lancaster, RT, Warshaw, AL, Henderson, WG, et al. Morbidity and mortality after liver resection: results of the patient safety in surgery study. J Am Coll Surg. (2007) 204:1284–92. doi: 10.1016/j.jamcollsurg.2007.02.067
2. Cescon, M, Vetrone, G, Grazi, GL, Ramacciato, G, Ercolani, G, Ravaioli, M, et al. Trends in perioperative outcome after hepatic resection: analysis of 1500 consecutive unselected cases over 20 years. Ann Surg. (2009) 244:805–14. doi: 10.1097/SLA.0b013e3181a63c74
3. Belghiti, J, Hiramatsu, K, Benoist, S, Massault, PP, Sauvanet, A, and Farges, O. Seven hundred forty-seven hepatectomies in the 1990s: an update to evaluate the actual risk of liver resection. J Am Coll Surg. (2000) 191:38–46. doi: 10.1016/S1072-7515(00)00261-1
4. Imamura, H, Seyama, Y, Kokudo, N, Maema, A, Sugawara, Y, Sano, K, et al. One thousand fififty-six hepatectomies without mortality in 8 years. Arch Surg. (2003) 138:1198–206. doi: 10.1001/archsurg.138.11.1198
5. van den Broek, MAJ, van Dam, RM, Malagó, M, Dejong, CHC, van Breukelen, GJP, and Olde Damink, SWM. Feasibility of randomized controlled trials in liver surgery using surgery-related mortality or morbidity as endpoint. Br J Surg. (2009) 96:1005–14. doi: 10.1002/bjs.6663
6. Kehlet, H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. (1997) 78:606–17. doi: 10.1093/bja/78.5.606
7. Delaney, CP, Zutshi, M, Senagore, AJ, Remzi, FH, Hammel, J, and Fazio, VW. Prospective, randomized, controlled trial between a pathway of controlled rehabilitation with early ambulation and diet and traditional postoperative care after laparotomy and intestinal resection. Dis Colon Rectum. (2003) 46:851–9. doi: 10.1007/s10350-004-6672-4
8. Gatt, M, Anderson, AD, Reddy, BS, Hayward-Sampson, P, Tring, IC, and MacFie, J. Randomized clinical trial of multimodal optimization of surgical care in patients undergoing major colonic resection. Br J Surg. (2005) 92:1354–62. doi: 10.1002/bjs.5187
9. Kehlet, H, and Wilmore, DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg. (2008) 248:189–98. doi: 10.1097/SLA.0b013e31817f2c1a
10. Lv, L, Shao, YF, and Zhou, YB. The enhanced recovery after surgery (ERAS) pathway for patients undergoing colorectal surgery: an update of meta-analysis of randomized controlled trials. Int J Color Dis. (2012) 27:1549–54. doi: 10.1007/s00384-012-1577-5
11. Ljungqvist, O, Scott, M, and Fearon, KC. Enhanced recovery after surgery: a review. JAMA Surg. (2017) 152:292–8. doi: 10.1001/jamasurg.2016.4952
12. Vlug, MS, Wind, J, Hollmann, MW, Ubbink, DT, Cense, HA, Engel, AF, et al. Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study). Ann Surg. (2011) 254:868–75. doi: 10.1097/SLA.0b013e31821fd1ce
13. Jones, C, Kelliher, L, Dickinson, M, Riga, A, Worthington, T, Scott, MJ, et al. Randomized clinical trial on enhanced recovery versus standard care following open liver resection. Br J Surg. (2013) 100:1015–24. doi: 10.1002/bjs.9165
14. Hughes, MJ, McNally, S, and Wigmore, SJ. Enhanced recovery following liver surgery: a systematic review and meta-analysis. HPB. (2014) 16:699–706. doi: 10.1111/hpb.12245
15. Luo, D, Wan, X, Liu, J, and Tong, T. Optimally estimating the sample mean from the sample size, median, mid-range and/or mid-quartile range. Stat Methods Med Res. (2018) 27:1785–805. doi: 10.1177/0962280216669183
16. Wan, X, Wang, W, Liu, J, and Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. (2014) 14:135. doi: 10.1186/1471-2288-14-135
17. Lee, A, Chiu, CH, Cho, MW, Gomersall, CD, Lee, KF, Cheung, YS, et al. Factors associated with failure of enhanced recovery protocol in patients undergoing major hepatobiliary and pancreatic surgery: a retrospective cohort study. BMJ Open. (2014) 4:e005330. doi: 10.1136/bmjopen-2014-005330
18. Hughes, MJ, Chong, J, Harrison, E, and Wigmore, S. Short-term outcomes after liver resection for malignant and benign disease in the age of ERAS. HPB (Oxford). (2016) 18:177–82. doi: 10.1016/j.hpb.2015.10.011
19. Takamoto, T, Hashimoto, T, Inoue, K, Nagashima, D, Maruyama, Y, Mitsuka, Y, et al. Applicability of enhanced recovery program for advanced liver surgery. World J Surg. (2014) 38:2676–82. doi: 10.1007/s00268-014-2613-0
20. Wong-Lun-Hing, EM, van Woerden, V, Lodewick, TM, Bemelmans, MHA, Olde Damink, SWM, Dejong, CHC, et al. Abandoning prophylactic abdominal drainage after hepatic surgery: 10 years of no-drain policy in an enhanced recovery after surgery environment. Dig Surg. (2017) 34:411–20. doi: 10.1159/000455246
21. Coolsen, MM, van Dam, RM, van der Wilt, AA, Slim, K, Lassen, K, and Dejong, CHC. Systematic review and meta-analysis of enhanced recovery after pancreatic surgery with particular emphasis on pancreaticoduodenectomies. World J Surg. (2013) 37:1909–18. doi: 10.1007/s00268-013-2044-3
22. Coolsen, MM, Wong-Lun-Hing, EM, van Dam, RM, van der Wilt, AA, Slim, K, Lassen, K, et al. A systematic review of outcomes in patients undergoing liver surgery in an enhanced recovery after surgery pathways. HPB. (2013) 15:245–51. doi: 10.1111/j.1477-2574.2012.00572.x
23. Koea, JB, Young, Y, and Gunn, K. Fast track liver resection: the effect of a comprehensive care package and analgesia with single dose intrathecal morphine with gabapentin or continuous epidural analgesia. HPB Surg. (2009) 2009:1–8. doi: 10.1155/2009/271986
24. Hendry, PO, van Dam, RM, Bukkems, SF, McKeown, D, Parks, RW, Preston, T, et al. Randomized clinical trial of laxatives and oral nutritional supplements within an enhanced recovery after surgery protocol following liver resection. Br J Surg. (2010) 97:1198–206. doi: 10.1002/bjs.7120
25. Pearse, RM, Moreno, RP, Bauer, P, Pelosi, P, Metnitz, P, Spies, C, et al. Mortality after surgery in Europe: a 7 day cohort study. Lancet. (2012) 380:1059–65. doi: 10.1016/S0140-6736(12)61148-9
26. Poon, RT, Fan, ST, Lo, CM, Liu, CL, Lam, CM, Yuen, WK, et al. Improving perioperative outcome expands the role of hepatectomy in management of benign and malignant hepatobiliary diseases: analysis of 1222 consecutive patients from a prospective database. Ann Surg. (2004) 240:698–710. doi: 10.1097/01.sla.0000141195.66155.0c
27. Fan, ST, Lo, CM, Liu, CL, Lam, CM, Yuen, WK, Yeung, C, et al. Hepatectomy for hepatocellular carcinoma: toward zero hospital deaths. Ann Surg. (1999) 229:322–30. doi: 10.1097/00000658-199903000-00004
28. Gustafsson, UO, Scott, MJ, Hubner, M, Nygren, J, Demartines, N, Francis, N, et al. Guidelines for perioperative Care in Elective Colorectal Surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg. (2019) 43:659–95. doi: 10.1007/s00268-018-4844-y
29. Zimmitti, G, Roses, RE, Andreou, A, Shindoh, J, Curley, SA, Aloia, TA, et al. Greater complexity of liver surgery is not associated with an increased incidence of liver-related complications except for bile leak: an experience with 2,628 consecutive resections. J Gastrointest Surg. (2013) 17:57–65. doi: 10.1007/s11605-012-2000-9
30. Dimick, JB, Pronovost, PJ, and Lipsett, PA. The effect of ICU physician staffing and hospital volume on outcomes after hepatic resection. J Intensive Care Med. (2002) 17:41–7. doi: 10.1177/088506660201700104
31. Lam, VW, Laurence, JM, Johnston, E, Hollands, MJ, Pleass, HC, and Richardson, AJ. A systematic review of two-stage hepatectomy in patients with initially unresectable colorectal liver metastases. Cytokines Cell Mol Therapy. (2013) 15:483–91. doi: 10.1111/j.1477-2574.2012.00607.x
32. Sandström, R, Drott, C, Hyltander, A, Arfvidsson, B, Scherstén, T, Wickström, I, et al. The effect of postoperative intravenous feeding (TPN) on outcome following major surgery evaluated in a randomized study. Ann Surg. (1993) 217:185–95. doi: 10.1097/00000658-199302000-00013
33. Ergenc, M, Karpuz, S, Ergenc, M, and Yegen, C. Enhanced recovery after pancreatic surgery: a prospective randomized controlled clinical trial. J Surg Oncol. (2021) 124:1070–6. doi: 10.1002/jso.26614
Keywords: enhanced recovery after surgery, systematic review and meta-analysis, failure, liver surgery, meta analysis
Citation: Ren Q, Wu M, Li HY, Li J and Zeng ZH (2023) Failure of enhanced recovery after surgery in liver surgery: a systematic review and meta analysis. Front. Med. 10:1159960. doi: 10.3389/fmed.2023.1159960
Edited by:
Marc Micó-Carnero, August Pi i Sunyer Biomedical Research Institute (IDIBAPS), SpainReviewed by:
Lei Zhao, Capital Medical University, ChinaCarlos Rojano Alfonso, August Pi i Sunyer Biomedical Research Institute (IDIBAPS), Spain
Copyright © 2023 Ren, Wu, Li, Li and Zeng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Menghang Wu, MTU4MjgzMjY0MDdAMTYzLmNvbQ==
 Qiuping Ren
Qiuping Ren Menghang Wu1,2*
Menghang Wu1,2*