- 1Family and Community Medicine Department, College of Medicine, Hebron University, Hebron, Palestine
- 2Consultant Community Medicine, Faculty of Medicine and Health Sciences, An-Najah National University, Nablus, Palestine
- 3Consultant Family Medicine, Department of Family and Community Medicine, Faculty of Medicine and Health Sciences, An-Najah National University, Nablus, Palestine
- 4Faculty of Medicine and Health Sciences, An-Najah National University, Nablus, Palestine
- 5Consultant Family Medicine, Ministry of Health, Gaza, Palestine
- 6Ministry of Health, Alhussein Teaching Hospital, Karbala, Iraq
Background: The main objective of this study was to evaluate the antimicrobial therapy knowledge, attitudes, and practices of primary care physicians in the West Bank and Gaza.
Methods: Between January and April 2021, this cross-sectional survey was conducted. A link to the online survey was sent via confidential email lists to 336 primary care physicians who treated patients in Ministry of Health clinics. The survey questions scoring system was devised in order to evaluate the physicians’ practice, knowledge, and attitudes. Our scoring system identified favorable (good) and unfavorable (average and poor) antibiotic practices. In addition to independent t-test, the Chi-square test was used to compare the two groups of physicians’ knowledge, attitudes, and practices with their background characteristics. A multivariate analysis was performed to identify potential confounding variables having significant relationships.
Results: Of the 336 distributed questionnaires, 316 were completed, with a response rate of 94%. More than half (54.7%) were males, half (51.6%) were between 30 and 45 years of age, and most were general practitioners (74.1%). The overall good knowledge and attitude scores were 125 (39.6%) and 194 (61.4%), respectively. More than half (58.2%) had good antibiotic prescription practices. Females reported significantly more favorable practices than males, as did family medicine specialists compared with general practitioners. Finally, knowledge about antibiotic prescriptions had a substantial impact on changing their practices. However, physicians’ attitudes toward antibiotic prescriptions did not have a significant role in shaping their practices.
Conclusion: Overuse of antibiotics is a significant health issue in Palestine and worldwide. Most physicians know that improper antibiotic usage can cause antimicrobial resistance. More than two-thirds avoided needless antimicrobial prescriptions. In practicing antimicrobial stewardship, most prescribed fewer antibiotics and did not prescribe because of patient pressure. Family medicine specialists, female doctors, and those with high knowledge scores regardless of caseload were more likely to have good practices.
Introduction
Antibiotics are generally considered safe drugs, they are prescribed to relieve symptoms of bacterial infection, particularly in primary care, and they are used in the treatment of various diseases such as acute otitis media, group A beta-hemolytic streptococcal pharyngitis, epiglottitis, and bronchitis (1). Despite having low cost and being readily available, global concerns regarding antibiotic usage exist (2).
Overuse of antibiotics is a significant health issue worldwide; between 20 and 30% of antibiotic use is believed to be ineffective or useless (3). Antibiotic resistance is a globally growing issue (4), and this issue has increased the risk of morbidity and mortality. For example, in Europe, 25,000 deaths have been recorded (5) due to infection with antibiotic-resistant microorganisms.
Upper respiratory tract infections (URTI) which are defined as the nose, pharynx, larynx, and trachea subglottic infections, are known to be the most common cause of inappropriate antibiotic use and are a common reason for primary care consultations (6). Although most URTIs are viral in origin, antibiotic prescriptions for the treatment of URTI have increased in recent years, with World Health Organization (WHO) reporting prescription increases from 43 to 71% between 1982 and 2006 (7). This makes the use of antibiotics inappropriate and ineffective (8). Moreover, the improper use of antibiotics in viral illnesses increases the likelihood of inadequate response to regular therapy in antibiotic-resistant patients, causing contagion for longer periods of time, and placing strain on healthcare systems (9).
Despite global awareness, the prevalence of antibiotic resistance in some countries is still not fully recognized by some physicians (10, 11); furthermore, some physicians continue to prescribe antibiotics even though they know it is not necessary (12). It is believed that doctors’ decision to prescribe antibiotics could be affected by patients perception of good quality care; thus, some physicians tend to respond to patients’ pressure to avoid their dissatisfaction with the care they receive (10). In addition, in many countries, including Palestine, patients can receive antibiotics from pharmacists without a prescription.
Our literature review has shown that there is no official assessment of primary care physicians’ knowledge, attitudes, and practices regarding antimicrobial therapy in the occupied West Bank Territories and Gaza. This study aimed to address this gap across the Occupied West Bank Territories and Gaza.
Methods
Study design and population
This cross-sectional study was carried out at the Primary Healthcare centers (PHC) in the Occupied West Bank and the Gaza strip from January to April 2021. Ministry of Health’s Primary Healthcare centers are distributed throughout the country and serve as the patients’ first point of contact with the healthcare system. The study included all PHC physicians who worked at these centers. We excluded physicians who work in administrative positions and do not treat patients. An online survey link was sent through closed email lists to 336 primary care physicians.
The sample size was calculated using the formula: [n = Z2*P*(1-P)/d2], where Z is the confidence level statistic (Z = 1.96), P is the expected proportion of subjects with good practice, and d is the precision. A sample size of 245 was calculated to be the minimum required, assuming that 20% of primary care physicians have good practices (13), and a 95% confidence interval (CI), with 0.05 absolute precisions on either side of the predicted proportion. We inflated the number to 336 to account for an expected non-response rate of 40% among participants (14).
All procedures in this study were carried out in accordance with the Helsinki Declaration. The study was approved by the Institutional Review Board of An-Najah National University (Med. Nov. 2020/16).
The Palestinian Ministry of Health’s Primary Healthcare Department granted permission to conduct the study, and participants were approached and invited to participate voluntarily. We accompanied the questionnaire with a cover letter highlighting the objectives of the study and assuring respondents that their responses would be kept strictly confidential and anonymous. An online informed consent to participate was obtained from all participants by asking them to confirm their agreement with the information provided and their willingness to participate online by tapping the button “I agree.”
Measures
The questionnaire was based on extensive literature review (2, 15) and consisted of 40 items with 4 sections: (1) demographic and practice data (8 questions, with a question asking how many prescriptions for antibiotics were written in the last 7 days); (2) antibiotic prescriptions practices (10 questions with yes/no responses); (3) assessing the physicians’ knowledge (4 questions with yes/no responses and 4 scenarios with appropriate/unsure/not appropriate responses); and (4) attitude assessment (9 questions with 4-point Likert scale responses from strongly agree to strongly disagree).
We pre-tested the questionnaire to ensure its validity and reliability. For content validity, three experts in the field reviewed it, and then we translated it into Arabic. A pilot study on a sample of 19 physicians checked the tool’s simplicity and readability, and the time needed for completion. The necessary adjustments were made to finalize the questionnaire.
A scoring system was created to assess the physician’s practice, knowledge, and attitudes. The correct answers were summed to get the final score for each participant. The practice score ranged between 0 and 10. Physicians with good practice received scores ranging from 8 to 10, average practice ranged from 6 to 8, and poor practice scored less than 6. The total knowledge score ranged from 0 to 12. Greater than 10 was deemed to be good knowledge; 8 to 10 was average knowledge; and less than 8 was poor knowledge. Each of the four clinical case scenarios received a score of 0 for an incorrect response, 2 for correct, and 1 for unsure. The total score for attitudes ranged from 9 to 36. The total attitude score was divided into three levels based on Bloom’s cutoff point (16); a score of 29 or greater was considered good or appropriate attitudes, 22 to 29 average attitudes, and less than 22 poor attitudes. The primary study outcome, practice, was dichotomized as either favorable or unfavorable. The favorable practice group represents Physicians’ with good practice, whereas the unfavorable practice group represents Physicians’ with average or poor practice.
Data analysis
We used IBM SPSS Statistics for Windows, version 21 (IBM Corp., Armonk, NY, United States) for data analysis. A two-tailed p < 0.05 indicated statistical significance. The Kolmogorov–Smirnov test was utilized to ascertain the data’s normality; the results confirmed that the data followed a normal distribution. Frequencies, percentages, and mean ± standard deviation (SD) were used to describe physicians’ characteristics. We used Chi-square and the independent t-test to compare the physicians’ knowledge, attitudes, and practice with their between different groups background characteristics and the independent t-test, where applicable. Finally, we employed multivariate analysis using binary logistic regression was conducted to track possible confounders of significant associations.
Results
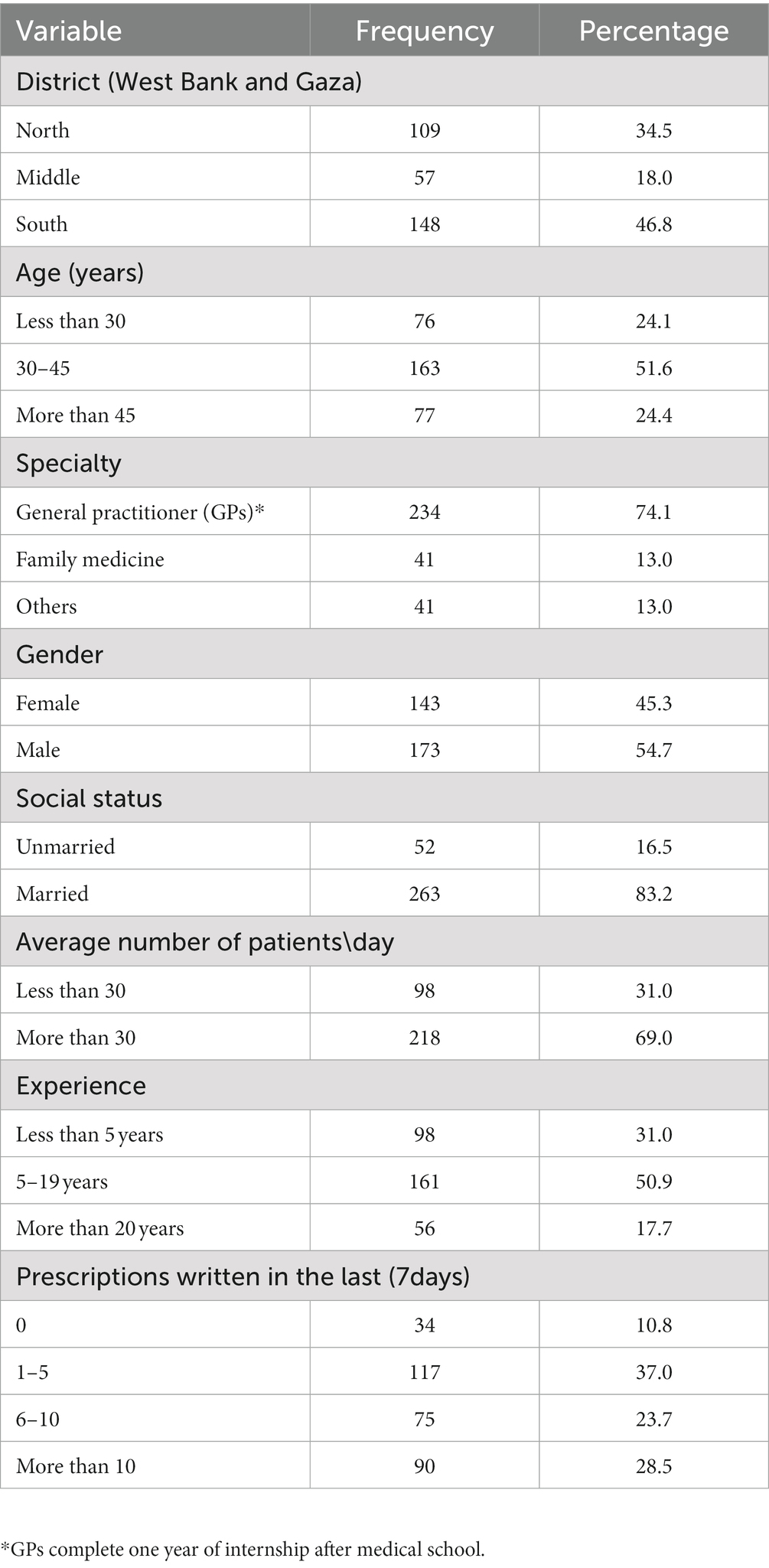
A total of 336 physicians received the questionnaire and 316 responded with a 94% response rate. Table 1 shows the physicians’ demographic characteristics. Males represented 54.7% of the respondents (173). Half (163, 51.6%) of all respondents were between 30 and 45 years of age. Most respondents were general practitioners (74.1%). The majority of the physicians (69.0%) treated more than 30 patients per day, with half (50.9%) having 5 to 19 years of practice experience (see Table 1).
Knowledge
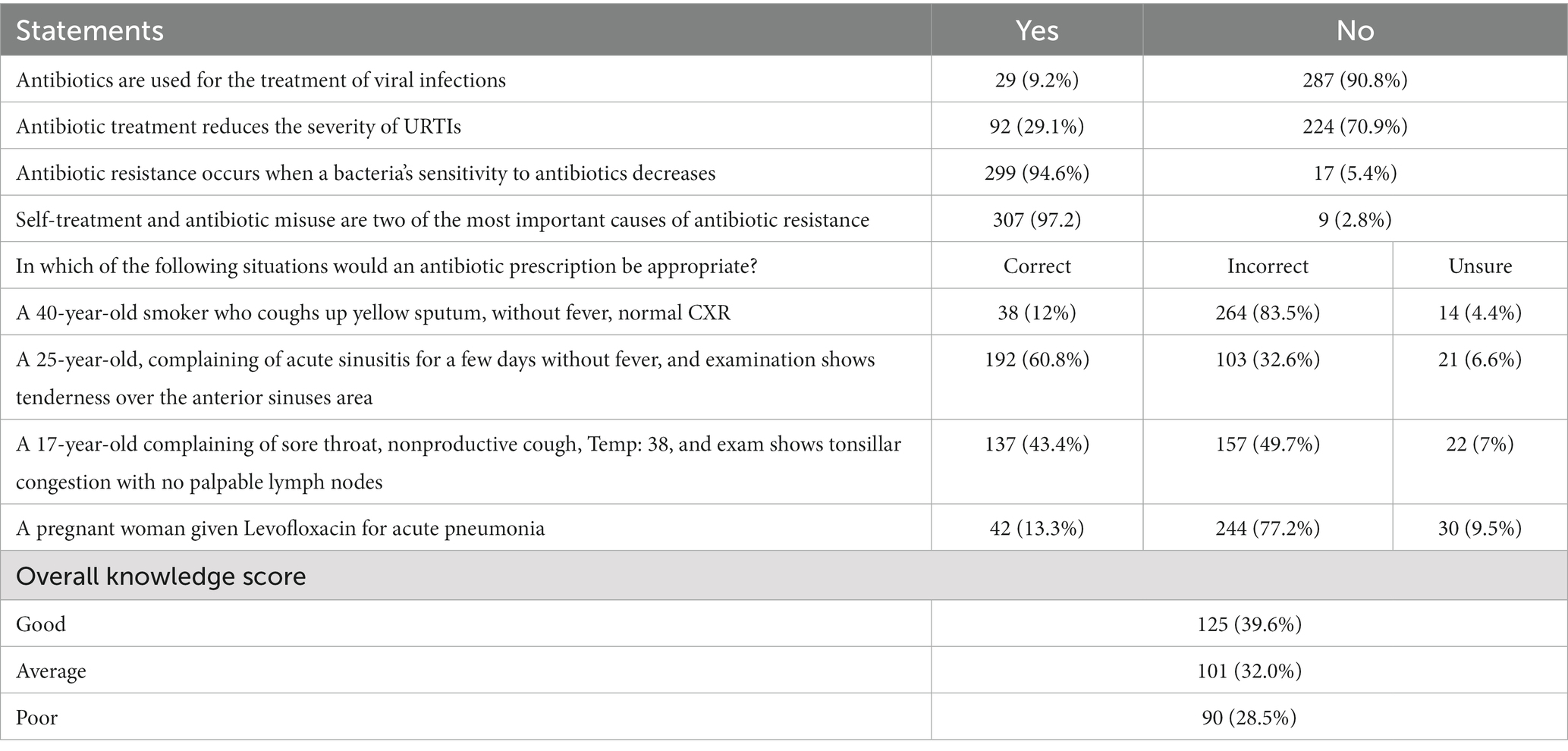
Table 2 shows physicians’ knowledge about antibiotic use. Most doctors knew antibiotics are not used for viral infections (287, 90.8%) and that antibiotics do not reduce symptoms (224, 70.9%). Most physicians knew why antibiotics resistance occurs (299, 94.6%), and self-treatment and antibiotic misuse are the most important factors (307, 97.2%). Clinical case scenarios were used to check the knowledge of the physicians. For example: Doctors were asked in which clinical cases they would prescribe antibiotics. The majority responded that it is incorrect to prescribe antibiotics to smokers with yellow sputum who had no fever (264, 83.5%), and only (4.4%) were unsure. The overall knowledge score on the four clinical case scenarios was: 125 (39.6%) good, 101 (32.0%) average, and 90 (28.5%) poor.
Attitudes
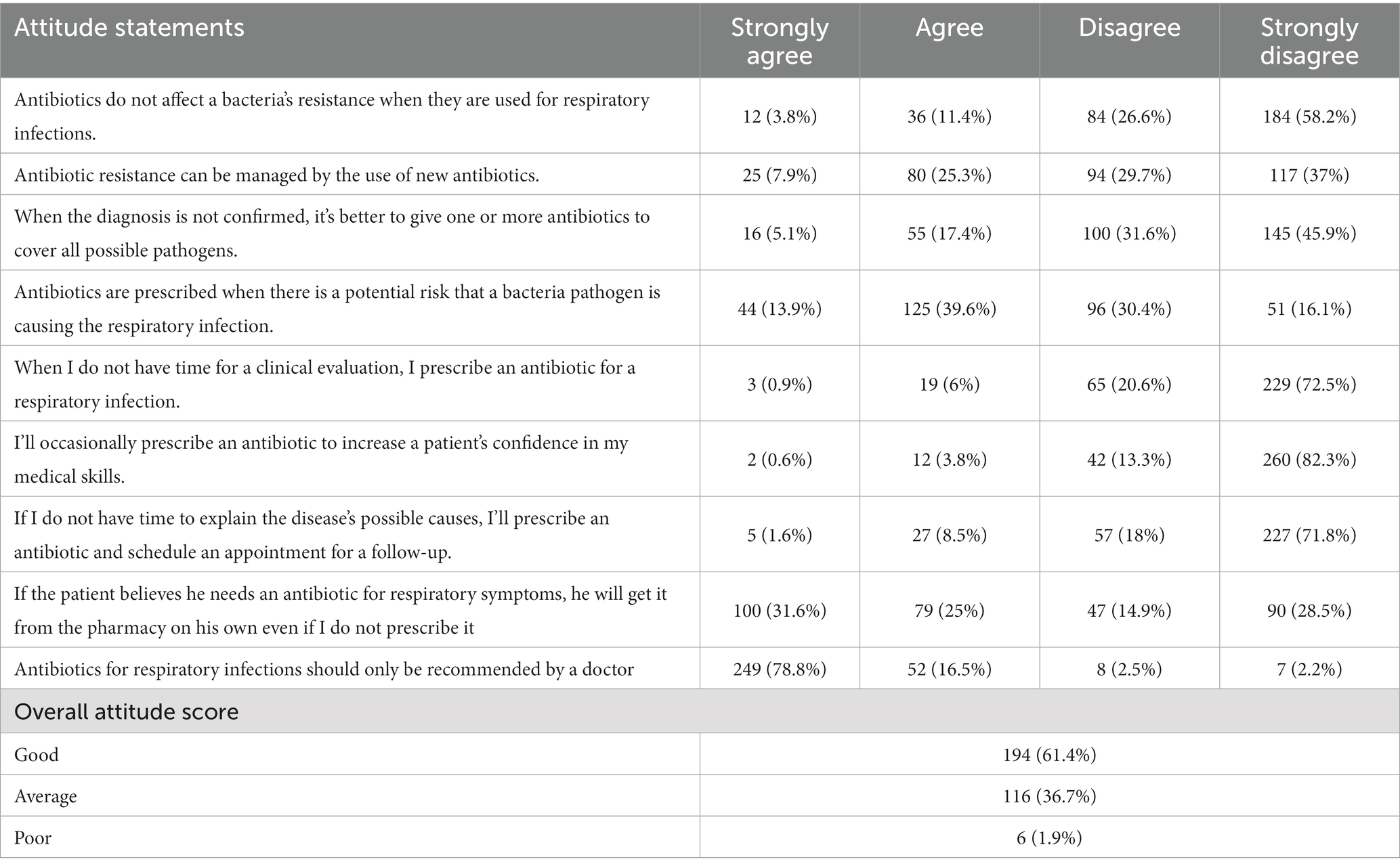
Table 3 shows the physicians’ attitudes about antibiotic use. Over half (58.2%) strongly disagreed that a bacteria’s resistance was unaffected when used to treat respiratory infection. Almost half of the physicians did not prescribe one or more antibiotics to cover all pathogens for a non-confirmed diagnosis (145, 45.9%), or if they did not have time for a clinical examination (229, 72.5%), or did not have time to explain the disease’s possible causes (227, 71.8%). Most would not prescribe antibiotics to improve their patients’ trust in their skills (260, 82.3%). Over half agreed or strongly agreed (56.6%) that patients who thought they needed antibiotics would get them from a pharmacy even if a doctor did not prescribe them. The total scores of attitudes toward antibiotics were good (194, 61.4%), average (116, 36.7%), and poor (6, 1.9%).
Practice
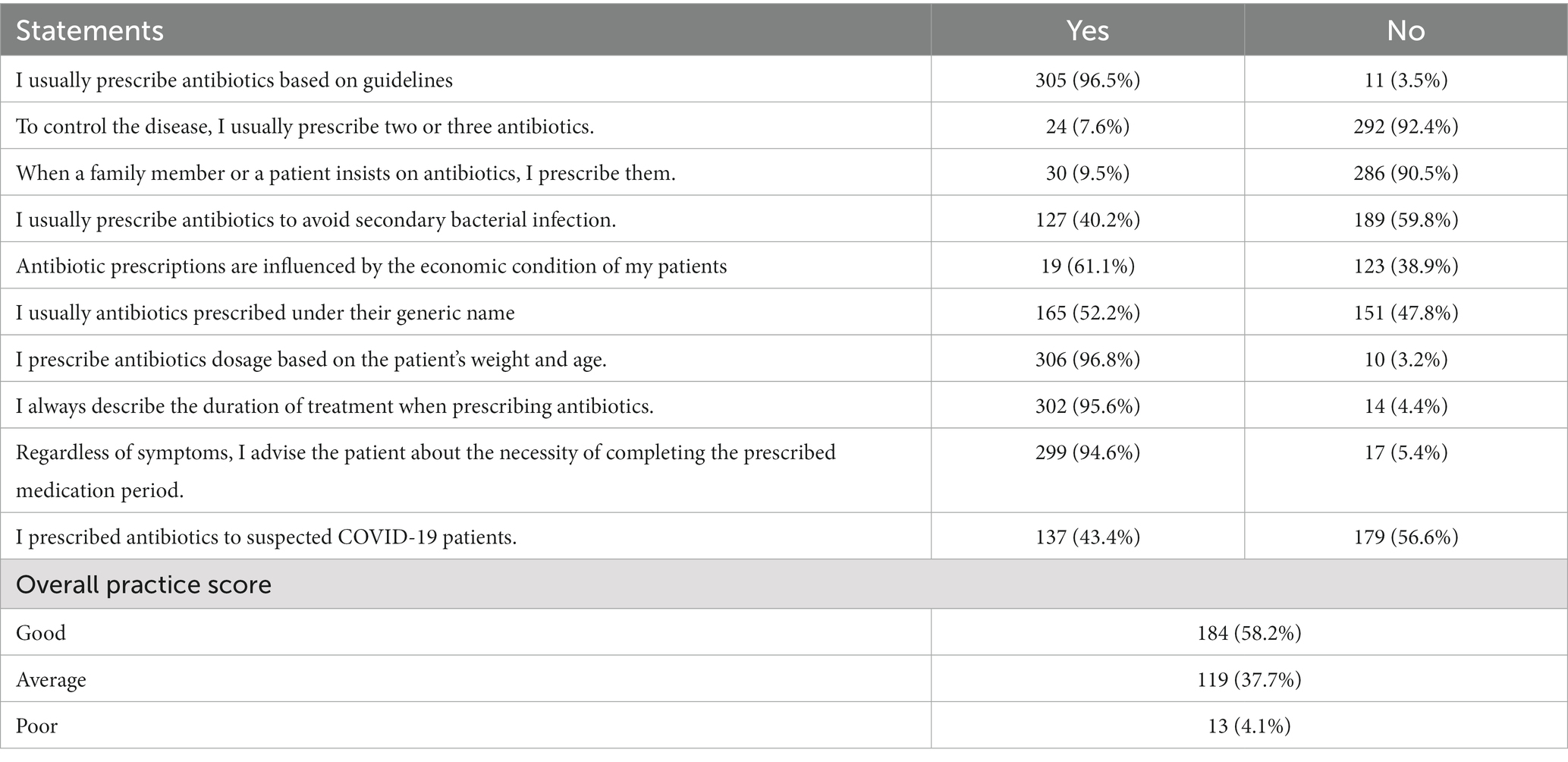
Table 4 shows physicians’ antibiotic prescription practice. Most of the physicians (305, 96.5%), indicated that guidelines influence their selection of prescribed antibiotics, and prescribe no more than one antibiotic at a time (292, 92.4%). The majority indicated that they do not feel pressured by patients or family members to prescribe antibiotics (286, 90.5%), do not prescribe antibiotics to prevent secondary infection (189, 59.8%), or to patients with suspected COVID-19 (179, 56.9%). Practice scores were: 184 (58.2%) good, 119 (37.7%) average, and 13 (4.1%) poor.
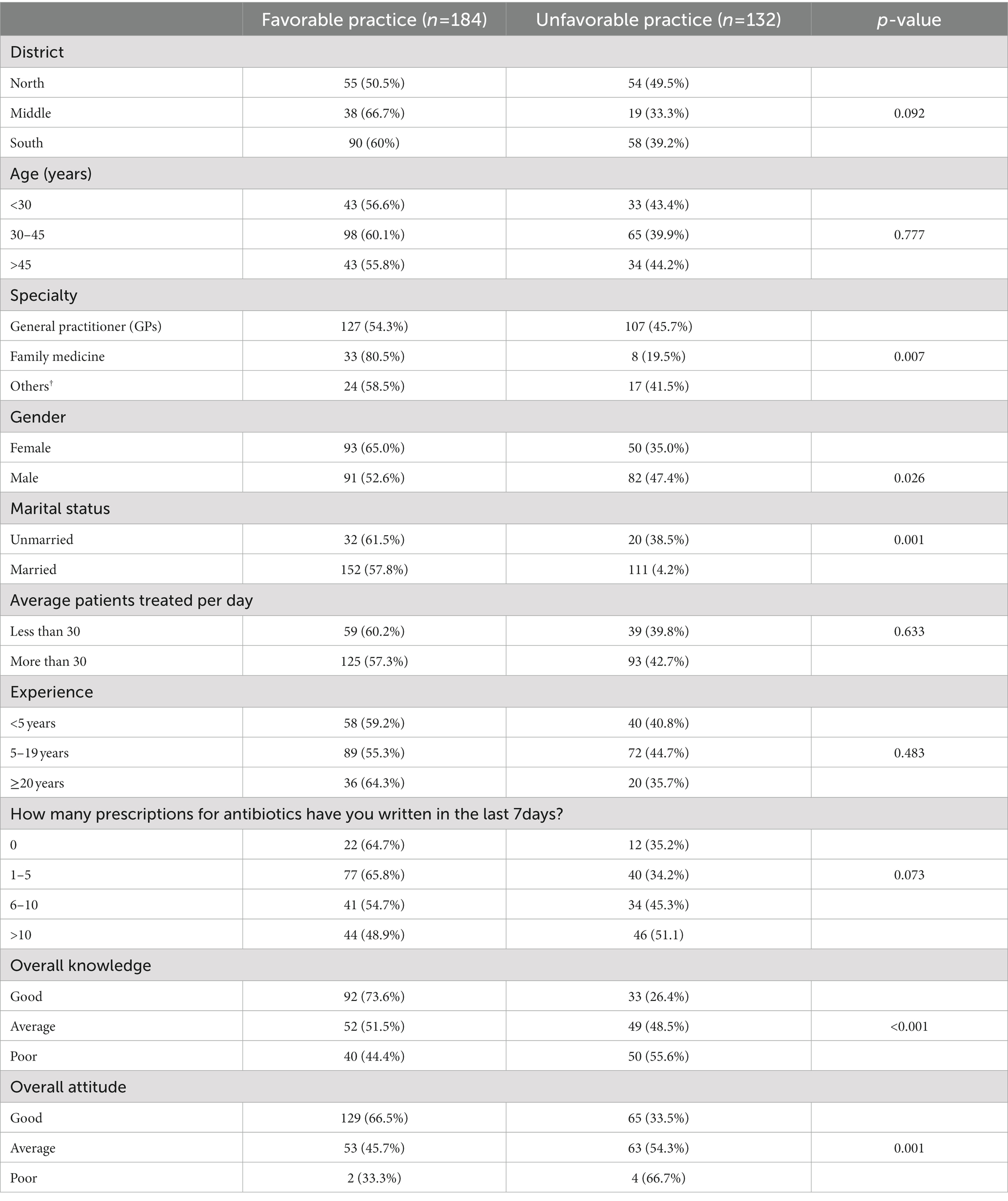
The statistically significant associations identified between favorable antibiotics prescription practices included: specialty, gender, and marital status. Family medicine specialists had a more favorable practice than GP (value of p = 0.007). Likewise, female physicians showed favorable practice than males (value of p = 0.026). Higher scores on attitudes and knowledge were associated with favorable practice and not related to the number of patients seen in a day or years of experience. See Table 5.
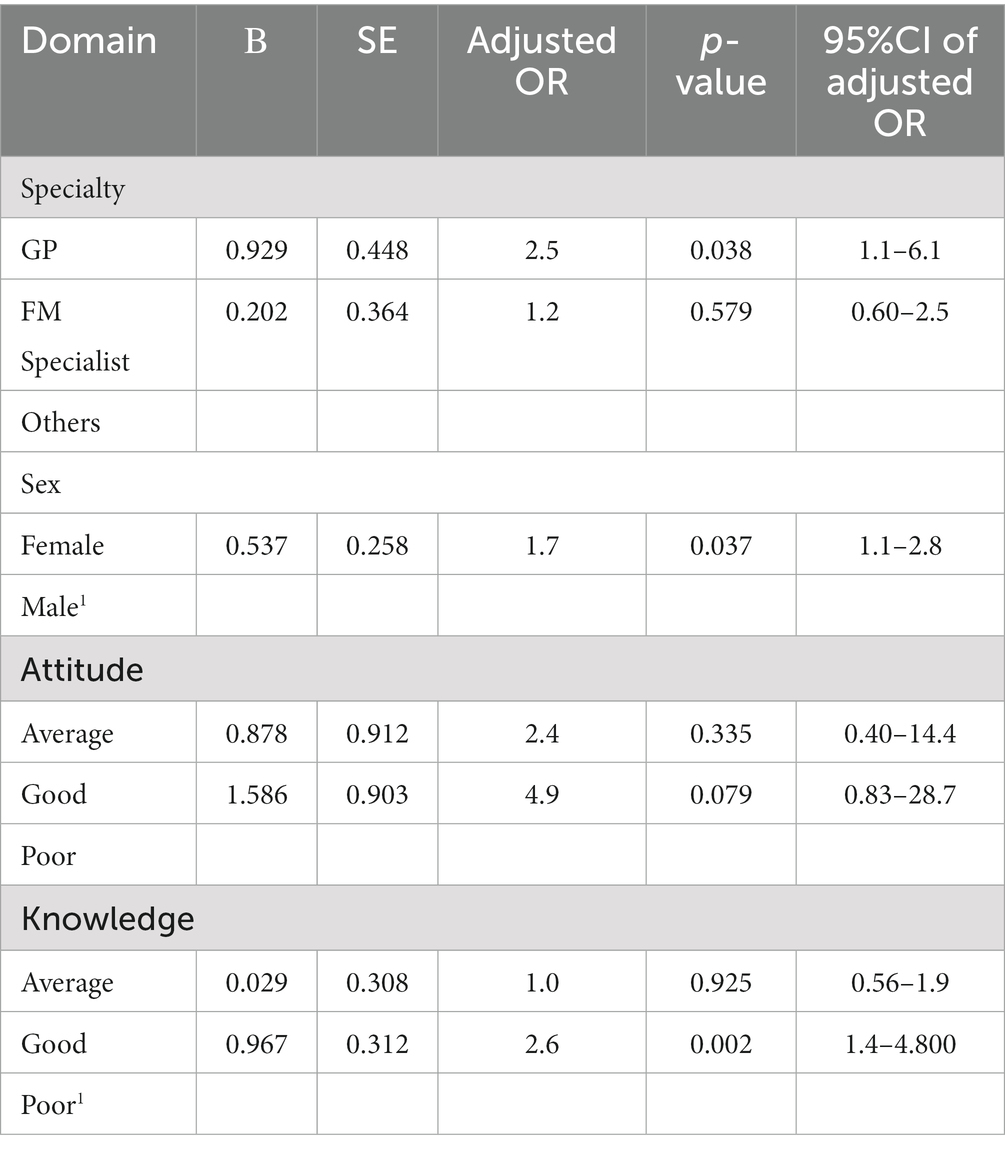
Multivariate logistic regression confirmed the earlier findings that Family Medicine specialists reported favorable practice than GPs (p value = 0.038), and females reported significantly favorable practice than males (value of p = 0.037). Finally, knowledge about antibiotic prescriptions showed a significant role in shaping favorable practice (value of p = 0.002) (Table 6). On the other hand, physicians’ attitudes about antibiotics prescriptions did not have a significant role in shaping their practice (value of p = 0.079).
Discussion
This is the first study assessing the knowledge, attitudes and practices regarding the use of antibiotics by primary care physicians in the Ministry of Health clinics in the West Bank and Gaza. This is an important because physicians in these areas practice without clear antibiotic prescribing guidelines or specific restrictions.
Almost 40% demonstrated good knowledge about antibiotics usage. It is worth mentioning that 60.8% agreed incorrectly with prescribing antibiotics for acute sinusitis after a few days without fever. Our findings suggest that Palestinian primary care physicians need educational initiatives to improve their knowledge about the appropriate use of antibiotics. Studies have shown that educational interventions improve practice, specifically 62% of studies reviewed in a systematic review showed improved guideline adherence, decreased total number of antibiotic prescriptions, improved physicians’ attitudes and behaviors, and improved pharmacy practice related to antibiotic prescriptions (17).
Attitudes and reported practice by Palestinian primary care physicians were only slightly better, 61.4 and 58.2%, respectively. Appropriate attitudes demonstrated no significant association favorable practice.
Public advocacy and education about over prescribing antibiotics and the detrimental effects will play a crucial role in increasing physicians’, all health professionals’, and patients’ knowledge of antibiotics usage (18). In order to address the educational needs of physicians, the creation of evidence-based antibiotic prescribing recommendations endorsed by relevant national/regional medical organizations should be a priority. These guidelines should be extensively publicized to physicians and pharmaceutical firms, and will promote prudent prescribing of antimicrobials and reduce antibiotic misuse (19).
However, in the Palestinian community, pharmacists play a role in influencing patients’ decisions about antibiotics. It is concerning that most physicians agreed that patients will get antibiotics for viral infections from a pharmacy on their own even if not prescribed. This is not only a Palestinian problem as other countries such as Saudi Arabia have similar findings (2).
Our finding that the majority of physicians refused to prescribe antibiotics to increase patients’ confidence in their medical practice is positive as another study in the governmental hospitals outpatient clinics in the northern occupied Palestinian territories (20) found that patient demand for antibiotics contributed to antibiotic misuse in order to assure patient satisfaction with their care.
Favorable antibiotic prescription practice was significantly different between family medicine specialists and GPs or practitioners from other specialties. This suggests the value of the family medicine specialty, particularly in middle-income countries such as Palestine, where this specialty is relatively new. More family medicine trained physicians can improve the quality of care and it is important to support and empower them in sharing their knowledge with GPs and other colleagues (18).
Furthermore, it is notable that there was a statistically significant difference in favorable practice between females and males. This could be attributable to the fact that females make up the majority of family medicine physicians in Occupied Palestine and Gaza. Other factors such as age, district, and years of practice did not have an impact on a physician’s practice in our study. This is consistent with the findings in studies done in Saudi Arabia, Scotland, and France (2, 15). In contrast, a study conducted in Indonesia showed that physicians with less than 7 years of practice experience were less likely to prescribe antibiotics (21). Hence, younger physicians had more contemporary training. Since physicians in Occupied Palestine and Gaza are not required to do continuing medical education, they are more likely to practice medicine that is not up to date (22–24). This underlines the importance of implementing guidelines that are continually improved and to require some kind of practice improvement activities.
Finally, previous researchers have linked a high number of patients treated daily to high antibiotic prescription rates. This has been linked to time pressures or decision fatigue (22). Surprisingly, our research found no link between these two variables. It may be that participants attempted to respond in a more socially acceptable manner, or because the small sample size did not reflect the correct rate (25).
The study limitations include: The self-report nature of the questionnaire allowed more socially acceptable responses instead of reporting actual practice. While we ensured confidentiality in an attempt to reduce the self-report bias, the option of completing the questionnaire online or on paper may have affected the degree of honesty, but was done to improve completion rate. The United Nations Relief and Works Agency (UNRWA) clinics were not included in our sample so our findings cannot be generalized to the GPs practicing in that setting. We chose Ministry of health (MOH) clinics on the West Bank and the Gaza Strip to understand what government sector sponsored activities are needed to improve antibiotic use.
Conclusion
Most of the physicians were knowledgeable about what constitutes improper use of antibiotics and how it can, among other factors, contribute to antimicrobial resistance. More promising figures were seen in physicians’ attitudes to prescribing with more than two-thirds avoiding unnecessary antimicrobial prescriptions and when antibiotics are not indicated. A similar pattern was also seen in practicing antimicrobial stewardship where the majority used a conservative approach to the number of antibiotics prescribed or did not prescribe because of patient pressure. Of note, good practice was more likely seen in family medicine specialists, female doctors, and those who scored high in knowledge questions regardless of caseload.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
All methods involving human participants in this study were conducted per ethical research standards. The study was conducted in conformity with the ethical norms of An-Najah National University (ANNU). The Ministry of Health approved authorization for the study to be conducted in PHC settings, and participants were approached and invited voluntarily to participate. Participants were assured of their confidentiality and anonymity. This study was performed in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. It was approved by the Institutional Review Board (IRB) of An-Najah National University.
Author contributions
BM: designing the work, conducting data analyses and interpretations, drafting the work, and final approval of the published version. ZN: analysis and interpretation of data, drafting of the work, and final approval of the published version. SH: designing the work, drafting the work, final approval of the published version, and agreement to be accountable for all aspects of the work, including ensuring that any questions about the work’s accuracy or integrity are appropriately investigated and resolved. YA: acquisition of data, drafting of the work, and final approval of the published version. NM: acquisition of data, drafting of the work, and final approval of the published version. MA: data collection and drafting of the work. FA: drafting of the work and final approval of the published version. All authors contributed to the final manuscript’s development and approval.
Acknowledgments
We are grateful to the Palestinian Ministry of Health for assisting us in distributing and collecting questionnaires.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1139871/full#supplementary-material
References
1. Zoorob, R, Sidani, MA, Fremont, RD, and Kihlberg, C. Antibiotic use in acute upper respiratory tract infections. Am Fam Physician. (2012) 86:817–22.
2. Al-Homaidan, HT, and Barrimah, IE. Physicians’ knowledge, expectations, and practice regarding antibiotic use in primary health care. Int J Health Sci (Qassim). (2018) 12:18–24.
3. CDC. Measuring Outpatient Antibiotic Prescribing. Available at: https://www.cdc.gov/antibiotic-use/data/outpatient-prescribing/index.html (Accessed February 21, 2023)
4. Hassali, MA, Kamil, TKT, Md Yusof, FA, Alrasheedy, AA, Yusoff, ZM, Saleem, F, et al. General practitioners’ knowledge, attitude and prescribing of antibiotics for upper respiratory tract infections in Selangor, Malaysia: findings and implications. Expert Rev Anti-Infect Ther. (2015) 13:511–20. doi: 10.1586/14787210.2015.1012497
5. Laxminarayan, R, Duse, A, Wattal, C, Zaidi, AKM, Wertheim, HFL, Sumpradit, N, et al. Antibiotic resistance-the need for global solutions. Lancet Infect Dis. (2013) 13:1057–98. doi: 10.1016/S1473-3099(13)70318-9
6. National Institute for Health and Clinical Excellence. Respiratory tract infections–antibiotic prescribing. NICE Clin Guide. (2008) 69:1–240.
7. Medicines Use in Primary Care in Developing and Transitional Countries: Fact Book Summarizing Results from Studies Reported Between 1990 and 2006. Geneva: World Health Organization (2009).
8. Arroll, B. Antibiotics for upper respiratory tract infections: an overview of Cochrane reviews. Respir Med. (2005) 99:255–61. doi: 10.1016/j.rmed.2004.11.004
9. Wu, J, and Lee, MCL. The relationships between test performance and students’ perceptions of learning motivation, test value, and test anxiety in the context of the English benchmark requirement for graduation in Taiwan’s universities. Lang Test Asia. (2017) 7:1–21. doi: 10.1186/s40468-017-0041-4
10. Thriemer, K, Katuala, Y, Batoko, B, Alworonga, J-P, Devlieger, H, Van Geet, C, et al. Antibiotic prescribing in DR Congo: a knowledge, attitude and practice survey among medical doctors and students. PLoS One. (2022) 8. Epub ahead of print. doi: 10.1371/JOURNAL.PONE.0055495
11. Baadani, AM, Baig, K, Alfahad, WA, Aldalbahi, S, and Omrani, AS. Physicians knowledge, perceptions, and attitudes toward antimicrobial prescribing in Riyadh, Saudi Arabia. Saudi Med J. (2015) 36:613–9. doi: 10.15537/smj.2015.5.11726
12. Khatib, R, McCaig, D, and Giacaman, R. Treatment of infection: a cross-sectional survey of antibiotic drug utilisation in the Ramallah district of Palestine. Int J Pharm Pract. (2010) 14:211–7. doi: 10.1211/ijpp.14.3.0008
13. Shively, NR, Buehrle, DJ, Clancy, CJ, and Decker, BK. Prevalence of inappropriate antibiotic prescribing in primary care clinics within a veterans affairs health care system. Antimicrob Agents Chemother. (2018) 62, 62:e00337. doi: 10.1128/AAC.00337-18
14. Ogoina, D, Iliyasu, G, Kwaghe, V, Otu, A, Akase, IE, Adekanmbi, O, et al. Predictors of antibiotic prescriptions: a knowledge, attitude and practice survey among physicians in tertiary hospitals in Nigeria. Antimicrob Resist Infect Control. (2021) 10:1–17. doi: 10.1186/s13756-021-00940-9
15. Pulcini, C, Williams, F, Molinari, N, Davey, P, and Nathwani, D. Junior doctors’ knowledge and perceptions of antibiotic resistance and prescribing: a survey in France and Scotland. Clin Microbiol Infect. (2011) 17:80–7. doi: 10.1111/j.1469-0691.2010.03179.x
16. Bloom, BS. Learning for mastery. Instruction and curriculum. Regional education laboratory for the Carolinas and Virginia, topical papers and reprints, number 1. Eval Comment. (1968) 1:12.
17. Teixeira Rodrigues, A, Roque, F, Falcão, A, Figueiras, A, and Herdeiro, MT. Understanding physician antibiotic prescribing behaviour: a systematic review of qualitative studies. Int J Antimicrob Agents. (2013) 41:203–12. doi: 10.1016/j.ijantimicag.2012.09.003
18. Hosoglu, S, Classen, AY, and Akturk, Z. Antibiotic prescription in primary care from the perspective of family physicians: a qualitative study. J Infect Dev Ctries. (2021) 15:1117–23. doi: 10.3855/jidc.13924
19. Senok, AC, Ismaeel, Y, and Al-qashar, FA. Pattern of upper respiratory tract infections and physicians antibiotic prescribing practices in Bahrain. Med Princ Pract. (2009):170–4. doi: 10.1159/000204345
20. Taha, AA, Sedda, D, and Salam, AA. Knowledge, attitudes and practice survey about antimicrobial resistance and Prescribing among physicians in governmental hospitals in north of Palestine. Palest Med Pharm J. (2019) 4:63–72.
21. Andrajati, R, Tilaqza, A, and Supardi, S. Factors related to rational antibiotic prescriptions in community health centers in Depok City, Indonesia. J Infect Public Health. (2017) 10:41–8. doi: 10.1016/j.jiph.2016.01.012
22. Linder, JA, Doctor, JN, Friedberg, MW, Reyes Nieva, H, Birks, C, Meeker, D, et al. Time of day and the decision to prescribe antibiotics. JAMA Intern Med. (2014) 174:2029–31. doi: 10.1001/jamainternmed.2014.5225
23. Silverman, M, Povitz, M, Sontrop, JM, Li, L, Richard, L, Cejic, S, et al. Antibiotic prescribing for nonbacterial acute upper respiratory infections in elderly persons. Ann Intern Med. (2017) 166:765–74. doi: 10.7326/M16-1131
24. Cadieux, G, Tamblyn, R, Dauphinee, D, and Libman, M. Predictors of inappropriate antibiotic prescribing among primary care physicians. C Can Med Assoc J. (2007) 177:877–83. doi: 10.1503/cmaj.070151
25. Wu, J, Taylor, D, Ovchinikova, L, Heaney, A, Morgan, T, Dartnell, J, et al. Relationship between antimicrobial-resistance programs and antibiotic dispensing for upper respiratory tract infection: an analysis of Australian data between 2004 and 2015. J Int Med Res. (2018) 46:1326–38. doi: 10.1177/0300060517740813
Keywords: primary care, antibiotics, family medicine, West Bank and Gaza, upper respiratory tract infections
Citation: Maraqa B, Nazzal Z, Hamshari S, Matani N, Assi Y, Aabed M and Alameri F (2023) Palestinian physicians’ self-reported practice regarding antibiotic use for upper respiratory tract infections in primary healthcare. Front. Med. 10:1139871. doi: 10.3389/fmed.2023.1139871
Edited by:
Enamul Kabir, University of Southern Queensland, AustraliaReviewed by:
Ana V. Pejcic, University of Kragujevac, SerbiaGermán Peñalva, Institute of Biomedicine of Seville (CSIC), Spain
Copyright © 2023 Maraqa, Nazzal, Hamshari, Matani, Assi, Aabed and Alameri. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Suha Hamshari, cy5oYW1zaGFyaUBuYWphaC5lZHU=
†ORCID: Bessan Maraqa, https://orcid.org/0000-0002-6997-0449
Zaher Nazzal, https://orcid.org/0000-0002-2655-6109
Suha Hamshari, https://orcid.org/0000-0003-0736-3368
 Bessan Maraqa
Bessan Maraqa Zaher Nazzal
Zaher Nazzal Suha Hamshari
Suha Hamshari Nardine Matani
Nardine Matani Yasmeen Assi
Yasmeen Assi Mousa Aabed
Mousa Aabed Furqan Alameri6
Furqan Alameri6