- 1Department of Anesthesiology, Huzhou Key Laboratory of Basic Research and Clinical Translation for Neuromodulation, Huzhou Central Hospital, The Affiliated Huzhou Hospital, Zhejiang University School of Medicine, Affiliated Central Hospital Huzhou University, Huzhou, China
- 2Huzhou Central Hospital, The Affiliated Huzhou Hospital, Zhejiang University School of Medicine, Affiliated Central Hospital Huzhou University, Huzhou, China
Background: As an optional regional anesthesia approach, pericapsular nerve group (PENG) block has been successfully utilized to manage pain for hip surgeries without affecting motor function. The present meta-analysis aimed to verify the efficacy of PENG block for postoperative analgesia in patients undergoing hip surgery.
Methods: A total of 497 academic articles were identified after a systematic search in the databases of PubMed, Embase, Web of Science, and Cochrane Library up to 25 August 2022. The primary outcome was postoperative 24-h morphine consumption. Secondary outcomes included the time of the first request for rescue analgesia, static and dynamic pain scores 6 and 24 h after surgery, and incidence of postoperative nausea and vomiting (PONV). We calculated mean differences (MDs) with 95% confidence intervals (CIs) for postoperative 24-h morphine consumption, time of the first request for rescue analgesia, static and dynamic pain scores 6 and 24 h after surgery, and odds ratios (ORs) with 95% CIs for incidence of PONV. The chi-square test was used for heterogeneity analysis, and heterogeneity was assessed by I2. Statistical analysis was performed using Review Manager 5.4.
Results: Numerous electronic databases were searched, and finally, nine studies were identified. There was no significant difference in morphine consumption during the postoperative 24 h [MD: −2.57, 95% CI: (−5.42, 0.27), P = 0.08] and the time of the first request for rescue analgesia [MD: 1.79, 95% CI: (−1.06, 4.64), P = 0.22] between the PENG block and control groups. PENG block did not reveal a significant difference in 6 h [MD: −0.17, 95% CI: (−0.92, 0.57), P = 0.65] [MD: −0.69, 95% CI: (−1.58, 0.21), P = 0.13] and 24 h [MD: −0.25, 95% CI: (−1.54, 1.05), P = 0.71], [MD: 0.05, 95% CI: (−0.84, 0.93), P = 0.91] static and dynamic pain scores compared with other nerve block methods. Moreover, the two groups have a similar risk of PONV (OR: 1.29, 95% CI = 0.53–3.10, P = 0.57).
Conclusion: This review shows that PENG block can act as an alternative multimodal analgesia for hip surgery, and compared with the other kinds of nerve block, there was no significant difference in the postoperative analgesic effect of PENG block.
Systematic review registration: Supplementary Datasheet 1, identifier: CRD 42022356496.
1. Introduction
Approximately 1.6 million people worldwide suffer a hip fracture each year, and this number is increasing by 25% every 10 years, as the population continues to grow (1). With the increasing aging of the world population, it is estimated that by 2050, the number of patients with hip fractures will reach 6.3 million (2). Early surgical treatment is recommended for hip fractures. Hip surgery can cause moderate to severe pain (3). In the process of rehabilitation, the restriction of exercise due to pain leads to adverse results. Multimodal analgesia in conjunction with nerve block techniques is often used to treat pain during the surgical period of hip fracture, as adequate pain management has been shown to reduce complications and promote postoperative activity. Pericapsular nerve group (PENG) block is a new blocking concept in which a local anesthetic is injected around the anterior hip capsule to block the nerves innervating the anterior hip capsule, mainly by blocking the hip branch of the femoral and para-occlusive nerves that travel between the anterior inferior iliac spine and the iliopubic ramus (4, 5). The anterior hip capsule is innervated by the femoral, accessory obturator, and obturator nerves (6). According to recent anatomical studies, the iliopubic ridge and the medial aspect of the inferior acetabulum are considered to be the relevant bony landmarks guiding the blocking of these three neuroarticular branches when performing the PENG block technique (5). These anatomical underpinnings led Girón-Arango et al. (4) to report, for the first time, PENG block, a new technique for selectively blocking the articular branches of the femoral, paracentral, and obturator nerves. This ultrasound-guided PENG block differs from other blocks, in that it targets the branch of the joint that innervates the anterior part of the hip and, if done properly, does not result in limb weakness (4). It is used in hip surgery as an alternative to other regional nerve blocks such as fascia iliaca compartment block or femoral nerve block (7). Several newly randomized controlled trials (RCTs) have been used to estimate the efficacy of PENG block in participants undergoing hip surgery. Pascarella et al. (8) reported that PENG block showed superior results in reducing opioid requirements and pain intensity after hip surgery. Comparatively, PENG block did not reduce opiate demand or the maximum postoperative pain score in participants who underwent hip surgery (9, 10).
In view of the inconsistent results of these RCTs, we carried out a systematic review and meta-analysis to identify the effects of PENG block, with a focus on the analgesic effects compared with other peripheral nerve blocks in participants after hip surgery.
2. Methods
This meta-analysis was planned and conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist (11). The authors registered the protocol in the International Prospective Register of Systematic Reviews (Registration Number: CRD42022356496). The current study did not require ethics approval or informed consent since no patient information was collected.
2.1. Search strategy
We searched the electronic databases of PubMed, Embase, Web of Science, and Cochrane Library from the establishment of the database to 25 August 2022. The process of searching was systematically executed by two researchers (L.Y. and X.S.), independently, without language, publication year, journal, or region restrictions. The following search terms were used: (“Pericapsul*”) AND (“nerve block” OR “Block, Nerve” OR “Blocks, Nerve” OR “Nerve Blocks” OR “Nerve Blockade” OR “Blockade, Nerve” OR “Blockades, Nerve” OR “Nerve Blockades” OR “Chemical Neurolysis” OR “Chemical Neurolyses” OR “Neurolyses, Chemical” OR “Neurolysis, Chemical” OR “Chemodenervation” OR “Chemodenervations”). Appropriate adjustments were made when searching the database and if the full-text article was available. The search strategies for each database are included in the Supplementary Table 1.
2.2. Selection criteria
Any studies that met the following criteria were included: (1) RCTs; (2) studies that included adult patients with hip surgery; (3) studies that compared the effect of PENG block with that of other peripheral nerve blocks; and (4) studies that reported postoperative pain-related outcomes. Conversely, the following types of articles were excluded: (1) non-randomized studies; (2) studies that compared the effect of PENG block with sham block; and (3) studies in which numerical data related to postoperative analgesia were not available. When there were any differences of opinion between the two authors selecting the included studies, a senior author (H.L.) was involved and made the final decision.
2.3. Data extraction
Two authors (L.Y. and X.S.) independently examined and screened the final enrolled RCTs and collected the following data: first author, publication year, country, sample size, type of surgery, type of anesthesia, treatment of PENG block group, treatment of control group, and primary outcome. Medians, interquartile ranges, and ranges were approximated as means and standard deviations using the quantile estimation method and the Box-Cox method of McGrath et al. (12) as well as the method for unknown non-normal distributions approach of Cai et al. (13). When the two independent examiners did not agree, a third reviewer (H.L.) made the final decision.
2.4. Primary and secondary outcomes
The primary outcome was postoperative 24-h intravenous morphine equivalent doses, which was defined as the sum of analgesic drug conversion to intravenous morphine consumption over 24 h postoperatively. The secondary outcome included the time of the first request for rescue analgesia, the static and dynamic pain scores at 6 and 24 h after surgery, and the incidence of PONV. Pain score is defined as a participant's reported feeling of discomfort using an 11-point visual analog scale (VAS) or a numerical rating scale (NRS) (0: none, 10: extreme pain). PONV is defined as a discomfort sensation in which the participant has the impulsion to vomit or is forced to expel the stomach contents from the mouth (14).
2.5. Quality assessment and certainty of evidence assessment
Two authors (L.Y. and X. S.) independently evaluated the risk of bias and quality of evidence. The risk of bias was assessed by using the Cochrane Risk of Bias tool for randomized trials, based on seven aspects: random sequence generation, allocation concealment, blinding of participants, blinding of outcome assessors, incomplete outcome data, selective reporting, and other potential bias; risk levels were categorized as low, unclear, or high (15). The GRADEpro guideline development tool was used to evaluate the evidence quality of each outcome (16, 17). Intensity levels of evidence were categorized as high-quality, medium-quality, low-quality, or very low-quality evidence. Any differences in the evaluation process were resolved by a third senior author (H.L.).
2.6. Statistical analysis
Meta-analysis was performed using Review Manager 5.4 (Cochrane Collaboration). The data used were the mean differences (MD) and odds ratio (OR), presented as 95% confidence intervals (CI). When the p-value was < 0.05 and the 95% CI did not include 1 for OR and 0 for the MD, the difference was considered statistically significant. The chi-square test was used for heterogeneity analysis, and heterogeneity was assessed by I2. When the I2-values were < 25%, 25–50%, and >50%, the heterogeneity levels corresponded to low, medium, and high. A decision was made to use a random effect model due to the anticipated heterogeneity in this study. The sensitivity analyses were performed, removing one study at a time and combining the other studies, to assess whether a single study significantly affected the pooled results.
Data presented in the original literature were used as the primary source for extraction; when data were not shown, we contacted the authors for more information. As a final resort, when mean and SD values were not reported for an outcome [the postoperative 24-h intravenous morphine equivalent doses (18, 19) and the static and dynamic pain scores at 6 and 24 h after surgery (19, 20)], these values were imputed using the calculation methods of two statistical experts McGrath et al. (12) and Cai et al. (13).
2.7. Assessment of publication bias
Due to the small number of studies in each comparison (the number available for analysis was 3–6), we could not reliably assess the risk of publication bias. Therefore, the publication bias test was not performed in this study.
3. Results
3.1. Study selection
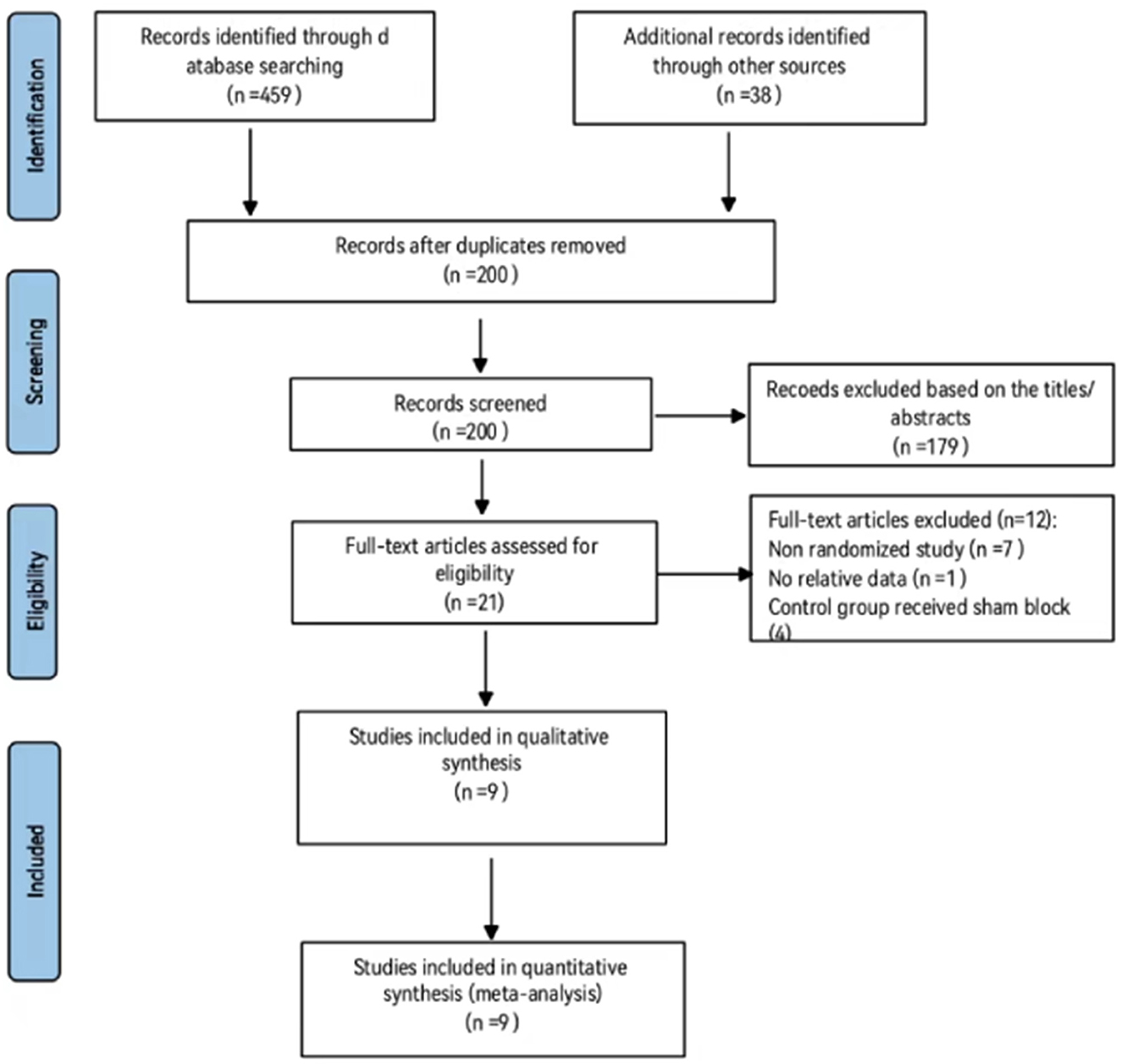
A total of 497 papers were found in the database search. Of these, 297 papers were duplicates; therefore, 200 papers were selected for this study. In addition, 146 (case report: 41; cohort study: 7; comment: 13; conference abstract: 10; protocol: 1; review: 26; withdrawal statement: 6; and letter: 42) and 33 (analgesia during postural changes: 7; anatomical research: 9; chronic pain treatment: 6; PENG block in other body parts: 9; hip arthroscope: 1; and combined with other block methods) papers were excluded using the titles and abstracts, respectively. The full text of the remaining 21 papers was reviewed and evaluated for eligibility. Out of which, 12 papers were excluded from the final analysis for the following reasons: non-randomized studies (n = 7), no relative data (n = 1), and when the effect of the PENG block was compared with the sham block (n = 4). Finally, nine RCTs were included in the meta-analysis (18–26) (Figure 1).
The characteristics of the included RCTs are shown in Table 1. Participants in one RCT underwent hip surgery under general anesthesia (21), seven RCTs enrolled those who were under spinal anesthesia (19, 20, 22–26), and one RCT enrolled patients who were under general anesthesia or spinal anesthesia (18). In the spinal anesthesia group, three RCTs (19, 20, 24) administered intrathecal opioids (fentanyl or morphine) combined with local anesthetics; however, the other two studies (23, 26) used only local anesthetics without adjuvants. The remaining studies did not describe the use of drugs for spinal anesthesia (18, 22, 25). The types of surgery were total hip arthroplasty (19–21, 23) and hip fracture surgery (18, 22, 24–26).
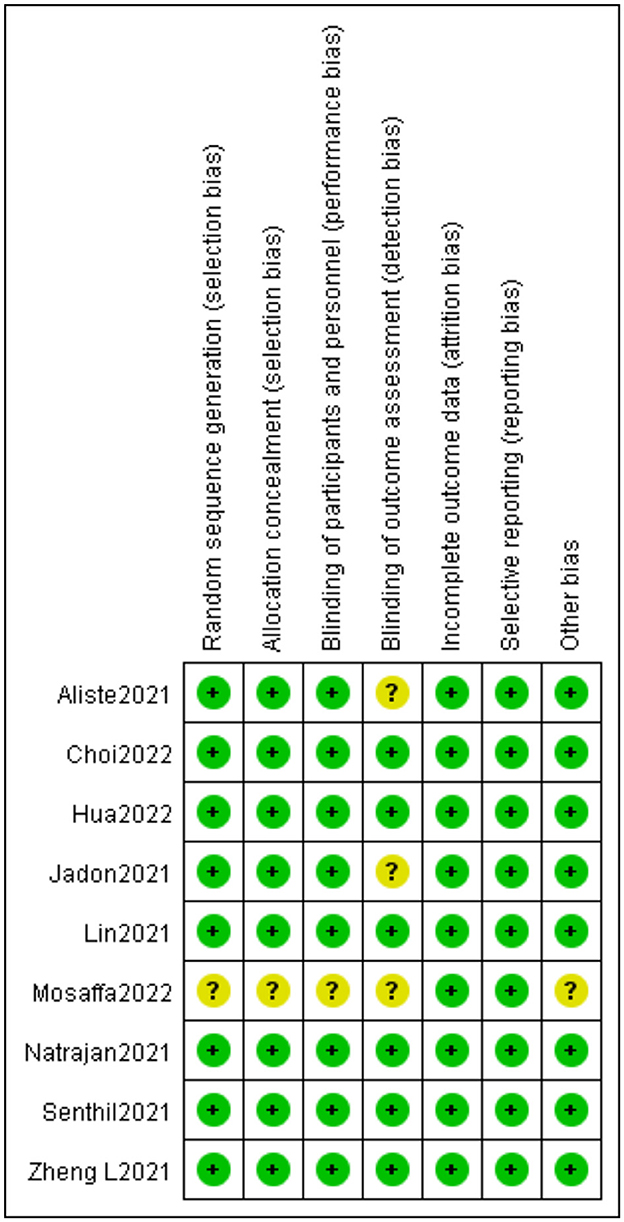
3.2. Risk of bias assessment
The risk of bias assessment results is shown in Figure 2. A low level of the overall risk of bias was observed for the included nine trials. Randomization of all patients into each group by appropriate methods was sufficient for allocation concealment in most studies. The two RCTs reviewed lacked sufficient details in the blinding outcome assessors, and in this case, we are conservative and thus inclined to classify the trial as “unclear risk of bias” (20, 24). Furthermore, when the random sequence generation, allocation concealment, blinding of participants and personnel, and blinding of outcome assessment were not described, we judged these bias evaluation items to be “unclear risk of bias” (22).
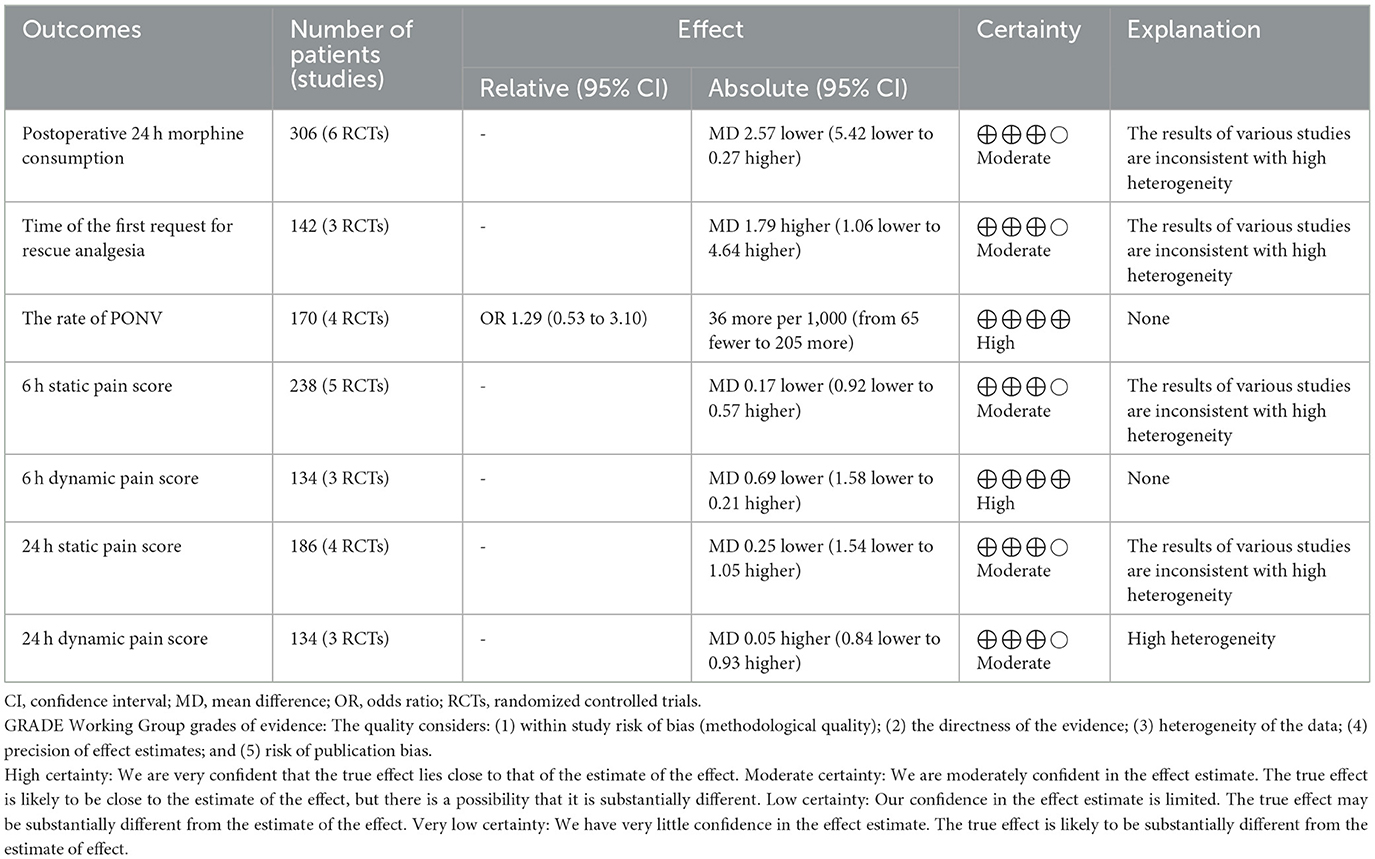
3.3. GRADE
The main results are shown in Table 2. When using the GRADE guidelines to assess the strength of the synthesized evidence, the evidence level of dynamic pain score 6 h after the operation, and the incidence of PONV were high. The certainty of the evidence was downgraded by high statistical heterogeneity and the results of various studies were inconsistent. Therefore, the other indicators obtained a moderate level of quality evaluation.
3.4. Primary outcome
3.4.1. Postoperative 24-h morphine consumption
In total, six studies described postoperative 24-h morphine consumption (18–23). Overall, the PENG block group used 2.57 mg less morphine than the control group within 24 h after the hip operation, but this was not enough for a statistically significant difference [MD: −2.57, 95% CI (−5.42, 0.27), moderate quality evidence, I2 = 58%, P = 0.08] (Figure 3A).
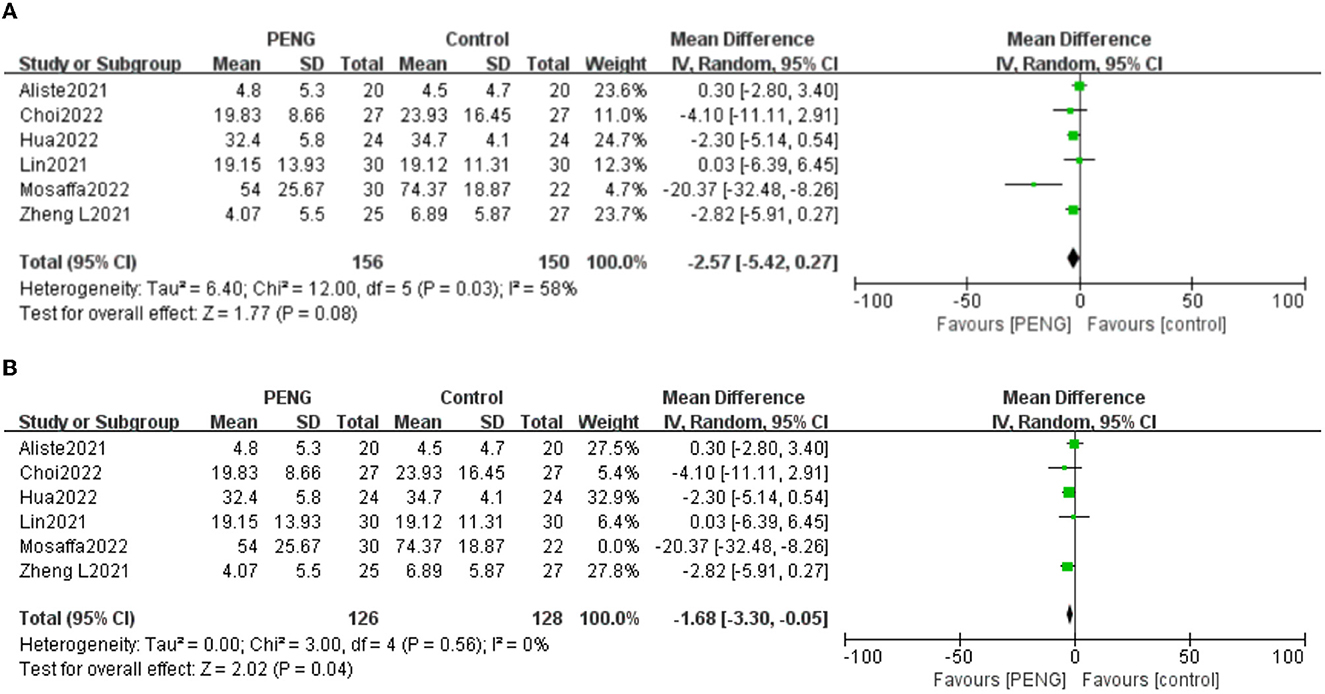
Figure 3. (A) Forest plot of postoperative 24 h morphine consumption. (B) Forest plot of postoperative 24 h morphine consumption after sensitivity analysis.
Sensitivity analysis showed that when the study of Mosaffa et al. (22) was removed, the pooled results were reversed, and the heterogeneity was significantly reduced [MD: −1.68, 95% CI (−3.30, −0.05), I2 = 0%, P = 0.04] (Figure 3B). This shows that the study of Mosaffa et al. (22) is the main heterogeneity source and the result is unstable.
3.5. Secondary outcomes
3.5.1. The time of the first request for rescue analgesia
Three studies reported the time of the first request for rescue analgesia (22, 24, 25). There were no significant differences between the two groups [MD: 1.79, 95% CI (−1.06, 4.64), I2 = 94%, P = 0.22] (Figure 4A). The certainty of the evidence was evaluated as moderate.
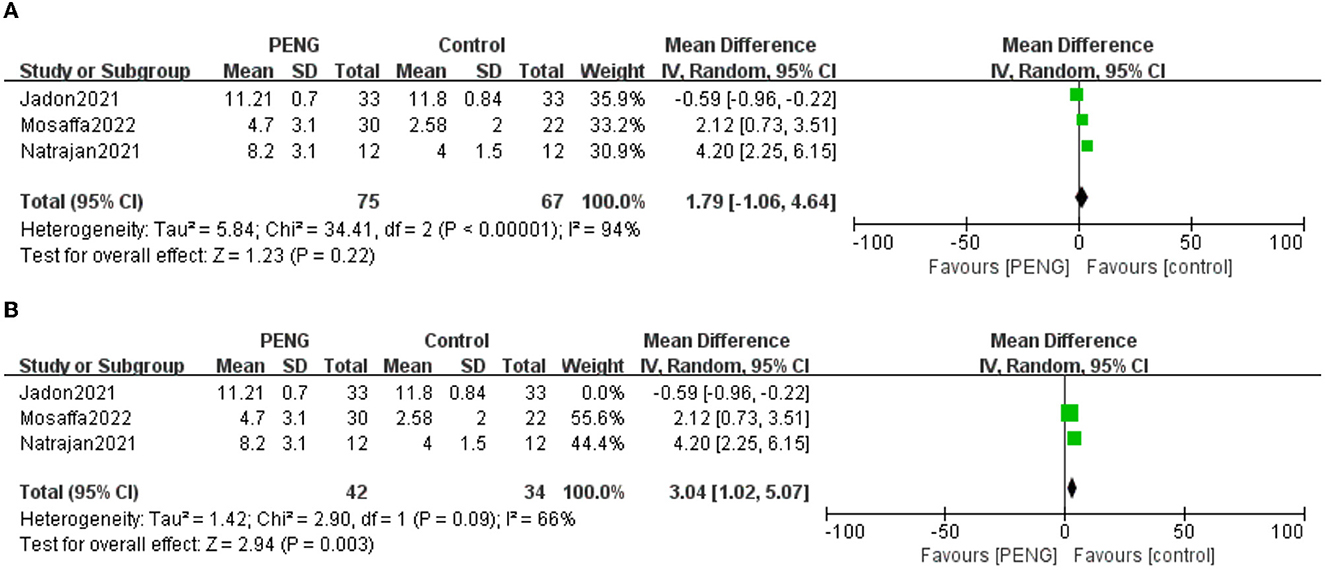
Figure 4. (A) Forest plot of the time of the first request for rescue analgesia. (B) Forest plot of the time of the first request for rescue analgesia after sensitivity analysis.
The sensitivity analysis showed that the study of Jadon et al. (24) significantly affected the result and heterogeneity of the pooled analysis [MD: 3.04, 95% CI (1.02, 5.07), I2 = 66%, P = 0.003] (Figure 4B). Therefore, this indicated that it was an unstable outcome.
3.5.2. Static pain scores 6 h after surgery
Participants included in the five trials (19–22, 26) were asked to grade the static pain scores 6 h postoperative. No significant differences were found between the two groups [MD: −0.17, 95% CI (−0.92, 0.57), moderate quality evidence, I2 = 60%, P = 0.65]. Subgroup analysis was done according to the different types of surgery. The subgroup analysis revealed a high degree of heterogeneity within the “total hip arthroplasty” subgroup [MD: −0.46, 95% CI (−1.96, 1.04), I2 = 67%, P = 0.55] (Figure 5A).
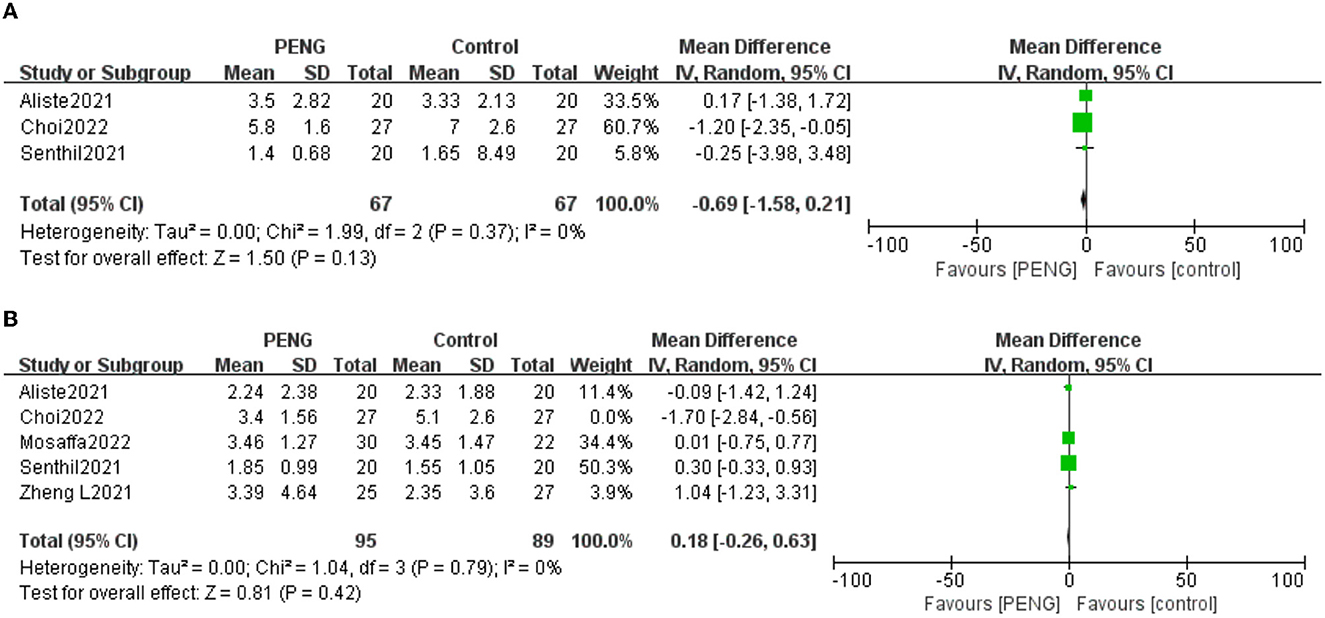
Figure 5. (A) Forest plot of the static pain scores 6 h postoperative. (B) Forest plot of the static pain scores 6 h postoperative after sensitivity analysis.
When examining the sources of heterogeneity, we carried out a sensitivity analysis. We found that the pooled analysis results remained unchanged after excluding the data of Choi et al. (21) but the heterogeneity decreased (MD = 0.18; 95% CI = −0.26 to 0.63; P = 0.42; I2 = 0%) (Figure 5B), indicating that this study is the main source of heterogeneity.
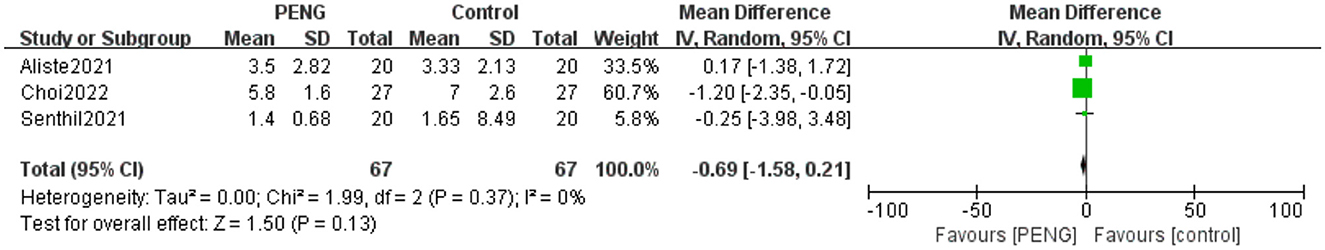
3.5.3. Dynamic pain scores 6 h after surgery
Three studies reported dynamic pain scores 6 h after surgery (20, 21, 26). There was no significant difference between the two groups [MD: −0.69, 95% CI (−1.58, 0.21), high-quality evidence, I2 = 0%, P = 0.13] (Figure 6). We performed a sensitivity analysis and confirmed the stability of this result.
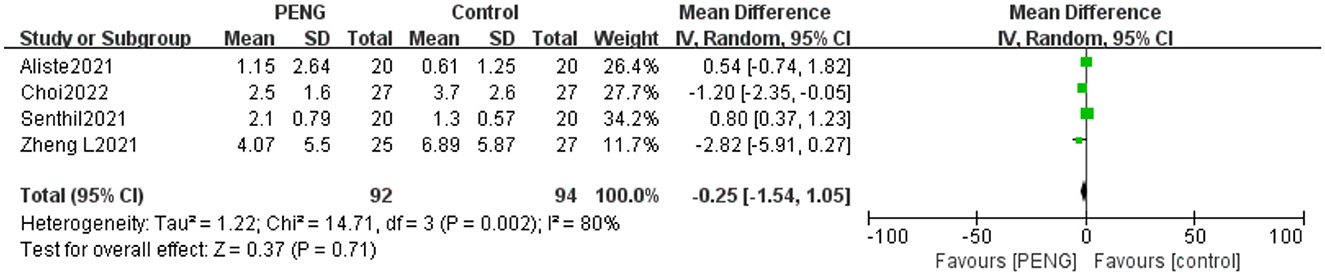
3.5.4. Static pain scores 24 h after surgery
Four studies reported static pain scores 24 h after surgery (19–21, 26). There was no significant difference between the PENG block and the other nerve block techniques [MD: −0.25, 95% CI (−1.54, 1.05), moderate quality evidence, I2 = 80%, P = 0.71] (Figure 7).
We performed sensitivity analyses and found that the pooled analysis result is stable, and the heterogeneity was still high.
3.5.5. Dynamic pain scores 24 h after surgery
Three trials reported the dynamic pain scores 24 h after surgery (20, 21, 26). No significant differences were found between the two groups [MD: 0.05, 95% CI (−0.84, 0.93), moderate quality evidence, I2 = 61%, P = 0.91] (Figure 8A).
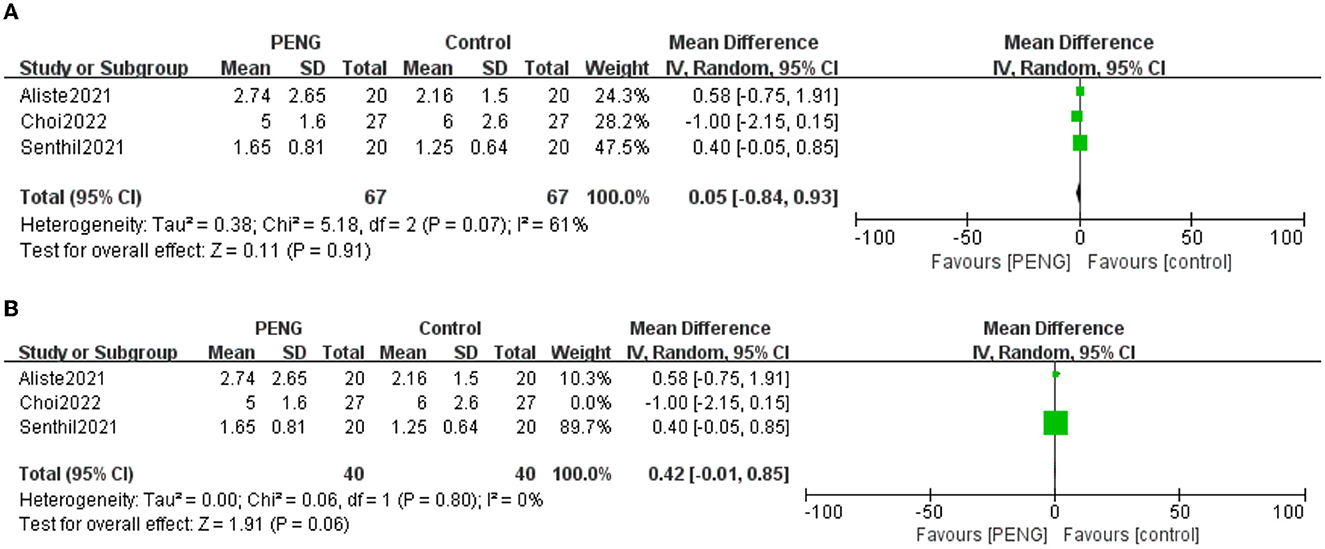
Figure 8. (A) Forest plot of the dynamic pain scores 24 h postoperative. (B) Forest plot of the dynamic pain scores 24 h postoperative after sensitivity analysis.
We carried out a sensitivity analysis and found that the pooled analysis results remained unchanged after excluding the data of Choi et al. (21), but the heterogeneity was low (MD = 0.42; 95% CI = −0.01 to 0.85; P = 0.06; I2 = 0%) (Figure 8B), indicating the main source of heterogeneity.
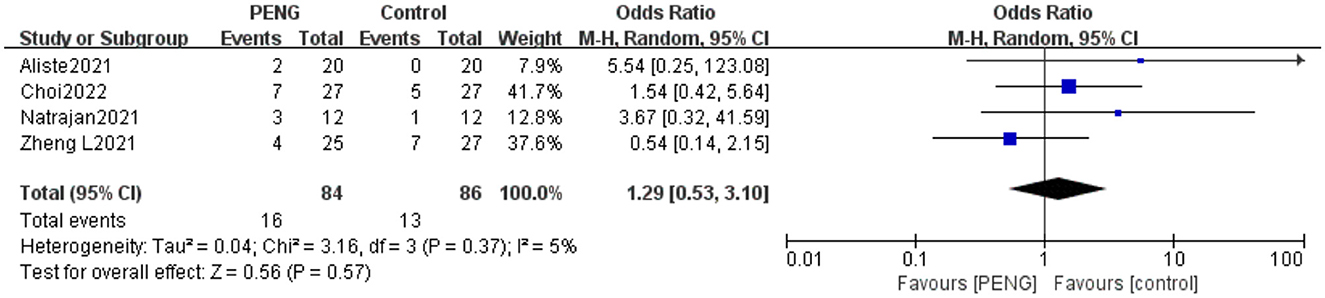
3.5.6. Incidence of PONV
Four studies reported the incidence of PONV (19–21, 25). The pooled effect showed that the incidence of PONV was similar between the two groups (OR: 1.29, 95% CI = 0.53–3.10, high-quality evidence, I2 = 5%, P = 0.57) (Figure 9). The sensitivity analysis confirmed that the result is stable.
4. Discussion
During this meta-analysis and systematic review, we evaluated the role of PENG block in the effectiveness of postoperative analgesia after hip surgery. We did not find any significant difference in PENG block in postoperative pain-related indicators and PONV compared with other nerve block techniques. Statistically, PENG block seemed to be as effective as other types of nerve blocks for alleviating pain after hip surgery. We note that the pooled result of postoperative 24-h morphine consumption in published relevant meta-analysis is inconsistent with ours (27). Due to different perspectives and inclusion criteria, the included studies are not quite the same. The purpose of this study was to compare PENG block with other nerve block methods and exclude those studies with a control group that received a sham block.
Traditionally, regional nerve block in hip surgery is performed using femoral nerve or fascia iliaca block. While partially effective, these blockade methods lead to a decrease in muscle strength (28). In the present research, the quadriceps muscle strength was similar between the PENG block group and the sham block group after surgery, and the ranges of quadriceps muscle activity and “time to first walk” were even significantly better in the PENG group (8, 9, 29). The exercise retention effect enables patients to move early after surgery, which in itself is associated with fewer complications, shorter hospital stays, and lower mortality (30, 31). As a result, the PENG block is capable of moving as quickly and with less pain than patients in the sham group. Furthermore, several studies have reported that the PENG block also protects motor function better than the femoral nerve and fascia iliaca compartment block (18, 20, 26).
We performed a sensitivity analysis for each comparison; some pooled results were reversed, and the heterogeneity decreased significantly. The studies rejected by the sensitivity analysis were reviewed, and we found that the reasons for rejection included some bias risks that were unclear (22), the style of anesthesia was different from other studies and general anesthesia was chosen (21), and a lack of description of the blind methods from the evaluator of the results (24). However, the reversed results did not contradict our conclusion. It is worth noting that although the nerve block methods of the control group in the nine RCTs were different, the sensitivity analysis did not find that this would lead to heterogeneity and unsteadiness of the pooled results. We will continue to pay attention to the relevant research results in the future and go on to update the current meta-analysis.
Several limitations exist in the present study. First, because the number of RCTs is not yet adequate and the evaluation methods of muscle strength index vary greatly, data types include dichotomous variables and continuous variables. We do not perform a quantitative analysis comparing the PENG block to control groups in preventing quadriceps weakness. Second, in several measurements, moderate to high heterogeneity was observed. Due to the small number of RCTs included for each pooled outcome, only the static pain scores 6 h postoperative were successfully analyzed in subgroups. The results of the subgroup and sensitivity analyses together showed that the study by Choi et al. (21) was the main source of heterogeneity. The study administered general anesthesia differently from other studies, which may have contributed to its increased heterogeneity. Other pooled results that could not be analyzed by subgroups could only be analyzed by sensitivity analysis and pooled analysis using a random effects model.
More and more researchers believe that it is inappropriate to go back and re-select fixed effect or random effect models after knowing the size of the heterogeneity (32). Compared with the fixed effect model, the random effect model gives a more conservative pooled value and a broader inter-group variability, with an increasing preference for a random-effect analysis a priori (32). Third, sensitivity analysis showed that certain results were unstable, and the meta-analysis should be strengthened by further studies. Fourth, the number of studies included is small, and the sample size was 12–33 patients per group, which may increase the possibility of class I errors. Because of the small number of studies per comparison, we could not reliably assess the risk of publication bias. Therefore, no publication bias test was performed in this study. Fifth, for ethical reasons, RCTs apply other nerve block methods as a control group to compare with the PENG block. This meta-analysis combined analgesia-related data from multiple nerve block methods as a control group, and in doing so, there was a risk of elevated heterogeneity, although sensitivity analysis did not identify this as a source of high heterogeneity.
5. Conclusion
In summary, PENG block provides an effective analgesic, similar to other peripheral nerve blocks in hip surgery. Considering that PENG block can better preserve motor function, it can be used as a promising regional anesthetic technique to replace other nerve blocks in hip surgery. At the same time, we encourage more relevant research to update this meta-analysis.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
LY conceived and designed the study. LY and XS performed the literature search and drafted the manuscript. HL was responsible for providing methodology and manuscript editing. All authors critically revised the manuscript and approved the final version for submission.
Funding
This study was supported in part by grants from the Scientific Research Funding of the Huzhou Science and Technology Bureau (Grant No. 2021GY11 to LY and XS), the National Natural Science Foundation of China (NSFC81300957 and NSFC82171227 to HL), and the Zhejiang Provincial Natural Science Foundation (LY22H090019 to HL).
Acknowledgments
We are grateful to Kai Sun, MD (Department of Anesthesiology, The Second Affiliated Hospital Zhejiang University School of Medicine) for providing many valuable suggestions to improve the quality of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1084532/full#supplementary-material
Supplementary Table S1. Search strategies for each database.
Abbreviations
PENG, Pericapsular nerve group; MD, mean difference; CI, confidence interval; PONV, postoperative nausea and vomiting; OR, odds ratio; RCTs, randomized controlled trials; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; VAS, visual analog scale; NRS, numerical rating scale; SD, standard deviation.
References
1. Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. (2006) 17:1726–33. doi: 10.1007/s00198-006-0172-4
2. Miyamoto RG, Kaplan KM, Levine BR, Egol KA, Zuckerman JD. Surgical management of hip fractures: an evidence-based review of the literature. I: femoral neck fractures. J Am Acad Ortho Surg. (2008) 16:596–607. doi: 10.5435/00124635-200810000-00005
3. Skinner HB, Shintani EY. Results of a multimodal analgesic trial involving patients with total hip or total knee arthroplasty. Am J Orthop. (2004) 33:85–92.
4. Girón-Arango L, Peng PWH, Chin KJ, Brull R, Perlas A. Pericapsular nerve group (Peng) block for hip fracture. Reg Anesth Pain med. (2018) 43:859–63. doi: 10.1097/AAP.0000000000000847
5. Short AJ, Barnett JJG, Gofeld M, Baig E, Lam K, Agur AMR, et al. Anatomic study of innervation of the anterior hip capsule: implication for image-guided intervention. Reg Anesth Pain Med. (2018) 43:186–92. doi: 10.1097/AAP.0000000000000778
6. Birnbaum K, Prescher A, Hessler S, Heller KD. The sensory innervation of the hip joint–an anatomical study. Surg Radiol Anat. (1997) 19:371–5. doi: 10.1007/BF01628504
7. Morrison C, Brown B, Lin DY, Jaarsma R, Kroon H. Analgesia and anesthesia using the pericapsular nerve group block in hip surgery and hip fracture: a scoping review. Reg Anesth Pain Med. (2021) 46:169–75. doi: 10.1136/rapm-2020-101826
8. Pascarella G, Costa F, Buono RD, Pulitanò R, Strumia A, Piliego C, et al. Impact of the pericapsular nerve group (Peng) block on postoperative analgesia and functional recovery following total hip arthroplasty: a randomised, observer-masked, controlled trial. Anaesthesia. (2021) 76:1492–8. doi: 10.1111/anae.15536
9. Lin D-Y, Brown B, Morrison C, Fraser NS, Chooi CSL, Cehic MG, et al. The pericapsular nerve group (Peng) block combined with local infiltration analgesia (Lia) compared to placebo and lia in hip arthroplasty surgery: a multi-center double-blinded randomized-controlled trial. BMC Anesthesiol. (2022) 22:252. doi: 10.1186/s12871-022-01787-2
10. Amato PE, Coleman JR, Dobrzanski TP, Elmer DA, Gwathmey FW Jr., Slee AE, et al. Pericapsular nerve group (Peng) block for hip arthroscopy: a randomized, double-blinded, placebo-controlled trial. Reg Anesth Pain Med. (2022) 23:907. doi: 10.1136/rapm-2022-103907
11. Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (Prisma-P) 2015: elaboration and explanation. BMJ. (2015) 350:g7647. doi: 10.1136/bmj.g7647
12. McGrath S, Zhao X, Steele R, Thombs BD, Benedetti A. Estimating the sample mean and standard deviation from commonly reported quantiles in meta-analysis. Stat Methods Med Res. (2020) 29:2520–37. doi: 10.1177/0962280219889080
13. Cai S, Zhou J, Pan J. Estimating the sample mean and standard deviation from order statistics and sample size in meta-analysis. Stat Methods Med Res. (2021) 30:2701–19. doi: 10.1177/09622802211047348
14. Madenoglu H, Yildiz K, Dogru K, Kurtsoy A, Güler G, Boyaci A. Randomized, double-blinded comparison of tropisetron and placebo for prevention of postoperative nausea and vomiting after supratentorial craniotomy. J Neurosurg Anesthesiol. (2003) 15:82–6. doi: 10.1097/00008506-200304000-00003
15. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
16. Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. Grade guidelines: 1. Introduction-grade evidence profiles and summary of findings tables. J Clin Epidemiol. (2011) 64:383–94. doi: 10.1016/j.jclinepi.2010.04.026
17. Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ. (2004) 7454:1490. doi: 10.1136/bmj.328.7454.1490
18. Lin D-Y, Morrison C, Brown B, Saies AA, Pawar R, Vermeulen M, et al. Pericapsular nerve group (Peng) block provides improved short-term analgesia compared with the femoral nerve block in hip fracture surgery: a single-center double-blinded randomized comparative trial. Reg Anesth Pain Med. (2021) 46:398–403. doi: 10.1136/rapm-2020-102315
19. Zheng L, Jo Y, Hwang J, Rhim H, Park E, Oh C, et al. Comparison of the analgesic efficacy of periarticular infiltration and pericapsular nerve group block for total hip arthroplasty: a randomized, non-inferiority study. Ann Palliat Med. (2022) 11:1222–30. doi: 10.21037/apm-21-2785
20. Aliste J, Layera S, Bravo D, Jara A, Munoz G, Barrientos C, et al. Randomized comparison between pericapsular nerve group (Peng) block and suprainguinal fascia iliaca block for total hip arthroplasty. Reg Anesth Pain Med. (2021) 46:874–8. doi: 10.1136/rapm-2021-102997
21. Choi YS, Park KK, Lee B, Nam WS, Kim D-H. Pericapsular nerve group (Peng) block versus supra-inguinal fascia iliaca compartment block for total hip arthroplasty: a randomized clinical trial. J Pers med. (2022) 12:408. doi: 10.3390/jpm12030408
22. Mosaffa F, Taheri M, Rasi AM, Samadpour H, Memary E, Mirkheshti A. Comparison of pericapsular nerve group (Peng) block with fascia iliaca compartment block (Ficb) for pain control in hip fractures: a double-blind prospective randomized controlled clinical trial. Orthop Traumatol Surg Res. (2022) 108:103135. doi: 10.1016/j.otsr.2021.103135
23. Hua H, Xu Y, Jiang M, Dai X. Evaluation of pericapsular nerve group (Peng) block for analgesic effect in elderly patients with femoral neck fracture undergoing hip arthroplasty. J Healthc Eng. (2022) 2022:7452716. doi: 10.1155/2022/7452716
24. Jadon A, Mohsin K, Sahoo RK, Chakraborty S, Sinha N, Bakshi A. Comparison of supra-inguinal fascia iliaca versus pericapsular nerve block for ease of positioning during spinal anaesthesia: a randomised double-blinded trial. Indian J Anaesth. (2021) 65:572–8. doi: 10.4103/ija.IJA_417_21
25. Natrajan P, Bhat RR, Remadevi R, Joseph IR, Vijayalakshmi S, Paulose TD. Comparative study to evaluate the effect of ultrasound-guided pericapsular nerve group block versus fascia iliaca compartment block on the postoperative analgesic effect in patients undergoing surgeries for hip fracture under spinal anesthesia. Anesth Essays Res. (2021) 15:285–9. doi: 10.4103/aer.aer_122_21
26. Senthil KS, Kumar P, Ramakrishnan L. Comparison of pericapsular nerve group block versus fascia iliaca compartment block as postoperative pain management in hip fracture surgeries. Anesth Essays Res. (2021) 15:352–6. doi: 10.4103/aer.aer_119_21
27. Huda AU, Ghafoor H. The use of pericapsular nerve group (Peng) block in hip surgeries is associated with a reduction in opioid consumption, less motor block, and better patient satisfaction: a meta-analysis. Cureus. (2022) 14:e28872. doi: 10.7759/cureus.28872
28. Gasanova I, Alexander JC, Estrera K, Wells J, Sunna M, Minhajuddin A, et al. Ultrasound-guided suprainguinal fascia iliaca compartment block versus periarticular infiltration for pain management after total hip arthroplasty: a randomized controlled trial. Reg Anesth Pain Med. (2019) 44:206–11. doi: 10.1136/rapm-2018-000016
29. Zheng J, Pan D, Zheng B, Ruan X. Preoperative pericapsular nerve group (Peng) block for total hip arthroplasty: a randomized, placebo-controlled trial. Reg Anesth Pain Med. (2022) 47:155–60. doi: 10.1136/rapm-2021-103228
30. Baer M, Neuhaus V, Pape HC, Ciritsis B. Influence of mobilization and weight bearing on in-hospital outcome in geriatric patients with hip fractures. Sicot J. (2019) 5:4. doi: 10.1051/sicotj/2019005
31. Kuru T, Olçar HA. Effects of early mobilization and weight bearing on postoperative walking ability and pain in geriatric patients operated due to hip fracture: a retrospective analysis. Turk J Med Sci. (2020) 50:117–25. doi: 10.3906/sag-1906-57
Keywords: pericapsular nerve group block, postoperative pain, regional, opioid consumption, anesthesia
Citation: Yu L, Shen X and Liu H (2023) The efficacy of pericapsular nerve group block for postoperative analgesia in patients undergoing hip surgery: A systematic review and meta-analysis of randomized controlled trials. Front. Med. 10:1084532. doi: 10.3389/fmed.2023.1084532
Received: 30 October 2022; Accepted: 03 February 2023;
Published: 24 February 2023.
Edited by:
Shun Ming Chan, Tri-Service General Hospital, TaiwanReviewed by:
Yong tao Sun, Shandong Provincial Qianfoshan Hospital, ChinaAbhijit Nair, Ministry of Health, Oman
Copyright © 2023 Yu, Shen and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: He Liu,  bGgxMjEwNjFAMTYzLmNvbQ==
bGgxMjEwNjFAMTYzLmNvbQ==
 Liang Yu
Liang Yu Xiaojuan Shen2
Xiaojuan Shen2 He Liu
He Liu