
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med. , 09 February 2023
Sec. Pulmonary Medicine
Volume 10 - 2023 | https://doi.org/10.3389/fmed.2023.1041115
This article is part of the Research Topic COVID-19: Integrating Artificial Intelligence, Data Science, Mathematics, Medicine and Public Health, Epidemiology, Neuroscience, Neurorobotics, and Biomedical Science in Pandemic Management, volume II View all 92 articles
Background: Oxidative stress plays an important role in the pathogenesis of many diseases. This study aimed to investigate the relationship between nuclear factor kappa B (NF-κB) and oxidative stress and the severity of the disease in new COVID-19 patients, and, to compare the levels of NF-κB, oxidized LDL (oxLDL), and lectin-like oxidized-LDL receptor-1 (LOX-1) with oxygen saturation, which is an indicator of the severity parameters of the disease in COVID-19 patients.
Methods: In this prospective study, 100 COVID-19 patients and 100 healthy subjects were selected.
Results: LOX-1, NF-κB, and oxLDL were found to be higher in COVID-19 patients compared to the healthy subjects (p < 0.001 for all). According to the results of correlation analysis, it was found that there was no significant relationship between oxygen saturation and LOX-1, NF-κB and oxLDL parameters. There was significant relationship between oxLDL with LOX-1 and NF-κB in patients with COVID-19 disease. ROC analysis results of the highest discrimination power were oxLDL (AUC: 0.955, CI: 0.904–1.000; sensitivity: 77%, and specificity: 100%, for cutoff: 127.944 ng/l) indicating COVID-19.
Conclusion: Oxidative stress plays an essential role in COVID-19. NF-κB, oxLDL, and LOX-1 seem to represent good markers in COVID-19. Our study also showed that oxLDL has the highest power in distinguishing patients with COVID-19 from the healthy subjects.
The virus, which emerged in late 2019 and called SARS-CoV-2 by the World Health Organization, spread rapidly around the world, causing a pandemic. While the disease called corona virus disease 2019 (COVID-19) progressed with asymptomatic or mild symptoms in some people, severe disease findings requiring hospitalization were observed in approximately 20% of the cases. The morbidity and mortality of COVID-19 is mostly associated with acute viral pneumonia and associated severe acute respiratory distress syndrome (ARDS) (1, 2).
Oxidative stress and inflammation cause oxidation of lipids and lipoproteins, and play an important role in the pathogenesis of many diseases (3). Oxidized LDL (oxLDL) formation is seen in various diseases resulting in oxidative stress and the presence of reactive oxygen species (ROS) (4). OxLDL leads to the progression of lesions in atherosclerosis, diabetes mellitus (DM), aging, non-alcoholic fatty liver, metabolic syndrome (MS), cardiovascular diseases (CVD) and cerebrovascular diseases, nephrotic syndrome, chronic renal failure, diabetic nephropathy, nephrosclerosis, and acute renal failure. It causes and plays an important role in the pathogenesis of the disease (5–7). It is expressed by pro-inflammatory and pro-oxidative stress in lectin-like oxidized-LDL receptor-1 (LOX-1) cells and endothelium, monocyte, macrophage, smooth muscle cells, cardiomyocytes, fibroblast, adipocyte, airway epithelial cells, dendritic cells, and thrombocytes (8–10).
LOX-1 expression increased by oxLDL stimulates the growth and proliferation of smooth muscle cells (SMC) with nuclear factor kappa B (NF-κB) and JNK signaling pathways, causing SMCs to move from the media to the subendothelial area. LOX-1 plays an important role in fibroblast growth and collagen synthesis stimulated by angiotensin II and transforming growth factor beta (TGF-β). The presence of LOX-1 in activated platelets is associated with thrombus formation (7).
In this respect, our aim in this study is to investigate the relationship between NF-κB and oxidative stress and the severity of the disease in new COVID-19 patients, and, to compare the levels of NF-κB, oxLDL, and LOX-1 with oxygen saturation (SO2), which is an indicator of the severity parameters of the disease in COVID-19 patients.
The study was designed prospectively. All procedures in our study comply with the 1964 Declaration of Helsinki and any subsequent amendments or comparable ethical standards. The study was approved by the Mehmet Ali Aydinlar University Faculty of Medicine Ethics Committee and informed consent was obtained from all participants (ATADEK-2020/17).
Of two hundred subjects who were admitted to Atakent Hospital emergency department between 15 March 2020 and 15 November 2022, 100 subjects with COVID-19 were included in this study. The recommended criteria established by the Scientific Committee of the Ministry of Health were used for the selection of possible COVID-19 patients. These criteria are having at least one sign or symptom of fever or acute respiratory illness (cough and respiratory distress); the presence of clinical features that cannot be explained by any other disease; the patient or a relative has a history of traveling to another country for 14 days prior to the onset of symptoms; and close contact with a patient confirmed to be COVID-19 positive by reverse transcription polymerase chain reaction (RT-PCR). Their diagnoses were confirmed by radiologist. The patients were selected from those over the age of 18 who applied to Acibadem Atakent Hospital with positive COVID-19 PCR and/or Thorax CT (100 cases) and 100 healthy subjects. Studies show that thorax CT has higher sensitivity than RT-PCR. RT-PCR false negatives can be quite high due to the immature development of nucleic acid detection technology, differences in detection rate from different manufacturers, low patient viral load, or inappropriate clinical sampling (11). In our study, 33 patients (33%) had positive RT-PCR results, 67 patients (67%) had negative RT-PCR results, and thorax CT results of all 89 patients were typically compatible with COVID-19 pneumonia. Patients were classified as uncomplicated, mild–moderate pneumonia, and severe pneumonia. Patients with symptoms such as fever, muscle/joint pain, cough, and sore throat, without respiratory distress (respiratory rate <24 per minute, SpO2 >93% in room air) and with normal chest X-ray and/or lung tomography were classified as uncomplicated. Patients with symptoms such as fever, muscle/joint pain, cough and sore throat, respiratory rate <30/min, SpO2 >90 in room air, and mild–moderate pneumonia findings on chest X-ray or tomography were classified as mild–moderate pneumonia. Patients with symptoms such as fever, muscle/joint pains, cough, and sore throat, with tachypnea (≥30/min), with SpO2 level below ≤90% in room air, and bilateral diffuse pneumonia findings on chest X-ray or tomography were classified as severe pneumonia. Control subjects were selected from individuals who were confirmed by PCR and clinical evaluation as not having COVID-19 disease and had no additional disease. All patients were of Turkish descent.
Age of COVID-19 diagnosis: ≥18 years. Patients who presented with positive SARS-CoV-2 RNA finding in throat swab samples and were diagnosed with COVID-19 according to the World Health Organization guidelines or having positive RT-PCR test with oxygen saturation rate below 90%.
Patients aged <18 years, cancer, obesity, diabetes, smoking, pregnant, and still hospitalized but not yet discharged from the hospital were excluded from this study.
After being diagnosed with COVID-19, treatment was given to all patients in line with the recommendations of the Scientific Board of the Turkish Ministry of Health. All patients were started on hydroxychloroquine loading 2*400 followed by 2 × 200 mg for a total of 5 days/azithromycin (500 mg on the first day followed by 250 for a total of 5 days) plus oseltamivir 75 mg given twice. Favipiravir was reserved for severe cases with dyspnea and SpO2 <90%. It was given in the dose of 1,600 mg twice on day one followed by 600 mg for the next 4 days.
The chest CT examinations were reported in accordance with the Radiological Society of North America (RSNA) Consensus Statement on Reporting Chest CT Findings Related to COVID-19.
Combined pharyngeal and nasopharyngeal swab samples were obtained for RT-PCR assay.
Samples were drawn into plain tubes with no additive, in the morning after an overnight fasting (10–12 h) from patients with COVID-19 and their respective controls. Serum samples were separated from cells immediately after centrifugation (4,000 rpm, 10 min at 4°C), aliquoted, and stored at −80°C until assayed for NF-κB, oxLDL, and LOX-1.
Routine biochemical parameters were measured by the autoanalyzer (Siemens Dimension, Germany). Serum C-reactive protein (CRP) levels were measured by a photometric method (Siemens Dimension, Germany). Complete blood count parameters were obtained with automatic hematology analyzer (Sysmex XN-2000, Germany).
Oxygen saturation (SO2) levels were measured by blood gas analyze (Siemens Rapid 500, Germany).
Serum NF-κB levels were measured by a commercially available competitive enzyme-linked immunoassay kit (R&D Systems, Minneapolis, MN, United States). The coefficients of intra- and inter-assay variations were 4.6% (n = 20) and 5.4% (n = 20), respectively.
Serum oxLDL levels were measured by a commercially available competitive enzyme linked immunoassay kit (R&D Systems, Minneapolis, MN, United States). The coefficients of intra- and inter-assay variation were 4.5% (n = 20) and 5.3% (n = 20), respectively.
Serum LOX-1 levels were measured by a commercially available competitive enzyme linked immunoassay kit (R&D Systems, Minneapolis, MN, United States). The coefficients of intra- and inter-assay variation were 4.7% (n = 20) and 5.8% (n = 20), respectively.
In the statistical analysis of the study, the criteria discussed were defined by mean, standard deviation, frequency, and percentage values. The distribution of all analyzed parameters was confirmed using the Kolmogorov–Smirnov test. Results for normally distributed continuous variables were expressed as means ± standard deviations. Chi-Square test was used to compare frequencies and percentages between the groups. Student’s t-test was used for comparisons of two groups. One-way ANOVA and Tukey test as post-hoc were used in the comparison of three groups. Correlation analysis was performed using Spearman’s correlation analysis. In the study cases, receiver operating characteristic (ROC) curve analysis was used to investigate the performance of important criteria in determining disease diagnosis. As a result of the ROC analysis, cutoff points were determined by using the Youden Index. A p value below 0.05 was expressed as significant. Post-hoc power analysis was performed for the study, and the power of the study was found to be 100% at α = 0.05, for all three parameters (LOX-1, NF-κB, and oxLDL). All statistical analyses were carried out using Statistical Product and Service Solutions (SPSS) v. 21.0 (IBM, Armonk, NY, United States) package program.
Both groups were selected from patients and healthy subjects matched for gender and age (no statistically significant difference). Dot graph of population age distribution was also shown in Figure 1. When the clinical results of the patients were evaluated, no significant difference was found between diastolic blood pressure (DBP), systolic blood pressure (SBP), and SO2 levels. However, PCR and radiological findings were found to be significantly positive in patients with COVID-19 (both p < 0.001). No significant difference was found between the groups in terms of survive status (Table 1). Clinical parameters of the COVID-19 patients are also shown in Table 2.
Hematological values and routine biochemical tests of the patients were evaluated, and no significant difference was found (Tables 3, 4). There was no significant difference in total cholesterol, high density lipoprotein (HDL), LDL, and triglyceride levels between the groups (p > 0.05 for all; Table 4). All three parameters LOX-1, NF-κB, and ox-LDL were found to be higher in COVID-19 patients compared to the healthy subjects (p < 0.001 for all) (Table 5). There was significant relationship between oxLDL with LOX-1 (r: 0.921; p < 0.0001) and NF-κB (r: 0.712; p < 0.0001) in patients with COVID-19 disease. The TC scanning of these patients was evaluated and no correlation was found between the change in TC and biomarker levels.
In the subgroups formed according to disease severity, LOX-1 levels in patients with severe pneumonia were found to be statistically significantly higher than both uncomplicated COVID-19 patients (p < 0.01) and mild–moderate pneumonia patients (p < 0.05). While oxLDL levels were found to be higher in patients with severe pneumonia than only uncomplicated COVID-19 patients (p < 0.05), no significant difference was found between NF-κB values according to disease severity. In Ex patients, LOX-1, NF-κB, and oxLDL levels were all found to be higher compared to the healed patients (p < 0.05 for all), (Table 6).
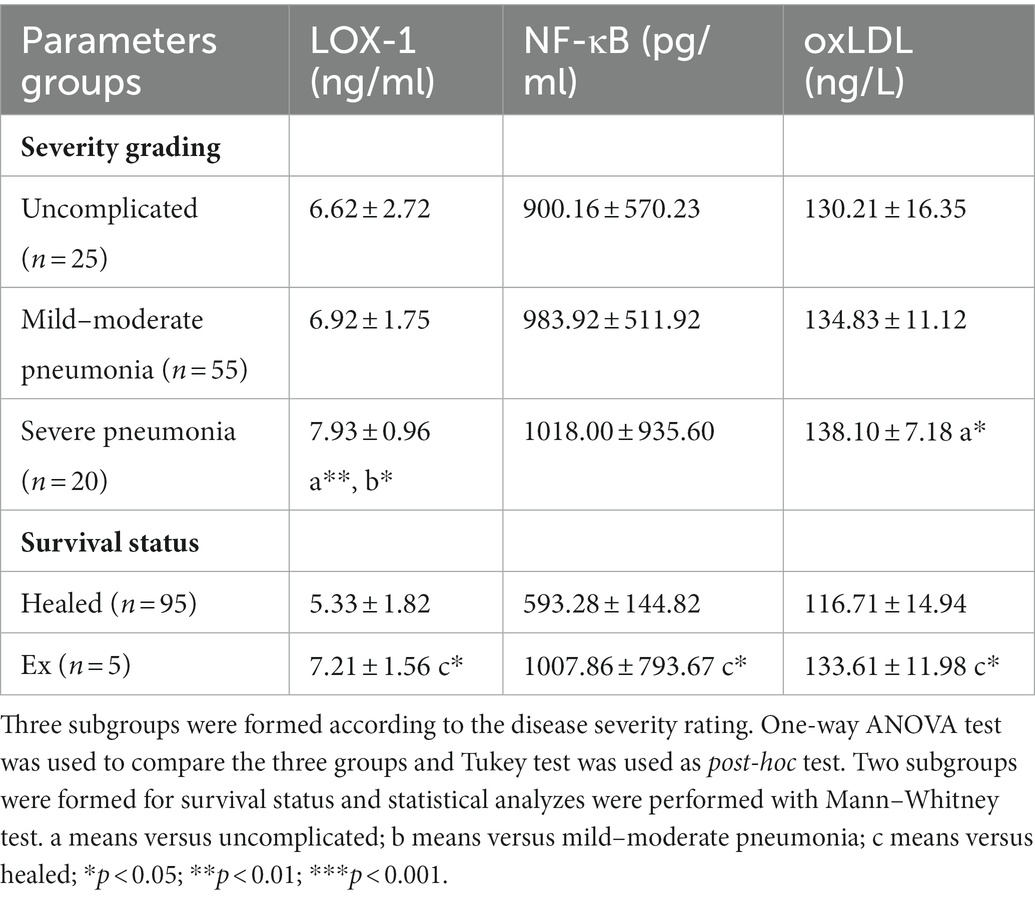
Table 6. Oxidative stress-related biomarkers of the subgroups according to severity grading and survival status.
ROC analysis results for important biochemical parameters showed that all three parameters (LOX-1, NF-κB, and oxLDL) had high discrimination power from patients with COVID-19 (Figure 2). Accordingly, LOX-1 was found to be the parameter with the lowest discrimination power (AUC: 0.787, CI: 0.722–0.852; sensitivity: 88%; and specificity: 62%, for cutoff: 1.93 ng/ml), while the parameter with the highest discrimination power was oxLDL (AUC: 0.26, CI: 0.892–0.961; sensitivity: 81%; and specificity: 87%, for cutoff: 124.38 ng/l) (Table 7).
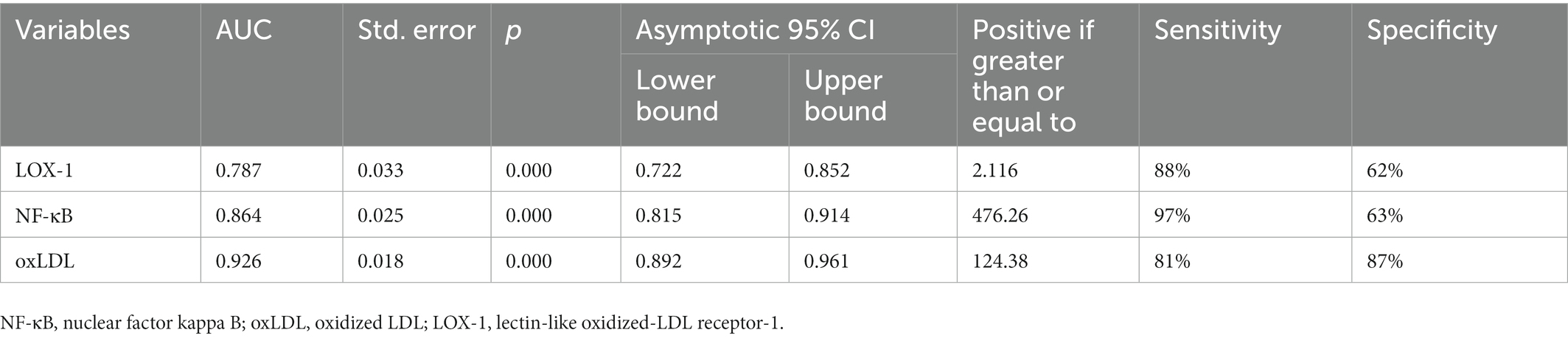
Table 7. Cutoff values, sensitivity and specificity values by ROC analysis for LOX-1, NF-κB and ox-LDL values indicating COVID-19.
To the best of our knowledge, this is the first report to showing changes in three key parameters as NF-κB, oxLDL, and LOX-1 in systemic oxidative stress using an analysis of multiple biomarkers in COVID-19 patients. We believe that oxidative stress plays an important role in the pathological development of COVID-19.
The most important contributions of the laboratory findings are that they give an idea about the staging, prognosis, and therapeutic monitoring of COVID-19. Many laboratory tests can be very helpful in determining the severity of the disease and in determining the risk of development of ARDS, disseminated intravascular coagulation (DIC), and multiple organ failure (1, 2). Biochemical monitoring of COVID-19 patients with in vitro diagnostic tests is crucial for assessing disease diagnosis, severity, and progression, as well as monitoring therapeutic intervention. In addition to the laboratory tests commonly used in routine, new evidence suggests that serious COVID-19 patients may be at risk for cytokine storm syndrome. Defining laboratory tests that will contribute to the diagnosis and follow-up of COVID-19 patients is very important to distinguish between severe and non-severe cases, and to identify those with low or high mortality risk, in addition to the stage of diagnosis.
We examine the biochemical events that characterize the progression of COVID-19 in relation to three markers sensitive to increased ROS as possible candidates in the of NF-κB, oxLDL, and LOX-1. NF-κB is a transcription factor, oxLDL is a critical factor in atherogenesis, and LOX-1 is the major receptor for oxLDL in human endothelial cells.
Stimuli that increase LOX-1 expression are cytokines, interferon-V (IFN-V), oxLDL and other modified lipoproteins, free radicals, TNF-α, interleukin (IL-1β), TGF-β1, superoxide anion hydrogen peroxide (H2O2), 8-isoprostoglandin F2-α, and lysophosphatidylcholine (7, 12–14). Macrophages trained by oxLDL encounter large amounts of oxidized lipids in the infected areas and exhibit greater oxidized lipid uptake, leading to transient lipid depletion (8).
In COVID-19, thrombosis occurs because of blood clotting, causing blockages in the heart, lungs and vessels. Thrombotic events occur very frequently in intensive care patients for a variety of reasons. Chemokines (E, P selectin), intracellular adhesion molecule-1 (ICAM-1), and vascular cell adhesion molecule-1 (VCAM-1) by activation of NF-κB because of stimulation of vascular cells by binding oxLDL to LOX-1 lead to increased expression of granulocyte and macrophage colony-stimulating factors and monocyte chemotactic protein-1 (MCP1), leading to proatherogenic effects (7).
In SARS-CoV-infected macrophages, NF-κB is activated by the CARD9-BCL10 (Caspase recruitment domain family member 9-B-cell lymphoma/leukemia 10) module and triggers the major inflammatory adapter protein apoptosis-associated speck-like protein containing a caspase recruitment domains (ASC) (15). Reactive oxygen and nitrogen species are also a signaling molecule responsible for the release of pro-inflammatory cytokines. In particular, it activates redox-sensitive transcription factors such as NF-κB, which play a key role in inflammation (16). Oral and intravenous glutathione (GSH), GSH precursor N-acetyl-cysteine (NAC), and alpha lipoic acid (ALA) are known to block NF-κB. These molecules are new treatment approaches used for respiratory distress and cytokine storm syndrome in COVID-19 pneumonia (17). In current study, all three parameters LOX-1, NF-κB, and oxLDL were found to be higher in COVID-19 patients compared to the healthy subjects. Moreover, there were significant relationship between oxLDL with LOX-1 and NF-κB in patients with COVID-19 disease. At the same time, no significant difference was found between the groups in total-cholesterol, HDL-cholesterol, and LDL-cholesterol levels. Interestingly, Hu et al. (9) showed that serum lipid levels, especially total-cholesterol, HDL-cholesterol, and LDL-cholesterol, were significantly lower in patients with COVID-19 infection. In fact, up to 90% of circulating oxLDL can be found in oxLDL immune complexes (oxLICs). Preparation of OxLIC-mediated inflammatory signalosomes in macrophages is dependent on CARD9. It is a critical adapter protein and a central integrator in innate immune cell activation that triggers the inflammatory signaling pathway in response to viral infection. CARD9 signalosome, a triple protein complex consisting of CARD9, BCL10, and MALT1 (CBM complex), leads to the activation of NF-κB and mitogen activated protein kinase (MAPK) signaling result in up-regulation of several cytokines and chemokines (10). Wei et al. (18) reported that the development of hypolipidemia started in patients with mild symptoms and gradually worsened in relation to the severity of the disease. Acute inflammation caused by SARS-COV-2 alters lipid metabolism. Pro-inflammatory cytokines such as TNF-, IL-6, and IL-1β have been reported to modulate lipid metabolism by altering liver function and reducing cholesterol influx and transport. It was reported that IL-6 increased dramatically in 96% of all patients. They demonstrated that pro-inflammatory cytokines such as IL-6 are a significant contributor to lipid abnormalities in patients. This strongly suggests that pro-inflammatory cytokines such as IL-6 are a significant contributor to lipid abnormalities in patients. Lipids are highly vulnerable to the degradation of free radicals, which are usually raised in host cells with a viral infection (19). Assignment of oxLDL in the serum of patients will be required to determine this possibility.
Pincemail et al. (20) have recently proven that systemic oxidative stress increases lipid peroxidation in critically ill COVID-19 patients, as well as deficiencies in some antioxidants (vitamin C, glutathione, and thiol proteins) and trace elements (selenium). Strong positive correlations between lipid peroxides and Cu and the negative correlation between γ-tocopherol and Cu highlighted the role played by copper in increased oxidative stress in COVID-19 patients. Oxidative stress is increased in patients with COVID-19 and is associated with mortality (21).
LOX-1 levels were found to be higher in patients with severe pneumonia compared to both uncomplicated COVID-19 patients and patients with mild to moderate pneumonia, while oxLDL levels were found to be higher in patients with severe pneumonia than in patients with only uncomplicated COVID-19. At the same time, in Ex patients, LOX-1, NF-κB, and oxLDL levels were all found to be higher compared to the healed patients. NF-κB, oxLDL, and LOX-1 levels are independent risk factors in determining the prognosis of COVID-19. COVID-19 is a disease whose activity is still very high and continues to spread rapidly. Scientists continue to search for markers that can help with the early detection and prognosis of this disease. The results of our study are consistent with studies reporting that oxidative stress markers are significantly increased in COVID-19 patients (22, 23). We think that the biochemical parameters mentioned in our study are important in determining the prognosis of the disease and may be beneficial, together with other risk factors, in terms of the need for transfer to the intensive care unit after the initial evaluation of the patients in the emergency unit (24–26).
In general, increased oxidative stress with all symptoms in patients diagnosed with COVID-19; may cause an increase in the symptoms of this chronic disease in individuals with other chronic diseases. This may cause the progression of COVID-19 in individuals to be severe and heavy. Accordingly, it has been predicted that supplementing diagnosed COVID-19 patients with strong antioxidant substances may have a protective effect. For example, ginger extract is a wealthy source of antioxidants and can be used to prevent the glycation and oxidative stress-induced damage of biomolecules in various health complications including inflammation (27). In many studies, the administration of various antioxidants as both prophylactic and therapeutic support to COVID-19 patients has been shown to reduce their symptoms (17, 28–47).
In the current study, 33 patients (33%) had positive RT-PCR results, 67 patients (67%) had negative RT-PCR results, and thorax CT results of all 89 patients were typically compatible with COVID-19 pneumonia. Combined pharyngeal and nasopharyngeal swab (RT-PCR) tests may be negative, especially in the early phase of the disease or when the viral load is low, and CT plays an important role in the diagnosis of COVID-19 during this period. The sensitivity of CT in the diagnosis of COVID-19 was found to be 98%, while the sensitivity of RT PCR, which is the gold standard diagnostic test, was found to be 71% in the early period (11). Although RT-PCR test is the gold standard for the diagnosis of COVID-19, chest X-ray and CT have an important role in the diagnosis, follow-up, and staging of pneumonia (48, 49).
Although our study has strengths, it has some limitations. However, as can be seen in the results we presented, we see that the presence or absence of each of these comorbid diseases does not cause a change in NF-κB, oxLDL, and LOX-1 levels, which are the main parameters of our study. The limitation of this study is the small number of the patients included in a single center. We used a convenience sample which may increase the risk of selection bias. Our study did not allow us to conclude whether increased oxidative stress could be directly attributed to COVID-19 disease.
NF-κB, oxLDL, and LOX-1 seem to represent good markers in COVID-19. Oxidative stress may play a critical role in the development of COVID-19 disease and of damage to the COVID-19 patients. Our study also showed that oxLDL has the highest power in distinguishing patients with COVID-19 from healthy subjects. Since increased oxidative stress was observed in patients who died compared to those who recovered, we think that the use of NF-κB, oxLDL, and LOX-1 levels at the onset of COVID-19 disease is a valuable starting point for the general assessment of oxidative stress, and thus provides better triage for patients in terms of disease severity. Antibiotics are produced and fought against bacteria, but the battle against viruses must be very different. At this point, the strongest weapon is the immune system. Because viruses undergo mutations and can appear in different masks. According to these results, it was predicted that supplementation with strong antioxidant substances may have a protective effect in diagnosed COVID-19 patients. The levels of these biomolecules can guide future patient-targeted therapies in clinical practice.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
The studies involving human participants were reviewed and approved by the study was approved by the Mehmet Ali Aydinlar University Faculty of Medicine Ethics Committee and informed consent was obtained from all participants (ATADEK 2020/17). The patients/participants provided their written informed consent to participate in this study.
PU and HU participated in the design of the study and wrote the manuscript. PU and ÇC collected and determined the patients. AY, SD, RG, and HU carried out the ELISA test. SD performed the statistical analysis. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ALA, Alpha lipoic acid; ARDS, Acute respiratory distress syndrome; ASC, Apoptosis-associated speck-like protein containing a caspase recruitment domains; CRP, C-reactive protein; CVD, Cardiovascular diseases; DBP, Diastolic blood pressure; DM, Diabetes mellitus; GSH, Glutathione; HDL, High density lipoprotein; ICAM-1, Intracellular adhesion molecule-1; IFN-V, Interferon-V; IL-1β, Interleukin-1 beta; LOX-1, Lectin-like oxidized-LDL receptor-1; MAPK, Mitogen activated protein kinase; MCP1, Monocyte chemotactic protein-1; MS, Metabolic syndrome; NAC, N-acetyl-cysteine; NF-κB, Nuclear factor kappa B; oxLDL, Oxidized low density lipoprotein; oxLIC, oxLDL immune complex; ROC, Receiver operating characteristic; ROS, Reactive oxygen species; RT-PCR, Reverse transcription polymerase chain reaction; SBP, Systolic blood pressure; SMC, Smooth muscle cells; SO2, Oxygen saturation; SPSS, Statistical product and service solutions; TGF-β, Transforming growth factor beta; VCAM-1, Vascular cell adhesion molecule-1.
1. Sarangi, MK, Padhi, S, Dheeman, S, Karn, SK, Patel, LD, Yi, DK, et al. Diagnosis, prevention, and treatment of coronavirus disease: a review. Expert Rev Anti-Infect Ther. (2022) 20:243–66. doi: 10.1080/14787210.2021.1944103
2. Chen, JM. Novel statistics predict the COVID-19 pandemic could terminate in 2022. J Med Virol. (2022) 94:2845–8. doi: 10.1002/jmv.27661
3. Kim, HJ, Yuan, J, Norris, K, and Vaziri, ND. High-calorie diet partially ameliorates dysregulation of intrarenal lipid metabolism in remnant kidney. J Nutr Biochem. (2010) 21:999–1007. doi: 10.1016/j.jnutbio.2009.08.006
4. Schreurs, MP, and Cipolla, MJ. Cerebrovascular dysfunction and blood-brain barrier permeability induced by oxidized LDL are prevented by apocynin and magnesium sulfate in female rats. J Cardiovasc Pharmacol. (2014) 63:33–9. doi: 10.1097/FJC.0000000000000021
5. Oteiza, A, Li, R, McCuskey, RS, Smedsrød, B, and Sørensen, KK. Effects of oxidized low-density lipoproteins on the hepatic microvasculature. Am J Physiol Gastrointest Liver Physiol. (2011) 301:G684–93. doi: 10.1152/ajpgi.00347.2010
6 Maiolino, G, Rossitto, G, Caielli, P, Bisogni, V, Rossi, GP, and Calò, LA. The role of oxidized low-density lipoproteins in atherosclerosis: the myths and the facts. Mediat Inflamm. (2013) 2013:1–13. doi: 10.1155/2013/714653
7. Pirillo, A, Norata, GD, and Catapano, AL. LOX-1, OxLDL, and atherosclerosis. Mediat Inflamm. (2013) 2013:1–12. doi: 10.1155/2013/152786
8. Levitan, I, and Shentu, TP. Impact of oxLDL on cholesterol-rich membrane rafts. J Lipids. (2011) 2011:1–11. doi: 10.1155/2011/730209
9. Hu, X, Chen, D, Wu, L, He, G, and Ye, W. (2020). Low Serum Cholesterol Level among Patients with COVID-19 Infection in Wenzhou, China. Available at: https://ssrn.com/abstract=3544826 (Accessed June 10, 2022).
10. Zhong, X, Chen, B, Yang, L, and Yang, Z. Molecular and physiological roles of the adaptor protein CARD9 in immunity. Cell Death Dis. (2018) 9:52. doi: 10.1038/s41419-017-0084-6
11. Fang, Y, Zhang, H, Xie, J, Lin, M, Ying, L, Pang, P, et al. Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology. (2020) 296:E115–7. doi: 10.1148/radiol.2020200432
12. Yoshimoto, R, Fujita, Y, Kakino, A, Iwamoto, S, Takaya, T, and Sawamura, T. The discovery of LOX-1, its ligands and clinical significance. Cardiovasc Drugs Ther. (2011) 25:379–91. doi: 10.1007/s10557-011-6324-6
13. Xu, S, Ogura, S, Chen, J, Little, PJ, Moss, J, and Liu, P. LOX-1 in atherosclerosis: biological functions and pharmacological modifiers. Cell Mol Life Sci. (2013) 70:2859–72. doi: 10.1007/s00018-012-1194-z
14. Navarra, T, Del Turco, S, Berti, S, and Basta, G. The lectin-like oxidized low-density lipoprotein receptor-1 and its soluble form: cardiovascular implications. J Atheroscler Thromb. (2010) 17:317–31. doi: 10.5551/jat.3228
15. Poeck, H, Bscheider, M, Gross, O, Finger, K, Roth, S, Rebsamen, M, et al. Recognition of RNA virus by RIG-I results in activation of CARD9 and inflammasome signaling for interleukin 1 beta production. Nat Immunol. (2010) 11:63–9. doi: 10.1038/ni.1824
16. DeDiego, ML, Nieto-Torres, JL, Regla-Nava, JA, Jimenez-Guardeño, JM, Fernandez-Delgado, R, Fett, C, et al. Inhibition of NF-κB-mediated inflammation in severe acute respiratory syndrome coronavirus-infected mice increases survival. J Virol. (2014) 88:913–24. doi: 10.1128/JVI.02576-13
17. Horowitz, RI, Freeman, PR, and Bruzzese, J. Efficacy of glutathione therapy in relieving dyspnea associated with COVID-19 pneumonia: a report of 2 cases. Respir Med Case Rep. (2020) 30:101063. doi: 10.1016/j.rmcr.2020.101063
18. Wei, X, Zeng, W, Su, J, Wan, H, Yu, X, Cao, X, et al. Hypolipidemia is associated with the severity of COVID-19. J Clin Lipidol. (2020) 14:297–304. doi: 10.1016/j.jacl.2020.04.008
19. Zidar, DA, Juchnowski, S, Ferrari, B, Clagett, B, Pilch-Cooper, HA, Rose, S, et al. Oxidized LDL levels are increased in HIV infection and may drive monocyte activation. J Acquir Immune Defic Syndr. (2015) 69:154–60. doi: 10.1097/QAI.0000000000000566
20. Pincemail, J, Cavalier, E, Charlier, C, Cheramy-Bien, JP, Brevers, E, Courtois, A, et al. Oxidative stress status in COVID-19 patients hospitalized in intensive care unit for severe pneumonia. A pilot study. Antioxidants (Basel). (2021) 10:257. doi: 10.3390/antiox10020257
21. Avila-Nava, A, Pech-Aguilar, AG, Lugo, R, Medina-Vera, I, Guevara-Cruz, M, and Gutiérrez-Solis, AL. Oxidative stress biomarkers and their association with mortality among patients infected with SARS-CoV-2 in Mexico. Oxidative Med Cell Longev. (2022) 2022:1–8. doi: 10.1155/2022/1058813
22. Delgado-Roche, L, and Mesta, F. Oxidative stress as key player in severe acute respiratory syndrome coronavirus (SARS-CoV) infection. Arch Med Res. (2020) 51:384–7. doi: 10.1016/j.arcmed.2020.04.019
23. Mehri, F, Rahbar, AH, Ghane, ET, Souri, B, and Esfahani, M. Changes in oxidative markers in COVID-19 patients. Arch Med Res. (2021) 52:843–9. doi: 10.1016/j.arcmed.2021.06.004
24. Gadotti, AC, Lipinski, AL, Vasconcellos, FT, Marqueze, LF, Cunha, EB, Campos, AC, et al. Susceptibility of the patients infected with Sars-Cov2 to oxidative stress and possible interplay with severity of the disease. Free Radic Biol Med. (2021) 165:184–90. doi: 10.1016/j.freeradbiomed.2021.01.044
25. Spencer, E, Rosengrave, P, Williman, J, Shaw, G, and Carr, AC. Circulating protein carbonyls are specifically elevated in critically ill patients with pneumonia relative to other sources of sepsis. Free Radic Biol Med. (2022) 179:208–12. doi: 10.1016/j.freeradbiomed.2021.11.029
26. Jain, SK, Parsanathan, R, Levine, SN, Bocchini, JA, Holick, MF, and Vanchiere, JA. The potential link between inherited G6PD deficiency, oxidative stress, and vitamin D deficiency and the racial inequities in mortality associated with COVID-19. Free Radic Biol Med. (2020) 161:84–91. doi: 10.1016/j.freeradbiomed.2020.10.002
27. Anwar, S, Almatroudi, A, Allemailem, KS, Jacob Joseph, R, Khan, AA, and Rahmani, AH. Protective effects of ginger extract against Glycation and oxidative stress-induced health complications: an in vitro study. PRO. (2020) 8:468. doi: 10.3390/pr8040468
28. Mrityunjaya, M, Pavithra, V, Neelam, R, Janhavi, P, Halami, PM, and Ravindra, PV. Immune-boosting, antioxidant and anti-inflammatory food supplements targeting pathogenesis of COVID-19. Front Immunol. (2020) 11:570122. doi: 10.3389/fimmu.2020.570122
29. Suhail, S, Zajac, J, Fossum, C, Lowater, H, McCracken, C, Severson, N, et al. Role of oxidative stress on SARS-CoV (SARS) and SARS-CoV-2 (COVID-19) infection: a review. Protein J. (2020) 39:644–56. doi: 10.1007/s10930-020-09935-8
30. Loffredo, L, and Violi, F. COVID-19 and cardiovascular injury: a role for oxidative stress and antioxidant treatment? Int J Cardiol. (2020) 312:136. doi: 10.1016/j.ijcard.2020.04.066
31. de Las, HN, Martín Giménez, VM, Ferder, L, Manucha, W, and Lahera, V. Implications of oxidative stress and potential role of mitochondrial dysfunction in COVID-19: therapeutic effects of vitamin D. Antioxidants (Basel). (2020) 9:897. doi: 10.3390/antiox9090897
32. De Flora, S, Balansky, R, and La Maestra, S. Rationale for the use of N-acetylcysteine in both prevention and adjuvant therapy of COVID-19. FASEB J. (2020) 34:13185–93. doi: 10.1096/fj.202001807
33. Martín Giménez, VM, Inserra, F, Tajer, CD, Mariani, J, Ferder, L, Reiter, RJ, et al. Lungs as target of COVID-19 infection: protective common molecular mechanisms of vitamin D and melatonin as a new potential synergistic treatment. Life Sci. (2020) 254:117808. doi: 10.1016/j.lfs.2020.117808
34. Beltrán-García, J, Osca-Verdegal, R, Pallardó, FV, Ferreres, J, Rodríguez, M, Mulet, S, et al. Oxidative stress and inflammation in COVID-19-associated sepsis: the potential role of anti-oxidant therapy in avoiding disease progression. Antioxidants (Basel). (2020) 9:936. doi: 10.3390/antiox9100936
35. Ntyonga-Pono, MP. COVID-19 infection and oxidative stress: an under-explored approach for prevention and treatment? Pan Afr Med J. (2020) 35:12. doi: 10.11604/pamj.2020.35.2.22877
36. Polonikov, A. Endogenous deficiency of glutathione as the Most likely cause of serious manifestations and death in COVID-19 patients. ACS Infect Dis. (2020) 6:1558–62. doi: 10.1021/acsinfecdis.0c00288
37. Qin, M, Cao, Z, Wen, J, Yu, Q, Liu, C, Wang, F, et al. An antioxidant enzyme therapeutic for COVID-19. Adv Mater. (2020) 32:e2004901. doi: 10.1002/adma.202004901
38. Trujillo-Mayol, I, Guerra-Valle, M, Casas-Forero, N, Sobral, MMC, Viegas, O, Alarcón-Enos, J, et al. Western dietary pattern antioxidant intakes and oxidative stress: importance during the SARS-CoV-2/COVID-19 pandemic. Adv Nutr. (2021) 12:670–81. doi: 10.1093/advances/nmaa171
39. Soto, ME, Guarner-Lans, V, Soria-Castro, E, Manzano Pech, L, and Pérez-Torres, I. Is antioxidant therapy a useful complementary measure for Covid-19 treatment? An algorithm for its application. Medicina (Kaunas). (2020) 56:386. doi: 10.3390/medicina56080386
40. Shneider, A, Kudriavtsev, A, and Vakhrusheva, A. Can melatonin reduce the severity of COVID-19 pandemic? Int Rev Immunol. (2020) 39:153–62. doi: 10.1080/08830185.2020.1756284
41. Poe, FL, and Corn, J. N-Acetylcysteine: a potential therapeutic agent for SARS-CoV-2. Med Hypotheses. (2020) 143:109862. doi: 10.1016/j.mehy.2020.109862
42. El-Missiry, MA, El-Missiry, ZMA, and Othman, AI. Melatonin is a potential adjuvant to improve clinical outcomes in individuals with obesity and diabetes with coexistence of Covid-19. Eur J Pharmacol. (2020) 882:173329. doi: 10.1016/j.ejphar.2020.173329
43. Lammi, C, and Arnoldi, A. Food-derived antioxidants and COVID-19. J Food Biochem. (2021) 45:e13557. doi: 10.1111/jfbc.13557
44. Jorge-Aarón, RM, and Rosa-Ester, MP. N-acetylcysteine as a potential treatment for COVID-19. Future Microbiol. (2020) 15:959–62. doi: 10.2217/fmb-2020-0074
45. Wang, JZ, Zhang, RY, and Bai, J. An anti-oxidative therapy for ameliorating cardiac injuries of critically ill COVID-19-infected patients. Int J Cardiol. (2020) 312:137–8. doi: 10.1016/j.ijcard.2020.04.009
46. Guloyan, V, Oganesian, B, Baghdasaryan, N, Yeh, C, Singh, M, Guilford, F, et al. Glutathione supplementation as an adjunctive therapy in COVID-19. Antioxidants (Basel). (2020) 9:914. doi: 10.3390/antiox9100914
47. Sies, H, and Parnham, MJ. Potential therapeutic use of ebselen for COVID-19 and other respiratory viral infections. Free Radic Biol Med. (2020) 156:107–12. doi: 10.1016/j.freeradbiomed.2020.06.032
48. Xie, X, Zhong, Z, Zhao, W, Zheng, C, Wang, F, and Liu, J. Chest CT for typical coronavirus disease 2019 (COVID-19) pneumonia: relationship to negative RT-PCR testing. Radiology. (2020) 296:E41–5. doi: 10.1148/radiol.2020200343
49. Luraschi, R, Barrera-Avalos, C, Vallejos-Vidal, E, Alarcón, J, Mella-Torres, A, Hernández, F, et al. The comparative analysis of two RT-qPCR kits for detecting SARS-CoV-2 reveals a higher risk of false-negative diagnosis in samples with high quantification cycles for viral and internal genes. Can J Infect Dis Med Microbiol. (2022) 2022:1–10. doi: 10.1155/2022/2594564
Keywords: COVID-19, nuclear factor kappa B, lipid metabolism, oxidized LDL, lectin-like oxidized-LDL receptor-1
Citation: Uysal P, Yüksel A, Durmus S, Cuhadaroglu Ç, Gelisgen R and Uzun H (2023) Can circulating oxidative stress-related biomarkers be used as an early prognostic marker for COVID-19? Front. Med. 10:1041115. doi: 10.3389/fmed.2023.1041115
Received: 10 September 2022; Accepted: 18 January 2023;
Published: 09 February 2023.
Edited by:
Reza Lashgari, Shahid Beheshti University, IranReviewed by:
Talat Kilic, İnönü University, TürkiyeCopyright © 2023 Uysal, Yüksel, Durmus, Cuhadaroglu, Gelisgen and Uzun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hafize Uzun, ✉ aHV6dW41OUBob3RtYWlsLmNvbQ==,
†ORCID: Hafize Uzun https://orcid.org/0000-0002-1347-8498
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.