
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Med., 15 September 2022
Sec. Healthcare Professions Education
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.975229
This article is part of the Research TopicReviews in Healthcare Professions EducationView all 6 articles
The BOPPPS teaching strategy has been used recently in many medical courses as an improved and more practical pedagogy in China. Nevertheless, the effectiveness of this pedagogy has not been fully assessed in terms of knowledge and skill outcomes in medical education. This meta-analysis aimed to evaluate the effectiveness of the BOPPPS strategy compared with traditional lecture-based learning (LBL) in Chinese medical education. The English electronic databases of Web of Science, PubMed, Embase, and the Cochrane Library and the Chinese electronic databases of CNKI, CQVIP, Wanfang, and CBM were used to search the publications related to the BOPPPS teaching strategy before 6 Jun 2022. Eligibility publications were retrieved and the data were extracted by two researchers independently according to the predefined inclusion and exclusion criteria. Quality analysis was performed using the Cochrane risk-of-bias tool, and the meta-analysis was performed using RevMan 5.3 and StataSE. We retrieved 367 records and 41 studies with a total of 5,042 medical students in the meta-analysis, which included 34 randomized controlled trials (RCTs) and 7 Cohort studies. In the cumulative meta-analysis, BOPPPS strategy significantly increased skill scores (SS) (SMD: 1.15, 95% CI: 1.00–1.30, P < 0.00001), knowledge examination scores (KES) (SMD: 1.56, 95% CI: 1.24–1.89, P < 0.00001), comprehensive ability scores (CAS) (SMD: 1.22, 95%CI: 0.85–1.59; P < 0.00001), and teaching satisfaction (TS) (OR: 3.64; 95%CI: 2.97–4.46; P < 0.0001) compared to the LBL model among those medical students. Statistically similar results were obtained in the sensitivity analysis. These results showed that the BOPPPS method is an effective teaching strategy for Chinese medical students to improve SS, knowledge scores, CAS, and TS when compared with LBL in medical education. Because of the limited quantity and quality of the included studies, further rigorous studies are needed to conclude with more confidence.
The BOPPPS teaching strategy was first proposed by Douglas Kerrin from the University of British Columbia in 1978 (1), which divides into six distinct steps: bridge-in (B), objective (O), pre-assessment (P), participatory learning (P), post-assessment (P), and summary (S), i.e., BOPPPS. Based on the constructivism learning theory, the BOPPPS teaching strategy constructs a complete framework and process for the achievement of teaching objectives (2). The flowchart of class design for the BOPPPS strategy compared to lecture-based learning (LBL) was attached in Supplementary Appendix 1.
In Chinese universities, the BOPPPS teaching strategy was firstly attempted in 2011 for the improvement of teaching effectiveness and comprehensive ability in learning plant ecology for postgraduates (3), classroom teaching quality of English courses (4), and academic performance of medical cell biology course for graduates compared with the traditional instructions (5). Recently, it has been developed and extensively trialed in China’s higher medical education to increase the efficiency of education and learning processes due to a clear organizing teaching process and to convert students into active learners (6, 7).
Traditionally, the instructor is the center of the class teaching with a full lecture in the classroom, which may inhibit the learning initiative and enthusiasm of students, and consequently, their interaction and active learning are limited with the passive receiving the knowledge (7, 8). For the BOPPPS teaching strategy, it forms a systematic, coherent, and operational six-step of teaching, which could help instructors in disassembling and analyzing teaching activities to improve the teaching process (8). According to the closed-loop teaching six-step, the instructional content could be conveniently designed, and the instructional process could be evaluated and revised by instructors. The BOPPPS teaching strategy further focuses on the participation of students, interaction, and feedback ability and strengthens the closed-loop teaching unit. Compared with LBL, the core objects of the BOPPPS strategy is a learner-centered teaching activity in which learners participate in discussing the content with peers or mentors during class, self-assessment of learning effects, and objectives after class (9). Particularly during the participatory learning phase, students can participate in various active learning activities such as problem-discussion and immediate feedback which emphasizes full interaction between classmates and/or teachers to stimulate Students’ enthusiasm and interest for the improvement of self-efficacy, knowledge, and communication ability (2).
For the past 10 years, the BOPPPS teaching strategy has been used in teaching many medical subjects, covering nearly all medical disciplines such as internal medicine, surgery, pathology, physiology, healthcare, management education, etc. in China (10). There has been a beneficial shift in academic accomplishment levels in medical disciplines education, with an increase in interest in the BOPPPS teaching strategy. Increased research has been published on BOPPPS in Chinese medical education over the last decade. Various studies on the effectiveness of BOPPPS in medical education have been conducted. These studies reported positive effects on the development of Student’s skills and knowledge, and the improvement of self-learning ability, academic performance, and learning satisfaction, as compared to the control group that received traditional LBL instruction.
Nevertheless, the outcomes of the BOPPPS teaching strategy on medical education have been ambiguous or inconsistent in China. Most studies have a small sample size, and few have used quantitative synthesis in the evaluation of the effectiveness of the BOPPPS teaching strategy. It is possible and valuable to conduct a quantitative synthesis of the data using rigorous methods. This meta-analysis aimed to evaluate the overall effectiveness of the BOPPPS teaching strategy compared to LBL teaching in China’s higher medical education, which included final knowledge examination score (KES), skill score (SS), comprehensive ability score (CAS), and teaching satisfaction (TS).
This meta-analysis and systematic review were designed according to the PRISMA (preferred reporting items for systematic reviews and meta-analyses, PRISMA) guidelines (11). The checklist included items deemed essential for transparent reporting of a systematic review. The PRISMA Checklist was attached in Supplementary Appendix 2.
The PICOS (population, intervention, comparison, outcome, and study design) framework was used to determine the inclusion criteria of studies. The following studies will be included: (a) the participants for the studies were medical students in Chinese medical schools; (b) the experimental group received the intervention of BOPPPS teaching strategy; (c) the groups of LBL were as control; (d) the core curriculums covered clinical medicine and/or biomedicine disciplines; (e) the studies were two-group controlled (randomized/non-randomized); (f) the outcomes presented as data or descriptions of each controlled studies included at least one of the following measurements: SS, KES, CAS, TS; (g) only studies full-text published in English language and Chinese language were included; (f) all above-mentioned studies conducted before 6 Jun 2022.
Any study which did not meet the aforementioned inclusion criteria was excluded. The following studies will be excluded: (a) the participants of non-clinical medicine students (e.g., dental, nursing, pharmacy, or any allied health profession) in Chinese medical schools; (b) incomplete the six-stage of BOPPPS teaching strategy in the experimental group; (c) reviews, editorials, conference papers, case reports; (d) duplicate studies or overlapping participants; (e) insufficient data to calculate the outcomes and/or not report a quantitative outcome for the effectiveness; (f) non-English language and non-Chinese language studies.
PubMed, Web of Science, Embase, and Cochrane Library were searched without any restrictions before 6 Jun 2022. Asterisks were used as a truncation symbol for searching. English key search terms included BOPPPS (bridge, objective, pre-assessment, participatory, post-assessment, summary) and student*. Chinese electronic databases of CNKI, Wanfang, CQVIP, and CBM were searched before 6 Jun 2022. Chinese key search terms included BOPPPS and medicine and student. The specific set of MeSH terms or title or keywords or abstract was used to search the English databases, and the topic or title or keywords or abstract was used to search the Chinese databases. The retrieved strategy of studies from databases was shown in Supplementary Appendix 3.
According to a predefined form, data were searched, collected, and extracted by two independent reviewers (K. Xu and J. Wang). From each study, the following information was extracted: the surname of the first author, year of publication, student characteristics and sample size of the participants, course name, intervention methods, and outcome measures. Any disagreements between these two reviewers on the eligibility of the extracted data were resolved through discussion with a third research team member (X. Ma) until an agreement was reached.
In this meta-analysis, the primary outcomes were the final KES, SS, and CAS in the BOPPPS group and the control group. The TS was a secondary outcome. Subgroup analyses of study design, hometown, training levels (undergraduates and graduates), course type (theory and practice), and course contents were conducted to find out a potential source of heterogeneity in the above outcomes.
The Cochrane risk of bias 2 (RoB2 v9) tool was used to evaluate the quality of individual included studies (12). Evaluation criteria included the following five domains and overall bias: randomization process, deviation from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result. Funnel plots were used to evaluate publication bias. During the assessment process, two reviewers (K. Xu and J. Wang) independently conducted the risk of bias. Disagreements would be resolved through consensus or the involvement of a third reviewer (D. Zeng). According to the Cochrane risk of bias instructions, the risk of bias for each study was rated as high, with some concerns, and low risk. For any single outcome, studies with a high risk of overall bias were excluded from the meta-analysis.
Statistical analysis of heterogeneity and the meta-analysis for effectiveness outcomes were performed using the Review Manager (RevMan) software (V.5.3, the Cochrane Collaboration, UK). Galbraith plot analysis of heterogeneity was carried out using the StataSE software (version 14, StataCorp LP USA). For the continuous data including SS, KES, and CAS, the effect sizes were estimated with the standardized mean difference (SMD) and its 95% confidence intervals (CI). The odds ratio (OR) and 95%CI were calculated to estimate the dichotomous data such as TS. Publication bias was examined independently in funnel plots (13). The Z-test was used for overall effect and the Chi-square test for multiple subgroups comparison was performed to evaluate the subgroup’s result differences, and P < 0.05 was considered statistically significant (14). Heterogeneity among included studies was evaluated with the inconsistency (I2) metric (15). Degrees of statistical heterogeneity were low (I2<30%), moderate (I2 = 30–50%), and high (I2>50%), respectively. If I2 was < 50%, the fixed-effects model was used, which represents low to moderate heterogeneity or no statistical heterogeneity among the studies. Otherwise, the random effect model was used for analysis (I2 ≥ 50%) (16).
The methodological flowchart of PRISMA was shown in Figure 1. A total of 367 potentially relevant records were firstly retrieved from the electronic database, and a total of 210 duplicate records were excluded. According to the title and abstract, 95 publications were then excluded because some were irrelevant to the subject of the meta-analysis such as nursing, stomatology, pharmacy, and others were experience summaries or questionnaire surveys without quantitative measurement of the scores. After reading the full text, another 20 articles were excluded since some were insufficient data to be extracted (n = 14), and/or trials without controls (n = 6). Eventually, 41 RCTs were included in this meta-analysis based on the inclusion criteria.
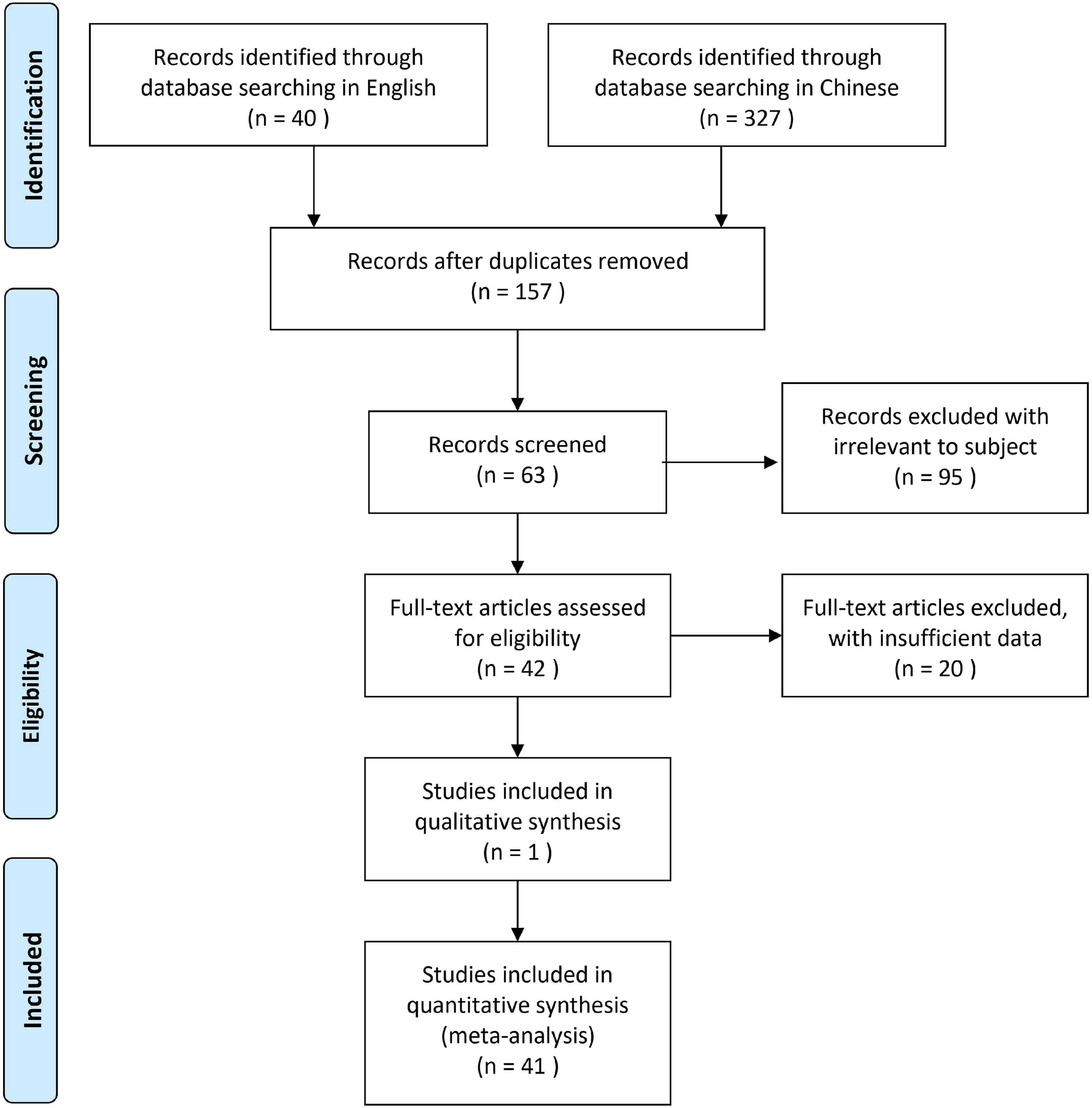
Figure 1. The methodological flowchart of PRISMA for the selection of the included studies in this meta-analysis.
The basic characteristics of the 41 studies were presented in Table 1. All of the studies that were included concerning medical curriculum education for students of MBBS (Bachelor of medicine and bachelor of surgery). The years of the publications were before 6 Jun 2022. A total of 2,305 medical students participated in the BOPPPS teaching strategy and 2,737 medical students in the LBL, which were included in the 41 studies (17–57). All of the students in included studies were from medical school. Out of these 41 articles, only one was published in English, and forty were published in Chinese. There were 34 randomized controlled trials (RCTs), and 7 Cohort studies compared with the previous year’s Students’ scores.
There were 21 trials on theoretical courses and 20 trials on practical courses. There were 34 trials related to undergraduates of clinical medicine and 7 trials on university graduates with standardized clinical training in hospitals. In addition, the curriculums for medical students included 5 studies for basic medicine courses, 5 studies for traditional Chinese medicine (TCM) courses, and 31 studies for clinical medicine courses (Table 1). The trial curriculums in the included studies had 9 studies on the knowledge of internal medicine (6, 8, 13, 23, 25, 30, 31, 38), 6 studies on surgery (7, 9, 19, 22, 28, 39), 5 studies on TCM (1, 15, 17, 32, 35), 5 studies on clinical diagnostics (3, 11, 14, 24, 41), 4 studies on obstetrics and gynecology (12, 33, 36, 37), 2 studies on anesthesiology (24, 33), 2 studies on human anatomy (4, 34), 2 studies on pathology (2, 26), 2 studies on pediatrics (16, 27), 1 studies on emergency medicine (10), 1 studies on evidence-based medicine (20), 1 studies on general medicine (5), and 1 studies on physiology (18).
According to the instructions in the Cochrane Collaboration Handbook (12), the assessment for each outcome included the five domain ratings plus the overall judgment. According to five domain ratings, the overall bias of each included study was considered as “low risk of bias.” All the included studies reported their outcome data and therefore the majority (n = 37, 90.2%) had low attrition bias, four studies (9.8%) had some unclear risk of bias due to insufficient information on allocation and outcome data, and the majority of included studies were of high quality in Figure 2 for overall assessment and in Supplementary Appendix 4 for each included study. Then, the shape of the funnel plot of KES, SS, CAS, and TS was nearly symmetrical, indicating negligible evidence of significant publication bias (Figures 3A–D).
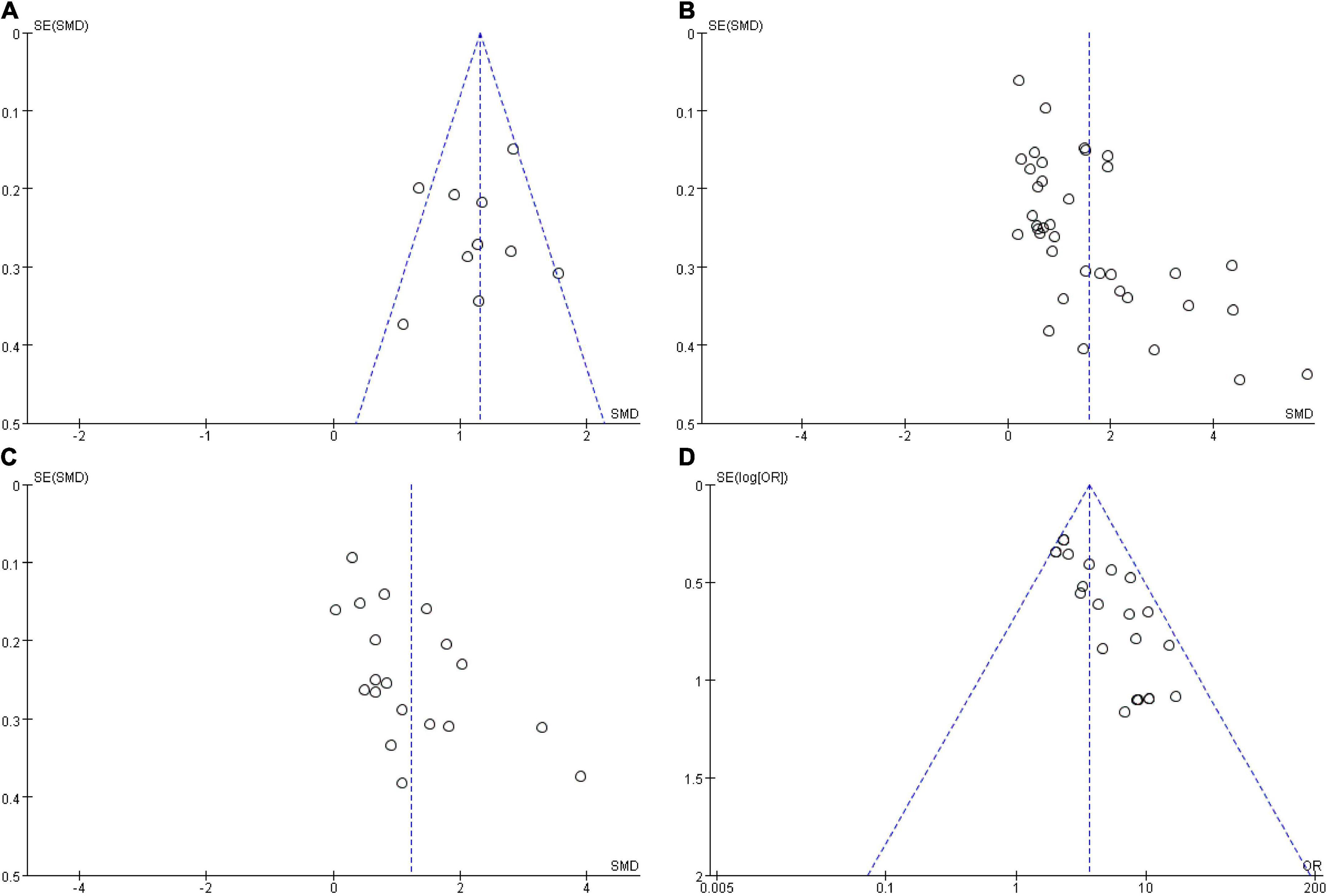
Figure 3. Funnel plots for publication bias. (A) Publication bias of skill scores; (B) publication bias of knowledge examination scores; (C) publication bias of comprehensive ability scores; (D) publication bias of teaching effect satisfactory. OR, odds ratio; SMD, standardized mean difference.
There were 10 included studies data related to the SS evaluation with 429 and 424 students in the BOPPPS and LBL groups, respectively. Compared with the LBL teaching, the pooled effect of 10 studies (SMD 1.15, 95% CI: 1.00–1.30, Z = 15.43, P < 0.00001) showed a significant improving effect on SS in the group of BOPPPS. The fixed-effects model was used for the meta-analysis because of the moderate heterogeneity (P = 0.04, I2 = 49% < 50%) of the data (Figure 4).
There were 37 included studies data related to the final KES evaluation with 2,568 and 2,481 students in the BOPPPS and LBL groups, respectively. The pooled effect of those studies (SMD 1.56, 95% CI: 1.24–1.89, Z = 9.94, P < 0.00001) showed that knowledge scores improved significantly in BOPPPS teaching strategy with a large effect compared to LBL teaching. The random-effects model was used for the meta-analysis because of the significant statistical heterogeneity (P < 0.00001, I2 = 96% > 50%) among studies (Figure 5).
There were 19 included studies data related to the CAS evaluation with 1,141 and 1,104 students in the BOPPPS and LBL groups, respectively. In this meta-analysis, the CAS by a mean of 1.22 were significantly improved in the BOPPPS teaching strategy group compared with that of the traditional LBL model (95%CI: 0.85–1.59; P < 0.00001). The random-effects model was used for the meta-analysis because of the significant statistical heterogeneity (P < 0.00001, I2 = 94%) of the data (Figure 6).
There were 23 included studies data related to the satisfaction evaluation with 1,197 and 1,198 students in the BOPPPS and LBL groups, respectively. The meta-analysis in the BOPPPS group found a significantly higher odds ratio in TS compared with that of the LBL teaching (OR: 3.64; 95%CI: 2.97–4.46; P < 0.0001). The fixed-effects model was used for the meta-analysis because of the lower heterogeneity (P = 0.15, I2 = 24%) of the data (Figure 7).
Galbraith plot of heterogeneity was shown in Figure 8 and the subgroup analysis was shown in Table 2 for KES and Table 3 for CAS (in Supplementary Appendixes 5, 6). Among subgroups aspects, we found differences regarding the efficiency of BOPPPS in the subgroups of attempted discipline contents and students training levels. The subgroup analysis demonstrated significant differences in the effects of BOPPPS on KES domain when comparing undergraduates and university graduates (P < 0.0001). The outcome revealed that there was a larger effect size (SMD 1.75, 95% CI 1.35–2.15) for undergraduates than that for university graduates (SMD 0.80, 95% CI 0.55–1.05). In addition, subgroup analysis of course contents showed that there were significant differences in the effects of BOPPPS on KES and CAS among 13 courses. The outcome demonstrated that the BOPPPS strategy was significantly superior to traditional LBL teaching in the courses teaching of pathology (SMD 3.13, 95% CI 0.77–5.50) and internal medicine (SMD 2.01, 95% CI 1.19–2.84).
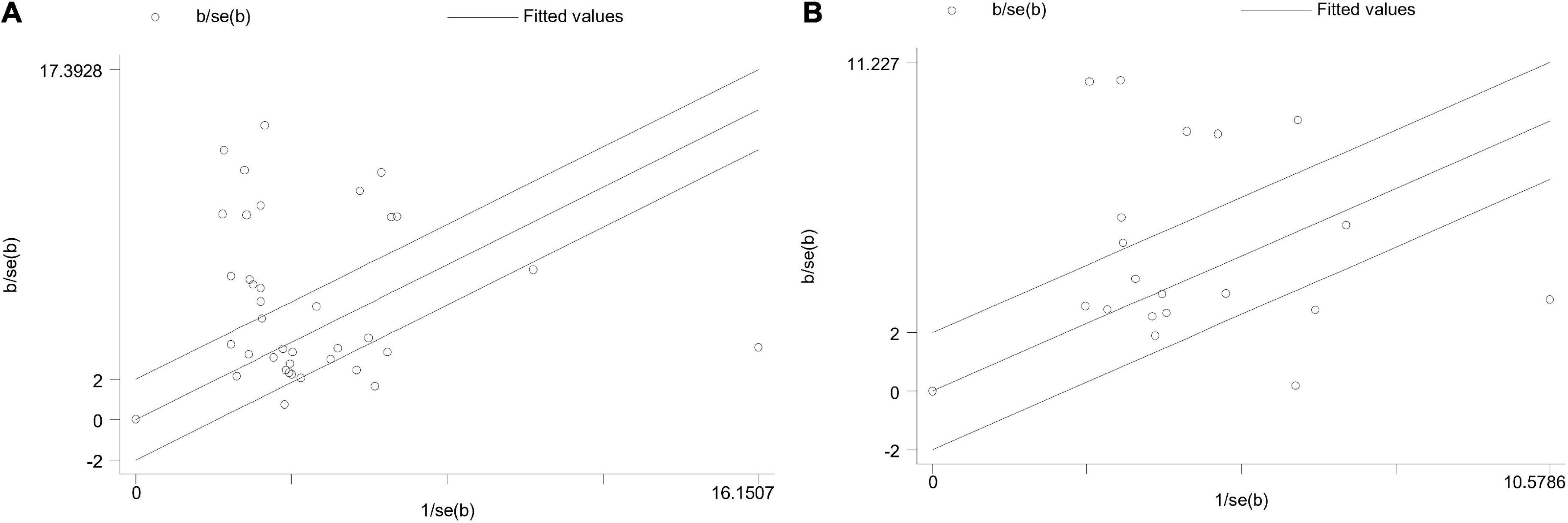
Figure 8. Galbraith plot analysis of heterogeneity. (A) Galbraith plot of knowledge examination scores; (B) Galbraith plot of comprehensive ability scores.
A sensitivity analysis was performed to investigate the influence of each study on the overall meta-analysis summary estimate in Supplementary Appendix 7. Statistically similar results were obtained, which suggested the stability of this meta-analysis.
The greatest challenge for China medical schools is the training of qualified clinicians, which can both adapt to the hospital environment with rapidly changing and meet the needs of the Chinese people. Although the fact that the BOPPPS teaching strategy has been widely embraced in education systems around the world, its implementation in China is still in its infancy. Compared with lecture-based instruction, the BOPPPS teaching strategy is not a routine pedagogy in China medical education. Many factors such as medical education systems or cultural backgrounds maybe influence the selection of the BOPPPS teaching strategy. Firstly, the traditional teacher centered model has been dominating the Chinese medical education system. For both students and teachers, the traditional teaching model has almost formed prescribed educational experiences. Secondly, the lack of a high-quality and energetic teaching team is one of the important factors hindering the successful implementation of the BOPPPS teaching strategy. Thirdly, medical curriculum standards and education levels vary dramatically among different schools in China. Therefore, there is an urgent need to carry out a large number of educational reformations and rearrangements to successfully improve the Chinese medical education system.
We take into account the fact that the education systems, backgrounds of culture, history, and philosophy in China are distinct from those in western countries (58). To evaluate the potential effectiveness and differences in quantitative outcomes of the BOPPPS teaching strategy compared to the LBL teaching method in China, the target population in the current meta-analysis should be limited to medical students in Chinese medical schools.
In the study, 41 studies relevant to inclusion criteria were identified and demonstrated significant improvement with the BOPPPS teaching strategy in learning outcomes compared to traditional instructions. We analyzed the effectiveness of the BOPPPS teaching strategy in comparison with traditional lecture-based instruction using a meta-analysis to obtain a positive conclusion, which is the first meta-analysis providing comprehensive insights into the efficiency of the BOPPPS teaching strategy in Chinese medical education.
The meta-analysis results of the effectiveness indicator showed that when compared with the LBL group, the SS, KES, CAS, and TS of the BOPPPS group were higher, suggesting that the BOPPPS teaching strategy could stimulate the enthusiasm and interest of medical students, boost Students’ skills and intrinsic motivation in learning; and improve the self-directed learning ability, academic performance (6, 59). On the other hand, the BOPPPS teaching strategy with a six-phase framework was adapted to organize and accelerate the teaching cycle as a whole including goal, behavior, learning activity, and evaluation (60), which help teachers generate innovative teaching ideas and timely adjustment of teaching schedule. Besides, numerous knowledge points covered in medical education, the LBL methods do not encourage problem-solving and learning activities (61). The results of the meta-analysis showed that the students in the BOPPPS group demonstrated better mastery of the knowledge and greater active self-learning and comprehensive ability.
The pooled effect size of KES (SMD 1.56, 95% CI: 1.24–1.89), CAS (SMD 1.22, 95%CI: 0.85–1.59), SS (SMD 1.15, 95% CI: 1.00–1.30), and TS (OR: 3.64; 95%CI: 2.97–4.46) showed that BOPPPS learning remained more effective than traditional LBL learning. There are several possible explanations for this meta-analysis results. First, compared to traditional learning, the BOPPPS learning allowed students to review pre-assessment, post-assessment, and other materials as often as necessary, and this likely enhanced comprehensive ability and learning performance. Second, the BOPPPS teaching is a novelty model for Chinese medical students, and has greatly stimulated their interest and intrinsic motivation in subject learning. Students in the BOPPPS group appeared to be more proactive in course learning, which led them to obtain higher KES and TS. Third, although most Chinese medical schools use unified textbooks and syllabuses for all students, students in the BOPPPS group with definite learning objectives are more likely to get higher knowledge scores compared to the LBL group. Hence, the superiority of the BOPPPS teaching strategy relative to the traditional LBL teaching could be more evident according to comprehensive ability and knowledge performance.
For the outcome indicators of KES and CAS, there is a large heterogeneity among the included studies. The random-effects model was applied in that meta-analysis. Subgroup analyses consistently demonstrated that the KES and CAS were significantly different in students training levels and course contents. Although the effectiveness of the BOPPPS teaching strategy is very complex, those subgroup analyses partially explained the differences. This subgroup analysis revealed that the level of students training and the course contents may be much important factors affecting the effectiveness of the BOPPPS teaching. The knowledge level of students was dramatically different between undergraduates and university graduates. The curriculum teaching with the BOPPPS strategy should be based on the sound fundamental knowledge background and learning interests of students. Because university graduates have finished multidisciplinary medical courses, their focuses and interests are clinical practice and operational skills. For the undergraduates who completed part of the medicine course in schools, their learning enthusiasms and interests were easier to be stimulated with the BOPPPS teaching strategy (10), and thus improvement of academic performance.
Unlike LBL, the BOPPPS teaching strategy is not a routine pedagogy in medical education in many countries. This teaching strategy has a helpful six-phase framework for designing learning activities and thus can be used to assist teachers in disassembling and analyzing the teaching process to improve Students’ learning outcomes in medical education (62). In recent years, the BOPPPS teaching strategy has been extensively trialed in China’s higher education for the improvement of efficiency in medical education (6, 7, 10). Particularly, the COVID-19 pandemic has greatly impacted the education sector and the way of teaching and learning (63). Online teaching has become an important part of teaching strategy and thus, incorporation of the BOPPPS into a combined offline and online teaching should also be tried.
To better apply the BOPPPS teaching strategy in Chinese medical education environments, the important elements of the BOPPPS strategy should be considered before the class. First, a high-quality and qualified teaching team is needs for the successful implementation of BOPPPS teaching strategy. Second, teachers should select an appropriate curriculum content, and design a feasible teaching program based on teaching experiences that could improve the knowledge and clinical skill without excessive heavy course load and time for medical students. Third, the teaching strategy of BOPPPS is a two-dimensional cooperative relationship, which includes the dominant relationships between peers, students, and teachers. Students should be encouraged to participate in multimodal activities such as problem-gathering and discussion, self-assessment, and active feedback for the improvement of self-efficacy. Fourth, according to the BOPPPS teaching six-step, internet online-offline assisted teaching tools should be used to increase the communication opportunities with teachers and decrease the burden on teachers in the teaching activities. In addition, because of different learning obstacles and learning style preferences among undergraduate and postgraduate medical students, it is necessary to use teaching modalities targeting the specific characteristics of those Chinese medical students (64, 65). Before the class of BOPPPS teaching, students learning obstacles and style preferences should be evaluated. Correspondingly, teachers should remodel the BOPPPS teaching six-step, containing additional bridging course contexts, and classroom components of participatory learning for the improvement of teaching effectiveness.
However, there were also several limitations in the present systematic review and meta-analysis. First, the systematic literature search encompassed four English databases (PubMed, Web of Science, Embase, and Cochrane Library) and four Chinese databases (CNKI, Wanfang, CQVIP, and CBM) with inclusion and exclusion criteria. Second, the meta-analysis quality was dependent on the data quality from the included studies, and the included literature quality was with a low overall bias of 90.2% studies, and none of them described the allocation concealment or blinding sources. Third, there was a large heterogeneity among the included studies regarding KES and CAS. Results of subgroup analyses should be interpreted with caution because of the diversity of influencing factors. Fourth, there were no standard guidelines for the application of BOPPPS in medical disciplines and no standard criteria for the effective evaluation of BOPPPS teaching strategy in China. In addition, in some of the included studies, questionnaire surveys as an additional measurement were used to assess the comprehensive ability of BOPPPS in medical education. Finally, the participants included Chinese medical students and the study compared the effects of the BOPPPS teaching strategy and LBL only. It also needs to evaluate and compare the effectiveness of BOPPPS with other teaching methods with Bayesian network meta-analysis in the future.
In conclusion, the current meta-analysis demonstrates that the BOPPPS teaching strategy is more effective than traditional LBL methods in medical education for enhancing the knowledge scores, SS, CAS, as well as improving TS among Chinese medical students. The BOPPPS teaching strategy appears to be superior to LBL teaching, and the use of this model may be optimal for improving Chinese medical education. Based on the limitations of this meta-analysis, we believe that high-quality studies with well-designed RCTs to assess the effectiveness of the BOPPPS teaching strategy are needed in the Chinese medical education system in the future.
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
XM performed the design and conceived the original idea. XM and DZ were responsible for the drafting of the manuscript. JW and KX were responsible for the literature search, data extraction, and statistical analysis. LL supervised the study and coordinated the teaching management. All authors have read and approved the final manuscript.
This work was supported by the Project for Excellent Talents in Xihua University (Grant No. 202026) and the Key Project for Education and Teaching Reform in Xihua University (Grant Nos. XJJG2021040 and XJJG2021096).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.975229/full#supplementary-material
1. Pattison P, Russell D. Instructional Skills Workshop Handbook. Vancouver, BC: UBC Centre for Teaching and Academic Growth (2006).
2. Ma X, Ma X, Li L, Luo X, Zhang H, Liu Y. Effect of blended learning with BOPPPS model on Chinese student outcomes and perceptions in an introduction course of health services management. Adv Physiol Educ. (2021) 45:409–17. doi: 10.1152/advan.00180.2020
3. Wang R, Zhang Z. The exploration and practice of BOPPPS teaching in the course of plant reproductive ecology. China Forest Educ. (2011) 29:55–7.
4. Wu J. Classroom teaching quality supervision system in college English based on SIOP and BOPPPS: with the example of one college. J Yibin Univ. (2014) 14:122–5.
5. Yuan F, Nafisa K, Xu R. Thinking and practice of medical cell biology teaching. Educ Teach Forum. (2015) 38:132–3.
6. Yang Y, You J, Wu J, Hu C, Shao L. The effect of microteaching combined with the BOPPPS model on dental materials education for predoctoral dental students. J Dental Educ. (2019) 83:567–74. doi: 10.21815/JDE.019.068
7. Yang N. Research on the application of BOPPPS teaching mode in the interactive integration of online and offline teaching in colleges and universities during post epidemic period. Adv Soc Sci Educ Hum Res. (2020) 490:265–8. doi: 10.2991/assehr.k.201127.052
8. Cui H. Application and exploration of BOPPPS model in oral Chinese teaching as a foreign language. IES. (2019) 12:123–9. doi: 10.5539/ies.v12n12p123
9. Zijun L, Sen Q. The construction. of BOPPPS teaching model in the course of inorganic chemistry course. In: Proceedings of the 2018 3rd International Conference on Society Science and Economics Development (ICSSED 2018). Nanjing: DEStech Publications Inc (2018). p. 157–9.
10. Hu K, Ma RJ, Ma C, Zheng QK, Sun ZG. Comparison of the BOPPPS model and traditional instructional approaches in thoracic surgery education. BMC Med Educ. (2022) 22:447. doi: 10.1186/s12909-022-03526-0
11. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. (2009) 6:e1000100. doi: 10.1371/journal.pmed.1000100
12. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. editors. Cochrane. Handbook for Systematic Reviews of Interventions Version 6.2 (Updated February 2021) Cochrane. (2021). Available online at: www.training.cochrane.org/handbook (accessed June 10, 2022).
13. Cook DA, Levinson AJ, Garside S, Dupras DM, Erwin PJ, Montori VM. Internet-based learning in the health professions: a meta-analysis. JAMA. (2008) 300:1181–96. doi: 10.1001/jama.300.10.1181
14. Wang J, Xu Y, Liu X, Xiong W, Xie J, Zhao J. Assessing the effectiveness of problem-based learning in physical diagnostics education in China: a meta-analysis. Sci Rep. (2016) 6:36279. doi: 10.1038/srep36279
15. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
16. Alenzi EO, Kelley GA. The association of hyperglycemia and diabetes mellitus and the risk of chemotherapy-induced neutropenia among cancer patients: a systematic review with meta-analysis. J Diabetes Complications. (2017) 31:267–72. doi: 10.1016/j.jdiacomp.2016.09.006
17. Chen K, Qian X, Xiao Q, Zhang YM. Application of BOPPPS teaching mode in standardized training and clinical teaching of TCM pediatric residents. J Pediatr TCM. (2021) 17:103–6.
18. Chen LM, Duan XY, Wang H, Xie F. Research on the application of BOPPPS in pathology teaching under the background of information technology. Chin Health Nutr. (2020) 30:28.
19. Cheng C, He F, Wang T. Application of BOPPPS combing with CBL method in experimental teaching of physical diagnosis under the background of “Internet+”. Zhonghua General Med. (2020) 18:1573–6.
20. Chu L, Shi L, Cheng S, Xu SY, Liu Q, Deng ZL, et al. Teaching practice of BOPPPS teaching mode in the integration course of movement system disease. Mod Med Health. (2021) 37:1557–9.
21. Deng HX, Wu RH, Jia S, Zhao X, Wang ZL, Lan Z, et al. The flipped classroom based on BOPPPS module applied in the course teaching of general practice. Educ Teach Forum. (2019) 39:178–9.
22. Di JN, Zhang L, Liu JY, Xin YB, Xu RG, Tong Q, et al. The application of BOPPPS mode based on the concept of OBE in the clinical training of respiratory medicine. Chin J Med Educ. (2021) 41:523–7.
23. Duan LH, Zeng Y, Han H. Application of BOPPS mode in orthopedics theory teaching. Chin Contemp Med. (2021) 28:186–9.
24. Gao J, Deng YJ, Wang L, Ma XQ, Lu N, Duan CY. Application of BOPPPS teaching mode combined with mind mapping in internal medicine teaching. Med Educ Res Pract. (2018) 26:895–8.
25. Gu J, Ji SG. The application of BOPPPS combined with O2O to resident training of neurosurgery department. Chin Contin Med Educ. (2020) 12:14–6.
26. Guo F. Exploration of BOPPPS teaching method for emergency medicine based on Bibo platform. Health Vocat Educ. (2018) 36:84–6.
27. Li XF, Gao Y, Han ZL, Qiu GC. Practice of BOPPPS mode in the standardized training of non-radiology residents. Chin Contin Med Educ. (2021) 13:68–71.
28. Li J, Zhang W, Chen B, Yang H, Liu SJ. Application and evaluation of BOPPPS combined with CBL teaching methods in the clinical practice of gynecology and obstetrics. Chin Med Herald. (2018) 15:68–71.
29. Li J, Xu JX, Wang C, Shao C, Xu Y. The application of teaching model of BOPPPS combined with rain classroom in clinical practice in internal medicine. J Qiqihar Med Coll. (2021) 42:1263–5.
30. Li L, Zhang Y, Fu XH, Peng XN, Yu CH. Application of mobile classroom based on BOPPPS model in the teaching of diagnostics. Chin High Med Educ. (2021) 2021:117–8.
31. Li S, Wang GH, Zhang YF, Zhao HW, Liu WY, Ma HH, et al. Application of “BOPPPS + micro-lecture” teaching mode in fundamentals of diagnostics. Chin Med Educ. (2022) 41:52–6.
32. Li SF, Zuorihan A, Gu XL, Chen F, Ayi XM, Wang R, et al. The application of BOPPPS model combined with case analysis method in pediatric trainee teaching. J Xinjiang Med Univ. (2017) 40:123–4.
33. Liu Q, Wang XQ, Zhou HM, Yuan J, Wang L, Xue X. Research on the application of BOPPPS teaching model in clinical teaching of internal medicine of TCM. World Latest Med Inf Dig. (2019) 19:363–4.
34. Liu XY, Lu C, Zhu H, Wang X, Jia S, Zhang Y, et al. Assessment of the effectiveness of BOPPPS-based hybrid teaching model in physiology education. BMC Med Educ. (2022) 22:217. doi: 10.1186/s12909-022-03269-y
35. Liu YD, Du YJ, Ma JL. Application of BOPPPS combined with mobile APP teaching mode in clinical teaching of spinal surgery. Chin J Med Educ. (2020) 40:1006–10.
36. Ma B, Luo XF, Shen XP, Liu YL, Li LJ, Tian JH, et al. Evaluation on effectiveness of BOPPPS method in evidence-based medicine teaching. Chin J Evid Based Med. (2019) 19:904–8.
37. Miao XL, Mu BR, Wei CW. Application of BOPPPS teaching mode based on the network platform in clinical case discussion teaching for anesthesiology residents. Chin Post Grad Med Educ. (2021) 5:468–71.
38. Parhati R, Xu BY, Alia A, Deng Q, Sheng WB. Application of BOPPPS combined with CBL method in orthopaedic teaching for international students. J Xinjiang Med Univ. (2018) 41:921–4.
39. Qin YH, Li L, Pan YZ, Qi TT, Huang LJ. Application and exploration of CBL combined with BOPPPS mode in neurology practice. J Qiqihar Med Coll. (2022) 43:271–5.
40. Shen XJ, Wang LC, Feng XH. The application of BOPPPS teaching method in the theoretical teaching of medicine diagnostics. Chin High Med Educ. (2016) 2016:99–100.
41. Shen XJ, Wang LC, Feng XH. The application of BOPPPS combined with PDG teaching method in the theoretical teaching of internal medicine. Chin High Med Educ. (2017) 2017:114–5.
42. Sun YR, Wang XY, Han LJ, Zhang N, Yu XW. Reflections on the teaching design of pathology course based on BOPPPS teaching model. Chin High Med Educ. (2020) 2020:79–80.
43. Tan H, Hu LY, Li ZH, Wu JY, Zhou WH. The application of BOPPPS combined with virtual simulation technology in the simulation training of neonatal asphyxia resuscitation. Chin J Med Educ. (2022) 42:155–8.
44. Tao W, Wang W. Application of BOPPPS and PBL in surgery teaching. Chin Contin Med Educ. (2020) 12:39–41.
45. Wan YX, Tao BD, Liu K, Zhang DD. Practical research on the combined teaching mode based on BOPPPS and split classroom in online courses of anesthesiology under the background of the coronavirus epidemic. Chin High Med Educ. (2020) 2020:64–5.
46. Wang HW, Wang JD, Lv LT, Zhang TT, Sun JH, Li J. The application and implementation strategy of BOPPPS teaching mode in clinical teaching rounds design in department neurology. J Qiqihar Med Coll. (2021) 42:1912–6.
47. Xing ZW. Application of PBL combined with CBL mode in clinical teaching of medical oncology. Chin Contin Med Educ. (2019) 11:27–9.
48. Xu YJ, Jin MY, Liu ZY, Li GP. Research on the blended teaching mode of BOPPPS and Chaoxing Xuetong in basic theory teaching of TCM. Lishizhen Med Mater Med Res. (2019) 30:1481–2.
49. Yang XH, Meng T. Application of BOPPPS combined with Bibo platform in the teaching of obstetrics for undergraduates. Health Vocat Educ. (2018) 36:48–50.
50. Yang Y, Su SX, Zhang X, Tu LG, Kong LP. Evaluation of the effect of BOPPPS combined with situational teaching method with smart-vocational platform in human anatomy. Anat Res. (2021) 43:178–81.
51. Yao HZ, Ying HN. The role of BOPPPS teaching model in improving the clinical teaching quality in internal medicine of TCM. J Chin Med Manage. (2022) 30:173–4.
52. Zhang DD, Lu YM, Guo ZQ, Zhou YZ, Song ZX, Bai X, et al. Research on the application of BOPPPS teaching method in online obstetrics and gynecology PBL teaching. Chin Higher Med Educ. (2021) 2021:123–4.
53. Zhang YY, Xu XY, Zhao HQ. Exploration of BOPPPS teaching model in clinical teaching of ward inspection in the standardized training of residents in the department of obstetrics and gynecology. Chin Mod Dr. (2018) 56:131–4.
54. Zhao H, Wang YM, He Q, Li XN, Zhang XC. The application of BOPPPS teaching mode based on micro-lecture in the teaching of isolation and protection technology for medical students. Chin J Infect Control. (2022) 21:287–90.
55. Zhao Y, Gao Z, Chen W, Jiang P, Chen RX. Evaluation of the effect of BOPPPS combined with PDG method in surgical clinical trainee teaching. Hunan J TCM. (2021) 37:117–9.
56. Zhou Y, Lv J, Ma J. Application of BOPPPS combined with CBL teaching method in the teaching of nephrology for international medical students under the COVID-19 pneumonia epidemic. Course Educ Res. (2021) 3:168–70.
57. Zhou Y, Fu YP. Application of BOPPPS method in ECG course teaching for medical students. Chin High Med Educ. (2020) 2020:99–100.
58. Ma X, Zhang L, Wang J, Luo Y, Wu Y. A perceptions assessment of patient-oriented problem-solving teaching strategy for medical immunology course in Chinese students. J Baltic Sci Educ. (2016) 15:706–11. doi: 10.33225/jbse/16.15.706
59. Wang S, Xu X, Li F, Fan H, Zhao E, Bai J. Effects of modified BOPPPS-based SPOC and flipped class on 5th-year undergraduate oral histopathology learning in China during COVID-19. BMC Med Educ. (2021) 21:540. doi: 10.1186/s12909-021-02980-6
60. Niu Z, Lou Z. Application of BOPPPS teaching model in adult education teaching design. China Adult Educ. (2017) 16:97–9.
61. Xie H, Liu L, Wang J, Joon KE, Parasuram R, Gunasekaran J, et al. The effectiveness of using non-traditional teaching methods to prepare student health care professionals for the delivery of mental state examination: a systematic review. JBI Database Syst Rev Implement Rep. (2015) 13:177–212. doi: 10.11124/01938924-201513070-00016
62. Shih WL, Tsai CY. Effect of flipped classroom with BOPPPS model on learners’ learning outcomes and perceptions in a business etiquette course. Asia Pac Edu Res. (2020) 29:257–68. doi: 10.1007/s40299-019-00475-z
63. Gonçalves-Manso DS, Rodrigues MP, Secio-Silva A, Alves EL, Oliveira VS, Carvalho P, et al. Strategies adopted by undergraduate teaching assistants in physiology and biophysics education during the COVID-19 pandemic. Adv Physiol Educ. (2022) 46:351–7. doi: 10.1152/advan.00042.2022
64. Wang X, Liu XY, Jia S, Jiao R, Zhang Y, Tang L, et al. TESOT: a teaching modality targeting the learning obstacles in global medical education. Adv Physiol Educ. (2021) 45:333–41. doi: 10.1152/advan.00191.2020
Keywords: BOPPPS (bridge-in, objective, pre-assessment, participatory learning, post-assessment, and summary), clinical medicine, medical education, medical students, curriculum, traditional learning, meta-analysis
Citation: Ma X, Zeng D, Wang J, Xu K and Li L (2022) Effectiveness of bridge-in, objective, pre-assessment, participatory learning, post-assessment, and summary teaching strategy in Chinese medical education: A systematic review and meta-analysis. Front. Med. 9:975229. doi: 10.3389/fmed.2022.975229
Received: 03 July 2022; Accepted: 29 August 2022;
Published: 15 September 2022.
Edited by:
Ahsan Sethi, Qatar University, QatarReviewed by:
Rui-Jie Ma, Shandong University, ChinaCopyright © 2022 Ma, Zeng, Wang, Xu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xingming Ma, bWluZzIwMjB4bUAxNjMuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.