- Department of General Surgery, Zhongshan Hospital of Traditional Chinese Medicine, Guangzhou University of Traditional Chinese Medicine, Zhongshan, China
Purpose: Biliary drainage is an important modality for extrahepatic obstructive jaundice both in patients with palliative and resectable. Currently, endoscopic biliary drainage is preferred in clinical practice, including endoscopic nasobiliary drainage (ENBD) and endoscopic biliary stenting (EBS), both of which have their own advantages and disadvantages. The purpose of our study was to compare the safety and efficacy of endoscopic biliary stenting (EBS) only vs. EBS plus nasobiliary drain for obstructive jaundice.
Methods: We consecutively reviewed patients with endoscopic biliary drainage in our institution from November 2014 to March 2021. Combined (ENBD plus stent) and single approach (EBS only) were defined as combined approach and single modality, respectively, and all eligible patients were divided into a combined approach group and a single modality group. We compared combined vs. single modality approaches to investigate whether there were statistical differences in liver chemistries, postoperative adverse events, and stent patency time.
Results: In 271 patients, a total of 356 times endoscopic biliary drainages were performed. All eligible patients were divided into the combined approach group (n = 74) and the single modality group (n = 271). The combined approach was associated with a lower incidence of postoperative cholangitis and bleeding and greater improvement in liver chemistries, although it was not statistically significant. However, it was superior to the single modality group in terms of hospital stay (12.7 ± 5.2 vs. 14.5 ± 7.9 days, p = 0.020 < 0.05) and stent patency time (8.1 ± 3.9 vs. 4.3±2.7 months, p = 0.001 < 0.05).
Conclusion: Endoscopic combined (ENBD plus stent) drainage is a more advantageous biliary drainage method that is characterized by more adequate biliary drainage, a lower incidence of postoperative adverse events, and longer effective biliary drainage time.
Introduction
Jaundice is defined as serum bilirubin ≥2 mg/dl, of which obstructive jaundice is the most common in the surgical department. It is referred to as surgical jaundice because it requires surgical intervention due to the blockage of the intrahepatic and extrahepatic bile ducts. However, obstructive jaundice is almost caused by the obstruction of extrahepatic bile ducts, such as bile duct stones, benign strictures, metastatic carcinomas, bile duct, pancreatic, and duodenal tumors. Endoscopic retrograde cholangiopancreatography (ERCP) is an important modality for the treatment of obstructive jaundice due to its superiority and availability. Improved diagnostic imaging and surgical procedures have clear benefits for the management of obstructive jaundice, however, we know that most malignant obstructive jaundice has lost the opportunity for radical surgery when it is identified. Biliary drainage has become the most important palliative treatment for these patients, which not only improves their quality of life (QOL), such as relieving jaundice and severe pruritus but also improves their survival rate (1, 2). Similarly, preoperative biliary drainage (PBD) is an essential procedure for resectable patients, which not only improves liver chemistries, coagulation, and nutritional status, but also improves immune function, promotes liver regeneration, and reduces the risk of intraoperative and postoperative complications (3–6). In addition, another study confirmed that PBD can improve postoperative mortality, morbidity, and resection rate (7).
Current biliary drainage includes percutaneous transhepatic biliary drainage (PTCD), endoscopic nasobiliary drainage (ENBD), and endoscopic biliary stenting (EBS), all of which are used clinically due to their own advantages and disadvantages. PTCD is still the main procedure for alleviating jaundice in institutions without ERCP-related equipment and professionally trained endoscopists. However, it is a more invasive procedure, which not only has the risk of adverse events such as cholangitis, pancreatitis, bleeding, and liver abscess, but also has the risk of tumor implantation (8, 9). Considering the patient's quality of life and avoiding tumor spread and serious complications, surgeons prefer endoscopic biliary drainage (10–12), which includes ENBD and EBS. Unlike ENBD, which not only allows us to observe biliary drainage more directly, regularly flush and dredge the nasobiliary duct and perform cholangiography, but also allows for cytology (13) and microbial culture to guide subsequent treatment, EBS does not. EBS has a higher incidence of cholangitis than ENBD due to stent obstruction and intestinal bacterial reflux (14–17). However, it has advantages in liver chemistries and immune function by maintaining intestinal hepatic circulation, metabolism, and vitamin absorption (18, 19). It also has the advantage of being aesthetically pleasing and free of nasopharyngeal discomfort. Plastic and nasobiliary ducts are common in developing countries due to the expense and availability of metal stents. At present, there is no consensus on the choice of endoscopic biliary drainage, which is usually based on the clinical experience of the institution and patient preferences.
Therefore, we hypothesized that endoscopic combined (ENBD plus stent) drainage is superior to EBS alone for obstructive jaundice. The purpose of our study was to compare the safety and efficacy of endoscopic biliary stenting (EBS) only vs. EBS plus nasobiliary drain for obstructive jaundice.
Materials and methods
Patients
Our study is a single-center retrospective cohort study, which was reviewed by the Ethics Committee of Zhongshan Hospital of Traditional Chinese Medicine, Guangzhou University of Traditional Chinese Medicine and waived the ethical requirements. All patients obtained written informed consent. We consecutively reviewed patients with obstructive jaundice who underwent endoscopic biliary drainage in our institution between November 2014 and March 2021. All data were obtained through electronic medical record systems and telephone follow-ups. The inclusion and exclusion criteria for this study are as follows. Inclusion criteria: (a) total serum bilirubin (TSB) > 2 mg/dl; (b) obstructive jaundice identified by computed tomography (CT), magnetic resonance cholangiopancreatography (MRCP) or ERCP; and (c) cause of biliary obstruction determined by imaging or endoscopic pathology. Exclusion criteria: (a) patients with intrahepatic biliary obstruction; (b) patients with other causes of jaundice, such as hepatocellular and hemolytic jaundice; (c) patients with missing primary data; and (d) patients with only ENBD.
Data collected included clinical characteristics, ERCP procedures, and their efficacy. Clinical characteristics included gender, age, etiology of obstructive jaundice, number of ERCPs, diabetes mellitus, history of malignancy and surgery, and preoperative cholangitis and pancreatitis. The ERCP procedures included whether or not to perform endoscopic sphincterotomy (EST), method of biliary drainage, type and number of stents, operation time, and technical success rate. The efficacy indicators included length of hospital stay, liver chemistries, postoperative cholangitis, pancreatitis and bleeding, and stent patency time. Liver chemistries indicators included serum alkaline phosphatase (ALP), glutamyl transpeptidase (GGT), serum total bilirubin (TSB), alanine aminotransferase (ALT), and aspartate aminotransferase (AST).
The diagnosis of cholangitis is based on clinical manifestations, such as fever, abdominal pain, jaundice, shock, altered consciousness, and increased white blood cells (WBCs) and serum total bilirubin. The diagnosis of pancreatitis is based on a patient's serum amylase level >3 times the upper limit of normal, or clinical manifestations, such as fever and abdominal pain, and imaging studies, such as abdominal ultrasound, CT, or magnetic resonance imaging (MRI). Postoperative bleeding was defined as symptoms, such as melena, hematemesis, or ENBD with bloody drainage, or a decrease in hemoglobin of ≥20 g/L requiring blood transfusion.
Combined (ENBD plus stent) and stent only were defined as combined approach and single modality, respectively, and all eligible patients were divided into the combined approach group (n = 74) and the single modality group (n = 271).
Endoscopic procedures
All ERCP procedures were performed by surgeons who perform more than 200 ERCPs per year. Both groups used the same endoscopic treatment system (such as, duodenoscope, contrast agent, contrast method, and pressure), the same anesthesia method, and postoperative follow-up. The only difference between the two groups was that the combined approach group had ENBD. All placed ENBDs were the same length and were sized to match the bile duct diameter and metal stent.
Statistical analysis
Categorical variables and normally distributed quantitative variables were represented by frequency (percentage) and mean ± standard deviation (SD), respectively. Based on the characteristics of the data, we appropriately applied the t-test, the chi-square test, and Fisher's exact test to assess differences between groups. While the Wilcoxon and Kruskal–Wallis tests were applied for non-normally distributed data. All statistical analysis were performed with SPSS version 25 (IBM, Armonk, NY, USA). A two-sided p < 0.05 was used to indicate statistical significance. All methods in our studies were carried out in accordance with relevant guidelines and regulations.
Results
The flow of the study is shown in Figure 1.
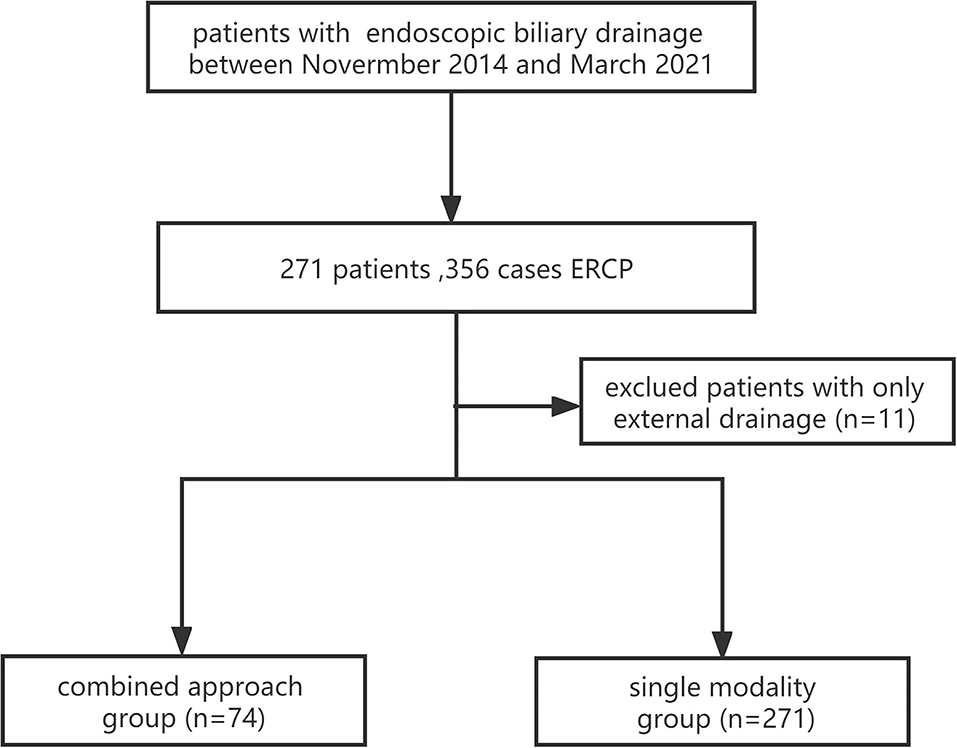
Figure 1. A flowchart of the study (the combined approach group: ENBD plus stent; and the single modality group: stent only).
A total of 271 patients with obstructive jaundice underwent endoscopic biliary drainage from November 2014 to March 2021, with a total of 356 ERCPs. Among these patients, 11 patients with ENBD only were excluded, and the eligible patients were divided into the single modality group (n = 271) and the combined approach group (n = 74).
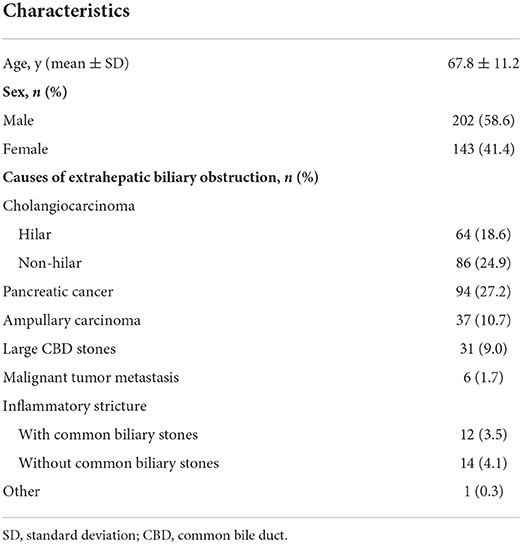
The clinical characteristics of eligible patients are shown in Table 1. The mean age of all eligible patients was 67.8 ± 11.2 years, and there were 202 (58.6%) men and 143 (41.4%) women, respectively. The causes of obstructive jaundice were extrahepatic cholangiocarcinoma, pancreatic cancer, ampullary cancer, large common biliary stones, metastatic lesions, and others. The other was a patient with sclerosing cholangitis. The primary tumors of 6 metastatic cancers were two liver cancer, two gallbladder cancer, one gastric cancer, and one colon cancer.
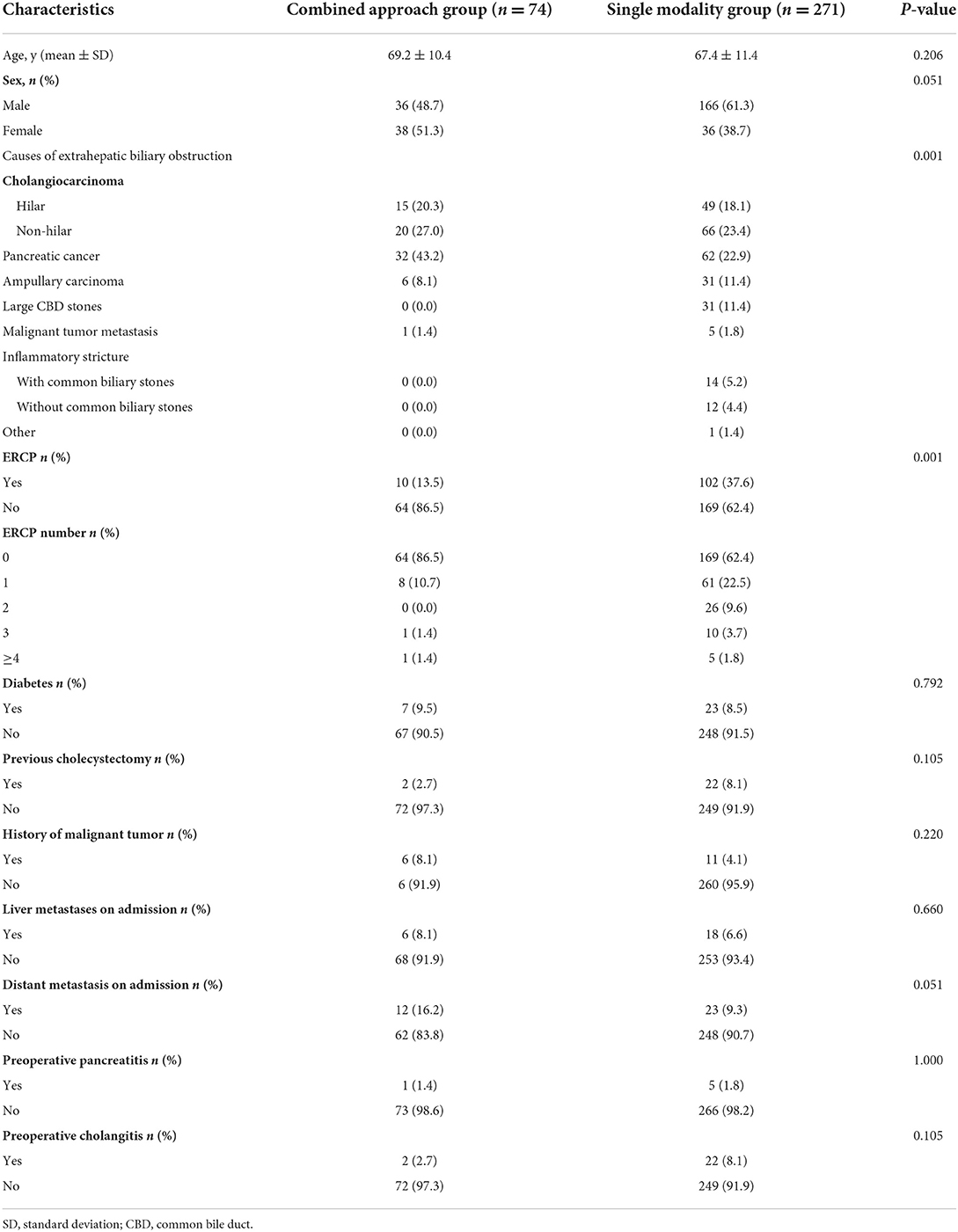
The clinical characteristics of the two groups are shown in Table 2. There were no statistically significant differences between the two groups in mean age, sex, diabetes, preoperative cholangitis and pancreatitis, and history of cholecystectomy and malignancy. The etiology of obstruction was statistically significant between the two groups (p = 0.001), and there were more patients with bile duct stones and inflammatory strictures in the single modality group than in the combined group. We saw that the proportion of previous ERCPs in the single modality group was significantly higher than that in the combined approach group (37.6 vs. 13.5%, p = 0.001), especially the number of ERCPs ≥ 2. Although the proportion of liver metastases and distant metastases in the combined approach group was higher than that in the single modality group, there was no statistical difference (8.1 vs. 6.6%, p = 0.660; 16.2 vs. 9.3%, p = 0.051).
The ERCP procedures in the two groups are shown in Table 3. During ERCP, EST is usually performed to facilitate stent implantation and removal of common biliary stones. We saw that the proportion of EST was higher in the combined approach group than in the single modality group (72.9 vs. 31%, p = 0.001). There were 2 patients with failed stent placement in the single modality group, but none in the combined approach group. However, there was no significant difference in the technical success rate between the two groups (99.3 vs. 100%, p = 1.000). To prevent or relieve pancreatitis, we usually place pancreatic plastic stents in selected patients. We saw no difference in the proportion of pancreatic duct stents between the two groups (14.9 vs. 14.0%, p = 0.854). We saw that the proportion of multiple biliary stents placed in the single modality group was significantly higher than that in the combined approach group (36.5 vs. 20.3%, p = 0.008). The single modality group preferred multiple plastic stents, however, the combined approach group was mostly a single metal stent.
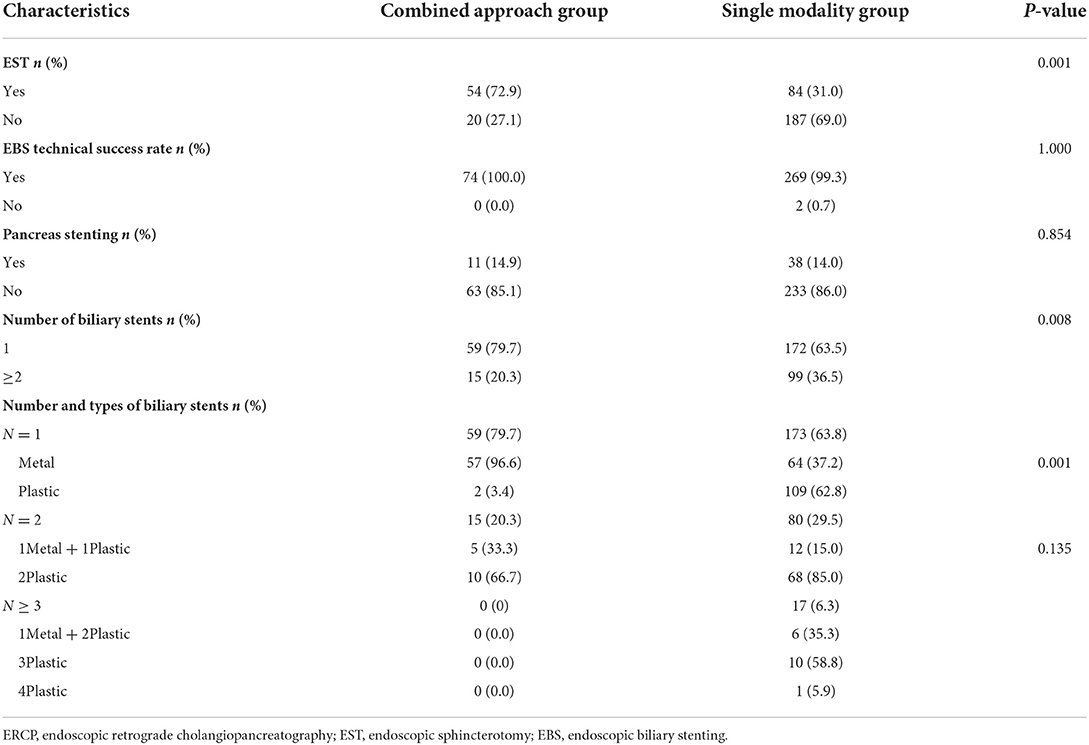
Table 3. Comparison of the combined approach group and the single modality group in ERCP procedures.
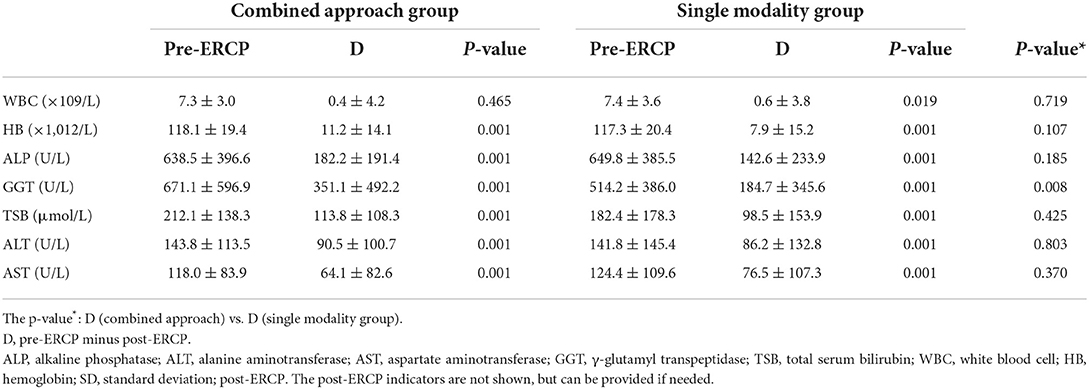
The laboratory parameters are shown in Table 4. In terms of preoperative-postoperative changes in WBC, it was decreased in both groups, and the difference was statistically significant in the single modality group, but not in the combined approach group. However, its change was not statistically different between the two groups (0.4 ± 4.2 vs. 0.6 ± 3.8, p = 0.719). We saw a statistically significant decrease in hemoglobin (HB) in the combined approach group and the single modality group (11.2 ± 14.1, p = 0.001, 7.9 ± 15.2, p = 0.001), however, there was no difference in the change in HB (11.2 ± 14.1 vs. 7.9 ± 15.2, p = 0.107). After ERCP, ALP decreased statistically in the two groups (638.5 ± 396.6 vs. 436.2 ± 335.0 U/L, p = 0.001 and 649.8 ± 385.5 vs. 433.3 ± 245.1 U/L, p = 0.001). Although there was no difference in ALP change between the two groups, the combined approach group was more significant than the single modality group (182.2 ± 191.4 vs. 142.6±233.9 U/L, p = 0.185). There were statistically significant differences in GGT changes between the combined approach group and the single modality group (671.1 ± 596.9 vs. 321.1 ± 225.5 U/L, p = 0.001 and 514.2 ± 386.0 vs. 329.9 ± 223.4 U/L, p = 0.001), and the change was more significant in the combined approach group (351.1 ± 492.2 vs. 184.7 ± 345.6 U/L, p = 0.008). TSB decreased statistically in the two groups (212.1 ± 138.3 vs. 98.3 ± 79.8 μmol/L, p = 0.001 and 182.4 ± 178.3 vs. 84.4 ± 80.1 μmol/L, p = 0.001). The change was more significant in the combined approach group than in the single modality group (113.8 ± 108.3 vs. 98.5 ± 153.9 μmol/L, p = 0.425). We saw that in the two groups, liver chemistries had been significantly improved, and there was no difference in the changes between the two groups. The changes in ALT and AST were 90.5 ± 100.7 U/L (p = 0.001), 64.1 ± 82.6 U/L (p = 0.001) in the combined approach group, and 86.2 ± 132.8 U/L, 76.5 ± 107.3 U/L (p = 0.001) in the single modality group. There was no significant difference in ALT and AST changes between the two groups (p = 0.803 and p = 0.370).
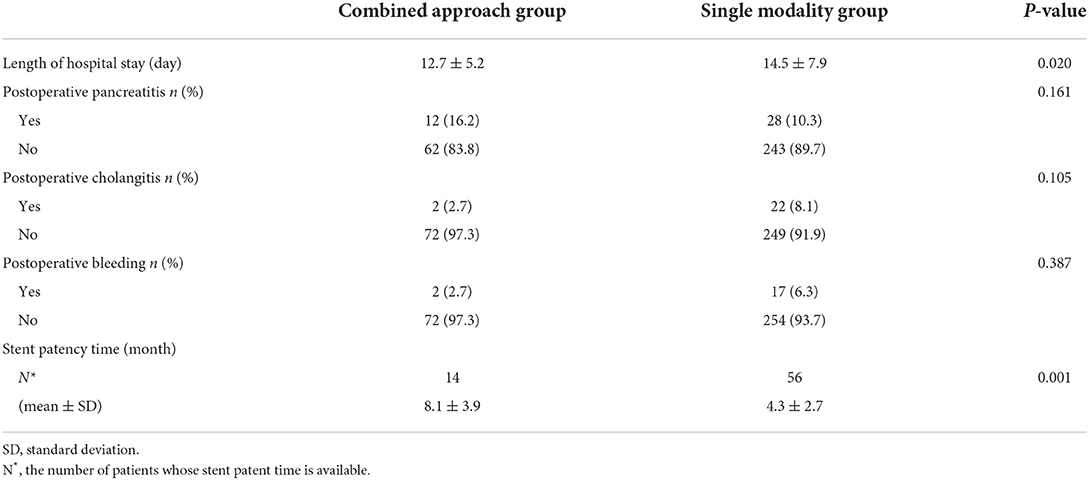
The efficacy and adverse events after EBS are shown in Table 5. The length of hospital stay was significantly shorter in the combined approach than in the single modality (12.7 ± 5.2 vs 14.5 ± 7.9 days, p = 0.020). We found a higher incidence of postoperative pancreatitis in the combined approach group than in the single modality group (16.2 vs. 10.2%), however, the results were reversed for postoperative cholangitis and bleeding (2.7 vs. 8.1 and 2.7 vs. 6.3%), but these were not statistically significant. In terms of stent patency time, we obtained detailed data on stent patency time, with 14 patients in the combined approach group and 56 patients in the single modality group. The shortest and longest times were 3 and 18 months in the combined approach group, respectively, and 15 days and 16 months in the single modality group. We saw that the stent patency time in the combined approach group was significantly longer than that in the single modality group (8.1 ± 3.9 vs. 4.3 ± 2.7 months, p = 0.001).
Discussion
We know that the most common causes of extrahepatic obstructive jaundice are cholangiocarcinoma, pancreatic cancer, and ampullary malignancies. When the disease is recognized, they are inoperable due to the advanced stage. Therefore, biliary drainage to relieve hyperbilirubinemia has become the most important treatment for these patients (20, 21). It not only relieves severe itching to improve the quality of life, but also restores the enterohepatic circulation of bilirubin to improve the nutritional status of patients, and alleviates the effects of hyperbilirubinemia on other organ functions (22), which are beneficial to the survival of patients. In addition, PBD is an essential procedure for those patients who can be radically resected (19), which reduces postoperative adverse events and improves survival. Some studies have shown that the median survival time of cholangiocarcinoma patients with bilirubin > 2 mg/dl was 4.8 months (95% CI, 3.1–9.4 months), however, 15.2 months (95% CI, 11.7–19.3 months) in patients with bilirubin ≤2 mg/dl (23). Similarly, another study also confirmed that even in patients with normal bilirubin, successful biliary drainage improves patient survival (1). In the institutions available for ERCP, the current biliary drainage prefers endoscopic biliary drainage over PTCD. Infection after ERCP is an inevitable serious complication, and its fatality rate is 8–20% (24, 25), and EBS increases its risk even more. Although EBS unblocks the passage of bile from the liver or gallbladder into the gut, it disrupts the mechanical and functional anti-reflux barriers, leading to an increased risk of acute cholangitis, pancreatitis, and liver abscesses, especially in the lower common biliary carcinoma and ampullary malignancies.
For patients with malignant obstructive jaundice, the median survival even after radical surgery is 1–4 years (26), whereas for patients with palliative biliary drainage may be only a few months. Therefore, the choice of the biliary drainage method needs to take into account the improvement of liver chemistry, postoperative adverse events, and effective drainage time. Our study found that the combined approach was superior to the single modality in terms of the stent patency time (8.1 ± 3.9 vs. 4.3 ± 2.7 months, p = 0.001). Repeated hospitalizations and multiple ERCPs not only increase the economic and physical burden but also cause mental distress and affect the quality of life in the end stage. Longer stent patency times mean fewer stent replacements, and the clinical characteristics of patients provide some evidence to some extent. In our study, we saw that the proportion of previous ERCPs was significantly higher in the single modality group than in the combined approach group (37.6 vs. 13.5%, p = 0.001), and even more so in multiple ERCPs. Our ideal biliary drainage would be better-improved liver chemistry, lower postoperative adverse events, and longer functional biliary drainage. In terms of improvement in liver chemistry indications in our study, we saw significant improvements in ALP, GGT, TSB, ALT, and AST in both groups, and more significantly in the combined approach group, but it was not statistically significant. Similarly, the incidence of postoperative cholangitis and bleeding in the combined approach group was lower than that in the single modality group, and the difference was not statistically significant. However, considering the differences in liver and distant metastases between the two groups at admission (8.1 vs. 6.6%, p = 0.660 and 16.2 vs. 9.3%, p = 0.051), we can see that the condition was more serious in the combined approach group. Therefore, this provided some evidence to some extent that combined (ENBD plus stent) drainage is more advantageous than stent drainage only in extrahepatic biliary obstructive jaundice.
In our study, we saw that the single modality group was more inclined to place multiple biliary stents than the combined approach group (36.5 vs. 20.3%, p = 0.008). Moreover, we found that the single modality group tended to be more plastic (62.8 vs. 3.4%, p = 0.001), even when placing multiple stents, there would be more choices for placing multiple metal stents. The cost of a single plastic stent is slightly lower than that of a metal stent. However, in clinical practice, surgeons usually tend to place multiple plastic stents for adequate drainage, and the overall cost is not less than that of metal stents. Moreover, multiple previous studies suggested that patients with bilateral multiple biliary stent drainage had an increased incidence of adverse events, such as cholangitis and liver abscess after ERCP (27–29). According to our clinical experience, patients with multiple common biliary plastic stents complain of upper abdominal discomfort, especially in patients with ≥3 plastic stents. The study by Cassani et al. showed that in the drainage of hilar biliary malignant tumors, there was no significant difference between plastic stents and metal stents in clinical success rate, cholangitis, acute pancreatitis, and stent displacement. However, in terms of stent blockage and tumor growth, plastic stents are obviously superior to metal stents (23). However, in current clinical practice, metal stents are almost fully covered with self-expanding metal stents, and compared with plastic stents, there is no significant difference in tumor growth in the stent. Moreover, when the metal stent is blocked, we need to unclog or replace it with ERCP again. However, the plastic stent needs to be replaced. Multiple studies have confirmed that fully covered metal stents have longer patient survival, a lower risk of stent dysfunction, cholangitis, and fewer re-interventions (3, 20, 30–32), and the patient's health-related quality of life (such as, general and disease-specific) is better (33). The study by Zhang et al. showed that patients with ENBD for biliary drainage had a significantly lower incidence of acute cholangitis, pancreatitis, and stent dysfunction (34).
Therefore, we prefer endoscopic combined (ENBD plus stent) drainage for patients with extrahepatic obstructive jaundice, especially for patients with malignant tumors of the lower end of the common biliary and ampulla. However, multiple studies have shown that ENBD is lower than EBS in postoperative cholangitis (14, 16, 35, 36) and stent dysfunction (14, 18, 19, 36) for malignant biliary obstruction drainage. A previous study showed that the temporary placement of ENBD in patients with fully covered self-expanding metal stents can reduce the incidence of postoperative cholangitis (37). Similarly, the bridge preoperative biliary drainage, that is, ENBD is replaced with a biliary stent when it is dysfunctional or intolerant, which can shorten the preoperative hospital stay and have a longer preoperative biliary drainage time (38). In our study, combined (ENBD plus stent) drainage can adequately drain the biliary tract and reduce the number of stents and procedure time, which fully utilizes ENBD and EBS. It is manifested as a more advantageous biliary drainage method, with sufficient biliary drainage, a lower incidence of postoperative adverse events, and longer successful biliary drainage time. We know that patients with malignant biliary obstruction are mostly elderly and have multiple underlying diseases. The longer the procedure time, the higher the incidence of postoperative adverse events, which affect the morbidity and mortality of patients. The causes of biliary stent dysfunction are usually refluxed food particles, blood clots, sludge, and small stones. For patients with ENBD plus stent drainage, when the biliary drainage dysfunction occurs, we can remove the ENBD or unblock the biliary stent, and the biliary drainage may be successful again.
Although, nasobiliary drainage is undoubtedly a good option for drainage, its displacement and nasopharyngeal discomfort are unavoidable problems, which lead to nasobiliary ducts rarely used in the West. However, nasobiliary application is more common in Asia because malignant patients are more concerned with clinical symptoms, such as jaundice and pruritus rather than nasopharyngeal discomfort. Due to the above reasons, we could not include nasopharyngeal discomfort in our study. The advantage of EBS is more stability and immobilization. However, for patients with PBD, EBS may not be a good choice because of stent removal and the impact on subsequent surgery. The EBSplus stent in our study may be more suitable for those patients with unresectable malignant obstructive jaundice, which may prolong stent patency, reduce adverse events, and improve quality of life. Compared with EBS alone, it is also possible to provide patients with psychological comfort and support, which is very important for patients with these advanced tumors, while its suitability for other patients remains to be studied.
This study also has many limitations. First, patient quality of life (QOL) is an important indicator, especially considering the limited life expectancy of patients with advanced malignancies, however, our study did not incorporate QOL measures. Second, our study assumes that the size of the biliary stent does not affect its function.
Conclusion
In conclusion, combined (ENBD plus stent) drainage is a more advantageous biliary drainage method, which is characterized by more adequate biliary drainage, a lower incidence of postoperative adverse events, and a longer effective biliary drainage time.
Data availability statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Zhongshan Hospital of Traditional Chinese Medicine, Guangzhou University of Traditional Chinese Medicine. The patients/participants provided their written informed consent to participate in this study.
Author contributions
HL designed and performed the research and wrote the paper. ML designed the research and supervised the report. CS and ZY provided clinical advice. All authors read and approved the final manuscript. All authors contributed to the study conception and design. All authors read and approved the final manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Paik WH, Park YS, Hwang J-H, Lee SH, Yoon CJ, Kang S-G, et al. Palliative treatment with self-expandable metallic stents in patients with advanced type III or IV hilar cholangiocarcinoma: a percutaneous versus endoscopic approach. Gastrointest Endosc. (2009) 69:55–62. doi: 10.1016/j.gie.2008.04.005
2. Arvanitakis M, Van Laethem JL, Pouzere S, Le Moine O, Deviere J. Predictive factors for survival in patients with inoperable Klatskin tumors. Hepatogastroenterology. (2006) 53:21–7.
3. Moole H, Bechtold M, Puli SR. Efficacy of preoperative biliary drainage in malignant obstructive jaundice: a meta-analysis and systematic review. World J Surg Oncol. (2016) 14:182. doi: 10.1186/s12957-016-0933-2
4. Chen P, Li B, Zhu Y, Chen W, Liu X, Li M, et al. Establishment and validation of a prognostic nomogram for patients with resectable perihilar cholangiocarcinoma. Oncotarget. (2016) 7:37319–30. doi: 10.18632/oncotarget.9104
5. Yoshida Y, Ajiki T, Ueno K, Shinozaki K, Murakami S, Okazaki T, et al. Preoperative bile replacement improves immune function for jaundiced patients treated with external biliary drainage. J Gastrointest Surg. (2014) 18:2095–104. doi: 10.1007/s11605-014-2674-2
6. Sauvanet A, Boher JM, Paye F, Bachellier P, Sa Cuhna A, Le Treut V-P, et al. Severe jaundice increases early severe morbidity and decreases long-term survival after pancreaticoduodenectomy for pancreatic adenocarcinoma. J Am Coll Surg. (2015) 221:380–9. doi: 10.1016/j.jamcollsurg.2015.03.058
7. Coates JM, Beal SH, Russo JE, Vanderveen KA, Chen SL, Bold RJ, et al. Negligible effect of selective preoperative biliary drainage on perioperative resuscitation, morbidity, and mortality in patients undergoing pancreaticoduodenectomy. Arch Surg. (2009) 144:841–7. doi: 10.1001/archsurg.2009.152
8. Sakata J, Shirai Y, Wakai T, Nomura T, Sakata E, Hatakeyama K. Catheter tract implantation metastases associated with percutaneous biliary drainage for extrahepatic cholangiocarcinoma. World J Gastroenterol. (2005) 11:7024–7. doi: 10.3748/wjg.v11.i44.7024
9. Laurent A, Tayar C, Cherqui D. Cholangiocarcinoma: preoperative biliary drainage. HPB. (2008) 10:126–9. doi: 10.1080/13651820802007472
10. Ruys AT, Gouma DJ, van Gulik TM. Percutaneous transhepatic biliary drainage catheter tract recurrence in cholangiocarcinoma. Br J Surg. (2011) 98:317. doi: 10.1002/bjs.7404
11. Kawashima H, Itoh A, Ohno E, Itoh Y, Nagino M, et al. Preoperative endoscopic nasobiliary drainage in 164 consecutive patients with suspected perihilar cholangiocarcinoma: a retrospective study of efficacy and risk factors related to complications. Ann Surg. (2013) 257:121–7. doi: 10.1097/SLA.0b013e318262b2e9
12. Barkay O, Mosler P, Schmitt CM, Lehman GA, Frakes JT, Johanson JF, et al. Effect of endoscopic stenting of malignant bile duct obstruction on quality of life. J Clin Gastroenterol. (2013) 47:526–31. doi: 10.1097/MCG.0b013e318272440e
13. Yagioka H, Hirano K, Isayama H, Tsujino T, Sasahira N, Nagano R, et al. Clinical significance of bile cytology via an endoscopic nasobiliary drainage tube for pathological diagnosis of malignant biliary strictures. J Hepatobiliary Pancreat Sci. (2011) 18:211–5. doi: 10.1007/s00534-010-0333-x
14. Kawakami H, Kuwatani M, Onodera M, Haba S, Eto K, Ehira N, et al. Endoscopic nasobiliary drainage is the most suitable preoperative biliary drainage method in the management of patients with hilar cholangiocarcinoma. J Gastroenterol. (2011) 46:242–8. doi: 10.1007/s00535-010-0298-1
15. Hochwald SN, Burke EC, Jarnagin WR, Fong Y, Blumgart LH. Association of preoperative biliary stenting with increased postoperative infectious complications in proximal cholangiocarcinoma. Arch Surg. (1999) 134:261–6. doi: 10.1001/archsurg.134.3.261
16. Fujii T, Yamada S, Suenaga M, Kanda M, Takami H, Sugimoto H, et al. Preoperative internal biliary drainage increases the risk of bile juice infection and pancreatic fistula after pancreatoduodenectomy: a prospective observational study. Pancreas. (2015) 44:465–70. doi: 10.1097/MPA.0000000000000265
17. Cortes A, Sauvanet A, Bert F, Janny S, Sockeel P, Kianmanesh R, et al. Effect of bile contamination on immediate outcomes after pancreaticoduodenectomy for tumor. J Am Coll Surg. (2006) 202:93–9. doi: 10.1016/j.jamcollsurg.2005.09.006
18. Sasahira N, Hamada T, Togawa O, Yamamoto R, Iwai T, Tamada K, et al. Multicenter study of endoscopic preoperative biliary drainage for malignant distal biliary obstruction. World J Gastroenterol. (2016) 22:3793–802. doi: 10.3748/wjg.v22.i14.3793
19. Kawakubo K, Kawakami H, Kuwatani M, Haba S, Kudo T, Taya YA, et al. Lower incidence of complications in endoscopic nasobiliary drainage for hilar cholangiocarcinoma. World J Gastrointest Endosc. (2016) 8:385–90. doi: 10.4253/wjge.v8.i9.385
20. Almadi MA, Barkun JS, Barkun AN. Stenting in malignant biliary obstruction. Gastrointest Endosc Clin N Am. (2015) 25:691–711. doi: 10.1016/j.giec.2015.06.002
21. Boulay BR, Birg A. Malignant biliary obstruction: from palliation to treatment. World J Gastrointest Oncol. (2016) 8:498–508. doi: 10.4251/wjgo.v8.i6.498
22. Myatra S, Divatia JV, Jibhkate B, Barreto GS, Shrikhande SV. Preoperative assessment and optimization in periampullary and pancreatic cancer. Indian J Cancer. (2011) 48:86–93. doi: 10.4103/0019-509X.75839
23. Cassani LS, Chouhan J, Chan C, Lanke G, Chen H-C, Wang X, et al. Biliary decompression in perihilar cholangiocarcinoma improves survival: a single-center retrospective analysis. Dig Dis Sci. (2019) 64:561–9. doi: 10.1007/s10620-018-5277-z
24. Motte S, Deviere J, Dumonceau JM, Serruys E, Thys J-P, Cremer M. Risk factors for septicemia following endoscopic biliary stenting. Gastroenterology. (1991) 101:1374–81. doi: 10.1016/0016-5085(91)90091-X
25. Allison MC, Sandoe JA, Tighe R, Simpson IA, Hall RJ, Elliot TSJ. Endoscopy committee of the British Society of Gastroenterology. Antibiotic prophylaxis in gastrointestinal endoscopy. Gut. (2009) 58:869–80. doi: 10.1136/gut.2007.136580
26. Rerknimitr R, Kladcharoen N, Mahachai V, Kullavanijaya P. Result of endoscopic biliary drainage in hilar cholangiocarcinoma. J Clin Gastroenterol. (2004) 38:518–23. doi: 10.1097/01.mcg.0000123204.36471.be
27. Iwano H, Ryozawa S, Ishigaki N, Taba K, Senyo M, Yoshida K, et al. Unilateral versus bilateral drainage using self-expandable metallic stent for unresectable hilar biliary obstruction. Dig Endosc. (2011) 23:43–8. doi: 10.1111/j.1443-1661.2010.01036.x
28. De Palma GD, Galloro G, Siciliano S, Iovino P, Catanzano C. Unilateral versus bilateral endoscopic hepatic duct drainage in patients with malignant hilar biliary obstruction: results of a prospective, randomized, and controlled study. Gastrointest Endosc. (2001) 53:547–53. doi: 10.1067/mge.2001.113381
29. Staub J, Siddiqui A, Murphy M, Lam R, Parikh M, Pleskow D, et al. Unilateral versus bilateral hilar stents for the treatment of cholangiocarcinoma: a multicenter international study. Ann Gastroenterol. (2020) 33:202–9. doi: 10.20524/aog.2020.0451
30. Zorrón Pu L, de Moura EG, Bernardo WM, Baracat FI, Mendonca EQ, Kondo A, et al. Endoscopic stenting for inoperable malignant biliary obstruction: a systematic review and meta-analysis. World J Gastroenterol. (2015) 21:13374–85. doi: 10.3748/wjg.v21.i47.13374
31. Hong WD, Chen XW, Wu WZ, Zhu QH, Chen XR. Metal versus plastic stents for malignant biliary obstruction: an update meta-analysis. Clin Res Hepatol Gastroenterol. (2013) 37:496–500. doi: 10.1016/j.clinre.2012.12.002
32. Sawas T, Al Halabi S, Parsi MA, Vargo JJ. Self-expandable metal stents versus plastic stents for malignant biliary obstruction: a meta-analysis. Gastrointest Endosc. (2015) 82:256–67.e7. doi: 10.1016/j.gie.2015.03.1980
33. Walter D, van Boeckel PG, Groenen MJ, Weusten BLAM, Witteman BJ, Tan G, et al. Higher quality of life after metal stent placement compared with plastic stent placement for malignant extrahepatic bile duct obstruction: a randomized controlled trial. Eur J Gastroenterol Hepatol. (2017) 29:231–7. doi: 10.1097/MEG.0000000000000762
34. Zhang W, Che X. Comparison of effect between nasobiliary drainage and biliary stenting in malignant biliary obstruction: a systematic review and updated meta-analysis. World J Surg Oncol. (2020) 18:71. doi: 10.1186/s12957-020-01848-1
35. Sugiyama H, Tsuyuguchi T, Sakai Y, Nisikawa T, Miyazaki M, Yokosuka O. Preoperative drainage for distal biliary obstruction: endoscopic stenting or nasobiliary drainage? Hepatogastroenterology. (2013) 60:231–4. doi: 10.5754/hge12621
36. Lin H, Li S, Liu X. The safety and efficacy of nasobiliary drainage versus biliary stenting in malignant biliary obstruction: a systematic review and meta-analysis. Medicine. (2016) 95:e5253. doi: 10.1097/MD.0000000000005253
37. Wan X, Chen S, Zhao Q, Li T, Luo S, Cai X, et al. The efficacy of temporary placement of nasobiliary drainage following endoscopic metal stenting to prevent post-ERCP cholangitis in patients with cholangiocarcinoma. Saudi J Gastroenterol. (2018) 24:348–54. doi: 10.4103/sjg.SJG_94_18
Keywords: extrahepatic obstructive jaundice, endoscopic biliary drainage (EBD), endoscopic nasobiliary drainage (ENBD), endoscopic biliary stent (EBS), efficacy
Citation: Liu H, Shi C, Yan Z and Luo M (2022) A single-center retrospective study comparing safety and efficacy of endoscopic biliary stenting only vs. EBS plus nasobiliary drain for obstructive jaundice. Front. Med. 9:969225. doi: 10.3389/fmed.2022.969225
Received: 14 June 2022; Accepted: 23 August 2022;
Published: 14 September 2022.
Edited by:
Abhilash Perisetti, University of Arkansas for Medical Sciences, United StatesReviewed by:
Chetan Mittal, Parkview Health, United StatesKetan Vagholkar, Padmashree Dr. D. Y. Patil University, India
Copyright © 2022 Liu, Shi, Yan and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ming Luo, bHVvbWluZ3pzc3p5eUAxMjYuY29t
 Huan Liu
Huan Liu Chuanke Shi
Chuanke Shi