- 1KM Science Research Division, Korea Institute of Oriental Medicine, Daejeon, South Korea
- 2Digital Health Research Division, Korea Institute of Oriental Medicine, Daejeon, South Korea
- 3Global Cooperation Center, Korea Institute of Oriental Medicine, Daejeon, South Korea
- 4KM Convergence Research Division, Korea Institute of Oriental Medicine, Daejeon, South Korea
- 5Korean Medicine Convergence Research Information Center, College of Korean Medicine, Kyung Hee University, Seoul, South Korea
- 6Department of Clinical Korean Medicine, Graduate School, Kyung Hee University, Seoul, South Korea
- 7School of Primary Care, Population Sciences and Medical Education, Faculty of Medicine, University of Southampton, Southampton, United Kingdom
- 8Antenna Foundation, Geneva, Switzerland
- 9BM Korean Internal Medicine Clinic, Daegu, South Korea
- 10Changpo Kyunghee Clinic, Pohang, South Korea
- 11I-MOM Korean Medicine Clinic, Jeju, South Korea
- 12You and Green Korean Medical Clinic, Daejeon, South Korea
- 13You and Green Korean Medical Clinic, Busan, South Korea
Background: This study aimed to explore individual prevalence of respiratory symptoms and to describe the Korean population's treatment approaches, preventive health behaviors, and mental health conditions during the pandemic.
Methods: We analyzed responses from an online nationwide survey, conducted between February 2021 to May 2021, about people's experiences during the pandemic. Statistical analysis was also performed to see if there were any significant differences in treatment and prevention strategies between different groups of respondents (between those had respiratory symptoms, compared with those who did not, and between those tested positive for COVID-19, compared with those who did not).
Results: A total of 2,177 survey respondents completed the survey and, of these, only 142 had experienced symptoms. The most frequently reported respiratory infections related symptoms were runny or blocked nose (47.6%), cough (45.5%), fever (44.1%), sore throat (42.0%), and fatigue (30.1%). More than half of the respondents (53.1%) used complementary and alternative medicine (CAM) approaches as means of preventive measures. In terms of preventive behaviors, the more emphasized behaviors were mask-wearing (58.9%) and hand-washing after coming home (42.7%). The majority of the respondents (64.9%) did not show signs of mental health issues.
Conclusion: In South Korea, conventional medicine was mainly used for COVID-19 treatment whereas CAM was commonly used as preventive measures. COVID-19 was also found to have less impact on the general population's mental health. The findings of this study may shed light on how the pandemic impacted the general population.
Introduction
The coronavirus disease 2019 (COVID-19) is a recent pandemic which highly impacts the public health and wellbeing (1–3). The severity of disease varies greatly from person to person, ranging from asymptomatic to mild flu-like symptoms to multiorgan failure, and even to death (4). Despite vaccination, non-pharmaceutical interventions including social distancing, putting on mask, and quarantine are still being implemented in many countries to prevent the widespread outbreaks of COVID-19. In the meantime, the pandemic response is still focusing on reducing hospitalization and fatality for those susceptible to COVID-19.
During the initial phase of the pandemic, South Korea was considered to have a well-organized epidemic control where various measures were taken to limit the spread of outbreak including mass population testing, tracing and isolating close contacts, and mandatory mask-wearing (5, 6). The government has also tried to contain the outbreak without a total lockdown of the country by imposing social distancing measures (7). The vaccination of COVID-19 began at the end of August 2021. Despite the efforts, the number of COVID-19 infections remains high.
Individuals' health-related behavior and lifestyle have changed significantly due to COVID-19 (8). Amid the COVID-19 outbreak, people began to engage in the recommended preventive health behaviors such as mask mandates, physical distancing, washing hands, and disinfecting surfaces (9). Social distancing, restrictions on daily activities and social gatherings, and closure of schools and universities have highly impacted the mental health of general population. On the other hand, COVID-19 produces similar symptoms to other viral respiratory infections (10). While most viral respiratory infections cause a relatively mild disease, COVID-19 is potentially much more serious and requires more attention. As there are many crossover symptoms between COVID-19 and respiratory infections (11, 12), it is important to make a conclusive diagnosis through proper testing.
In order to control the pandemic, the epidemiological community turned their attention to evaluating measures that might help contain the virus while vaccinations and pharmaceutical interventions were being developed. While there are many studies conducted on vaccinations and clinical manifestations of COVID-19, preventive studies have been limited to those conducted in China, United States, United Kingdom, Australia, Netherlands, Germany, and Italy (13–16). Several reviews also highlighted the benefits of herbal medicine, physical activity, and dietary supplements as a complement for the treatment and prevention of COVID-19 (17–20).
In light of these considerations, a national survey was conducted to explore individual prevalence of respiratory symptoms and to describe the Korean population's treatment approaches, preventive health behaviors, and mental health conditions during the pandemic.
Methods
Study design and setting
A nationwide survey, conducted via online Limesurvey platform in February 2021, was translated and modified from an international retrospective survey led by a team of researchers from University of Southampton and University of Geneva. The original survey was modified and localized by a research team from Korea Institute of Oriental Medicine and Kyunghee University to ensure that the translated survey was on-target, contextually precise, and culturally correct. The translated version was piloted to test the survey functionalities and to refine the whole survey before starting actual data collection. The survey was then disseminated to the general public within Korea using social media and online advertisement by means of convenience sampling and snowball sampling techniques. This study received ethical approval from Kyunghee University [KHSIRB-20-574 (EA), November 2020] and University of Southampton (ERGO 56975, May 2020). The STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines were followed for reporting this study (21).
Participants
All members of the public aged 16 and above were eligible to participate in this survey. Survey participants were required to provide informed consent for the use of their data at the start of the survey. Those who were under the age of 16 or lacked mental capacity to consent to the survey were excluded.
Variables and bias
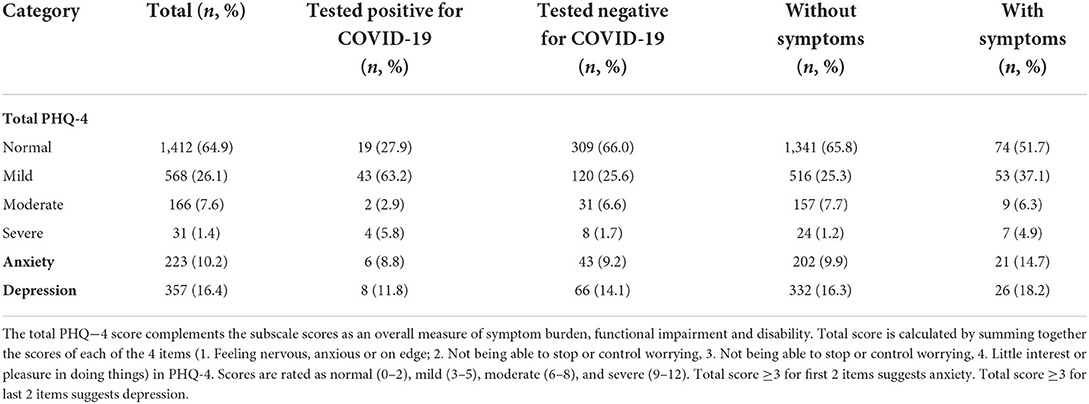
Respondents were asked about the presence and duration of COVID-19 symptoms, the type of treatment they received during their initial COVID-19 illness (e.g., conventional medicine or other approaches), actions taken as risk-reduction measures (e.g., vaccination, masking, social distancing etc.), type of approaches attempted to prevent COVID-19 and impact of the pandemic on mental health and wellbeing. The mental health status of the respondents was investigated using Patient Health Questionnaire for Depression and Anxiety (PHQ-4), which is a composite 4-item scale consisting of two core criteria for each depressive and anxiety disorder (22). PHQ-4 was used in order to examine both anxiety and depression due to COVID-19.
As this study was a retrospective survey, it may be subject to self-reporting bias and recall bias. To minimize the potential bias of this study, the survey questions were carefully designed and constructed. As the length of the recall period can affect data accuracy, the length of the recall period was also fairly short since the survey was conducted during early pandemic. Besides, a reminder was given to the survey respondents at the beginning of the survey if they had any memory aids such as medication diaries to enhance recall and reduce under-reporting.
Statistical methods
Statistical analyses were performed using R Statistical Software (v4.1.2; R Core Team 2021. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/). Demographic data and information about pre-existing health conditions were collated and analyzed descriptively. Statistical analysis was also carried out to investigate any differences in treatment and preventive approaches between those had respiratory symptoms, compared with those who did not, and between those who tested positive for COVID-19, compared with those who did not. Fisher's exact test was used to examine between-group differences, with p < 0.05 taken to indicate statistical significance. The most recent data was used for analysis when there were duplicate entries.
Results
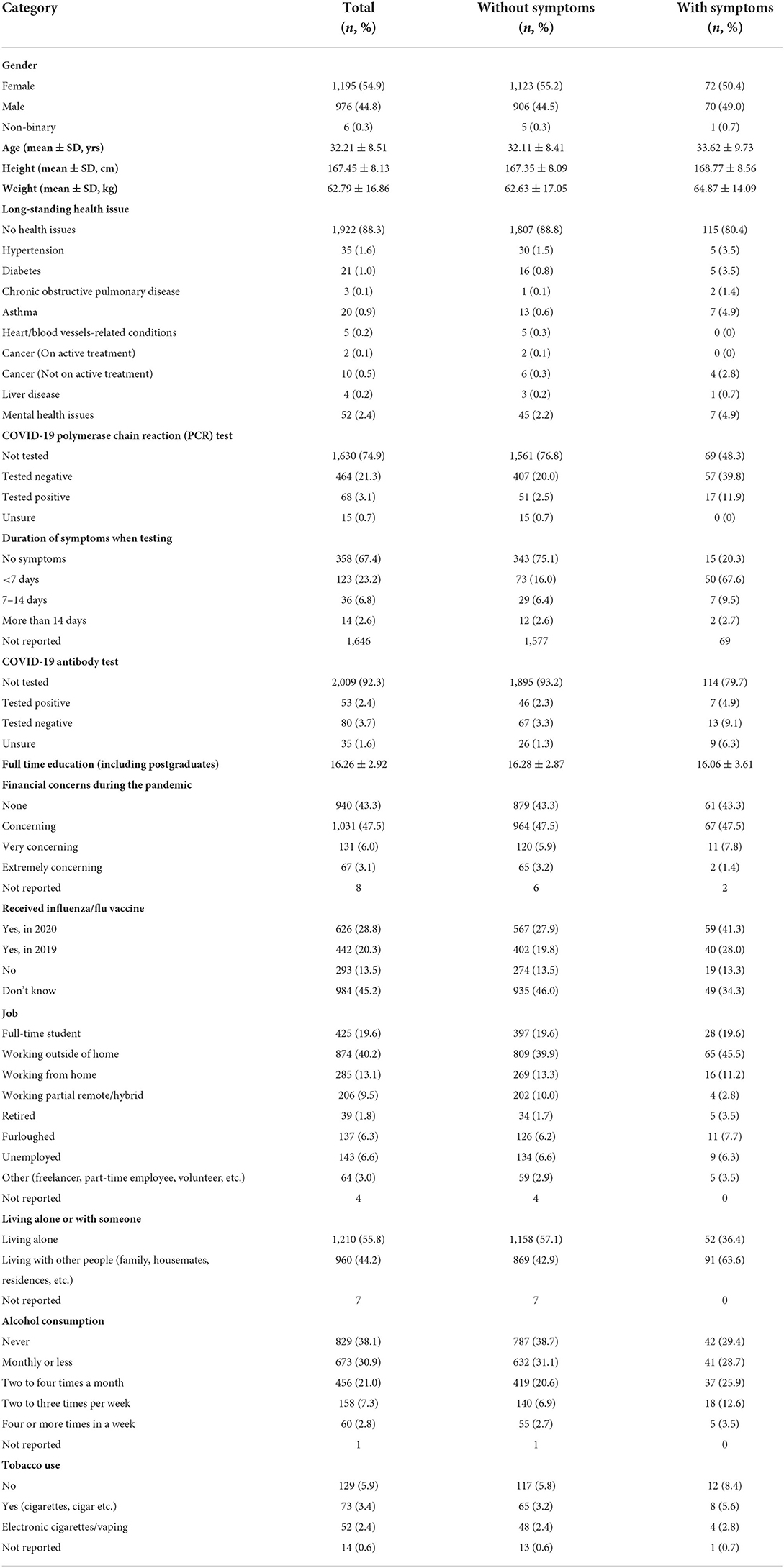
General characteristics of survey respondents
There were 3,188 responses between 9 February 2021 and 3 May 2021 which, excluding 980 partial entries and 31 duplicates, left a final sample of 2,177 for analysis (Table 1). The represented mean age was 32.2 years and 1,922 (88.3%) had no pre-existing health issues. A total of 68 (3.1%) were tested positive for COVID-19 and only 17 (11.9%) presented respiratory infections related symptoms.
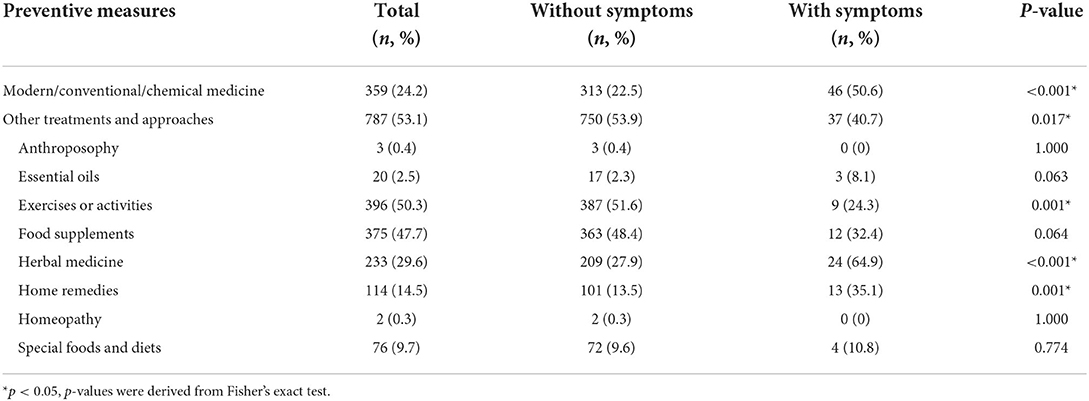
Preventive measures used by survey respondents
More than half of the survey respondents (53.1%) used complementary and alternative medicine (CAM) approaches as means of preventive measures (Table 2). Exercises or physical activities (n = 396, 50.3 %) were the most commonly used measures, followed by food supplements (n = 375, 47.7%) and herbal medicine (n = 233, 29.6%). On the other hand, conventional medicine (n = 46, 50.6%) was the most commonly used preventive measures among respondents with respiratory symptoms, while those who used CAM approaches mainly used herbal medicines (n = 24, 64.9%), followed by home remedies (n = 13, 35.1%), and food supplements (n = 12, 32.4%). A significant difference was also found between those with respiratory symptoms and those without in the preventive measure used among the CAM approaches. Those with respiratory symptoms preferred using herbal medicine (p < 0.001) and home remedies (p = 0.001) while those without respiratory symptoms preferred exercising or doing physical activities (p = 0.001) as preventive means.
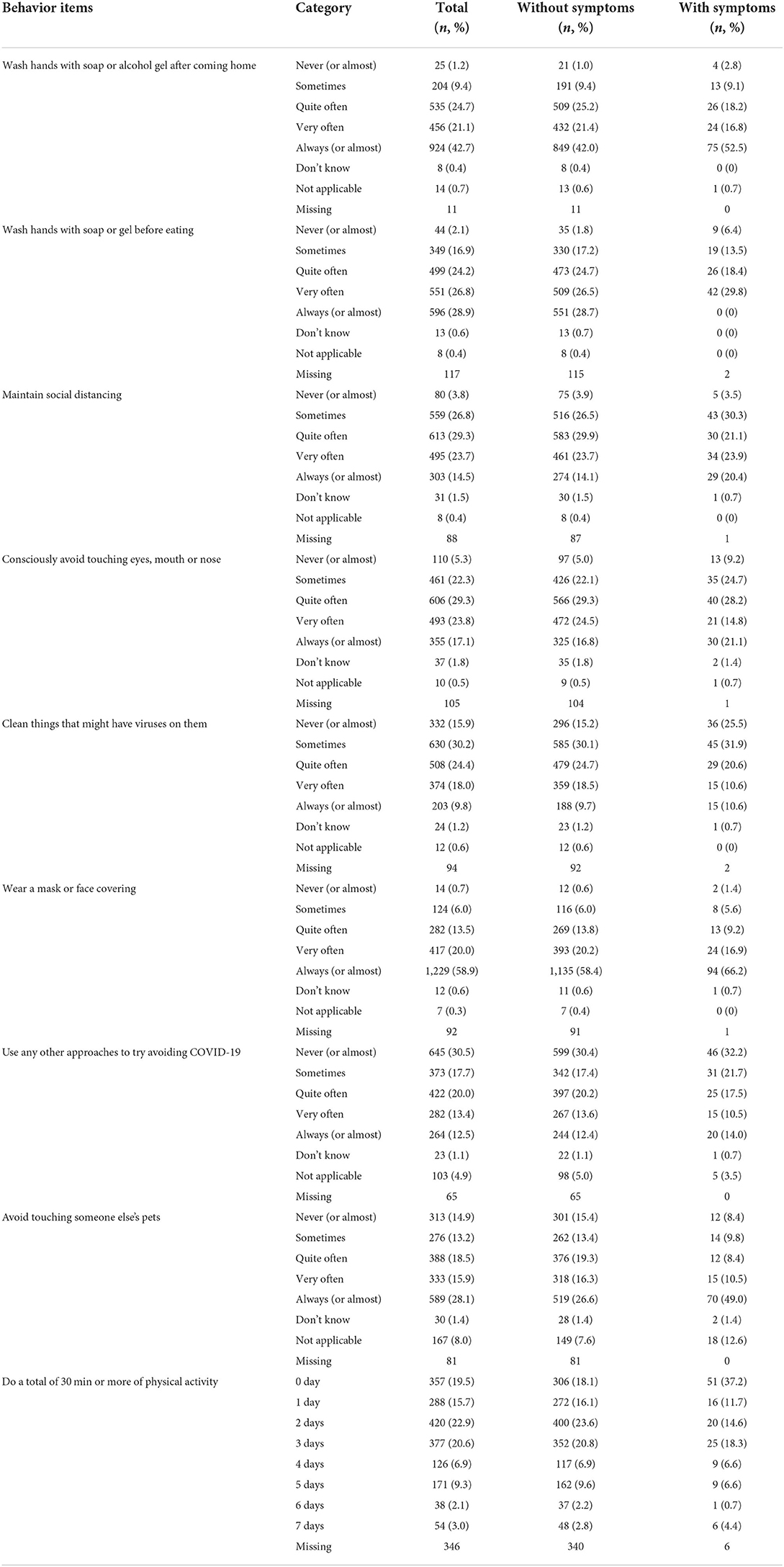
Preventive behaviors of survey respondents
Among the respondents' preventive behaviors, the more emphasized behaviors were mask-wearing and hand-washing behavior, where 58.9% of the respondents checked the former and 42.7% checked latter as “Always (or almost).” Those with respiratory symptoms had better preventive behavior in almost all areas (Table 3).
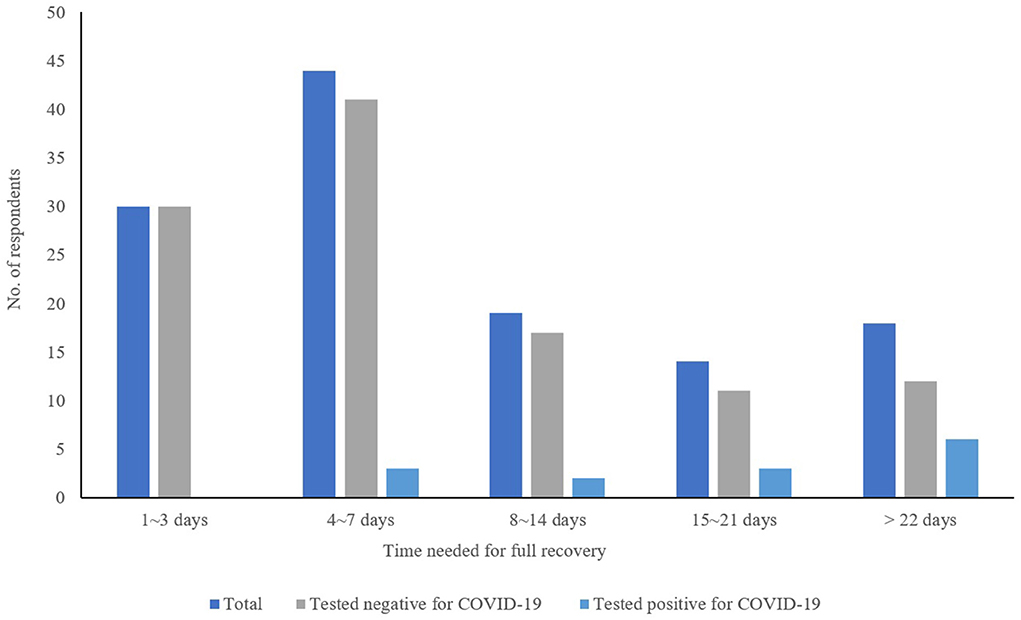
Symptoms and treatment measures reported by survey respondents
The most frequently reported respiratory infections related symptoms were runny or blocked nose (47.6%), cough (45.5%), fever (44.1%), sore throat (42.0%), and fatigue (30.1%) as shown in Table 4. Significant differences were also found between symptoms reported and COVID-19. Those who tested positive for COVID-19 reported higher prevalence of loss of smell or taste (p < 0.001) and muscles/joints aches (p = 0.016). Most of the respondents improved after 1-week of treatment (n = 68, 52.7%) and fully recovered (n = 74, 59.2%) within a week (Figure 1).
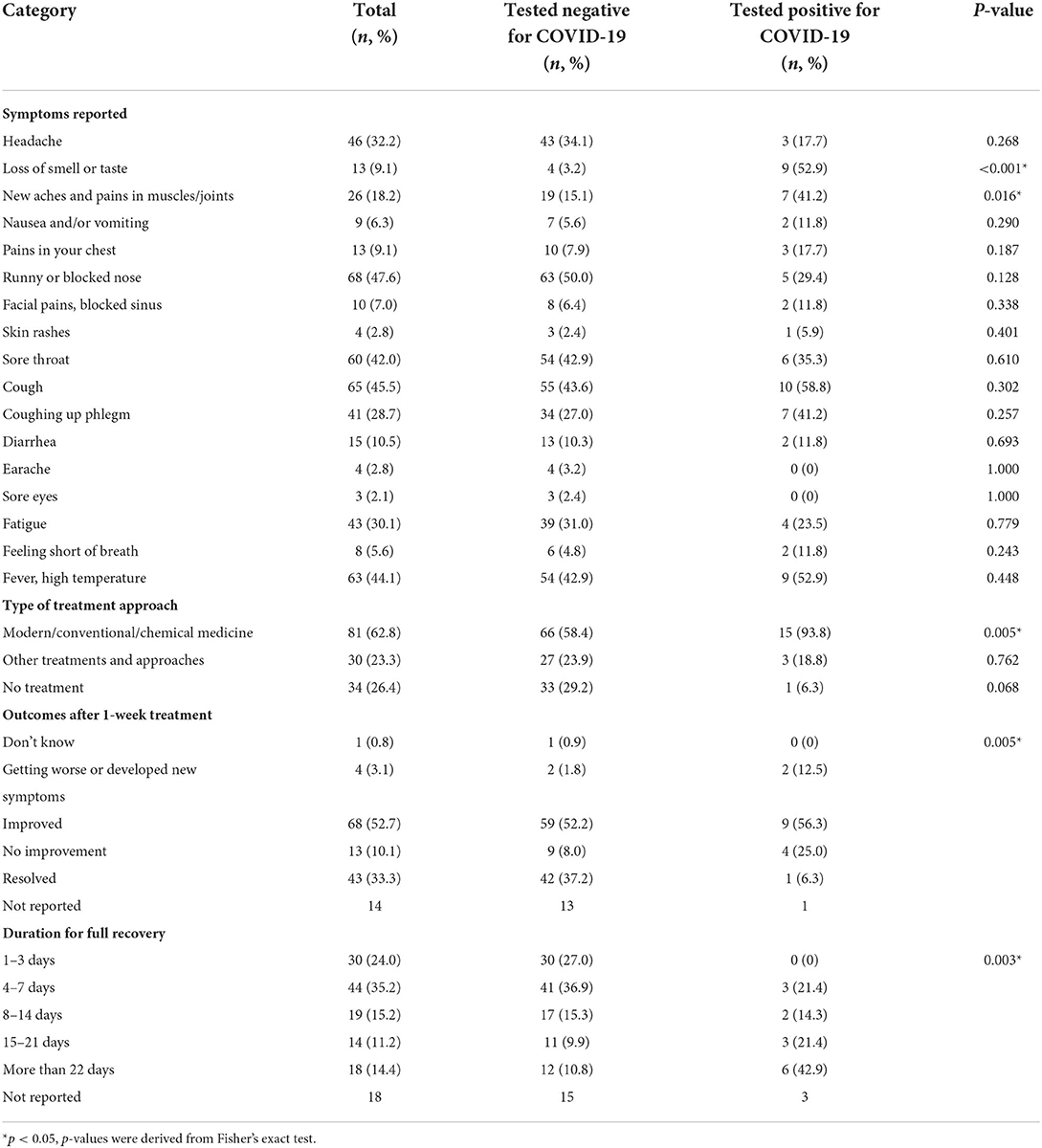
Table 4. Symptoms and treatment measures reported by survey respondents with symptoms, tested COVID-19 positive or negative.
Mental health status of survey respondents
This survey also included questions on mental health conditions which were based on the Patient Health Questionnaire-4 (PHQ-4), a self-report screening scale for anxiety and depression (Table 5). Majority of the respondents (64.9%) did not show signs of mental health issues.
Discussion
This study demonstrated that the majority of survey respondents had adequate understanding of COVID-19 prevention measures as relevant good practices. We found that individuals with respiratory infection-related symptoms were also more likely to engage in preventive behaviors, such as wearing masks in public places, washing their hands with soap or alcohol gel, and maintaining social distances, indicating health vulnerability affects individual engagement in preventive behaviors.
The majority of respondents in this study had implemented good personal preventive behaviors, where more than 80% of them reported putting on mask when leaving their home. This finding is similar to that of a recent survey in China which reported that 81% of their respondents mentioned wearing a mask in public (15). Another Chinese nationwide study reported that 97.9% of their respondents put on a mask in public and washed their hands more frequently than usual as a preventive measure (13).
However, the mask wearing rate in our finding was higher than other countries. According to a cross-sectional survey, the prevalence of putting on masks was considerably low in Australia (45.5–51.4%) and relatively higher in United Kingdom (70.8%) and United States (75.6–77.4%) (16).
With regard to preventive measures, the more commonly reported measures were exercise or activities, food supplements and herbal medicine. This finding is also similar to a survey study conducted in European countries where more than 50% of the survey respondents from Netherlands and Germany followed a healthy diet or took dietary supplements (14), but in contrast with their findings where only 34.2% practiced regular exercise. Additionally, exercise or physical activities has been found to improve resilience and reduce depressive symptoms (23). Our study adds an additional advantage of exercise or physical activities given its high usage as preventive measures.
Respondents in our survey also rated their mental health as average during the pandemic. Differing from other countries, our respondents did not experience any lockdown measures or extreme restrictions which may somehow reduce the impact of the pandemic on mental health (24). As this survey took place at the early stage of the pandemic, its impact on mental health was relatively small compared to the current status where the pandemic has been ongoing for years. Almost half of the respondents regarded their financial status as concerning during the pandemic. Loneliness and anxiety about money issues had a negative impact on mental health during the pandemic which could have risen due to loss of job, loss of loved ones, quarantine measure, and social distancing (25–27). Therefore, COVID-19 pandemic prevention measures should also include mental health and psychosocial considerations.
The variation in the symptoms reported also indicate that COVID-19 related symptoms often overlap with other respiratory infection related symptoms. Our findings showed that those who tested positive for COVID-19 infection had a significantly higher prevalence of symptoms such as loss of smell or taste, muscle and joint pains which are most representative symptoms of COVID-19 as reported in many previous studies (28–30). Due to the national healthcare policy, conventional medicine was mainly used for the treatment of COVID-19 (31–33). Herbal medicine was also used as treatment and prevention approaches but was not popular (34, 35). Most Korean citizens stored over-the-counter (OTC) conventional medication, such as acetaminophen and ibuprofen, as preventive means that these types of medicines were out of stock from most of the drugstores. Home stocking of OTC medications could also be due to delayed start of the vaccination compared to other countries since Korea started COVID-19 vaccination for the general population around end of August 2021 (36, 37).
However, there are several limitations in this study. The survey was completed purely with the respondents' personal experience and should not be used to infer about the experience or epidemiology of all individuals who had COVID-19 infection. This study was also subjected to selection bias, which may not be entirely representative of the Korean population, as our respondents are mainly in their 30 s and elderly people are under-represented. Besides, this study is based on subjective questioning and the reported symptoms and outcomes were not validated or confirmed.
Implications
This is the first study to explore the varying physical, psychological symptoms and patient experience during the ongoing COVID-19 pandemic in South Korea. Our findings show that there is a need for differentiated approaches based on individual needs and vulnerability in the engagement in preventive behaviors. We did not investigate on COVID-19 vaccination since no vaccine was available at the time of data collection; therefore, future studies could also explore the association between COVID-19 vaccination and different preventive health behaviors. Future research may also take pandemic-related factor such as vaccination doses or long COVID into account as they could refine our understanding on the impact of pandemic on general population. Future longitudinal studies and interventions would be needed to provide more insights to improve the management of pandemic in the long run.
Conclusion
In South Korea, conventional medicine was mainly used for COVID-19 treatment whereas CAM was commonly used as preventive measures. COVID-19 was also found to have less impact on the general population's mental health. The findings of this study may shed light on how the pandemic impacted the general population. Future COVID-19 and pandemic planning should take individual's experiences into consideration.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, on reasonable request.
Ethics statement
The studies involving human participants were reviewed and approved by Kyunghee University [KHSIRB-20-574 (EA), November 2020] and University of Southampton (ERGO 56975, May 2020). The patients/participants provided their written informed consent to participate in this study.
Author contributions
This work is conceptualized by MW, BG, JH, X-YH, and ML. The study methodology was designed by MW, BG, JH, and X-YH validated by HL, T-HK, HWL, and ML. Formal analysis and data curation were performed by MY and LA. The original draft was written by LA, ES, and MY and reviewed by J-WL, YJ, JK, EK, YP, HWL, and ML. This project was supervised and administered by ML. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by Korea Institute of Oriental Medicine (KSN20224112). This funding source did not participate in the design of this study or play any role during its execution, analyses, interpretation of the data, manuscript drafting, or decision to submit results.
Acknowledgments
We would like to thank the research team from University of Southampton and the University of Geneva for providing the original survey questions and all technical support. This study was part of an international retrospective survey on the prevention, treatment, occurrence and outcomes of COVID-19 in the community (RTO-COVID-19) involving 14 countries.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Meyer J, Mcdowell C, Lansing J, Brower C, Smith L, Tully M, et al. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. Int J Environ Res Public Health. (2020) 17:6469 doi: 10.3390/ijerph17186469
2. Violant-Holz V, Gallego-Jiménez MG, González-González CS, Muñoz-Violant S, Rodríguez MJ, Sansano-Nadal O, et al. Psychological health and physical activity levels during the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. (2020) 17:9419. doi: 10.3390/ijerph17249419
3. Shanbehzadeh S, Tavahomi M, Zanjari N, Ebrahimi-Takamjani I, Amiri-Arimi S. Physical and mental health complications post-COVID-19: scoping review. J Psychosom Res. (2021) 147:110525. doi: 10.1016/j.jpsychores.2021.110525
4. Nasserie T, Hittle M, Goodman SN. Assessment of the frequency and variety of persistent symptoms among patients with COVID-19: a systematic review. JAMA Netw Open. (2021) 4:e2111417. doi: 10.1001/jamanetworkopen.2021.11417
5. Dighe A, Cattarino L, Cuomo-Dannenburg G, Skarp J, Imai N, Bhatia S, et al. Response to COVID-19 in South Korea and implications for lifting stringent interventions. BMC Med. (2020) 18:321. doi: 10.1186/s12916-020-01791-8
6. Ryu S-K, Chung S-G. Korea's early COVID-19 response: findings and implications. Int J Environ Res Public Health. (2021) 18:8316. doi: 10.3390/ijerph18168316
7. Kim W, Jung TY, Roth S, Um W, Kim C. Management of the COVID-19 pandemic in the Republic of Korea from the perspective of governance and public-private partnership. Yonsei Med J. (2021) 62:777–91. doi: 10.3349/ymj.2021.62.9.777
8. Zhou Y, Draghici A, Abbas J, Mubeen R, Boatca ME, Salam MA. Social media efficacy in crisis management: effectiveness of non-pharmaceutical interventions to manage COVID-19 challenges. Front Psychiatry. (2021) 12:626134. doi: 10.3389/fpsyt.2021.626134
9. Aschwanden D, Strickhouser JE, Sesker AA, Lee JH, Luchetti M, Terracciano A, et al. Preventive behaviors during the COVID-19 pandemic: associations with perceived behavioral control, attitudes, and subjective norm. Front Public Health. (2021) 9:662835. doi: 10.3389/fpubh.2021.662835
10. Pormohammad A, Ghorbani S, Khatami A, Razizadeh MH, Alborzi E, Zarei M, et al. Comparison of influenza type A and B with COVID-19: a global systematic review and meta-analysis on clinical, laboratory and radiographic findings. Rev Med Virol. (2021) 31:e2179. doi: 10.1002/rmv.2179
11. Dadashi M, Khaleghnejad S, Abedi Elkhichi P, Goudarzi M, Goudarzi H, Taghavi A, et al. COVID-19 and influenza co-infection: a systematic review and meta-analysis. Front Med. (2021) 8:681469–681469. doi: 10.3389/fmed.2021.681469
12. Dao TL, Hoang VT, Colson P, Million M, Gautret P. Co-infection of SARS-CoV-2 and influenza viruses: a systematic review and meta-analysis. J Clin Virol Plus. (2021) 1:100036. doi: 10.1016/j.jcvp.2021.100036
13. Huang Y, Wu Q, Wang P, Xu Y, Wang L, Zhao Y, et al. Measures undertaken in china to Avoid COVID-19 infection: internet-based, cross-sectional survey study. J Med Int Res. (2020) 22:e18718. doi: 10.2196/18718
14. Meier K, Glatz T, Guijt MC, Piccininni M, Van Der Meulen M, Atmar K, et al. Public perspectives on protective measures during the COVID-19 pandemic in the Netherlands, Germany and Italy: a survey study. PLoS ONE. (2020) 15:e0236917. doi: 10.1371/journal.pone.0236917
15. Lu C-L, Zheng R-X, Xue X, Zhang X-W, Liu X-H, Jin X-Y, et al. Traditional Chinese medicine for COVID-19 pandemic and emerging challenges: an online cross-sectional survey in China. Integ Med Res. (2021) 10:100798. doi: 10.1016/j.imr.2021.100798
16. Macintyre CR, Nguyen P-Y, Chughtai AA, Trent M, Gerber B, Steinhofel K, et al. Mask use, risk-mitigation behaviours and pandemic fatigue during the COVID-19 pandemic in five cities in Australia, the UK and USA: a cross-sectional survey. Int J Infect Dis. (2021) 106:199–207. doi: 10.1016/j.ijid.2021.03.056
17. Dai T, Zhang L, Dai X, Zhang X, Lu B, Zheng Y, et al. Multimode participation of traditional Chinese medicine in the treatment of COVID-19. Int Med Res. (2021) 10:100781. doi: 10.1016/j.imr.2021.100781
18. Lordan R, Rando HM, Greene CS. Dietary supplements and nutraceuticals under investigation for COVID-19 prevention and treatment. mSystems. (2021) 6:e00122-21. doi: 10.1128/mSystems.00122-21
19. Mullin GE, Limektkai B, Wang L, Hanaway P, Marks L, Giovannucci E. Dietary supplements for COVID-19. Adv Exp Med Biol. (2021) 1318:499–515. doi: 10.1007/978-3-030-63761-3_29
20. Saeidi A, Tayebi SM, To-Aj O, Karimi N, Kamankesh S, Niazi S, et al. Physical activity and natural products and minerals in the SARS-CoV-2 pandemic: an update. Ann Appl Sport Sci. (2021) 9:e976. doi: 10.29252/aassjournal.976
21. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. (2007) 370:1453–7. doi: 10.1016/S0140-6736(07)61602-X
22. Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. (2009) 50:613–21. doi: 10.1016/S0033-3182(09)70864-3
23. Carriedo A, Cecchini JA, Fernandez-Rio J, Méndez-Giménez A. COVID-19, psychological well-being and physical activity levels in older adults during the nationwide lockdown in Spain. Am J Geriatr Psychiatry. (2020) 28:1146–55. doi: 10.1016/j.jagp.2020.08.007
24. Yoo KJ, Kwon S, Choi Y, Bishai DM. Systematic assessment of South Korea's capabilities to control COVID-19. Health Policy. (2021) 125:568–76. doi: 10.1016/j.healthpol.2021.02.011
25. Buselli R, Corsi M, Veltri A, Baldanzi S, Chiumiento M, Lupo ED, et al. Mental health of health care workers (HCWs): a review of organizational interventions put in place by local institutions to cope with new psychosocial challenges resulting from COVID-19. Psychiatry Res. (2021) 299:113847. doi: 10.1016/j.psychres.2021.113847
26. Chen PJ, Pusica Y, Sohaei D, Prassas I, Diamandis EP. An overview of mental health during the COVID-19 pandemic. Diagnosis. (2021) 8:403–12. doi: 10.1515/dx-2021-0046
27. Deng J, Zhou F, Hou W, Silver Z, Wong CY, Chang O, et al. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci. (2021) 1486:90–111. doi: 10.1111/nyas.14506
28. Drozdzal S, Rosik J, Lechowicz K, Machaj F, Szostak B, Majewski P, et al. COVID-19: pain management in patients with SARS-CoV-2 infection-molecular mechanisms, challenges, and perspectives. Brain Sci. (2020) 10:465. doi: 10.3390/brainsci10070465
29. Mastrangelo A, Bonato M, Cinque P. Smell and taste disorders in COVID-19: from pathogenesis to clinical features and outcomes. Neurosci Lett. (2021) 748:135694. doi: 10.1016/j.neulet.2021.135694
30. Santos REA, Da Silva MG, Do Monte Silva MCB, Barbosa DM, Gomes A, et al. Onset and duration of symptoms of loss of smell/taste in patients with COVID-19: a systematic review. Am J Otolaryngol. (2021) 42:102889. doi: 10.1016/j.amjoto.2020.102889
31. Kang J, Jang YY, Kim J, Han S-H, Lee KR, Kim M, et al. South Korea's responses to stop the COVID-19 pandemic. Am J Infect Control. (2020) 48:1080–6. doi: 10.1016/j.ajic.2020.06.003
32. Kwon S, Chung H, Kang Y, Jang I, Choi J-Y, Jung IC, et al. The role of Korean Medicine in the post-COVID-19 era: an online panel discussion part 1 – clinical research. Int Med Res. (2020) 9:100478. doi: 10.1016/j.imr.2020.100478
33. Park S, Hahm D-H, Joo M, Kim K, Kwon S, Choi H, et al. The role of Korean medicine in the post-COVID-19 era: an online panel discussion part 2 – basic research and education. Int Med Res. (2020) 9:100488. doi: 10.1016/j.imr.2020.100488
34. Ang L, Lee HW, Choi JY, Zhang J, Soo Lee M. Herbal medicine and pattern identification for treating COVID-19: a rapid review of guidelines. Int Med Res. (2020) 9:100407. doi: 10.1016/j.imr.2020.100407
35. Jeon S-R, Kang JW, Ang L, Lee HW, Lee MS, Kim T-H. Complementary and alternative medicine (CAM) interventions for COVID-19: an overview of systematic reviews. Int Med Res. (2022) 11:100842. doi: 10.1016/j.imr.2022.100842
36. Shim E. Projecting the impact of SARS-CoV-2 variants and the vaccination program on the fourth wave of the COVID-19 pandemic in South Korea. Int J Environ Res Public Health. (2021) 18:7578. doi: 10.3390/ijerph18147578
Keywords: COVID-19, behavior, public health, social measures, wellbeing, health care
Citation: Ang L, Yim MH, Song E, Lee HW, Lee H, Kim T-H, Willcox M, Hu X-Y, Houriet J, Graz B, Lee J-W, Jang Y, Kim JT, Kim E, Park YH and Lee MS (2022) A nationwide survey on the management of the COVID-19 pandemic and respiratory disease in South Korea. Front. Med. 9:965651. doi: 10.3389/fmed.2022.965651
Received: 10 June 2022; Accepted: 29 August 2022;
Published: 23 September 2022.
Edited by:
Yonggang Zhang, Sichuan University, ChinaReviewed by:
Gang Sun, Johns Hopkins University, United StatesHaewon Byeon, Inje University, South Korea
Rama Shankar Rath, All India Institute of Medical Sciences Gorakhpur, India
Copyright © 2022 Ang, Yim, Song, Lee, Lee, Kim, Willcox, Hu, Houriet, Graz, Lee, Jang, Kim, Kim, Park and Lee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Myeong Soo Lee, ZHJtc2xlZSYjeDAwMDQwO2dtYWlsLmNvbQ==; bXNsZWUmI3gwMDA0MDtraW9tLnJlLmty
 Lin Ang
Lin Ang Mi Hong Yim
Mi Hong Yim Eunhye Song
Eunhye Song Hye Won Lee
Hye Won Lee Hyangsook Lee
Hyangsook Lee Tae-Hun Kim
Tae-Hun Kim Merlin Willcox
Merlin Willcox Xiao-Yang Hu
Xiao-Yang Hu Joelle Houriet
Joelle Houriet Bertrand Graz8
Bertrand Graz8 Je-Won Lee
Je-Won Lee Myeong Soo Lee
Myeong Soo Lee