- 1Department of Pediatrics, Division of Oncology and Hematology, Charité – Universitätsmedizin Berlin, Freie Universität Berlin, Humboldt-Universität zu Berlin, Berlin Institute of Health, Berlin, Germany
- 2Institute of General Practice and Interprofessional Care, University Hospital Tübingen, Tübingen, Germany
- 3Bosch Health Campus, Stuttgart, Germany
- 4Department of Pediatrics, Faculty of Medicine, University of São Paulo, São Paulo, Brazil
Introduction: External applications from anthroposophic medicine (EAAM) are touch-based applications such as rhythmical massages, embrocations, and compresses that serve as components of complementary treatment concepts for various diseases. The aim of this review is to gain an understanding of typical indications and outcomes and to systematically assess the effectiveness and safety of EAAM.
Materials and methods: Medline/PubMed, CINAHL, the Cochrane Library, Embase, and PsycINFO were searched through May 2021 and supplemented by searches in specialized databases and personal requests to experts in the field. Studies and case reports on EAAM in patients, as well as healthy individuals, were included in the qualitative synthesis. Outcome parameters depending on each study were grouped as effect themes and assigned to study clusters using Thematic Analysis for a thematic overview of effect patterns.
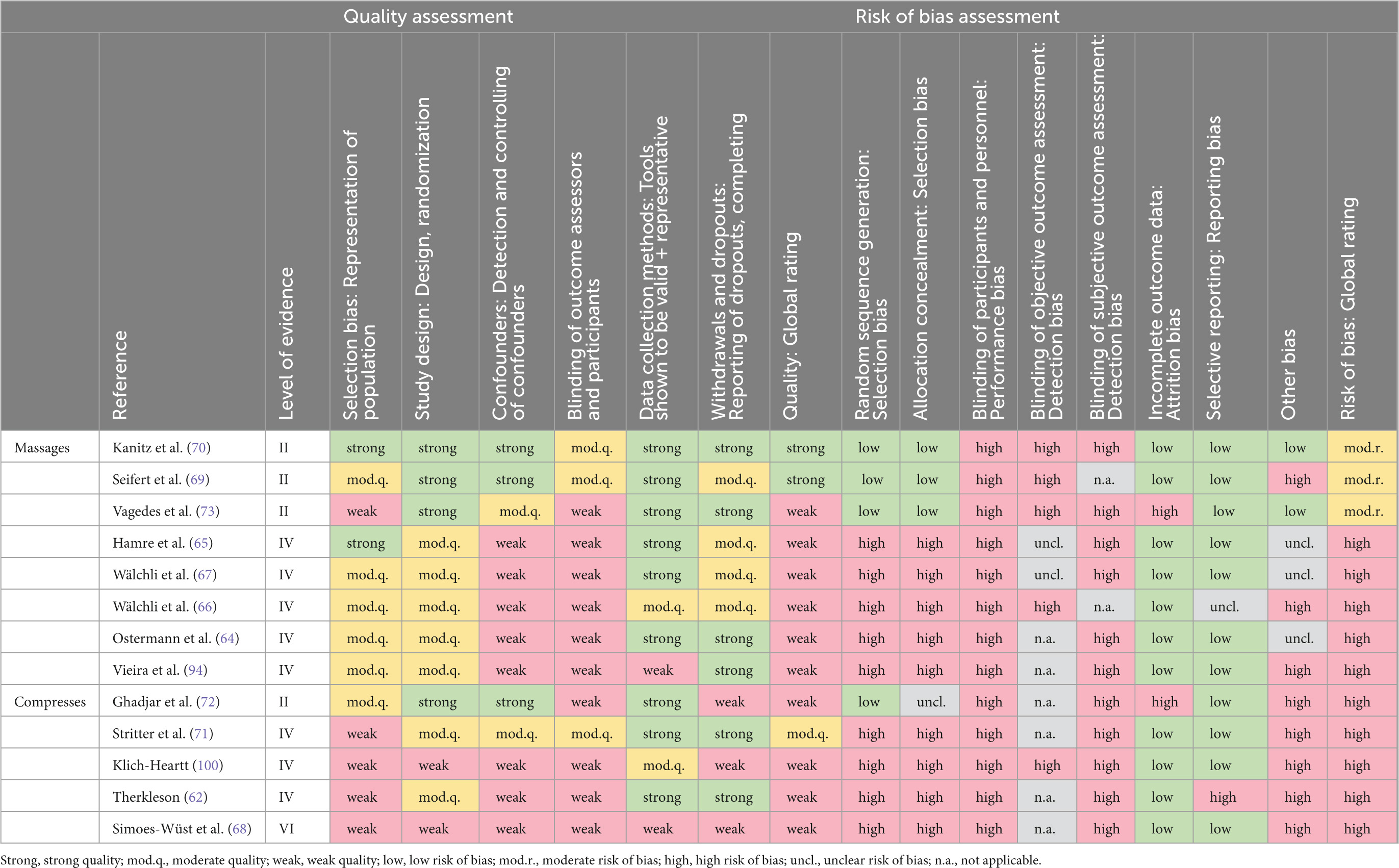
Results: Four RCTs, 7 cohort studies, 1 mixed-methods, 1 retrospective, 4 qualitative studies, 3 case series, and 25 case reports on EAAM were identified. The analysis indicated various effects of EAAM on physiological as well as psychological health indicators and patterns of effect development. Study quality was found to be high for only 2 studies, and moderate for 1 study, and all remaining 45 studies showed a moderate or high risk of bias or were not ratable with used rating tools.
Conclusion: The included studies present a wide range of potential indications for EAAM, while showing methodological drawbacks. To determine whether EAAM can be considered an effective treatment option, clinical studies exploring the effect of different EAAM modalities on defined patient groups are recommended for the future.
Systematic review registration: [https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=214030], identifier [CRD42020214030].
Introduction
Supporting individual patient needs at times goes beyond the limits of conventional medicine. Integrating methods from traditional, complementary, and integrative medicine into treatments may extend therapeutic options and add valuable knowledge on health promotion (1, 2). While biomedical clinical treatments often place great value on the established diagnosis and its specific treatment, integrative treatments offer holistic treatment with a focus on individual health and well-being (3, 4). External applications and massage techniques involving interpersonal attention, touch, and natural substances play a central role in complementary medical systems and are used in various medical conditions (5–9).
Effect mechanisms of external applications
In general, external applications unfold their effects through several different mechanisms: the effect of physical treatment, the touch of the therapist, a calming environment, and the substance on the skin (10). These factors, as well as warmth and olfaction, have been found to be beneficial for social interaction, emotional state, and relaxation (11). While little is known about the effects of external applications, some of the crucial facets of external applications have been subject to research.
Temperature and added substances
The effect of applications with altered temperatures on the organism can be explained by the principle of hormesis, a physiological regulatory reaction to activation by external stimuli or moderate stressors, such as heat or cold (12, 13). These reactions might also result from substances with heating and cooling capacities due to their chemical composition. An example of hormesis on a cellular level was described as the heat shock response, where heat is understood to trigger the organism to activate self-regulatory processes and therefore modulate longevity (14). Natural substances such as essential oils added to external applications are assumed to unfold their aromatherapeutic effects through scent and olfactory receptors on the skin (15). Certain odors may alter endogenous opioid pathways that reduce pain and anxiety and have antibacterial, antifungal, anti-inflammatory, immunomodulatory, and antioxidant effects (16). Positive effects on physiological and psychological parameters have been found with aromatherapy (17, 18), while the effects of aromatherapy on other health indicators have been found to be inconclusive (19). While research on the impact of individual substances on the body is scarce, research within the field of aromatherapy points to challenges in the differentiation of the principle of action of essential oils (20). However, lavender essential oil is presumed to have relaxing and sedative as well as analgesic, anticonvulsive, and neuroprotective capacities (21, 22). Ginger and mustard were found to have warming properties in external hydrotherapeutic treatments (23, 24).
Interpersonal touch and massage
Through the complex system of nerve fibers on the skin, the sense of touch is of great importance for haptic and tactile perception and social interaction (25). At the hormonal level, touch can inhibit the release of cortisol, while it can promote the release of dopamine, serotonin, and oxytocin. Oxytocin, in particular, is associated with modulating pain, increasing wound healing, and reducing stress (11, 26–28). Touching the skin with a certain pace and pressure stimulates pressure receptors. This has shown positive affective valence by stimulating especially C-tactile afferents in the skin, leading to increased vagal activity that may mediate the positive effects of touch (29, 30). Psychological effects of touch are shown in improved emotion regulation and attentiveness as well as decreased stress, depression, and anxiety levels (30, 31). The effects of massage therapy have been the subject of many studies, proposing stress relief and effects on symptoms through physiologic and psychological mechanisms, such as improvement in hypothalamus–pituitary–adrenocortical (HPA) axis function, reduction in heart rate, and increase in blood flow as underlying mechanisms (32), resulting in beneficial effects on various health conditions (9).
External applications in anthroposophic medicine
Anthroposophic medicine (AM) is an integrative medical system developed in Europe around 1900 by Rudolf Steiner and M. D. Ita Wegman. AM is based on the views of the spiritualist movement of Anthroposophy and is intended to be applied in combination with recognized science-based medical methods (33). Aiming at a holistic promotion of health, AM facilitates a multimodal spectrum of methods that are mostly based on experience (34). Medical views in AM are based on the concept of Four Levels of Formative Forces in humans consisting of the physical body and its vital processes (Body), psychological processes (Soul), and the superordinate consciousness (Spirit) (33). According to AM, the human organism also consists of interconnected Threefold Functional Subsystems: One for sensory perception and consciousness (Nerve-Sense System), one for cardiovascular and respiratory function (Rhythmic System), and one for muscular activity and volition (Motor-Metabolic-Limb System) (34, 35). In AM, etiologies and pathogenesis of diseases are seen as abnormal interactions between these different levels and subsystems and are defined as defective processes of maturation or defective impulses leading the organism to disbalance (34–36). The AM methods spectrum includes the use of medications made from natural products, art and movement therapies, counseling, meditation practice, hydrotherapy, and different massage and nursing techniques in the form of external applications from anthroposophic medicine (EAAM). With the intention to synergize the effects of different therapeutic modalities, AM treatment concepts are often multimodal, individually tailored, and take into account the physical, emotional, mental, spiritual, and social situation of a person (34) and are supposed to address vital processes (37). The therapeutic goals of AM recognize and stimulate self-efficacy by enabling flexible autonomic self-regulation as well as psycho-emotional and spiritual self-regulation (34), a concept raised in a similar manner in Salutogenesis where it is described as heterostasis in the body (38, 39).
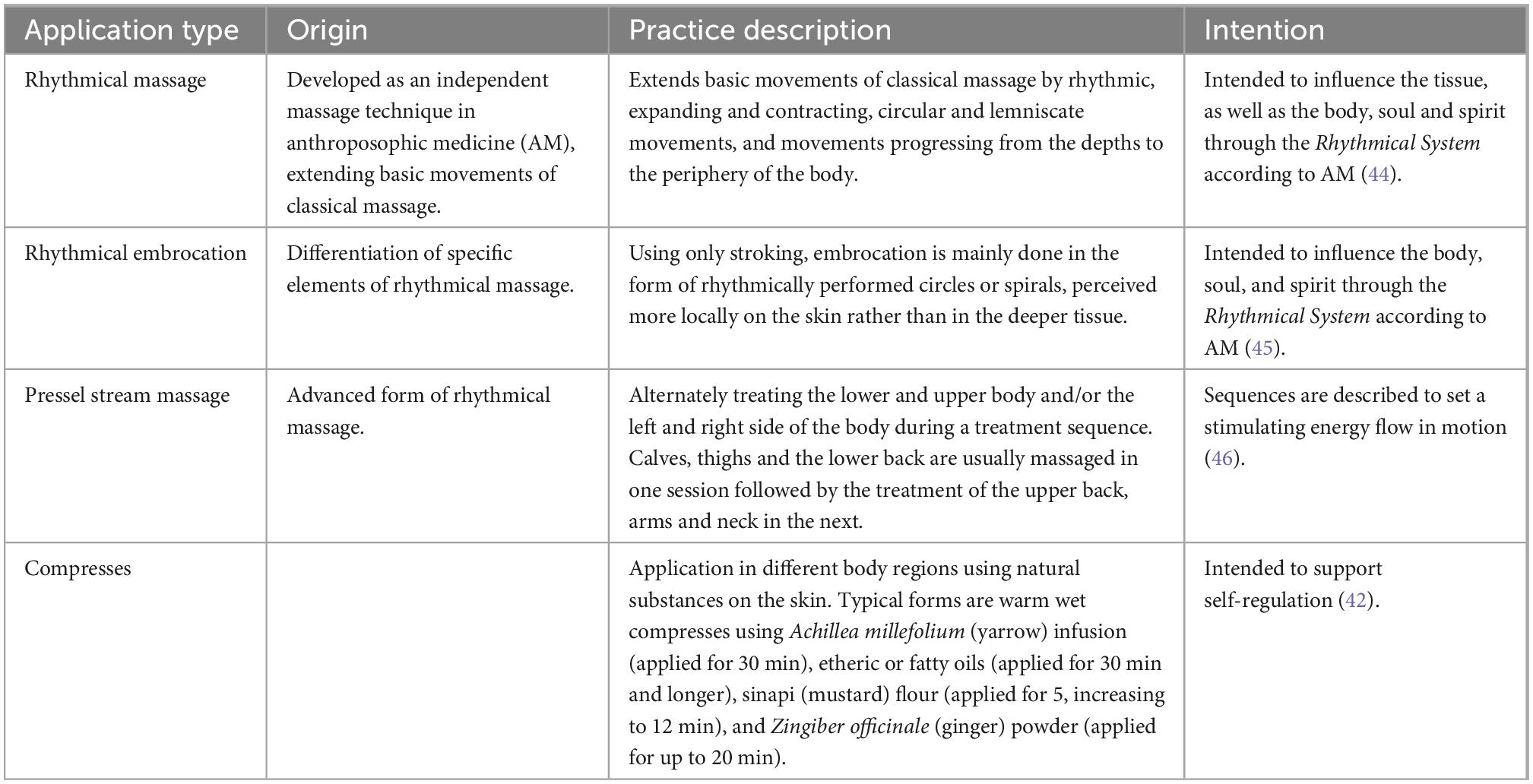
External applications from anthroposophic medicine are intended to stimulate autonomic self-regulation and salutogenic processes by physically influencing the distribution of warmth in the organism, and therefore, integrating the functions of Body, Soul, and Spirit according to AM (40, 41). Applications such as massage including rhythmical massage (RM), rhythmical embrocation (RE), Pressel stream massage (PM), and compress or wrap applications are used. They are performed by trained nurses, physiotherapists, or caregivers. Applications combine interpersonal attention, touch, pressure, and rhythmic movements with temperature with aroma by using tempered water, etheric or fatty oils, essences, tinctures, and ointments on the skin (34). The applications are performed as part of integrative treatment concepts or as single interventions (42, 43). The massages are usually applied 1–2 times a week in units of 30–60 min and cycles of 8–12 treatments, and the duration of the compresses depends on the applied substance (42, 43). All EAAMs are generally followed by a therapeutic resting period of 30 min (42). Table 1 shows an overview of the different types of EAAM.
State of research on external applications from anthroposophic medicine
While literature reviews are available for multimodal application and other treatment modalities of AM (47–51), a systematic review on EAAM has not yet been published and is necessary for establishing the safety and evaluating the effectiveness of the method.
Aims of the review
Given the research gap regarding EAAM, the overall aim of this mixed methods systematic review is to clarify existing applications and indications and to assess the effects and safety of EAAM. This aim has three specific outcomes: the analysis will describe typical indications for EAAM, typical outcomes will be summarized, and the effectiveness and safety will be systematically assessed.
Materials and methods
The review was planned following the principles of a mixed methods systematic review (52) and registered in the International Prospective Register of Systematic Reviews (PROSPERO) (Registration ID: CRD42020214030). The study selection and assessment were conducted in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (53) and following the recommendations of the Cochrane Collaboration (54). Data analysis and synthesis were conducted qualitatively.
Eligibility criteria
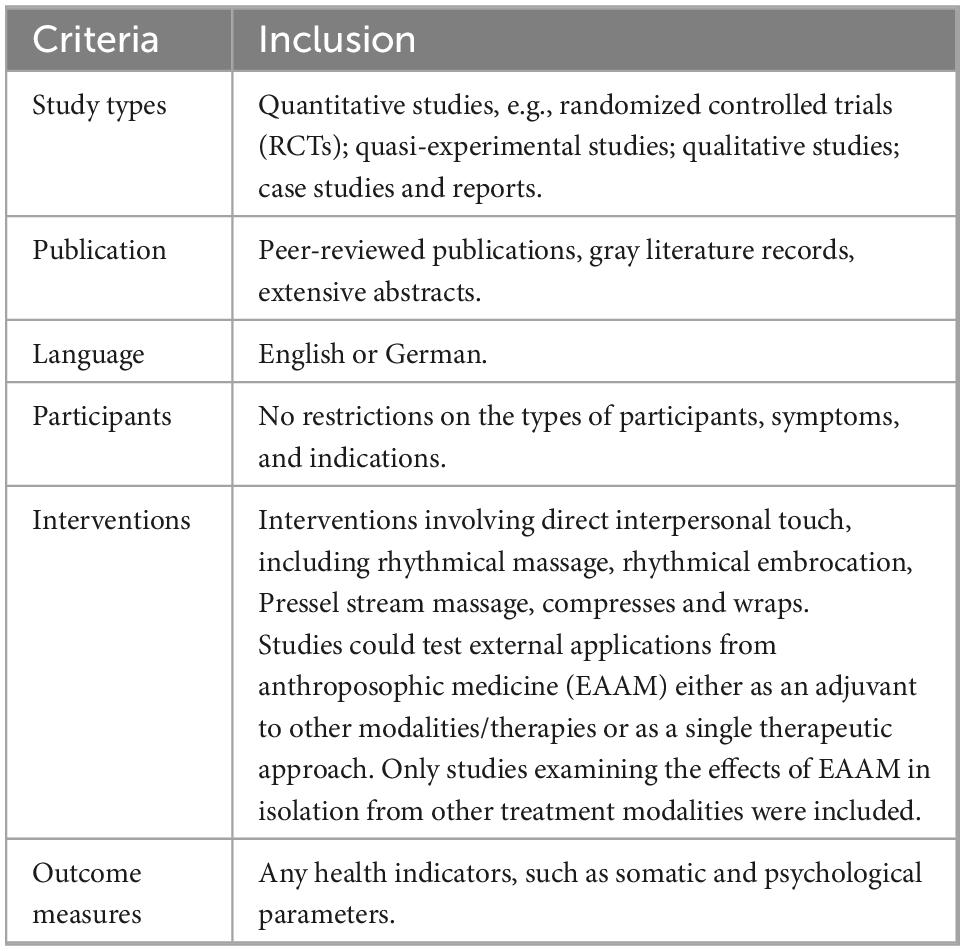
For the description of eligibility criteria, refer to Table 2. Only isolated EAAM interventions were included; multimodal treatments, for instance as part of a wider AM regimen, were excluded. Hydrotherapy interventions were excluded since they do not necessarily involve interpersonal touch. Interventions that used EAAM-like applications but not specified as applications of AM were excluded as well.
Search strategy
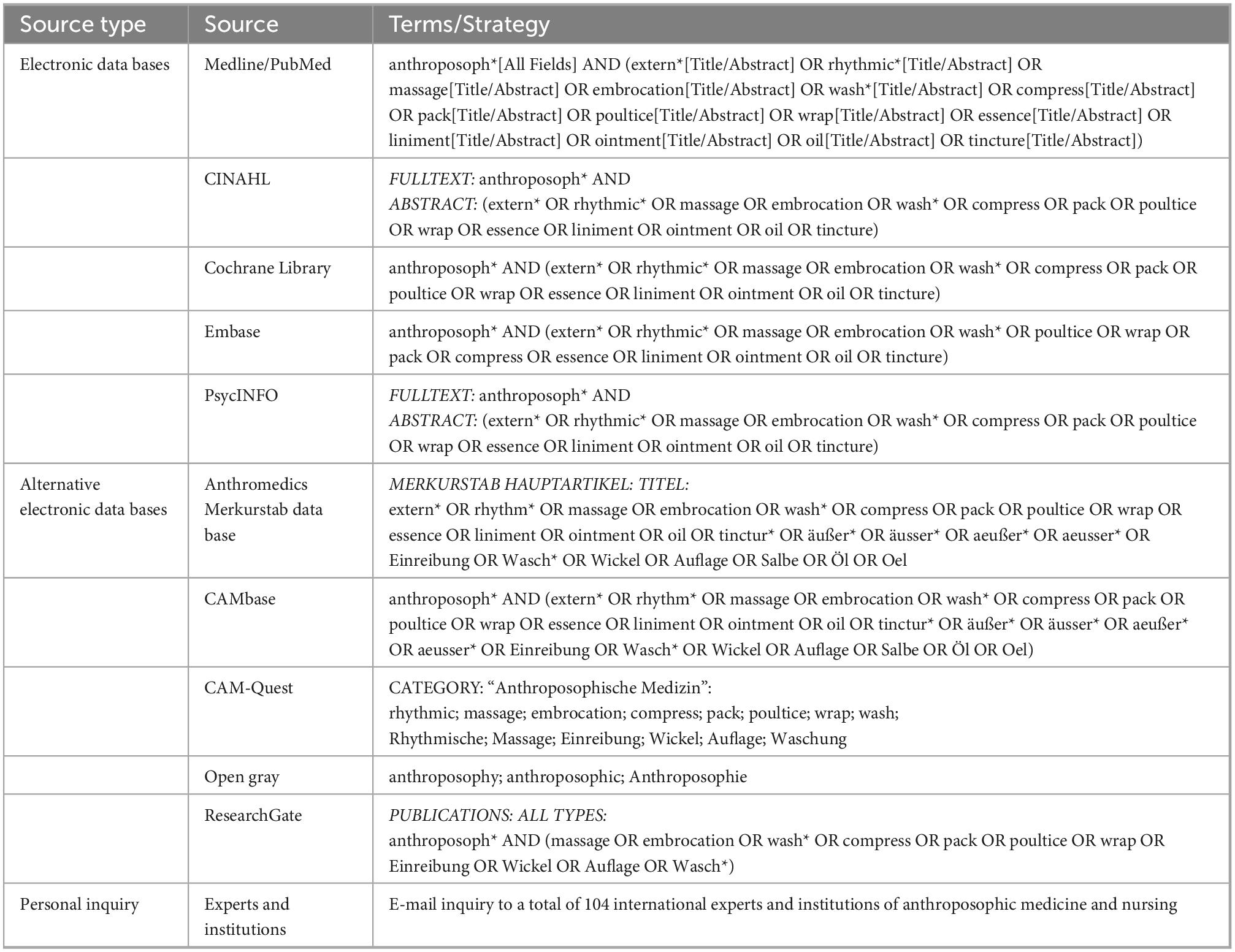
The literature search was built around search terms for “anthroposophic medicine” and “External Applications.” The following electronic databases were searched from their inception through 31 May 2021: Medline/PubMed, CINAHL, the Cochrane Library, Embase, and PsycINFO. The Anthromedics Merkurstab archive1, CAMbase2, CAM-Quest3, ResearchGate4, and the System for Information on Grey Literature in Europe5 for inclusion of gray literature. The search strategy was adapted for each database as necessary and conducted in English and/or German, depending on the database. Additionally, 104 international experts and professional institutions of AM were asked to contribute articles of relevance by direct contact via e-mail from 15 April 2019 and submissions were accepted until 31 May 2021. The complete search strategy for each database is shown in Table 3. Finally, reference lists of identified original articles were searched manually.
Qualitative analysis of studies
Using a Thematic Analysis approach to identify, analyze, and report patterns (themes) within the data, an inductive text analysis of the included records was carried out with MAXQDA2020 (Release 20.4.1) (55). First, the result sections of the included studies were coded according to the described effects on outcomes. Then, key themes regarding the treatment effects were generated based on these codes and summarized in a brief description of the subthemes separately for massage and compress studies. Subsequently, significant effects (p ≤ 0.05) of massages and compresses on participants were summarized for each of the generated themes.
Quality assessment of the individual studies
Since studies of different methodologies were eligible for inclusion the assessment of study quality was undertaken in 3 steps. First, we sorted the studies by the level of evidence. For the detailed quality assessment, the recommended tool for risk of bias assessment of controlled trials in systematic reviews Cochrane Risk of Bias Tool (RoB) (56) was used and supplemented by the Quality Assessment Tool for quantitative studies (QA-Tool) by the Effective Public Health Practice Project (57). This quality assessment provided insight into the available study types and appropriate classification of studies according to their methodology.
All assessments were conducted by IM. Half of the QA-Tool assessments as well as half of the RoB assessments were also performed by JE independently. The remaining assessments were reviewed by JE. Conflicts of rating were discussed until a consensus was reached.
Level of evidence assessment
We first performed a Level of Evidence (LoE) assessment for all included studies, using an adapted version of the Evidence-based Nursing Care Guidelines Scheme (58), p. 7; as a heuristic framework assigning LoE by 7 levels.
Study quality assessment
For the quality assessment of the quantitative studies, we used the QA-Tool. The tool assesses study quality according to a strong, moderate, or weak rating quality along with the following domains: selection bias, study design, confounders, blinding, data collection methods, withdrawals and dropouts, intervention integrity, and analyses (57). Studies with no weak component rating were rated as having overall strong quality, studies with one weak component rating were rated as having moderate quality, and studies with two or more weak ratings were rated as having weak quality.
Risk of bias assessment
The RoB tool assesses the risk of bias in the domains of selection bias, performance bias, attrition bias, reporting bias, and detection bias using 8 criteria (56). Each criterion in the quantitative studies was rated as low risk, unclear risk, or high risk of bias. To provide comparability with the QA-tool, we supplemented the RoB-rating with an assessment of the overall risk of bias. Studies that met at least six of the criteria were rated as having an overall low risk of bias, studies that met four to five criteria were rated as having a moderate risk of bias, and studies that met zero to three criteria were rated as having a high risk of bias.
Results
Literature search
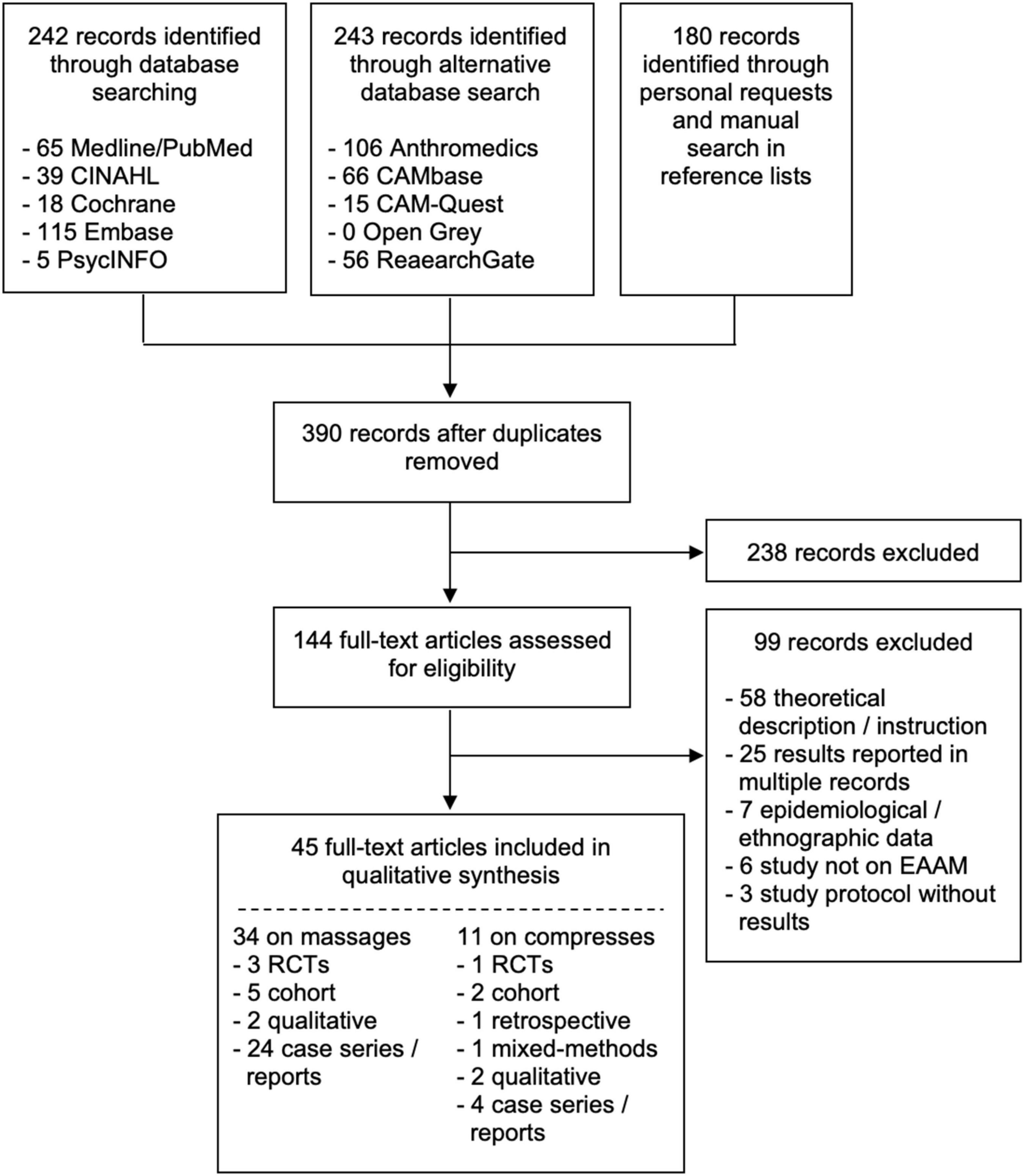
The literature search revealed a total of 665 records, resulting in 390 non-duplicate records of which 238 were excluded because they did not report on EAAM studies in English or German. Out of 144 full-texts assessed for eligibility, 99 articles were excluded because they were theoretical descriptions or instructions of EAAM (58 records), were double publications on the same study (25 records), reported epidemiological or ethnographic data (7 records), were not studied on EAAM (6 records), or were study protocols without results (3 records).
Finally, 45 studies were included, out of these 34 studies were on massage interventions and 11 were on compresses interventions. On massages, there were 3 RCTs, 5 cohort studies, 2 qualitative studies, and 24 case reports or series. On compresses, there were 1 RCT, 1 mixed methods study, 2 cohort studies, 1 retrospective study, 2 qualitative studies, and 4 case reports or series. The flowchart of the results of the literature search is depicted in Figure 1.
Publication characteristics
Of the 45 studies, 18 were published in peer-reviewed journals (59–76), and 27 studies were records of gray literature (77–103). Fifteen studies were only available in the form of an abstract (77, 80, 82, 85, 87, 88, 90–95, 97, 101, 102).
The first included study was published in 2001, in fact as the second edition of a study originally published in 1992 (98). The number of studies published each year reached a peak between the years 2010 and 2016 (Figure 2).
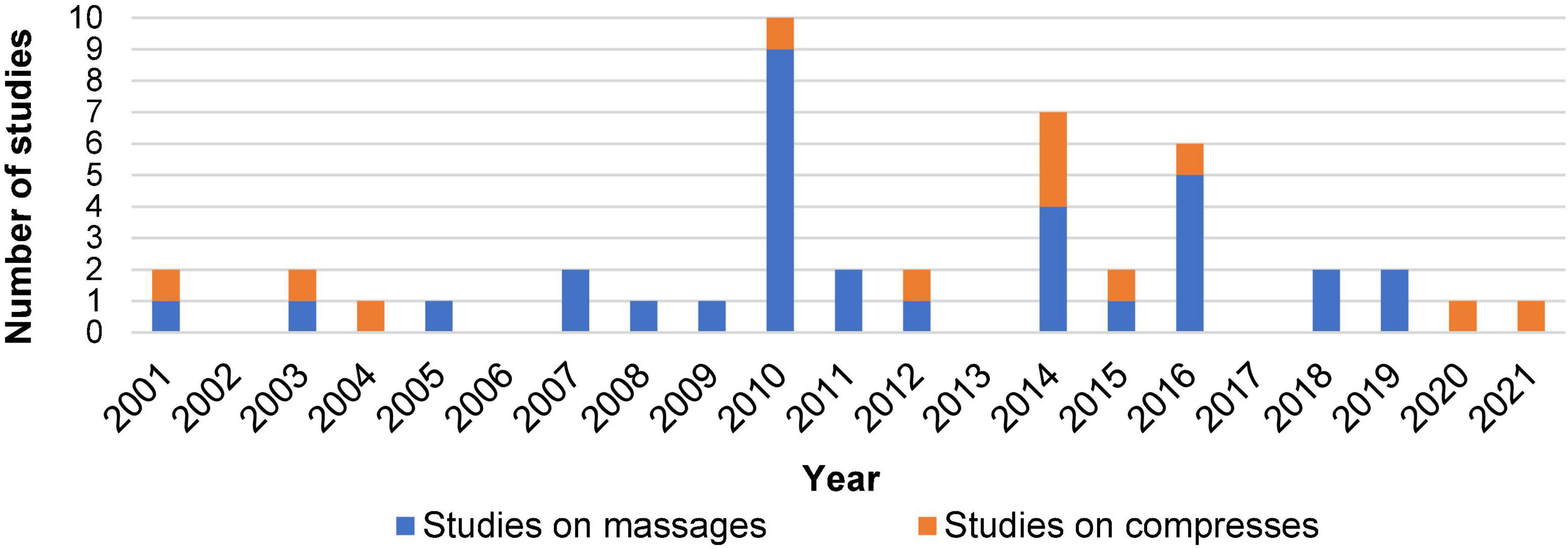
Figure 2. The number of studies on EAAM in a given year reported in absolute terms. Studies exploring a mixed intervention of massages and other application types were counted as massage studies.
Study characteristics
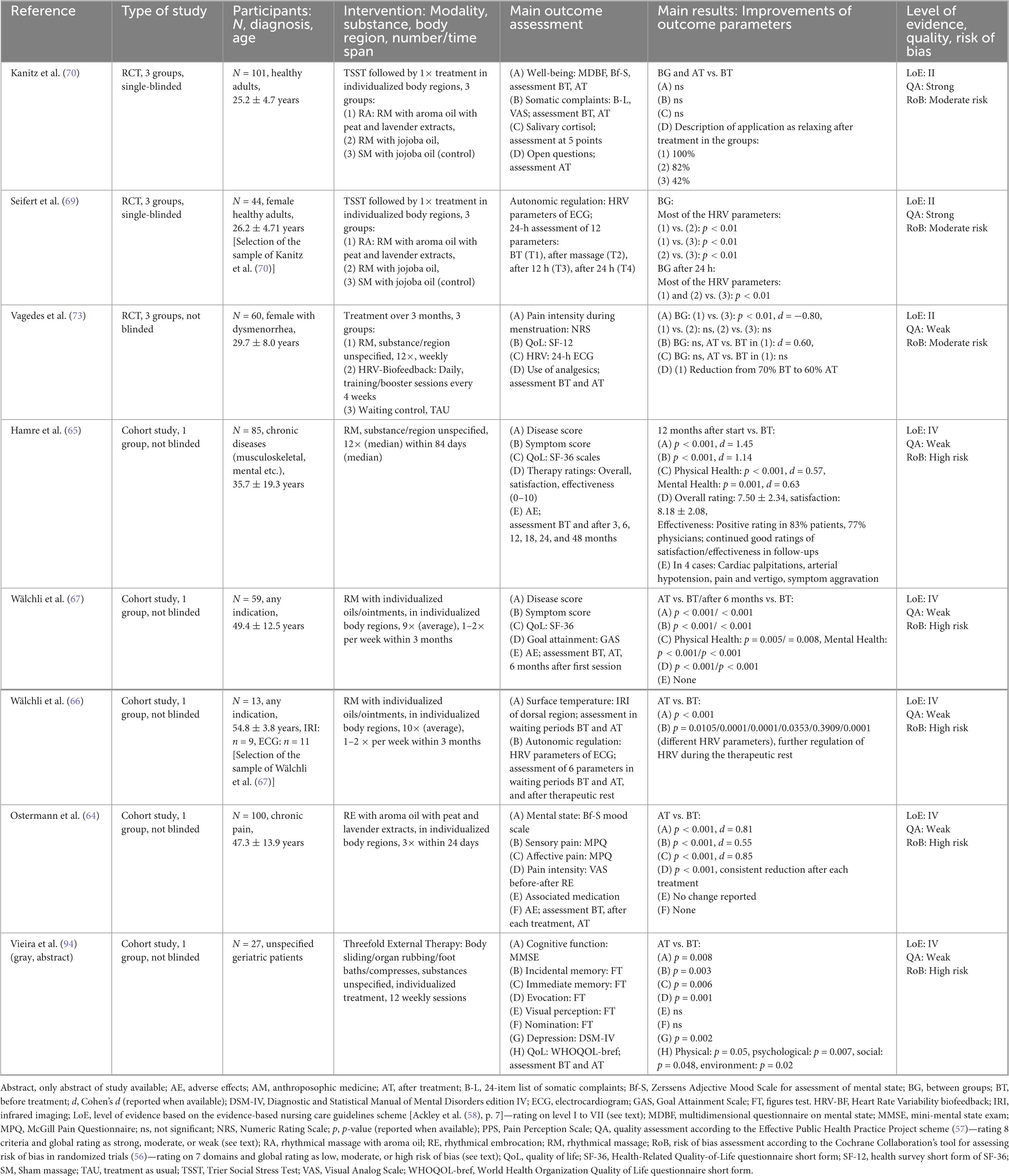
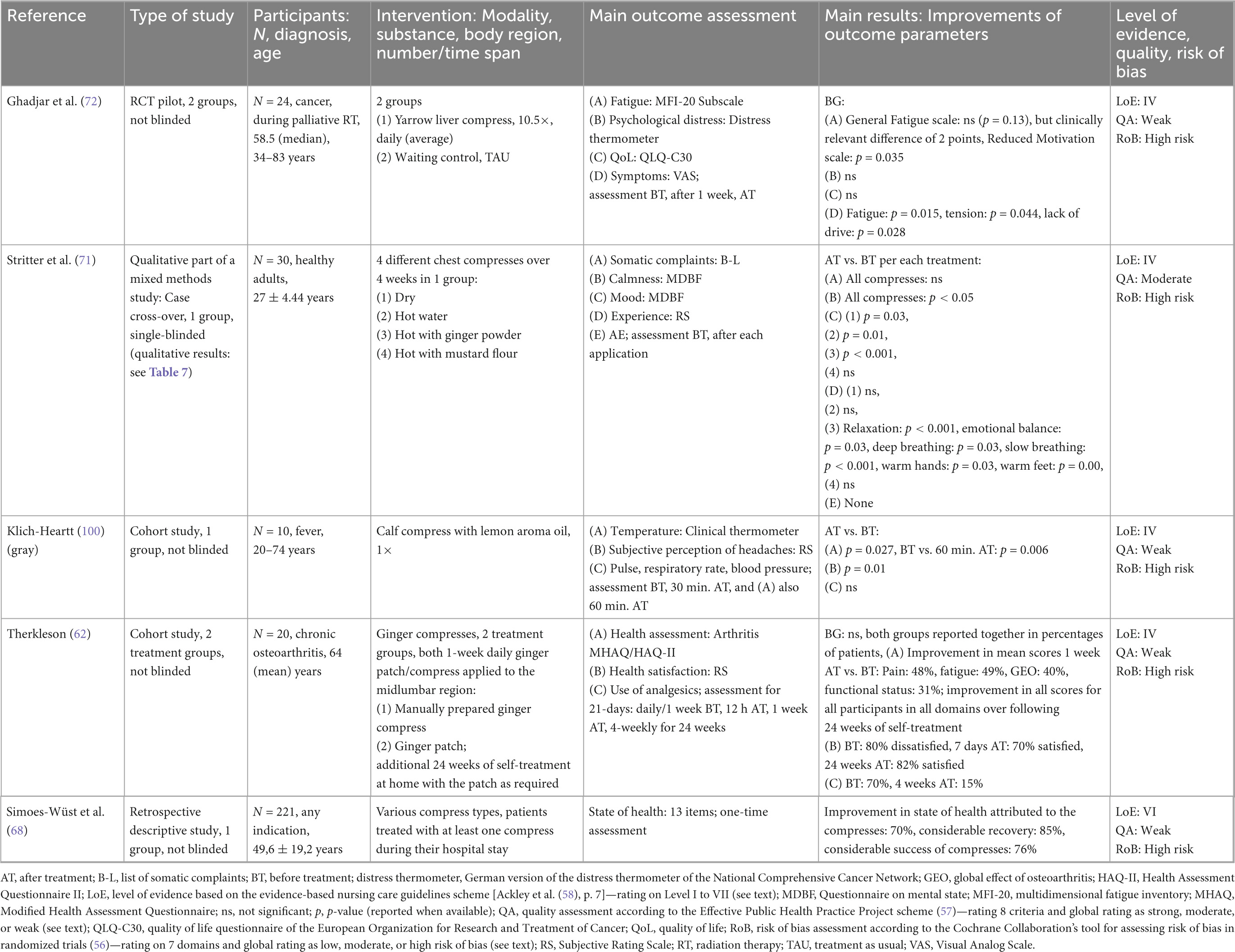
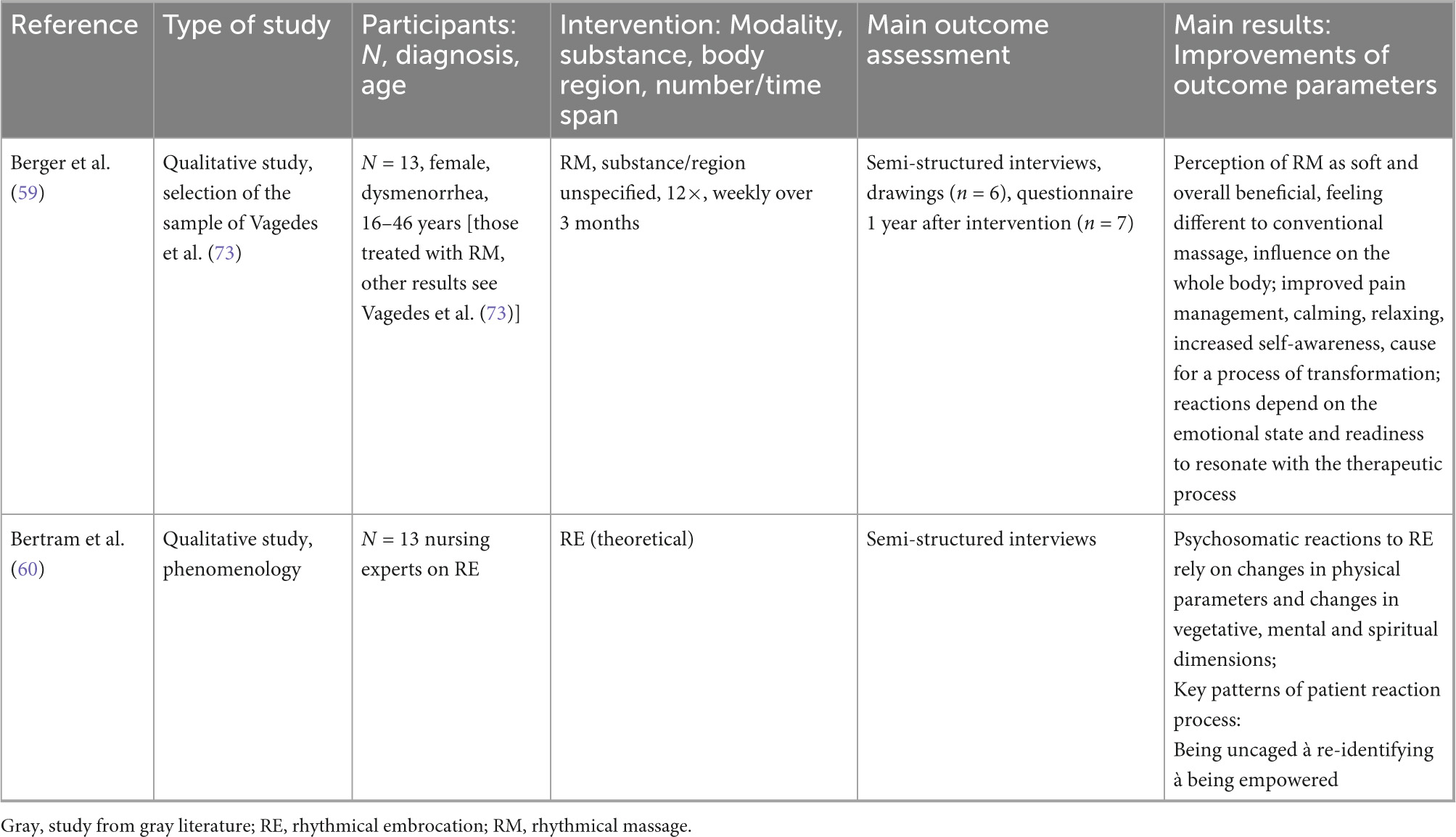
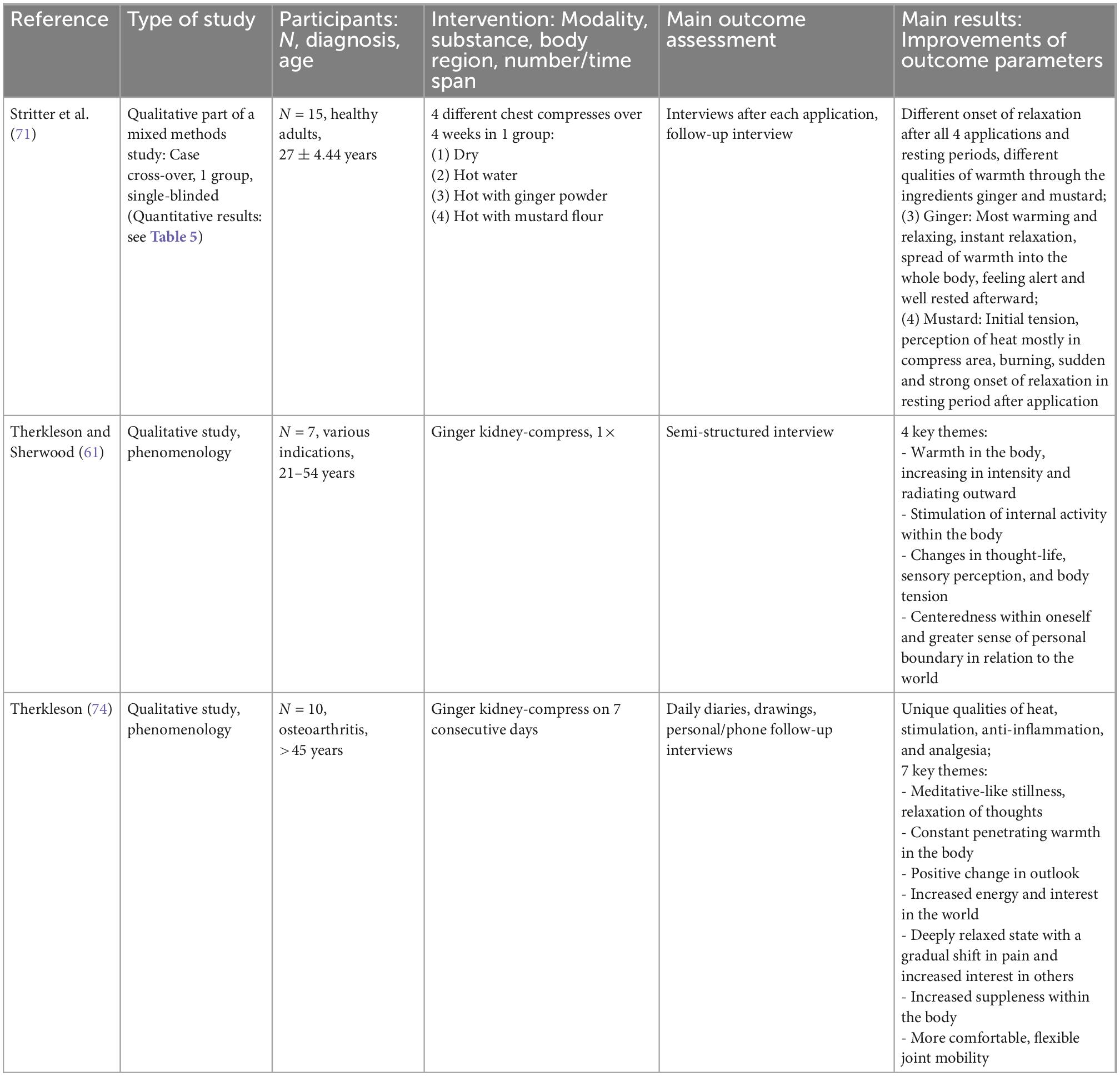
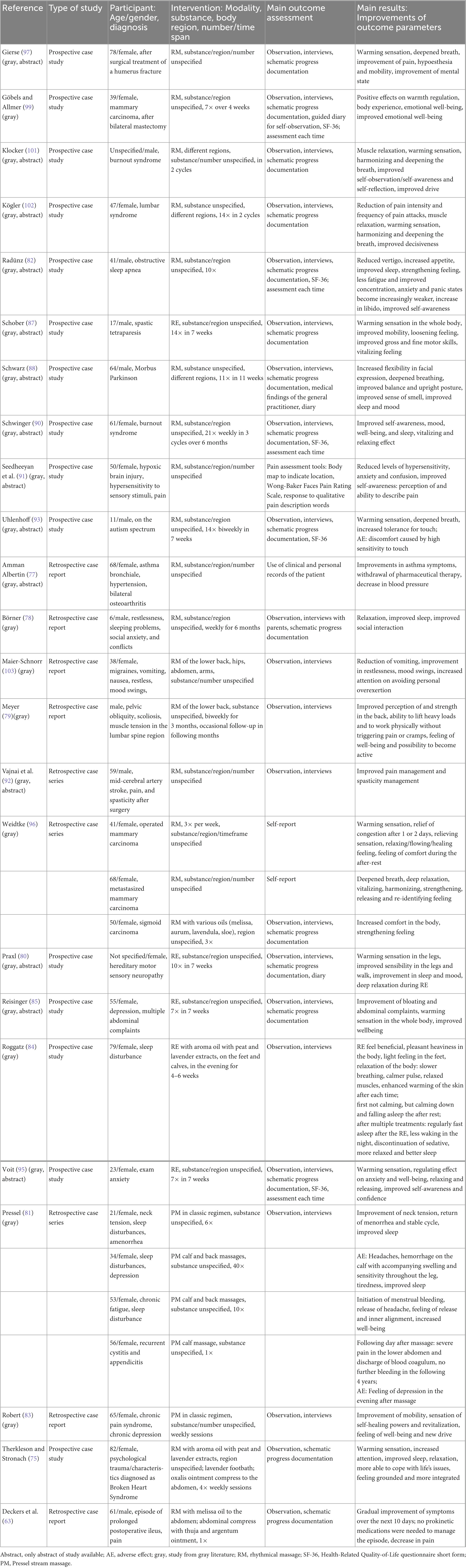
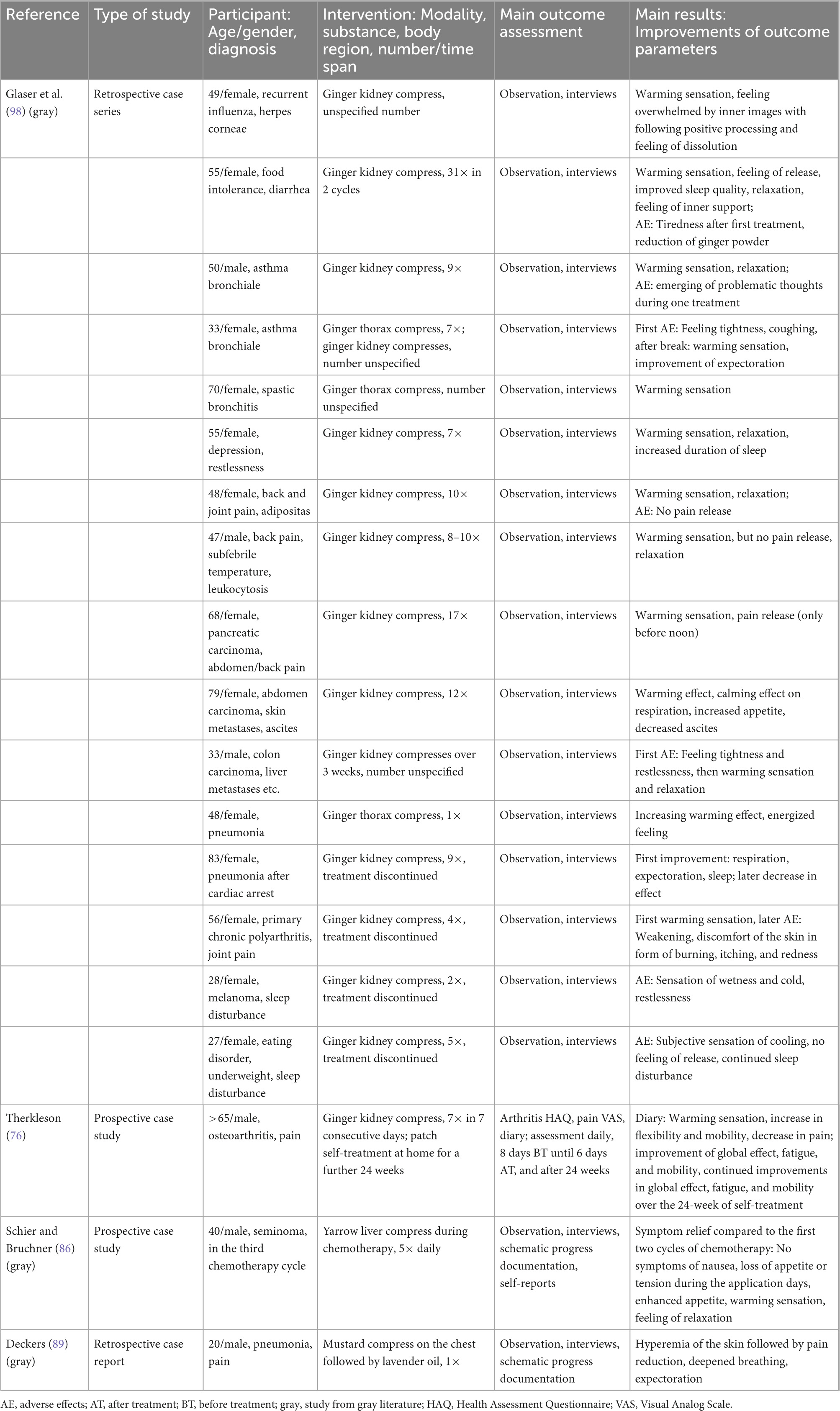
Characteristics of the study methodologies, samples, interventions, outcome assessments, and results are shown in Tables 4–9. The studies in the result tables are sorted by their assigned LoE and grouped in tables per studies on massages and studies on compresses.
Setting and participant characteristics
Of the 45 included studies, 21 studies originated from Germany (59, 60, 63–65, 69–73, 78, 79, 81, 83, 84, 86, 89, 96, 98, 99, 103), 15 studies originated from Switzerland (66–68, 80, 82, 85, 87, 88, 90, 93, 95, 101, 102), 5 studies originated from New Zealand (61, 62, 74–76), 2 studies originated from the United Kingdom (91, 92), 1 study originated from Brazil (94), and 1 study originated from the United States (100).
Participants were recruited during inpatient treatment in integrative AM clinics in 10 studies (63, 68, 76, 86, 89, 91, 92, 96, 98, 99), during outpatient treatment in integrative AM clinics in 3 studies (64, 66, 67), during inpatient treatment in conventional or unspecified clinics in 7 studies (61, 62, 72, 74, 75, 94, 100), in private practices in 2 studies (78, 81), mainly in primary care practice in 1 study (65), through physician referral or advertisement in 2 studies (59, 73), and through advertisement at a university hospital in 3 studies (69–71). In 17 studies, the recruitment of participants was not specified. All EAAMs to patients were applied complementary to their respective usual treatment regimen if there was one.
In total, 45 studies reported results on 815 participants. Seventy of them participated in different study parts and are, therefore, part of multiple publications. The reported age of the participants ranged from 6 to 83 years, with some studies reporting mean age, some median age, some age ranges, and some not reporting the age of the participants at all. Of the participants in all studies, 74% were female participants and 20% were male participants. In 6% (3 studies), the authors did not report the gender of the participants (60, 74, 94).
Seven studies included patients with various symptoms among the participants (61, 66–68, 83, 94, 98). One study included patients with various chronic diseases, e.g., musculoskeletal or mental diseases (65), and one study included patients with chronic pain (64). Four studies included patients with cancer, e.g., with nausea and fatigue (72, 86, 96, 99). Three studies were on patients with gynecological issues, e.g., with dysmenorrhea or amenorrhea (59, 73, 81). Five studies included patients with neurological disorders, such as hypersensitivity to sensory stimuli after brain injury (91), migraines (103), Morbus Parkinson (88), pain and spasticity after artery stroke (92), and sensory neuropathy (80). Seven studies included patients with orthopedic diseases, of these, 3 studies were on patients with chronic osteoarthritis (62, 74, 76), 2 on patients with spinal disorders (79, 102), 1 on a patient after surgery on humerus fracture (97), and 1 on a pediatric patient with spastic tetraparesis (87). Three studies included patients with pulmonary diseases, such as pneumonia (89), asthma bronchiale (77), and sleep apnea (82). Eight studies included patients with psychiatric or psychological symptoms, out of these, there were 2 studies on patients with burnout syndrome (90, 101); the other was on a geriatric patient with sleep disturbance (84) and on patients with depression and concurrent abdominal complaints (85), exam anxiety (95), psychological trauma (75); 1 included a pediatric patient with restlessness (78) and 1 included a pediatric patient on the autism spectrum (93). One study included patients with acute fever (100) and 1 study included a patient with prolonged postoperative ileus (gastroenterological) (63). Three studies were on healthy adults (69–71), and 1 study performed a qualitative analysis of interviews with nursing experts (60).
Intervention characteristics
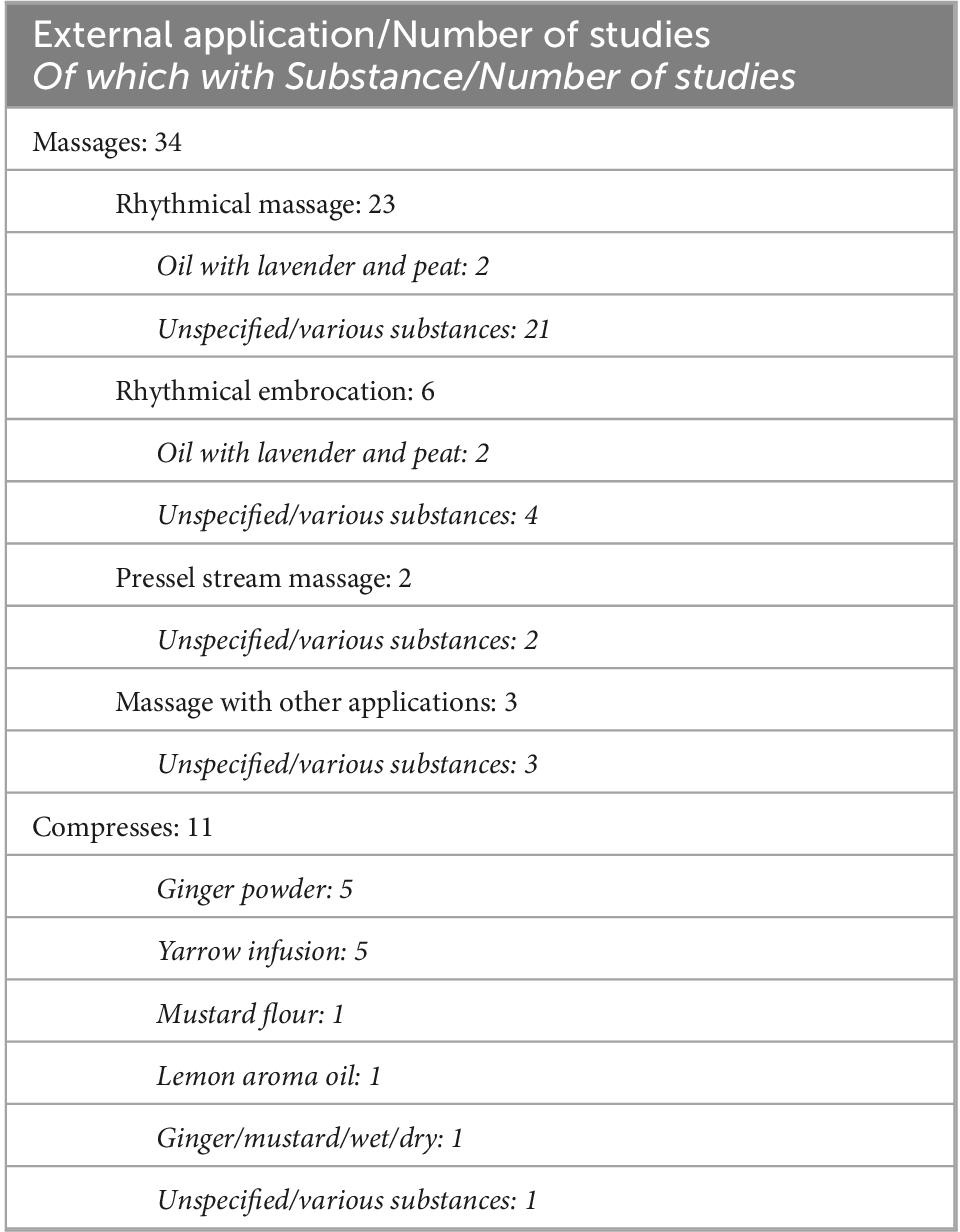
Of the 45 studies, 34 were on massage interventions and 11 on compress interventions. Table 10 describes the distribution of studies per application type and substance.
Of the 34 massage studies, 23 studies were on RM, of which 2 studies were on RM with aroma oil with peat and lavender extracts (69, 70), and 21 studies were on RM with unspecified or various substances (59, 65–67, 73, 77–79, 82, 87, 88, 90–93, 96, 97, 99, 101–103). Six studies were on RE of which 2 were on RE with aroma oil with peat and lavender extracts (64, 84) and 4 were on RE with unspecified substances (60, 80, 85, 95). Two studies were on PM with unspecified substances (81, 83). Three studies were on massages mixed with compresses and/or footbaths: 1 using various aroma oils and ointments (63), 1 using aroma oil and ointment with peat, lavender, and oxalis extracts (75), and 1 using unspecified substances (94).
Of the 11 studies on compresses, 5 studies were on ginger powder compresses (61, 62, 74, 76, 98), 2 on yarrow infusion compresses (72, 86), 1 on a mustard flour compress (89), 1 on lemon aroma oil compresses (100), and 2 on differing compresses, 1 comparing ginger and mustard with neutral dry and wet compresses (71), and 1 describing effects of various compresses (68).
Of the 4 RCTs, 2 compared RM with aroma oil with peat and lavender extracts to RM with neutral oil and sham massage with neutral oil (69, 70), 1 compared RM with heart rate variability biofeedback and treatment as usual (73), and 1 compared yarrow liver compress therapy to treatment as usual (72). One study compared 4 compresses (mustard, ginger, hot water, and hot dry) with different substances within one treatment group (71), and 1 study used different forms of application for ginger compresses (manual application vs. patch) (62). The other studies did not use comparisons or control groups.
Outcome measures
The 13 included quantitative studies focused on both the subjective assessment of physical outcomes such as symptom manifestation and therapy effectiveness and objectively measured physical and psychological outcomes.
Physical measures
Physiological outcomes were assessed using subjective instruments by the 24-Item List of Somatic Complaints (B-L) (70, 71), by measuring the manifestation of disease and symptoms by Visual Analog Scales (70, 72), disease scores and symptom scores (65, 67), and a questionnaire for the state of health assessment (68). Health assessment in patients with osteoarthritis was conducted by Modified Health Assessment Questionnaires for arthritis (MHAQ, HAQ-II) (62), and fatigue in a patient with cancer was assessed using the multidimensional fatigue inventory (MFI-20) (72). Pain intensity was assessed by a numeric rating scale in patients with dysmenorrhea (73), and sensory and affective pain in patients with chronic pain were assessed by the McGill Pain Questionnaire (MPQ), while pain intensity was assessed with a Visual Analog Scale (64). The intensity of headaches during fever was assessed using a rating scale for subjective assessment by the patients (100). The use of analgesics and other medication was assessed in 3 studies (62, 64, 73). Overall therapy effectiveness was assessed in 3 studies using rating scales (62, 65) and the Goal Attainment Scale (67).
Objective measures of physiological parameters assessed autonomic regulation using heart rate variability data from electrocardiogram assessments in 3 studies (66, 69, 73). Body surface temperature was assessed by infrared imaging of the dorsal region in 1 study (66). Body temperature by a clinical thermometer and also pulse, respiratory rate, and blood pressure were assessed in patients with fever (100). One study assessed salivary cortisol (70).
Psychological assessments
The mental state was assessed in 3 studies by the Multidimensional Questionnaire on Mental State (MDBF) (70, 71) and Zerssens Adjective Mood Scale (Bf-S) (64, 70). One study used the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) to assess symptoms of depression (94) and 1 study used the German version of the distress thermometer of the National Comprehensive Cancer Network to assess psychological distress (72). As outcome assessments for the cognitive state, the Mini-mental State Exam (MMSE) and Figures Tests (FT) were used (94). Rating scales were used to assess the experience of relaxation and warmth (71) and additional open questions were used to assess the remarks of participants (70).
Physical–psychological assessment
Quality of life (QoL) was assessed by Health-Related Quality-of-Life questionnaire short forms SF-36 (65, 67) and SF-12 (73), World Health Organization Quality of Life questionnaire short form (WHOQOL-bref) (94), and the Quality of life questionnaire of the European Organization for Research and Treatment of Cancer (QLQ-C30) (72).
Assessment of long-term effects
All quantitative studies assessed short-term effects, while 3 studies also assessed long-term effects (62, 65, 67).
Outcome assessment in qualitative studies and case reports
The qualitative studies included interviews (59–61, 71, 74). The case reports mainly used observations and interviews for outcome assessment, while some case studies additionally used questionnaires for outcome assessment, such as the Health-Related Quality-of-Life questionnaire short form (SF-36) (82, 95, 99), the Arthritis Health Assessment Questionnaire (HAQ) and a Visual Analog Scale for pain assessment (76), and diaries (76, 80, 88, 99) for progress documentation. One case series exclusively used patient self-reports in 2 cases (96).
Assessment of adverse effects and safety
While most studies assessed positive effects on the patients, there were 4 quantitative studies (62, 64, 65, 67) and the mixed-methods study (71) which additionally assessed adverse effects. Three case series and reports reported adverse effects (81, 93, 98).
Outcomes
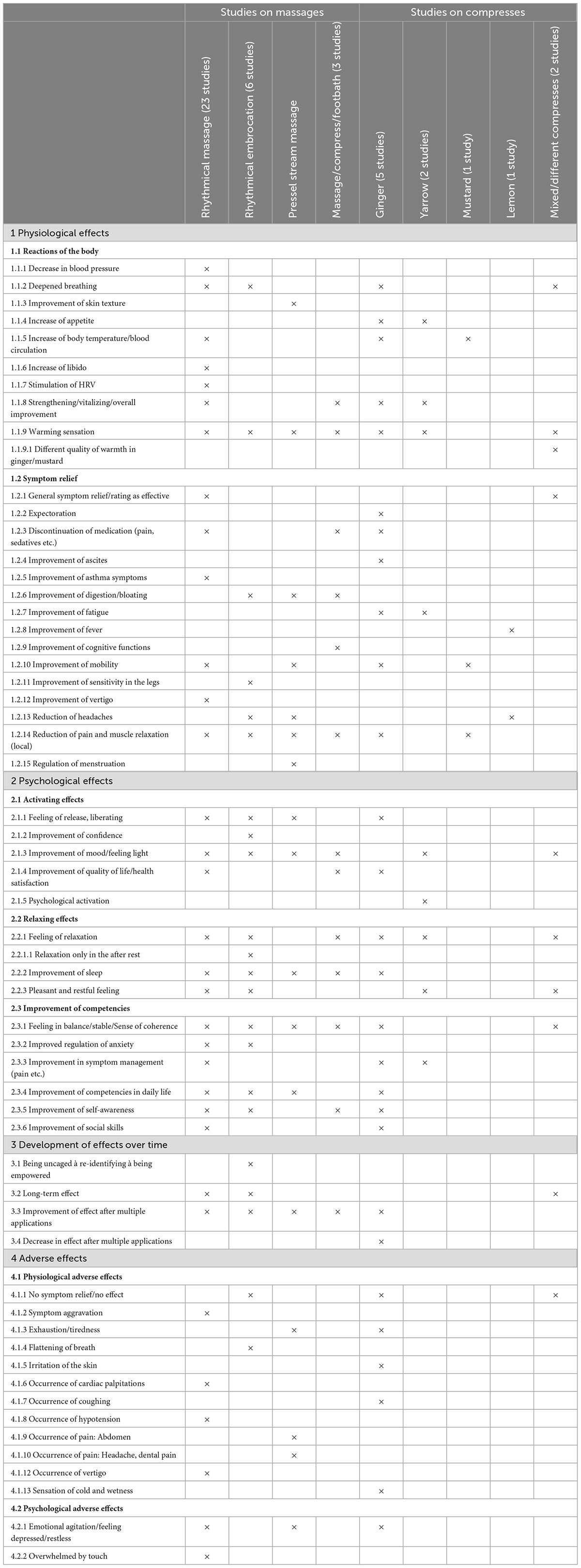
Effect themes
The Thematic Analysis of the 45 studies resulted in 4 themes describing different areas of effects (1) physical effects, (2) psychological effects, (3) effect development over time, and (4) adverse effects. The 4 themes contained 7 subthemes. An overview of the themes and subthemes is shown in Table 11, where study clusters are marked when a theme was extracted from a study cluster at least once. Each of the developed themes could be extracted from the outcomes of the massage and compress studies with different characteristics and in some studies with significant effects, as described below.
Physical effects of massages
In the studies on massage interventions, physiological effects were presented in the form of various reactions of the body and symptom relief. Reactions of the body showed in form of improvement of general condition and vitalization (59, 63, 65, 67, 82, 83, 90, 96, 99, 102), a warming sensation in the whole body (75, 80, 81, 84, 85, 87, 95, 96, 101), deepened breathing (84, 87, 88, 93, 95, 96, 102), an increase in body temperature and blood circulation (66, 87, 93, 97, 101, 102), a decrease in blood pressure (77), a stimulation of heart rate variability (HRV) (66, 69), an improvement of skin texture (81) and an increase in libido (82). Symptom relief after massage interventions was shown in the form of general symptom relief and general rating of applications as effective (65, 67), a reduction in local pain and muscle relaxation (63, 64, 73, 81, 83, 97, 99, 101, 102), an improvement of mobility (83, 87, 88, 96, 97), improvements of digestion and bloating (63, 81, 85), reductions in headaches (81, 95), improvements in asthma symptoms (77), an improvement of sensitivity in the legs (80), an improvement of vertigo (82), a regulation of the menstrual cycle (81), improvements in cognitive function (94), and the possibility for discontinuation of analgesia and sedatives (63, 77).
Significant effects of massages on physical outcomes
The quantitative studies on massage interventions revealed significant effects for some of the stated physiological outcomes: RM treatment for 3 months compared to treatment as usual (TAU) led to a significant reduction in pain intensity in patients with dysmenorrhea between groups (p < 0.01) (73). RM led to a significant pre-post reduction in disease manifestation (short-term: p < 0.001/long-term: p < 0.001) and symptom scores (short-term and long-term: p < 0.001) in patients with various indications (67) and to a significant reduction in disease manifestation (p < 0.001) and symptom scores (p < 0.001) in patients with chronic disease (65). After RM, the patients’ rating of therapy goal attainment was also significantly higher (short-term and long-term: p < 0.001) in the various indications sample (67). RE had significant positive effects on sensory (p < 0.001, d = 0.55) and affective (p < 0.001, d = 0.85) pain, and pain intensity (p < 0.001), in patients with chronic pain (64). An intervention using embrocations together with compresses and footbaths led to a significant increase in cognitive function (p = 0.008) and incidental (p = 0.003) and immediate (p = 0.006) memory as well as an increase in evocation capacity (p = 0.001) in elderly patients (94). Significant positive effects in autonomic regulation (assessed by HRV) between treatment with RM with aroma oil over a treatment with RM with neutral oil (p < 0.01 in most HRV parameters) and over a treatment with sham massage (p < 0.01 in most HRV parameters) were evident in healthy adults (69). RM also had significant positive effects on autonomic regulation (HRV) (p < 0.001 in most HRV parameters) and surface temperature (IRI) (p < 0.001) in patients with various indications (66).
Physical effects of compresses
Effects on physical parameters in the studies on compress interventions were extracted as reactions of the body such as an improvement of general condition and vitalization (61, 62, 74, 98), warming sensations in the whole body (61, 71, 74, 76, 98) that were described as a different quality of warmth in ginger and mustard (71), deepened breathing (71, 98), an increase in appetite (86, 98), and increases in body temperature and blood circulation (61, 76, 89, 98, 100). Compresses led to symptom relief in the form of general symptom relief and rating of treatments as effective (68), improvements in fatigue symptoms (62, 72), improvements in mobility (62, 74, 76, 89), reduction in local pain and muscle relaxation (62, 74, 76, 89, 98), a reduction in headaches (100), a stimulation of expectoration (98), and improvements of fever (100) and ascites (98).
Significant effects of compresses on physical outcomes
Significant effects of compress interventions on physical outcomes were significantly reduced fever (measured temperature) (after treatment: p = 0.027, after 60 min: p = 0.006) and headaches (p = 0.01) after lemon compresses (100). After ginger compresses, significant effects on healthy adults were deepened breathing (p = 0.03), slowed breathing (p < 0.001), and the sensation of warmer hands (p = 0.03) and warmer feet (p < 0.001) (71).
Psychological effects of massages
The effects of massages on psychological outcomes were presented as activating effects such as an improved mood and feeling light (64, 67, 70, 80–82, 87, 94–97, 99, 102), a feeling of release and liberation (60, 81, 87, 95, 96), improvements in QoL and health satisfaction (73, 82, 94, 99, 101), and improved confidence (95). The relaxing effects of massages were improvements in sleep (75, 78, 80–82, 84, 88, 90, 99), a pleasant restful feeling (59, 65, 78, 84, 85, 90, 99), and a feeling of relaxation (59, 70, 75, 80, 84, 87, 88, 90, 95, 96, 99). Some participants described the effects of improved competencies through massages, like strengthening through an increased perception of balance and meaning (60, 75, 80, 81, 83, 85, 95, 96, 99), an improved self-awareness (59, 70, 75, 79, 84, 87, 88, 90, 95, 96, 99, 103), an improvement of competency in daily life (59, 60, 79, 81, 82, 87, 88, 93, 95, 102, 103), an improved ability to regulate anxiety (82, 91, 95, 102), improved capacities for symptom management (79, 91, 92, 97), and improved social skills (78, 82, 90).
Significant effects of massages on psychological outcomes
Rhythmical massage had significant positive effects on QoL in patients with chronic diseases (physical and mental: p < 0.001) (65), dysmenorrhea (no p-value reported, d = 0.60) (73) and in patients with various indications (physical short-term: p = 0.005/physical long-term: p = 0.005, mental short-term: p < 0.001/mental long-term: p < 0.001) (67). RM significantly improved mood (p < 0.001, d = 0.81) in patients with chronic pain (64). An intervention using embrocations along with compresses and footbaths led to a significant increase in QoL (Physical: p = 0.05, psychological: p = 0.007, social: p = 0.048, environment: p = 0.02), and a significant decrease in depression (p = 0.002) in elderly patients (94).
Psychological effects of compresses
The effects of compresses on psychological outcomes were extracted in the form of activating, relaxing effects, and effects of competencies as well: After compresses, patients described improvement in mood and feeling light (71, 86), feelings of release and liberation (98), improvements in QoL and health satisfaction (62), and a feeling of psychological activation (72). Feelings of overall relaxation (71, 72, 74, 98), pleasant and restful feelings (68, 86), and an improvement of sleep (98) were described after compressing as well. Furthermore, strengthening through an increased perception of balance and meaning (71, 76), improvements in symptom management (76, 86), daily life competencies (61, 74), self-awareness (61), and social skills (74) also showed after compress interventions.
Significant effects of compresses on psychological outcomes
Daily yarrow liver compresses for 7–14 days led to a significant reduction in fatigue (p = 0.015), tension (p = 0.044), lack of drive (p = 0.028), and an improvement of the scale on reduced motivation in fatigue (p = 0.035) compared to TAU in patients with cancer during radiation therapy (72). After ginger compresses, healthy adults were significantly more relaxed (p < 0.001) and emotionally balanced (p = 0.03) (71). Their mood was significantly improved after dry compresses and compresses using hot water and ginger (all compresses: p < 0.05), and calmness was significantly improved after dry, hot water, ginger, and mustard compresses (all compresses: p < 0.05) (71).
Development of effects in massage
In the massage studies, development of effects over time was described in manifesting an increase of effects after multiple applications in various studies (63, 82–84, 96, 99) as well as long-term effects (65–67, 85, 88, 103), and a pattern of effect consisting of a feeling of liberation, followed by a feeling of re-identification and a feeling of empowerment (60).
Significant long-time effects of massages
One study on patients with various indications reported significant long-term effects in a pre-post reduction in disease manifestation (p < 0.001), symptom scores (p < 0.001), therapy goal attainment (p < 0.001), and QoL (physical: p = 0.005, mental: p < 0.001) (67).
Development of effects in compresses
The studies on compresses depicted a development of effects over time as well, shown in an increase of effects after multiple applications (62, 76) as well as a decrease of effect over time in some cases (98) and long-term effects (68). No significant long-term effects of compresses were reported.
Adverse effects of massages
Adverse physical effects in massage studies were symptom aggravation, arterial hypotension, cardiac palpitations, vertigo after treatment (65), exhaustion and tiredness after the treatment (81), flattening of breath (85), pain in the abdomen (81), headaches, and dental pain (65, 81, 103). The adverse psychological effect after massages was emotional agitation and a depressed and restless feeling (59, 81), and being overwhelmed by the interpersonal touch (93).
Adverse effects of compresses
In the compress studies, adverse effects were only reported in a case series on ginger compressions in the form of exhaustion after the treatment, irritation of the skin, cough, an unpleasant sensation of cold and wetness, emotional agitation, and feelings of restlessness (98).
Study quality
Since the study methodologies, the outcome measurements and the samples were heterogeneous and the studies were generally of low quality, the data did not allow for meta-analysis of the results. Study quality according to LoE, QA-Tool, and RoB is presented in Table 12.
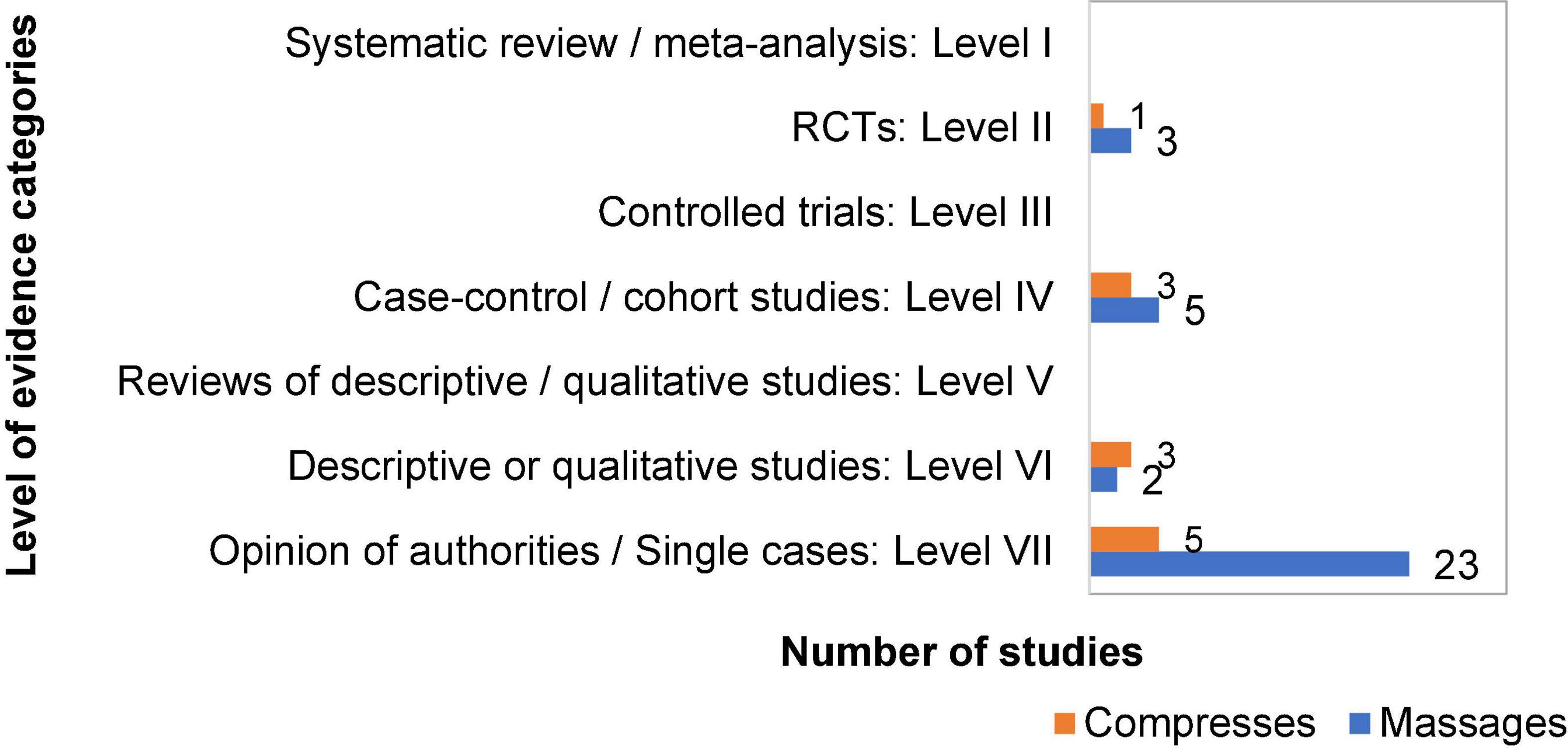
Level of evidence
The assignment of the individual studies to the heuristic of LoE resulted in a distribution of the studies between the levels according to their methodology (Figure 3). Level II was assigned 3 studies on massages (69, 70, 73) and 1 study on compresses (72). Level IV was assigned 5 studies on massages (64–67, 94) and 3 studies on compresses (62, 71, 100). Level VI was assigned 2 studies on massages (59, 60) and 3 studies on compresses (61, 68, 74). Level VII was assigned 23 studies on massages (75, 77–85, 87, 88, 90–93, 95–97, 99, 101–103) and 5 studies on compresses (63, 76, 86, 89, 98). Mixed methods studies were counted as quantitative studies (Level IV). Studies exploring a mixed intervention of massages and other application types were counted as massage studies.
Study quality assessment
Out of the 13 quantitative studies, 2 had strong quality (69, 70), 1 had moderate quality (71), and 10 had weak quality (62, 64–68, 72, 73, 94, 100) (Table 12). Two studies showed strong quality in representation of the population (selection bias), while 6 studies had moderate and 5 had weak quality in this domain. The study design was of strong quality in 4 studies (RCTs), moderate in 7 studies, weak in 2 studies, with 3 strong, 2 moderate, and 8 weak in the detection and controlling of confounders. Blinding of outcome assessors and participants was moderate in 3 studies and weak in 10 studies. Data collection methods were strong in 9 studies, moderate in 2 studies, and weak in 2 studies. Reporting of withdrawals and dropouts was strong in 6 studies, moderate in 4 studies, and weak in 3 studies.
Risk of bias assessment
Out of the 13 quantitative studies, 3 had a moderate risk of bias (69, 70, 73) and 10 had a high risk of bias (62, 64–68, 71, 72, 94, 100) (Table 12). The risk of selection bias was high in most studies as only 4 studies reported random sequence generation and only 3 studies reported adequate allocation concealment. While no study reported blinding of participants or personnel to the intervention, the study comparing different compresses reported blinding of participants to the used substances (71). No study reported adequate blinding of outcome assessors. Attrition bias was low in most studies as well as reporting bias. Other bias was caused mainly by small sample sizes and was only low in two studies.
Discussion
This mixed methods systematic review of 45 studies on EAAM included 34 studies on massage interventions and 11 studies on compress interventions. In both groups, various substances were applied. The methodologies of the included studies ranged from RCTs to cohort, retrospective, mixed methods and qualitative studies, and case series and reports. While a broad range of possible indications for applications could be identified by the Thematic Analyses of all included studies, limited statistically significant evidence for improvements was found in the outcomes. The safety of the different EAAMs needs further detailed evaluation.
External and internal validity
Overall, the results of this review are applicable mainly to European patients interested in integrative medical treatments and might be most applicable to the female gender. Further studies on EAAM applied to different participants are needed to ensure the external validity of the results. The employed methodology and the results of the quality and risk of bias assessments limit the interpretability of the results. More studies of high quality with low risk of bias need to be conducted and compared before conclusions can be drawn about the impact of EAAM.
Touching body, soul, and spirit: Intersections with other theories on health
The results on the effects of EAAM in this review suggest various health promoting effects, and therefore, match the findings on the health promoting capacities of the application of warmth and substances (14, 16–18, 21–24) as well as on touch and massage (9, 30, 31). The importance given to rhythmical stroking in massages matches the findings on the impact of a certain pace and pressure to stimulate especially C-tactile afferents in the skin to reach a positive effect and affective value (29).
While scientific medical and psychological research investigates if and how treatments affect individuals, Anthroposophy and AM already present views on effect mechanisms (104, 105). Suiting interpretations of the effect mechanisms of EAAM could also be detected in some of the included studies of this review, postulating a stimulation of self-regulation by the integration of the Four Levels of Formative Forces and/or through the regulation of the Threefold Functional Subsystems of the organism (80, 83–89, 95, 96, 99–101). In addition, the emergent effect themes could be interpreted as the influence of EAAM on the Formative Forces of the body (Material Body and vital Etheric Body), soul, and spirit according to AM (34): Physiological effects could be translated as affecting the body (Material Body and vital Etheric Body), psychological effects as affecting the soul, and the effects on psychological competencies could be translated as affecting the spirit.
However, as underlined by the findings of this review, the explanations of EAAM effect mechanisms according to AM do not translate directly into evidence according to conventional scientific research standards. To bridge this gap between the findings of this review and conventional scientific research, a digression into other scientific theories on health can provide alternative models to explain the effects of EAAM.
Benefits of interpersonal attention
External applications from anthroposophic medicine use interpersonal attention and touch. While the health-promoting capacities of touch have been described repeatedly (30, 106), two theories from psychological research specifically emphasize the importance of social contact to promote health. The Social Baseline Theory states that through social regulation of emotion, interaction with other people helps individuals to conserve somatic and neural resources, inhibit the release of stress hormones, reduce the risk of developing physical and mental illnesses, and promote health and longevity (107). The Tend and Befriend Model defines interpersonal tending as a natural reaction to stress and therefore as a baseline condition for health (108). These findings support the assumption that EAAM, as applications involving interpersonal contact and attention, may support health. In addition, findings suggest advantages for the practitioners when giving touch as well (109).
Impact of intentions and expectations
External applications from anthroposophic medicine are performed in a defined recurrent way, similar to rituals, and are often based on beliefs in their specific effect mechanisms according to AM. An approach to explain the efficacy of including a certain meaning in medical treatments is the Meaning Model, proposing that positive responses to applications may result from patients feeling listened to and attended to by caregivers, receiving an explanation for their disease that is consistent with their own worldview, receiving care and compassion, and experiencing an increased sense of mastery or control over their health (110). The setting of EAAM may, therefore, promote placebo effects (111) that can be used to ensure maximum benefit for patients (112, 113).
Holistic, positive, and dynamic approach to health
External applications from anthroposophic medicine are presumed to have health-promoting effects, to affect health holistically and dynamically. Holistic and positive support models underscore this, such as approaches of positive psychology and positive health [Seligman (114)] and person-centered medicine (115) as well as the Health Wellness Model, which promotes the integration of body, mind, and spirit to promote health (116). The consideration of spiritual factors for health promotion is mentioned in the literature as well, proposing that health care that addresses spiritual needs may contribute to recovery (117). The salutogenic definition of health defines a strong Sense of Coherence where one perceives the world as comprehensible, manageable, and meaningful as an indicator of health (38). Dynamic well-being conditioned by biopsychosocial potential (118) and health-defining heterostasis in the body (38, 39) are other concepts similar to the concept of flexible regeneration in organisms such as the EAAM underlying intention to stimulate self-regulation of the organism through treatments in order to enable healing (40, 41).
Strengths and limitations of this review
This is the first review of EAAM. We used the design of a mixed methods systematic review to cover the heterogeneous empirical literature on the different types of EAAM, sample characteristics, methodologies, and outcome parameters (52). The broad scope of the review and the extensive literature search process enables a comprehensive overview of the areas of use and effectiveness of EAAM. Studies in English and German were included, covering most of the available literature on the topic. The quality of the included studies and the applicability of the results were assessed. In order to sort the heterogeneous result data of the included studies, we decided to use the approach of a Thematic Analysis. While using this method to summarize results is not common in review papers, it was quite helpful to inductively get an overview of the effect patterns in the included studies.
However, the heterogeneity of the included studies limits their generalizability. Only a small number of quantitative studies could be identified, which limits the expressiveness of the review. Many of the studies were only accessible in the form of gray literature and/or abstracts. As assessed by the LoE classification, the validity of the included studies had to be described as low in many of the studies. Study quality was assessed as low and the risk of bias as high in most studies. The safety of EAAM could only be assessed qualitatively on the basis of a few of the included studies reporting it.
We used a combination of the 3 tools LoE assessment, QA-Tool, and RoB to sort and adequately evaluate the quality and validity of the heterogeneous studies. Quality assessment of the included studies was conducted by two members of the research group (IM, JE). However, the QA-Tool and the RoB are repetitive in some domains and would have benefited from better tailored tools for the evaluation.
Implications for research and clinical practice
The implementation of complementary EAAM in clinical practice can be an opportunity to consider the patient’s needs for caregiving as well as spiritual needs in some patients in a manner of person-centered medicine.
Since the interpretability of the evidence found in this review is limited by the methodological quality of the included studies, we endorse studies of high quality on the different EAAM for different patient groups. These studies should ensure rigorous methodology and reports (119). In order to gain a deeper understanding of the interpretations of the effect mechanisms of EAAM according to Anthroposophy, a phenomenological analysis (120) based on the result and discussion sections of the included studies and/or theoretical manuscripts on EAAM might be of merit.
Users should adhere to the procedure specifications of the different EAAMs, and caution is advised with regard to the mentioned adverse effects. EAAM is not indicated in patients with adverse attitudes toward touch or in patients with sensitive skin or tissue damage. As illness was described in sections by Steiner and Wegman as depending on personal faculties (37), the underlying views of AM might be perceived as discriminating against people with diseases. When applying EAAM, users should, therefore, be cautious about their intentions with the applications. Furthermore, it is strongly advised to use EAAM complementarily to evidence-based treatments to promote well-being as intended (33, 121).
Conclusion
The mixed methods systematic review illustrates the potential benefits of the different EAAM modalities as complementary treatments. The data reveal a broad spectrum of effect themes, suggesting that EAAM is suitable to address physical and psychological health indicators by improving the general condition and inducing symptom relief as well as psychologically activating and relaxing effects. Limitations in study quality, varying application modalities, different outcome assessments, and different sample characteristics complicate a substantiated comparison of the outcomes. We recommend further clinical studies exploring the effects and safety of distinguished EAAM modalities on defined patient groups to determine to what extent EAAM can be considered an effective and safe treatment option.
Data availability statement
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
IM contributed to the conceptualization, methodological planning, data analysis, writing, and revision of the manuscript. SB contributed to the revision and editing. JE contributed to the data analysis. HC and GS contributed to the supervision, revision, and editing. WS contributed to the conceptualization, supervision, revision, and editing. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by the Christophorus Foundation (Grant No. 373 CST). The funders had no role in the design and conduct of the review; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Acknowledgments
We thank Jan Keller for his valuable remarks, all experts and institutions for contributing literature and sources and the Christophorus Foundation for the financial support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
- ^ https://www.anthromedics.org
- ^ https://www.cambase.de
- ^ https://www.cam-quest.org
- ^ https://www.researchgate.net
- ^ https://www.opengrey.eu/
References
1. Baars E, Hamre H. Whole medical systems versus the system of conventional biomedicine: a critical, narrative review of similarities, differences, and factors that promote the integration process. Evid Based Complement Altern Med. (2017) 2017:2014–23. doi: 10.1155/2017/4904930
2. Gannotta R, Malik S, Chan A, Urgun K, Hsu F, Vadera S. Integrative medicine as a vital component of patient care. Cureus. (2018) 10:8–12. doi: 10.7759/cureus.3098
3. Brown C. The integration of healing and spirituality into health care. J Interprof Care. (1998) 12:373–81. doi: 10.3109/13561829809024944
4. Krenner L. Integrative medizin – die wiederentdeckung der ganzheit. In: Frass M, Krenner L editors. Integrative Medizin. Berlin: Springer (2019). p. 3–21. doi: 10.1007/978-3-662-48879-9_1
5. Ernst E, Pittler M, Wider B, Boddy K. Massage therapy: is its evidence-base getting stronger. Complement Health Pract Rev. (2007) 12:179–83. doi: 10.1177/1533210107306090
6. Uvnäs-Moberg K. Wie funktionieren massage und berührung? In: Uvnäs-Moberg K editor. Oxytocin, das Hormon der Nähe. Berlin: Springer Spektrum (2009). p. 215–8.
7. Musial F, Weiss T. The healing power of touch: the specificity of the “Unspecific” effects of massage. Forsch Komplementarmed. (2014) 21:282–3. doi: 10.1159/000368449
8. Mühlenpfordt I, Stritter W, Bertram M, Ben-Arye E, Seifert G. The power of touch: external applications from whole medical systems in the care of cancer patients (literature review). Support Care Cancer. (2020) 28:461–71. doi: 10.1007/s00520-019-05172-7
9. Field T. Massage therapy research review. Complement Ther Clin Pract. (2016) 24:19–31. doi: 10.1016/j.ctcp.2016.04.005
10. Bächle-Helde B. Sind alternative pflegemethoden evidenzbasiert? Eine literaturstudie am beispiel von wickel und auflagen. Pflegewissenschaften. (2011) 11:597–603.
11. Uvnäs-Moberg K. Oxytocin may mediate the benefits of positive social interaction and emotions. Psychoneuroendocrinology. (1998) 23:819–35. doi: 10.1016/S0306-4530(98)00056-0
12. Matai L, Sarkar G, Chamoli M, Malik Y, Kumar S, Rautela U, et al. Dietary restriction improves proteostasis and increases life span through endoplasmic reticulum hormesis. Proc Natl Acad Sci U.S.A. (2019) 116:17383–92. doi: 10.1073/pnas.1900055116
13. Gálvez I, Torres-Piles S, Ortega-Rincón E. Balneotherapy, immune system, and stress response: a hormetic strategy? Int J Mol Sci. (2018) 19:1687. doi: 10.3390/ijms19061687
14. Rattan S. Hormetic modulation of aging and longevity by mild heat stress. Dose Response. (2005) 3:533–46. doi: 10.2203/dose-response.003.04.008
15. Lee S, Depoortere I, Hatt H. Therapeutic potential of ectopic olfactory and taste receptors. Nat Rev Drug Discov. (2019) 18:116–38. doi: 10.1038/s41573-018-0002-3
16. Schneider R, Singer N, Singer T. Medical aromatherapy revisited—Basic mechanisms, critique, and a new development. Hum Psychopharmacol. (2019) 34:1–10. doi: 10.1002/hup.2683
17. Boehm K, Büssing A, Ostermann T. Aromatherapy as an adjuvant treatment in cancer care – a descriptive systematic review. African J Tradit Complement Altern Med. (2012) 9:503–18. doi: 10.4314/ajtcam.v9i4.7
18. Ali B, Al-Wabel N, Shams S, Ahamad A, Khan S, Anwar F. Essential oils used in aromatherapy: a systemic review. Asian Pac J Trop Biomed. (2015) 5:601–11. doi: 10.1016/j.apjtb.2015.05.007
19. Lee M, Choi J, Posadzki P, Ernst E. Aromatherapy for health care: an overview of systematic reviews. Maturitas. (2012) 71:257–60. doi: 10.1016/j.maturitas.2011.12.018
20. Czakert J, Stritter W, Blakeslee S, Seifert G. Plant fragrances are like music for our senses: a scoping review of aromatherapy in gynecologic cancers and breast cancer care. J Integr Complement Med. (2022) 28:377–90. doi: 10.1089/jicm.2021.0368
21. Cavanagh H, Wilkinson J. Biological activities of lavender essential oil. Phyther Res. (2002) 16:301–8. doi: 10.1002/ptr.1103
22. Koulivand P, Khaleghi Ghadiri M, Gorji A. Lavender and the nervous system. Evid Based Complement Altern Med. (2013) 2013:681304. doi: 10.1155/2013/681304
23. Kuderer S, Helmert E, Szöke H, Joos S, Kohl M, Svaldi J, et al. Increasing warmth in adolescents with anorexia nervosa: a randomized controlled crossover trial examining the efficacy of mustard and ginger footbaths. Evid Based Complement Altern Med. (2020) 2020:2416582. doi: 10.1155/2020/2416582
24. Vagedes J, Helmert E, Kuderer S, Müller V, Voege P, Szõke H, et al. Effects of footbaths with mustard, ginger, or warm water only on objective and subjective warmth distribution in healthy subjects: a randomized controlled trial. Complement Ther Med. (2018) 41:287–94. doi: 10.1016/j.ctim.2018.09.024
25. Montagu A. Touching: the Human Significance of the Skin. New York, NY: Columbia University Press (1971).
26. Eliava M, Melchior M, Knobloch-Bollmann H, Wahis J, da Silva Gouveia M, Tang Y, et al. A new population of parvocellular oxytocin neurons controlling magnocellular neuron activity and inflammatory pain processing. Neuron. (2016) 89:1291–304. doi: 10.1016/j.neuron.2016.01.041
27. Detillion C, Craft T, Glasper E, Prendergast B, DeVries A. Social facilitation of wound healing. Psychoneuroendocrinology. (2004) 29:1004–11. doi: 10.1016/j.psyneuen.2003.10.003
28. Field T, Hernandez-Reif M, Diego M, Schanberg S, Kuhn C. Cortisol decreases and serotonin and dopamine increase following massage therapy. Int J Neurosci. (2005) 115:1397–413. doi: 10.1080/00207450590956459
29. Pawling R, Cannon P, McGlone F, Walker SC. C-tactile afferent stimulating touch carries a positive affective value. PLoS One. (2017) 12:e0173457. doi: 10.1371/journal.pone.0173457
30. Field T. Touch for socioemotional and physical well-being: a review. Dev Rev. (2010) 30:367–83. doi: 10.1016/j.dr.2011.01.001
31. Holt-Lunstad J, Birmingham W, Light K. Influence of a “warm touch” support enhancement intervention among married couples on ambulatory blood pressure, oxytocin, alpha amylase, and cortisol. Psychosom Med. (2008) 70:976–85. doi: 10.1097/PSY.0b013e318187aef7
32. Nelson N. Massage therapy: understanding the mechanisms of action on blood pressure. A scoping review. J Am Soc Hypertens. (2015) 9:785–93. doi: 10.1016/j.jash.2015.07.009
33. Steiner R, Wegman I. True Knowledge of the Human Being as a Foundation for the art of Medicine. In: Fundamentals of Therapy An Extension of the Art of Healing through Spiritual KnowledgeAn Extension of the Art of Healing Through Spiritual Knowledge. London: Anthroposophical Publishing Co (1925). p. 7–19.
34. Kienle G, Albonico H, Baars E, Hamre H, Zimmermann P, Kiene H. Anthroposophic medicine: an integrative medical system originating in Europe. Glob Adv Heal Med. (2013) 2:20–31. doi: 10.7453/gahmj.2012.087
35. Siber H. Anthroposophische medizin. In: Frass M, Krenner L editors. Integrative Medizin. Berlin: Springer (2019). p. 455–79. doi: 10.1007/978-3-662-48879-9_21
36. Steiner R. Anthroposophische Leitsätze 1–37. In: Was in der Anthroposophischen Gesellschaft Vorgeht 1924/25. Dornach: Rudolf Steiner Online Archiv (2010). p. 1–22.
37. Steiner R, Wegman I. Why Man is Subject to Illness. In: Fundamentals of Therapy An Extension of the Art of Healing Through Spiritual Knowledge. London: Anthroposophical Publishing Co (1925). p. 18–24.
38. Antonovsky A. The salutogenic model as a theory to guide health promotion. Health Promot Int. (1996) 11:11–8. doi: 10.1093/heapro/11.1.11
39. Franke A. Was ist gesundheit? 2nd ed. In: Franke A editor. Modelle von Gesundheit und Krankheit. Bern: Verlag Hans Huber (2010). p. 31–54.
40. Steiner R. 3rd ed. In: Steiner R editor. Anthroposophische Menschenerkenntnis und Medizin. GA 319. Dornach: Rudolf Steiner Verlag (1994).
41. Steiner R. 32nd ed. In: Steiner R editor. Theosophie. Einführung in übersinnliche Welterkenntnis und Menschenbestimmung. GA 9. Dornach: Rudolf Steiner Verlag (2003).
42. Kusserow M. Äußere Anwendungen in der anthroposophischen praxis und klinik. Der Merkurstab. (2014) 67:136–40.
43. Glöckler M. Äußere anwendungen – ein therapeutischer weg zur aktivierung der ich-organisation. Der Merkurstab. (2014) 67:88–91.
45. Große-Brauckmann E. Qualitätskriterien für rhythmische einreibungen nach wegman/hauschka. In: Layer M editor. Praxishandbuch Rhythmische Einreibungen nach Wegman/Hauschka. Bern: Verlag Hans Huber (2003). p. 57–117.
46. Pressel E. Massage nach Dr. med. Simeon pressel. Einblick in hintergründe, entwicklung, durchführung und wirkungsweise. Der Merkurstab. (2007) 60:45–9.
47. Kienle G, Glockmann A, Grugel R, Hamre H, Kiene H. Klinische forschung zur anthroposophischen medizin – update eines «health technology assessment» -berichts und status quo. Forsch Komplementarmed. (2011) 18:269–82. doi: 10.1159/000331812
48. Büssing A, Cysarz D, Edelhäuser F, Bornhöft G, Matthiessen P, Ostermann T. The oil-dispersion bath in anthroposophic medicine – an integrative review. BMC Complement Altern Med. (2008) 8:61. doi: 10.1186/1472-6882-8-61
49. Büssing A, Ostermann T, Majorek M, Matthiessen P. Eurythmy therapy in clinical studies: a systematic literature review. BMC Complement Altern Med. (2008) 8:8. doi: 10.1186/1472-6882-8-8
50. Schlaeppi M, Büssing A, Müller-Hübenthal B, Heusser P. Anthroposophische medizin in der onkologie. Onkologe. (2010) 16:901–5. doi: 10.1007/s00761-010-1891-x
51. Kienle G, Kiene H. Influence of Viscum album L (European Mistletoe) extracts on quality of life in cancer patients: a systematic review of controlled clinical studies. Integr Cancer Ther. (2010) 9:142–57. doi: 10.1177/1534735410369673
52. Stern C, Lizarondo L, Carrier J, Godfrey C, Rieger K, Salmond S, et al. Methodological guidance for the conduct of mixed methods systematic reviews. JBI Evid Synth. (2020) 18:2108–18. doi: 10.11124/JBISRIR-D-19-00169
53. Moher D, Liberati A, Tetzlaff J, Altman D, Altman D, Antes G, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
54. Higgins J, Green S. Cochrane handbook for systematic reviews of interventions. In: Higgins J, Green S editors. Cochrane Handbook for Systematic Reviews of Interventions. Chichester: John Wiley & Sons (2019). doi: 10.1002/9781119536604
55. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
56. Higgins J, Altman D, Gøtzsche P, Jüni P, Moher D, Oxman A, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:1–9. doi: 10.1136/bmj.d5928
57. National Collaborating Centre for Methods and Tools. Quality Assessment tool for Quantitative Studies. Effective Public Health Practice Project. Toronto: McMaster University (2010).
58. Ackley B, Ladwig G, Swan B, Tucker S. Evidence-Based Nursing Care Guideline: Medical-Surgical Interventions. St. Louis, Missouri: Mosby Elsevier (2008).
59. Berger B, Böning A, Martin H, Fazeli A, Martin D, Vagedes J. Personal perception and body awareness of dysmenorrhea and the effects of rhythmical massage therapy and heart rate variability biofeedback—a qualitative study in the context of a randomized controlled trail. Complement Ther Med. (2019) 45:280–8. doi: 10.1016/j.ctim.2019.04.007
60. Bertram M, Ostermann T, Matthiessen P. Erforschung der rhythmischen einreibungen nach wegman/hauschka – eine strukturphänomenologische untersuchung. Pflege. (2005) 18:227–35. doi: 10.1024/1012-5302.18.4.227
61. Therkleson T, Sherwood P. Patients’ experience of the external therapeutic application of ginger by anthroposophically trained nurses. Indo Pacific J Phenomenol. (2004) 4:1–11. doi: 10.1080/20797222.2004.11433892
62. Therkleson T. Topical ginger treatment with a compress or patch for osteoarthritis symptoms. J Holist Nurs. (2014) 32:173–82. doi: 10.1177/0898010113512182
63. Deckers B, Von Schoen-Angerer T, Voggenreiter B, Vagedes J. External nursing applications in the supportive management of prolonged postoperative ileus description of interventions and case report. Holist Nurs Pract. (2016) 30:216–21. doi: 10.1097/HNP.0000000000000158
64. Ostermann T, Blaser G, Bertram M, Michalsen A, Matthiessen P, Kraft K. Effects of rhythmic embrocation therapy with solum oil in chronic pain patients: a prospective observational study. Clin J Pain. (2008) 24:237–43. doi: 10.1097/AJP.0b013e3181602143
65. Hamre H, Witt C, Glockmann A, Ziegler R, Willich S, Kiene H. Rhythmical massage therapy in chronic disease: a 4-year prospective cohort study. J Altern Complement Med. (2007) 13:635–42. doi: 10.1089/acm.2006.6345
66. Wälchli C, Saltzwedel G, Krüerke D, Kaufmann C, Schnorr B, Rist L, et al. Physiologic effects of rhythmical massage: a prospective exploratory cohort study. J Altern Complement Med. (2014) 20:507–15. doi: 10.1089/acm.2012.0833
67. Wälchli C, Saltzwedel G, Rist L, Bach-Meguid B, Eberhard J, Decker M, et al. Clinical outcomes of rhythmical massage: a prospective cohort study with swiss outpatients. Altern Complement Ther. (2014) 20:248–58. doi: 10.1089/act.2014.20509
68. Simoes-Wüst A, Saltzwedel G, Herr I, Rist L. Wie patienten wickelanwendungen (ein)schätzen: ergebnisse einer umfrage in einem anthroposophischen akutspital. Schweiz Z Ganzheitsmedizin. (2012) 24:299–305. doi: 10.1159/000342725
69. Seifert G, Kanitz J, Rihs C, Krause I, Witt K, Voss A. Rhythmical massage improves autonomic nervous system function: a single-blind randomised controlled trial. J Integr Med. (2018) 16:172–7. doi: 10.1016/j.joim.2018.03.002
70. Kanitz J, Reif M, Rihs C, Krause I, Seifert G. A randomised, controlled, single-blinded study on the impact of a single rhythmical massage (anthroposophic medicine) on well-being and salivary cortisol in healthy adults. Complement Ther Med. (2015) 23:685–92. doi: 10.1016/j.ctim.2015.07.008
71. Stritter W, Gross M, Miltner D, Rapp D, Wilde B, Eggert A, et al. More than just warmth–the perception of warmth and relaxation through warming compresses. Complement Ther Med. (2020) 54:102537. doi: 10.1016/j.ctim.2020.102537
72. Ghadjar P, Stritter W, von Mackensen I, Mehrhof F, Foucré C, Ehrhardt V, et al. External application of liver compresses to reduce fatigue in patients with metastatic cancer undergoing radiation therapy, a randomized clinical trial. Radiat Oncol. (2021) 16:1–9. doi: 10.1186/s13014-021-01757-x
73. Vagedes J, Fazeli A, Boening A, Helmert E, Berger B, Martin D. Efficacy of rhythmical massage in comparison to heart rate variability biofeedback in patients with dysmenorrhea—a randomized, controlled trial. Complement Ther Med. (2019) 42:438–44. doi: 10.1016/j.ctim.2018.11.009
74. Therkleson T. Ginger compress therapy for adults with osteoarthritis. J Adv Nurs. (2010) 66:2225–33. doi: 10.1111/j.1365-2648.2010.05355.x
75. Therkleson T, Stronach S. Broken heart syndrome, a typical case. J Holist Nurs. (2015) 33:345–50. doi: 10.1177/0898010115569883
76. Therkleson T. Ginger therapy for osteoarthritis, a typical case. J Holist Nurs. (2014) 32:232–9. doi: 10.1177/0898010113520467
77. Ammann Albertin L. Rhythmical massage in co-occurring asthma and hypertension: a case report. Der Merkurstab. (2016) 1:55.
78. Börner E. Rhythmische massage – grundlegende gedanken anhand einer falldarstellung aus der pädiatrie. Mit einem blick auf die craniosacrale therapie. Der Merkurstab. (2001) 54:111–6.
79. Meyer R. Qualitäten der rhythmischen massage und ihre möglichkeiten bei erkrankungen der wirbelsäule. Der Merkurstab. (2003) 56:306–9.
80. Praxl M. Rhythmischen Einreibungen nach Wegman/Hauschka bei einer Patientin mit HMSN Typ 2 (Heriditäre motorisch sensible Neuropathie), Zusammenfassung der MSc Thesis. Graz: Interuniversitäres Kolleg Graz/Seggau (2010).
81. Pressel E. Massage nach simeon pressel: wirkung auf den weiblichen zyklus – vier kasuistiken. Der Merkurstab. (2014) 67:143–7.
82. Radünz S. Die Rhythmische Massage nach Dr. Ita Wegman als Therapie bei Patienten mit Einer Obstruktiven Schlafapnoe, Zusammenfassung der MSc Thesis. Graz: Interuniversitäres Kolleg Graz/Seggau (2011).
83. Robert A. Die massage nach Dr. med. Simeon pressel – hilfe und begleitung für den heutigen menschen. Der Merkurstab. (2018) 71:454–8. doi: 10.14271/DMS-21015-DE
84. Roggatz C. Rhythmische Einreibungen in der Altenpflege – Die Wirkung der Rhythmischen Einreibung auf den Schlaf. Bachelorthesis. Frankfurt: University of Applied Sciences Frankfurt (2016).
85. Reisinger I. Rhythmische Einreibung nach Wegman/Hauschka bei einer Erschöpfungsdepression, Zusammenfassung der MSc Thesis. Graz: Interuniversitäres Kolleg Graz/Seggau (2010).
86. Schier J, Bruchner N. Schafgarbe-tee-leberwickel bei chemotherapie-assoziierten beschwerden bei einem 40-jährigen patienten mit seminom – eine kasuistik. Der Merkurstab. (2016) 69:134–8. doi: 10.14271/DMS-20620-DE
87. Schober R. Die Wirkung der Rhythmischen Massage in der Heilpädagogik an einem Kind mit spastischer Tetraparese, Zusammenfassung d. MSc Thesis. Graz: Interuniversitäres Kolleg Graz/Seggau (2010).
88. Schwarz A. Die Rhythmische Massage nach Dr. Ita Wegman als begleitende Therapie bei Morbus Parkinson, Zusammenfassung der MSc Thesis. Graz: Interuniversitäres Kolleg Graz/Seggau (2010).
89. Deckers B. Senfwickel-behandlung bei pneumonie – eine kasuistik. Der Merkurstab. (2014) 67:141–2.
90. Schwinger B. Behandlung des Burnout-Syndroms mit der Rhythmischen Massage nach Dr. Ita Wegman, Zusammenfassung der MSc Thesis. Graz: Interuniversitäres Kolleg Graz/Seggau (2010).
91. Seedheeyan S, Rose A, Florschutz G. Don’t touch me! Rhythmical massage therapy for pain management in a patient with acquired brain injury: a single case study. Der Merkurstab. (2016) 1:53.
92. Vajnai G, Seedheeyan S, Ţuţuianu C, Rose A, Florschutz G. Service description and a single case study of applying rhythmical massage therapy in clinical practice for left mid-cerebral artery stroke rehabilitation and assessing the effectiveness of the treatments. Der Merkurstab. (2016) 1:53.
93. Uhlenhoff R. Rhythmische Massage in der Heilpädagogik Anwendungsbeobachtung an einem Kind mit Autismus, Zusammenfassung der MSc Thesis. Graz: Interuniversitäres Kolleg Graz/Seggau (2010).
94. Vieira P, Facina A, Hosomi J, Ghelman R, Nakamura M, Melo M. Contribution of anthroposophic external therapies in cognition, mood and quality of life of the elderly. Der Merkurstab. (2012) 6:579.
95. Voit R. Rhythmische Einreibung nach Wegman/Hauschka bei einer Jugendlichen mit Versagensängsten speziell bei mündlichen Prüfungen, Zusammenfassung der MSc Thesis. Graz: Interuniversitäres Kolleg Graz/Seggau (2010).
96. Weidtke A. Rhythmische massage nach ita wegman in der onkologie. Der Merkurstab. (2009) 62:344–51.
97. Gierse B. Die Wirkung der Rhythmischen Massage als rehabilitative Maßnahme nach operativer Behandlung einer Humeruskopftrümmerfraktur linksseitig, Zusammenfassung der MSc Thesis. Graz: Interuniversitäres Kolleg Graz/Seggau (2011).
98. Glaser H, Heine R, Sauer M, Simon L. Ingwerstudie. Praxisintegrierte Studie zur Darstellung der Frühwirkungen von Ingwer (Zingiberis Officinalis) als Äußere Anwendung. 2nd ed. Filderstadt: Verband anthroposophische orientierter Pflegeberufe e.V (2001).
99. Göbels R, Allmer C. Die Behandlung mit rhythmischer massage bei einer patientin mit mammakarzinom. Der Merkurstab. (2014) 67:126–35.
100. Klich-Heartt E. External Calf Compresses with Lemon as a Nursing Adjunct for Fever Treatment. San Rafael, CA: Dominican University of California (2003).
101. Klocker M. Die Auswirkung der Nachruhe bei der Behandlung des Burnout-Syndroms unter Anwendung der Rhythmischen Massage, Zusammenfassung der MSc. Thesis. Graz: Interuniversitäres Kolleg Graz/Seggau (2010).
102. Kögler T. Die Behandlung des Lumbalsyndroms Unter Anwendung der Rhythmischen Massage, Zusammenfassung der MSc Thesis. Graz: Interuniversitäres Kolleg Graz/Seggau (2010).
103. Maier-Schnorr C. Die behandlung der migräne mit rhythmischer massage. Der Merkurstab. (2007) 60:153–5.
104. Sparby T. Body, soul, and spirit: an explorative qualitative study of anthroposophic meditation and spiritual practice. Religions. (2020) 11:314. doi: 10.3390/rel11060314
105. Heusser P, editor. Anthroposophische geisteswissenschaft und naturwissenschaftliche medizin. In: Anthroposophische Medizin und Wissenschaft. Bern: Schattauer (2011). p. 211–42.
106. Serino A, Haggard P. Touch and the body. Neurosci Biobehav Rev. (2010) 34:224–36. doi: 10.1016/j.neubiorev.2009.04.004
107. Beckes L, Coan J. Social baseline theory: the role of social proximity in emotion and economy of action. Soc Personal Psychol Compass. (2011) 5:976–88. doi: 10.1111/j.1751-9004.2011.00400.x
108. Taylor S, Master S. Social responses to stress: the tend and befriend model. In: Contrada R, Baum A editors. The Handbook of Stress Science: Biology, Psychology, and Health. New York, NY: Springer (2010). p. 101–9.
109. Edvardsson J, Sandman P, Rasmussen B. Meanings of giving touch in the care of older patients: becoming a valuable person and professional. J Clin Nurs. (2003) 12:601–9. doi: 10.1046/j.1365-2702.2003.00754.x
110. Brody H. Ritual, medicine, and the placebo response. In: Sax W, Quack J, Weinhold J editors. The Problem of Ritual Efficacy. New York, NY: Oxford University Press (2010). p. 151–67. doi: 10.1093/acprof:oso/9780195394405.003.0008
111. Kaptchuk T. The placebo effect in alternative medicine: can the performance of a healing ritual have clinical significance? Ann Intern Med. (2002) 136:817–25. doi: 10.7326/0003-4819-136-11-200206040-00011
112. Kirmayer L. Unpacking the placebo response: insights from ethnographic studies of healing. In: Raz A, Harris C editors. Placebo Talks: Modern Perspectives on Placebos in Society. New York, NY: Oxford University Press (2016). p. 119–43. doi: 10.1093/acprof:oso/9780199680702.003.0008
113. Benedetti F, Carlino E, Pollo A. How placebos change the Patient’s brain. Neuropsychopharmacology. (2011) 36:339–54. doi: 10.1038/npp.2010.81
114. Seligman M. Positive health. Appl Psychol. (2008) 57(Suppl. 1):3–18. doi: 10.1111/j.1464-0597.2008.00351.x
115. Miles A, Mezzich J. The care of the patient and the soul of the clinic: person-centered medicine as an emergent model of modern clinical practice. Int J Pers Cent Med. (2011) 1:207–22. doi: 10.5750/ijpcm.v1i2.61
116. Larson J. The conceptualization of health. Med Care Res Rev. (1999) 56:123–36. doi: 10.1177/107755879905600201
117. Büssing A, Koenig H. Spiritual needs of patients with chronic diseases. Religions. (2010) 1:18–27. doi: 10.3390/rel1010018
118. Bircher J. Towards a dynamic definition of health and disease. Med Heal Care Philos. (2005) 8:335–41. doi: 10.1007/s11019-005-0538-y
119. Schulz K, Altman D, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. (2010) 152:726–32. doi: 10.7326/0003-4819-152-11-201006010-00232
120. Giorgi A. The theory, practice, and evaluation of the phenomenological method as a qualitative research procedure. J Phenomenol Psychol. (1997) 28:235–60. doi: 10.1163/156916297X00103
Keywords: external application, integrative medicine, anthroposophic medicine, touch, mixed methods systematic review
Citation: Mühlenpfordt I, Blakeslee SB, Everding J, Cramer H, Seifert G and Stritter W (2022) Touching body, soul, and spirit? Understanding external applications from integrative medicine: A mixed methods systematic review. Front. Med. 9:960960. doi: 10.3389/fmed.2022.960960
Received: 03 June 2022; Accepted: 29 November 2022;
Published: 22 December 2022.
Edited by:
Arch Mainous, University of Florida, United StatesReviewed by:
Fatemeh Darsareh, Hormozgan University of Medical Sciences, IranEron Grant Manusov, The University of Texas Rio Grande Valley, United States
Copyright © 2022 Mühlenpfordt, Blakeslee, Everding, Cramer, Seifert and Stritter. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Inga Mühlenpfordt, ✉ aS5tdWVobGVucGZvcmR0QGdteC5kZQ==
 Inga Mühlenpfordt
Inga Mühlenpfordt Sarah B. Blakeslee
Sarah B. Blakeslee Janina Everding1
Janina Everding1 Holger Cramer
Holger Cramer Georg Seifert
Georg Seifert Wiebke Stritter
Wiebke Stritter