
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med., 05 August 2022
Sec. Intensive Care Medicine and Anesthesiology
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.883126
This article is part of the Research TopicGlobal Excellence in Intensive Care Medicine and Anesthesiology: North AmericaView all 5 articles
 Krzysztof Laudanski1,2,3*
Krzysztof Laudanski1,2,3* Ann Marie Huffenberger4
Ann Marie Huffenberger4 Michael J. Scott1,4
Michael J. Scott1,4 Maria Williams4
Maria Williams4 Justin Wain5
Justin Wain5 Juliane Jablonski6
Juliane Jablonski6 C. William Hanson III1,4
C. William Hanson III1,4Background: Our study addresses the gaps in knowledge of the characterizations of operations by remote tele-critical care medicine (tele-CCM) service providers interacting with the bedside team. The duration of engagements, the evolution of the tele-CCM service over time, and the distress during interactions with the bedside team have not been characterized systematically. These characteristics are critical for planning the deployment of teleICU services and preventing burnout among remote teleICU providers.
Methods: REDCap self-reported activity logs collected engagement duration, triggers (emergency button, tele-CCM software platform, autonomous algorithm, asymmetrical communication platform, phone), expediency, nature (proactive rounding, predetermined task, response to medical needs), communication modes, and acceptance. Seven hospitals with 16 ICUs were overseen between 9/2020 and 9/2021 by teams consisting of telemedicine medical doctors (eMD), telemedicine registered nurses (eRN), and telemedicine respiratory therapists (eRT).
Results: 39,915 total engagements were registered. eMDs had a significantly higher percentage of emergent and urgent engagements (31.9%) vs. eRN (9.8%) or eRT (1.7%). The average tele-CCM intervention took 16.1 ± 10.39 min for eMD, 18.1 ± 16.23 for eRN, and 8.2 ± 4.98 min for eRT, significantly varied between engagement, and expediency, hospitals, and ICUs types. During the observation period, there was a shift in intervention triggers with an increase in autonomous algorithmic ARDS detection concomitant with predominant utilization of asynchronous communication, phone engagements, and the tele-CCM module of electronic medical records at the expense of the share of proactive rounding. eRT communicated more frequently with bedside staff (% MD = 37.8%; % RN = 36.8, % RT = 49.0%) but mostly with other eRTs. In contrast, the eMD communicated with all ICU stakeholders while the eRN communicated chiefly with other RN and house staff at the patient's bedside. The rate of distress reported by tele-CCM staff was 2% among all interactions, with the entity hospital being the dominant factor.
Conclusions: Delivery of tele-CCM services has to be tailored to the specific beneficiary of tele-CCM services to optimize care delivery and minimize distress. In addition, the duration of the average intervention must be considered while creating an efficient workflow.
Telemedicine is a growing healthcare delivery modality with expansion accelerating after the onset of COVID-19 (1–3). This growth is particularly visible in tele-Critical Care Medicine (tele-CCM) due to the exacerbated pandemic needs and significant providers shortage (4, 5). However, the evolution of tele-CCM has been primarily organic and highly siloed with grass-root interactions between academic, federal, and private entities (1, 6). Until recently, growth has been dominated by a few industry partners and academic entities with relatively little diffusion of the protocols. Regulations and standards are mostly based on recommendations and expert opinions with limited support in evidence (5, 7–9). COVID-19 increased the stance of tele-CCM, but barriers cast uncertainty on post-pandemic development (5, 9, 10).
To date, task execution by the tele-CCM team has been studied relatively sparsely, even though the clinical workflows are critical for delivering high-reliable care (11). Placing unrealistic demands and expectations on providers will strain service delivery and increase the likelihood of burnout. There are gaps in knowledge regarding the frequency and duration of tele-ICU consultations. These metrics are critical for understanding the expected load on providers and service capacity.
The tele-ICU & bedside team dynamics are fundamental as communication is critical for care delivery. Fostering ingenuity of the bedside and tele-ICU staff is the strategy for finding ways of deploying TCC services, especially if the goals and visions of the tele-ICU deployment are unclear (12–14). The workflow must adapt interactions between tele- and bedside providers to address the needs most appropriate (11, 13–15). After launching the tele-CCM partnerships, the initial set of tasks will be modified to the most acceptable services. However, only few studies demonstrated a regionalization of the services (16–18). The execution of the primary goals will be influenced by the clinical and cultural specificity of the unit. Once the equilibrium between tele-CCM & bedside partnership is reached, maturation of service will take place (13). It is unknown how long the process of service evolution takes place.
The perception of tele-CCM performance has been predominantly studied from the bedside perspective (19–21). However, the remote team perception of the impact, professionalism, and potential distress secondary to interaction needs are critical for optimal interaction. Lack of understanding will inevitably affect the performance of the tele-CCM team and their engagement with the bedside. Inadequate interactions cause tension and emotional distress and contribute to burnout.
Here, we focused on characterizing the team dynamics of the tele-CCM staff providing care in large medical system. We aimed to characterize the execution of clinical tasks, their expediency, and the time needed for completion among three types of tele-CCM teams. We hypothesized that the execution of tasks would vary across the units depending on the local culture. We also studied team communication during task execution and their perception of acceptance of recommendations, emphasizing the distress caused by such interactions.
Considering this is a quality and improvement project, the study is exempted from the IRB's approval.
The staff of the Penn E-lert™ consisted of 16 board-certified intensivists (eMD), 11 registered respiratory therapists (eRT), and 25 registered nurses (eRN), supported by our centralized telehealth coordinator team (eTHC).
The staffing model includes daytime and nighttime shift rotation equally staffed with three to four eRN, one eRT, and one eTHC who work 12-h continuous shifts. An unstructured sign-out to each other, noting the most urgent issues, occurs at 7 AM and 7 PM during shift changes. In addition, between 7 PM and 7 AM, one eMD joins the multidisciplinary tele-CCM team in the centralized hub.
The system supervised seven hospitals with 15 ICUs, each with different profiles comprising 295 beds (Supplementary Table 1). Staff within the ICUs comprises nurses (staffing ratio-1:2), RT (staffing ratio-1:8), and a variable combination of advanced practice providers, house staff, and medical attendings. All bedside medical attendings are board-certified in critical care.
The Penn E-lert model has been established as a mixture of 33% reactive, 33% proactive, and 33% quality assurance but can adapt to the needs of the bedside team. The Penn E-lert mission is to provide highly reliable care within the health system. The tele-CCM team serves as the critical care consults hub for the multidisciplinary bedside staff who have the primary responsibility for patients. Penn E-lert actions could be triggered by a formalized review of patient medical records (proactive rounding). Several proactive tasks are well-defined to improve cooperativeness and homogeneity of responses (Supplementary Table 2). Tasks are also tailored to the provider's role in the system. eRTs and eRNs reported these tailored tasks as aggregated tasks. Prior video training assured common understanding by all staff.
The engagement was defined as any task related to patient care executed by a member of the team. An engagement by one member of the task force was independently executed from the action of other members. After initial reviews, eRNs and eRTs could escalate clinical issues to eMDs if they deemed the patient status severe enough to warrant intensivist review. eMDs would then review further and interact with bedside staff. The Penn E-lert and bedside staff could initiate interactions by either (1) engaging the emergency button installed in each ICU room or (2) contacting over the telephone by noting each other's mobile number as a member of the care team within the patient electronic medical record or, (3) engaging via an in-room audio-video system on the tele-CCM platform, or (4) using an asynchronous secure text message platform (22–24).
Routine tasks were addressed within 2 h, urgent tasks were addressed within 15 min, and emergent tasks demanded an immediate response. By default, proactive rounding was classified as a routine task unless other exceptional circumstances occurred.
Tasks were classified into six main categories: clinical intervention (any action to affect patient healthcare delivery), quality and assurance (review of the record or intervention to assure compliance with documentation), safety (intervention addressing potential harm), education (teaching provided to staff), debrief (review of complicated clinical situation, respectively), recording (documenting clinical situation per agreement with units), and others (unclassified). Any task could be classified with two of these descriptors.
Penn E-lert determined the need to communicate with the bedside team in response to engaging activity. In some cases, the intervention was terminated on review without requiring further external or internal communication. However, internal communication between members within Penn E-lert may still occur. For example, if communication with the bedside staff was needed, staff members connected via audio-video functions within the ICU room, telephone, secure text message, or consultation notes within the electronic medical record. At times, utilizing multiple communication avenues simultaneously were indicated within the survey.
At the end of an engagement, tasks' duration, complexity, and perceived difficulty spent on the task were recorded. Penn E-lert staff recorded their perception of the acceptance of the recommendation given during the interaction (accepted, acknowledged, not accepted) and if the engagement caused distress.
Data was collected between 9/1/2020 and 9/31/2021 using the final electronic REDCap survey database with staff inputting the data manually (Supplementary Material 1; Supplementary Figure 1) (25, 26). Each of the interventions is defined as “engagement” throughout the manuscript.
The Shapiro-Wilk W test and distribution plots were used to test the normality of distribution variables. Homogeneity of variance was evaluated with Levene's test. Parametric variables were expressed as mean ± SD and compared using a t-Student test. For multiple parametric comparisons, ANOVA was used with post-hoc Turkey's case. χ2 was used to compare the frequencies between ordinary and nominal variables. A double-sided p-value < 0.05 was considered statistically significant for all tests. Statistical analyses were performed with Statistica 11.0 (StatSoft Inc., Tulsa, OK) or SPSS (IBM; Amonk; NY).
Over the observed time, 2,286 engagements were recorded by eMD [nroutine = 1,551 (67.8%); nurgent = 559 (24.5%); nemergent = 171 (7.5%); nunclassified = 5 (0.2%). The majority of eMD tasks involved ARDS (40.5%), intensivist support (30.5%), and unstable trends (14.9%) (Figure 1A). eRNs executed 10,319 engagements [nroutine = 5,240 (50.8%); nurgent = 795 (7.7%); nemergent = 215 (2.1%); nunlassified = 4,069 (39.4%)]. RASS & delirium (38.7%), others (18.1%) and aggregated time (17.2%) were most commonly executed eRN tasks (Figure 1C). Finally, 27,310 engagements were recorded by eRTs [nroutine = 26,820 (98.2%); nurgent = 392 (1.4%); nemergent = 79 (0.3%); nunclassified = 19 (0.1%)] with the vast majority of tasks being routine and focusing on compliance (36.8%), deferring (16.7%) and SBT/SAT (15.4%) (Figure 1E).
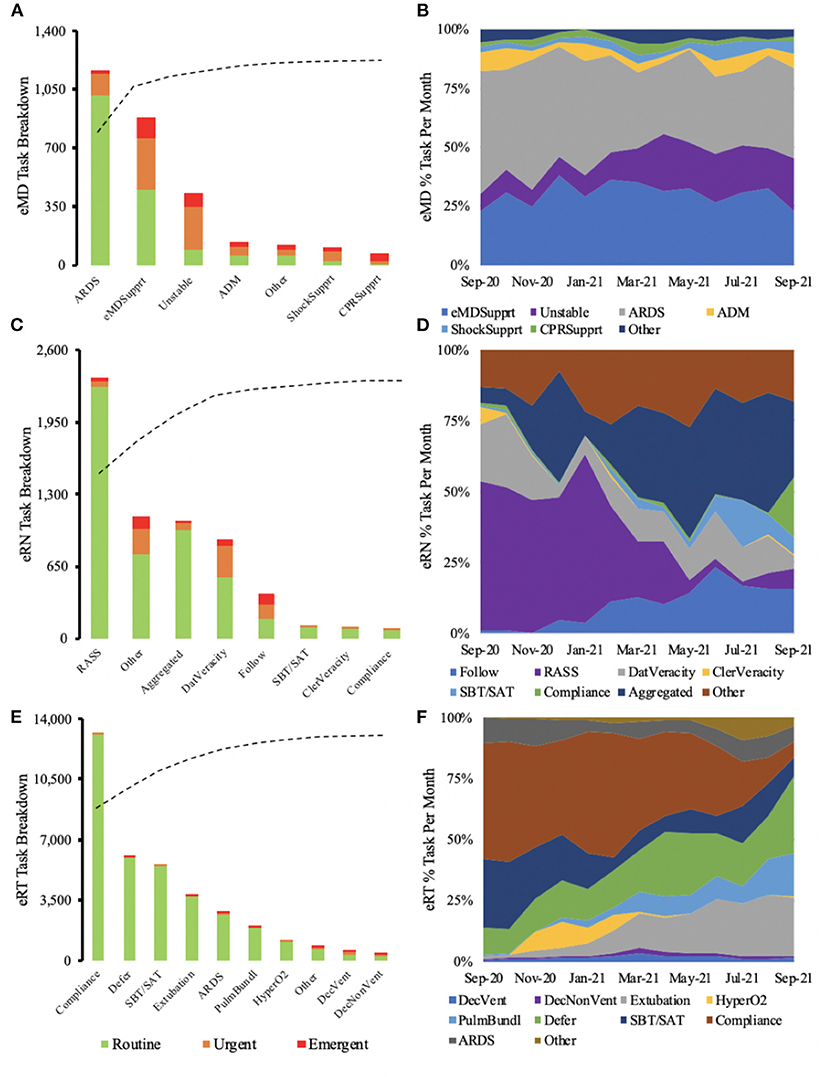
Figure 1. Majority of routine eMD tasks were associated with ARDS, while the majority of urgent and emergent interactions required eMD support (A). Over the year, eMD tasks remained similar, with a slight increase in tasks involving unstable patients toward the end of the year (B). eRN routine tasks were dominated by RASS (C), but when observed over the year, RASS saw a steep decline toward the end of the year (D). The majority of eRT routine tasks consisted of compliance (E). As time progressed, there was a decrease in compliance and an increase in task deference (F).
31.9% of eMD engagements were deemed urgent or emergent, significantly higher than eRN (9.8%) and eRT (1.7%). On the other hand, eRT had significantly more routine tasks 98.2%, compared to the other specialties (Figures 1A,C,E; Table 1). However, variability existed between providers in each group (Supplementary Figure 2).
There was a little fluctuation in the different tasks performed for eMD across the observed year (Figure 1B). eRNs saw a significant reduction in RASS & delirium with the expansion of aggregated tasks toward the end of the year (Figure 1D). eRTs tasks switched from predominant compliance to defer and extubation (Figures 1E,F).
There were significant differences in the time devoted to the tasks depending on the expediency across the different specialties (Figure 2). The average intervention took 16.13 ± 10.39 min for eMDs, 18.1 ± 16.23 for eRNs, and 8.19 ± 4.98 min for eRTs. Again, there were significant differences in time spent for different completing different assignments (Figure 2).
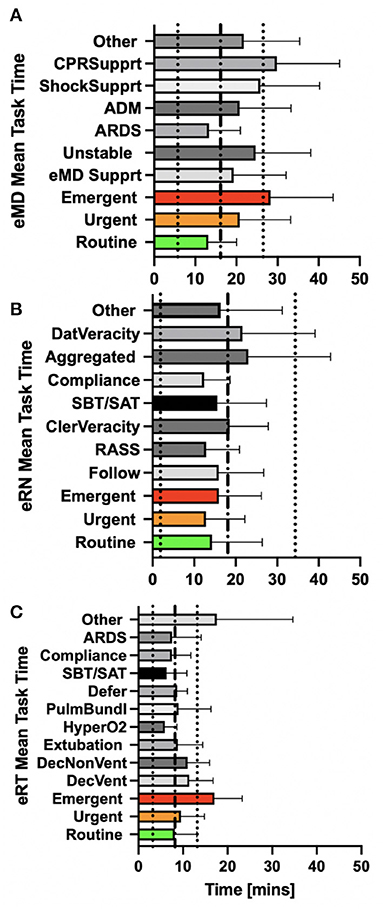
Figure 2. eMDs spent more time on tasks requiring CPR support followed by tasks that were deemed emergent (A). eRNs spent the most time on aggregated patient tasks (B). eRTs spent the most time on tasks described as other (C).
Initially, pro-active rounding triggers dominated with subsequent increases in ARDS autonomous algorithm triggers, telephone calls, secure text messages, and communications within the tele-CCM module in the electronic medical record (Figure 3A).
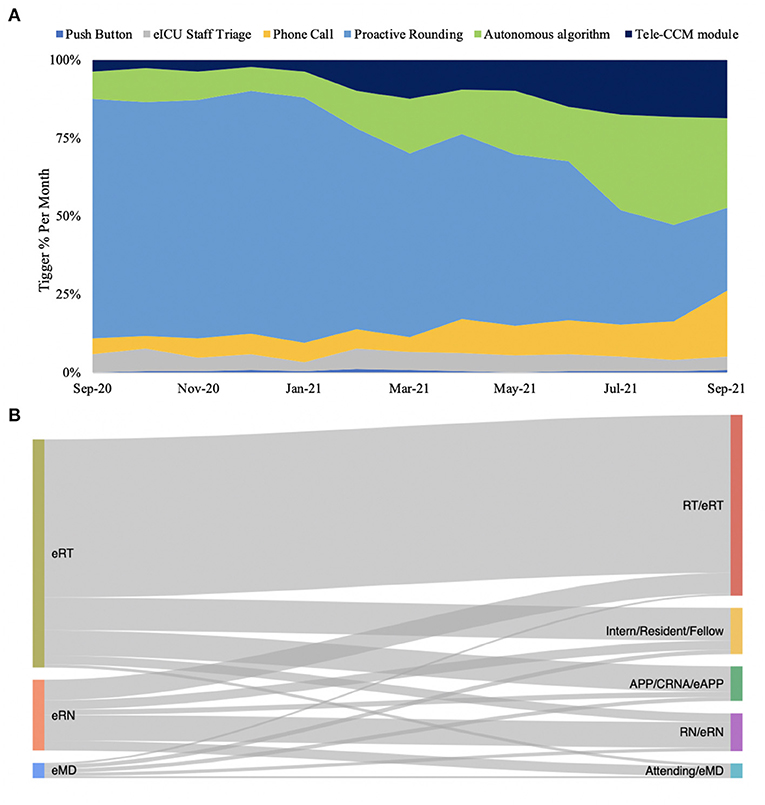
Figure 3. Push button was the greatest trigger for eMD, eRN and eRTs overall but there was a slight increase in Sniffer and Phone calls as triggers near the end of the year (A), with the most significant amount of communication involving RT/eRTs (B).
With eMD, eRN, and eRT engagements combined, no follow-up communication occurred in 70.1% of engagements, while communication did occur in 29.9% of recorded engagements. Among the Penn e-Lert staff, eRT communicated more frequently with bedside staff (% MD = 37.8%; % RN = 36.8, % RT = 49.0%). In cases when communication occurred between Penn E-lert and bedside staff, a significant variation between eMD, eRT, and eRN communication patterns were seen (Figure 3B; Supplementary Table 3). The eRNs communicated much more frequently amongst the Penn E-lert staff, while eMDs and eRTs communicated mostly with bedside staff (Figure 3B; Supplementary Table 3). eMDs communicated with various bedside stakeholders while eRNs engaged predominantly with bedside RNs.
There was a significant variance in the tasks delivered to each hospital and a significant variance across the different ICUs within each hospital (Figure 4, Supplementary Figure 5). Hospital 4 and 7 required more frequent ARDS interventions, while Hospital 1 utilized Penn E-lert eMDs (Figure 4A). Clinical follow-up dominated services provided to Hospital 4, Hospital 7, and Hospital 6, while RASS & delirium were the primary engagements within Hospital 5 in the case of eRTs. In the case of eRT, the task executed were remarkably heterogeneous, with deferring being at the highest incidence in Hospital 2 and Hospital 7. Hospital 3 predominantly requested unstable vented and unstable non-vented, while Hospital 4 requested compliance. Similar services were regionalized between units of the same profile regarding services provided by eMDs, eRTs, and eRNs (Supplementary Figure 5).
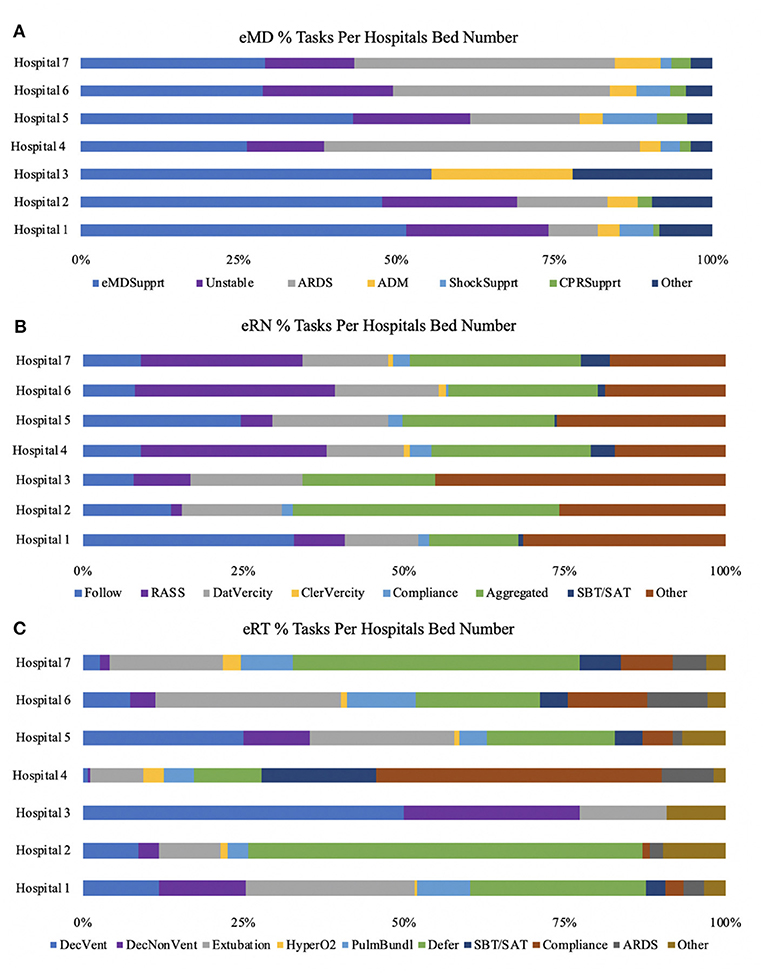
Figure 4. Percentages of tasks performed varied for each specialty based on the different hospitals. eMD support made up a large percentage of all hospital systems (A). eRN tasks consisting of RASS was most significant across the larger hospital systems (hospital 4,6,7) (B). eRTs had more task variability across the different hospital systems, but critical tasks were deference, extubation, and declining vent (C).
The outcomes of the tele-CCM services can be measured in several ways. There was a total of 465 emergent and 1,746 urgent engagements. The push-button trigger was utilized in 132 and 21 of these engagements. These situations represent conditions where the level of the healthcare delivery was not adequate, triggering requests from the bedside for immediate support to advert clinical deterioration and thereby reducing mortality.
There were 2,641 aggregated tasks by eRNs that turned into 393 engagements consisting of checking alarms (n = 107, 27%), high risk extubation elements (n = 79, 20%), GI and DVT prophylaxis (n = 66, 7%), admissions (48, 12%), and other (n = 43, 11%). These engagements represent situations in which routine tasks turned into clinical interventions to avoid clinical deterioration and thereby reduce morbidity.
Finally, surveillance of compliance with hyperoxia avoidance and ARDS triggered by the autonomous algorithm resulted in modification of ventilator setting in and hyperoxia (n = 25, 6%), ARDS (n = 25, 6%). More importantly, Penn E-lert staff were able to identify ARDS-like patients earlier than the ARDS detection algorithm in 1,097 cases triggering the clinical adjustment in treatment when counting both eMD and eRT engagements.
Not surpassingly, COVID-19 patients were deferred more frequently to eRT service as compared to non-COVID patients. A total of 1,636 engagements involving COVID-19 patients were deferred to eRT staff resulting in PPE saving an amount of $41,848.88 and a total time of 272 h or roughly 11 days (27). A total of 3,027 engagements involving non-COVID-19 patients occurred, but we do not know how many were for the patients in isolation.
A significant number of the interactions were not specified in terms of acceptance as reported by Penn E-lert staff (eMD = 67.8% eRN = 64%; eRT= 54.4%). In cases when tele-CCM staff ranked the level of acceptance, eRT's reported excessive number of interactions described as rejected (Supplementary Table 4). However, eRNs had the highest ratio of interactions with “reject” as characterization while eMDs the lowest (% RejectedeMD = 1%; % RejectedeRN = 1.4%; % RejectedeRT = 1.2%) (Supplementary Figure 3; Supplementary Table 4).
eRTs reported no distressful interactions, while eMDs had a distressing rate of 1.8% and eRNs had a rate of 1.9%. The different levels of interaction expediency had similar rates of distress, but certain hospital services had a significantly higher level of distressful interactions per bed (Supplementary Figure 4).
This is the first study detailing the workflow of the tele-CCM unit to foster a highly reliable service within the health system. The Tele-CCM team served as the critical care consultation hub for the multidisciplinary bedside staff who had primary responsibility for the patients. Our model utilized a pyramid model where eRTs and eRNs responded and analyzed the data provided by a computer system or a pre-defined list of tasks (28). If unable to address the problem, the case was escalated to an eMD. This model is optimal for utilizing expertise and skills by different providers.
We demonstrated that eRNs and eRTs effectively adopted the workflow to filter and assess the information provided by several clinical inputs to direct the work of eMD. Consequently, eRT and eRN tasks were dominated by routine tasks while eMDs responded to emergencies and urgent calls. eMD engagements were significantly longer. Across all healthcare providers, longer engagement times were seen during urgent and emergent tasks (29). This finding is consistent with the observation that emergencies are more engaging and complex. Also, an estimate of how long it takes to address the emerging clinical issues determines system operational capability. We determine that eRN or eMD can address around 36 interactions per 12-shift, a maximum of 16 min per interaction. In the case of eRTs, that capacity was significantly higher (~60 per shift). These numbers may guide staffing needs. No study has addressed the critical issue of engagement duration, and current estimates are opinion-based (30).
There was significant variability in tasks executed over time among eRN and eRT but not eMD. This may suggest that eMD reacted to eRN and eRT nudges generated during the proactive rounding. However, the eRN and eRT proactive rounding significantly fluctuated over time and may reflect adaptability to changing demand during waves of COVID-19 and adapting policies and priorities of the hospital. Emergent and urgent tasks tended to happen during night shifts, as has been published before (31).
We demonstrated a very high regionalization in the care delivered even between the units of similar profiles. Though this may represent a difference in the case mix, it may also reflect that different cultures and staffing models in these locations produced a unique set of demands that teleCCM staff could actively augment. Consequently, teleICU programs should be tailored to the needs of the bedside providers (32). In the case of our program, these needs were gradually adopted and modified by the staff as reflected in the change from proactive tasks to engagements triggered by specific inputs (tele-CCM module, automated alarms). The phenomenon of service customization was frequently suggested but rarely quantified (33). Remarkably, teleCCM services evolved, suggesting that the remote service providers adapted their behavior based on their needs (34). The importance of this observation allows determining how long it takes for teleCCM service to mature. Furthermore, we demonstrated that staff could find novel, or more efficient ways, to utilize the system and provide more accurate delivery via organic and grassroots processes. This study provides an indirect suggestion supporting this observation (35).
We demonstrated that most tasks did not trigger communication outside tele-CCM providers. This may reflect a high degree of triggered non-actionable alerts, a common healthcare problem. Additionally, the Penn E-lert team often deemed the engagements undertaken by the bedside team to be appropriate (36). However, the exact nature of engagements without communication remains unclear.
As mentioned above, we captured a high degree of internal collaboration within the remote site, while a minority of these cases resulted in interaction with bedside staff. These interactions occurred via all available communication channels with the variability of communication modes among eRN and eMD based on bedside stakeholders. In contrast, eRT collaborated mostly with RT at the bedside. These differences may reflect the high burden of protocolized tasks for eRTs compared to the tasks of MDs and eRNs. As a result, their workflow may be less protocolized and require staff to address unique problems more frequently.
The quantification of service benefits was demonstrated on several levels. Earlier recognition of ARDS and subsequent less frequent emergence of ARDS clearly demonstrate a measurable effect on clinical care (37). A similar actuarial calculation can be done for push-button situations, missed deep venous thrombosis prophylaxis, and stress ulcer prophylaxis. These interactions avert clinical deterioration and thereby reduce morbidity (38). Implementation of eRT, eRN, and eMD instead of bedside staff reduced PPE use and staff exposure to COVID-19 (4).
The acceptance rate for the recommendation varied considerably between the hospitals and units. Some hospitals implemented Penn E-lert significantly longer than others. The duration of engagement fosters trust and acceptance of recommendation. However, we did not account for the nature of interactions between bedside and remote teams as well as the acceptance of the technology (39).
Finally, we were able to quantify the rate of distress during engagements among the remote ICU staff at roughly ~2%. In a very limited post-hoc interview, the primary drivers were the lack of control and professionalism in conversations (40). Interestingly, a dominant factor in the frequency of stressful interactions was not the role of stakeholders but the entity interacted (41). Again, this may reflect challenges with the early adoption of telemedicine within certain hospitals (38).
The study has a couple of limitations. First, the data was entered by Penn E-lert staff voluntarily. We estimated that several interactions were not entered, especially those considered routine. This may account for significant differences in the type and volume of entries by different providers. We estimate that 30% of entries are most likely missing from the survey. Although several tasks were highly standardized and consistent, and educational materials were provided to reinforce the data collection definitions and expectations over time, there is a possibility of a different interpretation. High variability between providers in recorded numbers of entries may results in over-representation of a particular type of attending vs. those who tend to file less. Staff estimated time without corroboration with more independent measures. The service demand may change based on patient severity scores, but this data was not accessible during this analysis. Finally, REDCap survey tool was insufficient in capturing all the tasks delivered if they were not pre-programmed.
We quantified the interactions of the tele-CCM staff in terms of their nature, duration, expediency, and value. High regionalization of service delivery and distress were observed, suggesting that delivery of tele-CCM services has to be tailored to the needs of the specific beneficiary of tele-CCM services.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Considering this is a quality and improvement project, the study is exempted from IRB's approval.
KL: conceptualization, data collection, manuscript writing, and reviewing. MS, AH, MW, and JJ: execution and manuscript reviewing. JW: data visualization and manuscript reviewing. CH: execution, funds acquisition, and manuscript reviewing. All authors reviewed the final version of the manuscript and agreed to its publication.
We would like to thank the PENN E-lert's staff, for able assistance.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.883126/full#supplementary-material
eMD, telemedicine medical doctor; eRN, telemedicine registered nurse; eRT, telemedicine respiratory therapist; eTHC, telehealth coordinator team; tele-CCM, tele-critical care medicine; TCC, telemedicine critical care; ARDS, acute respiratory distress syndrome; ADM, admissions; ShockSupprt, shock support; CPRSupprt, cardiopulmonary resuscitation support; SBT/SAT, spontaneous breathing trial/spontaneous awakening trial; DecVent, intubated patient status declining; DecNon Vent, non-intubated patient status declining; HyperO2, Hyperoxia; PulmBundl, pulmonary bundle protocol; DVT, deep vein thrombosis; GI; Gastrointestinal.
1. Becker C, Frishman WH, Scurlock C. Telemedicine and Tele-ICU: the evolution and differentiation of a new medical field. Am J Med. (2016) 129:e333–4. doi: 10.1016/j.amjmed.2016.05.045
2. Anders SH, Woods DD, Schweikhart S, Ebright P, Patterson E. The effects of health information technology change over time: a study of Tele-ICU functions. Appl Clin Inform. (2012) 3:239–47. doi: 10.4338/ACI-2011-12-RA-0073
3. Lilly CM, McLaughlin JM, Zhao H, Baker SP, Cody S, Irwin RS. A multicenter study of ICU telemedicine reengineering of adult critical care. Chest. (2014) 145:500–7. doi: 10.1378/chest.13-1973
4. Srinivasan SR. Editorial: tele-ICU in the age of COVID-19: built for this challenge. J Nutr Health Aging. (2020) 24:536–7. doi: 10.1007/s12603-020-1376-6
5. Lieneck C, Weaver E, Maryon T. Outpatient telehealth implementation in the United States during the COVID-19 global pandemic: a systematic review. Medicina. (2021) 57:462. doi: 10.3390/medicina57050462
6. Venditti A, Ronk C, Kopenhaver T, Fetterman S. Tele-ICU “myth busters”. AACN Adv Crit Care. (2012) 23:302–11. doi: 10.4037/NCI.0b013e31825dfee2
7. Lilly CMFK, Ries M, Pastores S, Vender J, Pitts JA, Hanson WC. A national tele-ICU survey. Chest. (2012) 142:40–7. doi: 10.1378/chest.12-0310
8. Vranas KC, Slatore CG, Kerlin MP. Telemedicine coverage of intensive care units: a narrative review. Ann Am Thorac Soc. (2018) 15:1256–64. doi: 10.1513/AnnalsATS.201804-225CME
9. Reynolds HN. The tele-ICU: formative or out-of-date or both? Practice models and future directions. In: Koenig MA, editor. Telemedicine in the ICU. Cham: Springer International Publishing (2019). p. 3–19.
10. Blewett LA, Osterholm MT. What's next for the US health care system after COVID-19? Am J Public Health. (2020) 110:1365–6. doi: 10.2105/AJPH.2020.305836
11. Becker CD, Yang M, Fusaro M, Fry M, Scurlock CS. Optimizing tele-ICU operational efficiency through workflow process modeling and restructuring. Crit Care Expl. (2019) 1:e0064. doi: 10.1097/CCE.0000000000000064
12. Kahn JM, Rak KJ, Kuza CC, Ashcraft LE, Barnato AE, Fleck JC, et al. Determinants of intensive care unit telemedicine effectiveness. An ethnographic study. Am J Resp Crit Care Med. (2019) 199:970–9. doi: 10.1164/rccm.201802-0259OC
13. Krupp A, Di Martino M, Chung W, Chaiyachati K, Agarwal AK, Huffenberger AM, et al. Communication and role clarity inform TeleICU use: a qualitative analysis of opportunities and barriers in an established program using AACN framework. BMC Health Serv Res. (2021) 21:277. doi: 10.1186/s12913-021-06287-6
14. Xyrichis A, Iliopoulou K, Mackintosh NJ, Bench S, Terblanche M, Philippou J, et al. Healthcare stakeholders' perceptions and experiences of factors affecting the implementation of critical care telemedicine (CCT): qualitative evidence synthesis. Cochrane Database Syst Rev. (2021) 2:Cd012876. doi: 10.1002/14651858.CD012876.pub2
15. Williams LS, Johnson E, Armaignac DL, Nemeth LS, Magwood GS. A mixed methods study of tele-ICU nursing interventions to prevent failure to rescue of patients in critical care. Telemed J Ehealth. (2019) 25:369–79. doi: 10.1089/tmj.2018.0086
16. Ramnath VR, Khazeni N. Centralized monitoring and virtual consultant models of tele-ICU care: a side-by-side review. Telemed J Ehealth. (2014) 20:962–71. doi: 10.1089/tmj.2014.0024
17. Kumar S, Merchant S, Reynolds R. Tele-ICU: efficacy and cost-effectiveness of remotely managing critical care. Perspect Health Inf Manag. (2013) 10:1f. doi: 10.2174/1874431101307010024
18. Reynolds HN, Bander J, McCarthy M. Different systems and formats for tele-ICU coverage: designing a tele-ICU system to optimize functionality and investment. Crit Care Nurs Q. (2012) 35:364–77. doi: 10.1097/CNQ.0b013e318266bc26
19. Mullen-Fortino M, DiMartino J, Entrikin L, Mulliner S, Hanson CW, Kahn JM. Bedside nurses' perceptions of intensive care unit telemedicine. Am J Crit Care. (2012) 21:24–31; quiz 2. doi: 10.4037/ajcc2012801
20. Hoonakker PLT, Pecanac KE, Brown RL, Carayon P. Virtual collaboration, satisfaction, and trust between nurses in the tele-ICU and ICUs: results of a multilevel analysis. J Crit Care. (2017) 37:224–9. doi: 10.1016/j.jcrc.2016.10.018
21. Canfield C, Galvin S. Bedside nurse acceptance of intensive care unit telemedicine presence. Crit Care Nurse. (2018) 38:e1–4. doi: 10.4037/ccn2018926
22. Registered Respiratory Therapist (RRT): National Board for Respiratory Care. (2020). Available online at: https://www.nbrc.org/examinations/rrt/ (accessed July 7, 2020).
23. Armaghan R, Geesey B, Juby J, Amador-Castaneda J, Bollinger A, Roberts KJ, et al. Practice of respiratory therapists in pennsylvania: a statewide survey. Respir Care. (2020) 65:973. doi: 10.4187/respcare.07153
24. Poston JT, Patel BK, Davis AM. Management of critically ill adults with COVID-19. JAMA. (2020) 323:1839–41. doi: 10.1001/jama.2020.4914
25. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. (2019) 95:103208. doi: 10.1016/j.jbi.2019.103208
26. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42:377–81. doi: 10.1016/j.jbi.2008.08.010
27. Barklan J. Analysis: PPE Costs Increase Over 1,000% During COVID-19 Crisis. McKnight Long-Term Care News (2020).
28. Radogna AV, Capone S, Di Lauro GA, Fiore N, Longo V, Giampetruzzi L, et al. A Novel Tele-Medicine System to Improve Therapy Monitoring in Chronic Respiratory Diseases. Cham: Springer International Publishing (2019).
29. Lurie N, Carr BG. The role of telehealth in the medical response to disasters. JAMA Intern Med. (2018) 178:745–6. doi: 10.1001/jamainternmed.2018.1314
30. Ramakrishnan M, Taduru SS, Patel P, Younis M, Hamarshi M. External intensivists versus in-house intensivists: analysis of outcomes of nighttime coverage of ICUs by external on-call and in-house on-call intensivists. Mo Med. (2019) 116:331–5.
31. Ganesan S, Magee M, Stone JE, Mulhall MD, Collins A, Howard ME, et al. The impact of shift work on sleep, alertness and performance in healthcare workers. Sci Rep. (2019) 9:4635. doi: 10.1038/s41598-019-40914-x
32. Rogove H. How to develop a tele-ICU model? Crit Care Nurs Quart. (2012) 35:357–63. doi: 10.1097/CNQ.0b013e318266bdf5
33. Broens TH, Huis in't Veld RM, Vollenbroek-Hutten MM, Hermens HJ, van Halteren AT, Nieuwenhuis LJ. Determinants of successful telemedicine implementations: a literature study. J Telemed Telecare. (2007) 13:303–9. doi: 10.1258/135763307781644951
34. Becker CD, Forman L, Gollapudi L, Nevins B, Scurlock C. Rapid implementation and adaptation of a telehospitalist service to coordinate and optimize care for COVID-19 patients. Telemed J E Health. (2021) 27:388–96. doi: 10.1089/tmj.2020.0232
35. Armaignac DL, Saxena A, Rubens M, Valle CA, Williams LS, Veledar E, et al. Impact of telemedicine on mortality, length of stay, and cost among patients in progressive care units: experience from a large healthcare system. Crit Care Med. (2018) 46:728–35. doi: 10.1097/CCM.0000000000002994
36. Brilli RJ, Spevetz A, Branson RD, Campbell GM, Cohen H, Dasta JF, et al. Critical care delivery in the intensive care unit: defining clinical roles and the best practice model. Crit Care Med. (2001) 29:2007–19. doi: 10.1097/00003246-200110000-00026
37. Zumstein KK, Lamphere TR, Powell SA, Solly WR, Moran A, Kellar B, et al. Using tele-ICU to provide respiratory therapy students experience with COVID-19 patients. Respiratory Care. (2021) 66(Suppl. 10):3604761.
38. Becker CD, Fusaro MV, Al Aseri Z, Millerman K, Scurlock C. Effects of telemedicine icu intervention on care standardization and patient outcomes: an observational study. Crit Care Expl. (2020) 2:e0165. doi: 10.1097/CCE.0000000000000165
39. Franzini L, Sail KR, Thomas EJ, Wueste L. Costs and cost-effectiveness of a telemedicine intensive care unit program in 6 intensive care units in a large health care system. J Crit Care. (2011) 26:329. e1–6. doi: 10.1016/j.jcrc.2010.12.004
40. Piquette D, Reeves S, LeBlanc VR. Stressful intensive care unit medical crises: how individual responses impact on team performance. Crit Care Med. (2009) 37:1251–5. doi: 10.1097/CCM.0b013e31819c1496
41. Mascayano F, van der Ven E, Moro MF, Schilling S, Alarcón S, Al Barathie J, et al. The impact of the COVID-19 pandemic on the mental health of healthcare workers: study protocol for the COVID-19 HEalth caRe wOrkErS (HEROES) study. Soc Psychiatry Psychiatric Epidemiol. (2022) 2022:1–13. doi: 10.1007/s00127-021-02211-9
Keywords: tele-ICU, tele-CCM, critical care, workflow, communication, intensive care unit, distress, implementation
Citation: Laudanski K, Huffenberger AM, Scott MJ, Williams M, Wain J, Jablonski J and Hanson CW III (2022) Operation analysis of the tele-critical care service demonstrates value delivery, service adaptation over time, and distress among tele-providers. Front. Med. 9:883126. doi: 10.3389/fmed.2022.883126
Received: 24 February 2022; Accepted: 28 June 2022;
Published: 05 August 2022.
Edited by:
Sairam Parthasarathy, University of Arizona, United StatesReviewed by:
Juliana Nichterwitz Scherer, University of the Rio dos Sinos Valley, BrazilCopyright © 2022 Laudanski, Huffenberger, Scott, Williams, Wain, Jablonski and Hanson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Krzysztof Laudanski, a2xhdWRhbnNraUBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.