
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CLINICAL TRIAL article
Front. Med. , 06 May 2022
Sec. Rheumatology
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.878218
This article is part of the Research Topic Primary Sjögren's Syndrome: From Immunological to Rheumatological Aspects View all 8 articles
A commentary has been posted on this article:
Commentary: Efficacy and safety of acupuncture on symptomatic improvement in primary Sjögren's syndrome: A randomized controlled trial
 Xinyao Zhou1†
Xinyao Zhou1† Haodong Xu1,2†
Haodong Xu1,2† Jinzhou Chen1,3†
Jinzhou Chen1,3† Hengbo Wu1,4
Hengbo Wu1,4 Yi Zhang1,5
Yi Zhang1,5 Feng Tian6
Feng Tian6 Xiaopo Tang1
Xiaopo Tang1 Huadong Zhang1
Huadong Zhang1 Lin Ge1
Lin Ge1 Kesong Li1
Kesong Li1 Wen Jiang1
Wen Jiang1 Zhishun Liu7*
Zhishun Liu7* Quan Jiang1*
Quan Jiang1*
Aim: We sought to evaluate the efficacy of acupuncture in treating the main symptoms of primary Sjögren’s syndrome, specifically dryness, pain, and fatigue.
Methods: A total of 120 patients with primary Sjögren’s syndrome were randomized in a parallel-group, controlled trial. Participants received acupuncture or sham acupuncture for the first 8 weeks, then were followed for 16 weeks thereafter. The primary outcome was the proportion of participants with a ≥ 30% reduction in ≥ 2 of 3 numeric analog scale scores for dryness, pain, and fatigue. The secondary outcomes included the European League Against Rheumatism (EULAR) Sjögren’s Syndrome Patient-reported Index (ESSPRI); the EULAR Sjögren’s Syndrome Disease Activity Index; the Schirmer test score; unstimulated saliva flow; serum immunoglobulin G, A, and M concentrations; the Medical Outcome Study Short Form 36 score; salivary gland ultrasound imaging; and the Hospital Anxiety and Depression Scale score.
Results: The proportions of patients meeting the primary endpoint were 28.33% (17/60) in the acupuncture group and 31.66% (19/60) in the sham group, without a statistically significant difference (P = 0.705). The IgG concentration at week 16 and the homogeneity in ultrasonography of the salivary glands at week 8 showed significant differences between the 2 groups (P = 0.0490 and P = 0.0334, respectively). No other differences were observed between the 2 groups. ESSPRI and unstimulated saliva flow were improved in both groups compared to baseline, albeit with a significant difference between them.
Conclusion: In patients with primary Sjögren’s syndrome, acupuncture did not satisfactorily improve symptoms compared to placebo. However, interesting discoveries and possible underlying reasons were demonstrated and discussed, which may be useful to studies in the future.
Clinical Trial Registration: [www.ClinicalTrials.gov], identifier [NCT02691377].
Primary Sjögren’s syndrome (pSS) is a systemic autoimmune disease (1) with the main symptoms of dryness, pain, and fatigue (2), which causes physical and psychological discomfort (3) and reduces the quality of life among both patients whose exocrine glands are affected and those with multiorgan dysfunction. Available treatments are only partially effective for symptom improvement. In the relief of dryness, toadstool alkali agonist showed some effect (4) through the stimulation of salivary secretion. However, in the alleviation of pain and fatigue, no sufficient (5) evidence of treatment efficacy exists thus far. Three randomized controlled trials (RCTs) of hydroxychloroquine (6) were conducted, but none of them reported any statistical improvement in those main symptoms, and a number of studies on infliximab and etanercept (7) left uncertain conclusions about symptom melioration.
Acupuncture, a non-drug therapy that originated in China and has spread worldwide, is often used to improve physical symptoms (8), including dryness, pain, and fatigue. It has been applied for the treatment of Sjögren’s syndrome, but the evidence of its effectiveness is inadequate. A systematic review (9) studied the efficacy of acupuncture on xerostomia and salivary production, but it included 10 RCTs of low quality and was therefore inconclusive. Another systematic review (10) suggests that acupuncture is related to better treatment of dry mouth and eyes in pSS. Due to the uncertainty of the effectiveness of acupuncture in patients with pSS, higher-quality RCTs are necessary to study the efficacy and safety of acupuncture in pSS.
Therefore, in this study, we aimed to evaluate the efficacy of acupuncture on the improvement of the main symptoms (dryness, pain, and fatigue) of pSS over an 8-week treatment period and assess the maintenance of effectiveness throughout a 24-week follow-up period.
This randomized, parallel, sham-controlled trial was conducted at Guang’anmen Hospital (GAMH), China Academy of Chinese Medical Sciences, in Beijing, China. The study course per patient was 24 weeks; baseline measurements were taken at week 0, then followed by 8 weeks of treatment with 20 sessions of acupuncture and 16 weeks of follow-up assessments.
Patients were included if they were diagnosed as having primary SS according to the American–European Consensus Group (11) classification criteria, had a disease course of < 10 years, and were > 18 years old. Moreover, they either had to have not taken any medicines for pSS, or had to have stopped them for ≥ 4 weeks before recruitment, or had to be taking the same kinds and doses of non-steroidal anti-inflammatory drugs, oral glucocorticoids, cholinergic agonists, artificial eye drops, and herbal decoctions for ≥ 4 weeks before recruitment, or had to be taking the same kinds and doses of immunosuppressants (e.g., Tripterygium wilfordii, methotrexate, cyclophosphamide, cyclosporin, azathioprine, and hydroxychloroquine sulfate) for > 6 months before recruitment.
Participants who met one of the following conditions were excluded: had secondary Sjögren’s syndrome; had a serious systemic disorder (e.g., lymphoma; central nervous system, renal, or pulmonary involvement; myositis; or vasculitis) or severe renal or liver failure; had a history of acupuncture treatments within last 20 days; had an acupuncture contraindication (e.g., allergy to metals, skin lesions on relative acupoints, etc.); had participated in any other clinical trials within the last 30 days before recruitment; were planning to be pregnant or were at risk of becoming pregnant (i.e., no contraception use); had a physical or psychological problem that might confound the trial results, interfere with other subjects’ participation, or might make it risky to follow the investigators’ requirements; and were known for or showed persistent drug or alcohol abuse.
Participants were allocated to the acupuncture or sham acupuncture (SA) group with equal chance, based on randomization assignments using a sequence of numbers generated using the Statistical Analysis System version 9.2 (SAS Institute, Cary, NC, United States) by the Institute of Basic Research in Clinical Medicine, China Academy of Chinese Medical Sciences. These assignments were sent to a study member, who placed them into sealed, opaque envelopes with dates and signature labels placed over the seals. This study member subsequently did not take part in any patient interviews, acupuncture sessions, data collection, or statistical analysis. Except for the acupuncturist, all relevant parties were blinded.
During weeks 0–8, 120 patients were randomly treated with acupuncture or SA 3 times a week for the first 4 weeks, then 2 times a week for the next 4 weeks. The needles of the 2 study arms were indistinguishable in appearance and feelings brought to patients. The sham needles were 0.30 mm wide and 25 mm long (12) and consisted of an adhesive pad with a blunt tip. The adhesive pad was made of a sterile cylindrical polyethylene foam (10 mm in diameter and 5 mm in height) with adhesive tape at the bottom. In all, the only difference between the normal and sham needles was that the tips of the sham needles did not taper (13). In the acupuncture group, Hwato acupuncture needles (40 × 0.25 mm; Suzhou Medical Appliance Factory, Suzhou, China) were used. The acupoints used in the acupuncture/SA groups were as follows: bilateral Wai guan (SJ5), bilateral Zhaohai (KI6), Cheng-jiang (RN24), Lianquan (RN23), bilateral Tai yang (EX-HN5), bilateral Cuanzhu (BL2), bilateral Sizhukong (SJ23), and bilateral Jiache (ST6). Equal manipulation via twirling, lifting, and thrusting motions of all needles was performed in the acupuncture group but not in the sham group. Needles in both arms were kept in place for 30 min each session, with the Deqi sensation present only in the acupuncture group (14). The same qualified and registered clinical acupuncturist was trained to maintain consistent performance in both the acupuncture and SA groups by following the standard operating procedure formula. After the 8-week intervention, patients were followed for another 16 weeks to evaluate the long-term effectiveness of treatment.
The primary outcome was the proportion of patients with a ≥ 30% improvement in ≥ 2 of 3 numeric analog scale (NAS) scores for dryness, pain, and fatigue after intervention at week 8 compared to baseline. NAS scores (0–10 points, with 0 points for the best, 10 points for the worst) were requested 3 times a week in week 1–4, and 2 times a week in week 5–8, in total of 20 NAS scores in 8-week intervention, and in week 12, 16, 20, and 24 for follow-up with different measurements. The mean scores of NAS from weeks 2 to 8 were set as the primary endpoint, while those of week 0 were considered the baseline NAS scores. The methodology and evidence of setting the requirement of a ≥ 30% improvement in ≥ 2 of 3 indicators is closely related to clinical efficacy and are consistent or similar to the main results of multiple previous clinical trials (5, 8, 15).
The secondary outcomes included NAS scores (mean ± standard deviation [M ± SD]) for dryness, pain, and fatigue as well as the European League Against Rheumatism (EULAR) Sjogren’s syndrome Patient-reported Index (ESSPRI); the EULAR Sjögren’s Syndrome Disease Activity Index (ESSDAI) (16); the Medical Outcome Study Short Form 36 (SF-36) score; the Hospital Anxiety and Depression Scale (HADS) score (17); the Schirmer test score; unstimulated saliva flow; the erythrocyte sedimentation rate (ESR); the C-reactive protein (CRP) level; serum immunoglobulin (Ig) G, IgA, and IgM levels; and an ultrasound examination of the salivary gland structures.
All salivary gland ultrasonography examinations were performed independently by the same examiner with professional training and sufficient operating experience. Homogeneity, the presence of hypoechogenic areas and hyperechogenic reflections, and the clearness of salivary gland borders were scored according to the scoring system proposed by De Vita (18, 19). The scores of these 4 parameters for the 4 salivary glands were then summed up, ranging from 0 to 48 points for each. Scores calculated at weeks 0 and 8, respectively, were compared.
The sample size was pre-decided by the hypothesized primary outcome. According to an existing literature review (5), the proportion of patients who reported a ≥ 30% improvement in NAS scores of ≥ 2 of the 3 items with placebo treatment was 17.9%. We used this proportion for our placebo group because no data were available for SA at the time. A sample size of 52 patients per group would be sufficient to detect a 2% null difference in proportions, with a 2-sided 5% level of significance and a power of 80%. The number of subjects was increased to 60 participants in each group (for a total of 120 participants) when a dropout rate of 15% was taken into consideration.
Statisticians and investigators were blinded to the patients’ allocation. Statistical analysis was performed using Stata version 15.1 (StataCorp LLC, College Station, TX, United States) and GraphPad Prism version 8.4 (GraphPad Software, San Diego, CA, United States). We used the first ESSPRI and NAS scores as the baseline scores. Thus, participants without a single session of acupuncture were excluded from statistical analysis. Missing data for the primary outcome were extrapolated using the last-observation-carried-forward (LOCF) approach.
Continuous data are presented using M ± SD values if they were normally distributed; otherwise, they are presented as median ± interquartile range values. Categorical data are presented as frequencies and percentages. In comparisons between the 2 groups, the chi-squared test or Fisher’s exact test was used for primary outcomes. For secondary outcomes, a t-test was used if the data were normally distributed; otherwise, the Wilcoxon rank-sum test was applied. An analysis of covariance was used for the baseline adjustment analysis of continuous data. For repeated outcome measurements, a general linear model was used for analyzing continuous data.
The threshold of statistical significance of the 2-tailed P-value was 0.05. For repeated outcome measurements, the P-values were corrected using the Huynh–Feldt adjustment method.
From March 2016 to September 2018, 120 patients with pSS treated at GAMH were recruited into this trial (ClinicalTrials.gov identifier: NCT02691377). The last follow-up assessment of the last patient was completed on March 11, 2019.
All 120 patients were equally (60 patients per group) and randomly assigned to the acupuncture or SA group. The mean age was 56.7 ± 8.2 years in the SA group and 53.8 ± 12.1 years in the acupuncture group, and 88.3% of patients in the SA group and 98.3% of patients in the acupuncture group were female. The disease course of pSS was 35.3 ± 29.4 months in the SA group and 28.9 ± 23.4 months in the acupuncture group, respectively. There were no significant differences in any characteristics between the 2 groups at baseline. Fourteen participants (11.67%) at week 8 and 30 patients (33.3%) at week 24 were lost to follow-up; these losses to follow-up and their reasons are further described in Figure 1. Study participants’ demographic characteristics and concomitant treatment are summarized in Table 1 and their ESSDAI domains are discussed in Table 2.
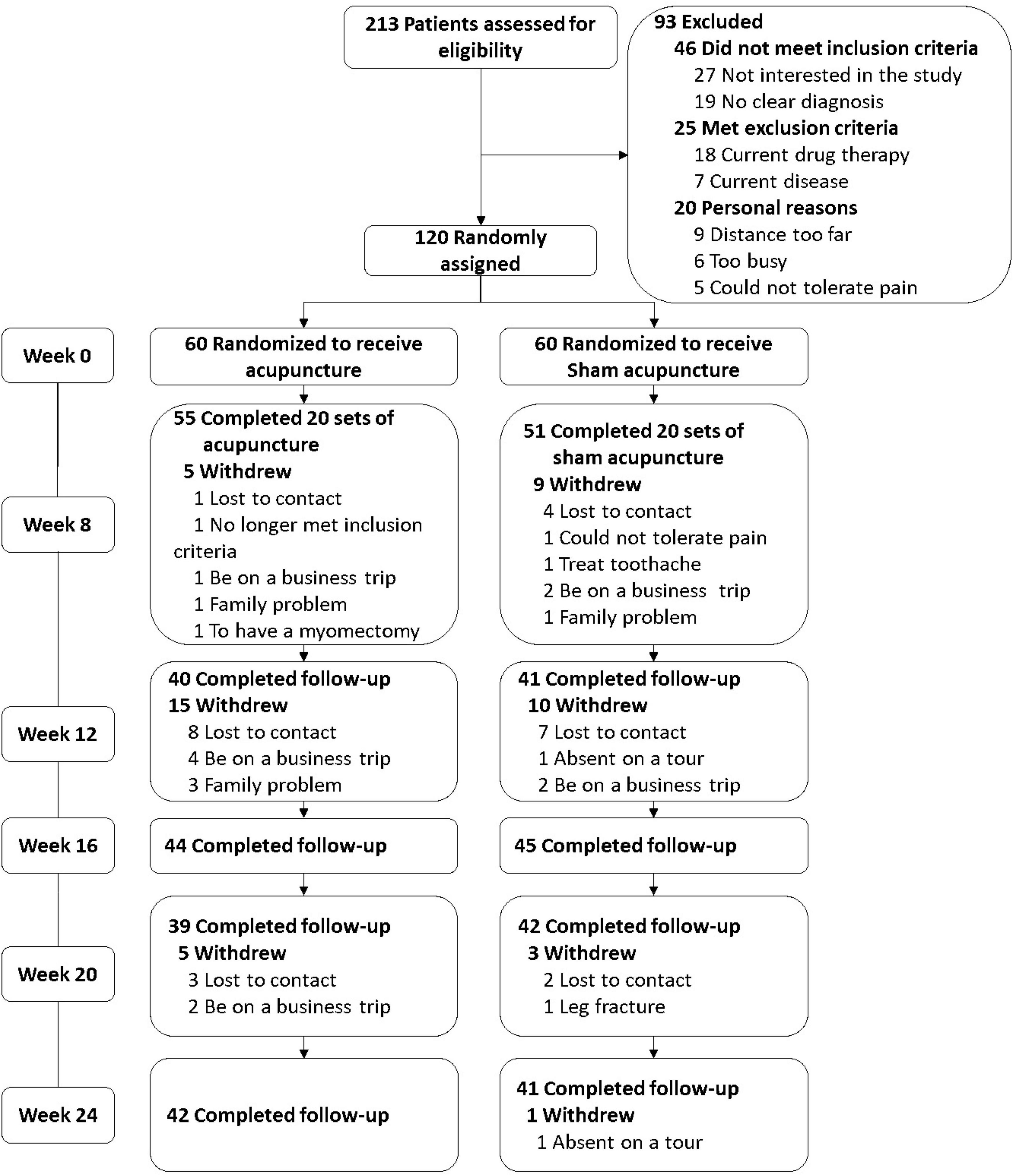
Figure 1. Study flow. The NAS scores at week 0 were was set as baseline of primary outcome. 70.0% (42/60) of the patients received acupuncture between weeks 0 and 8 and then were successfully followed up between weeks 8 and 24, 68.3% (41/60) in the sham group.
At week 8, the proportions of patients meeting the primary endpoint (≥ 30% reduction in ≥ 2 of the 3 NAS scores for dryness, pain, and fatigue) were 28.33% (17/60) in the acupuncture group and 31.66% (19/60) in the SA group, without a statistically significant difference (P = 0.705 after LOCF imputation) (Table 3).
In addition, we also compared the proportions of patients who experienced a ≥ 30% reduction in 2 of the 3 NAS scores in the 2 groups in other weeks during follow-up (Table 3), including the actual values of the odds ratios. However, no significant difference between the groups was obtained at any week.
No difference in NAS scores for dryness, fatigue, or pain was observed between the 2 groups during any week. However, there was a general decreasing trend in NAS scores observed in both groups during the intervention and follow-up periods (Table 4 and Figure 2).
In a post hoc analysis, the minimally clinically important improvements (MCIIs) in NAS scores for dryness, pain, and fatigue were calculated as −1, −2, and −3 point(s) on 10-point scales, respectively. There was no significant difference between the 2 groups in the proportion of patients with MCII scores at week 8 in each of the 3 scales or in ≥ 2 of 3 of the scales, nor was there a significant difference in the proportion of patients with an improvement of 1, 2, or 3 point(s) in the NAS scores for pain, fatigue, or dryness or in ≥ 2 of 3 of the scores (Table 5).
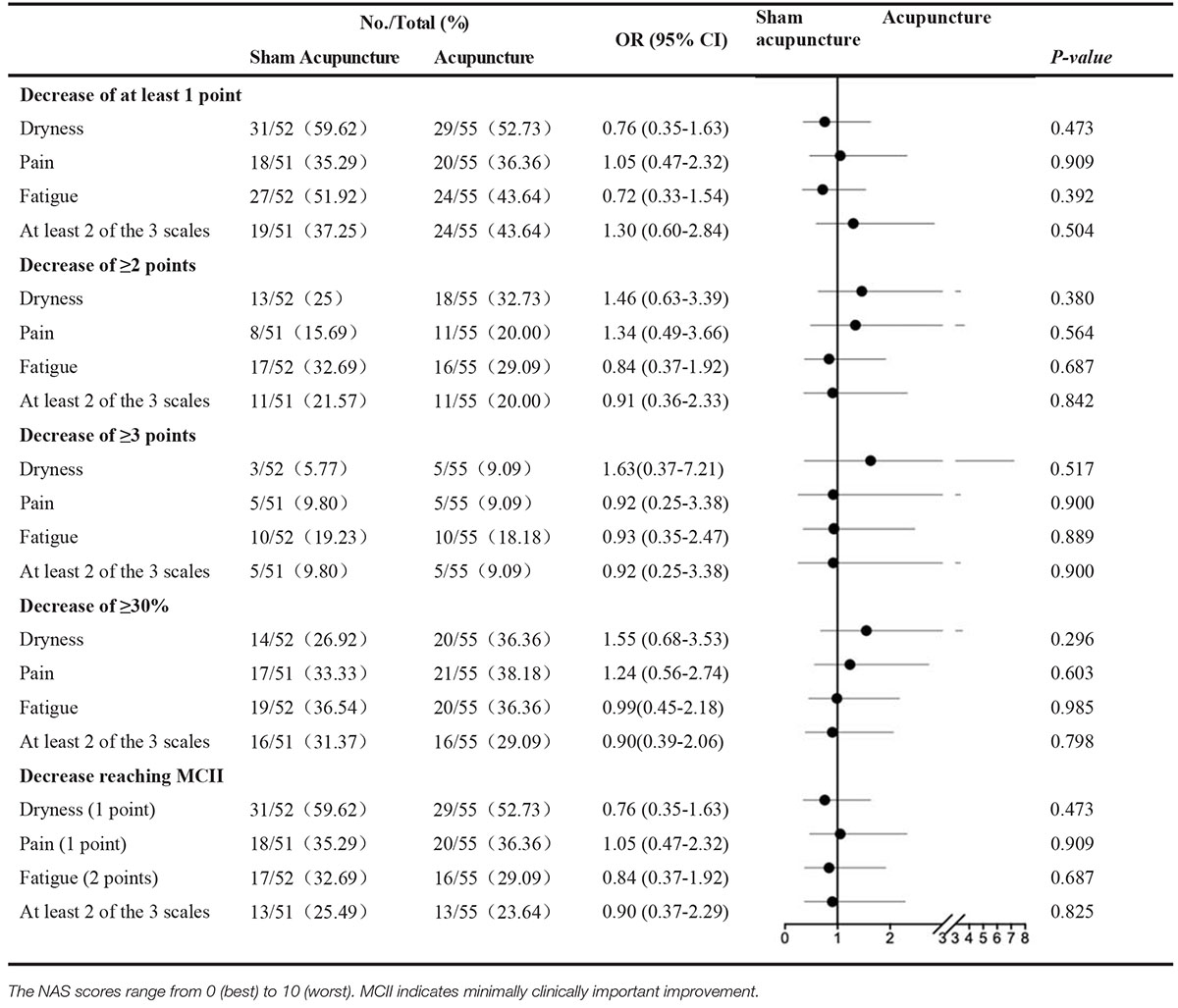
Table 5. Sensitivity of evolution in NAS scores in dry, pain and weak in patients with pSS, between baseline and week 8.
In week 16, the IgG concentration (M ± SD) of the SA group showed a significant difference (P = 0.0490) compared to that of the acupuncture group (17.65 ± 7.20 g/L vs. 16.97 ± 5.46 g/L) (Table 4). No other difference in ESSPRI, ESSDAI, SF-36, the HADS anxiety subscore, the HADS depression subscore, Schirmer test results, unstimulated saliva flow, ESR, the CRP level, or the IgA or IgM concentration between the 2 groups was obtained in any other week. Compared to week 0, there was a downward trend in unstimulated salivary flow in both groups, more pronounced in the acupuncture group, but no significant difference was found between the two groups (Figure 3). In exploring the differences between before and after the intervention period in the 2 groups, we observed significant differences in ESSPRI between weeks 0 and 8, weeks 0 and 12, weeks 0 and 16, and weeks 0 and 24 between the groups and noted significant differences in unstimulated saliva flow between weeks 0 and 8, weeks 0 and 16, and weeks 0 and 24 between the groups (Table 6).
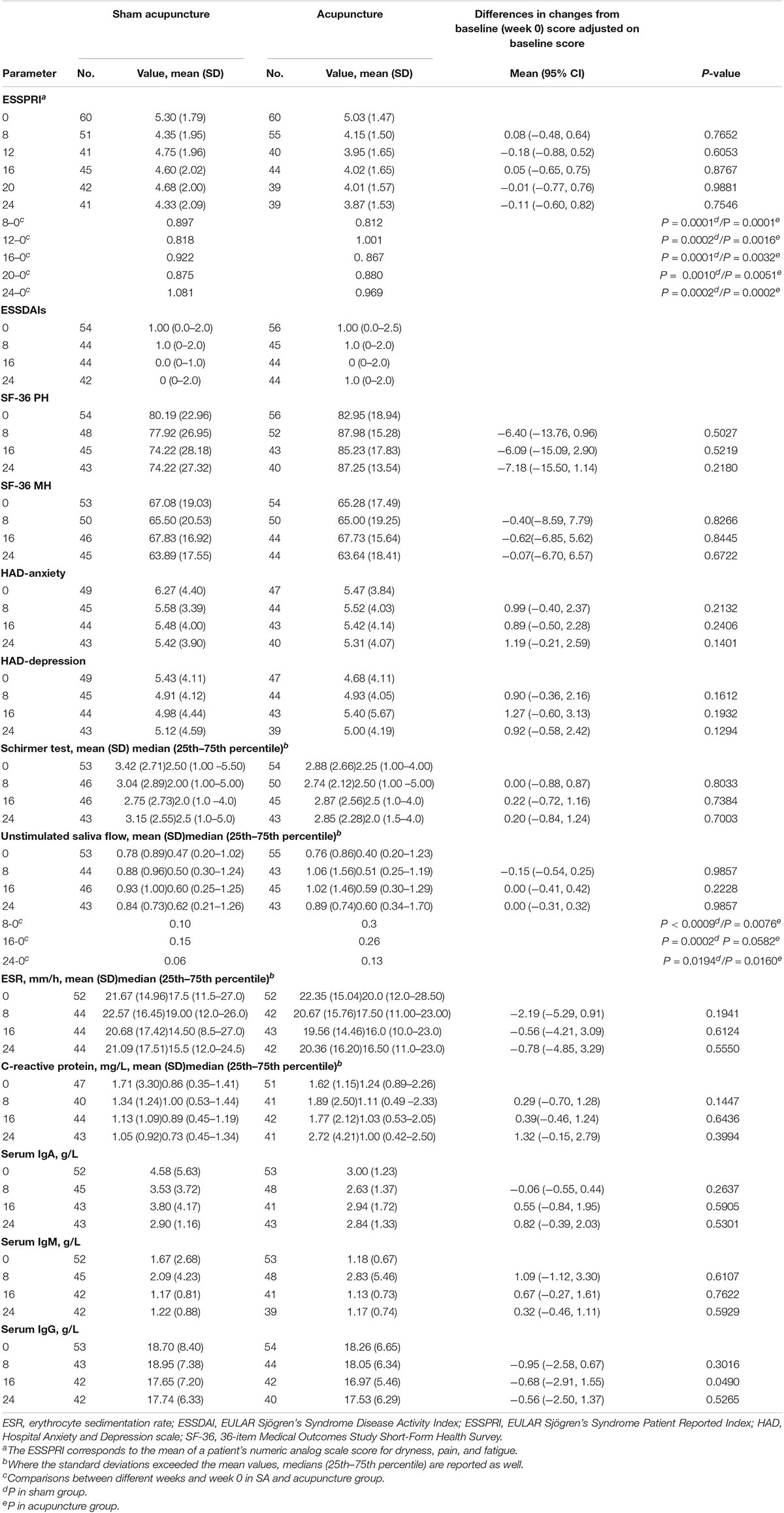
Table 6. ESSPRI, ESSDAI, evaluation of disease activity by practitioner, patient-related outcome, and biological variables, by group.
We quantified and calculated the ultrasonography improvement ratio of the 2 groups before and after the 8-week intervention in 4 different dimensions of ultrasonography (18, 19). Both groups acquired improvements in salivary gland ultrasound scores, with a 18.7% improvement in the SA group and a 35.2% improvement in the acupuncture group noted in terms of homogeneity, respectively, and these were significantly different results (P = 0.0334). No significant difference was obtained in the other 3 dimensions (Table 7).
To assess blinding, in week 8, we asked patients if they felt a “deep penetration,” “shallow penetration,” or “no penetration.” Choosing either former two options indicated successful blinding. None of the participants answered “no penetration,” which suggested that the blinding was successful. 78.1% of patients in acupuncture group reported that they had deep penetration, and 60.0% in sham acupuncture group (P = 0.122). Additionally, 78.0% of patients were willing to recommend acupuncture treatment to others, showing a good satisfaction.
During the first 8 weeks, there was 1 serious adverse event in the placebo group and 2 in the acupuncture group. In the last 16 weeks, there was 1 serious adverse event in the placebo group and none in the acupuncture group. More details of the adverse events are described in Table 8.
This study did not show that acupuncture improved the main symptoms of pSS compared to placebo treatment, although acupuncture and SA both reduced ESSPRI (M ± SD) and increased unstimulated saliva flow (Table 6). Nearly 33% of participants in both groups (31.66% in the SA group, 28.33% in the acupuncture group) had a ≥ 30% improvement in ≥ 2 of 3 NAS scales at week 8 and met the primary study endpoint. The IgG concentration at week 16 and the homogeneity in ultrasonography of the salivary glands at week 8 showed significant differences between the 2 groups.
The presence of other studies with similar negative outcomes in the literature reflects the persistence of extensive difficulties in alleviating the symptoms of patients with pSS. Hydroxychloroquine, infliximab, etanercept (5–7), and interleukin-6 receptor inhibition (20) did not improve symptoms compared to placebo treatment. The success of B-cell–activating factor receptor blockage for symptomatic improvement was uncertain as well (21).
However, the fact that the IgG concentration differed at week 16 and the homogeneity improved at week 8 in the acupuncture group, with a significant difference compared to the SA group, indicated the existence of an immunity response in pSS patients. The acupuncture regulates the immune system possibly by activating neuronal networks (22) and a variety of bioactive chemicals through peripheral, spinal, and supraspinal mechanisms (23). As a result, the infiltration of lymphocytes into saliva glands might be restrained, and the homogeneity in ultrasound were improved, which was also observed previously by us in a non-obese diabetic mouse model (unpublished data). Further, the symptom of dryness was relieved in both study groups, with a faster decrease in dryness observed in the acupuncture group, but without a statistically significant difference from the SA group. It may be attributed to the small sample size.
In this study, IgG was discovered being different between the 2 groups at week 16, 2 months after the intervention. Previous researches also shared relative conclusions that acupuncture is able to regulate immune systems (24, 25). However, that the difference was observed 2 months after the intervention is in opposition to the stereotype of acupuncture, which typically has strong instant effects (26, 27), and mainly in the area of pain relief. On the contrary, NAS scores for pain in this study did not show improvement, but those for dryness did. The dryness in pSS is led by the injury of salivary glands, which mainly due to immune imbalance. The alleviation of dryness and betterment of IgG observed in this study pointed out that more researches should be launched to unveil the underlying immune mechanism of acupuncture on pSS.
The results that ESSPRI and unstimulated saliva flow were improved significantly in both groups between before and after the intervention, implies that acupuncture benefits patients with symptoms of dryness, though no statistically significant difference was present between the groups. A few other studies have offered similar findings, revealing that acupuncture improved subjective ocular dryness (28) and promoted saliva secretion and symptomatic feelings (29). In terms of fatigue, no sign of fatigue relief was discovered in our study. However, several articles (30–32) mentioned the fatigue relief function of acupuncture or electro-acupuncture in other diseases, probably via the regulation of autonomic nerves (33).
The design of the placebo group in this study should be adjusted to avoid a possible efficacy of sham needles, especially in autoimmune diseases, as it was discovered that SA treatment provides some relief from symptoms (34, 35). In our study, the same acupoints in the two groups were stimulated, and the real needles could not penetrate much deeper than the sham ones because most of the acupoints selected were located on bony areas. In other clinical studies, the real needles penetrated much deeper and the sham ones were positioned away from the real acupoints (36, 37). In future studies, real acupoints should be avoided in the sham group, and a better and more specific combination of acupoints is necessary to minimize the efficacy of sham needles.
The real efficacy of acupuncture might not be well demonstrated in this study either, as all participants had consistent acupoints stimulated, which never happens in clinical acupuncture treatment given that acupoints are typically selected according to the individualization principle of traditional Chinese medicine (38). Meanwhile, nearly 33% of our participants met the primary outcome in both groups, indicating that, whether or not the needle penetrates the skin, stimulating acupoints can lead to clinical improvements, but more research is necessary to clarify the nuances of this effect.
The use of acupuncture did not satisfactorily improve symptoms in patients with pSS compared to those who received placebo treatment. However, interesting discoveries and possible underlying reasons were demonstrated and discussed, which may benefit studies in the future.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
This plan was reviewed and approved by the Ethics Committee of GAMH, China Academy of Chinese Medical Sciences (Ethics number: 2016-005-KY-01), and the study strictly adhered to the spirit of the Declaration of Helsinki of the World Medical Association and the appropriate international ethical guidelines for biomedical research involving humans. All volunteers who entered this clinical trial provided written informed consent.
XZ: study design, investigation, data curation, writing—original draft preparation, and project administration. HX: investigation, data curation, partly statistical analysis, writing—review, and editing. JC: study design, manuscript writing, data collection, and submission. HW and YZ: data collection and statistical analysis. KL and WJ: data collection. FT: statistical analysis. XT, HZ, and LG: study conduct and data collection. ZL: conceptualization, methodology, evidence-based acupuncturist, writing—review, and editing, and final improvement of the manuscript. QJ: conceptualization, supervision, and project administration critical revision. All authors read and approved the final manuscript.
This work was supported by Guang’anmen Hospital, China Academy of Chinese Medical Sciences—National Chinese Medicine Clinical Research Model Basement (No. 2015s320), the National Natural Science Youth Foundation of China (No. 81804069), the Science and Technology Innovation Project of China Academy of Chinese Medical Sciences (CI2021A01510), and the Fundamental Research Funds for the Central Public Welfare Research Institutes (ZZ15-YQ-023).
FT was employed by Beijing CreateMed Medicine Technology Co., Ltd., Beijing, China.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We are grateful to Xinhang Li for data collection, Man Han for ultrasound information, and Xun Gong for analysis communication.
1. Ramos-Casals M, Solans R, Rosas J, Camps MT, Gil A, Del Pino-Montes J, et al. Primary Sjögren syndrome in Spain: clinical and immunologic expression in 1010 patients. Medicine (Baltimore). (2008) 87:210–9. doi: 10.1097/MD.0b013e318181e6af
2. Ng WF, Bowman SJ. Primary Sjogren’s syndrome: too dry and too tired. Rheumatology (Oxford). (2010) 49:844–53. doi: 10.1093/rheumatology/keq009
3. Bowman SJ, Hamburger J, Richards A, Barry RJ, Rauz S. Patient-reported outcomes in primary Sjogren’s syndrome: comparison of the long and short versions of the profile of fatigue and discomfort–Sicca symptoms inventory. Rheumatology (Oxford). (2009) 48:140–3. doi: 10.1093/rheumatology/ken426
4. da Mata ADSP, Amaral JPAR, Thomson WM, Barcelos F, Vaz Patto J, Pereira RMN, et al. Patient-related outcomes in Sjögren syndrome treated with stimulants of salivary secretion: randomized clinical trial. Oral Dis. (2020) 26:313–24. doi: 10.1111/odi.13251
5. Gottenberg JE, Ravaud P, Puéchal X, Le Guern V, Sibilia J, Goeb V, et al. Effects of hydroxychloroquine on symptomatic improvement in primary Sjögren syndrome: the JOQUER randomized clinical trial. JAMA. (2014) 312:249–58. doi: 10.1001/jama.2014.7682
6. Bodewes ILA, Gottenberg JE, van Helden-Meeuwsen CG, Mariette X, Versnel MA. Hydroxychloroquine treatment downregulates systemic interferon activation in primary Sjögren’s syndrome in the JOQUER randomized trial. Rheumatology (Oxford). (2020) 59:107–11. doi: 10.1093/rheumatology/kez242
7. Yoon CH, Lee HJ, Lee EY, Lee EB, Lee WW, Kim MK, et al. Effect of hydroxychloroquine treatment on dry eyes in subjects with primary Sjögren’s syndrome: a double-blind randomized control study. J Korean Med Sci. (2016) 31:1127–35. doi: 10.3346/jkms.2016.31.7.1127
8. Sankar V, Brennan MT, Kok MR, Leakan RA, Smith JA, Manny J, et al. Etanercept in Sjögren’s syndrome: a twelve-week randomized, double-blind, placebo-controlled pilot clinical trial. Arthritis Rheum. (2004) 50:2240–5. doi: 10.1002/art.20299
9. Macfarlane GJ, Kronisch C, Dean LE, Atzeni F, Häuser W, Fluß E, et al. EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis. (2017) 76:318–28. doi: 10.1136/annrheumdis-2016-209724
10. Vickers AJ, Vertosick EA, Lewith G, MacPherson H, Foster NE, Sherman KJ, et al. Acupuncture Trialists’ collaboration. acupuncture for chronic pain: update of an individual patient data meta-analysis. J Pain. (2018) 19:455–74. doi: 10.1016/j.jpain.2017.11.005
11. Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, et al. Classification criteria for Sjögren’s syndrome: a revised version of the European criteria proposed by the American-European consensus group. Ann Rheum Dis. (2002) 61:554–8. doi: 10.1136/ard.61.6.554
12. Jiang Q, Zhang H, Pang R, Chen J, Liu Z, Zhou X. Acupuncture for Primary Sjögren syndrome (pSS) on symptomatic improvements: study protocol for a randomized controlled trial. BMC Complement Altern Med. (2017) 17:61. doi: 10.1186/s12906-017-1559-9
13. Liu B, Xu H, Ma R, Mo Q, Yan S, Liu Z. Effect of blinding with a new pragmatic placebo needle: a randomized controlled crossover study. Medicine (Baltimore). (2014) 93:e200. doi: 10.1097/MD.0000000000000200
14. Johnson MI, Benham AE. Acupuncture needle sensation: the emerging evidence. Acupunct Med. (2010) 28:111–4. doi: 10.1136/aim.2010.002535
15. Mariette X, Ravaud P, Steinfeld S, Baron G, Goetz J, Hachulla E, et al. Inefficacy of infliximab in primary Sjögren’s syndrome: results of the randomized, controlled trial of remicade in primary Sjögren’s syndrome (TRIPSS). Arthritis Rheum. (2004) 50:1270–6. doi: 10.1002/art.20146
16. Seror R, Theander E, Brun JG, Ramos-Casals M, Valim V, Dörner T, et al. Validation of EULAR primary Sjögren’s syndrome disease activity (ESSDAI) and patient indexes (ESSPRI). Ann Rheum Dis. (2015) 74:859–66. doi: 10.1136/annrheumdis-2013-204615
17. Ramos-Casals M, Tzioufas AG, Stone JH, Sisó A, Bosch X. Treatment of primary Sjögren syndrome: a systematic review. JAMA. (2010) 304:452–60. doi: 10.1001/jama.2010.1014
18. Hocevar A, Ambrozic A, Rozman B, Kveder T, Tomsic M. Ultrasonographic changes of major salivary glands in primary Sjogren’s syndrome. Diagnostic value of a novel scoring system. Rheumatology (Oxford). (2005) 44:768–72. doi: 10.1093/rheumatology/keh588
19. Hammenfors DS, Brun JG, Jonsson R, Jonsson MV. Diagnostic utility of major salivary gland ultrasonography in primary Sjögren’s syndrome. Clin Exp Rheumatol. (2015) 33:56–62.
20. Felten R, Devauchelle-Pensec V, Seror R, Duffau P, Saadoun D, Hachulla E, et al. Interleukin 6 receptor inhibition in primary Sjögren syndrome: a multicentre double-blind randomised placebo-controlled trial. Ann Rheum Dis. (2020) 18:annrheumdis-2020-218467. doi: 10.1136/annrheumdis-2020-218467 [Epub ahead of print].
21. Dörner T, Posch MG, Li Y, Petricoul O, Cabanski M, Milojevic JM, et al. Treatment of primary Sjögren’s syndrome with ianalumab (VAY736) targeting B cells by BAFF receptor blockade coupled with enhanced, antibody-dependent cellular cytotoxicity. Ann Rheum Dis. (2019) 78:641–7. doi: 10.1136/annrheumdis-2018-214720
22. Ulloa L, Quiroz-Gonzalez S, Torres-Rosas R. Nerve stimulation: immunomodulation and control of inflammation. Trends Mol Med. (2017) 23:1103–20. doi: 10.1016/j.molmed.2017.10.006
23. Zhang R, Lao L, Ren K, Berman BM. Mechanisms of acupuncture-electroacupuncture on persistent pain. Anesthesiology. (2014) 120:482–503. doi: 10.1097/ALN.0000000000000101
24. Xu Y, Hong S, Zhao X, Wang S, Xu Z, Ding S, et al. Acupuncture alleviates rheumatoid arthritis by immune-network modulation. Am J Chin Med. (2018) 46:997–1019. doi: 10.1142/S0192415X18500520
25. Yamaguchi N, Takahashi T, Sakuma M, Sugita T, Uchikawa K, Sakaihara S, et al. Acupuncture regulates leukocyte subpopulations in human peripheral blood. Evid Based Complement Alternat Med. (2007) 4:447–53. doi: 10.1093/ecam/nel107
26. Yang SH, Xie PC, Qin XL. [An instant pain-relief effect of balance acupuncture for relieving sore throat in acute pharyngitis patients]. Zhen Ci Yan Jiu. (2012) 37:324–7.
27. Wei XY, Chen H, Guo C, Tan WL, Zhan SH. The instant and sustained effect of electroacupuncture in postgraduate students with depression: an fMRI Study. Neuropsychiatr Dis Treat. (2021) 17:873–83. doi: 10.2147/NDT.S307083
28. Dhaliwal DK, Zhou S, Samudre SS, Lo NJ, Rhee MK. Acupuncture and dry eye: current perspectives. A double-blinded randomized controlled trial and review of the literature. Clin Ophthalmol. (2019) 13:731–40. doi: 10.2147/OPTH.S175321
29. Simcock R, Fallowfield L, Jenkins V. Group acupuncture to relieve radiation induced xerostomia: a feasibility study. Acupunct Med. (2009) 27:109–13. doi: 10.1136/aim.2009.000935
30. Farrell D, Artom M, Czuber-Dochan W, Jelsness-Jørgensen LP, Norton C, Savage E. Interventions for fatigue in inflammatory bowel disease. Cochrane Database Syst Rev. (2020) 4:CD012005.
31. Kluger BM, Rakowski D, Christian M, Cedar D, Wong B, Crawford J, et al. Randomized, controlled trial of acupuncture for fatigue in Parkinson’s disease. Mov Disord. (2016) 31:1027–32. doi: 10.1002/mds.26597
32. Cheng CS, Chen LY, Ning ZY, Zhang CY, Chen H, Chen Z, et al. Acupuncture for cancer-related fatigue in lung cancer patients: a randomized, double blind, placebo-controlled pilot trial. Support Care Cancer. (2017) 25:3807–14. doi: 10.1007/s00520-017-3812-7
33. Shu Q, Wang H, Litscher D, Wu S, Chen L, Gaischek I, et al. Acupuncture and moxibustion have different effects on fatigue by regulating the autonomic nervous system: a pilot controlled clinical trial. Sci Rep. (2016) 6:37846. doi: 10.1038/srep37846
34. Grillo CM, Zotelli VLR, Lúcia Bressiani Gil M, de Sousa MDLR. Would a placebo acupuncture needle be able to induce Deqi? J Acupunct Meridian Stud. (2018) 11:273–9. doi: 10.1016/j.jams.2018.06.007
35. Chae Y, Um SI, Yi SH, Lee H, Chang DS, Yin CS, et al. Comparison of biomechanical properties between acupuncture and non-penetrating sham needle. Complement Ther Med. (2011) 19(Suppl. 1):S8–12. doi: 10.1016/j.ctim.2010.09.002
36. Liu Z, Yan S, Wu J, He L, Li N, Dong G, et al. Acupuncture for chronic severe functional constipation: a randomized trial. Ann Intern Med. (2016) 165:761–9. doi: 10.7326/M15-3118
37. Liu Z, Liu Y, Xu H, He L, Chen Y, Fu L, et al. Effect of electroacupuncture on urinary leakage among women with stress urinary incontinence: a randomized clinical trial. JAMA. (2017) 317:2493–501. doi: 10.1001/jama.2017.7220
38. Liu W, Qdaisat A, Lopez G, Narayanan S, Underwood S, Spano M, et al. Association between acupoint selection, target symptoms, and traditional chinese medicine diagnosis in real-time clinical practice in a comprehensive cancer center. Integr Cancer Ther. (2020) 19:1534735420928490. doi: 10.1177/1534735420928490
Keywords: Sjögren’s syndrome, acupuncture, dryness, fatigue, pain
Citation: Zhou X, Xu H, Chen J, Wu H, Zhang Y, Tian F, Tang X, Zhang H, Ge L, Li K, Jiang W, Liu Z and Jiang Q (2022) Efficacy and Safety of Acupuncture on Symptomatic Improvement in Primary Sjögren’s Syndrome: A Randomized Controlled Trial. Front. Med. 9:878218. doi: 10.3389/fmed.2022.878218
Received: 17 February 2022; Accepted: 17 March 2022;
Published: 06 May 2022.
Edited by:
Jing He, Peking University People’s Hospital, ChinaReviewed by:
Jinxia Zhao, Peking University Third Hospital, ChinaCopyright © 2022 Zhou, Xu, Chen, Wu, Zhang, Tian, Tang, Zhang, Ge, Li, Jiang, Liu and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Quan Jiang, ZG9jdG9yanFAMTI2LmNvbQ==; Zhishun Liu, bGl1emhpc2h1bkBhbGl5dW4uY29t
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.