
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Med. , 03 June 2022
Sec. Gastroenterology
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.865035
This article is part of the Research Topic Recent Updates in Advanced Gastrointestinal Endoscopy View all 25 articles
Background and Aims: Severe discomfort during an upper gastrointestinal endoscopy (UGE) is often a stressful experience for patients undergoing the procedure. An increasing number of studies have shown that acupuncture may reduce discomfort during UGE. A systematic review in 2004 investigated the effect of acupuncture for gastrointestinal endoscopy, but these data have not been recently reviewed. Therefore, this study was conducted to evaluate the current evidence and provide up-to-date knowledge for clinical decision-making.
Methods: Nine databases were searched from inception to June 2021. Eligible randomized controlled trials (RCTs) were included. The outcome data were synthesized where necessary, and risks of bias of included studies were assessed using RevMan V.5.3.
Results: Twenty-three eligible RCTs with 3,349 patients were identified. It was found that acupuncture plus topical pharyngeal anesthesia with lidocaine hydrochloride (TPALH) resulted in greater improvements regarding visual analog scale (VAS) scores and the incidence of nausea and vomiting (INV) when compared with TPALH alone. These results were consistent among studies of manual acupuncture, electroacupuncture, auricular-plaster, superficial needle (SFN) and acupressure. In the meta-analysis, SFN plus TPALH showed significant improvement of VAS scores compared to sham SFN plus TPALH (MD −1.11, 95% CI −1.52 to −0.70, P < 0.00001). Most of included studies did not report any side effects in their findings, and were of medium-to-high risk of bias.
Conclusion: Acupuncture, as adjunctive therapy to TPA, may result in less patient discomfort than TPA alone. Findings from this review should be interpreted with caution due to the high heterogeneity identified. There is low-quality evidence supporting the use of acupuncture over sham. More rigorously designed RCTs are needed to inform clinical decision-making.
Systematic Review Registration: PROSPERO [CRD42014008966].
Severe discomfort due to strong gag reflexes and pain during upper gastrointestinal endoscopy (UGE) often results in a stressful experience for patients who undergo the procedure and occasionally hinders the success of the procedure (1, 2). As a result, sedated UGE procedures with less discomfort and pain have been the predominant method used in endoscopic clinics in Europe and North America (3, 4). However, there are concerns regarding the cost and adverse events (e.g., cardiopulmonary events, allergic reactions) associated with the use of sedatives for UGE, especially in the elderly population with pre-existing cardiopulmonary disease (5, 6). Therefore, unsedated UGE is still being used by many physicians and patients in China and other developing countries (7, 8). Topical pharyngeal anesthesia (TPA), which has been reported to be effective in suppressing the threshold of the gag reflex, is often applied before an unsedated UGE to ease discomfort and pain (9–11). However, involuntary gagging cannot be suppressed among certain patients even after the use of TPA due to sensitive gag reflexes (9).
Acupuncture is a therapeutic intervention that involves the insertion of fine needles into the skin or deeper tissues at specific locations on the surface of the body with the aim of curing disease or promoting health, according to the theory of Traditional Chinese Medicine (12). Acupuncture has been frequently used to treat various diseases including nausea and vomiting associated with chemotherapy, pregnancy, and recovery from surgical procedures (13, 14), and some published studies have also demonstrated that acupuncture may be able to increase tolerance and reduce discomfort during UGE (15, 16). A systematic review in 2004 on the effect of acupuncture during gastrointestinal (GI) endoscopies included only six studies with inconclusive findings. However, it did not distinguish UGEs from colonoscopies, nor sedated from unsedated procedures, during which the patient status would be very different (17). On the other hand, the number of studies focusing on acupuncture to relieve patient discomfort during an unsedated UGE has increased, and many have reported that acupuncture was often used in conjunction with TPA during an unsedated UGE. However, there have been no systematic reviews concerning the effect of acupuncture on discomfort during UGE since 2004. Therefore, the current systematic review and meta-analysis was conducted with the aim of evaluating current evidence on acupuncture for the management of discomfort during an unsedated UGE, and thus providing up-to-date recommendations for clinical practice and decision-making.
This systematic review and meta-analysis were conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (18). The protocol was registered at PROSPERO with registration number CRD42014008966 (19).
The following databases were searched from inception to June 2021: MEDLINE, EMBASE, the Cochrane Central Register of Controlled Trials, Scopus, Web of Science, the Chinese Biomedical Literature Database, the China National Knowledge Infrastructure, Wanfang Database, VIP Database, the WHO International Clinical Trials Registry Platform portal, and ClinicalTrials.gov. The key search terms included: “endoscopy,” “upper gastrointestinal endoscopy,” “discomfort,” and “acupuncture,” etc. Tailored search strategies were developed for each database. Published review papers were searched to identify additional references.
Studies were included if they focused on (1) Population: patients who received an unsedated UGE (e.g., screening, surveillance, diagnosis; without the limitation of the brands or models of gastroscopes), regardless of age, sex, or race; (2) Intervention: were evaluating either invasive or non-invasive acupuncture therapies with or without concomitant treatment, with the aim of relieving discomfort during UGE (acupuncture hereby was defined as any treatment methods that achieve their effect by stimulating acupoints on body, including electroacupuncture, manual acupuncture, acupressure, etc.); (3) Comparison: were comparing acupuncture with any conservative interventions, not limited to the following: no treatment, placebo, sham acupuncture (SA), or other active conservative interventions (e.g., lubricant use, TPA, and sedation); and (4)Outcomes and Studies: were RCTs reporting at least one of the following outcomes, including discomfort severity using validated scales [e.g., visual analog scale (VAS), numerical rating scale (NRS)], incidence of nausea and vomiting (INV) during the UGE procedure, the proportion of patients satisfied with the process or patients who would opt for the same procedure again, and the incidence and types of adverse events related to acupuncture treatment regardless of language.
Studies were excluded if they (1) were investigating patients having chronic pharyngolaryngitis, severe digestive system diseases, persistent hiccups, severe nausea and retching, proven tumors in the upper digestive tract, severe mental disorders, or uncontrolled cardiopulmonary disease; (2) were only comparing different types of acupunctures without a comparison group of no treatment, placebo or sham acupuncture, medicine, or other conservative therapies; and (3) were not RCTs or were quasi-RCTs, or without a clear description of interventions, or did not provide outcome data.
Two reviewers (Ning Gao and Huan Chen) independently reviewed all retrieved papers by title and abstract to identify relevant papers, then the full texts of relevant papers were retrieved and reviewed for eligibility according to inclusion and exclusion criteria. Data were then extracted from the included studies, including author and year of the study, patient characteristics, study design, sample size, treatment type and regimen of experiment, control groups, outcomes measures, etc. Disagreements were resolved via discussion or arbitration by a third reviewer if necessary.
According to the “risk-of-bias” tool from the Cochrane Handbook for Systematic Reviews of Interventions, two reviewers independently evaluated the risk of bias for the included studies considering the following seven domains: random sequence generation, allocation concealment, blinding of patients and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other sources of bias (20). Each domain was rated as “low risk,” “high risk,” or “unclear risk.”
All studies were categorized based on the types of interventions. For continuous variables (e.g., VAS), the mean difference (MD) with standard deviation was used to present treatment effect. For dichotomous variables (e.g., INV), treatment effects were presented as a risk ratio (RR) with 95% confidence intervals (CIs).
Outcome data were synthesized to estimate the pooled effect size of acupuncture where applicable. The heterogeneity across studies would be assessed using the I2 and the chi-square tests and was considered significant at I2 > 50% or P < 0.1. A random-effects model was used if heterogeneity was significant, otherwise a fixed-effects model was used. Sensitivity analysis was conducted by removing a single study to explore if the influence of each study would change the direction of the pooled effect size in the meta-analysis.
A total of 2,462 studies were identified through an initial search. After removing duplicates, 1,939 studies were reviewed by title and abstract, and 1,756 studies were excluded for not meeting the inclusion criteria. Next, the full-text of 175 studies were obtained for further assessment, and 23 studies were considered eligible for the review according to the inclusion and exclusion criteria, and four studies were included in the meta-analysis. The details of the study selection process were shown in a PRISMA flow diagram (Figure 1).
The 23 RCTs included were conducted in Germany (one study) (21), Turkey (one study) (15), France (one study) (16), and China (20 studies), (22–41). A total of 3,349 patients (1,717 male and 1,393 female) who underwent UGE were included, with ages ranging from 16 to 86 years. Two studies did not report the number of male and female patients included (16, 34).
Among the 23 RCTs, seven studies used an electronic gastroscope and one study used a fibergastroscope, while 15 studies did not report the type of gastroscope used. Studies were categorized by types of acupuncture assessed, including electroacupuncture (EA, five studies), manual acupuncture (MA, 10 studies), auricular plaster therapy (AP, two studies), superficial needle (SFN, two studies), acupressure (one study), transcutaneous electric nerve stimulation (TENS, one study), and a combination of EA and AP (two studies). The most frequently used acupoints were PC-6 (Neiguan) and LI-4 (Hegu) on the hands, and ST-36 (Zusanli) on legs based on the symptoms presented during UGE.
Twenty-one studies initiated the acupuncture treatment prior to the UGE procedure and continued treatment throughout the procedure, while two studies only applied acupuncture before the procedure. The average duration of acupuncture treatment was in accordance with the duration of the UGE procedure and varied across patients and performers.
In terms of outcome reporting, 14 studies reported INV observed by the researcher, eight studies reported the VAS scores evaluated by patients to assess discomfort, and eight studies reported the proportion of patients satisfied with the entire process or those willing to undergo the procedure again. The VAS scores were evaluated by participants right when UGE had finished, and INV were observed by researcher according the signs of participants during the whole procedure. Four studies reported the incidence and types of adverse events related to acupuncture treatment. Some studies (15, 16, 21) also reported other outcomes, such as number of intubation attempts and eructation, the rate of successfully performed procedures, anxiety scores, etc. The details of the included studies were summarized in Tables 1, 2.
Most of the 23 studies had medium-to-high risk of bias, while one study had low risk of bias (21). Fourteen studies reported sound methods of random number generation, and nine studies did not contain detailed methods of randomization, while two studies out of nine were performed by experienced team which we assessed low risk of bias in randomization process. Five studies provided details regarding allocation concealment, while the rest did not. Six studies reported methods used for blinding patients and outcome assessors. Seventeen studies did not perform blinding of patients as their comparisons were between acupuncture and non-acupuncture treatment, and did not mention blinding of outcome assessors. Due to the characteristics of the acupuncture technique, doctors performing acupuncture treatment cannot be blinded. Almost all studies were considered low risk of attrition bias as the duration of intervention was short and no follow-up was conducted in any study other than two studies (28, 34). Except for a single study (21), the protocols were not available
to confirm whether the pre-designed outcomes were reported in their entirety (15, 16, 22–41). Two studies did not clarify whether baselines were comparable between different arms, and as such were considered to have other sources of bias (Figures 2, 3).
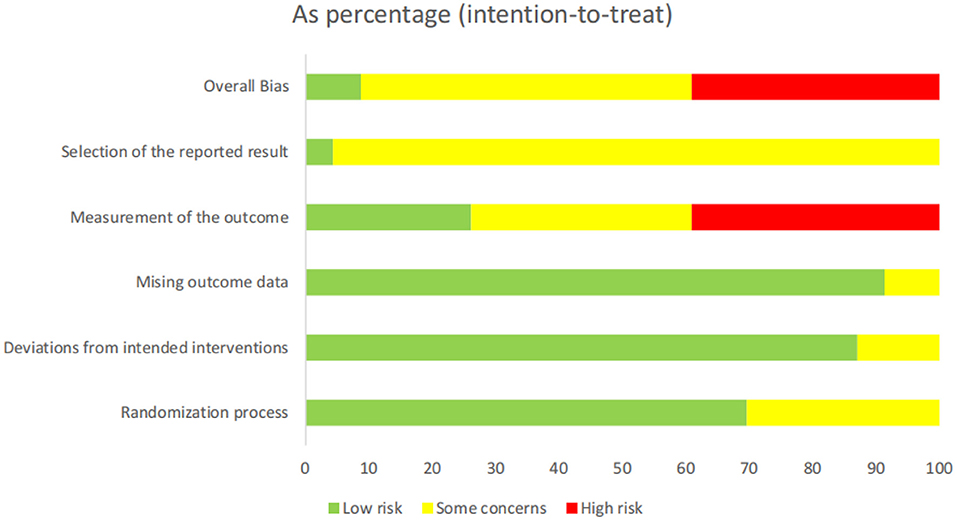
Figure 2. Risk of bias summary: review authors' judgement regarding each risk of bias item for each included study.
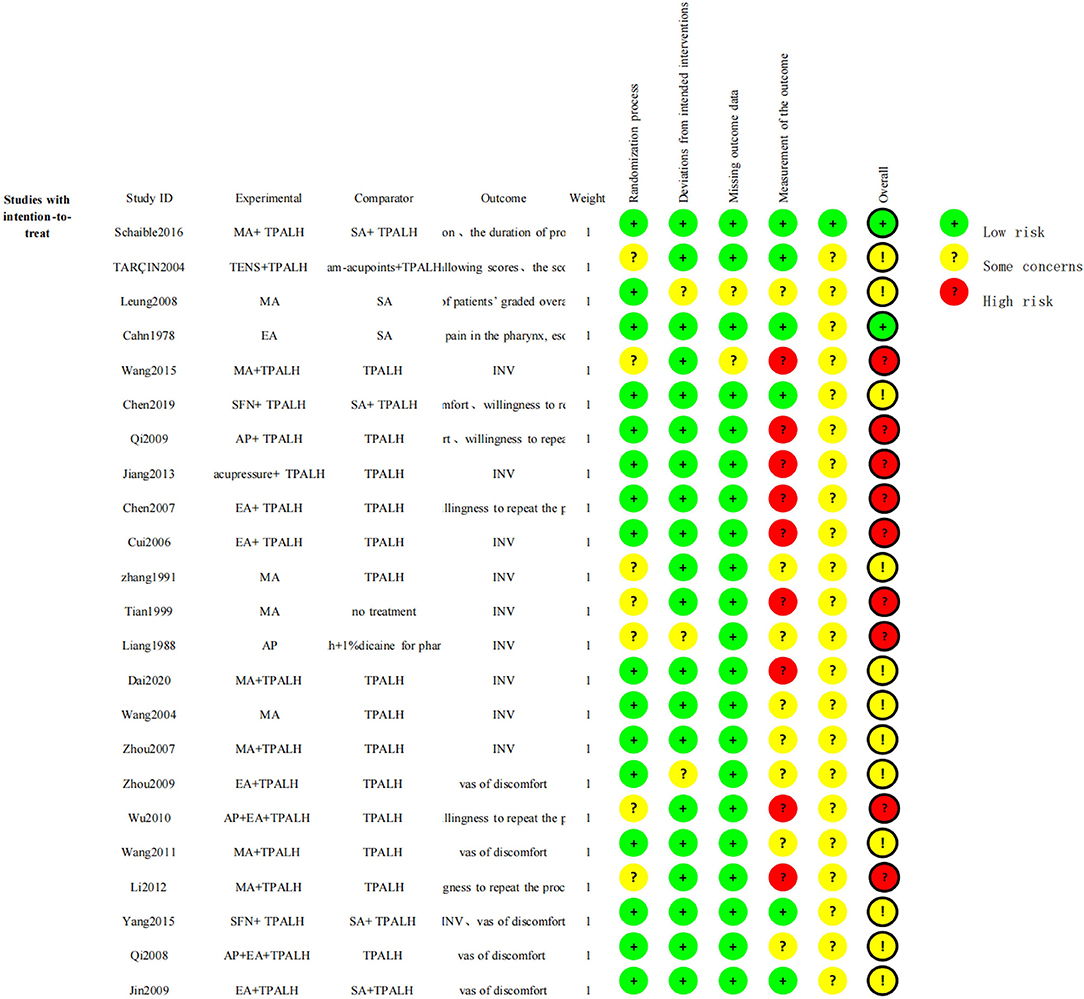
Figure 3. Methodological quality graph: review authors' judgements regarding each methodological quality item.
Ten studies (1,530 patients) investigated the effect of MA on improving discomfort among patients who underwent UGE. Among these studies, MA was compared with topical pharyngeal anesthesia with lidocaine hydrochloride (TPALH), sham-MA, usual care, and no treatment, with or without concomitant treatment. Two studies began MA and the UGE procedure at the same time (40, 41), while eight other studies began MA 3–20 min before the procedure and continued treatment until the end of the procedure (21, 24, 28, 34, 35, 37–41).
Five studies (406 patients) compared MA plus TPALH with TPALH alone. Dai et al. (39) and Zhou et al. (35) adopted the same acupuncture regimen (ST-36 and PC-6), while Wang (37) adopted ST-34, Wang et al. (28) adopted PC-6, and Li and Wang (24) adopted ST-36, PC-6 and LI-4.
A 2011 study by Wang reported that the VAS score of discomfort in the MA plus TPALH group was significantly lower compared to the TPALH alone group (3.81 ± 1.48 vs. 4.71 ± 1.43, MD −0.90, 95% CI −1.45 to −0.35, P = 0.001). In 2020, Dai reported significantly less INV in the MA plus TPALH group compared to the TPALH group (RR 0.57, 95% CI 0.35–0.94, P = 0.03), and Wang et al. (28) reported significantly less INV in the MA plus TPALH group that in the TPALH group (RR 0.62, 95% CI 0.43–0.88, P = 0.009). However, in a 2007 study by Zhou, the INV of each group (P < 0.05) was inconsistent with our calculation (RR 0.86, 95% CI 0.71–1.05, P = 0.14), in which we transformed the categorical data (overall effective rate) into dichotomous variables (event rate). Li and Wang (24) reported that the rate of patients willing to repeat the procedure in the MA plus TPALH group was 2.42 times higher compared to the TPALH-only group (RR 2.42, 95% CI 1.40–4.16; P = 0.001). By synthesizing the INV data from two studies (35, 39), it was determined that there was no significant difference between the MA plus TPALH and TPALH-only groups using a random-effect model (RR 0.74, 95% CI 0.47–1.15, P = 0.18, I2 = 66%, Figure 4).
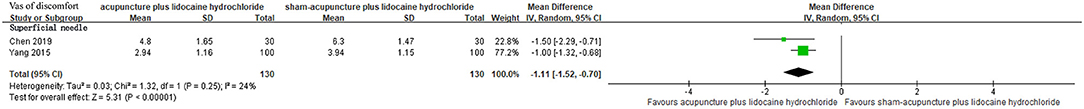
Figure 4. Forest plots of comparison between acupuncture plus lidocaine hydrochloride and sham acupuncture plus lidocaine hydrochloride.
Two studies (460 patients) investigated the effect of MA in comparison with TPALH but with varied timing of treatment and acupoints (40, 41). In 2004, Wang reported INV in the MA (PC-6) group was less than that in the TPALH group (RR 0.75, 95% CI 0.58–0.97; P = 0.03). In 1991, Zhang reported that INV was not statistically different between the two groups (PC-6, ST-36; RR 1.00, 95% CI 0.73–1.36; P = 1.00).
In 2008, a study by Leung (140 patients) compared MA to sham-MA, and reported that the VAS scores of discomfort (mainly pain) during the UGE were not significantly different between the two groups (1.6 ± 2.4 vs. 2.0 ± 2.7, MD −0.40, 95% CI −1.25 to 0.45, P = 0.35). This study also reported that there were no statistical differences regarding anxiety scores (MD −0.10, 95% CI −0.90 to 0.70, P = 0.81), the proportion of patients rating their overall tolerance as “excellent or good” (36 vs. 23%, P = 0.095), or the overall satisfaction scores (MD 0.30, 95% CI −0.46 to 1.06, P = 0.44) between the two groups.
Schaible et al. [(21); 354 patients] published a study comparing MA with sham-MA, where TPALH was used in both groups as standard care. This study reported that the rates of successfully performed UGE procedures (73.5 vs. 72.9%, P = 0.9045), as well as the proportions of patients willing to repeat the procedure (86.9 vs. 87.6%, P = 0.857), were not significantly different between the two groups. In addition, there were no significant differences in terms of heart rate, blood pressure, or oxygen saturation between the two groups at various time points (P-values were not provided). The percentage of patients with a reduced gag reflex was also not significantly different between the two groups (55.7 vs. 53.1%, P = 0.627).
The 1999 Tian study (90 patients) compared the effect of MA with no treatment during UGE. The treatment effect was ranked as follows: (1) marked effective: mild discomfort in the epigastric area, without nausea or vomiting; (2) effective: moderate discomfort in the epigastric area, and the frequency of nausea and vomiting decreased to 1–3 times per minute; (3) ineffective: no improvement on symptoms of discomfort in the epigastric area, or nausea and vomiting. Overall response rate (ORR), the proportion of “marked effective” and “effective” cases, were used as the primary outcomes in this study. A significant difference of ORR between the MA and no treatment groups was found (90 vs. 47.5%, P < 0.01) given the baseline characteristics were comparable between the two groups.
Five studies (674 patients) investigated the effect of EA on improvement of discomfort during UGE by comparing EA with TPALH or sham-EA, with or without concomitant treatment. The ST-36, LI-4, and PC-6 were used as principle acupoints in the regimens of these studies (16, 22, 23, 25, 26).
Three studies compared EA plus TPALH with TPALH alone. The ST-36 was used as the principle acupoint by all three studies (22, 23, 26).
A 2009 study by Zhou reported lower levels of VAS (discomfort) following treatment in the EA plus TPALH group compared to the TPALH-only group (3.19 ± 2.29 vs. 4.28 ± 2.6, MD −1.09, 95% CI −1.71 to −0.47, P = 0.0005). Chen et al. (26) reported INV was significantly lower in the EA plus TPALH group (RR 0.44, 95% CI 0.31–0.62; P < 0.00001). Cui reported in 2006 that the INV was significantly different between the two groups (P = 0.045), which was inconsistent with our calculation (RR 0.93, 95% CI 0.74–1.16; P = 0.50). Chen et al. (26) also reported the rate of patients willing to repeat the procedure in the EA plus TPALH group was approximately seven times higher than that in the control group (RR 6.92, 95% CI 2.23–21.47; P = 0.0008).
Two studies (192 patients) compared EA with sham-EA with or without TPALH as standard care (16, 25). In 2009, Jin reported the VAS score of discomfort in the EA plus TPALH group was significantly lower than that in the sham-EA plus TPALH group (3.82 ± 1.27 vs. 4.35 ± 1.40, P < 0.05), which was inconsistent with our calculation (MD −0.53, 95% CI −1.05 to −0.01; P = 0.05). Cahn et al. (16) reported that the incidences of eructation (P < 0.001), vomiting attempts (P < 0.001), and agitation (P < 0.001) assessed by the endoscopist were significantly lower in the experimental group, while the proportion of patients willing to repeat the procedure was not statistically different between the two groups (P > 0.05).
Two studies (280 patients) investigated the effect of AP during UGE and reported conflicting results (27, 36). Qi (27) reported that the VAS score of discomfort in the AP plus TPALH group was lower than that in the TPALH-only group (3.73 ± 1.32, 4.33 ± 1.33, MD −0.60, 95% CI −1.18 to −0.02; P = 0.04), and the proportion of patients willing to repeat the procedure was also higher in the AP plus TPALH group (RR 1.41, 95% CI 1.02–1.95; P = 0.04). On the contrary, Liang reported in 1988 that the INV in the AP group was higher than that in the atropine plus dicaine group (RR 1.29, 95% CI 0.73–2.29; P = 0.37).
Two studies (202 patients) compared the effect of AP plus EA and TPALH with TPALH alone (31, 32). The regimens and schedule of interventions were similar between the two studies. In 2008, Qi reported that the AP plus EA and TPALH group had significantly lower VAS scores of discomfort compared with the TPALH-only group (3.61 ± 1.43 vs. 4.51 ± 1.38, MD −0.90, 95% CI −1.45 to −0.35; P = 0.001), and the results of the 2010 Wu study on INV (RR 0.44, 95% CI 0.30–0.64; P < 0.0001) and the proportion of patients willing to repeat the procedure (RR 5.20, 95% CI 2.17–12.45; P < 0.0002) supported better outcomes in the AP plus EA and TPALH group compared with that of the TPALH-only group.
Two studies (260 patients) compared SFN plus TPALH with sham-SFN plus TPALH for discomfort during UGE (29, 33). Yang (33) reported that the experimental group was more effective in reducing INV (RR 0.48, 95% CI 0.35–0.67; P < 0.00001), while Chen (29) did not find a significant difference in INV between the two groups (RR 0.90, 95% CI 0.77–1.05, P = 0.17). For VAS scores of discomfort, both studies found that the SFN plus TPALH group showed greater improvement compared to control [Yang (33): MD −1.00, 95% CI −1.32 to −0.68, P < 0.00001; Chen (29): MD −1.50, 95% CI −2.29 to −0.71, P = 0.0002]. Chen (29) also reported the proportion of patients willing to repeat the procedure in the SFN group was higher than that in the control group (RR 2.33, 95% CI 1.04–5.25, P = 0.04).
The 2019 Chen study used VAS to primarily measure the feeling of pain, while the 2015 Yang study measured general discomfort during the UGE procedure. Considering that pain carries considerable weight in discomfort, the VAS score data of the two studies were combined. These new results revealed that patients receiving SFN plus TPALH reported a greater improvement on the VAS scores of discomfort compared to sham-SFN plus TPALH group using a random-effect model (MD −1.11, 95% CI −1.52 to −0.70, P < 0.00001; I2 = 24%, Figure 5).
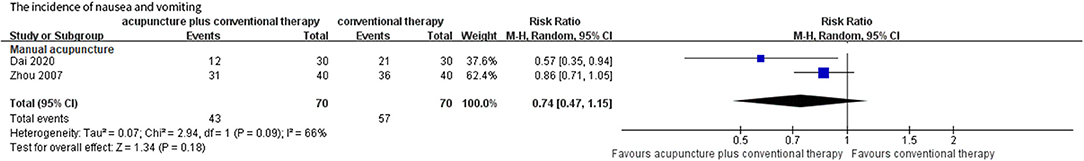
Figure 5. Forest plots of comparison between acupuncture plus lidocaine hydrochloride and lidocaine hydrochloride.
A single 2013 study by Jiang (156 patients) compared acupressure plus TPALH to TPALH alone (30). The study reported that patients in the experimental group had a lower INV compared to the control group (RR 0.80, 95% CI 0.68–0.95, P = 0.01).
One study by Tarçin et al. (327 patients) designed a four-arm study, comparing the effects of TENS plus TPALH, sham-TENS plus TPALH, sham-acupoints plus TPALH, and standard care with TPALH alone to assess discomfort during UGE (15). PC-6 was used as the acupoint of stimulation. As reported, there were no significant differences found between the groups on nausea-retching scores (P > 0.05), swallowing scores (P > 0.005), score of the endoscopists' opinion of the procedure (P > 0.005), and the proportion of patients who would accept re-endoscopy (P > 0.05).
Among the 23 studies, four studies (17.39%) reported that there were no adverse events associated with acupuncture. One study (4.35%) reported that a single patient in the EA group could not complete the UGE procedure due to discomfort. The remaining 18 studies (78.26%) did not report any adverse events.
Funnel plots and Egger's test were not feasible due to the limited number of studies included for each type of intervention in the review (42).
To the best of our knowledge, this is the first systematic review and meta-analysis to assess the effect of acupuncture on the improvement of discomfort during UGE procedures. Among the 23 included RCTs, the results (improvement of VAS or INV) were in favor of acupuncture plus TPA (primarily TPALH) compared with TPA alone, among studies of MA, EA, AP, SFN, and acupressure. However, the results appeared inconsistent when comparing acupuncture methods alone to anesthetics, sham acupuncture, usual care, or no treatment. Most of the included studies did not report any adverse events in their findings and were of medium-to-high risk of bias.
Some studies explored the anti-emetic effects of acupuncture that might be associated with an increase in the hypophyseal secretion of beta-endorphins and adrenocorticotropic hormone, together with subsequent suppression of the chemoreceptor trigger zone and vomiting center (43, 44). Studies have shown that the Neiguan (PC-6) acupoint, which is the most commonly used acupoint to treat GI symptoms, may reduce nausea through a variety of mechanisms, including neurotransmitters (e.g., the endogenous opioid system, serotonin transmission), a direct influence on the smooth muscle of the gut, somatovisceral reflex, sensory input inhibition, somatosympathetic reflex-induced gastric relaxation, vagal modulation, central cerebellar modulation, or psychological aspects (45, 46). Some studies have indicated that Zusanli (ST-36) and Neiguan (PC-6) have a synergistic effect on gastric myoelectrical activity (47, 48). However, the true mechanism by which acupuncture relieves discomfort during UGE remains inconclusive.
An early systematic review (2004) (17) on discomfort during GI endoscopy (including UGE and colonoscopy) with six RCTs found that the effect of acupuncture (EA and MA) on relieving discomfort was similar to active medication, but better than that of sham acupuncture, with or without TPA or a sedative (17). The results described in the current review suggest that regardless of the type of acupuncture, the VAS score of discomfort during UGE in groups with acupuncture plus TPA was significantly lower than of TPA-alone, which was not claimed in the previous review. These results could indicate that the use of acupuncture as an adjuvant therapy could enhance the effect of TPA and thus may reduce the amount of TPA required during UGE. When comparing EA or MA with sham acupuncture, the results in the current review were inconsistent across studies with or without TPA, which diverged from the conclusions of the previous study (17).
It was unfortunate that we did not find substantiative evidence regarding the minimum clinical important difference of the VAS scores of discomfort (one of the major measurements of discomfort) during GI endoscopy from previous studies and systematic reviews (17). The discomfort during UGE and colonoscopy procedures is often regarded as comparable due to one common mechanism - the pressure of air distension (49). One previous study reported that the VAS pain scores during a colonoscopy were significantly lower in patients receiving anesthetics plus acupuncture (1.4 ± 0.4) compared to patients receiving anesthetics plus sham acupuncture (3.0 ± 0.3), with a difference of −1.30 (−1.58, −1.02, P = 0.003) (50). Another study reported the VAS discomfort scores in EA and SA groups were significantly different at 24 mmHg (pressure of air distension) during a colonoscope (2.80 vs. 4.74, P = 0.013) (51). In the current review, the mean VAS scores of discomfort ranged from 2.94 to 4.80 after treatment in patients receiving TPA plus acupuncture, and from 3.94 to 6.3 in patients receiving TPA only, with MD ranging from −1.11 to −0.65 (P all <0.05). Although the data of the VAS scores presented above looks comparable across studies, it would be arbitrary to draw any conclusion with the limited data and substantial heterogeneity regarding type of acupuncture, regimens (including beginning and ending time of acupuncture treatment in relation to the endoscopy, the total duration of endoscopy, acupoints selected, intensity of simulation), skills of doctors, as well as level of risk of bias.
It is worth mentioning that the outcome measurements used by the studies included in this review varied considerably, which hindered the syntheses of effects across all studies. For instance, considering the level of discomfort, nearly half of the included studies did not use internationally recognized tools, such as VAS or NRS, to measure the level of discomfort. Instead, they developed a ranking system to categorize the effect of acupuncture without a consistent definition for each rank across multiple studies. In addition, numerous factors can influence the discomfort level during a UGE procedure, such as the size of endoscopy lens, physical sensitivity and characteristics of the patients (e.g., age, sex, tolerance, upper gastrointestinal diseases, and previous endoscopy experience), time of measurement, the UGE operator's experience (52), etc. However, limited information was reported on the above factors to allow for further understanding or analysis on the effect of acupuncture. Given the side effect of TPA or sedatives, a reduced dosage when combined with acupuncture should be another key reflection of the effect of acupuncture. However, not all studies reported on this outcome (28, 35). None of the studies reported any data on cost-effectiveness of the use of acupuncture during UGE.
The current review has many strengths. It included a greater number of studies than the previous review, focused specifically on unsedated UGE, and used a comprehensive search of both English and Chinese language biomedical databases. However, several limitations are also present. Firstly, the 23 RCTs were heterogeneous regarding the type and regimen of acupuncture and the control group, as well as outcome measurements, which limited our attempt to synthesize the effect from individual studies (Figure 6). Secondly, the tolerance of discomfort and acceptance of sedated UGE vary considerably among patients in different countries. More than 90% (21/23) of the included studies were conducted in Asian countries (i.e., China, Turkey), and only two were carried out in Europe (i.e., France, Germany), which may constrain the generalization of the results. Thirdly, with limited information, the review was not able to determine the specific characteristics of patients (e.g., sex, age) may benefit more from acupuncture, and which type of acupuncture and stimulation were superior to others. Fourthly, due to the lauguage capacity, we didnot search Korean or Japanese databases specially, which might add publication bias out of regional inequality.
In this review, it was shown that acupuncture, as an adjuvant therapy to TPA, may further decrease discomfort levels compared to TPA alone. When compared with sham acupuncture, usual care, or no treatment, the effect of acupuncture was not consistent. Findings from this review should be interpreted with caution given the heterogeneity and bias identified across the studies. Rigorously designed RCTs that measure standardized and clinically relevant outcomes are needed to inform clinical decision-making regarding the use of acupuncture for discomfort relief during unsedated UGE procedures.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
WW and ZL contributed to study conception and design. NG and HC searched the databases, reviewed studies, and assessed the quality of studies. YW and YG analyzed data and carried out the statistical analysis. This manuscript was drafted by NG and revised by WW and HC. All authors approved the final version of the manuscript.
This study was funded by the China Academy of Chinese Medical Sciences (Grant No. ZZ13-YQ-019). The funding agency had no role in the design or conduct of the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.865035/full#supplementary-material
UGE, upper gastrointestinal endoscopy; RCTs, randomized controlled trials; TPALH, topical pharyngeal anesthesia with lidocaine hydrochloride; VAS, visual analog scale; INV, incidence of nausea and vomiting; SFN, superficial needle; TPA, topical pharyngeal anesthesia; GI, gastrointestinal; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; NRS, numerical rating scale; MD, mean difference; RR, risk ratio; Cis, confidence intervals; SA, sham acupuncture; AP, auricular plaster; EA, electroacupuncture; MA, manual acupuncture; TENS, transcutaneous electric nerve stimulation; ORR, overall response rate.
1. Park JY, Kim BJ, Lee SW, Kang H, Kim JW, Jang IJ, et al. Influence of midazolam-related genetic polymorphism on conscious sedation during upper gastrointestinal endoscopy in a Korean population. Sci Rep. (2019) 9:3–10. doi: 10.1038/s41598-019-52517-7
2. Campo R, Brullet E, Montserrat A, Calvet X, Moix J, Rué M, et al. Identification of factors that influence tolerance of upper gastrointestinal endoscopy. Eur J Gastroenterol Hepatol. (1999) 11:201–4. doi: 10.1097/00042737-199902000-00023
3. Hazeldine S, Fritschi L, Forbes G. Predicting patient tolerance of endoscopy with conscious sedation. Scand J Gastroenterol. (2010) 45:1248–54. doi: 10.3109/00365521.2010.497939
4. Feld AD. Endoscopic sedation: medicolegal considerations. Gastrointest Endosc Clin N Am. (2008) 18:783–8. doi: 10.1016/j.giec.2008.06.009
5. Abraham NS, Fallone CA, Mayrand S, Huang J, Wieczorek P, Barkun AN. Sedation versus no sedation in the performance of diagnostic upper gastrointestinal endoscopy: a Canadian randomized controlled cost-outcome study. Am J Gastroenterol. (2004) 99:1692–9. doi: 10.1111/j.1572-0241.2004.40157.x
6. Kerker A, Hardt C, Schlief HE, Dumoulin FL. Combined sedation with midazolam/propofol for gastrointestinal endoscopy in elderly patients. BMC Gastroenterol. (2010) 10:1–5. doi: 10.1186/1471-230X-10-11
7. Wang HL, Ye F, Liao WF, Xia B, Zheng GR. Unsedated versus sedated gastrointestinal endoscopy: A questionnaire investigation in Wuhan, central China. J Huazhong Univ Sci Technol Med Sci. (2013) 33:857–61. doi: 10.1007/s11596-013-1211-y
8. Zheng HR, Zhang XQ Li LZ, Wang YL, Wei Y, Chen YM, et al. Multicentre prospective cohort study evaluating gastroscopy without sedation in China. Br J Anaesth. (2018) 121:508–11. doi: 10.1016/j.bja.2018.04.027
9. Evans LT, Saberi S, Kim HM, Elta GH, Schoenfeld P. Pharyngeal anesthesia during sedated EGDs: is “the spray” beneficial? A meta-analysis and systematic review. Gastrointest Endosc. (2006) 63:761–6. doi: 10.1016/j.gie.2005.11.059
10. Hwang SH, Park CS, Kim BG, Cho JH, Kang JM. Topical anesthetic preparations for rigid and flexible endoscopy: a meta-analysis. Eur Arch Otorhinolaryngol. (2015) 272:263–70. doi: 10.1007/s00405-014-3012-8
11. Heuss LT, Hanhart A, Dell-Kuster S, Zdrnja K, Ortmann M, Beglinger C, et al. Propofol sedation alone or in combination with pharyngeal lidocaine anesthesia for routine upper GI endoscopy: a randomized, double-blind, placebo-controlled, non-inferiority trial. Gastrointest Endosc. (2011) 74:1207–14. doi: 10.1016/j.gie.2011.07.072
12. Vickers A, Wilson P, Kleijnen J. Acupuncture. Qual Saf Heal Care. (2002) 11:92–7. doi: 10.1136/qhc.11.1.92
13. Lee A, Done ML. The use of nonpharmacologic techniques to prevent postoperative nausea and vomiting: a meta-analysis. Anesth Analg. (1999) 88:1362–9. doi: 10.1213/00000539-199906000-00031
14. Vickers AJ. Can acupuncture have specific effects on health? A systematic review of acupuncture antiemesis trials. J R Soc Med. (1996) 89:303–11. doi: 10.1177/014107689608900602
15. Tarçin O, Gürbüz AK, Poçan S, Keskin O, Demirtürk L. Acustimulation of the neiguan point during gastroscopy: its effects on nausea and retching. Turk J Gastroenterol. (2004) 15:258–62.
16. Cahn AM, Carayon P, Hill C. Acupuncture in gastroscopy. Lancet. (1978) 311:182–3. doi: 10.1016/S0140-6736(78)90614-1
17. Lee H, Ernst E. Acupuncture for GI endoscopy: a systematic review. Gastrointest Endosc. (2004) 60:784–9. doi: 10.1016/S0016-5107(04)02030-9
18. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. (2009) 339:332–6. doi: 10.1136/bmj.b2535
19. Wang W, Zhang T, Peng W, Wu J, Liu Z. Acupuncture for discomfort in patients during gastroscopy: a systematic review protocol. BMJ Open. (2014) 4:e005735. doi: 10.1136/bmjopen-2014-005735
20. Higgins JPT, Thomas JWV, (eds),. Cochrane Handbook for Systematic Reviews of Interventions Version 6.1. Cochrane (2020). Available from: www.training.cochrane.org/handbook (accessed January 3, 2022)
21. Schaible A, Schwan K, Bruckner T, Plaschke K, Büchler MW, Weigand M, et al. Acupuncture to improve tolerance of diagnostic esophagogastroduodenoscopy in patients without systemic sedation: results of a single-center, double-blinded, randomized controlled trial (DRKS00000164). Trials. (2016) 17:1–9. doi: 10.1186/s13063-016-1468-0
22. Cui B. Clinical trial on prevention and treatment of side effects during gastroscopy in middle-aged and senior people with Zusanli(ST-36) acupoint. China Acad Chin Med Sci. (2006) 9:865035. doi: 10.3389/fmed.2022.865035
23. Zhou Y, Fang H. Clinical effect of acupuncture at Neiguan(PC-6) and Zusanli(ST-36) during gastroscopy examination. In: Chinese Nursing Association National Academic Exchange Conference of Traditional Chinese and Western Medicine Nursing. Wuhan (2009). 4 p.
24. Li W, Wang L. A randomized controlled clinical trial for acupuncture to prevent adverse effect during gastroscopy. Chinese J Med Innov. (2012) 9:155–6.
25. Jin X, Yang Q, Liu W. Clinical observation of 102 cases by using electroacupuncture during gastroscopy. In: China Association of Traditional Chinese Medicine 21st Annual Congress on Spleen and Stomach Diseases. Nanjing (2009). p. 75–8.
26. Chen Y, Lu Q, Lan A. Clinical observation for acupuncture to prevent nausea and vomiting during gastroscopy. Chinese J Acupunct Moxibustion. (2007) 09:685–6.
27. Qi C. Theoretical Study and Clinical Observation of Auricular Acupoint Pressing on Improving Tolerance During Gastroscopy. Nanjing University of Traditional Chinese Medicine (2009).
28. Wang R, Cai H, Zheng W. Application of acupuncture anesthesia in gastrointestinal endoscopy. J Massage Rehabil Med. (2015) 6:32–3.
29. Chen M. Observation of Clinical Analgesic Effect of Superficial Needle on Gastroscopy. Nanjing: Nanjing University of Traditional Chinese Medicine (2019).
30. Jiang H. The application of acupressure on Neiguan point(PC-6) in patients during normal gastroscopy. Hunan J Tradit Chinese Med. (2013) 29:82–3.
31. Qi C, Jin X. Observation of clinical effects of electroacupuncture plus auricular plaster on gastroscopy. Shanxi J Tradit Chinese Med. (2008) 11:32–3.
32. Wu X, Ye R. Clinical observation of 50 cases by using acupuncture plus auricular plaster during gastroscopy. Henan J Tradit Chinese Med. (2010) 30:1018–9.
33. Yang J. Clinical Study of Superficial Needle Improving Tolerance During Gastroscopy. Nanjing: Nanjing University of Traditional Chinese Medicine (2015).
34. Leung WW, Mui WL, Ng SS, Lee JF, Ng EK. Lau JY. Acupuncture for diagnostic upper endoscopy in adults? A randomized sham-controlled trial. Gastrointest Endosc. (2008) 67:AB245. doi: 10.1016/j.gie.2008.03.646
35. Zhou J, Pan B, Feng J. Application of acupuncture at Neiguan(P-6) and Zusanli(ST-36) in gastroscopy. Bright Chinese Med. (2007) 04:53–5.
36. Liang F, Li Y, Liu J. Anesthesia effect of auricular acupoints pressing in fibergastroscopy. Guangxi J Tradit Chinese Med. (1988) 05:32.
37. Wang S. A randomized controlled clinical trial for acupuncture stimulation of Liangqiu(ST-34) to prevent adverse effect during gastroscopy. J Qilu Nurs. (2011) 17:60–1.
38. Tian Q, Wu W. Clinical observation for acupuncture to prevent nausea and vomiting during gastroscopy. Chin J Inf Tradit chinese Med. (1999) 04:64.
39. Dai Y, Sheng Y, Wu T. Clinical effect of acupuncture at Neiguan(PC-6) and Zusanli(ST-36) in gastroscopy. Front Med. (2020) 10:208–10.
40. Wang S. Observation on the effect of acupuncture at Neiguan point(PC-6) before gastroscopy. Chin J Dig Integr Tradit West Med. (2004) 5:303.
41. Zhang P, Hao X, Ma H. Comparison of the effect of acupuncture and active drugs before fibergastroscopy. J Weifang Med Coll. (1991)2:144–5.
42. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
43. Mayor D. An exploratory review of the electroacupuncture literature: clinical applications and endorphin mechanisms. Acupunct Med. (2013) 31:409–15. doi: 10.1136/acupmed-2013-010324
45. Bai L, Yan H, Li L, Qin W, Chen P, Liu P, et al. Neural specificity of acupuncture stimulation at pericardium 6: evidence from an fMRI study. J Magn Reson Imaging. (2010) 31:71–7. doi: 10.1002/jmri.22006
46. Streitberger K, Ezzo J, Schneider A. Acupuncture for nausea and vomiting: an update of clinical and experimental studies. Auton Neurosci Basic Clin. (2006) 129:107–17. doi: 10.1016/j.autneu.2006.07.015
47. Shiotani A, Tatewaki M, Hoshino E, Takahashi T. Effects of electroacupuncture on gastric myoelectrical activity in healthy humans. Neurogastroenterol Motil. (2004) 16:293–8. doi: 10.1111/j.1365-2982.2004.00504.x
48. Sarosiek I, Song G, Sun Y, Sandoval H, Sands S, Chen J, et al. Central and peripheral effects of transcutaneous acupuncture treatment for nausea in patients with diabetic gastroparesis. J Neurogastroenterol Motil. (2017) 23:245–53. doi: 10.5056/jnm16097
49. Wang WL, Wu ZH, Sun Q, Wei JF, Chen XF, Zhou DK, et al. Meta-analysis: the use of carbon dioxide insufflation vs. room air insufflation for gastrointestinal endoscopy. Aliment Pharmacol Ther. (2012) 35:1145–54. doi: 10.1111/j.1365-2036.2012.05078.x
50. Li CK, Nauck M, Löser C, Fölsch UR, Creutzfeldt W. Acupuncture to alleviate pain during colonoscopy. Dtsch Med Wochenschr. (1991) 116:367–70. doi: 10.1055/s-2008-1063621
51. Fanti L, Gemma M, Passaretti S, Guslandi M, Testoni PA, Casati A, et al. Electroacupuncture analgesia for colonoscopy: a prospective, randomized, placebo-controlled study. Am J Gastroenterol. (2003) 98:312–6. doi: 10.1111/j.1572-0241.2003.07231.x
Keywords: acupuncture, endoscopy, gastrointestinal, systematic review, meta-analysis
Citation: Gao N, Chen H, Wang Y, Guo Y, Liu Z and Wang W (2022) Acupuncture to Improve Patient Discomfort During Upper Gastrointestinal Endoscopy: Systematic Review and Meta-Analysis. Front. Med. 9:865035. doi: 10.3389/fmed.2022.865035
Received: 01 February 2022; Accepted: 14 April 2022;
Published: 03 June 2022.
Edited by:
Tony Tham, Ulster Hospital, United KingdomReviewed by:
Christopher Velez, Massachusetts General Hospital and Harvard Medical School, United StatesCopyright © 2022 Gao, Chen, Wang, Guo, Liu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhishun Liu, emhpc2h1bmpvdXJuYWxAMTYzLmNvbQ==; Weiming Wang, d2FuZ3dlaW1pbmcxYTFAMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.