
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med., 04 May 2022
Sec. Healthcare Professions Education
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.863257
Background: After learning new skills, healthcare professionals do not always apply them in practice, despite being motivated. This may be referred to as an intention-behavior gap. One example is the positioning of immobilized and disabled patients in hospitals, nursing homes, or neurorehabilitation clinics. Positioning is crucial to prevent complications such as pressure sores, pneumonia, and deep vein thrombosis. However, it is often not carried out optimally even when professionals have completed education programs. The LiN-method is a positioning procedure involving a special focus on aligning and stabilizing body parts, which has been shown to have advantages over conventional positioning. We assess which factors may facilitate or hinder the use of LiN in clinical practice after participants complete training.
Methods: A longitudinal survey with 101 LiN-course participants was conducted in Germany. Each participant completed a questionnaire directly after the course and 12 weeks later, including a report of the frequency of use in practice. They also completed a questionnaire which surveyed 23 aspects that might facilitate or hinder use of the new skills, covering the workplace, socio-collegial factors, motivation, self-confidence, and mindset.
Results: Most assessed aspects were associated with LiN-use, with the highest correlations found for confidence with the method, perceived ease of application, sufficient time, assessing one's skills as sufficient, remembering the relevant steps, and a work environment open to advanced therapeutic concepts. To reduce data complexity, the questionnaire was subjected to a factor analysis, revealing six factors. A regression analysis showed that four factors predicted use 12 weeks after course completion, in the following order of importance: (1) subjective aspects/confidence, (2) access to materials, (3) work context, and (4) competent support in the workplace.
Conclusion: Numerous aspects are associated with the use of recently acquired clinical or nursing skills, such as LiN. Many of these can be improved by appropriately setting up the workplace. The aspects most associated with use, however, are confidence with the method and self-perceived competence of healthcare professionals. While causality still needs to be demonstrated, this suggests that education programs should support participants in developing confidence and foster a mindset of continuous learning.
The intention-behavior gap is well-known and described in numerous domains, including the healthcare context (1, 2). It refers to the phenomenon that people have specific intentions for how they would like to act, but–often without understanding the reasons themselves– fail to act on these intentions. For example, nurses in hospitals know the importance of handwashing, yet often wash their hands less frequently than advised (3–5). Another important domain in the healthcare context is the positioning of severely affected immobile patients: Nurses, therapists, or caregivers often do not apply the positioning methods they learned frequently enough, or optimally, to prevent complications and enhance patient wellbeing (6–9). Determining why this is the case is crucial to derive recommendations on how to improve this situation.
To provide more background, numerous severely affected patients worldwide are unable to change their body position while hospitalized or being cared for at home. Reasons for immobility include stroke, dementia, or COVID-19 (10–12). Besides being discomforting for patients, this immobility can lead to complications such as pressure ulcers, deep vein thrombosis, pneumonia, and urinary tract infection (13–17). These factors can increase morbidity and mortality (18), hospital length of stay (19), and hospital costs (20, 21).
One way to address the risks of prolonged immobility is re-positioning patients in regular intervals (e.g., 2 h) (22, 23). This is frequently done in internal medicine, neurology, geriatrics, and intensive care units. The purpose of positioning is to prevent the aforementioned complications of prolonged immobility (24–26), to enhance patient comfort, and to improve the patient's respiratory condition (27). Positioning can also reduce the risk of aspiration, contractures, shoulder pain, and swelling (28, 29).
The LiN-method is a specific positioning concept developed around the year 2000. LiN is an abbreviation for the German term “Lagerung in Neutralstellung,” which translates to “Positioning in Neutral.” To regulate muscle tone and decrease the risk of contractures, the location of the body sections in relation to each other is analyzed and corrected in such a way that overstretching and shortening of muscles are avoided as much as possible. In contrast to conventional positioning, the body no longer adapts to the surface (often leading to malalignment, too much elongation, or shortening) and hollow spaces are avoided. The trunk and extremities are stabilized systematically with more blankets, bed covers, and pillows than usual to maintain the alignment of the whole body. Using more positioning material increases the supported areas, and the pressure on the body is thus lower in LiN-positions compared to conventional positions (30). In a randomized, multicenter, investigator-blinded, controlled trial, Pickenbrock et al. (31) compared the effects of LiN and conventional positioning on patient comfort and passive mobility. In 218 adult non-ambulatory patients with central neurological disorders, it was observed that patients perceived the LiN-positions as significantly more comfortable than the corresponding conventional positions. In addition, only in the LiN group, the passive mobility of the hips and shoulders improved when measured after 2 h of positioning. It was also shown that being positioned in LiN for 2 h had no negative effects on blood pressure, heart rate, and respiratory rate compared to being positioned conventionally (32).
However, despite the advantages of effective positioning methods, such as LiN, it is known that they are not always implemented in clinical practice. For example, nurses can often name the goals of positioning and different positions, but do not carry them out properly in practice (33–36). There is only scarce evidence on the effects of positioning training on clinical practice, but existing studies suggest that effects are often insufficient or even lacking (6, 7, 9).
It is currently unknown which specific factors contribute to the intention-behavior gap in positioning after completed training. We investigated potential reasons that might help or hinder healthcare professionals to regularly apply proper positioning methods in practice, using the example of the LiN-method. Conceivable are various aspects related to the workplace (e.g., accessibility of materials), colleagues' attitudes, study opportunities (e.g., refresher days), or confidence. Knowledge about the order of importance of these aspects may help to foster the use of effective practices, such as LiN, leading to benefits for patient health and enhancing the cost-effectiveness of courses offered to healthcare professionals. Therefore, the aim of this study was to assess how often LiN is applied in practice after course completion and which aspects may facilitate or hinder its application.
We used a longitudinal survey design with two time points. After completing a LiN-course, participants were asked if they were interested in participating in the study. Participants then completed a questionnaire directly after course attendance and 12 weeks later.
A questionnaire about the reasons that might influence the frequency of LiN-use was developed in collaboration with a group of 40 LiN-trainers. All experts were asked for their opinion on which aspects might facilitate or hinder the use of LiN in clinical practice. Most provided their answers in written form, others were interviewed personally. After collecting and synthesizing the experts' opinions, the following three groups of possible reasons were identified:
• Workplace (8 items, e.g., “There is enough staff.”).
• Social factors/colleagues (10 items, e.g., “My colleagues approve of LiN and are cooperative with respect to its use.”).
• Motivation, confidence, and attitudes (5 items, e.g., “I am confident that I am doing everything correctly during LiN-application.”).
Each potential reason was formulated as a questionnaire item. The questionnaire did not directly ask whether participants believed that these aspects affected their LiN-use. Rather, participants rated the degree to which the items applied in their situation. As answer options, a Likert-scale was used (1: does not apply at all, 2: hardly applies, 3: partly applies, 4: mostly applies, 5. completely applies). The complete questionnaire can be found in Table 1 (see Supplementary Material 1 for the original German version).
We collected the following variables of interest:
• Estimate of the expected future LiN-use [in % of patients with LiN indication, measured in 10% steps using a sliding scale, similar to Herold and Kirsch (37)].
• Sociodemographics (age, gender, occupational group, years in the profession, etc.).
• Self-reported frequency of LiN-use (in % of patients with LiN indication, measured in 10% steps using a sliding scale).
• Questionnaire of aspects of potential relevance to LiN-use (see previous section).
The surveys also included some additional variables not analyzed here (see Supplementary Materials 2, 3).
Participants were included if the following criteria applied: (1) practices a caring profession (e.g., nurse, geriatric nurse, healthcare worker), or works as a physical therapist, occupational therapist, or in another therapeutic profession; (2) applies positioning in professional everyday life; and (3) is not a caring relative (i.e., positions exclusively privately). We had originally planned to include 200 participants based on a power analysis assuming relatively small effect sizes (i.e., pwr::pwr.r.test() in R showed that this sample size was required to detect correlations of r = 0.2 with a power of 0.80 and alpha = 0.05, two-tailed, when not correcting for multiple comparisons) (38). However, due to the COVID-19 pandemic, many courses were canceled, resulting in a smaller sample size.
The secure SoSci Survey questionnaire tool (39) was used for questionnaire implementation and data collection. Participants received links to the questionnaire via email as well as several reminder emails. Each participant had the chance to win one of six vouchers (2 x €50, 2 x €100, 2 x €150). Completing both questionnaires took a maximum of 35 min.
For the statistical analysis, the quantitative data was analyzed using Python 3.8 (40) with Pandas (41), Numpy (42), and Matplotlib (43), and R (44). The data were assessed for distribution and spread and then analyzed.
We used the following approach:
1. We calculated Spearman-rank correlations between each of the 23 aspects and actual LiN-use at time point 2. Due to the ordinal data structure, Spearman's rank correlations instead of Pearson's correlation coefficients were used. To avoid false positive findings, we corrected for multiple comparisons using the Holm-Bonferroni procedure (45, 46). We also estimated 95% confidence intervals for the correlation coefficients following the approach by Fieller, Hartley, and Pearson (47), using an R-script provided by Bishara and Hittner [Supplement A in (48)].
2. For a better intuitive understanding of the data, we also visualized how the top-half and bottom-half of LiN users differed in terms of the 23 aspects and demographics, by categorizing participants using a median split on the LiN-use variable. While it is difficult to define what constitutes objectively high or low use, a median split can give an approximate idea of the characteristics of participants using it relatively often vs. rarely.
3. Due to expected correlations amongst some of the 23 aspects, we applied factor analysis (FA) to reduce the questionnaire items to factor groups. FA is a multivariate statistical technique for reducing a large number of variables to fewer dimensions and is commonly applied in nursing research (49). We used exploratory rather than confirmatory FA in case our three predetermined categories were not accurate. To test the applicability of FA to our dataset we conducted Bartlett's test and the Kaiser-Meyer-Olkin (KMO) test (50– 52). For the FA, we used the FactorAnalyzer package for Python (53) with varimax rotation. We used an Eigenvalue threshold of 1.0 to extract factors. As recommended by Watson and Thomson (49), we describe the parameters of our FA as well as the resulting reduced dimensions.
4. The resulting factor scores from the FA were used as predictors in a multiple regression analysis with the outcome variable LiN-use at time point 2. For the estimation of the weighting of relationships between the variables, we used the ordinary least squares (OLS) method.
From January to December 2020, 24 LiN basic courses were conducted in Germany by 14 different trainers (4 nurses, 7 physical therapists, 3 occupational therapists) with a total number of 230 course participants [mean: 9.58 participants per course, standard deviation (SD) = 2.448]. The typical length of a course was 2 days. 126 participants agreed to take part (55%). Out of these, 101 (92% female, mean age: 37 years, SD = 10.74, see Table 2 for more details) completed both questionnaires and were included in the data analysis (response rate: 80%).
Immediately after the course, participants expected to use LiN for a median of 60% of patients for whom LiN was appropriate. At follow-up, the median of the self-reported LiN-use was 40%.
Figure 1 shows the correlation coefficients between all questionnaire items with LiN-use, ordered in descending order by the size of the coefficients. Most correlations were significant, even after correcting for multiple comparisons (54, 55). Of note, confidence intervals around the correlation coefficients were relatively large (Figure 1), leaving some uncertainty regarding the size of the effects.
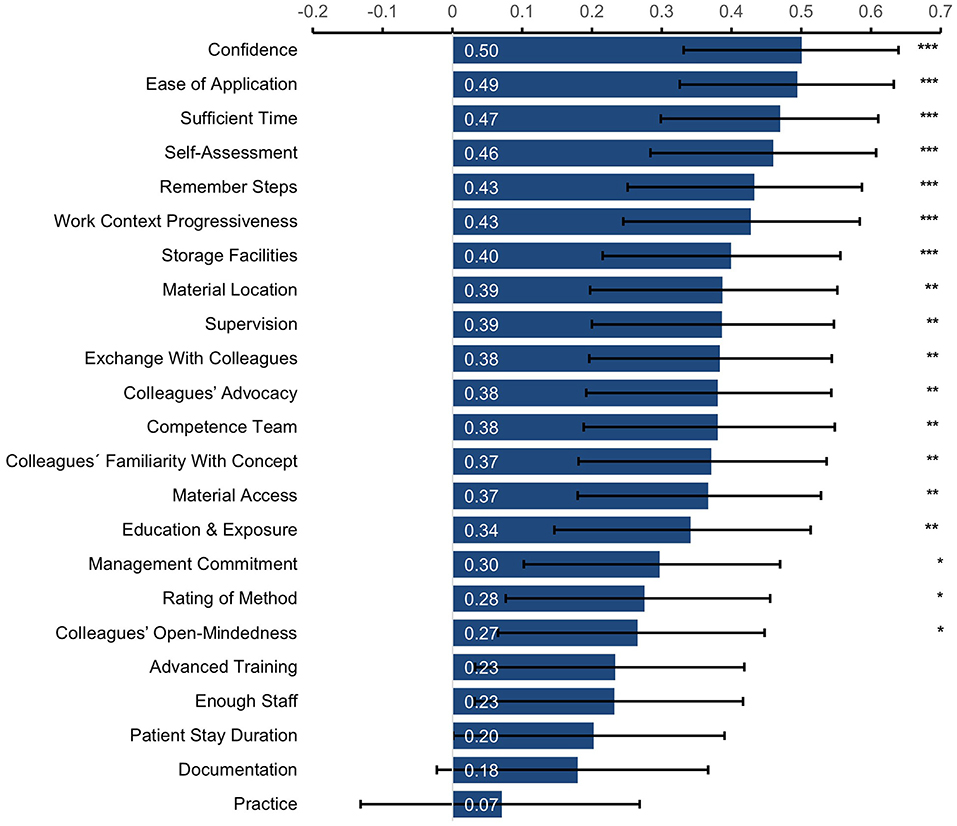
Figure 1. Spearman's rank correlation coefficients between self-reported LiN-use and the individual questionnaire items. Items are ordered by the size of the correlation coefficient. ***p < 0.001, **p < 0.01, *p < 0.05 (adjusted for multiple comparisons using Holm-Bonferroni correction). Error bars show 95% confidence intervals.
To further visualize the data, we divided participants into two groups, applying a median split, resulting in a high LiN-use group (N = 50) and a low LiN-use group (N = 42) with a calculated median of 40% (nine participants with a score of 40% were not assigned to either group). Table 2 shows demographics for both groups. Figure 2 depicts average ratings on all questionnaire items and shows that all questionnaire items were rated as higher by the high-use group compared to the low-use group.
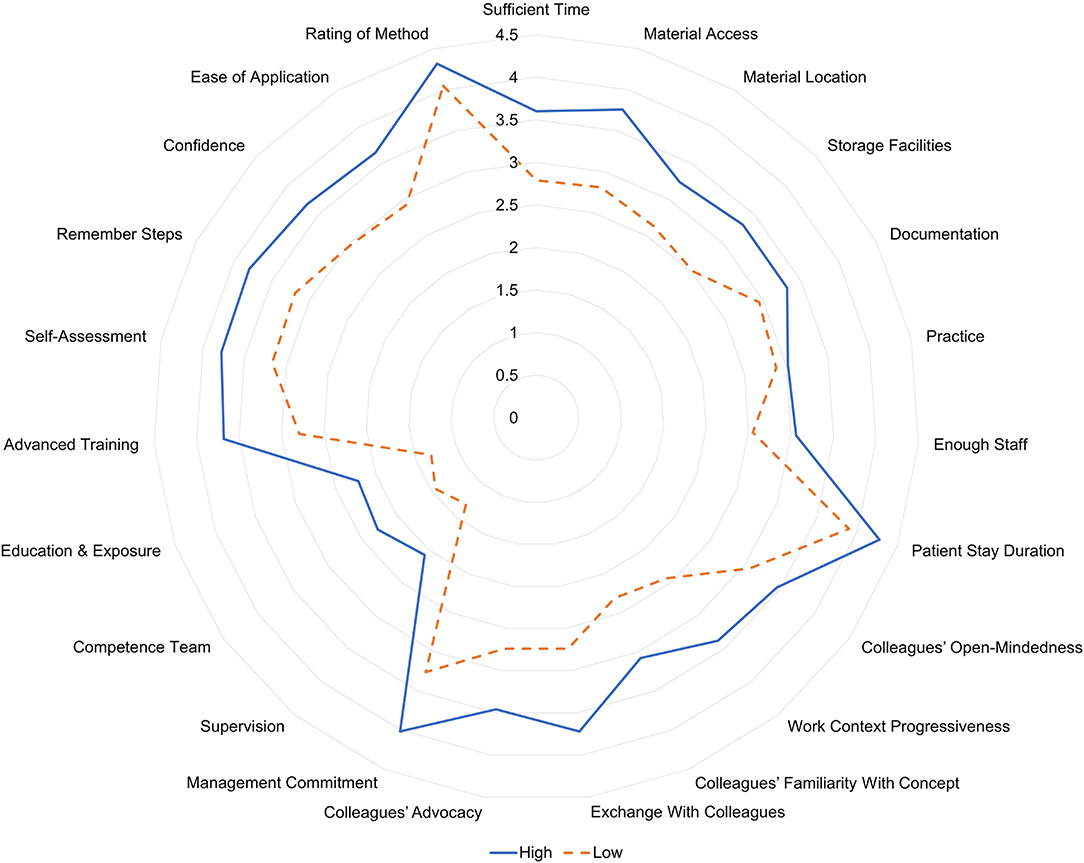
Figure 2. Comparison of item averages between the high LiN-use group and the low LiN-use group, derived by a median split.
FA is a statistical technique to reduce a high number of variables into fewer factors. It extracts maximum common variance from the individual variables and turns them into common scores. Despite a relatively small sample size, our analyses indicated that the data set was well-suited for FA (54): That is, the dataset had a KMO of 0.82 [with KMO value > 0.50 being considered acceptable (50, 51)], and Bartlett's Test of Sphericity (52) indicated that the observed correlation matrix was not an identity matrix (Chi-Square: 1082.78; p < 0.001).
The analysis procedure resulted in the selection of six factors. Table 3 shows how the items were grouped (indicated by bold font in each column). After reviewing the items contributing to each factor, we assigned the following six descriptive labels to the factors: 1. Subjective Aspects/Confidence, 2. Social Aspects, 3. Access to Materials, 4. Competent Support, 5. Training & Exposure, and 6. Work Context. The variance of the data explained by each factor ranged from 6 to 13% (see Table 3). All six factors together explained 56% of the variance.
After reducing our data set to six factors, we entered these factors into a regression analysis to predict LiN-use. We found that Factor 1 (Subjective Aspects/Confidence), Factor 3 (Access to Materials), Factor 4 (Competent Support), and Factor 6 (Work Context) positively predicted LiN-use, while Factor 2 (Social Aspects) and Factor 5 (Training & Exposure) did not. The overall model including all factors explained 45% of variance in actual LiN-use (adjusted R-squared).
The unstandardized regressors shown in Table 4 correspond to the predicted increase in LiN-use on the original measurement scale, as predicted by 1SD increase for the respective factor score. For example, a 1SD increase in the factor score for Factor 1 (Subjective Aspects/Confidence) is predicted to be associated with an absolute increase of 14% in LiN-use (on a scale from 0 to 100% of patients for whom LiN-use would be appropriate). The standardized regressors are provided as well to allow comparison across studies. They reflect the predicted increase in LiN-use in SD-units, as predicted by 1SD increase in the factor scores.
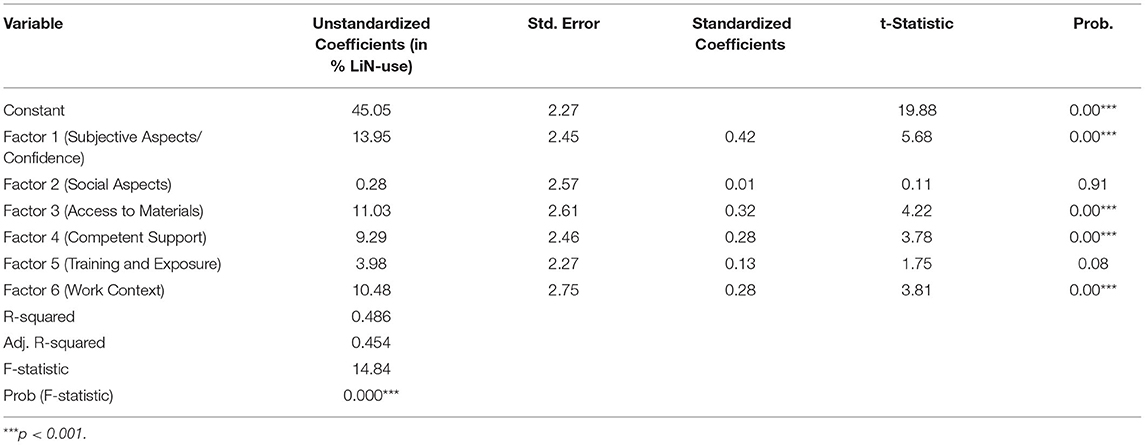
Table 4. Results of ordinary least squares (OLS) regression analysis predicting LiN-use (in % of patients for whom LiN-use would be appropriate) based on factor scores.
After completing a course on the LiN positioning method, participants expected to use the newly acquired skills for a median of 60% of patients for whom LiN-use was considered appropriate. However, despite this high motivation, 3 months later they reported using it only for a median of 40% of patients. This study used a data-driven approach to identify aspects that might explain this intention-behavior gap, without having specific hypotheses about the relative importance of the various aspects. We found that the aspects most correlated with LiN-use were self-reported confidence with the method, ease of application, having sufficient time, assessing one's skills as sufficient, remembering the steps, and work context progressiveness (all correlations > 0.40, Figure 1). We also carried out a factor analysis of the 23 assessed aspects, revealing six factors (Table 3). In a linear regression, four of these factors predicted LiN-use (Table 4). The factor explaining the most variance was again the one related to subjective aspects/confidence with the method, followed by a second factor related to the availability and accessibility of sufficient materials. The third most important factor related to having sufficient time, staff, and a progressive work environment, and the fourth one comprised supervision and a “competence team” (i.e., experienced LiN-team that can give advice) at work.
These results are relevant because previous research has shown that quality of positioning in clinical practice is often poor, and training only helps to a limited extent. Lincoln et al. (34) observed that up to 13% of positioning on stroke units of a hospital in England was poorly performed, as well as 30% of positioning on other wards (medicine and geriatric). Dowsell et al. (35) report that patients with stroke spent 26% of their time in poor positioning. In terms of the effects of training, Jones et al. (9) showed that a 4-h training in positioning accompanied by a workbook led to 61% of all assessed aspects of posture to be done correctly, as opposed to 56% before the training [see also (6)]. While this was a significant increase, it is still not satisfactory. In a study by Forster et al. (7), after a 9-h training of positioning, 21% of patients still spent their time in poor positioning, compared to 31% before (a non-significant difference).
Our study suggests how the quality of positioning and of education programs might be improved by targeting certain aspects that are linked with the use of newly acquired positioning skills. Prominent theories of self-regulation and behavior change propose that, in order to regulate behavior (e.g., learn to apply a new nursing task regularly), one may modulate both external situation/environment (in this case: hospital environment and team context) and internal states (55). The current results suggest that for the use of newly acquired healthcare skills, both pathways might be important and both may–and perhaps must–be targeted to enhance the implementation of relevant practices after training.
Many environmental and team factors which were found to be important–such as offering sufficient storage capacity, enough personnel, etc.–should and can be provided by hospitals and organizations themselves. An important consideration here is that the costs for preventing pressure ulcers are much lower than treating the sores (56, 57). However, in addition to these external factors, our study shows that the aspects that correlated most with LiN-use were participants' internal states (e.g., confidence).
It is important to keep in mind that the current study was correlational and cannot speak to the direction of causality: For example, confidence with the method might lead to higher use, but higher use of the method might also increase one's confidence. Future studies should use interventions to target specific aspects identified here to determine if this would lead to higher use. It is also worth considering the potential clinical significance of the effects. Guidelines regarding the interpretation of correlation coefficients differ vastly and depend on context. However, some of the higher correlations found here (>0.40, Figure 1) would be classified by most guidelines as at least “moderate” in size (58–60); and they are higher than what is typically found in behavioral and psychological studies (61, 62). Other correlations, however, were small and all the confidence intervals (Figure 1) were relatively large, leaving uncertainty regarding the size of the effects (56, 57). The regression model further showed that each of the calculated factor scores predicted relatively substantial increases in LiN-use: A 1SD increase in Factor 1 (Subjective Aspects/ Confidence), Factor 3 (Access to Materials), Factor 4 (Competent Support), and Factor 6 (Work Context) predicted absolute increases in LiN-use of 14, 11, 9, and 10%, respectively. The links found here might be meaningful in practice, especially if they accumulate across people and time (61), but more research is needed to determine their significance.
How then can subjective factors such as confidence and ease of application be increased? One option might be to offer ample practice opportunities during training, offering encouragement, and–as proposed by Williams (63)–fostering a growth mindset. A growth mindset (64, 65) –as opposed to a fixed mindset–emphasizes that our talents are not set in stone, that we can learn new skills, and that mistakes are not a sign of weakness but rather useful for learning. A recent review (66) suggests that interventions to foster this mindset might be useful in health professions education [see also (67)]. Another possible intervention may be to direct healthcare professionals to pay attention to the positive consequences of using the new skills–such as being aware of the subjective feeling they experience when they help patients feel more comfortable (68).
The study has a few limitations. First, due to the COVID-19 pandemic, more than 50% of the planned LiN-courses were canceled. Therefore, we were only able to acquire a sample size that was smaller than initially planned, as is typical for many studies conducted in this time span (69). However, our sample size was still large enough to detect effects. For the factor analysis and regression analysis, the sample size was on the lower end, but appeared to still be acceptable (51, 70); for future use of the questionnaire, the factor structure should be reassessed in larger samples. Second, the COVID-19 pandemic led to changes in the work situation of health care professionals, such as increased pressure and psychosocial burden, which might have influenced our results (71–73) (see Supplementary Material 3 for some relevant comments by participants). However, even without the pandemic context, large intention-behavior gaps have been documented in many domains of human behavior change (2, 74). Third, there is a chance of a response bias: For example, it is possible that participants who opted in for the study were more motivated to apply LiN than those who did not. We cannot determine if such a bias was present in our sample, but the fact that almost 55% of course participants chose to take part in the study suggests that our results at least apply to a large proportion of potential course participants. Moreover, even in a sample of somewhat more motivated participants, it would still be relevant to determine which factors are associated with use after a course, since–as discussed–even highly motivated participants often apply new skills less than they planned.
The study also has several strengths. It is one of the first studies that systematically assesses a whole range of potential aspects that might influence the application of newly acquired clinical practices, including both internal and environmental aspects. Even though some of our results may seem unsurprising (e.g., access to materials correlates with higher use), the research confirming these intuitions was still lacking, and the relative importance of the various aspects was unknown. Moreover, we conducted a factor analysis to group the various aspects into factors predicting clinical practice. Previous research on educational programs for preventing pressure ulcers has been very limited (75). Finally, our results may not only apply to LiN but also to other newly acquired clinical skills or behaviors that are relevant in the clinical context, as well as to the design of effective training programs (76, 77).
In conclusion, we identified a set of aspects associated with LiN-use in practice months after course completion. The most important aspects appear to be participants' confidence and ease of application. However, there were indeed numerous aspects–relating to work set-up, colleagues, and motivation–that were clearly associated with higher LiN-use. This is hopeful news, as it suggests that by addressing many of these aspects simultaneously, a real difference can be made in terms of facilitating the use of newly acquired clinical skills. As LiN and other effective positioning methods can substantially improve patient mobility and wellbeing, as well as reduce risk for pressure ulcers and other complications, this new knowledge may be crucial for informing training approaches for healthcare professionals and, thus, for optimal clinical care.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Research Ethics Committee of the Chamber of Physicians Westfalen-Lippe and the Medical Faculty of the Westphalian Wilhelms University Muenster (2019-574-f-S). The patients/participants provided their written informed consent to participate in this study.
VL and HP designed the study, the questionnaire, and prepared the study materials. VL prepared the online questionnaire. All authors performed the data collection, with DD responsible for the technical implementation. DD analyzed the data and created the figures of results. All authors drafted, edited, provided feedback, and approved the final version.
This study was funded by the LiN-Arge.
HP developed the LiN approach and is a member of LiN-Arge e.V., a non-profit organization that promotes the LiN approach. All authors have repeatedly received fees by LiN-Arge e.V. for working on research or other projects related to LiN in the past.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors would like to thank the course participants for their valuable contribution to the research, as well as the experts who provided their opinions and experiences during the development of the questionnaire. We are also grateful to Anna Fry Bechtel for proofreading and comments.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.863257/full#supplementary-material
1. Faries MD. Why we don't “just do it. Am J Lifestyle Med. (2016) 10:322–9. doi: 10.1177/1559827616638017
2. Sheeran P, Webb TL. The intention-behavior gap. Soc Personal Psychol Compass. (2016) 10:503–18. doi: 10.1111/spc3.12265
3. Wetzker W, Bunte-Schönberger K, Walter J, Pilarski G, Gastmeier P, Reichardt C. Compliance with hand hygiene: reference data from the national hand hygiene campaign in Germany. J Hosp Infect. (2016) 92:328–31. doi: 10.1016/j.jhin.2016.01.022
4. Kingston L, O'Connell NH, Dunne CP. Hand hygiene-related clinical trials reported since 2010: a systematic review. J Hosp Infect. (2016) 92:309–20. doi: 10.1016/j.jhin.2015.11.012
5. Fuller C, Besser S, Savage J, McAteer J, Stone S, Michie S. Application of a theoretical framework for behavior change to hospital workers' real-time explanations for noncompliance with hand hygiene guidelines. Am J Infect Control. (2014) 42:106–10. doi: 10.1016/j.ajic.2013.07.019
6. Jones A, Tilling K, Wilson-Barnett J, Newham DJ, Wolfe CDA. Effect of recommended positioning on stroke outcome at six months: a randomized controlled trial. Clin Rehabil. (2005) 19:138–45. doi: 10.1191/0269215505cr855oa
7. Forster A, Dowswell G, Young J, Sheard J, Wright P, Bagley P. Effects of a physiotherapist-led stroke training programme for nurses. Age Ageing. (1999) 28:567–74. doi: 10.1093/ageing/28.6.567
8. Tan C-E, Hi M-Y, Azmi NS, Ishak NK, Mohd Farid FA, Abdul Aziz AF. Caregiving self-efficacy and knowledge regarding patient positioning among malaysian caregivers of stroke patients. Cureus. (2020) 12:e7390. doi: 10.7759/cureus.7390
9. Jones A, Carr EK, Newham DJ, Wilson-Barnett J. Positioning of stroke patients: evaluation of a teaching intervention with nurses. Stroke. (1998) 29:1612–7. doi: 10.1161/01.STR.29.8.1612
10. Moore Z, Patton D, Avsar P, McEvoy NL, Curley G, Budri A, et al. Prevention of pressure ulcers among individuals cared for in the prone position: lessons for the COVID-19 emergency. J Wound Care. (2020) 29:312–20. doi: 10.12968/jowc.2020.29.6.312
11. Gorelick PB. The global burden of stroke: persistent and disabling. Lancet Neurol. (2019) 18:417–8. doi: 10.1016/S1474-4422(19)30030-4
12. Launer LJ. Statistics on the burden of dementia: need for stronger data. Lancet Neurol. (2019) 18:25–7. doi: 10.1016/S1474-4422(18)30456-3
13. Wu X, Li Z, Cao J, Jiao J, Wang Y, Liu G, et al. The association between major complications of immobility during hospitalization and quality of life among bedridden patients: a 3 month prospective multi-center study. PLoS ONE. (2018) 13:e0205729. doi: 10.1371/journal.pone.0205729
14. Mervis JS, Phillips TJ. Pressure ulcers: pathophysiology, epidemiology, risk factors, and presentation. J Am Acad Dermatol. (2019) 81:881–90. doi: 10.1016/j.jaad.2018.12.069
15. Guo F, Shashikiran T, Chen X, Yang L, Liu X, Song L. Clinical features and risk factor analysis for lower extremity deep venous thrombosis in Chinese neurosurgical patients. J Neurosci Rural Pract. (2015) 6:471–6. doi: 10.4103/0976-3147.169801
16. Brogan E, Langdon C, Brookes K, Budgeon C, Blacker D. Respiratory infections in acute stroke: nasogastric tubes and immobility are stronger predictors than dysphagia. Dysphagia. (2014) 29:340–5. doi: 10.1007/s00455-013-9514-5
17. Zhu C, Liu H, Wang Y, Jiao J, Li Z, Cao J, et al. Prevalence, incidence, and risk factors of urinary tract infection among immobile inpatients in China: a prospective, multi-centre study. J Hosp Infect. (2020) 104:538–44. doi: 10.1016/j.jhin.2019.11.018
18. Dellinger EP. Prevention of hospital-acquired infections. Surg Infect. (2016) 17:422–6. doi: 10.1089/sur.2016.048
19. Theisen S, Drabik A, Stock S. Pressure ulcers in older hospitalised patients and its impact on length of stay: a retrospective observational study. J Clin Nurs. (2012) 21:380–7. doi: 10.1111/j.1365-2702.2011.03915.x
20. Dick AW, Perencevich EN, Pogorzelska-Maziarz M, Zwanziger J, Larson EL, Stone PW, et al. decade of investment in infection prevention: a cost-effectiveness analysis. Am J Infect Control. (2015) 43:4–9. doi: 10.1016/j.ajic.2014.07.014
21. NAPS North American Precis, Syndicate. Pressure Ulcers Cost U.S. Healthcare $10.2 Billion and Contribute to Nearly 29,000 Hospital Deaths Each Year. AP News. Available online at: https://apnews.com/article/a9fcd7f85f3d43e491714a5d612cc079 (accessed January 2, 2022).
22. Gillespie BM, Chaboyer WP, McInnes E, Kent B, Whitty JA, Thalib L. Repositioning for pressure ulcer prevention in adults. Cochrane Database Syst Rev. (2014) 2014:CD009958. doi: 10.1002/14651858.CD009958.pub2
23. Krishnagopalan S, Johnson EW, Low LL, Kaufman LJ. Body positioning of intensive care patients: clinical practice versus standards. Crit Care Med. (2002) 30:2588–92. doi: 10.1097/00003246-200211000-00031
24. Banasik JL, Emerson RJ. Effect of lateral positions on tissue oxygenation in the critically ill. Heart Lung. (2001) 30:269–76. doi: 10.1067/mhl.2001.116012
25. Johnson KL, Meyenburg T. Physiological rationale and current evidence for therapeutic positioning of critically ill patients. AACN Adv Crit Care. (2009) 20:228–40. doi: 10.1097/NCI.0b013e3181add8db
26. Gillespie BM, Walker RM, Latimer SL, Thalib L, Whitty JA, McInnes E, et al. Repositioning for pressure injury prevention in adults: an abridged cochrane systematic review and meta-analysis. Int J Nurs Stud. (2021) 120:103976. doi: 10.1016/j.ijnurstu.2021.103976
27. Lasater-Erhard M. The effect of patient position on arterial oxygen saturation. Crit Care Nurse. (1995) 15:31–6. doi: 10.4037/ccn1995.15.5.31
28. Ada L, Goddard E, McCully J, Stavrinos T, Bampton J. Thirty minutes of positioning reduces the development of shoulder external rotation contracture after stroke: a randomized controlled trial. Arch Phys Med Rehabil. (2005) 86:230–4. doi: 10.1016/j.apmr.2004.02.031
29. de Jong LD, Nieuwboer A, Aufdemkampe G. Contracture preventive positioning of the hemiplegic arm in subacute stroke patients: a pilot randomized controlled trial. Clin Rehabil. (2006) 20:656–67. doi: 10.1191/0269215506cre1007oa
30. Pickenbrock H, Ludwig VU, Zapf A. Support pressure distribution for positioning in neutral versus conventional positioning in the prevention of decubitus ulcers: a pilot study in healthy participants. BMC Nurs. (2017) 16:60. doi: 10.1186/s12912-017-0253-z
31. Pickenbrock H, Ludwig VU, Zapf A, Dressler D. Conventional versus neutral positioning in central neurological disease: a multicenter randomized controlled trial. Dtsch Arztebl Int. (2015) 112:35–42. doi: 10.3238/arztebl.2015.0035
32. Pickenbrock H, Zapf A, Dressler D. Effects of therapeutic positioning on vital parameters in patients with central neurological disorders: a randomised controlled trial. J Clin Nurs. (2015) 24:3681–90. doi: 10.1111/jocn.12990
33. Mee LYS, Bee WH. A comparison study on nurses' and therapists' perception on the positioning of stroke patients in Singapore general hospital. Int J Nurs Pract. (2007) 13:209–21. doi: 10.1111/j.1440-172X.2007.00630.x
34. Lincoln NB, Willis D, Philips SA, Juby LC, Berman P. Comparison of rehabilitation practice on hospital wards for stroke patients. Stroke. (1996) 27:18–23. doi: 10.1161/01.STR.27.1.18
35. Dowswell G, Dowswell T, Young J. Adjusting stroke patients' poor position: an observational study. J Adv Nurs. (2000) 32:286–91. doi: 10.1046/j.1365-2648.2000.01475.x
36. Li Z, Zhou X, Cao J, Li Z, Wan X, Li J, et al. Nurses' knowledge and attitudes regarding major immobility complications among bedridden patients: a prospective multicentre study. J Clin Nurs. (2018) 27:1969–80. doi: 10.1111/jocn.14339
37. Herold A, Kirsch JJ. Komplikationen nach stapler-hämorrhoidektomie ergebnisse einer umfrage in deutschland. coloproctology. (2001) 23:8–16. doi: 10.1007/PL00001884
38. Champely S. pwr: Basic Functions for Power Analysis. R package version 1.3–0. (2020). https://CRAN.R-project.org/package=pwr
39. Leiner DJ. SoSci survey (version 3.1. 06) [computer software]. München: SoSci Survey GmbH (2019).
41. McKinney W. Data structures for statistical computing in python. In: Proceedings of the 9th Python in Science Conference. Austin, Texas. SciPy (2010). p. 56–61. doi: 10.25080/Majora-92bf1922-00a
42. Harris CR, Millman KJ, van der Walt SJ, Gommers R, Virtanen P, Cournapeau D, et al. Array programming with NumPy. Nature. (2020) 585:357–62. doi: 10.1038/s41586-020-2649-2
43. Hunter JD. Matplotlib: a 2D graphics environment. Comput Sci Eng. (2007) 9:90–5. doi: 10.1109/MCSE.2007.55
44. R Core Team, editor. R: A language and environment for statistical computing. R Vienna: Foundation for Statistical Computing (2020). Available online at: https://www.R-project.org/.
46. Aickin M, Gensler H. Adjusting for multiple testing when reporting research results: the Bonferroni vs Holm methods. Am J Public Health. (1996) 86:726–8. doi: 10.2105/AJPH.86.5.726
47. Fieller EC, Hartley HO, Pearson ES. Tests for rank correlation coefficients. I Biometrika. (1957) 44:470. doi: 10.2307/2332878
48. Bishara AJ, Hittner JB. Confidence intervals for correlations when data are not normal. Behav Res Methods. (2017) 49:294–309. doi: 10.3758/s13428-016-0702-8
49. Watson R, Thompson DR. Use of factor analysis in journal of advanced nursing: literature review. J Adv Nurs. (2006) 55:330–41. doi: 10.1111/j.1365-2648.2006.03915.x
50. Kaiser HF. An index of factorial simplicity. Psychometrika. (1974) 39:31–6. doi: 10.1007/BF02291575
51. Watkins MW. Exploratory factor analysis: a guide to best practice. J Black Psychol. (2018) 44:219–46. doi: 10.1177/0095798418771807
52. Bartlett MS. A further note on the multiplying factors for various' ' chi-square approximations in factor analysis. J R Stat Soc. (1954) 16:296–8. doi: 10.1111/j.2517-6161.1954.tb00174.x
53. Biggs J, Madnani N. Factor_analyzer Documentation, Release 0.3.1. Available online at: https://factor-analyzer.readthedocs.io/_/downloads/en/latest/pdf/ (accessed February 25, 2022).
54. Kang H. A guide on the use of factor analysis in the assessment of construct validity. J Korean Acad Nurs. (2013) 43:587–94. doi: 10.4040/jkan.2013.43.5.587
55. Gross JJ. The emerging field of emotion regulation: an integrative review. Rev Gen Psychol. (1998) 2:271–99. doi: 10.1037/1089-2680.2.3.271
56. Demarré L, Van Lancker A, Van Hecke A, Verhaeghe S, Grypdonck M, Lemey J, et al. The cost of prevention and treatment of pressure ulcers: a systematic review. Int J Nurs Stud. (2015) 52:1754–74. doi: 10.1016/j.ijnurstu.2015.06.006
57. Mathiesen ASM, Nørgaard K, Andersen MFB, Møller KM, Ehlers LH. Are labour-intensive efforts to prevent pressure ulcers cost-effective? J Med Econ. (2013) 16:1238–45. doi: 10.3111/13696998.2013.832256
58. Overholser BR, Sowinski KM. Biostatistics primer: part 2. Nutr Clin Pract. (2008) 23:76–84. doi: 10.1177/011542650802300176
59. Schober P, Boer C, Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesth Analg. (2018) 126:1763–8. doi: 10.1213/ANE.0000000000002864
61. Funder DC, Ozer DJ. Evaluating effect size in psychological research: sense and nonsense. Adv Method Pract Psychol Sci. (2019) 8:251524591984720. doi: 10.1177/2515245919847202
62. Gignac GE, Szodorai ET. Effect size guidelines for individual differences researchers. Pers Individ Dif. (2016) 102:74–8. doi: 10.1016/j.paid.2016.06.069
63. Williams CA. Mindsets may matter in nursing education. Nurs Educ Perspect. (2018) 39:373–4. doi: 10.1097/01.NEP.0000000000000267
64. Dweck CS, Yeager DS. Mindsets: a view from two eras. Perspect Psychol Sci. (2019) 14:481–96. doi: 10.1177/1745691618804166
66. Williams CA, Lewis L. Mindsets in health professions education: a scoping review. Nurse Educ Today. (2021) 100:104863. doi: 10.1016/j.nedt.2021.104863
67. Lewis LS, Williams CA, Dawson SD. Growth mindset training and effective learning strategies in community college registered nursing students. Teach Learn Nurs. (2020) 15:123–7. doi: 10.1016/j.teln.2020.01.006
68. Ludwig VU, Brown KW, Brewer JA. Self-regulation without force: can awareness leverage reward to drive behavior change? Perspect Psychol Sci. (2020) 15:1382–99. doi: 10.1177/1745691620931460
69. Tuttle KR. Impact of the COVID-19 pandemic on clinical research. Nat Rev Nephrol. (2020) 16:562–4. doi: 10.1038/s41581-020-00336-9
70. Mundfrom DJ, Shaw DG, Ke TL. Minimum sample size recommendations for conducting factor analyses. Int J Test. (2005) 5:159–68. doi: 10.1207/s15327574ijt0502_4
71. Jalili M, Niroomand M, Hadavand F, Zeinali K, Fotouhi A. Burnout among healthcare professionals during COVID-19 pandemic: a cross-sectional study. Int Arch Occup Environ Health. (2021) 94:1345–52. doi: 10.1007/s00420-021-01695-x
72. Zerbini G, Ebigbo A, Reicherts P, Kunz M, Messman H. Psychosocial burden of healthcare professionals in times of COVID-19 - a survey conducted at the University Hospital Augsburg. Ger Med Sci. (2020) 18:Doc05. doi: 10.3205/000281
73. Gold JA. Covid-19: adverse mental health outcomes for healthcare workers. BMJ. (2020) 369:m1815. doi: 10.1136/bmj.m1815
74. Pellegrino R, Crandall PG, Seo H-S. Using olfaction and unpleasant reminders to reduce the intention-behavior gap in hand washing. Sci Rep. (2016) 6:18890. doi: 10.1038/srep18890
75. Porter-Armstrong AP, Moore ZE, Bradbury I, McDonough S. Education of healthcare professionals for preventing pressure ulcers. Cochrane Database Syst Rev. (2018) 5:CD011620. doi: 10.1002/14651858.CD011620.pub2
76. Booth J, Hillier VF, Waters KR, Davidson I. Effects of a stroke rehabilitation education programme for nurses. J Adv Nurs. (2005) 49:465–73. doi: 10.1111/j.1365-2648.2004.03319.x
77. Loft MI, Poulsen I, Martinsen B, Mathiesen LL, Iversen HK, Esbensen BA. Strengthening nursing role and functions in stroke rehabilitation 24/7: a mixed-methods study assessing the feasibility and acceptability of an educational intervention programme. Nurs Open. (2019) 6:162–74. doi: 10.1002/nop2.202
Keywords: positioning, behavior change, skill acquisition, nursing, pressure ulcers, quality of care
Citation: Ludwig VU, Pickenbrock H and Döppner DA (2022) Factors Facilitating and Hindering the Use of Newly Acquired Positioning Skills in Clinical Practice: A Longitudinal Survey. Front. Med. 9:863257. doi: 10.3389/fmed.2022.863257
Received: 27 January 2022; Accepted: 28 March 2022;
Published: 04 May 2022.
Edited by:
Stefan J. Schaller, Charité Universitätsmedizin Berlin, GermanyReviewed by:
Frantisek Duska, Charles University, CzechiaCopyright © 2022 Ludwig, Pickenbrock and Döppner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vera U. Ludwig, dmVyYS5sdWR3aWdAcGVubm1lZGljaW5lLnVwZW5uLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.