
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med., 14 April 2022
Sec. Healthcare Professions Education
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.854403
This article is part of the Research TopicSelf-Care in Healthcare Workers for Sustainable Healthcare SystemsView all 9 articles
 Huel-Ju Tsai1,2
Huel-Ju Tsai1,2 Meng-Ting Tsou2,3,4*
Meng-Ting Tsou2,3,4*Background: This cross-sectional study aimed to analyze the association between burnout, work-related factors and metabolic syndrome (MetS) among various health-care workers (HCWs) at a tertiary hospital in Taiwan.
Methods: Relevant demographic data were obtained through written questionnaires. Information about psychosocial and work conditions, including assigned department, working hours, shifts, and sleep condition, was obtained. Burnout was evaluated according to the Chinese version of Maslach Burnout Inventory–Health Services Survey. MetS was analyzed according to the criteria of the National Cholesterol Education Program of Taiwan–Treatment Panel for Adults III.
Results: A total of 1,055 non-doctor/nurse and 2,078 doctor/nurse staff with a median age of 45.2 and 36.1 years participated in this study. The incidence of burnout was nearly 6.42 and 6.68% and that of MetS was 31.4 and 13.5% in non-doctor/nurse and doctor/nurse staff, respectively. The results showed that burnout induced a higher Odds ratio (OR) of MetS in the doctor/nurse group (OR = 1.96, p = 0.01). Other factors, such as night shift and seniority (>10 years), led to a higher OR of MetS, but a decreased risk was observed based on seniority (2–4 years). Further, young female participants and young doctors/nurses with burnout had a higher OR of MetS compare to other groups (OR = 2.43 and 2.32, p < 0.05).
Conclusion: The study results suggested positive relationship between burnout and MetS in young female staffs and young doctors/nurses. For doctor/nurse staff with higher seniority or more night shifts, strategies are needed to prevent burnout and MetS.
Health care workers (HCWs) need to respond immediately to patients and families, making their jobs stressful (1). HCWs are at risk for adverse health effects, including metabolic syndrome (MetS) and burnout, due to heavy workloads, patient cases, long service hours, and shift work (1–4).
According to Schaufeli et al., health professionals, police officers, and teachers have a high risk of burnout (5). If their relationship with patients/clients remains constant and intense, increased care requirements is associated with a higher risk of burnout (5). In a study conducted at a regional hospital in Taiwan, Chou et al. observed that among the five professions in the medical field, the highest prevalence of work-related stress occurred in nurses (66%), followed by medical assistants (61.8%), doctors (38.6%), administrative staff (36.1%), and medical technicians (31.9%) (2).
The association between age and burnout is not frequently explored in studies. Akkuş et al. analyzed the association between age and burnout and observed a decrease in the scores of the three domains of burnout with increasing age (6). In a meta-analysis, Gómez-Urquiza et al. observed that the age of young individuals was a significant factor in the emotional exhaustion and depersonalization domains of burnout (7).
In a study that analyzed a sample of the adult working population in Finland, Ahola et al. found that women with burnout had a U-shaped distribution. A negative association was observed between age and burnout in the first years of work (age: 18–40 years) and around the age of 60–64 years. In young women, a higher prevalence of burnout was found among younger workers (8).
In studies conducted by Chico-Barba et al. and Merces et al., MetS was prevalent in 38.7% Mexican nurses (9) and 24.4% primary care nursing professionals in Brazil, respectively (10). A study conducted in a tertiary hospital in Taiwan showed that the highest prevalence of MetS was observed in physicians (18.3%), followed by administrative staff (15.4%), medical technicians (9.4%), and nurses (6.6%) (3).
According to a previous study that reported the association between burnout and MetS among nursing staff working in Brazil primary health-care clinics, burnout increases the risk of MetS by 1.45% (95% confidence interval [CI] = 1.17–1.81) (10). Another study conducted on nursing staff working in tertiary hospital in Taiwan showed that those with burnout had a higher risk of MetS (odds ratio [OR] = 1.70, 95% CI = 1.04–3.05) (11). A study by Chico-Barba et al. observed an association between increased abdominal circumference and domains of emotional exhaustion burnout (adjusted OR [aOR] = 14.95; 95% CI = 1.5–148.7] and night shift (aOR = 12.39; 95% CI = 1.02–150.5) (9). However, few studies have explored the association between burnout, work factors, and professional categories and MetS among staff at a tertiary hospital in Taiwan.
In addition, age and sex have always been adjusted factors; however, in real-world setting, there are different proportions of hospital staff, including doctor/nurse and non-doctor/nurse groups, male and female groups and different age groups. Earlier studies have reported that age and profession affect burnout and MetS, respectively (6–10). Therefore, our hypothesis mainly included exploring the impact of burnout on MetS according to different age groups, sex and professions. This study aimed to determine the specific group in which burnout increases the risk of MetS. For these HCWs, in addition to traditional lifestyle modification education, this study provided evidence on preventive policies for burnout and the required work-related factors.
This cross-sectional study was conducted at the Health Evaluation Center, a 2,000-bed tertiary hospital in Northern Taiwan. MetS data were obtained from yearly routine physical examinations by HCWs.
Questionnaires were collected between December 2018 and March 2019 during employee physical examination. The contents of the self-administered questionnaire were explained to participants face to face before they were administered the questionnaire. If more than one-fourth of the questionnaire was not filled out, the questionnaire was excluded. Workforce in all departments, such as doctors, nurses, technicians, administrative staff, pharmacists, radiologists, and nutritionists, were included. Since doctors and nurses encounter the same conditions such as facing patients' problems on time, taking care of the patients, work patterns, and shift patterns, they were categorized into the doctor/nurse group and the remaining staff was categorized into the non-doctor/nurse for analysis. A total of 3,288 doctors/nurses and 1,943 non-doctors/nurses were invited to participate, and 2,078 and 1,055 of them, respectively, completed the questionnaire (actual response rate was 63.2 and 54.3%, respectively). In addition, a sample size of 2,533 achieved 90% power using the two tailed test (OR = 1.59, probability of null hypothesis = 0.15, alpha error = 0.05, power = 0.9, and R2 for other confounding factors = 0.5) (12). In total of 3,133 participants were included in this study, implying a sufficient statistical power.
Information was obtained through structured questionnaires, designed according to the Institute of Labor, Occupational Safety, and Health Ministry of Labor (13). In this survey, analysis of the internal consistency reliability showed the Cronbach α to be between 0.82 to 0.93, having good reliability. The questionnaire included: basic data and socioeconomic status (included age, education level, department, seniority, working hours, work style, Cronbach α: 0.93); personal lifestyle (included sleep duration, smoking, alcohol, exercise, fruit and vegetable intake, Cronbach α: 0.89); psychosocial work environment (Maslach Burnout Inventory–Health Services Survey test; MBI-HSS, Cronbach α: 0.82); mental health status (Brief Symptom Rating Scale-5, BSRS-5, Cronbach α: 0.90) (13).
Data on following baseline characteristics were collected, age, body height, body weight, waist circumference (WC), and blood pressure (BP). Height was measured with a standard stadiometer with an approximation value of 0.01 cm. Weight was measured using a set of calibrated electronic scales. The participants wore light clothes weighing ~0.01 kg. WC was measured at the anatomical region of the midpoint between the lower rib and the upper point of the iliac crest at the end of expiration. After the blood was drawn, rest for 10 min, and then start to use the digital electronic sphygmomanometer (MORON HEM7156, Japan) to measure the two arms. The arm with the higher blood pressure was taken as the measuring arm, and the first value was taken. Then, after a 10 min rest, measure the second time again, and average the two times to the final measured value (14). Height, weight, WC, and BP measurements were performed and recorded by trained nurses working at the Health Evaluation Center who were blinded to the patients' information.
Information concerning personal habits, including smoking status (yes/no: current or past/never), alcohol consumption (yes/no: ≥2 drinks per week/0–1 drink per week), exercise (yes: ≥3 times/week, ≥30 min/set), fruit intake (one serving: equivalent to one medium orange, apple, or guava), and vegetable intake (one serving: equivalent to a 15-cm plate or more than half a bowl), was collected (13). Information regarding the length of sleep duration and self-assessment of sleep quality was obtained through a self-administered questionnaire (13). Participants were asked to self-assess their sleep quality, and the response was classified as either “good” or “poor.”
Study participants were asked to provide information on the following during the past month before the survey: total weekly working hours and work style. The work style was divided into three classes according to the work shift that starts in the morning (D means day class: 8:00–16:00), evening (E means evening class: 16:00–24:00), and night (N means night class: 24:00–8:00). Night shift included the midnight work schedule. Participants were categorized into the following three types of work: regular class (D), night shift (E or N, fixed or rotation), and three shifts (D, E, and N rotation) (13).
Sample collection and analysis were performed in a standard laboratory with international accreditation (ISO-15189). All participants were informed to start fasting at 10:00 PM the night before and started blood draw at 8:00–10:00 AM the following day. at the Health Evaluation Center. The blood samplings were collected in a BD Vacutainer SSTTM (Becton Dickinson, Franklin Lakes, NJ, USA) sample collection tube. Sample collection and analysis principles were based on the standard requirements mentioned in the Clinical and Laboratory Standards Institute guidelines (specimen choice, collection, and handling; approved guideline H18-A3).
A Hitachi 7170 Automatic Analyzer (Hitachi Corp., Hitachinaka Ibaraki, Japan) was used to measure the levels of fasting glucose, lipid markers (including low- and high-density lipoprotein cholesterol [HDL-C: homogeneous enzymatic colorimetric assay], and triglycerides (TG).
Burnout domains were evaluated using the Chinese version of the MBI-HSS test (15) by Lu et al. (Cronbach's: 0.84) (16). The MBI-HSS evaluates three domains—emotional exhaustion (EE), depersonalization (DP), and personal accomplishment (PA); it included 22 questions. The seven-point Likert scale with scores ranging from 0 (never felt) to 6 (every day), measures the frequency of occurrence. The full scores of EE, DP and PA were 54, 30, and 48, respectively. According to the classification standard of Maslach et al. [15], an EE of score ≥27, a DP score of ≥13, and a PA ≤31 is categorized as high job burnout; if an EE score 17–26, a DP score 7–12, and a PA score 32–38 is considered moderate job burnout; and an EE score of ≤16, a DP score of ≤6, and a PA score of ≥39 is considered low job burnout. In previous studies, the psychological work demands, EE and DP were directly related to burnout; however, a negative association was observed between burnout with PA (15, 16). The scale has good reliability and validity. The internal consistency coefficients (Cronbach's α) of the three dimensions of EE, DP, and PA were 0.77, 0.83, and 0.82, respectively (16).
To analyze the metabolic score, we used the National Cholesterol Education Program–Adult Treatment Panel III (NCEP-ATP III) classification with specific cutoff values for abdominal obesity in the Taiwanese population.
For the standardization of the MetS criteria, individuals should meet at least three of the following five criteria to be included: (1) WC ≥90 cm for men and ≥85 cm for women, (2) HDL-C level <40 mg/dL for men and <50 mg/dL for women, (3) TG level ≥150 mg/dL, (4) BP ≥130/85 mmHg or receiving treatment for hypertension, and (5) fasting blood glucose ≥100 mg/dL or receiving treatment for type 2 diabetes mellitus (17).
The study protocol was reviewed and approved by the Research Ethics Committee on Human Beings of MacKay Memorial Hospital (research project number 18MMHISO150).
All participants provided written informed consent. Confidentiality in data collection was preserved, considering ethical issues, individual autonomy, and respect. This study was conducted in accordance with all guidelines of the Declaration of Helsinki. To ensure data confidentiality, patient identification information was replaced with a sheet number.
Descriptive analysis was performed to characterize the population sample. Data are presented as mean ± standard deviation for continuous variables and numbers and percentages for categorical variables. According to the cutoff value of the NCEP-ATP III, the MetS factors were classified into two categories. For each factor, frequencies and percentages were calculated.
Student's t-test was used to compare continuous variables between groups. For the analysis of categorical variables, the chi-square test was used. Spearman correlation coefficient matrix was used to analyze the relation between seniority with working hours and night shift. Multivariate logistic regression was used to investigate associations between MetS, burnout, and factors associated with work after adjusting for age, sex, educational level, and lifestyle characteristics and determine the association of burnout and prevalence of MetS in the age group stratified by sex and profession.
For statistical analysis, SPSS Statistics version 22 (IBM Corp., Armonk, NY, USA) for Windows was used, and p < 0.05 was considered bilateral.
A total of 2,078 doctors/nurses and 1,055 non-doctors/nurses were included in this study. Table 1 showed the mean age and proportion of male participants was significantly higher in the non-doctor/nurse group than that in the doctor/nurse group (45.24 ± 10.21 vs. 36.14 ± 9.83 years and 19.43% vs. 7.42%, respectively; p < 0.001). The educational level in the doctor/nurse group was significantly higher than that in the non-doctor/nurse group. Vegetable and fruit intake, exercise, and smoking behavior tended to be higher in the non-doctor/nurse group than in the doctor/nurse group. The seniority of the doctor/nurse staff was mostly ≤10 years. In contrast, seniority of 41% of the non-doctor/nurse staff was >10 years. The working hour was obviously higher in the doctor/nurse group than in the non-doctor/nurse group. Moreover, 44% of the doctor-nurse staff worked for >46 h per week, and nearly 61% of the doctor/nurse group needed to perform three shifts and night shift. No statistically statistic different was observed between the non-doctor/nurse and doctor/nurse groups in terms of the sleep duration (mean and standard deviation: 6.58 [0.78] vs. 6.60 [1.04] h; p = 0.325]. A higher prevalence of poor sleep quality was observed in the doctor/nurse group than that in the non-doctor/nurse group (64.43% vs. 54.78%; p < 0.001).
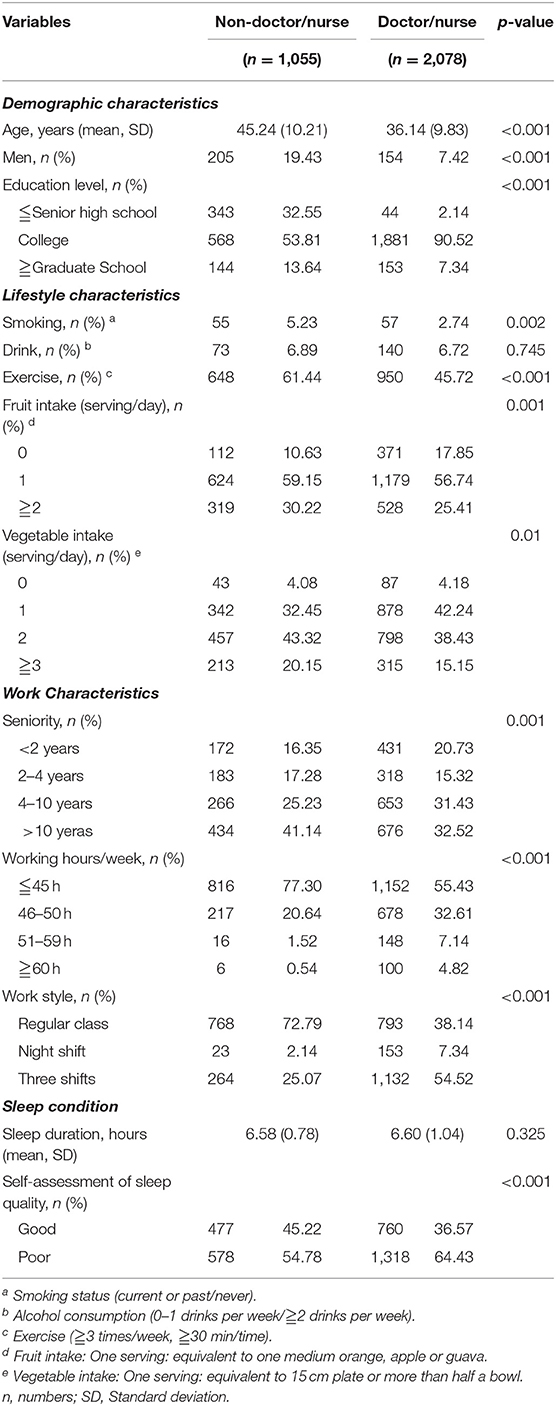
Table 1. Demographics, lifestyle factors, work-related characteristics, and sleep condition of the study in this table participants stratified according to profession.
Table 2 shows mentioned the prevalence and condition of MetS and burnout of the two groups. The prevalence of MetS and MetS factors in the non-doctor/nurse group was statistical significantly higher than that in the doctor/nurse group (MetS prevalence: total, 19.0%; 29.81% vs. 13.54, p < 0.001). In the non-doctor/nurse group, hyperglycemia and central obesity ranked by the prevalence as the first and second, respectively. In the doctor/nurse group, central obesity and high BP ranked by the prevalence as the first and second, respectively. Regarding the prevalence of burnout (burnout prevalence: total, 6.6%; non-doctor/nurse group vs. doctor/nurse group, 6.42% vs. 6.68%; p = 0.88), no statistically difference was observed between the groups. However, the analysis of the three domains showed that the score and prevalence of emotional exhaustion and depersonalization were higher in the doctor/nurse group than that in the non-doctor/nurse group.
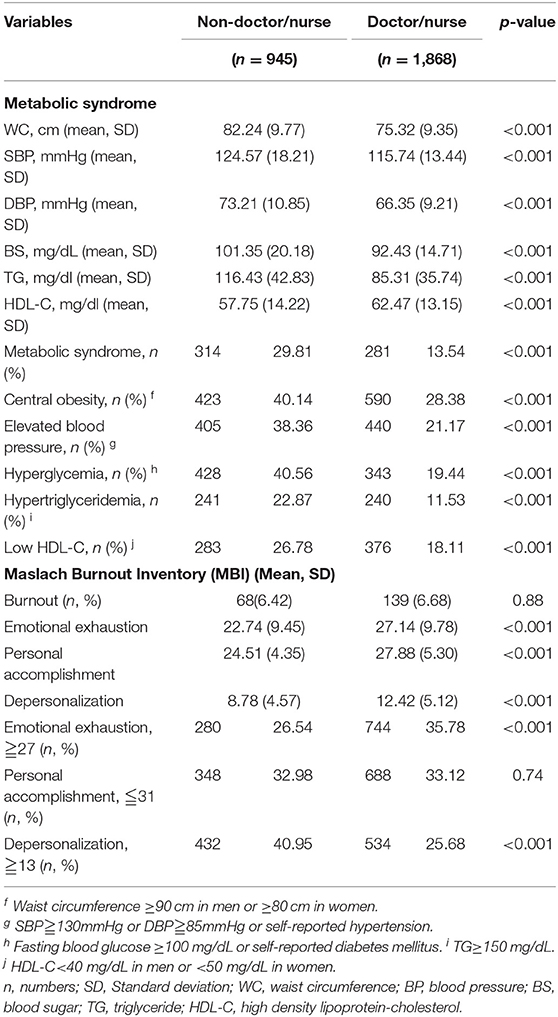
Table 2. Prevalence of MetS, components of MetS, burnout and burnout domains stratified according to profession.
After adjusting for age, sex, educational level, lifestyle characteristics, and sleep quality (Table 3), the results showed that burnout in the doctor/nurse group increased the risk of MetS by 1.96% (95% CI = 1.15–3.35; p = 0.01). In addition, the risk of MetS according to seniority was higher in participants working for >10 years (OR = 1.30; 95% CI = 1.02–2.90; p = 0.04); but lower participants working for seniority of 2–4 years (OR = 0.49; 95% CI = 0.26–0.99; p = 0.04). Night shift increased the risk of MetS in the doctor/nurse group (OR = 2.72; 95% CI = 1.39–5.34; p = 0.004).
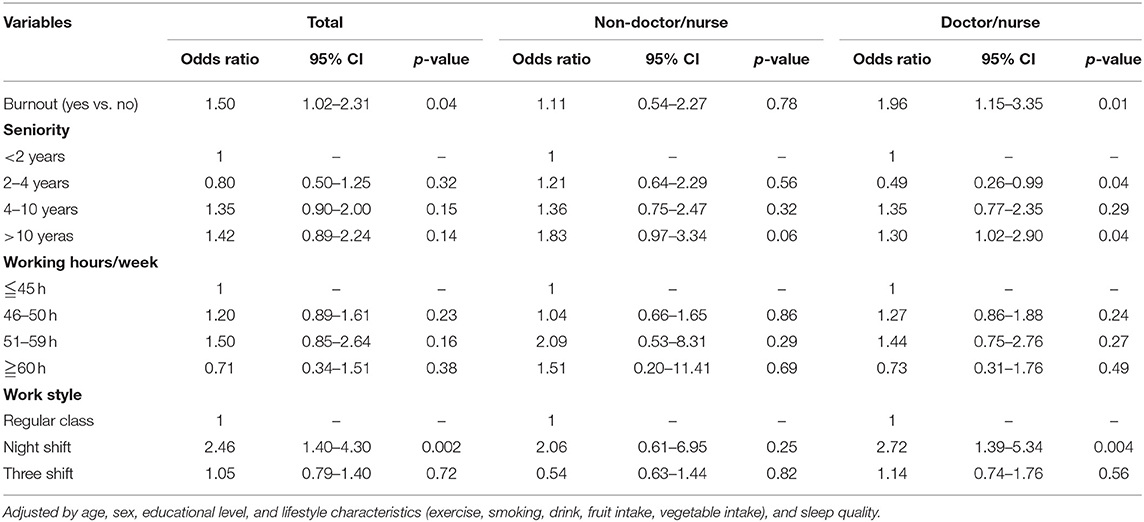
Table 3. Multivariate logistic regression analysis of burnout and working factors influencing MetS stratified according to profession.
Supplementary Table 1 showed the correlation of seniority with working hours/week and shift work by Spearman correlation coefficient matrix. The data showed below ±0.5 that means no or poor correlation.
The results obtained after stratification according to age and sex suggested that female participants with burnout had a higher prevalence of MetS than female participants without burnout in the younger stratum (OR = 2.34; 95% CI = 1.14–4.80) (Table 4). When stratifying according to age and profession, doctor/nurse staff with burnout had a higher prevalence of MetS than the doctor/nurse staff without burnout in the younger cohort (OR= 2.32, 95% CI = 1.11–4.87) (Table 5). In male participants, older participants or non-doctor/nurse staff, the prevalence of MetS was not statistically significantly different among the burnout and non-burnout groups (Tables 4, 5).
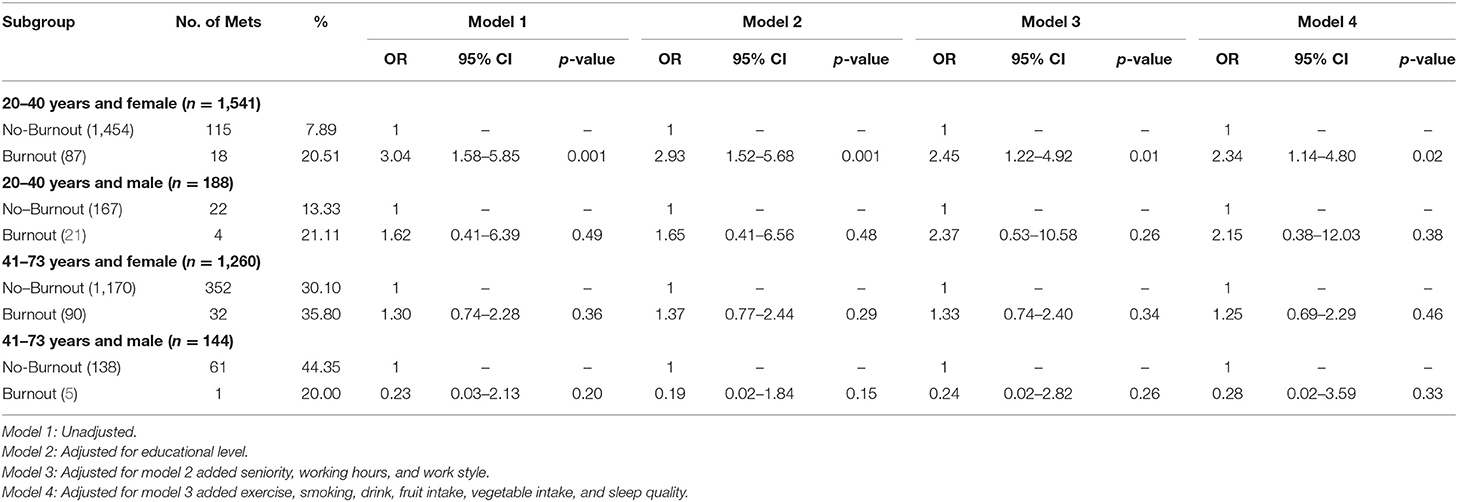
Table 4. The association between burnout and prevalence of MetS by using logistic regression analysis stratified according to age and sex.
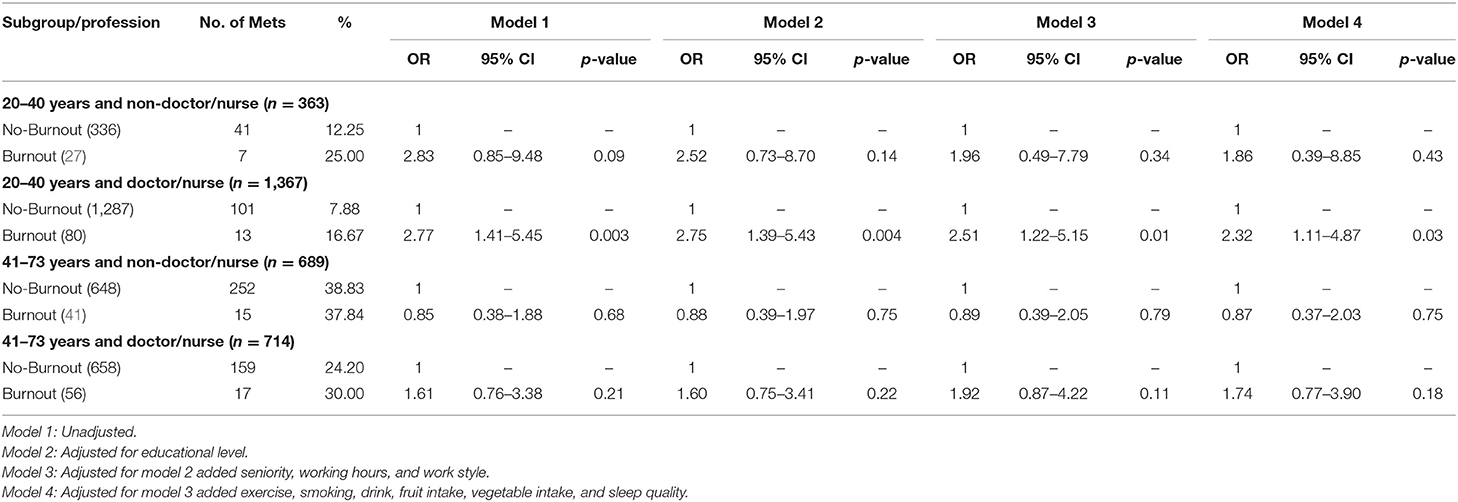
Table 5. The association between burnout and prevalence of MetS by using logistic regression analysis stratified according to age and profession.
In our study, doctor/nurse staff with night shifts and seniority >10 years had a higher OR of MetS, but those with seniority of 2–4 years had a decreased OR of MetS. In a further stratified analysis, it was found that female participants aged 20–40 years had a higher OR of MetS after adjusting for the burnout factor than those in other age and sex groups. At the same time, our results showed that young doctor/nurse staff with burnout had a higher OR of MetS compared to older doctor/nurse staff and non-doctor/nurse staff. Therefore, burnout associated with an increasing OR of MetS among young female professionals and doctors/nurses.
Our results showed that overall prevalence of MetS in all HCWs was 19.0%, higher than reported in another previous study in a tertiary hospital in Taiwan (12%) (3). The prevalence of MetS in the non-doctor/ nurse and doctor/nurse groups was 29.81 and 13.54%, respectively; the prevalence of MetS in the former group was similar to that reported in the general population in a previous Taiwanese study (25.5% of men and 31.5% of women) (18), whereas that in the latter group was lower than that reported in the general population, but similar to that reported in study conducted by Yeh et al. (3). The main reason may be that doctor/nurse group included young female professionals with healthy worker effect (3). A study by Hwang et al. analyzed a sample of the general population and observed that women aged <50 years had a low prevalence of MetS than men in the same age group (19), which was attributed to the hypothesis of a persistent hormone effect in premenopausal women (20). In our study, the doctor/nurse group predominantly included female professionals aged <40 years (92.6% and 36.1 years) compared to the non-doctor/ nurse group (80.6% and 45.2 years), and the hypothesis observed in the study by Hwang et al. can corroborate to the understanding of the lower prevalence of MetS in these groups.
However, in the study by Wei et al., the prevalence of MetS was 12.1% in a sample of workers in Taiwan (21), which is in contrast to our findings that the prevalence of MetS in hospital doctor/nurse employees was not lower and that those in the non-doctor/nurse group had a higher prevalence of MetS that as the general population. Therefore, hospital HCWs have a higher risk of being diagnosed with MetS due to the work environment. Bergmann et al., Chandola et al., and Garbarino et al. observed that work stress, long hours of work, and burnout are associated with MetS (22–24). In our study, we found that the prevalence of burnout among was 6.6, 6.42, and 6.68%, respectively, which not statistically significantly different (p = 0.88). However, in a previous regional hospital study in Taiwan, a higher prevalence of work-related burnout was observed in nurses (66%) and physicians (38.6%) (2).
There are several possible reasons for the different in the prevalence of burnout. First, we used the Chinese version of the MBI-HSS (15, 16), which has good reliability and validity for hospital employees (Cronbach's α: 0.84), which was different from other studies that used the Chinese version of the Copenhagen Burnout Inventory (2). Second, in this study, participants were younger (median age 38.4 years) than those in other studies (4, 9). Finally, our study participants had a high level of education (higher than college: 97.9%), and a previous study reported that women with high burnout scores had a higher frequency of low levels of education (25).
A previous study showed that the prevalence and risk of MetS increases with age, which has a positive correlation with seniority (17). A study in Mexico on tertiary hospital nurses showed that working in the night shift and seniority ≥15 years were associated with adiposity-based chronic disease (26). In our study, we found that doctor/nurse staff on night shift and with seniority >10 years had a higher risk of MetS; these results were consistent with those of previous studies (26–28). The novel finding in our study was that seniority of 2–4 years had a decreased risk of MetS, the possible reason was younger age of these group.
Cross-sectional studies by Copertaro et al. and Ha et al. and retrospective studies by Biggi et al. and Brum et al. have suggested an association between shift work and MetS (29–32). In a prospective study with a 5-year follow-up with 387 female employees of a Taiwan plant, Lin et al. showed that rotating shift work significantly increased the risk of MetS (33). Coworkers who initially had one or two risk factors for metabolic disease were 4.6 and 12.7 times more likely to develop the condition after 5 years. In a 4-year prospective study by Pietroiusti et al., an association between burnout and night shifts was observed in health workers (hazard ratio: 5.10; 95% CI = 2.15–12.11; p = 0.001) (34), thus corroborating with the hypothesis that a high level of stress during night shift may have an influence on MetS (23, 35).
A study by Chou et al. conducted with a sample from a Taiwanese hospital revealed that being in the younger age group, working overtime; being a nurse or doctor, and having a high-tension job were associated with high burnout (2). The burnout rate of nurses was >50% (2). Wang et al. showed that doctors had a higher stress rate than the general population. Shanafelt et al. reported that doctors had a greater degree of suffering than individuals in other professions (37.9% vs. 27.8%, respectively) (36, 37). Several studies have described that chronic work stress and long working hours, which could lead to reduction in sleep and exercise, and changes in eating habits, can be highly associated with the prevalence of MetS (3, 24, 27, 28). A study conducted in Mexico on tertiary hospital nurses showed that unhealthy lifestyle (<3 days per week and/or <30 min per session of physical activity and poor dietary habits) was associated with adiposity-based chronic disease (26). In our study, higher working hours, night shifts, lower exercise, and less healthy habits were found in doctor/nurse group compare to non-doctor/nurse group.
In our study, we found no statistically significant difference in terms of sleep duration between the non-doctor/nurse and doctor/nurse groups (6.58 vs. 6.60 h, p = 0.325), and poor self-assessment sleep quality was higher in the doctor/nurse group than in the non-doctor/nurse group (p < 0.001). Previous studies extensively review the published literature and provide a comprehensive overview on sleep quality in MetS, the results showed the sleep quality played an important role to be as a modulator of metabolic homeostasis (38, 39). The sleeping quality was adjusted in our analysis to avoid interference with the results.
The relationship between burnout, night shift, and sleep condition and MetS can be grouped into three categories. (1) Hormone activity: chronic stress is associated with hyperstimulation of the hypothalamic-pituitary axis; as a consequence, several hormones participate in these reactions, such as growth hormone, thyroid hormone, insulin, ghrelin, leptin, and cortisol (17–20, 40, 41). (2) Inflammation activity: burnout and sleep insufficiency increase the level of pro-inflammatory cytokine (such as C-reactive protein) (42, 43). (3) Sympathetic activity: a stressful lifestyle and short sleep duration stimulate the sympathetic–adrenal–medullary axis, stimulating the adrenal glands to release catecholamines (e.g., epinephrine and norepinephrine) (23, 24).
The components that showed the highest prevalence of MetS were hyperglycemia (40.56%) and central obesity (40.14%) in the non-doctor/nurse group and central obesity (28.38%) and hypertension (21.17%) in the doctor/nurse group. Similar findings were reported by Yeh et al., Pietroiusti et al., and Basei Rossa et al., who corroborate the hypothesis that blood glucose control, WC, and BP are important to improve the health status of hospital employees (3, 34, 44).
A previous study reported that burnout level reduced with increasing age in men, but the association was bimodal in women, with women aged 20–35 and >55 years showing the highest burnout level (45). When associations are examined by sex, women appear to report higher levels of burnout than that in men (46). The reasons included work and non-work stressors.
In the early stages of their careers, younger workers need to master their job requirements and face a greater risk of burnout (47). In addition, younger employees may need to juggle work–family conflicts, which is another risk factor that leads to burnout (48). However, with successful work mastery, employees can adapt to work requirements and demands, and burnout may begin to decline with age. In addition, work-family conflicts may also be reduced (49), thereby reducing their impact on burnout.
Associations between age and burnout were strongly moderated by sex. Men and women have different levels of exposure to work and non-work stressors (50). Generally, men are often exposed to better working conditions and lower work-family conflicts than women (51). Men and women in the workplace also tend to respond differently to different work and non-work stressors (work–family conflict) (52, 53).
In a further stratified analysis, we found that female professionals aged 20–40 years had a lower prevalence of MetS from previous studies but had a higher risk of MetS after adjusting for the burnout factor than professionals in other ages and sex groups. According to the above findings, burnout, shift work, and poor sleep conditions induce MetS. Different ages and sex induce burnout, which can further lead to MetS. This fact suggests that acquiring work mastery (such as a doctor/nurse job) combined with work–family conflicts (as the principal care provider in the family) is often higher in women than in men (51, 52). In general, women are more stressed, leading to burnout, which in turn induces a higher risk for MetS.
An analysis of the association between burnout and MetS in hospital HCWs, between the different professions, and an analysis stratified by age, sex, and profession were the strong points of this study. A unique feature of this study is that we draw on previous MetS analysis and burnout prevalence in medical teams, including younger age [a significant factor in the burnout domains (7); higher for young female nursing staff [OR, 20–40 years vs. 41–65 years = 1.74 vs. 1.29 (2)] and profession [the greater the constancy and the intense the relationship with the patients, the greater the care needs to be provided, which leads to a greater risk of burnout (5)]. To our knowledge, this is a result that has not been specifically analyzed yet.
This study has some limitations. First, it was a single-institution study. Second, the causality of the associations was not analyzed because of the cross-sectional study design. Third, the study had a small sample size of participants from different departments, including: doctors 110 (3.5%), nurses 1968 (62.8%), medical technology department [radiology 52 (1.7%), laboratory 105 (3.4%), pathology 42 (1.3%), others 284 (9.1%)], nutrition department 64 (2.0%), pharmacy department 98 (3.1%), and administration 410 (13.1%). We cannot perform a more detailed departmental analysis. Fourth, the actual response rate was a little low (63.2% [2,078/3,288] in the doctor/nurse staff and 54.3% [1,055/1,943] in the non-doctor/nurse staff). Most of the HCWs felt tired and dull to answer the questionnaire. They did not fill out the questionnaire more than third/fourth. Fifth, sparse effects that may increase the probability of monotone likelihood in this study [OR in Table 3 (night shift) and 4 (burnout) seems inflated in this study] as well as a further limitation (54). Sixth, the cross-sectional studies had Neyman bias because it was confirmed that the questionnaire could not obtain whether the subjects had a burnout in the past or present. However, under such a selection bias, the results are still statistically different, which means that the results still have research value. Finally, there is a need to acknowledge the lack of supporting data on the levels of hormone and pro–inflammation cytokines to further strengthen the explanations of the mechanisms.
In the future, prospective studies involving multiple medical centers are needed to confirm the evidence of this research. In addition, we hope to use the occupational health education and training program to let HCWs understand that a lot of information can be obtained through questionnaire analysis, which will help us improve our policies. More details about working conditions, work–family conflicts, and biochemical biomarker can be added to accumulate more knowledge about the causal relationship and mechanism between work stress, burnout and MetS.
A significant association between burnout and MetS was observed in young female professionals and young doctors/nurses. For the doctor/nurse staff with higher seniority or more night shifts, strategies are needed to prevent burnout and MetS. Agencies need to incorporate stress management into current guidelines to prevent the MetS, especially in the hospital workplace.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Human Research Ethics Committee at Mackay Memorial Hospital (project research number 18MMHISO150). The patients/participants provided their written informed consent to participate in this study.
M-TT participated in the design and conception of the study and its coordination, acquisition of data, carried out statistical analysis, and drafted the manuscript. H-JT participated in the conception and design of the study and reviewed the analysis and manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors thank all the healthcare workers who participated in the study and cooperated in completing the questionnaires.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.854403/full#supplementary-material
1. Wisetborisut A, Angkurawaranon C, Jiraporncharoen W, Uaphanthasath R, Wiwatanadate P. Shift work and burnout among health care workers. Occup Med. (2014) 64:279–86. doi: 10.1093/occmed/kqu009
2. Chou LP, Li CY, Hu SC. Job stress and burnout in hospital employees: comparisons of different medical professions in a regional hospital in Taiwan. BMJ Open. (2014) 4:e004185. doi: 10.1136/bmjopen-2013-004185
3. Yeh WC, Chuang HH, Lu MC, Tzeng IS, Chen JY. Prevalence of metabolic syndrome among employees of a Taiwanese hospital varies according to profession. Medicine. (2018) 97:e11664. doi: 10.1097/MD.0000000000011664
4. Gómez-Urquiza JL, De la Fuente-Solana EI, Albendín-García L, Vargas-Pecino C, Ortega-Campos EM, Cañadas-De la Fuente GA. Prevalence of burnout syndrome in emergency nurses: a meta-analysis. Crit Care Nurse. (2017) 37:e1–9. doi: 10.4037/ccn2017508
5. Schaufeli WB, Leiter MP, Maslach C. Burnout: 35 years of research and practice. Career Dev Int. (2009) 14:204–20. doi: 10.1108/13620430910966406
6. Akkuş Y, Karacan Y, Göker H, Aksu S. Determination of burnout levels of nurses working in stem cell transplantation units in Turkey. Nurs Health Sci. (2010) 12:444–9. doi: 10.1111/j.1442-2018.2010.00557.x
7. Gómez-Urquiza JL, Vargas C, De la Fuente EI, Fernández-Castillo R, Cañadas-De la Fuente GA. Age as a risk factor for burnout syndrome in nursing professionals: a meta-analytic study. Res Nurs Health. (2017) 40:99–110. doi: 10.1002/nur.21774
8. Ahola K, Honkonen T, Virtanen M, Aromaa A, Lönnqvist J. Burnout in relation to age in the adult working population. J Occup Health. (2008) 50:362–5. doi: 10.1539/joh.M8002
9. Chico-Barba G, Jiménez-Limas K, Sánchez-Jiménez B, Sámano R, Rodríguez-Ventura AL, Castillo-Pérez R, et al. Burnout and metabolic syndrome in female nurses: an observational study. Int J Environ Res Public Health. (2019) 16:1993–2004. doi: 10.3390/ijerph16111993
10. das Merces MC, Santana AIC, Lua I, da Silva DAR, Silva DSE, Gomes AMT, et al. Metabolic syndrome among primary health care nursing professionals: a cross-sectional population-based study. Int J Environ Res Public Health. (2019) 16:2686–99. doi: 10.3390/ijerph16152686
11. Tsou MT, Pai TP, Chiang TM, Huang WH, Lin HM, Lee SC. Burnout and metabolic syndrome among different departments of medical center nurses in Taiwan-Cross-sectional study and biomarker research. J Occup Health. (2021) 63:e12188. doi: 10.1002/1348-9585.12188
12. Jacob C. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. New York, NY: Lawrence Erlbaum Associates (1988).
13. Survey of Perception of Safety and Health in the Work Environment in 2016 Taiwan; ILOSH105-M309. Institute of Labor, Occupational Safety, Ministry of Labor (2018).
14. Taiwan Medical Association. Guidelines for Treatment of Hypertension. Available online at: http://www.tainanhealth.org.tw/druginformation/%E9%AB%98%E8%A1%80%E5%A3%93%20%E5%85%A8%E5%9C%8B%E9%86%AB%E5%B8%AB%E8%81%AF%E5%90%88%E6%9C%83.pdf (accessed February 22, 2022).
15. Maslach C, Leiter MP, Schaufeli W. Measuring burnout. In: Cartwright S, Cooper CL, editors. The Oxford Handbook of Organizational Well Being. Oxford: Oxford University Press (2008). p. 86–108. ISBN 9780199211913.
16. Lu L, Lee HM, Shieh TY. Occupational stress, health and occupational burnout among dentists: a study of clinical dentists in Kaohsiung. Res Appl Psychol. (2005) 27:59–80. doi: 10.12809/hkmj166143
17. Lin CC, Liu CS, Lai MM, Li CI, Chen CC, Chang PC, et al. Metabolic syndrome in a Taiwanese metropolitan adult population. BMC Public Health. (2007) 7:239–43. doi: 10.1186/1471-2458-7-239
18. Yeh CJ, Chang HY, Pan WH. Time trend of obesity, the metabolic syndrome and related dietary pattern in Taiwan: from NAHSIT 1993-1996 to NAHSIT 2005-2008. Asia Pac J Clin Nutr. (2011) 20:292–300.
19. Hwang LC, Bai CH, Chen CJ, Chien KL. Gender difference on the development of metabolic syndrome: a population-based study in Taiwan. Eur J Epidemiol. (2007) 22:899–906. doi: 10.1007/s10654-007-9183-5
20. Moran A, Jacobs DR Jr., Steinberger J, Steffen LM, Pankow JS, Hong CP, et al. Changes in insulin resistance and cardiovascular risk during adolescence: establishment of differential risk in males and females. Circulation. (2008) 117:2361–8. doi: 10.1161/CIRCULATIONAHA.107.704569
21. Wei CY, Sun CC, Wei JC, Tai HC, Sun CA, Chung CF, et al. Association between Hyperuricemia and Metabolic Syndrome: an epidemiological study of a labor force population in Taiwan. Biomed Res Int. (2015) 2015:369179. doi: 10.1155/2015/369179
22. Bergmann N, Gyntelberg F, Faber J. The appraisal of chronic stress and the development of the metabolic syndrome: a systematic review of prospective cohort studies. Endocr Connect. (2014) 3:R55–80. doi: 10.1530/EC-14-0031
23. Chandola T, Brunner E, Marmot M. Chronic stress at work and the metabolic syndrome: prospective study. BMJ. (2006) 332:521–5. doi: 10.1136/bmj.38693.435301.80
24. Garbarino S, Magnavita N. Work stress and metabolic syndrome in police officers. A prospective study. PLoS ONE. (2015) 10:e0144318. doi: 10.1371/journal.pone.0144318
25. Soares JJ, Grossi G, Sundin O. Burnout among women: associations with demographic/socio-economic, work, lifestyle and health factors. Arch Womens Ment Health. (2007) 10:61–71. doi: 10.1007/s00737-007-0170-3
26. Sánchez-Jiménez B, Sámano R, Chinchilla-Ochoa D, Morales-Hernández R, Rodríguez-Ventura A. Demographics and psychological factors associated with adiposity in nurses. Int J Environ Res Public Health. (2018) 15:634–41. doi: 10.3390/ijerph15040634
27. Cheng Y, Du CL, Hwang JJ, Chen IS, Chen MF, Su TC. Working hours, sleep duration and the risk of acute coronary heart disease: a case-control study of middle-aged men in Taiwan. Int J Cardiol. (2014) 171:419–22. doi: 10.1016/j.ijcard.2013.12.035
28. Kobayashi T, Suzuki E, Takao S, Doi H. Long working hours and metabolic syndrome among Japanese men: a cross-sectional study. BMC Public Health. (2012) 12:395–403. doi: 10.1186/1471-2458-12-395
29. Copertaro A, Bracci M, Barbaresi M, Santarelli L. Assessment of cardiovascular risk in shift healthcare workers. Eur J Cardiovasc Prev Rehabil. (2008) 15:224–9. doi: 10.1097/HJR.0b013e3282f364c0
30. Ha M, Park J. Shiftwork and metabolic risk factors of cardiovascular disease. J Occup Health. (2005) 47:89–95. doi: 10.1539/joh.47.89
31. Biggi N, Consonni D, Galluzzo V, Sogliani M, Costa G. Metabolic syndrome in permanent night workers. Chronobiol Int. (2008) 25:443–54. doi: 10.1080/07420520802114193
32. Brum MC, Filho FF, Schnorr CC, Bottega GB, Rodrigues TC. Shift work and its association with metabolic disorders. Diabetol Metab Syndr. (2015) 7:45. doi: 10.1186/s13098-015-0041-4
33. Lin YC, Hsiao TJ, Chen PC. Persistent rotating shift-work exposure accelerates development of metabolic syndrome among middle-aged female employees: a five-year follow-up. Chronobiol Int. (2009) 26:740–55. doi: 10.1080/07420520902929029
34. Pietroiusti A, Neri A, Somma G, Coppeta L, Iavicoli I, Bergamaschi A, et al. Incidence of metabolic syndrome among night-shift healthcare workers. Occup Environ Med. (2010) 67:54–7. doi: 10.1136/oem.2009.046797
35. Kang MG, Koh SB, Cha BS, Park JK, Woo JM, Chang SJ. Association between job stress on heart rate variability and metabolic syndrome in shipyard male workers. Yonsei Med J. (2004) 45:838–46. doi: 10.3349/ymj.2004.45.5.838
36. Wang LJ, Chen CK, Hsu SC, Lee SY, Wang CS, Yeh WY. Active job, healthy job? Occupational stress and depression among hospital physicians in Taiwan. Ind Health. (2011) 49:173–84. doi: 10.2486/indhealth.MS1209
37. Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. (2012) 172:1377–85. doi: 10.1001/archinternmed.2012.3199
38. Koren D, Dumin M, Gozal D. Role of sleep quality in the metabolic syndrome. Diabetes Metab Syndr Obes. (2016) 9:281–310. doi: 10.2147/DMSO.S95120
39. Iftikhar IH, Donley MA, Mindel J, Pleister A, Soriano S, Magalang UJ. Sleep duration and metabolic syndrome. An updated dose-risk metaanalysis. Ann Am Thorac Soc. (2015) 12:1364–72. doi: 10.1513/AnnalsATS.201504-190OC
40. Deneva T, Ianakiev Y, Keskinova D. Burnout Syndrome in physicians-psychological assessment and biomarker research. Medicina. (2019) 55:209. doi: 10.3390/medicina55050209
41. Smiley A, Wolter S, Nissan D. Mechanisms of association of sleep and metabolic syndrome. J Med Clin Res Rev. (2019) 3:1–9. doi: 10.33425/2639-944X.1089
42. Chiang JK. Short duration of sleep is associated with elevated high-sensitivity C-reactive protein level in Taiwanese adults: a cross-sectional study. J Clin Sleep Med. (2014) 10:743–9. doi: 10.5664/jcsm.3862
43. Toker S, Shirom A, Shapira I, Berliner S, Melamed S. The association between burnout, depression, anxiety, and inflammation biomarkers: C-reactive protein and fibrinogen in men and women. J Occup Health Psychol. (2005) 10:344–62. doi: 10.1037/1076-8998.10.4.344
44. Basei Rossa CE, Avancini Caramori PR, Manfroi WC. Metabolic syndrome in workers in a university hospital. Rev Port Cardiol. (2012) 31:629–36. doi: 10.1016/j.repce.2012.07.009
45. Marchand A, Blanc ME, Beauregard N. Do age and gender contribute to workers' burnout symptoms? Occup Med. (2018) 68:405–11. doi: 10.1093/occmed/kqy088
46. Bekker MHJ, Croon MA, Bressers B. Childcare involvement, job characteristics, gender and work attitudes as predictors of emotional exhaustion and sickness absence. Work Stress. (2005) 19:221–37. doi: 10.1080/02678370500286095
47. Lim N, Kim EK, Kim H, Yang E, Lee SM. Individual and work-related factors influencing burnout of mental health professionals: a meta-analysis. J Employment Couns. (2010) 47:86–96. doi: 10.1002/j.2161-1920.2010.tb00093.x
48. Ahola K, Honkonen T, Isometsä E, Kalimo R, Nykyri E, Koskinen S, et al. Burnout in the general population. Results from the Finnish Health 2000 Study. Soc Psychiatry Psychiatr Epidemiol. (2006) 41:11–7. doi: 10.1007/s00127-005-0011-5
49. Matthews RA, Bulger CA, Barnes-Farrell JL. Work social supports, role stressors, and work-family conflict: the moderating effect of age. J Vocat Behav. (2010) 76:78–90. doi: 10.1016/j.jvb.2009.06.011
50. Theorell T, Hammarström A, Gustafsson PE, Magnusson Hanson L, Janlert U, Westerlund H. Job strain and depressive symptoms in men and women: a prospective study of the working population in Sweden. J Epidemiol Community Health. (2014) 68:78–82. doi: 10.1136/jech-2012-202294
51. Byron Kris. A meta-analytic review of work-family conflict and its antecedents. J Vocat Behav. (2005) 67:169–98. doi: 10.1016/j.jvb.2004.08.009
52. Cinamon RG, Rich Y. Gender differences in the importance of work and family roles: implications for work–family conflict. Sex Roles. (2002) 47:531–41. doi: 10.1023/A:1022021804846
53. Michel JS, Kotrba LM, Mitchelson JK, Clark MA, Baltes BB. Antecedents of work–family conflict: a meta-analytic review. J Organ Behav. (2011) 32:689–725. doi: 10.1002/job.695
Keywords: health care workers, burnout, metabolic syndrome, Taiwan, sex
Citation: Tsai H-J and Tsou M-T (2022) Age, Sex, and Profession Difference Among Health Care Workers With Burnout and Metabolic Syndrome in Taiwan Tertiary Hospital—A Cross-Section Study. Front. Med. 9:854403. doi: 10.3389/fmed.2022.854403
Received: 13 January 2022; Accepted: 14 March 2022;
Published: 14 April 2022.
Edited by:
Mohamed Farouk Allam, Ain Shams University, EgyptReviewed by:
Dian Puspita Sari, Faculty of Medicine University of Mataram, IndonesiaCopyright © 2022 Tsai and Tsou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Meng-Ting Tsou, bXR0c291QGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.