
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Med. , 24 March 2022
Sec. Gastroenterology
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.853138
This article is part of the Research Topic Full-Course Management of Cirrhotic Portal Hypertension View all 6 articles
Cavernous transformation of the portal vein (CTPV) is a sequela of extrahepatic and/or intrahepatic portal vein obstruction caused by a combination of local and risk factors. It was ever taken as a relatively rare disease due to its scant literature, which was mainly based on clinical series and case reports. CTPV often manifests as gastroesophageal variceal bleeding, splenomegaly, and portal biliopathy after the long-term insidious presentation. It is unable for CTPV to be recanalized with anticoagulation because it is a complete obstruction of the mesentericoportal axis. Endoscopic therapy is mainly used for temporary hemostasis in acute variceal bleeding. Meso-Rex shunting characterized by portal-flow-preserving shunts has been widely performed in children with CTPV. The multitude of complications associated with CTPV in adults can be effectively addressed by various interventional vascular therapies. With the ubiquity of radiological examinations, optimal treatment for patients with CTPV becomes important. Multivisceral transplantation, such as liver-small intestinal transplantation, may be lifesaving and should be considered for patients with diffuse mesenteric venous thrombosis.
Cavernous transformation of the portal vein (CTPV) is usually secondary to long-standing portal vein thrombosis (PVT) or portal vein obstruction. As a sequela of portal vein obstruction, especially complete extrahepatic portal vein obstruction (EHPVO), fibroblasts transform the clot into a firm, collagenous plug in, which tortuous venous channels develop. On this basis, portal hypertension caused by PVT may promote the formation of periportal or intrahepatic venous collateral circulation, resulting in CTPV, bypassing extrahepatic portal venous occlusion over time, and interrupting portal inflow (1–5). CTPV may occur as early as 6–20 days after EHPVO, with an average time of approximately 5 weeks (3, 5, 6). It was first reported in 1869 by Balfour and Stewart and is also referred to as a portal cavernoma due to the sponge-like appearance of the portal vein (7).
Cavernous transformation of the portal vein may remain insidious for long-term presentation. It often manifests as gastroesophageal variceal bleeding, splenomegaly, and thrombocytopenia. The biliary tree may undergo morphological and functional changes due to CTPV, resulting in obstructive jaundice. It has recently been termed “portal biliopathy” (8). The mortality rate due to variceal hemorrhage is 5%, and the overall mortality rate is 10% in both adults and children with CTPV (9, 10). Even worse, more than 43% of obstetric patients with non-cirrhotic prehepatic portal hypertension and the development of esophageal varices will suffer significant variceal bleeding during pregnancy. This potentially catastrophic complication is associated with a 33% perinatal mortality rate (11). Recently, it was suggested that the presence of ascites may be of great importance to predict the incidence of death in patients with CTPV, mainly attributed to its close correlation with the deterioration of liver function (12–14). CTPV and chronic PVT remain a challenge at the time of transplant. They are relative contraindications to liver transplantation at many centers because the non-physiological portal flow may increase perioperative and postoperative risks associated with surgical techniques.
The hemodynamics of the portal venous system are characterized by low pressure, slow flow, and high volume. Similar to other venous thromboses, the formation of PVT is also multifactorial due to reduced blood flow, endothelial injury, and hypercoagulability. PVT is caused by a combination of local and risk factors (Figure 1).
The causes of CTPV and acute PVT in adults are similar. The commonly affected population may be divided into cirrhotic and non-cirrhotic patients. The composition ratio of cirrhotic and non-cirrhotic cases varies by region. A study of 254 autopsies from Sweden reported that 28% of PVT cases were cirrhotic, whereas non-cirrhotic PVT accounted for most of the rest (15). PVT occurs in ~20% of cirrhotic patients, who are a great body of inpatients in China. The development of cirrhotic PVT is closely associated with static portal blood flow due to portal hypertension and endothelial injury due to intestinal infection and therapeutic inflammation. In non-cirrhotic patients, a systemic hypercoagulable state is often implicated in PVT (Figure 1). The occurrence of vascular malformation in children suggests that a congenital defect is often a contributing factor, such as prior umbilical cannulation and infection. Inherited and acquired prothrombotic disorders (e.g., latent myeloproliferative disorder, protein C or protein S deficiency, and antiphospholipid syndrome) and thrombotic stimuli, such as pregnancy or oral contraceptives, intra-abdominal infection, and surgical procedures, have been observed in adults, while repeated abdominal infections, sepsis, abdominal invasive procedures, trauma, and congenital anomalies, with or without a prothrombotic state, have been alleged to lead to CTPV in children (16–19). After the exclusion of the aforementioned causes, the etiology of EHPVO remains obscure in up to 50% of patients (20).
The prevalence of PVT in the general population ranges from 0.7 to 1/105 (21). It is increased ~1,000-fold in cirrhotic patients, with a range of 0.6%−50%, increasing proportionally with liver cirrhosis severity (22, 23). Epidemiological data of non-cirrhotic PVT in the general population are limited by its infrequency. The prevalence of EHPVO was estimated to be as high as 1.0% in an autopsy study in Sweden (15). However, it was much lower (3.7 per 100,000 population) in another Swedish study based on hospital discharge diagnoses (21), suggesting that EHPVO commonly develops at a late stage of some diseases. CTPV among adults is quite rare, with an incidence of 15.6% among EHPVO (24).
The concept of CTPV as a relatively rare disease is mainly based on clinical series and case reports. The literature on CTPV is scant. Therefore, there is considerable heterogeneity in its treatment. Accordingly, the current therapies are mainly extrapolated from cohort studies and/or based on clinician expertise. Optimal treatment for patients with CTPV becomes important with increasing identification by imaging modalities.
Anticoagulation is the cornerstone of treatment for acute PVT without malignancy and should be initiated at diagnosis. Anticoagulant treatment must be considered in cirrhotic patients with PVT following the implementation of adequate prophylaxis for gastrointestinal bleeding (25). However, the main portal vein of CTPV is commonly considered to be unable to be recanalized with anticoagulation because it is a complete obstruction of the mesentericoportal axis. There is only one case reported in which the portal cavernoma was reversed by long-term (5 years) anticoagulation (26). Anticoagulation may lessen the degree of bile duct obstruction in certain patients with CTPV with cholangiopathy, probably by maintaining the patency of periportal or intrahepatic venous collaterals and reducing the compression of the bile duct (27). It is not beneficial for children to take long-term anticoagulation since the procoagulant state is an occasional cause of chronic non-cirrhotic EHPVO (28, 29).
Endoscopic therapy cannot reduce portal hypertension and is mainly used for temporary hemostasis in acute variceal bleeding. Endoscopic variceal ligation (EVL) is recommended for the management of active esophageal variceal bleeding (12, 30, 31). When acute bleeding from isolated gastric varices and gastroesophageal varices type 2 (GOV2) extends beyond the cardia, sclerotherapy or endoscopic therapy with tissue adhesive should be taken into account. Either ligation or endoscopic therapy tissue adhesive can be used for GOV1 bleeding. Primary prophylaxis with endoscopic treatment has been recommended for patients with cirrhosis with EHPVO by the Baveno VI consensus (31). Recently, endoscopic ultrasound-guided coil (EUS-coil) therapy has emerged as a promising option due to its therapeutic superiority over endoscopic glue injection. It is believed that EUS-coil therapy is the next intervention for primary and secondary hemostases of gastric variceal bleeding and will result in a paradigm shift (32, 33).
Multiple endoscopic procedures may become a local risk for PVT due to traumatic inflammation in the portal system. When portal-systemic collaterals are blocked by endoscopic procedures without being diverted, the increased portal pressure carries an increased risk of biliary complications, mostly from the suppression of periportal collateral vessels. Thus, portal decompression should be performed early, even if the risk of bleeding is not high (34–37).
Gastroesophageal devascularization between the portal and azygos veins alone without a shunt has been less performed recently due to its higher rebleeding rate and lower 5-year survival rate (38, 39). There are several surgical approaches by which portacaval shunts can be established to decompress portal hypertension (40–42). The experience from adults indicated that non-selective surgical shunts such as side-to-side splenorenal or meso-caval shunts can totally divert the portal flow toward the systemic circulation but apparently potentiate ischemia-perfusion to the liver at the same time (40, 43). In this regard, non-selective shunts and their derivative techniques are taken into account only in patients with refractory life-threatening bleeding (44–46). Selective shunts, such as the distal splenorenal shunt developed by Warren et al., have been considered as effective as non-selective shunts in controlling variceal bleeding. It preserves a portion of portal perfusion to the liver and is better in preventing portosystemic encephalopathy (40, 47). However, widespread use of distal splenorenal shunts has been limited in terms of technical requirements, particularly in adults (38).
Meso-Rex shunting is a recently established surgical technique. The patient's internal jugular vein is used as an autograft by which the superior mesenteric vein blood flow is diverted into the umbilical portion of the left portal vein. This technique sufficiently restores a substantial portion of physiological portal blood flow to the liver and avoids the long-term adverse consequences of portosystemic shunting, such as liver atrophy and growth retardation (16, 40, 45). This portal-flow-preserving shunt has been widely performed in children with CTPV. The bypass patency rates might reach 100% 1 year after the operation and remained at 78% during the 10-year follow-up. Of the 490 reported cases, only three deaths occurred (Table 1) (40, 45, 48–65).
Later, several modifications of meso-Rex bypass using alternate sources of venous inflow and graft conduits in children when standard meso-Rex shunting cannot be achieved (66, 67). It has been recommended by the Baveno consensus that meso-Rex bypass, the most physiological shunting and the only “curative surgery,” should be performed for patients in the early stage of EHPVO (31, 44, 68, 69). However, the controversy concerning the legitimacy of its utilization in an asymptomatic child is still unresolved. Available data show an inverse correlation between the restoration of appropriate portal flow to the liver following meso-Rex shunt and the age of the patient (49, 69). It has been proposed that the assessment of surgical feasibility should be performed in all children with CTPV in a more prophylactic manner (70–72), while in fact, many medical centers routinely defer preemptive meso-Rex bypass until intractable and refractory symptoms are established.
Inspired by the success of meso-Rex bypass in children with CTPV, a modified meso-Rex bypass (splenic vein to cystic part of the portal vein) was successfully performed in an adult patient after liver transplantation (73). Recently, a novel meso-Rex bypass with umbilical vein recanalization and intraoperative stenting was reported (58). It may reduce the risk of intravascular thrombosis and bypass vessel occlusion compared with traditional meso-Rex shunting. The limited data on surgical shunting in adults with CTPV will encourage more studies for adult patients.
Cavernous transformation of the portal vein was once considered an absolute contraindication for liver transplantation due to unsatisfactory portal flow to the graft (74, 75). However, incremental refinements of the surgical technique have allowed recipients with CTPV to undergo liver transplantation using a prominent collateral vein, dilated coronary vein, interposition graft, portal vein arterialization, or some anastomotic methods, including renoportal or cavoportal anastomosis, for inflow reconstruction. Occasionally, multivisceral transplantation, such as liver-small intestinal transplantation, may be lifesaving and should be considered for patients with diffuse mesenteric venous thrombosis (74, 76–83).
Surgical challenges have promoted the application of interventional technology in patients with CTPV. The multitude of complications due to CTPV can be effectively addressed by various interventional vascular therapies.
Cavernous transformation of the portal vein has previously been considered contraindicated for transjugular intrahepatic portosystemic shunt (TIPS) due to technical difficulties and its vital complications. However, it has been feasible for modified TIPS (mTIPS) creation in some patients with CTPV since 2006 (84). The procedure has been modified and evolved to include transjugular, transhepatic, and transsplenic accesses to assist with portal vein recanalization (Figure 2). Rates of technical success of recanalization have been reported in a range of 75–100% in incomplete occluded portal veins (85). Technical success is associated with the degree of occlusion of the main portal vein. Cavernous transformation may increase the technical difficulty. There are two strategies for intrahepatic portosystemic shunt placement, namely, (1) portal recanalization and conventional implantation of the stent to create intrahepatic portosystemic shunt and (2) insertion of the stent between the hepatic vein and a periportal collateral vessel without portal recanalization for whom recanalization of the portal vein is not possible but there are dilated veins of a cavernous transformation (86–92). In clinical practice, the second strategy is also challenged by the injury of surrounding collaterals (93, 94). Intraparenchymal injection of CO2 or wedged hepatic venous portography may be helpful to guide the intraparenchymal needle toward the target intrahepatic portal tree (93, 95). The existence of both a high- and a low-pressure portal venous network in patients with CTPV should be considered. Therefore, mTIPS creation requires careful selection of an intrahepatic portal vein with high pressure to achieve adequate portal decompression and improve clinical success (96). However, it is usually difficult to obtain an accurate hepatic venous pressure gradient (HVPG) in patients with portal hypertension due to the presence of intrahepatic venous-venous shunts (97). Thus, direct measurement of portal pressure and calculation of portosystemic pressure gradient (PPG) are more meaningful for the establishment of portosystemic shunt than HVPG. To reconstruct a physiological hepatopetal flow for patients with severe spontaneous portal-systemic shunts (SPSS), it is necessary to obliterate SPSS, such as balloon-occluded retrograde transvenous obliteration (BRTO), during mTIPS placement (69, 98).
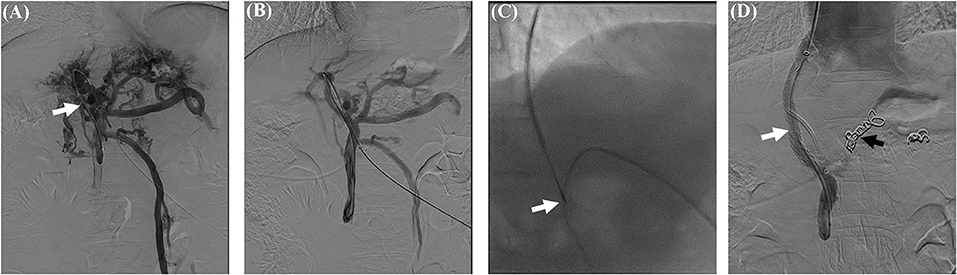
Figure 2. PVR-TIPS creation in a patient with CTPV. 53 years/M, CTPV with cirrhosis. (A) Percutaneous transhepatic portography revealed extrahepatic portal obstruction and collateral vein formation (white arrow). (B) Percutaneous portography after portal vein recanalization (PVR) by an 8 mm × 60 mm balloon catheter. (C) A catheter was placed in the portal vein as a marker for TIPS puncture (white arrow). (D) The portosystemic shunt was created with a covered stent (white arrow) after the embolization of the coronary vein with coils (black arrow). CTPV, cavernous transformation of the portal vein; PVR, portal vein recanalization; TIPS, transjugular intrahepatic portosystemic shunt.
Performance of portal vein recanalization (PVR) or its combination with TIPS was initially aimed at optimizing the transplant candidacy of patients with PVT or CTPV. Currently, the placement of intrahepatic portosystemic shunts has become an alternative treatment for PVT and CTPV, which is not a distinct contraindication to TIPS procedures. It has been considered salvage therapy when endoscopic treatment is unsuccessful in patients with chronic PVT and cavernous transformation (96). Although there are many technical difficulties in creating mTIPS, it is still a major procedure for chronic PVT or CTPV in China due to many cirrhotic patients.
Theoretically, the mTIPS technique focuses on addressing intrahepatic resistance and should be beneficial to cirrhotic CTPV. EHPVO alone is the characteristic of non-cirrhotic patients with CTPV. Insertion of portal vein stent (PVS) alone may alleviate extrahepatic portal hypertension and prevent rebleeding effectively only by recanalization of the obstructed portal vein, venoplasty, and stenting (96). PVS intervention may be more suitable for non-cirrhotic patients than mTIPS because it preserves adequate physiological blood inflow to the liver. However, it is reasonable to be aware of the possibility of catheterizing the portal vein remnant and the patency of the major splanchnic vessels by Doppler ultrasound and CT (99). A new classification for CTPV proposed by Marot et al. was formulated with the aim of selecting which patients could be considered for portal angioplasty. Intrahepatic involvement with extension to the origin of the hepatic segmental branches and distal branches was ultimately associated with technical failure or with early stent thrombosis due to insufficient blood outflow. Therefore, PVR alone should not be considered in these patients (100). Most of the patients (90%) had considerably improved portal hypertension-related symptoms. This procedure is known to be an effective treatment for PV obstruction after liver transplantation and from primary malignancy (101–105). A retrospective study with 42 cases with PV obstruction following non-transplant hepatobiliary or pancreatic surgery considered that portomesenteric venoplasty and stent placement are safe with a high rate of technical success if performed before chronic occlusion (102). The long-term stent patency in patients who underwent PVS varied with different ages, causes, and techniques they accepted (Table 2) (99–103, 105–110).
Similar to mTIPS, several routes for gaining access to the portal system are emerging in PVS intervention, even though the portal vein has been obliterated and becomes a fibrotic cord. These multimodality cutting-edge therapeutic approaches, which encompass transjugular, transhepatic-intrahepatic portal vein branch using US guidance, transsplenic-US guidance, trans-ileocolic-mini-laparotomy (i.e., hybrid approach), as well as the trans-recanalized paraumbilical vein either alone or in combination, push the development of PVS (Figure 3) (93, 99, 111–115). Transhepatic-intrahepatic portal vein branch using US guidance has been by far the most common way of gaining access to perform PVS (116). Direct access to the left portal vein risks Rex's recess (116); this option should consequently be weighed before meso-Rex bypass. For patients with atresia of the portal vein, which cannot be recanalized by the endovascular (the main portal vein) approach, a stent shunt between the intrahepatic portal branch and the large collateral vessel should be taken into consideration (96). Currently, there is no clear evidence supporting the use of either of these approaches over the others. It is also worth noting that the preservation of the splenic-mesenteric confluence and the left portal vein should be considered mandatory for patients to avoid compromising the possibility of meso-Rex shunting and liver transplantation (99). Moreover, PVS in non-cirrhotic CTPV may avoid the common complications related to mTIPS, including chronic recurrent encephalopathy, liver failure, and congestive cardiac failure (93).
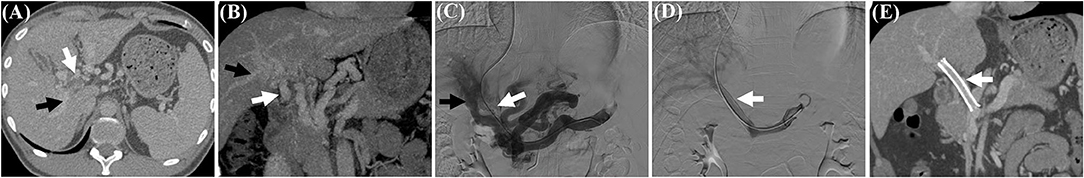
Figure 3. PVS in a patient with CTPV. 35 years/M, CTPV without cirrhosis. (A) and (B) CT images and reconstruction revealed occlusion of main portal vein and cavernoma (white arrow) and visible branches of th portal vein (black arrow). (C) Transjugular portography showed complete occlusion of the portal vein (white arrow) and collateral vein which is not directly connected with intrahepatic portal branches (black arrow). (D) An 8 mm × 60 mm bare stent was inserted into the main portal vein (white arrow), and the intrahepatic portal vein was clearly shown by portography. (E) CT reconstruction showed a patent stent (white arrow) in the main portal vein 1 year after the procedure. PVS, portal vein stenting; CTPV, cavernous transformation of the portal vein.
Extrinsic compression of the bile duct by collaterals and/or ischemic damage due to altered biliary vascularization has been implicated in the pathogenesis of portal cavernoma biliopathy (117). Invasive treatment strategies of portal cholangiopathy should only be performed in patients with clinical symptoms (accounting for ~5–38% of abnormalities seen by magnetic resonance cholangiopancreatography) in view of high bleeding risk, even in the presence of obvious stenosis on imaging (28, 117, 118).
Definitive management usually requires combined approaches aimed at treating both portal hypertension and biliary stenosis, including endoscopic bile duct dilation/stenting, stone extraction, cholecystectomy, bilioenteric anastomosis, and the portal decompression strategies mentioned above (117, 119, 120). In our previous study, we successfully treated a patient with CTPV with intractable biliary obstruction following TIPS placement using a novel magnet-assisted endoscopic biliary-duodenal anastomosis (121), which seems to be a promising solution for portal biliopathy under certain conditions, particularly in patients with a perceived increased risk of conventional bilioenteric anastomosis.
Patients with CTPV should be treated in regional central hospital with strong surgical and interventional teams. Meso-Rex bypass is recommended for children with CTPV. Incremental refinements of the interventional techniques, such as mTIPS creation and PVS, can greatly benefit adult patients with CTPV by reducing the need for liver transplantation or transforming contraindications of liver transplantation into indications. The optimal treatment for patients is a personal interventional strategy on the basis of their heterogeneity in mesentericoportal obstruction.
CT contributed to conception and design of the study. ZH analyzed the literature and drew the tables. BW wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
This study was supported by the National Natural Science Fund of China (82170625, U1702281), the National Key R&D Program of China (2017YFA0205404), and the 135 projects for disciplines of excellence of West China Hospital, Sichuan University (ZYGD18004).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Takahashi T, Kakita A, Inagi E, Furuta K, Izumika H, Yoshida M, et al. Cavernous transformation of the portal vein coinciding with early gastric cancer and cholelithiasis. Surg Today. (1994) 24:840–3. doi: 10.1007/bf01636319
2. Qi X, Han G, Yin Z, He C, Guo W, Niu J, et al. Cavernous vessels around a patent portal trunk in the liver hilum. Abdom Imaging. (2012) 37:422–30. doi: 10.1007/s00261-011-9779-9
3. Ma J, Yan Z, Luo J, Liu Q, Wang J, Qiu S. Rational classification of portal vein thrombosis and its clinical significance. PloS ONE. (2014) 9:e112501. doi: 10.1371/journal.pone.0112501
4. Luca A, Caruso S, Milazzo M, Marrone G, Mamone G, Crino F, et al. Natural course of extrahepatic non-malignant partial portal vein thrombosis in patients with cirrhosis. Radiology. (2012) 265:124–32. doi: 10.1148/radiol.12112236
5. Vaish AK, Kumar N, Jain N, Agarwal A. Cavernous transformation of portal vein a missed cause of extrahepatic portal hypertension. BMJ Case Reports. (2012) 2012:5331. doi: 10.1136/bcr.12.2011.5331
6. Ide T, Ohno Y, Nakanuma Y, Kanematsu T. Early development of cavernomatous vasculatures in portal venous thrombosis: morphometric kinetics in rabbit model. Hepatol Res. (2003) 27:136–42. doi: 10.1016/s1386-6346(03)00208-0
7. Balfour GW, Stewart TG. Case of enlarged spleen complicated with ascites, both depending upon varicose dilatation and thrombosis of the portal vein. Edinb Med J. (1869) 14:589–98.
8. Harmanci O, Bayraktar Y. How can portal vein cavernous transformation cause chronic incomplete biliary obstruction? World J Gastroenterol. (2012) 18:3375–8. doi: 10.3748/wjg.v18.i26.3375
9. Klopfenstein KJ, Grossman NJ, Fishbein M, Ruymann FB. Cavernous transformation of the portal vein: a cause of thrombocytopenia and splenomegaly. Clinical Pediatrics. (2000) 39:727–30. doi: 10.1177/000992280003901209
10. Cohen J, Edelman RR, Chopra S. Portal vein thrombosis: a review. Am J Med. (1992) 92:173–82. doi: 10.1016/0002-9343(92)90109-o
11. Wax JR, Pinette MG, Cartin A, Winn SS, Blackstone J. Cavernous transformation of the portal vein complicating pregnancy. Obstetrics Gynecol. (2006) 108:782–4. doi: 10.1097/01.AOG.0000204872.46203.bf
12. DeLeve LD Valla DC Garcia-Tsao G American association for the study liver D. Vascular disorders of the liver. Hepatology. (2009) 49:1729–64. doi: 10.1002/hep.22772
13. Qi XS, Bai M, He CY, Yin ZX, Guo WG, Niu J, et al. Prognostic factors in non-malignant and non-cirrhotic patients with portal cavernoma: an 8-year retrospective single-center study. World J Gastroenterol. (2013) 19:7447–54. doi: 10.3748/wjg.v19.i42.7447
14. Simonetto DA, Singal AK, Garcia-Tsao G, Caldwell SH, Ahn J, Kamath PS. ACG Clinical guideline: disorders of the hepatic and mesenteric circulation. Am J Gastroenterol. (2020) 115:18–40. doi: 10.14309/ajg.0000000000000486
15. Ogren M, Bergqvist D, Bjorck M, Acosta S, Eriksson H, Sternby NH. Portal vein thrombosis: prevalence, patient characteristics and lifetime risk: a population study based on 23,796 consecutive autopsies. World J Gastroenterol. (2006) 12:211–9. doi: 10.3748/wjg.v12.i13.2115
16. Sarin SK, Sollano JD, Chawla YK, Amarapurkar D, Hamid S, Hashizume M, et al. Consensus on extrahepatic portal vein obstruction. Liver international. (2006) 26:512–9. doi: 10.1111/j.1478-3231.2006.01269.x
17. Kobe A, Puippe G, Mullhaupt B, Pfammatter T. Recanalization of chronic non-cirrhotic, non-malignant splanchnic thromboses is feasible: a transsplenic assisted patient-tailored approach. J Vasc Interv Radiol. (2021) 32:1377–85. doi: 10.1016/j.jvir.2021.05.012
18. Sigalet DL, Mayer S, Blanchard H. Portal venous decompression with H-type mesocaval shunt using autologous vein graft: a North American experience. J Pediatr Surg. (2001) 36:91–6. doi: 10.1053/jpsu.2001.20018
19. Vasilescu C, Stanciulea O, Popa M, Colita A, Arion C. Subtotal laparoscopic splenectomy and esophagogastric devascularization for the thrombocytopenia because of portal cavernoma–case report. J Pediatr Surg. (2008) 43:1373–5. doi: 10.1016/j.jpedsurg.2008.02.005
20. Mörk H, Weber P, Schmidt H, Goerig RM, Scheurlen M. Cavernous transformation of the portal vein associated with common bile duct strictures: report of two cases. Gastrointest Endosc. (1998) 47:79–83. doi: 10.1016/s0016-5107(98)70305-0
21. Rajani R, Bjornsson E, Bergquist A, Danielsson A, Gustavsson A, Grip O, et al. The epidemiology and clinical features of portal vein thrombosis: a multicentre study. Aliment Pharmacol Ther. (2010) 32:1154–62. doi: 10.1111/j.1365-2036.2010.04454.x
22. Tsochatzis EA, Senzolo M, Germani G, Gatt A, Burroughs AK. Systematic review: portal vein thrombosis in cirrhosis. Aliment Pharmacol Ther. (2010) 31:366–74. doi: 10.1111/j.1365-2036.2009.04182.x
23. Lisman T, Violi F. Cirrhosis as a risk factor for venous thrombosis. Thromb Haemost. (2017) 117:3–5. doi: 10.1160/TH16-10-0782
24. Shukla A, Gupte A, Karvir V, Dhore P, Bhatia S. Long term outcomes of patients with significant biliary obstruction due to portal cavernoma cholangiopathy and extra-hepatic portal vein obstruction (EHPVO) with no shuntable veins. J Clin Exp Hepatol. (2017) 7:328–33. doi: 10.1016/j.jceh.2017.04.003
25. European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol. (2018) 69:406–60. doi: 10.1016/j.jhep.2018.03.024
26. Silva-Junior G, Turon F, Hernandez-Gea V, Darnell A, Garcia-Criado A, Garcia-Pagan JC. Unexpected disappearance of portal cavernoma on long-term anticoagulation. J Hepatol. (2014) 61:446–8. doi: 10.1016/j.jhep.2014.04.002
27. Shen Y, Yao Y, Wang Y, Wang L, Zou X. Obstructive jaundice caused by postsplenectomy cavernous transformation of the portal vein mimicking cholangiocarcinoma. Gastrointest Endosc. (2020) 92:786–7. doi: 10.1016/j.gie.2020.04.018
28. Elkrief L, Houssel-Debry P, Ackermann O, Franchi-Abella S, Branchereau S, Valla D, et al. Portal cavernoma or chronic non-cirrhotic extrahepatic portal vein obstruction. Clin Res Hepatol Ggastroenterol. (2020) 44:491–6. doi: 10.1016/j.clinre.2020.03.016
29. Abd El-Hamid N, Taylor RM, Marinello D, Mufti GJ, Patel R, Mieli-Vergani G, et al. Aetiology and management of extrahepatic portal vein obstruction in children: King's college hospital experience. J Pediatr Gastroenterol Nutr. (2008) 47:630–4. doi: 10.1097/MPG.0b013e31817b6eea
30. Al-Qurashi FO, Aladsani AA, Al Qanea FK, Faisal SY. Portal Hypertension of a delayed onset following liver abscesses in a 12-month-old infant: a case report and review of the literature. Pediatr Gastroenterol Hepatol Nutr. (2019) 22:400–6. doi: 10.5223/pghn.2019.22.4.400
31. de Franchis R, Baveno VIF. Expanding consensus in portal hypertension: report of the baveno VI consensus workshop: stratifying risk and individualizing care for portal hypertension. J Hepatol. (2015) 63:743–52. doi: 10.1016/j.jhep.2015.05.022
32. Bazarbashi AN, Li M, Ryou M. Letter to the editor: endoscopic ultrasound-guided coil therapy for secondary prevention after gastric variceal bleeding: a promising alternative. Hepatology. (2021) 74:2914. doi: 10.1002/hep.31997
33. Bazarbashi AN, Wang TJ, Jirapinyo P, Thompson CC, Ryou M. Endoscopic ultrasound-guided coil embolization with absorbable gelatin sponge appears superior to traditional cyanoacrylate injection for the treatment of gastric varices. Clin Transl Gastroenterol. (2020) 11:e00175. doi: 10.14309/ctg.0000000000000175
34. Gauthier-Villars M, Franchi S, Gauthier F, Fabre M, Pariente D, Bernard O. Cholestasis in children with portal vein obstruction. J Pediatrics. (2005) 146:568–73. doi: 10.1016/j.jpeds.2004.12.025
35. Choudhuri G, Tandon RK, Nundy S, Misra NK. Common bile duct obstruction by portal cavernoma. Dig Dis Sci. (1988) 33:1626–8. doi: 10.1007/BF01535956
36. Chaudhary A, Dhar P, Sarin SK, Sachdev A, Agarwal AK, Vij JC, et al. Bile duct obstruction due to portal biliopathy in extrahepatic portal hypertension: surgical management. Br J Surg. (1998) 85:326–9. doi: 10.1046/j.1365-2168.1998.00591.x
37. Ouchi K, Tominaga T, Unno M, Matsuno S. Obstructive jaundice associated with extrahepatic portal vein obstruction: report of two cases. Surg Today. (1993) 23:737–41. doi: 10.1007/BF00311715
38. Zhang H, Zhang N, Li M, Jin W, Pan S. Surgical treatment of portal vein cavernous transformation. World J Surg. (2004) 28:708–11. doi: 10.1007/s00268-004-7265-z
39. Belli L, Puttini M, Marni A. Extrahepatic portal obstruction: Clinical experience and surgical treatment in 105 patients. J Cardiovasc Surg. (1980) 21:439–48.
40. Elnaggar AS, Griesemer AD, Bentley-Hibbert S, Brown RS Jr, Martinez M, Lobritto SJ, et al. Liver atrophy and regeneration in non-cirrhotic portal vein thrombosis: effect of surgical shunts. Liver Transpl. (2018) 24:881–7. doi: 10.1002/lt.25024
41. Orloff MJ, Orloff MS, Girard B, Orloff SL. Bleeding esophagogastric varices from extrahepatic portal hypertension: 40 years' experience with portal-systemic shunt. J Am Coll Surg. (2002) 194:717–28;. doi: 10.1016/s1072-7515(02)01170-5
42. Hau HM, Fellmer P, Schoenberg MB, Schmelzle M, Morgul MH, Krenzien F, et al. The collateral caval shunt as an alternative to classical shunt procedures in patients with recurrent duodenal varices and extrahepatic portal vein thrombosis. Eur J Med Res. (2014) 19:36. doi: 10.1186/2047-783X-19-36
43. Orloff MJ. Fifty-three years' experience with randomized clinical trials of emergency portacaval shunt for bleeding esophageal varices in Cirrhosis: 1958-2011. JAMA surgery. (2014) 149:155–69. doi: 10.1001/jamasurg.2013.4045
44. Chocarro G, Junco PT, Dominguez E, Amesty MV, Nunez Cerezo V, Hernandez F, et al. Portal cavernoma in the era of mesoportal shunt (Rex) and liver transplant in children. Eur J Pediatr Surg. (2016) 26:7–12. doi: 10.1055/s-0035-1563402
45. Lautz TB, Keys LA, Melvin JC, Ito J, Superina RA. Advantages of the meso-Rex bypass compared with portosystemic shunts in the management of extrahepatic portal vein obstruction in children. J Am Coll Surg. (2013) 216:83–9. doi: 10.1016/j.jamcollsurg.2012.09.013
46. Stewart JK, Kuo WT, Hovsepian DM, Hofmann LV, Bonham CA, Sze DY. Portal venous remodeling after endovascular reduction of pediatric autogenous portosystemic shunts. J Vasc Interv Radiol. (2011) 22:1199–205. doi: 10.1016/j.jvir.2011.01.438
47. Warren WD, Millikan WJ Jr, Smith RB III, Rypins EB, Henderson JM, Salam AA, et al. Non-cirrhotic portal vein thrombosis. Physiology before and after shunts. Ann Surg. (1980) 192:341–9. doi: 10.1097/00000658-198009000-00009
48. Glatard AS, Hillaire S, d'Assignies G, Cazals-Hatem D, Plessier A, Valla DC, et al. Obliterative portal venopathy: findings at CT imaging. Radiology. (2012) 263:741–50. doi: 10.1148/radiol.12111785
49. Superina R, Bambini DA, Lokar J, Rigsby C, Whitington PF. Correction of extrahepatic portal vein thrombosis by the mesenteric to left portal vein bypass. Ann Surg. (2006) 243:515–21. doi: 10.1097/01.sla.0000205827.73706.97
50. de Ville de Goyet J, Alberti D, Clapuyt P, Falchetti D, Rigamonti V, Bax NM, et al. Direct bypassing of extrahepatic portal venous obstruction in children: a new technique for combined hepatic portal revascularization and treatment of extrahepatic portal hypertension. J Pediatr Surg. (1998) 33:597–601. doi: 10.1016/s0022-3468(98)90324-4
51. Sharif K, McKiernan P, de Ville de Goyet J. Mesoportal bypass for extrahepatic portal vein obstruction in children: close to a cure for most! J Pediatr Surg. (2010) 45:272–6. doi: 10.1016/j.jpedsurg.2009.08.019
52. Gehrke I, John P, Blundell J, Pearson L, Williams A, de Ville de Goyet J. Meso-portal bypass in children with portal vein thrombosis: rapid increase of the intrahepatic portal venous flow after direct portal hepatic reperfusion. J Pediatr Surg. (2003) 38:1137–40. doi: 10.1016/s0022-3468(03)00257-4
53. Mack CL, Superina RA, Whitington PF. Surgical restoration of portal flow corrects procoagulant and anticoagulant deficiencies associated with extrahepatic portal vein thrombosis. J Pediat. (2003) 142:197–9. doi: 10.1067/mpd.2003.93
54. Mack CL, Zelko FA, Lokar J, Superina R, Alonso EM, Blei AT, et al. Surgically restoring portal blood flow to the liver in children with primary extrahepatic portal vein thrombosis improves fluid neurocognitive ability. Pediatrics. (2006) 117:e405–12. doi: 10.1542/peds.2005-1177
55. Stringer MD. Improved body mass index after mesenterico-portal bypass. Pediatric surgery international. (2007) 23:539–43. doi: 10.1007/s00383-007-1920-z
56. Lautz TB, Sundaram SS, Whitington PF, Keys L, Superina RA. Growth impairment in children with extrahepatic portal vein obstruction is improved by mesenterico-left portal vein bypass. J Pediatr Surg. (2009) 44:2067–70. doi: 10.1016/j.jpedsurg.2009.05.016
57. Wu H, Zhou N, Lu L, Chen X, Liu T, Zhang B, et al. Value of preoperative computed tomography for meso-Rex bypass in children with extrahepatic portal vein obstruction. Insights Imaging. (2021) 12:109. doi: 10.1186/s13244-021-01057-8
58. Tang R, Yu L, Wu G, Li A, Tong X, Zhang Y, et al. Modified Meso-Rex bypass with umbilical vein recanalization and intra-operative stenting. Langenbecks Arch Surg. (2021) 406:2553–62. doi: 10.1007/s00423-021-02308-4
59. Guerin F, Bidault V, Gonzales E, Franchi-Abella S, De Lambert G, Branchereau S. Meso-Rex bypass for extrahepatic portal vein obstruction in children. Br J Surg. (2013) 100:1606–13. doi: 10.1002/bjs.9287
60. Lautz TB, Eaton S, Keys L, Ito J, Polo M, Wells JCK, et al. Metabolic profile of children with extrahepatic portal vein obstruction undergoing meso-Rex bypass. J Surg Res. (2018) 223:109–14. doi: 10.1016/j.jss.2017.10.010
61. Bhat R, Lautz TB, Superina RA, Liem R. Perioperative strategies and thrombophilia in children with extrahepatic portal vein obstruction undergoing the meso-Rex bypass. J Gastrointest Surg. (2013) 17:949–55. doi: 10.1007/s11605-013-2155-z
62. Brichard M, Iesari S, Lerut J, Reding R, Goffette P, Coubeau L. Meso-Rex bypass for the management of extrahepatic portal vein obstruction in adults (with video). Hepatobiliary Pancreat Dis Int. (2021) 21:25–31. doi: 10.1016/j.hbpd.2021.08.003
63. Tantemsapya N, Superina R, Wang D, Kronauer G, Whitington PF, Melin-Aldana H. Hepatic histology and morphometric measurements in idiopathic extrahepatic portal vein thrombosis in children, correlated to clinical outcome of Meso-Rex bypass. Ann Surg. (2018) 267:1179–84. doi: 10.1097/SLA.0000000000002128
64. Wei Z, Rui SG, Yuan Z, Guo LD, Qian L, Wei LS. Partial splenectomy and use of splenic vein as an autograft for meso-Rex bypass: a clinical observational study. Med Sci Mon: Intern Med J Exp Clini Res. (2014) 20:2235–42. doi: 10.12659/MSM.892482
65. de Franchis R, Baveno VF. Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. (2010) 53:762–8. doi: 10.1016/j.jhep.2010.06.004
66. Zhang JS, Li L, Cheng W. A New Procedure for the treatment of extrahepatic portal hypertension in children: portal cavernoma-rex shunt with interposition of grafted portal vessel. J Am Coll Surg. (2016) 222:e71–6. doi: 10.1016/j.jamcollsurg.2016.03.020
67. Audet M, Baiocchi GL, Portolani N, Becmeur F, Caga M, Giulini SM, et al. A surgical solution to extrahepatic portal thrombosis and portal cavernoma: the splanchnic-intrahepatic portal bypass. Digest Liver Dis. (2003) 35:903–6. doi: 10.1016/j.dld.2003.01.001
68. Shneider B, Emre S, Groszmann R, Karani J, McKiernan P, Sarin S, et al. Expert pediatric opinion on the Report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension. Pediatr Transplant. (2006) 10:893–907. doi: 10.1111/j.1399-3046.2006.00597.x
69. Shneider BL, Bosch J, de Franchis R, Emre SH, Groszmann RJ, Ling SC, et al. Portal hypertension in children: expert pediatric opinion on the report of the Baveno v consensus workshop on methodology of diagnosis and therapy in portal hypertension. Pediatr Transplant. (2012) 16:426–37. doi: 10.1111/j.1399-3046.2012.01652.x
70. Khodayar-Pardo P, Pena Aldea A, Ramirez Gonzalez A, Meseguer Carrascosa A, Calabuig Bayo C. very early presentation of extrahepatic portal vein obstruction causing portal hypertension in an infant: uncertainties in the management and therapeutic limitations. Case Reports Gastroenterol. (2016) 10:360–5. doi: 10.1159/000447485
71. de Ville de Goyet J, D'Ambrosio G, Grimaldi C. Surgical management of portal hypertension in children. Semin Pediatr Surg. (2012) 21:219–32. doi: 10.1053/j.sempedsurg.2012.05.005
72. di Francesco F, Grimaldi C, de Ville de Goyet J. Meso-Rex bypass–a procedure to cure prehepatic portal hypertension: the insight and the inside. J Am Coll Surg. (2014) 218:e23–36. doi: 10.1016/j.jamcollsurg.2013.10.024
73. Han D, Tang R, Wang L, Li A, Huang X, Shen S, et al. Case report of a modified Meso-Rex bypass as a treatment technique for late-onset portal vein cavernous transformation with portal hypertension after adult deceased-donor liver transplantation. Medicine. (2017) 96:e7208. doi: 10.1097/MD.0000000000007208
74. Yu YD, Kim DS, Han JH, Yoon YI. Successful treatment of a patient with diffuse portosplenomesenteric thrombosis using a pericholedochal varix for portal flow reconstruction during deceased donor liver transplantation: a case report. Transplant Proc. (2017) 49:1202–6. doi: 10.1016/j.transproceed.2017.03.066
75. Van Thiel DH, Schade RR, Starzl TE, Iwatsuki S, Shaw BW Jr, Gavaler JS, et al. Liver transplantation in adults. Hepatology. (1982) 2:637–40. doi: 10.1002/hep.1840020517
76. Zhang M, Guo C, Pu C, Ren Z, Li Y, Kang Q, et al. Adult to pediatric living donor liver transplantation for portal cavernoma. Hepatol Res. (2009) 39:888–97. doi: 10.1111/j.1872-034X.2009.00526.x
77. Kitajima T, Sakamoto S, Uchida H, Hamano I, Kobayashi M, Kanazawa H, et al. Living donor liver transplantation with alternative porto-left gastric vein anastomosis in patients with post-Kasai extrahepatic portal vein obstruction. Pediatr Transplant. (2013) 17:E100–3. doi: 10.1111/petr.12067
78. Rotellar F, Cienfuegos JA, Bueno A, Marti P, Valenti V, Zozaya G, et al. Portal revascularization in the setting of cavernous transformation through a paracholedocal vein: a case report. Transplant Proc. (2010) 42:3079–80. doi: 10.1016/j.transproceed.2010.08.006
79. Singh N, Washburn K, Black S, Schenk A. Techniques for management of portal vein thrombosis during liver transplantation. Case Reports Transplant. (2020) 2020:8875196. doi: 10.1155/2020/8875196
80. Cheng YF, Ou HY, Tsang LL, Yu CY, Huang TL, Chen TY, et al. Vascular stents in the management of portal venous complications in living donor liver transplantation. Am J Transplant. (2010) 10:1276–83. doi: 10.1111/j.1600-6143.2010.03076.x
81. Kim JD, Choi DL, Han YS. The paracholedochal vein: a feasible option as portal inflow in living donor liver transplantation. Annals Surg Treat Res. (2014) 87:47–50. doi: 10.4174/astr.2014.87.1.47
82. Quintini C, Spaggiari M, Hashimoto K, Aucejo F, Diago T, Fujiki M, et al. Safety and effectiveness of renoportal bypass in patients with complete portal vein thrombosis: an analysis of 10 patients. Liver Transpl. (2015) 21:344–52. doi: 10.1002/lt.24053
83. Hajdu CH, Murakami T, Diflo T, Taouli B, Laser J, Teperman L, et al. Intrahepatic portal cavernoma as an indication for liver transplantation. Liver Transpl. (2007) 13:1312–6. doi: 10.1002/lt.21243
84. Walser EM, Soloway R, Raza SA, Gill A. Transjugular portosystemic shunt in chronic portal vein occlusion: importance of segmental portal hypertension in cavernous transformation of the portal vein. J Vasc Interv Radiol. (2006) 17:373–8. doi: 10.1097/01.rvi.0000194898.97672.d6
85. Chen Y, Ye P, Li Y, Ma S, Zhao J, Zeng Q. Percutaneous transhepatic balloon-assisted transjugular intrahepatic portosystemic shunt for chronic, totally occluded, portal vein thrombosis with symptomatic portal hypertension: procedure technique, safety, and clinical applications. Eur Radiol. (2015) 25:3431–7. doi: 10.1007/s00330-015-3777-1
86. Abud A, Maddur H, Salem R. Management of symptomatic portal cavernoma cholangiopathy with transplenic portal vein recanalization and transjugular intrahepatic portosystemic shunt. Hepatology. (2021) 73:456–9. doi: 10.1002/hep.31411
87. Jourabchi N, McWilliams JP, Lee EW, Sauk S, Kee ST. TIPS Placement via combined transjugular and transhepatic approach for cavernous portal vein occlusion: targeted approach. Case Reports Radiol. (2013) 2013:635391. doi: 10.1155/2013/635391
88. Ali Habib, Kush Desai, Hickey R, Bartley Thornburg, Michael Vouche, Robert L, vogelzang, et al. Portal vein recanalization–transjugular intrahepatic portosystemic shunt using the transsplenic approach to achieve transplant candidacy in patients with chronic portal vein thrombosis. J Vasc Interv Radiol. (2015) 26:499–506. doi: 10.1016/j.jvir.2014.12.012
89. Knight GM, Clark J, Boike JR, Maddur H, Ganger DR, Talwar A, et al. TIPS for adults without cirrhosis with chronic mesenteric venous thrombosis and EHPVO refractory to standard-of-care therapy. Hepatology. (2021) 74:2735–44. doi: 10.1002/hep.31915
90. Klinger C, Riecken B, Schmidt A, De Gottardi A, Meier B, Bosch J, et al. Transjugular portal vein recanalization with creation of intrahepatic portosystemic shunt (PVR-TIPS) in patients with chronic non-cirrhotic, non-malignant portal vein thrombosis. Z Gastroenterol. (2018) 56:221–37. doi: 10.1055/s-0043-121348
91. Thornburg B, Desai K, Hickey R, Hohlastos E, Kulik L, Ganger D, et al. Pretransplantation portal vein recanalization and transjugular intrahepatic portosystemic shunt creation for chronic portal vein thrombosis: final analysis of a 61-patient cohort. J Vasc Interv Radiol. (2017) 28:1714–21 e2. doi: 10.1016/j.jvir.2017.08.005
92. Kallini JR, Gabr A, Kulik L, Ganger D, Lewandowski R, Thornburg B, et al. Noncirrhotic complete obliterative portal vein thrombosis: novel management using trans-splenic transjugular intrahepatic portosystemic shunt with portal vein recanalization. Hepatology. (2016) 63:1387–90. doi: 10.1002/hep.28429
93. Pargewar SS, Desai SN, Rajesh S, Singh VP, Arora A, Mukund A. Imaging and radiological interventions in extrahepatic portal vein obstruction. World J Radiol. (2016) 8:556–70. doi: 10.4329/wjr.v8.i6.556
94. Bilbao JI, Elorz M, Vivas I, Martinez-Cuesta A, Bastarrika G, Benito A. Transjugular intrahepatic portosystemic shunt (TIPS) in the treatment of venous symptomatic chronic portal thrombosis in non-cirrhotic patients. Cardiovasc Interv Radiol. (2004) 27:474–80. doi: 10.1007/s00270-004-0241-z
95. Bertocchini A, Falappa P, Grimaldi C, Bolla G, Monti L, de Ville de Goyet J. Intrahepatic portal venous systems in children with non-cirrhotic prehepatic portal hypertension: anatomy and clinical relevance. J Pediatr Surg. (2014) 49:1268–75. doi: 10.1016/j.jpedsurg.2013.10.029
96. Liu J, Zhou C, Shi Q, Ma J, Ye T, Zheng C, et al. Exploration of interventional therapy strategy for portal vein occlusion: a case series study. Eur J Gastroenterol Hepatol. (2020) 32:507–16. doi: 10.1097/MEG.0000000000001586
97. Miraglia R, Luca A, Maruzzelli L, Spada M, Riva S, Caruso S, et al. Measurement of hepatic vein pressure gradient in children with chronic liver diseases. J Hepatol. (2010) 53:624–9. doi: 10.1016/j.jhep.2010.04.027
98. Takahashi T, Yoshida H, Mamada Y, Taniai N, Tajiri T. Balloon-occluded retrograde transvenous obliteration for gastric varices in a child with extrahepatic portal venous obstruction. J Nippon Med Sch. (2009) 76:173–8. doi: 10.1272/jnms.76.173
99. Miraglia R, Maruzzelli L, Caruso S, Ricotta C, Riva S, Burgio G, et al. Successful portal vein stent placement in a child with cavernomatous replacement of the portal vein after partial liver transplantation: the importance of a recognizable portal vein remnant. Cardiovasc Intervent Radiol. (2015) 38:1658–62. doi: 10.1007/s00270-015-1084-5
100. Marot A, Barbosa JV, Duran R, Deltenre P, Denys A. Percutaneous portal vein recanalization using self-expandable nitinol stents in patients with non-cirrhotic non-tumoral portal vein occlusion. Diagnostic and interventional imaging. (2019) 100:147–56. doi: 10.1016/j.diii.2018.07.009
101. Lee JH, Yoon CJ, Choi WS. Transhepatic stent placement for portal vein obstruction after hepatobiliary and pancreatic surgery: long-term efficacy and risk factor for stent failure. Eur Radiol. (2021) 31:1300–7. doi: 10.1007/s00330-020-07139-3
102. Mugu VK, Thompson SM, Fleming CJ, Yohanathan L, Truty MJ, Kendrick ML, et al. Evaluation of technical success, efficacy, and safety of portomesenteric venous intervention following non-transplant hepatobiliary or pancreatic surgery. J Vasc Interv Radiol. (2020) 31:416-24 e2. doi: 10.1016/j.jvir.2019.08.011
103. Kato A, Shimizu H, Ohtsuka M, Yoshitomi H, Furukawa K, Miyazaki M. Portal vein stent placement for the treatment of postoperative portal vein stenosis: long-term success and factor associated with stent failure. BMC Surg. (2017) 17:11. doi: 10.1186/s12893-017-0209-y
104. Naik K. Percutaneous transhepatic portal vein angioplasty for portal vein stenosis after pediatric liver transplantation: a single center experience. Am Assoc Study Liver Dis. (2016) 64:512a–3a.
105. Naik KB, Hawkins CM, Gill AE, Gupta NA. Clinical efficacy of percutaneous transhepatic portal vein angioplasty for late-onset portal vein stenosis in pediatric liver transplant patients. Transplantation. (2018) 102:E282–E7. doi: 10.1097/Tp.0000000000002138
106. Semiz-Oysu A, Keussen I, Cwikiel W. Interventional radiological management of prehepatic obstruction of the splanchnic venous system. Cardiovasc Intervent Radiol. (2007) 30:688–95. doi: 10.1007/s00270-007-9097-3
107. Cavalcante A, Zurstrassen CE, Carnevale FC, Pugliese RPS, Fonseca EA, Moreira AM, et al. Long-term outcomes of transmesenteric portal vein recanalization for the treatment of chronic portal vein thrombosis after pediatric liver transplantation. Am J Transplant. (2018) 18:2220–8. doi: 10.1111/ajt.15022
108. Jeon UB, Kim CW, Kim TU, Choo KS, Jang JY, Nam KJ, et al. Therapeutic efficacy and stent patency of transhepatic portal vein stenting after surgery. World J Gastroenterol. (2016) 22:9822–8. doi: 10.3748/wjg.v22.i44.9822
109. European Association for the Study of the Liver. EASL Clinical practice guidelines: vascular diseases of the liver. J Hepatol. (2016) 64:179–202. doi: 10.1016/j.jhep.2015.07.040
110. Kim KS, Kim JM, Lee JS, Choi GS, Cho JW, Lee SK. Stent insertion and balloon angioplasty for portal vein stenosis after liver transplantation: long-term follow-up results. Diagnostic Intervent. (2019) 25:231–7. doi: 10.5152/dir.2019.18155
111. David A, Metairie S, Perret C, Schnee M, Archambeaud I, Frampas E, et al. Minilaparotomy-assisted transmesenteric approach for portal vein recanalization and transjugular intrahepatic portosystemic shunt in a non-cirrhotic patient with portal cavernoma. Diagnostic Intervent Imag. (2020) 101:417–9. doi: 10.1016/j.diii.2019.12.004
112. Muratore S, Flanagan S, Hunter D, Acton R. Recanalization of chronic extrahepatic portal vein obstruction in pediatric patients using a minilaparotomy approach. J Pediatr Gastroenterol Nutr. (2019) 68:384–8. doi: 10.1097/MPG.0000000000002206
113. Gupta A, Gangwani G, Mehta N, Wadhwa N, Ghuman S, Yadav A. Percutaneous recanalization of anastomotic portal vein in a pediatric patient after liver transplant without any recognizable portal vein remnant on imaging. Experimental Clin Transplant. (2020) 18:261–4. doi: 10.6002/ect.2017.0326
114. Matsui O, Yoshikawa J, Kadoya M, Gabata T, Takashima T, Urabe T, et al. Transjugular intrahepatic portosystemic shunt after previous recanalization of a chronically thrombosed portal vein via a transmesenteric approach. Cardiovasc Intervent Radiol. (1996) 19:352–5. doi: 10.1007/BF02570190
115. Diao YP, Yang N, Guo LL, Song XJ, Liu CW, Li YJ. Unconventional interventional therapy for cavernous transformation of the portal vein. Ann Vasc Surg. (2014) 28:1791.e9–11. doi: 10.1016/j.avsg.2014.03.005
116. Young V, Rajeswaran S. Management of portal hypertension in the pediatric population: a primer for the interventional radiologist. Semin Intervent Radiol. (2018) 35:160–4. doi: 10.1055/s-0038-1660794
117. Franceschet I, Zanetto A, Ferrarese A, Burra P, Senzolo M. Therapeutic approaches for portal biliopathy: a systematic review. World J Gastroenterol. (2016) 22:9909–20. doi: 10.3748/wjg.v22.i45.9909
118. Dhiman RK, Saraswat VA, Valla DC, Chawla Y, Behera A, Varma V, et al. Portal cavernoma cholangiopathy: consensus statement of a working party of the Indian national association for study of the liver. J Clin Exp Hepatol. (2014) 4:S2–14. doi: 10.1016/j.jceh.2014.02.003
119. Saraswat VA, Rai P, Kumar T, Mohindra S, Dhiman RK. Endoscopic management of portal cavernoma cholangiopathy: practice, principles and strategy. J Clin Exp Hepatol. (2014) 4:S67–76. doi: 10.1016/j.jceh.2013.08.011
120. Dokmak S, Aussilhou B, Sauvanet A, Levy P, Plessier A, Fteriche FS, et al. Safety of supramesocolic surgery in patients with portal cavernoma without portal vein decompression. Large single centre experience. HPB. (2016) 18:623–9. doi: 10.1016/j.hpb.2016.05.009
Keywords: cavernous transformation of the portal vein, meso-Rex bypass, portal vein recanalization, splenorenal shunt, TIPS
Citation: Wei B, Huang Z and Tang C (2022) Optimal Treatment for Patients With Cavernous Transformation of the Portal Vein. Front. Med. 9:853138. doi: 10.3389/fmed.2022.853138
Received: 12 January 2022; Accepted: 21 February 2022;
Published: 24 March 2022.
Edited by:
Zongxin Ling, Zhejiang University, ChinaReviewed by:
Liangzhi Wen, Army Medical University, ChinaCopyright © 2022 Wei, Huang and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chengwei Tang, c2hjcWNkbWVkQDE2My5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.