- 1Faculty of Medicine, University of Ottawa, Ottawa, ON, Canada
- 2Department of Anesthesiology and Pain Medicine, Toronto Western Hospital, University Health Network, Toronto, ON, Canada
- 3Department of Pathophysiology, University of Buenos Aires, Buenos Aires, Argentina
Quadriplegia is associated with a multitude of health complications affecting numerous organ systems. Complications during the perioperative periods are not uncommon in this patient population due to abnormal responses to surgical stressors. Such complications include autonomic dysreflexia, cardiac ischemia, and respiratory compromise. Currently, there is no clear consensus on the ideal technique for perioperative anesthesia management in this population. In addition, the relationship between the perioperative complications and anesthesia practices have not been explored in-depth. Therefore, we aimed to investigate perioperative complications in the context of anesthesia that are associated with patients with quadriplegia undergoing various surgical procedures. Our PRISMA compliant systematic review included 12 articles covering the literature from inception to January 12, 2021. The review showed complications being pulmonary, cerebral, but most importantly and commonly cardiac in nature, with many patients suffering hypertension, and many others hypotension. In addition, our review showed that autonomic dysreflexia is common and in majority of patients, it was managed successfully with good recovery. Based on our findings, the use of anesthesia, either general or spinal, can be considered. Future studies are needed to elucidate the exact mechanisms involved in perioperative complications and anesthetic management that are associated with patients with quadriplegia. This review will aid in developing general recommendations based on the information available in the literature to guide perioperative management of this vulnerable patient population.
Background
Patients with quadriplegia due to cervical spinal cord injuries exhibit multiple health concerns including cardiorespiratory, gastrointestinal, cerebral neuropsychological and endocrinological dysfunctions (1–12). In addition, during the perioperative period, complications such as autonomic dysreflexia, respiratory compromise, myocardial ischemia can impose further challenges to anesthesiologists. There are few anesthetic choices for managing such patients; however, current knowledge is unclear whether there is a distinct advantage of one anesthesia technique over another (1–12). While general anesthesia is the traditional choice, some studies have indicated that a spinal anesthesia is preferred as it poses less risk of cardiac complications, namely autonomic dysreflexia (1). Unfortunately, the relationship between the various perioperative complications and anesthesia techniques were not studied extensively. Nevertheless, there is no consensus among the literature regarding a standard of care for this cohort of complex patients. Moreover, literature is limited to few case reports or observational studies (1–12), and a systematic synthesis of literature is still lacking. Therefore, it is imperative to synthesize the current understanding of the perioperative complications and outcomes pertaining to perioperative anesthesia management of quadriplegic patients undergoing various surgical procedures.
In this systematic review, we aim to investigate various perioperative complications (cardiac, cerebral, and pulmonary) that are associated with patients with quadriplegia undergoing surgical procedures. Specific objectives of the review are to evaluate the nature and extent of perioperative complications in the context of anesthesia, and the outcome of patients with quadriplegia undergoing, non-obstetric and non-spinal cord related surgeries. In addition, this synthesis will explore the various anesthetic management options for such cases to better guide perioperative patient management.
Methods
Population
Participants for this study comprised of all adult quadriplegic patients who had undergone non-cardiac surgeries. Patients undergoing spine and obstetric surgeries were excluded.
Intervention and Comparator
In this review, the intervention was defined as presence of any type of anesthesia (general anesthesia, spinal anesthesia, conscious sedation, or combination). Patients with quadriplegia undergoing surgery and exhibiting similar complications without any anesthesia or only having local anesthesia were included as comparators (i.e., more than half of the total number of articles that mentioned the comparator group).
Search Strategy
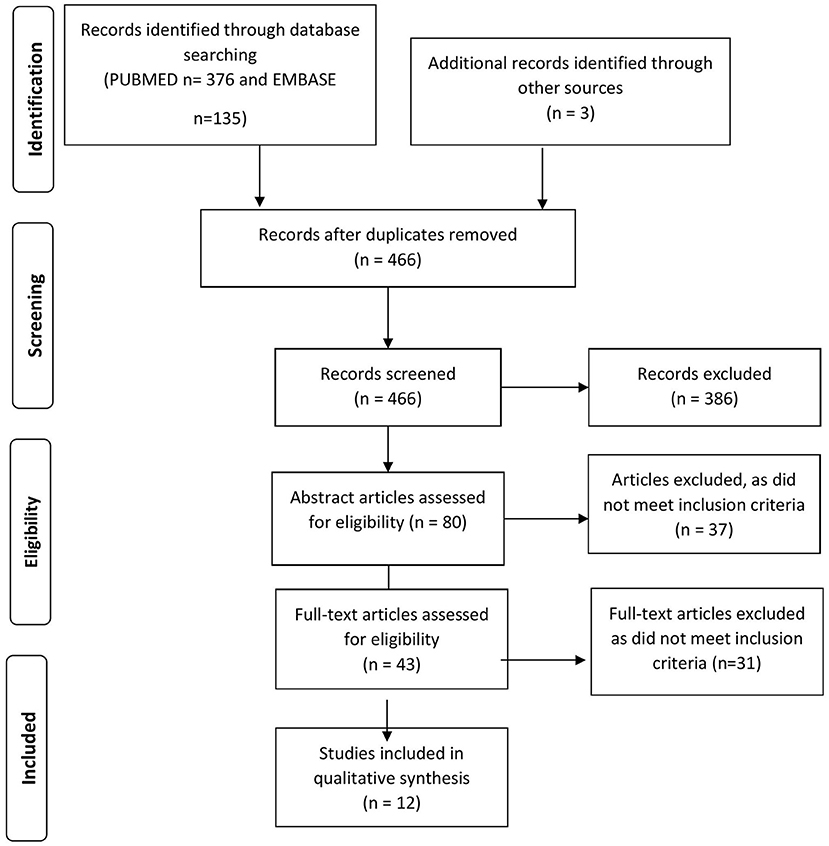
The databases MEDLINE (from inception to January 12, 2021), and EMBASE (from inception to January 12, 2021), were searched. To explore the research questions this systematic review was designed following the rigorous methodology (Figure 1) (13). The operator “and” was used to combine these search results with the terms. Manual searches of reference lists and trial registries were utilized to identify additional articles. The search was restricted to the English language and human studies only. The trained researcher (AAR) developed the search strategies and is described in detail in the Supplementary Material (Supplemental Digital Content: SDC. Supplementary Table 1). The following keywords/terms were used:
(((“Quadriplegia”[Mesh]) OR ((quadripleg*[Title/Abstract]) OR (tetrapleg*[Title/Abstract]))) AND ((((((“Anesthetics”[Mesh]) OR “Anesthesia”[Mesh]) OR “Anesthesia and Analgesia”[Mesh]) OR “Hypnotics and Sedatives”[Mesh]) OR “Analgesics”[Mesh]) OR ((((anesthetic*[Title/Abstract]) OR (anesthes*[Title/Abstract])) OR (sedativ*[Title/Abstract])) OR (anelges*[Title/Abstract])))) AND (((((((((“Autonomic Dysreflexia”[Mesh]) OR “Stroke”[Mesh]) OR “Myocardial Ischemia”[Mesh]) OR “Myocardial Infarction”[Mesh]) OR “Lung Diseases”[Mesh]) OR “Respiration Disorders”[Mesh]) OR “Heart Diseases”[Mesh]) OR “Hemodynamics”[Mesh]) OR (((((((((((autonomic dysreflexia*[Title/Abstract]) OR (stroke*[Title/Abstract])) OR (myocardial infarction*[Title/Abstract])) OR (myocardial ischemia*[Title/Abstract])) OR (pulmonary deficit*[Title/Abstract])) OR (pulmonary dysfunction*[Title/Abstract])) OR (hemodynamic*[Title/Abstract])) OR (respiratory acidosis*[Title/Abstract])) OR (respiratory alkalosis*[Title/Abstract])) OR (pulmonary complication*[Title/Abstract])) OR (complication*[Title/Abstract]))).
Selection Criteria and Reliability
Two independent reviewers (AAR and MS) evaluated the search results and the eligible studies for the potential inclusion were identified using the predefined selection criteria. If any disagreement occurred between the two authors, a third author (TC) was consulted to make the final decision.
Data Extraction and Quality Assessment
All study types including randomized controlled trials, prospective and retrospective studies, case series, and case reports were screened. Based on the screening of first fifty randomized pilot (4 selected) articles, we decided to include studies based on two essential criteria: first, the article should mention at least one of the (predefined) perioperative complications and second, it should clearly describe the type of anesthesia, if any is used. There was no gender restriction for this study. We excluded studies where patients with quadriplegia had surgery during pregnancy and/or for the spine-related disorders.
All studies were graded according to the level of evidence. Methodological quality was assessed based on selection, ascertainment, causality, and reporting of observational descriptive studies (case reports/series) as mentioned by Murad et al. (14). These qualitative analyses were performed by two reviewers (MS and AAR) and bias (which included attrition bias, detection bias, and selection bias) for each study were presented as binary notion: yes and no. Moreover, non-randomized observational studies (case-control, cohort studies and quasi experimental studies) were assessed according to the Newcastle-Ottawa Scale (NOS) (15) with points being awarded based on selection, comparability, and exposure. Any discrepancy during the bias assessment was resolved with the third reviewer (LV) as to minimize selection bias. The bias assessment detail is provided in the Supplementary Material (Supplemental Digital Content: SDC. Supplementary Table 2).
Outcome Measurements
The primary outcomes of this study were to know the incidence of three major perioperative complications (from surgery until discharge from the hospital) and their clinical presentation in patients with quadriplegia undergoing non-obstetric and non-spinal cord surgery. Major perioperative complication include: (1) cardiac events namely autonomic dysreflexia (AD) [any of the following presentation either alone or in combinations: sudden unexplained increase in systolic blood pressure (BP) > 180 mm Hg or diastolic BP > 100 mmHg, bradycardia (<60 bpm), tachycardia (>100 bpm), headache, blurred vision, severe nausea/vomiting, nasal stuffiness and sweating], myocardial ischemia/infarction [electrocardiographic (ECG) changes and or biochemical diagnosis], cardiac arrest (asystole, ventricular fibrillation), arrythmias, along with (2) cerebral events such as hemorrhagic or ischemic stroke (diagnosed on the imaging), and finally (3) pulmonary events namely apnea, oxygen desaturation requiring airway (invasive or non-invasive) intervention or change in the anesthetic technique, pulmonary embolism (confirmed with the imaging), extubation failure at the end of the surgery or continued ventilation postoperatively, and pneumonia (confirmed either radiologically or with presenting symptoms) during the hospital stay.
The secondary outcome consisted of (1) 30-day all-cause mortality and (2) overall post-surgical recovery. The latter was categorized by authors as “good” or “bad” depending on the length of hospital stay as well as unexpected medical sequelae. If studies did not mention the recovery period of patients post-operatively, it was noted as “not available.” The subgroup analysis includes delineating the type of anesthetic techniques (local anesthetics, monitored anesthesia care/sedation, regional, general anesthesia, or various combinations) and the complications.
Data Analysis and Synthesis
Basic descriptive analysis was performed, and data was presented as means, proportions, and percentages. Data information was also presented in tabular and graphic forms, where applicable.
Results
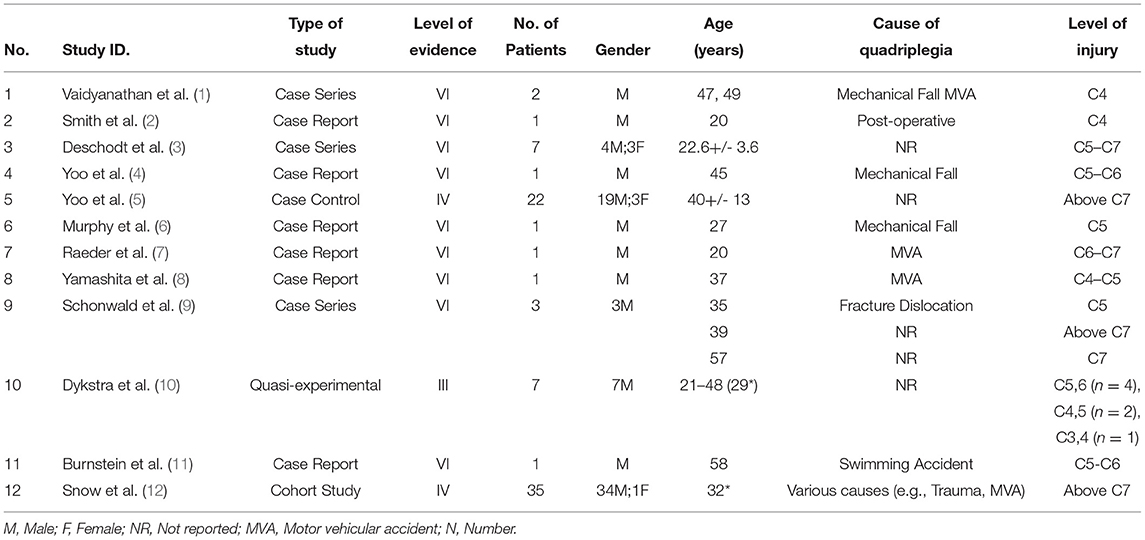
Our database search yielded a total of 511 articles (PubMed n = 376, and EMBASE n = 135) that were reduced to 466 results following removal of duplicates (Figure 1) and search development strategies are described in detail in the Supplementary Material (Supplemental Digital Content: SDC. Table 1). Articles were excluded in the preliminary study search based on title searches that did not meet our inclusion criteria. Next, a thorough abstract and manuscript search was conducted, and any articles that did not meet our inclusion criteria was not included. Three additional articles were searched as a cross-reference [PRISMA-P]. Following title, abstract and manuscript screens, 12 articles were finally included in the study (Tables 1–3). Nine studies were of level VI evidence, two were level IV and one was of level III (13). The articles included six case reports (50%), three case series (25%), one case control study (8%), one cohort study (8%), and one quasi-experimental study (8%).
Demographic characteristics: The studies included a total of 82 patients with 75 males (91%) and 7 female (9%) with an average age of 37 years (range 20-58 years) (Table 1). More than half the patients had quadriplegia due to the previous trauma from mechanical falls or accidents (54%) while the remaining group had quadriplegia due to an unspecified cause (46%). Majority (60%) of patients underwent urological procedures.
Primary Outcome
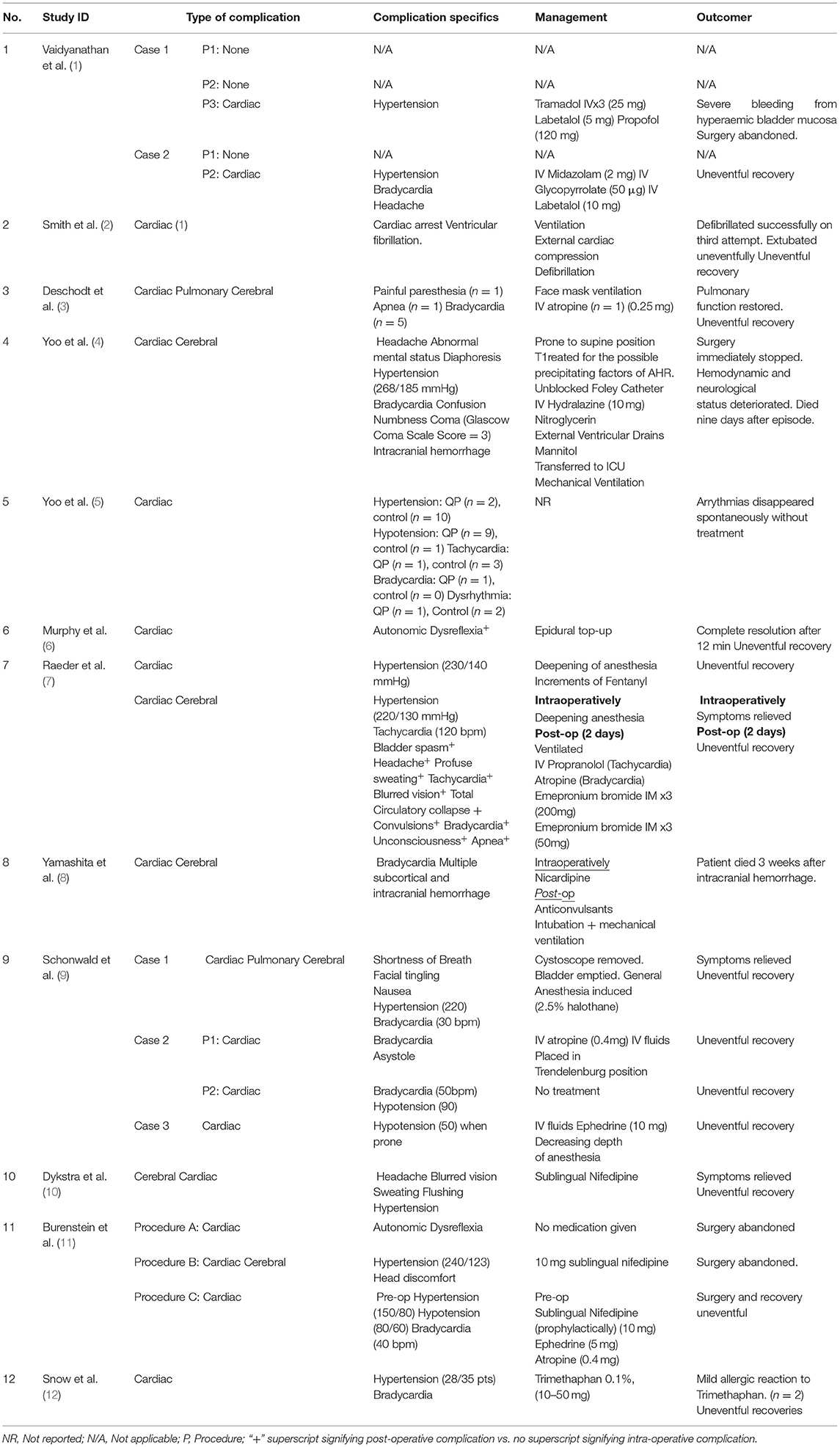
In our study, majority of perioperative complications were reported during intraoperative phase (10, n = 12 articles) and only (2, n = 12 articles) reported during the postoperative period. Regarding the complications, all 82 patients had cardiac events (100%) with the majority (54%) experiencing autonomic dysreflexia (presenting as hypertension (44 out of 82) and bradycardia (13 out of 82) followed by hypotension (11 out of 82), and tachycardia (2 out of 82). Cerebral and pulmonary events were reported in 7 (8.5%) and 2 (2.5%) patients, respectively.
Management of complications varied with the type of surgery and the severity of the complication. In 95% of patients, intraoperative complications were successfully managed medically without the cancellation of the surgery or procedure. However, in the remaining 5% of patients with severe complications, the surgery was terminated. In all terminated surgeries, patients had severe hypertension which met criteria for autonomic dysreflexia.
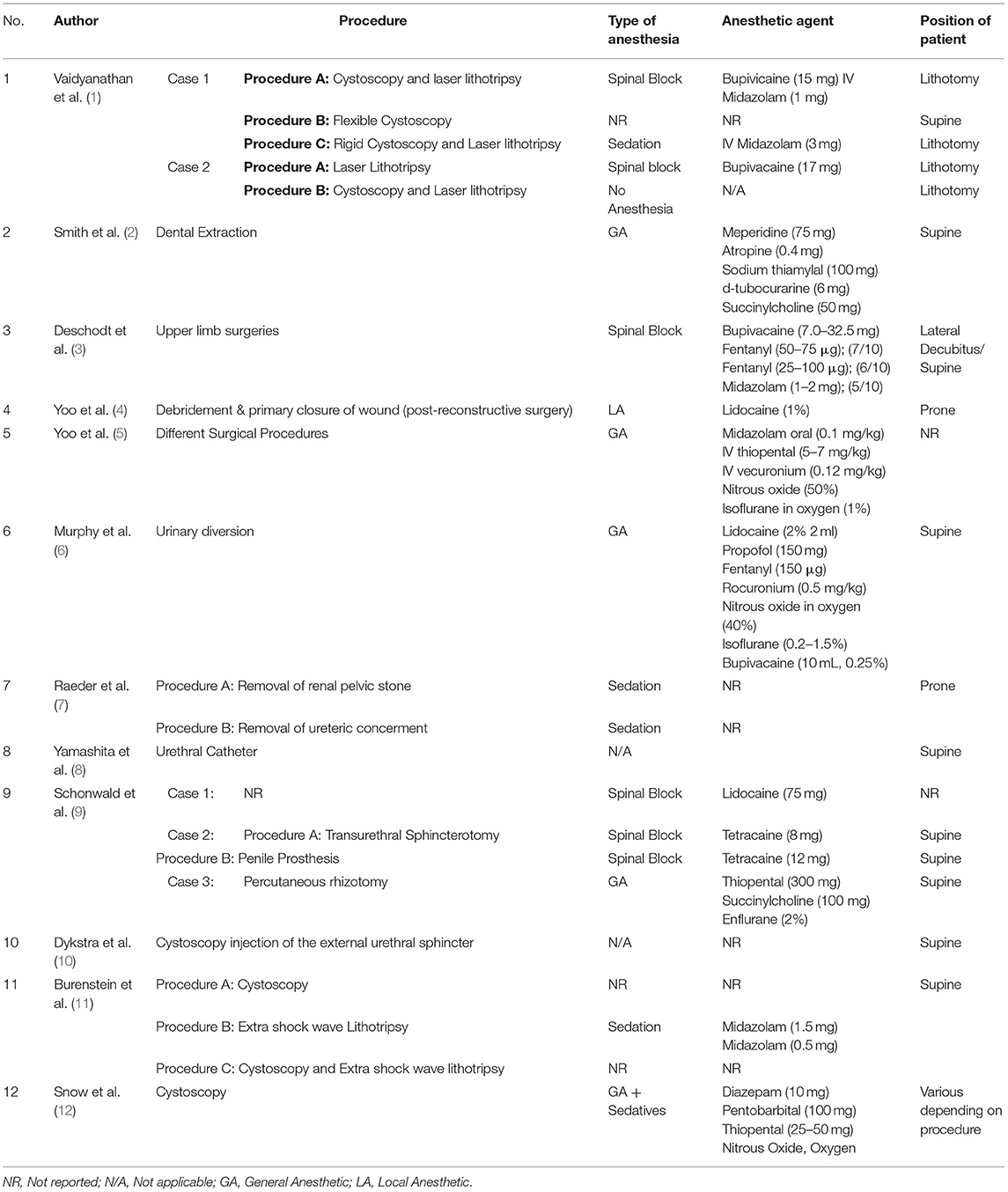
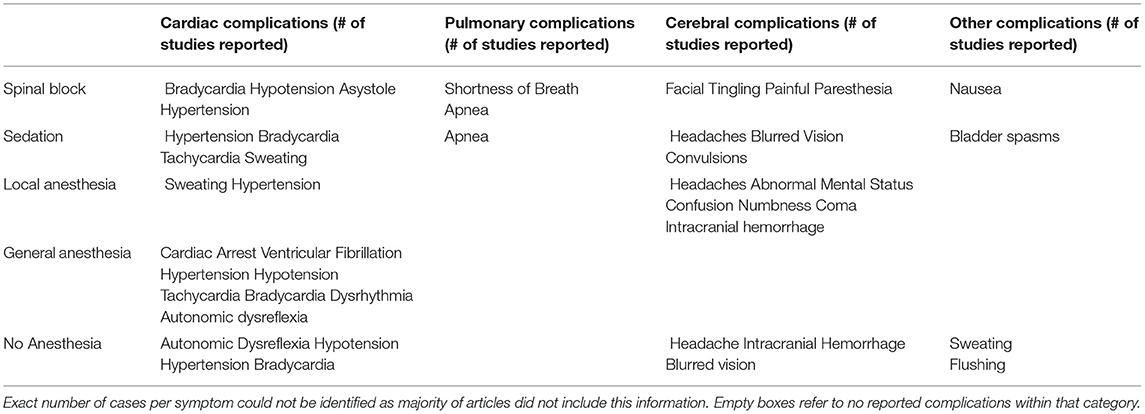
Other Outcomes and Subgroup Analysis
The 82 patients included in the study underwent a total of 89 procedures. General anesthesia was the most commonly (68.5%) used anesthesia technique followed by the spinal anesthesia (13.5%). Three procedures were done under conscious sedation, one procedure was done under local anesthesia alone while nine procedures did not require general anesthesia. (Table 4) Both sedation and spinal block anesthesia led to cardiac (bradycardia, hypotension, asystole, hypertension, sweating), pulmonary (shortness of breath, apnea), and cerebral complications (facial tingling, painful paresthesia, headaches, blurred vision, convulsions). On the other hand, local anesthesia reported only cardiac (sweating, hypertension) and cerebral complications (headaches, abnormal mental status, confusion, numbness, coma, and intracranial hemorrhage). In addition, general anesthesia protocols lead to only cardiac complications (cardiac arrest, ventricular fibrillation, hypertension, hypotension, tachycardia, bradycardia, dysrhythmia, autonomic dysreflexia). Lastly, not utilizing any anesthesia still caused cardiac (autonomic dysreflexia, hypotension, hypertension, bradycardia) and cerebral complications (headache, intracranial hemorrhage, blurred vision). While 10 out of the 12 articles did not comment on the 30-day mortality, only two deaths were reported following the procedures (9 and 13 days postoperatively, respectively). The length of hospital stay ranged from 1 day to 1 month, however the remaining 10 articles of studies did not report any follow-up periods.
Discussion
Our systematic review highlights some interesting clinical findings pertaining elements to major perioperative complications and anesthetic choices in patients with quadriplegia undergoing non-obstetric and non-spine related procedures/surgeries.
Perioperative Complications
With regards to the primary outcome, most complications were cardiac in nature, and interestingly many patients experienced hypertension, and others experienced hypotension in this review. This is in line with current literature where important perioperative complications reported include autonomic dysreflexia, bradycardia, hypotension, respiratory inadequacy, and muscle spasms (16).
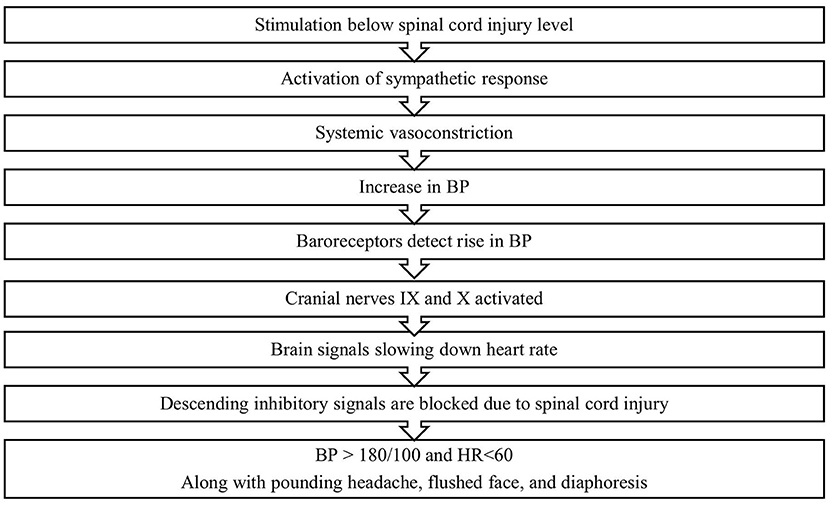
Autonomic Dysreflexia (AD) is a condition arising from previous spinal cord injury with severity and chance increasing as the level of injury increases (Figure 2) (17). AD is a life-threatening condition in which autonomic responses are dysregulated leading to severe hypertension in response to a noxious stimulus from below the site of injury (17). In about 85% of cases, this stimulus is caused by a urological procedure or issue such as a distended bladder, a problematic Foley catheter or an infection (17, 18). This is consistent with our findings, as the majority of our patients underwent a urological procedure. In addition, while patients with AD are at a much higher risk of death, our study only presented one patient who died within 30 days of the procedure (17). AD can also lead to severe cardiovascular dysfunction and painful headaches but objectively it is measured as a sudden increase in systolic blood pressure by 25 mm Hg (17). In addition, in line with our findings, AD occurs more frequently during urological surgery than any other surgery (17–19). Therefore, prior to surgery, triggers must be identified such as checking for catheter blockages, ensuring empty bowels and attention to skin changes or ulcerations (20). It is also recorded that some urological conditions may precede AD (21, 22).
Pulmonary and cerebral complications as part of the above-described AD were also observed during the procedures. While in some patients' vital capacities and ventilations are spared, their vital capacity and ventilation are reduced due to intercostal paralysis (3). As a consequence, patient must be given low concentrations of local anesthetics, and should be informed that if complications occur it might be necessary to switch to general anesthesia (3). In addition, a study showed a patient suffering from cerebral complications such as intracranial hemorrhage, headaches, irritability, and diaphoresis in response to AD (4). High catecholamine release in response to a noxious stimulus may be an explanation to the hypertensive crisis seen in these patients (4). Transformation of the anesthetic management should therefore be considered in such patients.
Choice of Anesthesia
In perioperative setting, patients with complete upper spinal cord injury have three options for anesthesia: monitored anesthesia care (with or without conscious sedation), regional anesthesia, and general anesthesia (20). Some patients may not require anesthetic agents if their surgery is below the site of injury, however, these patients must be well-educated on the risks and symptoms of AD and be asked to immediately report any changes such as headache, sweating, or difficulty breathing (23). Additional caution must be used when utilizing sedative agents as it may mask some symptoms due to ventilatory depression (20). In addition, patients may also choose to receive regional anesthesia. Spinal anesthesia appears to be a safer option and has become more and more widely accepted as it reduces risks of AD, and of spasms (20). Unfortunately, effectiveness and level of block have been reported to be difficult to ascertain, and therefore careful watching is required. Premedication using nifedipine has been shown to be effective, however anticholinergics have not shown much benefit unless it induces detrusor areflexia (20).
In our review, majority of studies have utilized some form of anesthesia technique, which is in line with the literature suggesting that perioperative complications are more common in patients who do not use anesthetic agents (16). Although there are few articles discussing the safety of not using any anesthetic agents, the ones present recommended that lack of anesthesia should be considered only with extreme caution and with an anesthesiologist on standby (23). This is supported by our review as two patients declined both general and spinal anesthesia during their cystoscopy procedures. Severe cardiac complications were reported in two cases where no anesthetic technique was utilized. In one patient, spinal anesthesia was offered that was associated with an uneventful postoperative period. It is prudent to block the afferent pathway of the AD by utilizing local, or regional anesthesia technique (1, 4). Therefore, our systematic review suggests that use of either general or spinal anesthesia is recommended over the sedation or local anesthesia.
Both general and spinal anesthesia are commonly used in surgical procedures for patients with high spinal cord injury. As of now, there is no consensus in the literature regarding a standard of care that should be applied for all patients.
Management of Complications
Our review showed that the AD is common and in majority of patients it was managed successfully with good recovery. This finding is in line with the literature, in which agents such as nifedipine, nitrates and captopril were preventively utilized with success (20). In some centers for example, 10 mg of oral nifedipine is given an hour prior to surgery to prevent AD (16). Although pharmacologic methods seem effective, identifying and eliminating triggers of AD, such as a distended bladder, have been utilized as first line treatment based on expert opinion and physiology rationale (17, 18).
Recommendations
Our review has attempted to provide better understanding of the AD after quadriplegia. A range of afferent stimuli can trigger an AD reaching the isolated spinal cord caudal to the level of spinal cord damage, mostly of visceral but less commonly of cutaneous and proprioceptive nature (17). This trigger can persist through the whole perioperative period including the immediate postoperative period. This systematic review emerged to shed some insights to both clinical and neurophysiological findings that could aid healthcare teams to better take care of this cohort of patients. Based on the available literature and expert opinion, it is reasonable to recommend following a few steps:
Patients with high spinal lesions without severe respiratory compromise undergoing non-obstetric and non-spinal surgery appear to be at an increased risk of developing perioperative complications, especially cardiac. Therefore, in such a context, risks and benefits of using particular anesthetic agents should be incorporated into the discussion. The literature recommends spinal blocks as a safe and effective method for these patients, but most procedures in our review utilize general anesthesia and perioperative complications were adequately managed (2, 5, 6, 11, 12). In addition, even for minor surgeries, one should be cautious in using local anesthesia with or without sedation (if the site of surgery is below the injury level) and patients should be fully aware of potential risks such as headache, sweating, or palpitation, difficulty breathing etc. The Presence of anesthesiologist for such cases is warranted. Agents, such as Nifedipine, should also be readily accessible to minimize or even prevent the effects of these complications. Patient reassurance can be provided given most patients had uneventful recoveries post-administration of a reversal agent or by deepening of the anesthetic agent, which is in line with our findings. In summary, general or spinal anesthesia is recommended over the sedation or local anesthesia.
Limitations
There are several limitations to our systematic review. Overall, there was a limited number of included studies looking at perioperative complications in patients with quadriplegia undergoing non-labor and non-spinal cord related surgeries (n = 12), but our sensitivity analysis showed similar results. In addition, most of the included articles were of evidence level IV or higher. As a result, the overall conclusions regarding this cohort of patients undergoing surgery and their management are limited. However, our strict methodology in the study design of this review, has led to upgraded or double upgraded according to the GRADE system, (24) so that we have moderate to high quality of included studies, what gives sufficient evidence for our findings. Nevertheless, the results of this review should be considered preliminary with the aim to motivate future prospective studies.
Also, both selection and attrition bias may be present in our study given the low number of articles and the heterogeneity in study data. On the other hand, all the data was organized in a standardized way, and many articles showed similar outcomes despite such differences, which is reflected in our sensitivity analysis, so that our results have good evidence.
Another limitation of our study involves the low number of female patients. This is backed by studies showing that males are in general more likely to suffer quadriplegia compared to females. Due to this, conclusions may be biased toward male patients, and more data would be needed to gain greater generalizability.
Conclusions
This systematic reviewshows various operative and anesthetic considerations for patients with quadriplegia undergoing various surgical procedures. The study highlighted intra-operative complications including those of cardiac, cerebral, and pulmonary nature as well as management strategies, overall patient outcomes, and anesthetic agents used. The work shows that a detailed anesthetic planning related to neurological but also neurophysiological details of each individual case is necessary to choose the best anesthetic approach.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
AR and MSa have contributed substantially for data search, synthesis and writing. MSi, BS, and LV have contributed in writing, editing and revising the manuscript. TC has contributed substantially on the concept development, data synthesis, interpretation, writing, and editing the manuscript. All authors contributed to the article and approved the submitted version.
Funding
MSi was supported by the Canadian Anesthesiology Society Career Scientist Award, and the merit awards program, department of anesthesiology and pain medicine, University of Toronto.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.852892/full#supplementary-material
References
1. Vaidyanathan S, Soni B, Selmi F, Singh G, Esanu C, Hughes P, et al. Are urological procedures in tetraplegic patients safely performed without anesthesia? A report of three cases. Patient Safety Surg. (2012) 6:3. doi: 10.1186/1754-9493-6-3
2. Smith B, Grenvik A. Cardiac arrest following succinylcholine in patients with central nervous system injuries. Anesthesiology. (1970) 33:558–559. doi: 10.1097/00000542-197011000-00024
3. Deschodt J, Lubrano J, Kassim M, et al. Cervical epidural anesthesia in tetraplegia. Hand Clin. (2002) 18:441–7. doi: 10.1016/s0749-0712(02)00018-5
4. Yoo K, Jeong C, Kim W, Lee HK, Kim SJ, Jeong ST, et al. Fatal cerebral hemorrhage associated with autonomic hyperreflexia during surgery in the prone position in a quadriplegic patient: a case report. Minerva Anesthesiology. (2010) 76:554–8.
5. Yoo KY, Lee JU, Kim HS, Im WM. Hemodynamic and catecholamine responses to laryngoscopy and tracheal intubation in patients with complete spinal cord injuries. Anesthesiology. (2001) 95:647–51. doi: 10.1097/00000542-200109000-00017
6. Murphy D, McGuire G, Peng P. Treatment of autonomic hyperreflexia in a quadriplegic patient by epidural anesthesia in the postoperative period. Anesth Analg. (1999) 89:148–9. doi: 10.1213/00000539-199907000-00025
7. Raeder JC, Gisvold SE. Perioperative autonomic hyperreflexia in high spinal cord lesions: A case report. Acta Anaesthesiol Scand. (1986) 30:672–3. doi: 10.1111/j.1399-6576.1986.tb02499.x
8. Yamashita T, Hiramusu H, Sakain N, Namba H. Cerebral hemorrhage due to posterior reversible encephalopathy syndrome associated with autonomic dysreflexia in a spinal cord injury patient. Neurol Med Chir. (2012) 52:640–3. doi: 10.2176/nmc.52.640
9. Schonwald G, Fish KJ, Perkash I. Cardiovascular complications during anesthesia in chronic spinal cord injured patients. Anesthesiology. (1981) 55:550–8. doi: 10.1097/00000542-198111000-00013
10. Dykstra D, Sidi A, Anderson L. The effect of Nifedipine on cystoscopy-induced autonomic hyperreflexia in patients with high spinal cord injuries. Survey Anesthesiol. (1988) 32:141. doi: 10.1097/00132586-198806000-00006
11. Burnstein A, Richlin D, Sotolongo JR. Nifedipine Pretreatment for Prevention of Autonomic Hyperreflexia during anesthesia-free extracorporeal shock wave lithotripsy. J Urol. (1992) 147:676–7. doi: 10.1016/s0022-5347(17)37344-5
12. Snow JC, Sideropoulos HP, Kripke BJ, Freed MM, Shah NK, Schlesinger RM. Autonomic hyperreflexia during cystoscopy in patients with high spinal cord injuries. Spinal Cord. (1978) 15:327–32. doi: 10.1038/sc.1977.49
13. Tetzlaff J, Page M, Moher D. PNS154 the Prisma 2020 statement: Development of and key changes in an updated guideline for reporting systematic reviews and meta-analyses. Value Health. (2020) 23:1154. doi: 10.1016/j.jval.2020.04.1154
14. Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evi-Based Med. (2018) 23:60–3. doi: 10.1136/bmjebm-2017-110853
15. The Ottawa Hospital Research Institute. Ottawa Hospital Research Institute. Available online at: http://ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed February 20, 2022).
16. Hambly PR, Martin B. Anaesthesia for chronic spinal cord lesions. Anaesthesia. (1998) 53:273–89. doi: 10.1046/j.1365-2044.1998.00337.x
17. Allen KJ, Leslie SW. Autonomic Dysreflexia. StatPearls. Treasure Island, FL: StatPearls Publishing (2021).
18. Liu N, Zhou M, Biering-Sou M, B F, Krassioukov AV. Iatrogenic urological triggers of autonomic dysreflexia: a systematic review. Spinal Cord. (2015) 53:500–9. doi: 10.1038/sc.2015.39
19. Liu N, Fougere R, Zhou MW, Nigro MK, Krassioukov AV. Autonomic dysreflexia severity during urodynamics and cystoscopy in individuals with spinal cord injury. Spinal Cord. (2013) 51:863–7. doi: 10.1038/sc.2013.113
20. Krassioukov A, Warburton DE, Teasell R, Eng JJ. Spinal cord injury rehabilitation evidence research team. a systematic review of the management of autonomic dysreflexia after spinal cord injury. Arch Phys Med Rehabil. (2008) 90:682–95. doi: 10.1016/j.apmr.2008.10.017
21. Bennett C. Urgent urological management of the paraplegic/quadriplegic patient. Urol Nurs. (2003) 23:436–7.
22. Persu C, Caun V, Dragomirimirim I, Geavlete P. Urological management of the patient with traumatic spinal cord injury. J Med Life. (2009) 2:296–302.
23. Petsas A, Drake J. Perioperative management for patients with a chronic spinal cord injury. BJA Education. (2015) 15:123–30. doi: 10.1093/bjaceaccp/mku024
Keywords: quadriplegia, spinal cord injury, cardiac changes, autonomic dysreflexia, anesthesia
Citation: Rizk AA, Saad M, Singh M, Schaller B, Venkatraghavan L and Chowdhury T (2022) Perioperative Complications and Anesthesia Practices in Managing Patients With Quadriplegia Undergoing Surgery: A Systematic Review. Front. Med. 9:852892. doi: 10.3389/fmed.2022.852892
Received: 11 January 2022; Accepted: 07 March 2022;
Published: 28 March 2022.
Edited by:
Somchai Amornyotin, Mahidol University, ThailandReviewed by:
Natalija Vukovic, University of Niš, SerbiaPasquale Sansone, University of Campania Luigi Vanvitelli, Italy
Copyright © 2022 Rizk, Saad, Singh, Schaller, Venkatraghavan and Chowdhury. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tumul Chowdhury, VHVtdWwuQ2hvd2RodXJ5QHVobi5jYQ==
 Abanoub Aziz Rizk
Abanoub Aziz Rizk Marina Saad
Marina Saad Mandeep Singh2
Mandeep Singh2 Lashmi Venkatraghavan
Lashmi Venkatraghavan Tumul Chowdhury
Tumul Chowdhury