- 1Medical Virtual Reality Research Group, Seoul National University College of Medicine, Seoul, South Korea
- 2Department of Anesthesiology and Pain Medicine, Seoul National University Bundang Hospital, Seongnam, South Korea
- 3Department of Anesthesiology and Pain Medicine, Seoul National University College of Medicine, Seoul, South Korea
- 4Department of Laboratory Medicine, Seoul National University Bundang Hospital, Seongnam, South Korea
Background: Venipuncture is one of the most frequent and frightening medical procedures for children. This randomized clinical trial aimed to evaluate whether pre-procedural immersive virtual reality (VR) education could decrease pain and anxiety during venipuncture procedure of children.
Methods: Sixty children scheduled for venipuncture at the phlebotomy unit were randomized into either the control or VR group. Before the procedure, children of the control group received conventional simple verbal instructions, whereas those of the VR group experienced a 4-min VR education regarding venipuncture. The primary outcome was the pain and anxiety of pediatric patients assessed with the children’s hospital of eastern ontario pain scale. Secondary outcomes were parental satisfaction, venipuncture time, repeated procedure and procedural difficulty rated by phlebotomists.
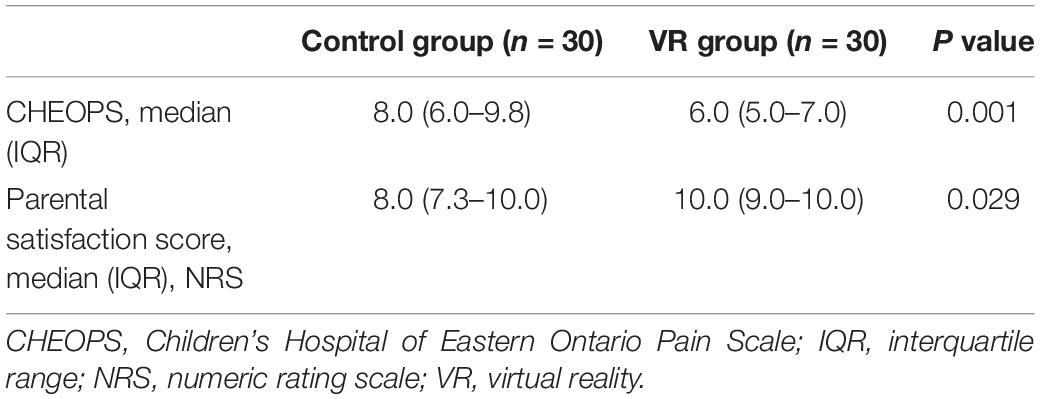
Results: The pain and anxiety score during the procedure was significantly lower in the VR group than in the control group (median [IQR], 6.0 [5.0–7.0] vs. 8.0 [6.0–9.8], P = 0.001). Parental satisfaction about the procedural process were higher in the VR group than in the control group (P = 0.029), and the degree of procedural difficulty was lower in the VR group, compared to the control group (P = 0.026).
Conclusion: The preprocedural VR education significantly reduced pain and anxiety of children and decreased the procedural difficulty of phlebotomists during venipuncture procedure.
Clinical Trial Registration: University hospital Medical Information Network Clinical Trials Registry (registration number: UMIN000042968, date of registration: January 9, 2021, URL: https://upload.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000049043).
Introduction
Venipuncture is one of the most frequently performed procedures in children. Approximately 50–80% of children aged <12 years experience high levels of pain and distress during venipuncture (1–3). Behavioral interventions to reduce the pain experienced during this procedure are based on the gate-control theory, which suggests that attention, thoughts, and beliefs influence pain sensation (4, 5). Distraction and education are the two most widely adopted behavioral approaches (6, 7). Diverting the attention of children via video games or animated cartoons during venipuncture significantly decreases needle-related pain (7, 8). Additionally, delivering information about painful procedures and teaching coping skills have been reported to alleviate procedural pain and anxiety in children (6, 9).
Virtual reality (VR) refers to a computer-generated realistic environment providing immersive and vivid experiences (10). Recently, VR systems have been utilized to alleviate pain or anxiety during medical procedures (1, 6, 7, 11–16). Distraction using a VR game was reported to effectively reduce “Worst pain” and “Pain unpleasantness” during venipuncture in children (1). Furthermore, VR systems providing procedural information through a simulated experience have been proven as an effective education platform to minimize peri-procedural anxiety in children (13–16). However, these previous studies used VR solely as a distraction tool to manage needle-related pain and anxiety.
To the best of our knowledge, no data exist regarding the effects of VR education on pain and anxiety during venipuncture in children. We hypothesized that VR education could decrease pain and anxiety during venipuncture in children. This randomized clinical trial was aimed to evaluate the effects of immersive VR education about venipuncture on procedural pain and anxiety in children. Additionally, parental satisfaction and procedural outcomes such as venipuncture time, repeated procedure, and difficulty score were also evaluated.
Materials and Methods
Study
This prospective randomized clinical trial was approved by the institutional review board of Seoul National University Bundang Hospital (IRB number: B-1911-574-301; date of approval: October 25, 2019) and registered at University hospital Medical Information Network Clinical Trials Registry (registration number: UMIN000042968; date of registration: January 9, 2021). Written informed consent was collected from the parents or guardians of children. Additionally, children aged ≥7 years received detailed instructions on this protocol and signed additional agreements. This study was conducted from February 2, 2021, to June 30, 2021, at Seoul National University Bundang Hospital (SNUBH).
Patients
Children aged 4–8 years who were scheduled to undergo venipuncture at the phlebotomy unit in SNUBH were enrolled in this study. Children with congenital disorders, hearing or visual impairments, intellectual developmental disabilities, cognitive deficits, epilepsy or seizure history, psychoactive medication prescriptions, and prior experience of venipuncture during the past year were excluded.
Randomization and Intervention
Enrolled children were randomly allocated to either the control or VR group via a computer-generated randomization code (Random Allocation Software, version 1.0; Isfahan University of Medical Sciences) in a 1:1 ratio. Randomization was performed by an independent researcher who was only in charge of patient assignment, 10 min before venipuncture. An opaque envelope with a randomization number was transferred to another researcher who performed the intervention in a separated area 5 min before entering the phlebotomy unit. Children in the control group received conventional, simple verbal instructions about the procedure, and those in the VR group underwent a 4-min VR education regarding venipuncture. Before the conventional instructions or VR education, the children were asked to indicate the expected venipuncture-related pain on a visual analog scale [range, 0 (no pain) to 10 (the worst pain)]. During the protocol, the children and their parents or guardians were not blinded to the intervention, whereas the evaluator and phlebotomy technicians were blinded to the group allocation.
Virtual Reality Education
The VR content was produced in collaboration with a VR producing company (JSC Games, Seoul, South Korea). All equipment and facilities in the phlebotomy unit in SNUBH were measured and rendered three-dimensionally to create a 360° three-dimensional virtual environment where users can experience immersive virtual education from a first-person perspective. The storyline of the VR education was written by phlebotomy technicians and anesthesiologists (J-WP, S-HH) and revised by pediatric psychiatrists in SNUBH. The VR education began with characters of “Hello Carbot” (Choi-Rock Contents Factory, Seoul, South Korea), a famous animated film in the Republic of Korea, greeting the children in front of the phlebotomy unit. The children then selected a main character conducting the education (Chatan or Mona; Figure 1A) according to their preferences. In a friendly tone, Chatan or Mona explained the purpose and process of venipuncture in detail, reminding the children to be brave and to not move during the procedure. The children underwent venipuncture in the VR phlebotomy unit after learning how to position themselves at phlebotomy desk and were encouraged to cooperate appropriately while trying not to feel anxious (Figure 1B). Through a licensing agreement with ChoiRock Contents Factory, we obtained the permission to use the characters. The VR experience was provided with a head-mounted VR display, OculusGo (OculusVR, Menlo Park, CA, United States; Figure 1C).
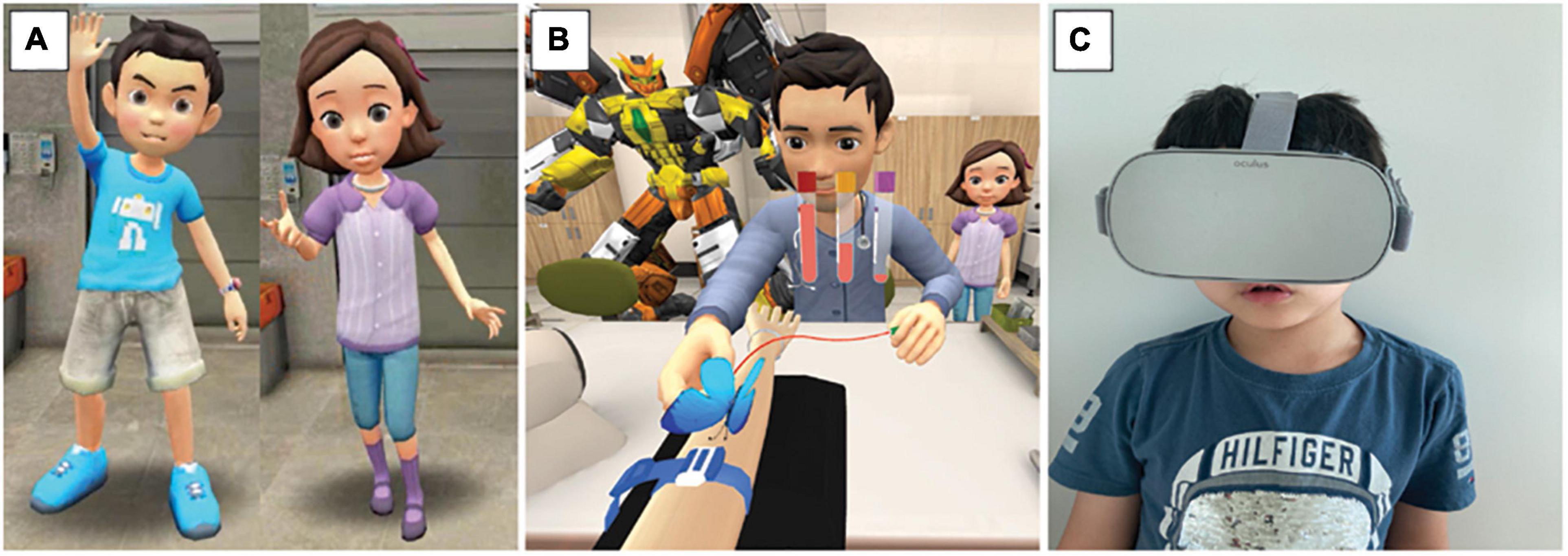
Figure 1. Virtual reality education system. (A) Children select Chatan (left) or Mona (right) as a main character; (B) and experience venipuncture procedure in a 360° and 3-dimensional virtual phlebotomy unit; (C) with a head-mounted virtual reality display.
Study Outcomes
After the intervention, the children entered the phlebotomy unit and underwent venipuncture as is usually practiced in SNUBH. The primary outcome was children’s anxiety and pain assessed using the Children’s Hospital of Eastern Ontario Pain Scale (CHEOPS), which was measured by a single blinded assessor during the procedure. The CHEOPS assesses six behaviors—cry, facial expression, verbal response, torso, hands, and legs (Supplementary Table 1); each behavior is coded with scores based on its intensity, and the total sum of the scores is considered to assess procedural pain and anxiety (the primary outcome of this study; score range: 4–13) (17).
Secondary outcomes were parental satisfaction and procedural outcomes. After the procedure, the parents or guardians of the children were asked to grade their satisfaction regarding the overall process of venipuncture using a numerical rating scale [range, 0 (very dissatisfied) to 10 (very satisfied)]. The time required for the venipuncture procedure (time from sitting at the phlebotomy desk to successful needle insertion for blood sampling) and the requirement of needle re-insertion due to bad patient cooperation were recorded by the blinded evaluator. Phlebotomy technicians rated the level of difficulty in performing venipuncture using the numerical rating scale [range, 0 (very easy) to 10 (very difficult)] immediately after the patients left the phlebotomy unit.
Statistical Analysis
Baseline characteristics included age, gender, height, weight, and preprocedural pain expectation. Continuous data are presented as median [interquartile range (IQR)], and categorical variables are presented as a number (percentage). The Mann–Whitney U test was used to compare continuous outcomes between the two groups. Categorical outcomes were analyzed using Fisher’s exact test. We used SPSS, version 21.0 (SPSS Inc., IBM, Chicago, IL, United States) for all statistical analyses. A two-sided P-value < 0.05 was considered to be statistically significant.
Sample Size
We conducted a power analysis using G*Power software, version 3.1.2 (Heinrich Heine University). A previous study reported that the mean and standard deviation of the CHEOPS score during venipuncture in the children were 9.3 and 2.4, respectively (18). A relative reduction in the pain and anxiety scores by 25% during venipuncture was considered clinically significant with respect to the VR education. A sample size of 30 children per group was calculated with a power of 0.9, significance level of 0.05, and an assumed dropout rate of 20%.
Results
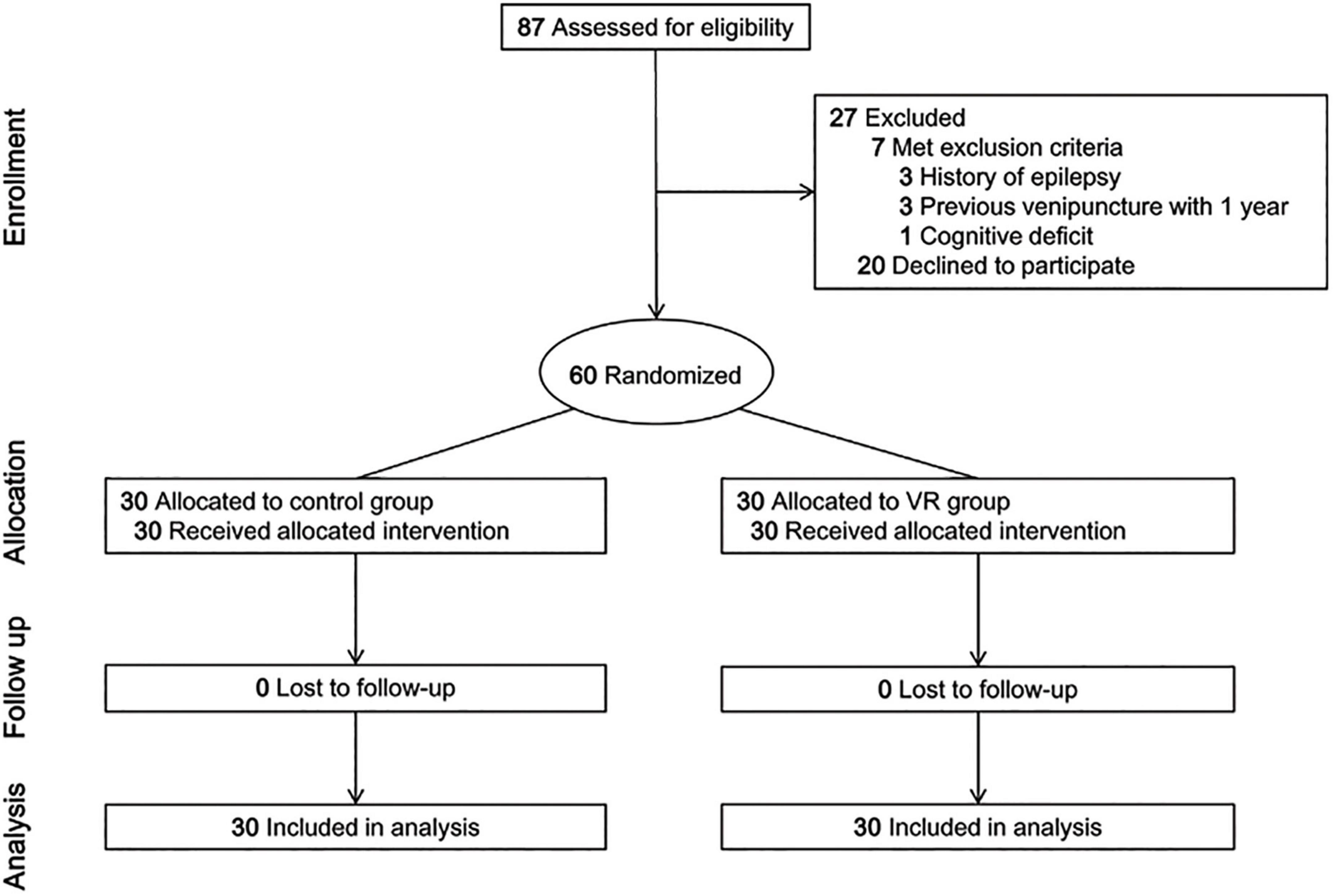
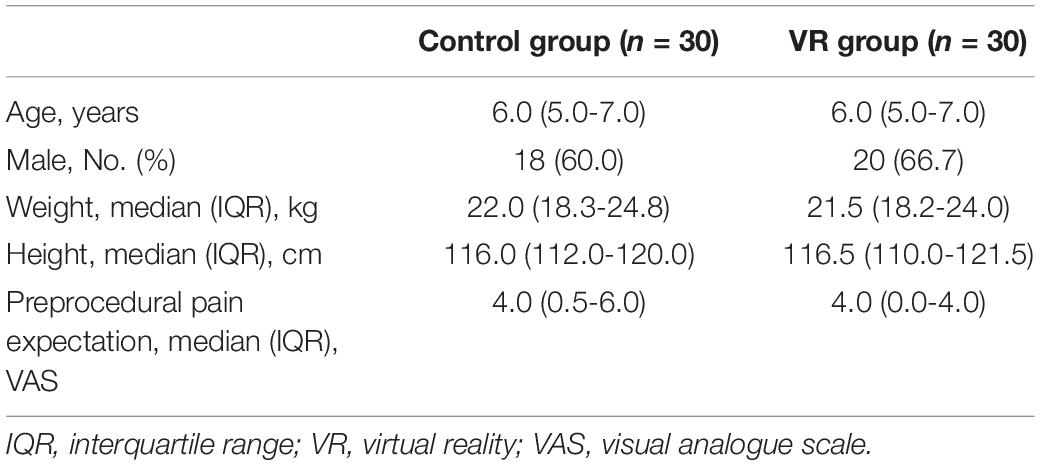
Eighty-seven children undergoing venipuncture were screened, and 27 of them were excluded (seven children met the exclusion criteria and 20 declined to participate). A total of 60 children (control group, 30; VR group, 30) participated in the study and none of them dropped out (Figure 2). The median (IQR) age was 6.0 (5.0–7.0) years in both groups (Table 1). Males accounted for 60.0 and 66.7% of the participants in the control group and the VR group, respectively. Children’s height, weight, and expectation of procedural pain were also comparable between the groups (Table 1).
Procedural anxiety and pain were assessed via the CHEOPS including six behaviors; the Mann–Whitney U test showed that those were less severe in the VR group. The CHEOPS score during the procedure was significantly lower in the VR group (median [IQR], 6.0 [5.0–7.0]) than in the control group (median [IQR], 8.0 [6.0–9.8]) (P = 0.001; Table 2). Parental satisfaction regarding the overall venipuncture process was higher in the VR group (median [IQR], 10.0 [9.0–10.0]) than in the control group (median [IQR], 8.0 [7.3–10.0]) (P = 0.029; Table 2).
Venipuncture duration was not significantly different between the groups (Table 3). Also, there was no difference in the incidence of repeated procedure. During the protocol, only one child required needle re-insertion due to inappropriate cooperation (in the control group). The degree of procedural difficulty graded by the phlebotomy technicians was lower in the VR group (median [IQR], 1.0 [0.0–2.0]) than in the control group (median [IQR], 2.0 [0.3–5.0]) (P = 0.026).
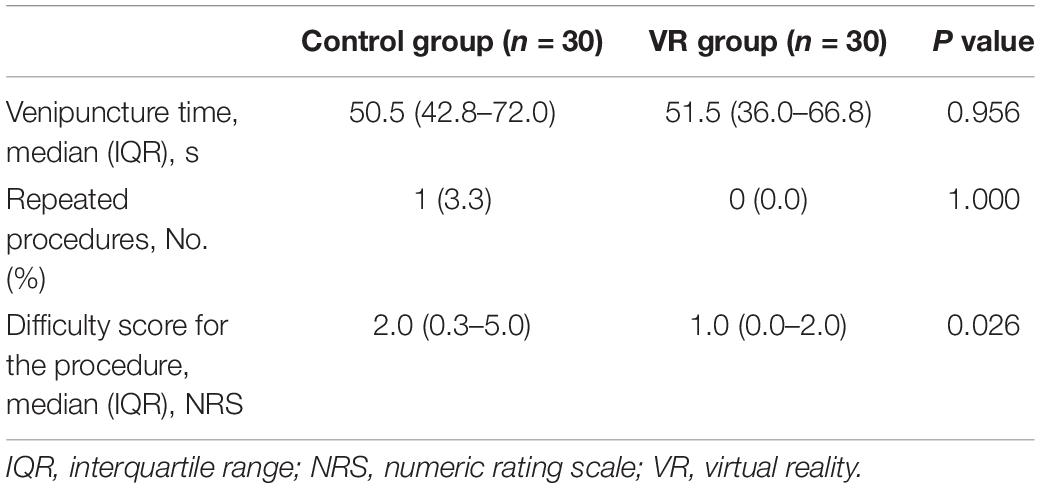
Table 3. Venipuncture time, the requirement of needle re-insertion, and difficulty score during the procedure.
Discussion
This was the first randomized controlled trial investigating the effects of VR education on pain and anxiety during venipuncture in children, one of the most common and fear-inducing medical procedures in children. VR education 5 min before entering the phlebotomy unit reduced procedural pain and anxiety in children and increased parental satisfaction, compared with conventional simple verbal instructions regarding the venipuncture procedure. Additionally, phlebotomy technicians reported greater ease in performing the procedure with children who had received VR education than with those who were given conventional instructions.
Previous studies have reported that VR education reduced periprocedural or perioperative anxiety in children, which is consistent with our results (13–16). Compared to 2-dimensional video education, 360°C 3-dimensional VR experience of the same content significantly reduced periprocedural anxiety in children undergoing chest radiography, which demonstrated the superior educational effect of VR (14). In the field of psychiatry, VR is utilized as an emerging method of exposure (19, 20). VR exposure in cognitive behavior therapy could be more effective than conventional in vivo approach in patients with social anxiety disorders (21). In a recent study, a VR adaptation of the Trier Social Stress Test showed the potential to induce endocrine responses comparable to those observed in the in vivo test (22). Clearly, VR technology is evolving into creating immersive and vivid experiences as realistic as in vivo experiences (20–23).
Prior to the present study, no data were available regarding the effects of pre-procedural VR education on pain and anxiety in children undergoing painful medical procedures. Immersive education regarding the procedure and a vivid virtual experience using a VR system might modulate the children’s knowledge, attitude, and expectations regarding venipuncture positively; this can influence pain sensation according to the gate-control theory (4, 5). Before the intervention, no significant difference was noted between the two groups in the expectations for needle-related pain.
Unmanaged pain and anxiety associated with medical procedures might not only cause short-term suffering but also lead to negative long-term complications such as post-traumatic stress syndrome, avoidance of medical treatment, and needle phobia (6, 11, 13). Therefore, the fact that VR education significantly decreases pain and anxiety during painful medical procedures is of great clinical value. To measure pain and anxiety objectively in the present study, we utilized the CHEOPS score, which has been applied to evaluate procedural pain and anxiety in children during acute pain-inducing situations such as venipuncture, fracture reduction, burn dressing, and laceration repair (17, 24, 25).
Patient or parental satisfaction is an important indicator of the quality of health care (26–28). Adequate satisfaction improves compliance with treatment; parents who are satisfied with the medical treatment for their child might pay more attention to their child’s health care and carefully follow doctors’ recommendations (29). Appropriate pain management is considered the most critical factor for parental satisfaction (30). Furthermore, venipuncture in children is a fairly challenging and stressful task for phlebotomists (31, 32). When performing needle-related procedures with anxious children (or parents), they report experiencing a high level of stress (31). Because children are easily influenced by the mood or stress of parents and healthcare providers, parental dissatisfaction or difficulty regarding the venipuncture procedure might worsen pain and anxiety in children (4, 31). In this study, encouragingly, the VR group children showed higher parental satisfaction and lower procedural difficulty than the control group children.
At the phlebotomy unit in SNUBH, children showing moderate or severe anxiety are allowed to sit on the parent’s lap in order to allow the parents to easily immobilize the children’s extremities during venipuncture (33). No significant difference was noted in the venipuncture duration and incidence of repeated procedure between the two groups probably because of active parental participation. The position was also reported to reduce children’s fear regarding the procedure (33). However, obvious difference was noted in the behaviors objectively assessed using the CHEOPS between the two groups in this study.
Conclusion
Immersive and vivid VR education prior to venipuncture significantly decreased procedural pain and anxiety in children, indicating that pre-procedural VR education could be an effective behavioral intervention. Further studies involving pre-procedural VR education in children undergoing painful medical procedures are required to support our findings.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of Seoul National University Bundang Hospital. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin. Written informed consent was obtained from the minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images included in this article.
Author Contributions
J-HR and S-HH conceptualized and designed the study, collected data, conducted the initial analysis, and drafted the initial manuscript. SH and JL designed the study, coordinated and supervised data collection, and reviewed the manuscript. S-HD and J-HK designed the study, conducted the initial analysis, and reviewed the manuscript. J-WP conceptualized and designed the study, supervised data collection, conducted the initial analysis, drafted the initial manuscript, and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Funding
All phases of this study were supported by grant no 09-2018-0003 from the SNUBH Research Fund. The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflict of Interest
S-HH and J-WP are the co-inventors of the patent, “Medical experience in hospitals provided with VR or AR system”, application of which is pending.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.849541/full#supplementary-material
References
1. Atzori B, Hoffman HG, Vagnoli L, Patterson DR, Alhalabi W, Messeri A, et al. Virtual reality analgesia during venipuncture in pediatric patients with onco-hematological diseases. Front Psychol. (2018) 9:2508. doi: 10.3389/fpsyg.2018.02508
2. Bolenius K, Brulin C, Graneheim UH. Personnel’s experiences of phlebotomy practices after participating in an educational intervention programme. Nurs Res Pract. (2014) 2014:538704. doi: 10.1155/2014/538704
3. Humphrey GB, Boon CM, van Linden van den Heuvell GF, van de Wiel HB. The occurrence of high levels of acute behavioral distress in children and adolescents undergoing routine venipunctures. Pediatrics. (1992) 90(1 Pt 1):87–91. doi: 10.1542/peds.90.1.87
4. Katz J, Rosenbloom BN. The golden anniversary of Melzack and Wall’s gate control theory of pain: celebrating 50 years of pain research and management. Pain Res Manag. (2015) 20:285–6. doi: 10.1155/2015/865487
5. Melzack R. From the gate to the neuromatrix. Pain. (1999) 82(Suppl. 1): S121–6. doi: 10.1016/S0304-3959(99)00145-1
6. Cohen LL. Behavioral approaches to anxiety and pain management for pediatric venous access. Pediatrics. (2008) 122, (Suppl. 3):S134–9. doi: 10.1542/peds.2008-1055f
7. Kuo HC, Pan HH, Creedy DK, Tsao Y. Distraction-based interventions for children undergoing venipuncture procedures: a randomized controlled study. Clin Nurs Res. (2018) 27:467–82. doi: 10.1177/1054773816686262
8. Inan G, Inal S. The impact of 3 different distraction techniques on the pain and anxiety levels of children during venipuncture: a clinical trial. Clin J Pain. (2019) 35:140–7. doi: 10.1097/AJP.0000000000000666
9. Suls J, Wan CK. Effects of sensory and procedural information on coping with stressful medical procedures and pain: a meta-analysis. J Consult Clin Psychol. (1989) 57:372–9. doi: 10.1037//0022-006x.57.3.372
10. Szekely G, Satava RM. Virtual reality in medicine. Interview by Judy Jones. BMJ. (1999) 319:1305. doi: 10.1136/bmj.319.7220.1305
11. Kennedy RM, Luhmann J, Zempsky WT. Clinical implications of unmanaged needle-insertion pain and distress in children. Pediatrics. (2008) 122, (Suppl. 3):S130–3. doi: 10.1542/peds.2008-1055e
12. Wong CL, Lui MMW, Choi KC. Effects of immersive virtual reality intervention on pain and anxiety among pediatric patients undergoing venipuncture: a study protocol for a randomized controlled trial. Trials. (2019) 20:369. doi: 10.1186/s13063-019-3443-z
13. Han SH, Park JW, Choi SI, Kim JY, Lee H, Yoo HJ, et al. Effect of immersive virtual reality education before chest radiography on anxiety and distress among pediatric patients: a randomized clinical trial. JAMA Pediatr. (2019) 173:1026–31. doi: 10.1001/jamapediatrics.2019.3000
14. Ryu JH, Park JW, Choi SI, Kim JY, Lee H, Yoo HJ, et al. Virtual reality vs. tablet video as an experiential education platform for pediatric patients undergoing chest radiography: a randomized clinical trial. J Clin Med. (2021) 10:2486. doi: 10.3390/jcm10112486
15. Ryu JH, Park JW, Nahm FS, Jeon YT, Oh AY, Lee HJ, et al. The effect of gamification through a virtual reality on preoperative anxiety in pediatric patients undergoing general anesthesia: a prospective, randomized, and controlled trial. J Clin Med. (2018) 7:284. doi: 10.3390/jcm7090284
16. Ryu JH, Park SJ, Park JW, Kim JW, Yoo HJ, Kim TW, et al. Randomized clinical trial of immersive virtual reality tour of the operating theatre in children before anaesthesia. Br J Surg. (2017) 104:1628–33. doi: 10.1002/bjs.10684
17. Blount RL, Loiselle KA. Behavioural assessment of pediatric pain. Pain Res Manag. (2009) 14:47–52. doi: 10.1155/2009/348184
18. Sikorova L, Hrazdilova P. The effect of psychological intervention on perceived pain in children undergoing venipuncture. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. (2011) 155:149–54. doi: 10.5507/bp.2011.024
19. Kothgassner OD, Felnhofer A. Lack of research on efficacy of virtual reality exposure therapy (VRET) for anxiety disorders in children and adolescents : a systematic review. Neuropsychiatr. (2021) 35:68–75. doi: 10.1007/s40211-020-00349-7
20. Carl E, Stein AT, Levihn-Coon A, Pogue JR, Rothbaum B, Emmelkamp P, et al. Virtual reality exposure therapy for anxiety and related disorders: a meta-analysis of randomized controlled trials. J Anxiety Disord. (2019) 61:27–36. doi: 10.1016/j.janxdis.2018.08.003
21. Bouchard S, Dumoulin S, Robillard G, Guitard T, Klinger E, Forget H, et al. Virtual reality compared with in vivo exposure in the treatment of social anxiety disorder: a three-arm randomised controlled trial. Br J Psychiatry. (2017) 210:276–83. doi: 10.1192/bjp.bp.116.184234
22. Zimmer P, Buttlar B, Halbeisen G, Walther E, Domes G. Virtually stressed? A refined virtual reality adaptation of the trier social stress test (TSST) induces robust endocrine responses. Psychoneuroendocrinology. (2019) 101:186–92. doi: 10.1016/j.psyneuen.2018.11.010
23. Clay CJ, Schmitz BA, Balakrishnan B, Hopfenblatt JP, Evans A, Kahng S. Feasibility of virtual reality behavior skills training for preservice clinicians. J Appl Behav Anal. (2021) 54:547–65. doi: 10.1002/jaba.809
24. Galinkin JL, Rose JB, Harris K, Watcha MF. Lidocaine iontophoresis versus eutectic mixture of local anesthetics (EMLA) for IV placement in children. Anesth Analg. (2002) 94:1484–8; table of contents. doi: 10.1097/00000539-200206000-00020
25. Hyland EJ, D’Cruz R, Harvey JG, Moir J, Parkinson C, Holland AJA. An assessment of early child life therapy pain and anxiety management: a prospective randomised controlled trial. Burns. (2015) 41:1642–52. doi: 10.1016/j.burns.2015.05.017
26. Tsironi S, Koulierakis G. Factors affecting parents’ satisfaction with pediatric wards. Jpn J Nurs Sci. (2019) 16:212–20. doi: 10.1111/jjns.12239
27. Lessa AD, Cabral FC, Tonial CT, Costa CAD, Andrades GRH, Crestani F, et al. Brazilian translation, cross-cultural adaptation, validity, and reliability of the EMpowerment of PArents in THe intensive care 30 (EMPATHIC-30) questionnaire to measure parental satisfaction in PICUs. Pediatr Crit Care Med. (2021) 22:e339–48. doi: 10.1097/PCC.0000000000002594
28. Chua GCC, Cyna AM. Satisfaction measures in pediatric anesthesia and perioperative care. Paediatr Anaesth. (2021) 31:746–54. doi: 10.1111/pan.14197
29. Savanheimo N, Vehkalahti MM, Pihakari A, Numminen M. Reasons for and parental satisfaction with children’s dental care under general anaesthesia. Int J Paediatr Dent. (2005) 15:448–54. doi: 10.1111/j.1365-263X.2005.00681.x
30. Ygge BM, Arnetz JE. Quality of paediatric care: application and validation of an instrument for measuring parent satisfaction with hospital care. Int J Qual Health Care. (2001) 13:33–43. doi: 10.1093/intqhc/13.1.33
31. Piazza J, Merkel S, Neusius H, Murphy S, Gargaro J, Rothberg B, et al. It’s not just a needlestick: exploring phlebotomists’ knowledge, training, and use of comfort measures in pediatric care to improve the patient experience. J Appl Lab Med. (2019) 3:847–56. doi: 10.1373/jalm.2018.027573
32. Block DR, Rickard TM, Johnson SR, Griesmann LD, Kang NS. Pediatric phlebotomy services: optimizing sample quality and improving the patient and parent experience. J Appl Lab Med. (2017) 1:453–6. doi: 10.1373/jalm.2016.021790
Keywords: anxiety, children, education, pain, venipuncture, virtual reality
Citation: Ryu J-H, Han S-H, Hwang SM, Lee J, Do S-H, Kim J-H and Park J-W (2022) Effects of Virtual Reality Education on Procedural Pain and Anxiety During Venipuncture in Children: A Randomized Clinical Trial. Front. Med. 9:849541. doi: 10.3389/fmed.2022.849541
Received: 06 January 2022; Accepted: 16 March 2022;
Published: 07 April 2022.
Edited by:
João Valente Cordeiro, National School of Public Health, New University of Lisbon, PortugalReviewed by:
Eron Grant Manusov, The University of Texas Rio Grande Valley, United StatesWadee Alhalabi, King Abdulaziz University, Saudi Arabia
Copyright © 2022 Ryu, Han, Hwang, Lee, Do, Kim and Park. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jin-Woo Park, amludWw4MjgyQGdtYWlsLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Jung-Hee Ryu1,2,3†
Jung-Hee Ryu1,2,3† Jin-Woo Park
Jin-Woo Park