- Department of Obstetrics and Gynecology, Shengjing Hospital of China Medical University, Shenyang, China
Background: The role of repeat cerclage (RC) among patients with prolapsed membranes remains controversial. We aimed to investigate the effectiveness of RC and assess the correlation between clinical factors and pregnancy outcome following RC.
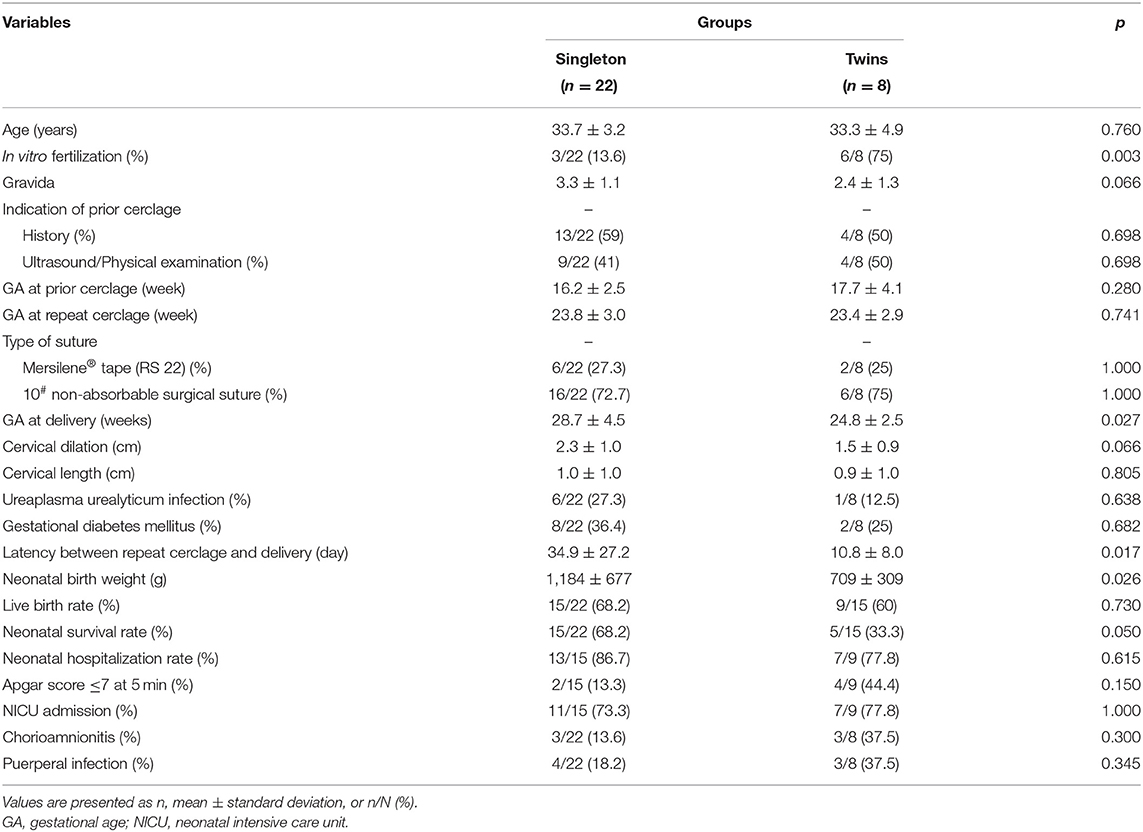
Methods: The clinical data of patients who underwent RC for prolapsed membranes after prior cerclage were retrospectively investigated. The clinical characteristics of patients were compared between singleton and twin pregnancies. The clinical characteristics of singleton pregnancies were compared between the gestational age (GA) at delivery <28 weeks' and ≥28 weeks' groups. Receiver operating characteristic (ROC) curve analysis was performed to determine predictive factors. Singleton patients were divided into two groups according to GA at RC as follows: GA <22.3 weeks and GA ≥22.3 weeks. Pregnancy outcomes were compared between groups.
Results: The mean GA at delivery of singleton pregnancies was significantly higher than that of twin pregnancies. The mean latency between RC and delivery of singleton pregnancies was significantly longer than their twin counterparts. There were significant differences in the pregnancy outcomes between the GA <22.3 weeks group and GA ≥22.3 weeks group. Kaplan–Meier survival curves showed a lower incidence of neonatal death in the GA ≥22.3 weeks group compared with that in the GA <22.3 weeks group.
Conclusions: RC may be an effective method to prolong the duration of pregnancy among patients with singleton pregnancy. However, the selection of RC for patients with twin pregnancies remains controversial. GA at RC appears to be fair for predicting pregnancy outcomes following RC.
Introduction
Cervical cerclage is a surgical intervention involving the placement of a stitch around the uterine cervix, with the aim of preventing cervical effacement and dilatation. However, women with cervical insufficiency remain at a high risk of second-trimester loss and preterm birth despite transvaginal cerclage suture (1, 2). Cervical cerclage indicated following clinical finding of prolapsing fetal membranes at the external cervical orifice is called an emergency cerclage. Cerclage has been reported to prolong gestational age (GA) and improve the pregnancy outcome; however, it is also known to increase the risk of preterm premature rupture of membranes, chorioamnionitis, and other complications (3–13).
The pregnancy outcome following emergency cerclage is affected by various clinical factors, such as nulliparity, in vitro fertilization, prolapsed membranes, cervical dilation, positive vaginal culture, GA at operation, infection, type of suture, and adjunctive pessary therapy (14). Prolapse of membranes following cervical cerclage is usually considered as cerclage failure. Repeat cerclage (RC), also called reinforcing cerclage, is a special kind of emergency cerclage that is considered a remedy for cerclage failure. Because of the high risk for rupture of membranes and delivery before neonatal viability after the procedure, only cases with prolapsed membranes after prior cerclage are chosen to undergo RC. Reports on the epidemiology of RC are limited, and the results obtained are conflicting in nature (15–21). Moreover, the clinical factors affecting pregnancy outcomes following RC have hardly ever been reported.
The aim of this study was to investigate the effectiveness of RC and assess the correlation between clinical factors and pregnancy outcome following RC in a Chinese population.
Materials and Methods
Patients and Study Design
In this retrospective cohort study, the clinical data of patients who underwent RC at the Shengjing Hospital of the China Medical University between January 2015 and December 2020 were evaluated. The study protocol was approved by the Institutional Review Board of the Shengjing Hospital of China Medical University, Shenyang, Liaoning Province, China (Approval number: 2020PS819K). Written informed consent was obtained from the patients for their participation in the study and the publication of this report.
The study inclusion criteria were as follows: GA between 16 and 28 weeks; cervical dilation ≥1 cm with prolapsed membranes, intact membranes, no uterine contraction, no vaginal bleeding, and no fetal abnormalities. Women with maternal complications such as infections or autoimmune diseases, chorioamnionitis, and incomplete clinical information were excluded.
The RC procedure (McDonald-type) (22) was performed under combined spinal epidural anesthesia using 5 mm Mersilene® tape (RS 22) or 10# non-absorbable surgical sutures. The previous cerclage knot was removed. All cerclage procedures were performed by experienced senior obstetricians. After the procedure, patients were advised bed rest and administered antibiotics and atosiban for at least 48 h; simultaneously, progesterone was continuously administered vaginally after discharge until delivery.
The clinical characteristics of patients were compared between singleton and twin pregnancies. Furthermore, the clinical characteristics of singleton pregnancies were compared between GA at delivery <28 weeks and ≥28 weeks. In addition, singleton patients were divided into two groups according to GA at RC as follows: GA <22.3 weeks and GA ≥22.3 weeks, and pregnancy outcomes were compared between these groups.
Statistical Analysis
The data were compared between the two groups using the analysis of variance or Mann–Whitney U test. The difference in percentages between the groups was compared using Fisher's exact probability test. The receiver operater characteristic (ROC) curves were analyzed to assess the discriminative ability of GA at RC. Survival curves were compared using Kaplan–Meier analysis and the log-rank test. A p < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS 23.0 statistical software (IBM Corp., Armonk, NY, USA).
Results
Repeat cerclage procedures were performed successfully in 30 patients. There were no cases of membrane rupture or immediate pregnancy loss during the procedures. All the patients were Chinese. Eight patients had a twin pregnancy, and one patient experienced intrauterine fetal death of one twin. Table 1 shows the comparison of clinical characteristics between singleton and twin pregnancies. The mean GA at delivery of singleton pregnancies was 28.7 weeks, with a neonatal survival rate of 68.2% (15/22). This was significantly higher than that of twin pregnancies. In addition, the mean latency between RC and delivery of singleton pregnancies was 3 weeks longer than that in their twin counterparts. Among the 30 pregnancies, 11 ended with immediate neonatal death due to extreme prematurity. Nine patients delivered vaginally following removal of the cerclage knot, and the remaining 10 patients underwent cesarean section due to scarred uterus, fetal malposition, oligohydramnios, or fetal distress.
Furthermore, the clinical characteristics of singleton pregnancies were compared between GA at delivery of <28 weeks and ≥28 weeks (Table 2). GA at RC was the only risk factor for second-trimester loss. ROC curve analysis demonstrated that GA at RC may be a discriminative parameter for predicting delivery at ≥28 weeks of gestation. The area under curve (AUC) for the prediction of delivery at ≥28 weeks of GA with RC was 0.746 (Figure 1). Using a GA cut-off of 22.3 weeks at RC, the sensitivity and specificity for predicting delivery at ≥28 weeks of gestation were 100% and 50%, respectively.
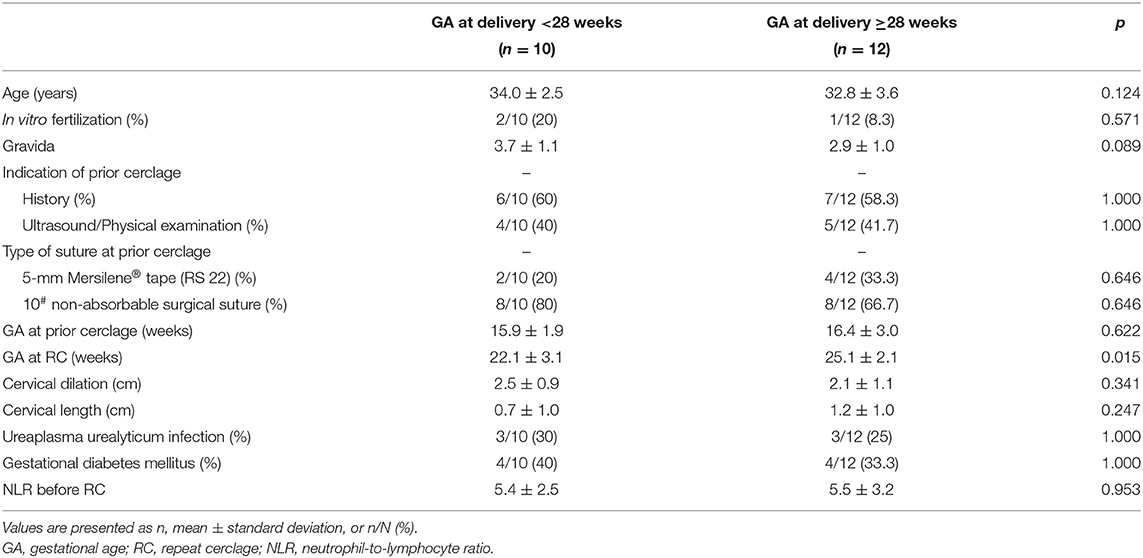
Table 2. Comparison of clinical characteristics among patients with singleton pregnancies between GA at delivery <28 weeks and ≥28 weeks.
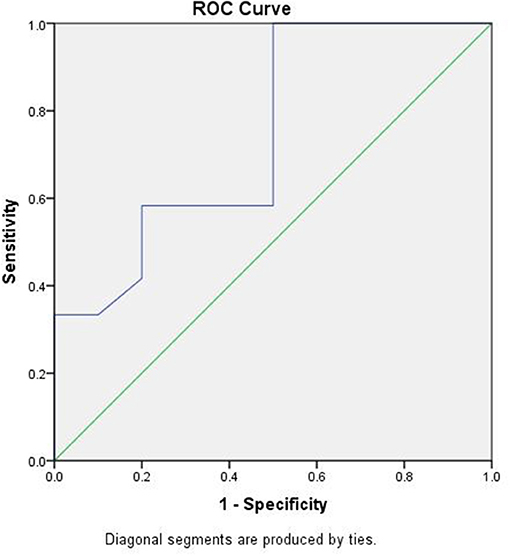
Figure 1. Receiver operater characteristic (ROC) curve of gestational age (GA) at repeat cerclage (RC) predicting delivery ≥28 weeks of gestation. The area under the curve (AUC) is 0.746. GA ≥22.3 weeks at RC had a sensitivity of 100% and specificity of 50%.
Based on the cut-off value, patients were divided into a GA <22.3 weeks at RC group and GA ≥22.3 weeks at RC group. Table 3 demonstrates the comparison of pregnancy outcomes between these two groups. The GA <22.3 weeks group showed a worse neonatal outcome compared to the GA ≥22.3 weeks group. There were seven neonatal deaths among all the singleton pregnancies. Kaplan–Meier survival curves showed a lower incidence of neonatal death in the GA ≥22.3 weeks group (17.6%) compared with that in the GA <22.3 weeks group (80%) (p = 0.019, log rank test; Figure 2).
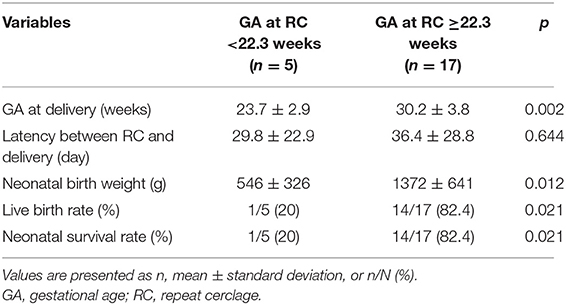
Table 3. Comparison of pregnancy outcomes among patients with singleton pregnancies according to GA at RC.
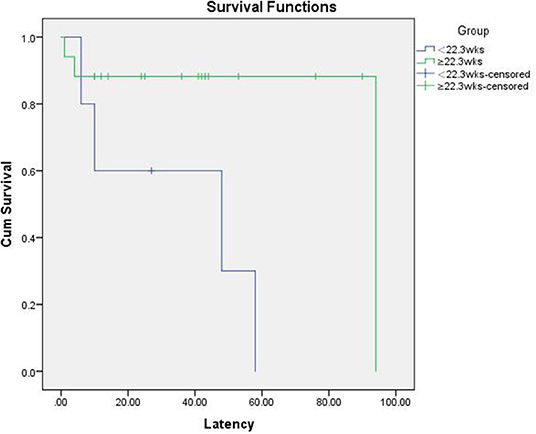
Figure 2. Kaplan–Meier survival curve for neonatal death with gestational age (GA) at repeat cerclage (RC) ≥22.3 weeks and <22.3 weeks.
Discussion
To the best of our knowledge, this is the first study investigating the effectiveness of RC for both singleton and twin pregnancies, as well as the first to assess the correlation between clinical factors and pregnancy outcomes following RC in a Chinese population. Evidence from our study suggests that the RC delays delivery by an average of five additional weeks for singleton pregnancies, which is consistent with the findings of Song et al. (15). RC may be an effective method to prolong the duration of pregnancy among patients with singleton pregnancies. On the contrary, RC for twin pregnancies showed an unsatisfactory outcome, such as a poor prolongation of pregnancy and an extremely low neonatal survival rate. This may imply a high risk of delivery before viability after RC for twin pregnancies. The selection of patients with twin pregnancies for RC, thus, remains controversial. Another main finding of our study was that GA at RC appears to be fair for predicting pregnancy outcomes following RC. ROC curve analysis demonstrated that GA at RC could be used to predict delivery at ≥28 weeks of gestation following RC. Our study indicates that the patients who underwent RC at ≥22.3 weeks GA were more likely to deliver after 28 weeks GA, while those who underwent RC at <22.3 weeks of gestation were unlikely to keep the fetus until 28 weeks of gestation. We also found that patients with lower GAs at RC showed worse neonatal outcomes; GA <22.3 weeks at RC was associated with earlier delivery, lower neonatal birth weight, and poorer live birth and neonatal survival rates.
Currently, there are few reports on RC in the literature. Song et al. (15) have suggested that RC improved the pregnancy outcome of patients with prolapsed membranes, including neonatal survival and quality of survival, consistent with our findings. In addition, they also proposed that neutrophil-to-lymphocyte ratio (NLR) might be used as a reliable factor for predicting pregnancy outcomes following RC (17). This was quite different from our finding, and this is likely due to the different populations studied or the limited sample size.
Fox et al. reported that RC appeared to delay delivery by an average of 7 weeks compared to that in the untreated group (16). Althuisius et al. reported the cases of two patients who delivered at term after undergoing RC (18). Baxter et al. reported five cases of ultrasound-indicated reinforcing cerclage; however, the pregnancy outcomes were not improved compared to those in their non-RC counterparts (19). Contag et al. claimed that the placement of RC for short cervix did not prolong the duration of pregnancy, delay GA at delivery, or modify the probability of preterm birth (20). Simcox et al. found that a reinforcing cerclage following primary cerclage failure hastened preterm delivery (21). However, the indications of RC in all the cases reported previously were only identified by ultrasonography after prior cervical cerclage, without the clinical finding of prolapsed membranes.
Predictors of pregnancy outcome following cervical cerclage have become the focus of attention for obstetricians over the last few decades. However, nearly all the studies on predictors of pregnancy outcomes following cervical cerclage have only focused on primary cerclage. Previous studies have shown that pre- and post-cerclage cervical length, positive vaginal culture at cerclage, amniotic fluid levels of neutrophil elastase, and interleukin 6 levels are predictors of latency between cerclage and GA at delivery (3, 5, 23–27). Cervical dilatation, volumetric assessment of cervical funneling, and a history of previous uterine instrumentation are independent predictors of cerclage failure (28–31). GA at emergency cervical cerclage plays an important role on the pregnancy outcome (5, 9, 32). Our study shows, for the first time, that GA at RC is associated with pregnancy outcomes following RC. Furthermore, GA at RC appears to be fair for predicting pregnancy outcomes, and this may help obstetricians identify a better timing to perform RC, predict the effectiveness of RC, and counsel patients with prolapsed amniotic membranes following prior cerclage.
Nevertheless, we acknowledge that there are some limitations to our study. Factors reflecting the severity of cervical insufficiency, such as the GA and indications of the primary cerclage of the patients, may affect the results of the study. However, the heterogeneity of the population and selection bias were not eliminated due to the retrospective design and the limited sample size. In addition, all the patients were of Chinese ethnicity; thus, the conclusions may not be applicable to other populations. Further prospective investigations, including a multicentre, large cohort, are needed in the future.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Review Board of Shengjing Hospital of China Medical University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
BC designed the study, collected the patients' information, and wrote the manuscript. YX and XN both participated in the collection of the patients' information. All authors approved the final manuscript.
Funding
This study was supported by the Scientific Research Fund of Liaoning Provincial Education Department (CN) (Award Number: FWZR2020009).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Yip SK, Fung HY, Fung TY. Emergency cervical cerclage: a study between duration of cerclage in situ with gestation at cerclage, herniation of forewater, and cervical dilatation at presentation. Eur J Obstet Gynecol Reprod Biol. (1998) 78:63–7. doi: 10.1016/S0301-2115(98)00023-2
2. Lipitz S, Libshitz A, Oelsner G, Kokia E, Goldenberg M, Mashiach S, et al. Outcome of second-trimester, emergency cervical cerclage in patients with no history of cervical incompetence. Am J Perinatol. (1996) 13:419–22. doi: 10.1055/s-2007-994381
3. Hatakeyama Y, Miura H, Sato A, Onodera Y, Sato N, Shimizu D, et al. Neutrophil elastase in amniotic fluid as a predictor of preterm birth after emergent cervical cerclage. Acta Obstet Gynecol Scand. (2016) 95:1136–42. doi: 10.1111/aogs.12928
4. Steenhaut P, Hubinont C, Bernard P, Debieve F. Retrospective comparison of perinatal outcomes following emergency cervical cerclage with or without prolapsed membranes. Int J Gynaecol Obstet. (2017) 137:260–4. doi: 10.1002/ijgo.12144
5. Kanbayashi S, Sato Y, Taga A, Satake Y, Emoto I, Maruyama S, et al. Positive vaginal culture at rescue cerclage predicts subsequent preterm delivery. J Matern Fetal Neonatal Med. (2018) 31:1161–5. doi: 10.1080/14767058.2017.1311313
6. Zhu LQ, Chen H, Chen LB, Liu YL, Tian JP, Wang YH, et al. Effects of emergency cervical cerclage on pregnancy outcome: a retrospective study of 158 cases. Med Sci Monit. (2015) 21:1395–401. doi: 10.12659/MSM.893244
7. Ehsanipoor RM, Seligman NS, Saccone G, Szymanski LM, Wissinger C, Werner EF, et al. Physical examination-indicated cerclage: a systematic review and meta-analysis. Obstet Gynecol. (2015) 126:125–35. doi: 10.1097/AOG.0000000000000850
8. Wierzchowska-Opoka M, Kimber-Trojnar Z, Leszczynska-Gorzelak B. Emergency cervical cerclage. J Clin Med. (2021) 10:1270. doi: 10.3390/jcm10061270
9. Delabaere A, Velemir L, Ughetto S, Accoceberry M, Niro J, Vendittelli F, et al. [Emergency cervical cerclage during mid-trimester of pregnancy: experience of clermont-ferrand]. Gynecol Obstet Fertil. (2011) 39:609–13. doi: 10.1016/j.gyobfe.2011.07.016
10. Chen Q, Chen G, Li N. Clinical effect of emergency cervical cerclage and elective cervical cerclage on pregnancy outcome in the cervical-incompetent pregnant women. Arch Gynecol Obstet. (2018) 297:401–7. doi: 10.1007/s00404-017-4602-7
11. Abo-Yaqoub S, Mohammed AB, Saleh H. The effect of second trimester emergency cervical cerclage on perinatal outcome. J Matern Fetal Neonatal Med. (2012) 25:1746–9. doi: 10.3109/14767058.2012.663822
12. Aydin T, Yucel B, Cinar E, Aksoy H, Aksoy U. An extraordinary complication of emergency cervical cerclage in a 20 weeks' gestation: cervicoisthmic rupture. J Obstet Gynaecol. (2015) 35:849–50. doi: 10.3109/01443615.2015.1013924
13. Ng KL, Kale AS, Gosavi AT. Ureterovaginal fistula after insertion of a mcdonald suture: case report and review of published reports. J Obstet Gynaecol Res. (2015) 41:1129–32. doi: 10.1111/jog.12671
14. Kosinska-Kaczynska K, Bomba-Opon D, Zygula A, Kaczynski B, Wegrzyn P, Wielgos M. Adjunctive pessary therapy after emergency cervical cerclage for cervical insufficiency with protruding fetal membranes in the second trimester of pregnancy: a novel modification of treatment. Biomed Res Int. (2015) 2015:185371. doi: 10.1155/2015/185371
15. Song JE, Lee KY, Jun HA. Repeat cerclage prolongs pregnancy in women with prolapsed membranes. Acta Obstet Gynecol Scand. (2011) 90:111–3. doi: 10.1111/j.1600-0412.2010.01006.x
16. Fox R, Holmes R, James M, Tuohy J, Wardle P. Serial transvaginal ultrasonography following McDonald cerclage and repeat suture insertion. Aust N Z J Obstet Gynaecol. (1998) 38:27–30. doi: 10.1111/j.1479-828X.1998.tb02952.x
17. Song JE, Lee KY, Son GH. Prognostic significance of neutrophil-to-lymphocyte ratio for repeat cerclage in women with prolapsed membranes. Biomed Res Int. (2018) 2018:1507398. doi: 10.1155/2018/1507398
18. Althuisius SM, Dekker GA, van Geijn HP, Bekedam DJ, Hummel P. Cervical incompetence prevention randomized cerclage trial (CIPRACT): study design and preliminary results. Am J Obstet Gynecol. (2000) 183:823–9. doi: 10.1067/mob.2000.108874
19. Baxter JK, Airoldi J, Berghella V. Short cervical length after history-indicated cerclage: is a reinforcing cerclage beneficial? Am J Obstet Gynecol. (2005) 193(3 Pt 2):1204–7. doi: 10.1016/j.ajog.2005.06.076
20. Contag SA, Woo J, Schwartz DB, Arrabal PP, O'Reilly G, Harper M. Reinforcing cerclage for a short cervix at follow-up after the primary cerclage procedure. J Matern Fetal Neonatal Med. (2016) 29:2423–7. doi: 10.3109/14767058.2015.1086740
21. Simcox R, Shennan A. Reinforcing cerclage in the prevention of preterm birth in women at high risk: a retrospective case-controlled study. Aust N Z J Obstet Gynaecol. (2012) 52:224–8. doi: 10.1111/j.1479-828X.2012.01440.x
22. McDonald IA. Suture of the cervix for inevitable miscarriage. J Obstet Gynaecol Br Emp. (1957) 64:346–50. doi: 10.1111/j.1471-0528.1957.tb02650.x
23. Song JE, Lee KY, Kim MY, Jun HA. Cervical funneling after cerclage in cervical incompetence as a predictor of pregnancy outcome. J Matern Fetal Neonatal Med. (2012) 25:147–50. doi: 10.3109/14767058.2011.565835
24. Azar ZF, Hakimi P, Ghojazadeh M, Ghatresamani F. Pre- and post-McDonald cerclage cervical length, width and funneling rate and their association with duration of pregnancy. Pak J Biol Sci. (2011) 14:502–6. doi: 10.3923/pjbs.2011.502.506
25. Pils S, Eppel W, Promberger R, Winter MP, Seemann R, Ott J. The predictive value of sequential cervical length screening in singleton pregnancies after cerclage: a retrospective cohort study. BMC Pregnancy Childbirth. (2016) 16:79. doi: 10.1186/s12884-016-0866-3
26. Diago Almela VJ, Martinez-Varea A, Perales-Puchalt A, Alonso-Diaz R, Perales A. Good prognosis of cerclage in cases of cervical insufficiency when intra-amniotic inflammation/infection is ruled out. J Matern Fetal Neonatal Med. (2015) 28:1563–8. doi: 10.3109/14767058.2014.960836
27. Endres LK, Wang EY. Interleukin-6 and tumor necrosis factor alpha as predictors of success after emergent cerclage. Am J Perinatol. (2004) 21:477–81. doi: 10.1055/s-2004-835965
28. Taghavi K, Gasparri ML, Bolla D, Surbek D. Predictors of cerclage failure in patients with singleton pregnancy undergoing prophylactic cervical cerclage. Arch Gynecol Obstet. (2018) 297:347–52. doi: 10.1007/s00404-017-4600-9
29. Fortner KB, Fitzpatrick CB, Grotegut CA, Swamy GK, Murtha AP, Heine RP, et al. Cervical dilation as a predictor of pregnancy outcome following emergency cerclage. J Matern Fetal Neonatal Med. (2012) 25:1884–8. doi: 10.3109/14767058.2012.668582
30. Namouz S, Porat S, Okun N, Windrim R, Farine D. Emergency cerclage: literature review. Obstet Gynecol Surv. (2013) 68:379–88. doi: 10.1097/OGX.0b013e31828737c7
31. Sheng JS, Schubert FP, Patil AS. Utility of volumetric assessment of cervical funneling to predict cerclage failure. J Matern Fetal Neonatal Med. (2017) 30:1066–71. doi: 10.1080/14767058.2016.1201470
Keywords: repeat cerclage, gestational age, prolapsed membranes, pregnancy outcome, retrospective analysis
Citation: Cai B, Xia Y and Na X (2022) Correlation Between Clinical Factors and Pregnancy Outcome Following Repeat Cerclage: A Retrospective Analysis of a Chinese Population. Front. Med. 9:846755. doi: 10.3389/fmed.2022.846755
Received: 31 December 2021; Accepted: 14 March 2022;
Published: 04 April 2022.
Edited by:
Doron Kabiri, Hebrew University Hadassah Medical School, IsraelReviewed by:
Maayan Ormianer, Hadassah Medical Center, IsraelDan Tirosh, Ben Gurion University of the Negev, Israel
Copyright © 2022 Cai, Xia and Na. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xinni Na, nxn_1990@163.com
 Benshuo Cai
Benshuo Cai Yajun Xia
Yajun Xia