- 1The First Department of Internal Medicine, School of Medicine, University of Occupational and Environmental Health, Japan, Kitakyushu, Japan
- 2Sato Clinic, Ebisu, Shibuya-ku, Tokyo, Japan
- 3Department of Rheumatology, Kawasaki Medical School, Kurashiki, Japan
- 4Department of Preventive Medicine and Community Health, University of Occupational and Environmental Health, Kitakyushu, Japan
- 5Department of Health Policy and Informatics, Tokyo Medical and Dental University Graduate School, Tokyo, Japan
Background: Short-term mortality and incidence of cerebrovascular and cardiovascular events (C-CVE) during hospitalization of patients with severe herpes zoster (HZ) have not been sufficiently investigated. We aimed to investigate short-term prognosis and incidence of C-CVE associated with HZ in hospitalized patients.
Methods: This retrospective cohort study from April 2016 to March 2018 included HZ inpatient cases selected from the Diagnosis Procedure Combination database—a Japanese nationwide inpatient database. HZ and C-CVE were diagnosed based on the 10th revision of the International Classification of Diseases and Injuries codes. The definition of primary exposure was that treatments were initiated within 7 days of admission, and antivirals were administered for ≥7 days. Main Outcomes were in-hospital deaths and C-CVE onset after hospitalization.
Results: Among 16,811,501 in-hospital cases registered from 1,208 hospitals, 29,054 cases with HZ were enrolled. The median age was 71.0 years, 15,202 cases (52.3%) were female, and the HZ types were the central nervous system (n=9,034), disseminated (n=3,051), and ophthalmicus (n=1,069) types. There were 301 (1.0%) in-hospital deaths and 385 (1.3%) post-hospitalization onset of C-CVE. The 30-day in-hospital survival rates with or without underlying disease were 96.8% and 98.5%, respectively. Age ≥75 years (hazard ratio [HR], 2.18; 95% confidence interval [CI], 1.55–3.05), liver cirrhosis or hepatic failure (HR, 5.93; 95% CI, 2.16–16.27), chronic kidney disease (HR, 1.82; 95% CI, 1.24–2.68), heart failure (HR, 1.65; 95% CI, 1.22–2.24), and old cerebrovascular events (HR, 1.92; 95% CI, 1.10–3.34) were associated with poor short-term prognosis. Age ≥75 years (odds ratio [OR], 1.70; 95% CI, 1.29–2.24), diabetes (OR, 1.50; 95% CI, 1.19–1.89), dyslipidemia (OR, 1.95; 95% CI, 1.51–2.51), hyperuricemia (OR, 1.63; 95% CI, 1.18–2.27), hypertension (OR, 1.76; 95% CI, 1.40–2.20), heart failure (OR, 1.84; 95% CI, 1.32–2.55), and glucocorticoid administration (OR, 1.59; 95% CI, 1.25–2.01) were associated with increased risks for in-hospital C-CVE onset.
Conclusions: The underlying diseases that could influence the short-term mortality of severe HZ were identified. Glucocorticoid is a possible risk factor for the in-hospital onset of C-CVE after severe HZ development.
Introduction
Herpes zoster (HZ) is an infection caused by the varicella-zoster virus (VZV). The risk of onset and severity increases in the elderly and in patients with underlying diseases that can lead to immunosuppression, such as connective tissue diseases (CTD) and malignancies (1–5). The incidence of HZ is increasing due to an aging society and the development of immunosuppressive therapy for autoimmune diseases, including CTD, and the occurrence of severe HZ may increase (6–8). Compared to other races, the incidence of HZ is higher in Japanese rheumatoid arthritis (RA) patients treated with a Janus kinase inhibitor (JAK-i), and the reasons have received attention (9, 10). Although it has been reported that mortality increases after the onset of HZ, the prognosis after the onset of HZ remains unclear due to substantial differences in survival rates among previous studies (11, 12). Moreover, information on the short-term prognosis of severe HZ and poor prognostic factors is limited. HZ is caused by various complications, including cerebrovascular and cardiovascular events (C-CVE) such as stroke and ischemic heart disease (IHD) (13). Reactivation of VZV can cause vasculitis, which can result in stroke and IHD (13, 14). The risk of developing C-CVE increases after HZ, and the risk of C-CVE may increase just after HZ onset (13, 15–18). There have been a few studies that have focused on patients hospitalized with severe HZ, which increases the incidence of death or C-CVE onset, and there is a paucity of studies that have examined short-term prognostic factors, the frequency of HZ-related C-CVE during hospitalization, and risk factors for developing C-CVE. Severe HZ increases the burden of medical costs for treating complications and sequelae (19), and the investigation of risk factors for severity and severe complications may be important public health information for taking preventive measures, including appropriate vaccination strategies against the onset and severe complications. We focused on patients with severe HZ that required hospitalization and investigated the short-term prognosis and prognostic factors and the incidence of C-CVE onset and risk factors of C-CVE onset after hospitalization for HZ treatment using the national administrative inpatient database in Japan.
Materials and Methods
Study Design
This was a retrospective cohort study using the Diagnosis Procedure Combination (DPC) database which is a nationwide inpatient database in Japan.
Setting
Data were collected by the DPC research group, funded by the Ministry of Health, Labour, and Welfare, Japan. In the study period, 1,208 hospitals participated in the survey of the DPC research group and provided their data for research purpose (20). The database contains patient information and detailed procedures for the Japanese national insurance system (21, 22). Patient information recorded in the DPC database includes diagnosis based on the 10th revision of the International Classification of Diseases and Injuries (ICD-10) codes at the time of admission, comorbidities, and complications after admission. The DPC database also contains information on administered drugs, blood products used, and outcomes at discharge (23, 24).
Participant Selection
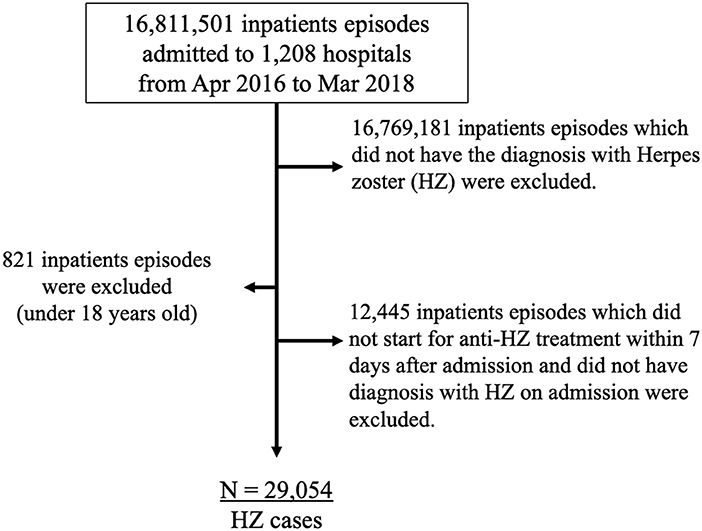
Cases were enrolled from April 1, 2016 to March 31, 2018. First, 41,499 in-hospital cases over 18 years old who have a diagnosis of HZ and treated with HZ-specific antivirals (acyclovir, famciclovir, valaciclovir, amenamevir, or vidarabine) for 7 days or more were extracted from the DPC database among a total of 16,811,501 inpatient cases from 1,208 hospitals in the DPC database. Second, of the 41,499 cases, 12,445 cases that did not start a specific antiviral treatment within 7 days after admission and did not have a diagnosis of HZ on admission were excluded. After the exclusion, there were a total of 29,054 cases diagnosed with HZ included in the study (Figure 1).
Definition of HZ and Underlying Diseases
The principal diagnosis of HZ was based on the ICD-10 code B02. The four types of HZ were classified as follows: central nervous system (CNS) (B02.0, B02.1), disseminated (B02.7), ophthalmicus (B02.3), and others (B02.8 and B02.9). It was expected that using the ICD-10 codes alone would identify patients who were not treated for HZ as well as those suspected with HZ who initiated treatment. To ensure robust diagnosis, we enrolled cases who received HZ-specific antivirals for at least 7 days, the standard duration of HZ treatment (25, 26). The principal diagnosis of underlying diseases was recorded using the following ICD-10 codes: malignancies, C00–C98; solid cancer, C00–C80, C97; malignant lymphoma and hematopoietic malignancies, C81–C96; human immunodeficiency virus disease, B20–B24; immunodeficiencies, D80–D84; Transplanted organ and tissue status, Z94; disorders of the thyroid gland, E05.1, E06.3; diabetes mellitus (DM); E10–E14; dyslipidemia, E78; hyperuricemia, E79.0, M10; depressive disorder, F31–F34; demyelinating diseases, G35–G37; chronic obstructive pulmonary disease (COPD), J44; asthma, J45; interstitial lung disease (ILD), J84, J99.0, J99.1; hypertension (HT) and HT-related diseases, I10–I15; heart failure (HF), I11.0, I13.0, I50, I97.1; chronic ischemic heart disease (cIHD), I25; sequelae of cerebrovascular disease (CVD), I69; inflammatory bowel diseases, K50 and K51; autoimmune hepatitis, K75.4; cirrhosis and hepatic failure, K70.3, K70.4, K71.7, K72, K74; chronic viral hepatitis, B18; CTD, L40.5, M05–M07, M30–M35, M45, M94.1 (*M07.4–M07.6, M30.2, M30.3, M31.5, M33.0, M34.2, and M35.3–M35.7 were excluded), RA; M05–M06, M31.5 (*M06.1 was excluded); systemic vasculitis, M30, M31 (*M30.2, M30.3, M31.5 were excluded); systemic lupus erythematosus, M32; others, L40.5, M06.1, M07, M33–35, M94.1 (*M07.4–M07.6, M33.0, M34.2, and M35.3–M35.7 were excluded); chronic kidney disease (CKD), N18; glomerular diseases, N00, N01, N03–N05, and N08.
Study Outcomes
The primary outcome was overall in-hospital survival at 30 and 60 days after the initiation of treatment for HZ. The secondary outcome was in-hospital C-CVE onset after admission for HZ treatment. The diagnosis of C-CVE was based on the ICD-10 codes as follows: cerebrovascular diseases (I60–I67) and cardiovascular diseases (I20–I24). The definition of the secondary outcome was extracted from the post-hospitalization onset of secondary diseases recorded in the DPC database. The study also aimed to investigate the prognostic factors associated with in-hospital mortality and risk factors for C-CVE onset associated with HZ after admission.
Statistical Analysis
Categorical variables are presented as numbers (%), and continuous variables are presented as medians with interquartile ranges (IQR) or numbers with percentages (%). An independent sample, the Mann–Whitney test, was employed to evaluate non-normally distributed data for comparison between the two groups. Classification data number (percentage) were aggregated. Chi-square or Fisher's exact test was performed. The log-rank test was used to compare the survival rates among the groups. Univariable Cox regression analysis and logistic regression analysis were used to screen for potential confounders associated with in-hospital mortality and in-hospital C-CVE onset after admission for HZ treatment. Associations among covariates and risk of in-hospital mortality were evaluated using multivariable Cox proportional hazards regression analysis, and associations between covariates and risk of in-hospital C-CVE onset after admission for HZ treatment were evaluated using multivariable logistic regression analysis. Hazard ratios (HRs) and odds ratios (ORs) with 95% confidence intervals (CIs) were determined after adjusting for potential confounders. Multivariable Cox regression analysis and logistic regression analysis were used to evaluate independent risk factors for in-hospital mortality and in-hospital C-CVE onset after admission for HZ treatment. The underlying diseases and confounding factors that are risk factors for HZ reported in previous studies were preferentially selected as explanatory variables for multivariable analysis using the Cox proportional hazards regression (2, 27).
Previously reported risk factors for C-CVE were preferentially selected as explanatory variables for multivariable logistic regression analysis (28, 29). We assumed that continuous variables (body mass index (BMI) and Brinkman index) were missing at random. Variables with missing values were not included in the multivariable analysis because obesity (BMI ≥ 25) and smoking history could be considered not to be confounding factors based on the results of univariable analysis. All tests were two-tailed, and the statistical significance was set at p < 0.05. All statistical analyses were performed using the R software package (version 4.0.0, R Foundation) (30).
Results
Patient Characteristics
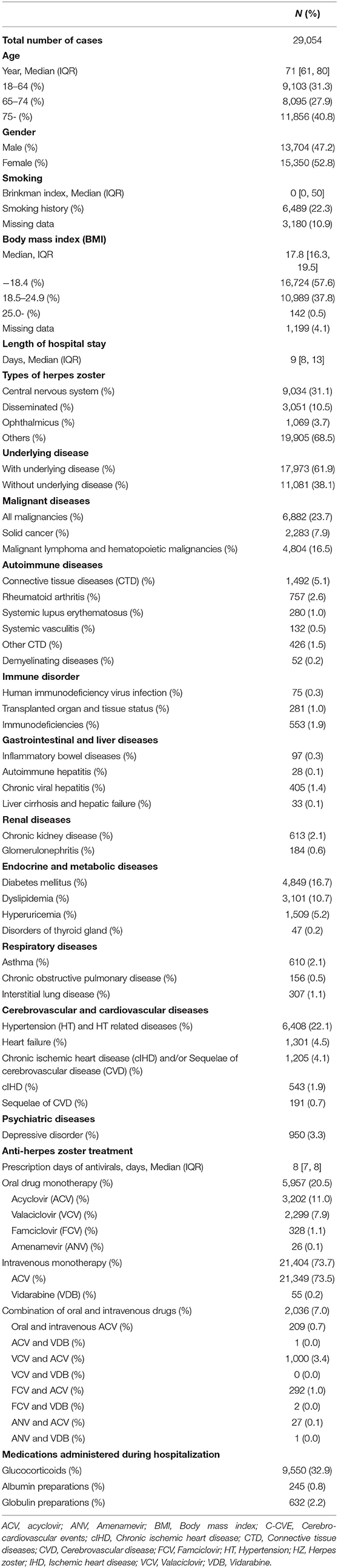
Baseline characteristics of the study cohort are presented in Table 1. The median age was 71 years, and 15,350 cases (52.8%) were women. The cohort comprised 9,103 (31.3%), 8,095 (27.9%), and 11,856 (40.8%) cases aged 18–64 years, 65–74 years (pre-old age), and ≥75 years (old age) of age, categories based on the Japanese Gerontological Society and the Japan Geriatrics Society (31). A total of 17,973 (51.9%) cases had underlying diseases. Glucocorticoid (GC) was administered during hospitalization in 9,550 (32.9%) cases. The median length of hospital stay after the initiation of HZ treatment was 8 days. Based on the severity of HZ, most cases (21,061 cases [72.5%]) were treated with intravenous antivirals (mostly acyclovir). The median length of antiviral administration was 8 days.
Study Outcomes
Survival Rates and Prognostic Factors
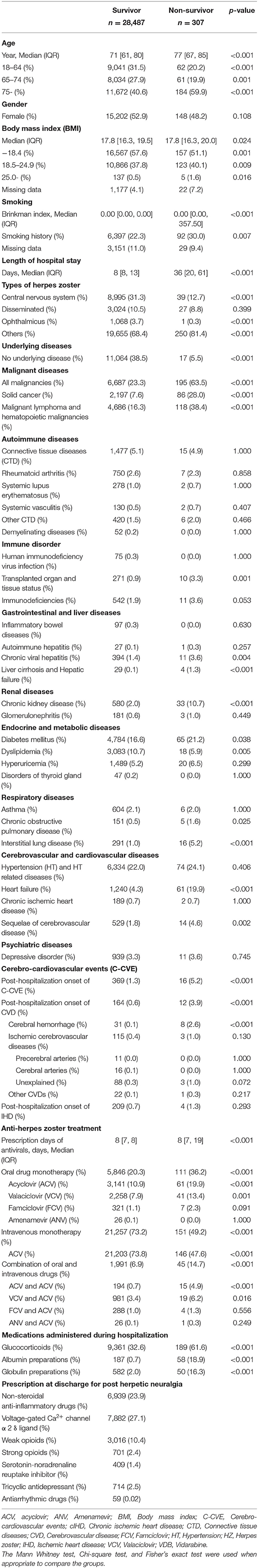
There were 307 in-hospital deaths (1.1%) in the study cohort. The overall survival rates at 30 and 60 days were 97.0% and 87.7%, respectively. The estimated 30- and 60-day survival rates after the start of HZ treatment for the groups with or without underlying disease were 96.8% (95% confidence interval [CI], 96.0–97.3)/86.9% (95% CI, 84.6–88.8), and 98.5% (95% CI, 96.8–99.3) and 94.3% (95% CI, 87.4–97.5), respectively (p<0.001) (Figure 2). The 30- and 60- day survival rates for each type of HZ are as follows: overall (30-day in-hospital survival rate, 97.0%; [95% CI, 96.3–97.5] and 60-day in-hospital survival rate, 87.7%; [95% CI, 85.7–89.5]), CNS (30-day in-hospital survival rate, 98.0%; [95% CI, 96.7–97.3]) and 60-day in-hospital survival rate, 88.3%; [95% CI, 85.3–89.5]), disseminated (30-day in-hospital survival rate, 96.6%; [95% CI, 93.4–98.3] and 60-day in-hospital survival rate, 85.3%; [95% CI, 75.6–91.3]), ophthalmicus (30-day in-hospital survival rate, 100%; [95% CI, NA–NA] and 60-day in-hospital survival rate, 100%; [95% CI, NA–NA]), and other (30-day in-hospital survival rate, 96.9%; [95% CI, 96.2–97.5 and 60-day in-hospital survival rate, 88.0%; [95% CI, 85.7–89.9]). The baseline characteristics of the survivor and non-survivor groups are summarized in Table 2. Compared with survivors, non-survivors were significantly older with higher rates of female sex, obesity, smoking history, malignancies, CKD, DM, chronic viral hepatitis, liver cirrhosis and hepatic failure, COPD, ILD, HF, cIHD and sequalae of CVD (old cerebrovascular events), GC administration, and albumin preparation administration. Comparison of the treatment approaches between the two groups revealed that there were more patients receiving oral antivirals and the combination of oral and intravenous antivirals, immunoglobulin, and albumin preparations, in the non-survivor group than in the survivor group. We analyzed the poor prognostic factors associated with in-hospital mortality due to HZ using the Cox proportional hazards regression model (Figure 3). By multivariable analysis, over 75 years of age (hazard ratio [HR], 2.17; [95% CI, 1.53–3.06, p < 0.001]), liver cirrhosis and hepatic failure (HR, 6.84; [95% CI, 2.17–21.63, p = 0.001]), CKD (HR, 1.88; [95% CI, 1.27–2.78, p = 0.002]) and HF (HR, 1.70; 95% CI, 1.24–2.34, p = 0.001), and sequalae of CVD (HR, 1.96; [95% CI, 1.08–3.56, p = 0.028]) were poor prognostic factors. All results of the Cox hazard regression analysis are shown in Supplementary Table 1.
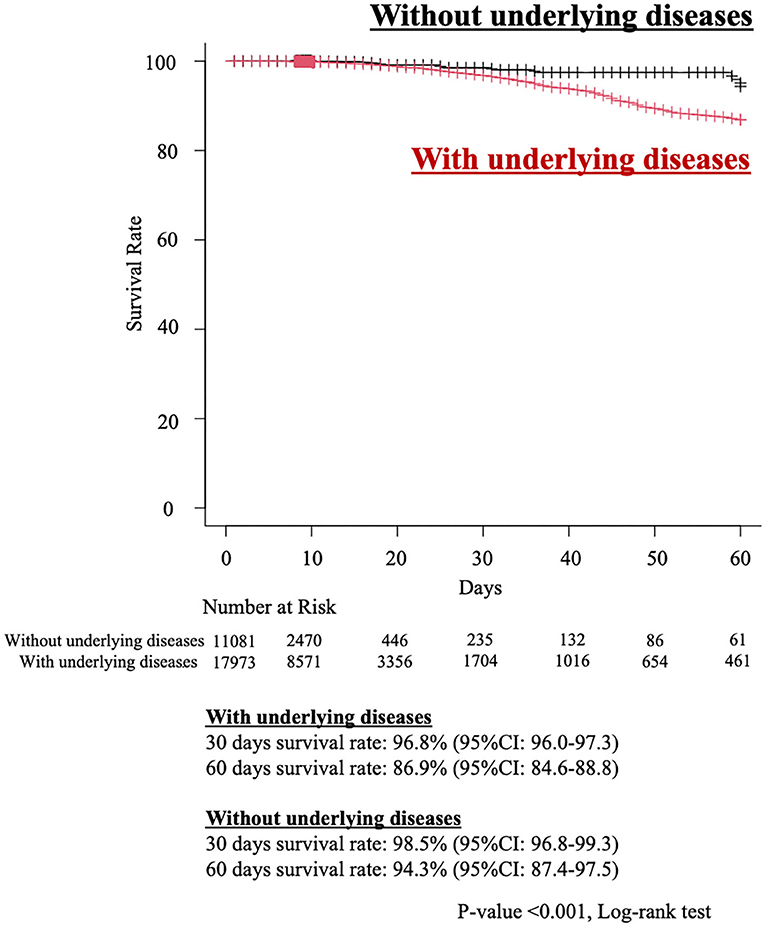
Figure 2. Estimated Kaplan–Meier overall survival curve of herpes zoster patients with or without underlying diseases. 95% CI, 95 percent confidence interval.
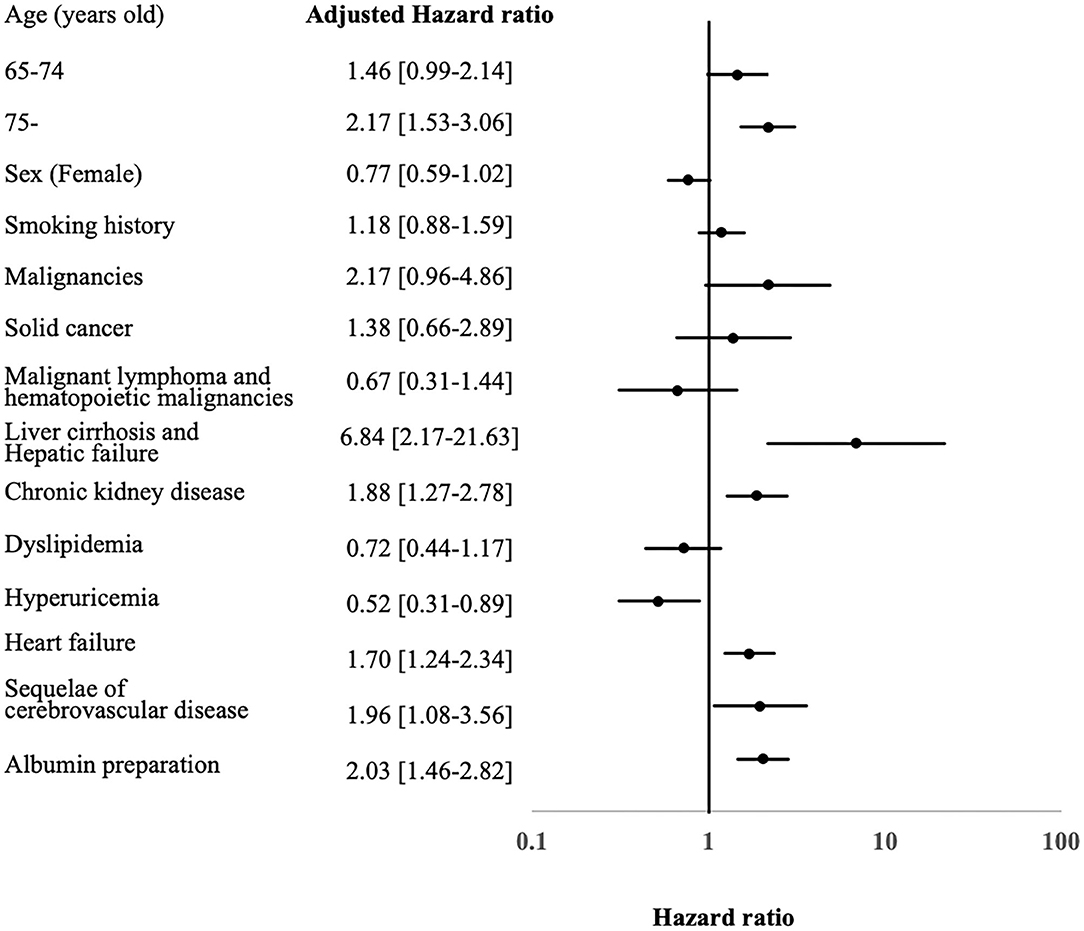
Figure 3. Predictors for poor prognosis of hospitalized herpes zoster cases. aHR, adjusted hazard ratio; C-CVE, cerebro-cardiovascular events; 95% CI, 95 percent confidence interval.
C-CVE In-hospital Onset Rates and Risk Factors
Three hundred and eighty five cases (1.3%) experienced in-hospital C-CVE onset after hospitalization. The baseline characteristics of the non-C-CVE onset and C-CVE onset groups are summarized in Table 3. Compared with the non-C-CVE onset group, the C-CVE onset group were significantly older and had significantly higher rates of death, male, smoking history, malignant lymphoma and hematopoietic malignancies, transplanted organ and tissue status, CKD, DM, dyslipidemia, hyperuricemia, asthma, ILD, HT, HF, cIHD, sequalae of CVD, transplanted organ and tissue status, and GC administration during hospitalization. Comparison of treatment approaches between the two groups revealed that there were more patients receiving oral antiviral monotherapy, immunoglobulin, and albumin preparation in the C-CVE onset group than in the non-C-CVE onset group. We analyzed the risk factors associated with in-hospital C-CVE onset after hospitalization for HZ treatment. By multivariable logistic regression analysis, older age ≥ 75 years (odds ratio [OR], 1.70; [95% CI, 1.30–2.24, p < 0.001]), DM (OR, 1.50; [95% CI, 1.19–2.49, p = 0.001]), hyperuricemia (OR, 1.65; [95% CI, 1.19–2.30]), HT (OR, 1.76; [95% CI, 1.41–2.30, p < 0.001]), HF (OR, 1.85; [95% CI, 1.33–2.57, p < 0.001]), and GC administration (OR, 1.63; [95% CI, 1.30–2.05, p < 0.001]) were identified as risk factors for in-hospital C-CVE onset (Figure 4). The results of the logistic regression analysis are shown in Supplementary Table 2.
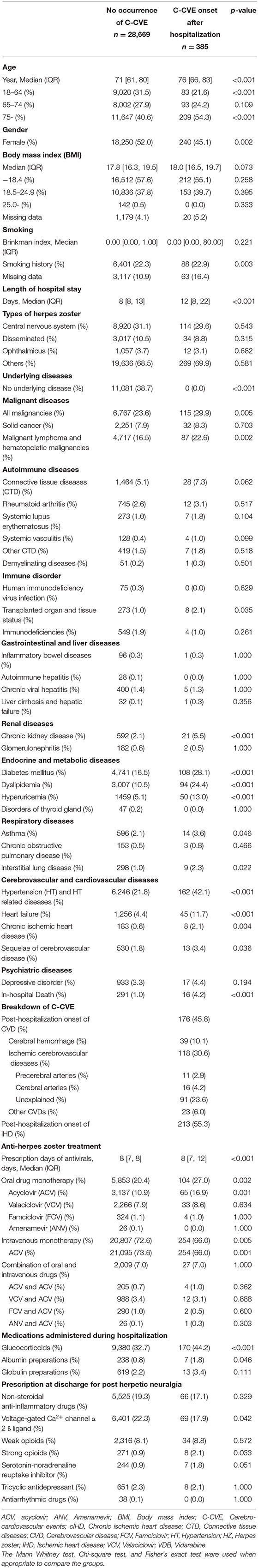
Table 3. Baseline clinical characteristics between C-CVE onset cases and no occurrence of C-CVE cases.

Figure 4. Predictors for risk factors of C-CVE onset after hospitalization. aOR, adjusted odds ratio; C-CVE, cerebro-cardiovascular events; 95% CI, 95 percent confidence interval.
Discussion
Brief Summary of This Study
We investigated short-term in-hospital mortality and incidence of C-CVE in 29,054 hospitalized cases with HZ and analyzed prognostic factors and risk factors for C-CVE onset after HZ. Over 75 years of age, cirrhosis, liver failure, CKD, HF, and sequelae of CVD were identified as short-term prognostic factors. Traditional C-CVE risk factors such as age ≥75 years, DM, dyslipidemia, hyperuricemia, HT, and HF were identified as risk factors for C-CVE development after hospitalization for HZ treatment, and GC administration was also identified as a new C-CVE risk factor.
Interpretation
The in-hospital mortality for HZ was similar to that reported in the study by Esteban-Vasallo et al. from Spain, conducted between 2003 and 2013. The study included data from the years before the widespread use of recombinant zoster vaccine (RZV), biologics, and JAK-I (32). Since there was no substantial discrepancy in the in-hospital mortality in our study, conducted using data from 2016 to 2018, the period when immunosuppressive therapy was developed, it is conceivable that biologics and JAK-i could have an impact on the development of HZ but might not have a significant impact on the severity of HZ. The incidence of HZ is higher in Japanese RA patients receiving JAK-i, but there may not be as much racial difference in mortality after HZ onset as HZ incidence in the unvaccinated population (5, 10, 33). Cirrhosis and liver failure, CKD, HF, and old cerebrovascular events, identified as risk factors for in-hospital mortality in this study, are also considered to be risk factors for severity of other viral infections such as influenza (34). HZ vaccines have been reported to be effective in preventing the onset and severity of HZ (35). For the prevention of severe conditions, the priority of vaccination might be based on the same criteria as that for vaccinations against other viral infections such as influenza because HZ is a common disease. It is important to address the prevention of HZ because if the onset and severity of HZ can be prevented, the complications of C-CVE might also be reduced. However, there are still many unclear points, such as the duration of the vaccine effects, therefore, further studies are needed on the timing of vaccination and the selection of priority vaccination targets.
Even in severe HZ, it was suggested that an inflammatory response (vasculitis) to the virus may occur from the acute stage after HZ onset, leading to the development of C-CVE. Inflammatory reactions in the artery and endothelial dysfunction are involved in the development of C-CVE (36, 37). Therefore, patients who have an underlying disease with arteriosclerosis and/or endothelial dysfunction such as diabetes may need to be especially attentive to the development of C-CVE after HZ. In addition to risk factors such as DM and HT, GC administration was newly identified as a risk factor for C-CVE onset after onset of HZ. GC has been previously reported to be a risk factor for C-CVE in CTD (38–40). GC administration may be used as adjunctive therapy for Ramsay-Hunt syndrome or for pain relief and prevention of sequelae of HZ, but administration of GC should be avoided because it may increase the risk of C-CVE (41). Since CTD, which requires a relatively frequent administration of GC, was not identified as a risk factor for C-CVE onset, it is possible that GC administration itself may lead to the C-CVE risk after HZ onset. In patients with a disease which is needed for long-term GC administration such as CTD, it would be desirable to reduce or avoid GC administration as much as possible to prevent HZ development and C-CVE onset after HZ.
Strengths of This Study
The strength of this study lies in the large sample size. We analyzed over 29,000 hospitalized HZ cases, the largest numbers ever studied. In previous studies, it could have been difficult to detect HZ-associated deaths and C-CVE onset associated with HZ during hospitalization due to the relatively low patient numbers. We were able to detect more than 300 cases of both in-hospital death and C-CVE onset, which allowed us to conduct analyses on short-term prognostic factors and risk factors for C-CVE onset.
In addition, the DPC database we used covers many acute care hospitals, including advanced care hospitals such as university hospitals, contributing to the generalization and comprehensiveness of the analysis results (42). Another strength of this study is that it covers a relatively small number of underlying diseases, such as CTD. Because relatively rare underlying diseases were included in the analysis, a more comprehensive analysis was possible.
Limitations
This study has several limitations. First, laboratory test results, imaging findings, and medical records were not available from the DPC database. Therefore, the diagnosis may uncertain. However, the diagnostic accuracy of DPC is moderate or high (43, 44), and previous studies using database have also used the ICD codes (25, 32). We used information on antivirals for HZ to improve diagnostic accuracy. Since antivirals for HZ are not administered for other infections, patients administered with antivirals for more than a certain period are more likely to be true HZ. Second, the DPC database contains no information before hospitalization, such as prescription drugs or HZ vaccination, and post-discharge outcomes. Since there is a possibility that the risk of HZ-related death and C-CVE may increase after discharge from the hospital, a long-term investigation should be conducted. The effect of vaccination on this study could be limited. Few people were vaccinated at the time of this analysis, because ZVL (zoster vaccine live) and RZV were approved in 2016 and 2018, respectively, for those over 50 years in Japan. ZVL is contraindicated during immunosuppressive and anticancer chemotherapy in Japan. Many patients with underlying diseases, such as CTD or malignancies, were not vaccinated. Future studies should examine any change in mortality and C-CVE incidence with vaccination. These limitations can be overcome by matching DPC data with the National Database of Health Insurance Claims data, which contain information on prescription drugs in outpatient settings. However, there are many institutional and technical problems in linking the two databases. If institutional changes and technological innovations permit us to link the databases before and during hospitalization, we would like to investigate the linking of individuals' data.
Conclusion
Aggressive HZ prevention, including vaccination, should be considered for patients older than 75 years and for patients with poor prognostic factors. In addition to the conventional C-CVE risk factors, GC might be a risk factor for the development of C-CVE after severe HZ onset.
Data Availability Statement
YI, KT, and KF had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. In this study, we used the DPC data provided by acute care hospitals in Japan to the DPC Research Institute. We conducted our study using this DPC database at the University of Occupational and Environmental Health, Japan. This database can only be accessed for research purpose.
Ethics Statement
Informed consent was waived for all patients included in this retrospective cohort study, and all information extracted was anonymized. The Institutional Review Board of the University of Occupational and Environmental Health, Japan approved this study (approval code: R2-007). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
YI, KT, and KN: conceptualization and design, acquisition, analysis, and interpretation of data. KF: acquisition, analysis and interpretation of data. YI: drafting of the manuscript and statistical analysis. KN, SN, SM, and YT: supervision. All authors: critical revision of the manuscript for important intellectual content. All authors contributed to the article and approved the submitted version.
Conflict of Interest
KN has received speaking fees from Sanofi, AbbVie, Eisai, Eli Lilly, Chugai, Pfizer, GSK, Astellas, UCB, and Mitsubishi-Tanabe, and research grants from Boehringer Ingelheim, Chugai, Eisai, AbbVie, Asahi Kasei, Ayumi, Eli Lilly, and UCB. SN has received consulting fees, speaking fees, and/or honoraria from Bristol-Myers, Pfizer, GlaxoSmithKline, Sanofi, Astellas, Asahi-Kasei, and Boehringer Ingelheim and has received research grants from Mitsubishi-Tanabe and Novartis. YT has received speaking fees and/or honoraria from Gilead, Abbvie, Behringer-Ingelheim, Eli Lilly, Mitsubishi-Tanabe, Chugai, Amgen, YL Biologics, Eisai, Astellas, Bristol-Myers, and Astra-Zeneca; received research grants from Asahi-Kasei, Abbvie, Chugai, Mitsubishi-Tanabe, Eisai, Takeda, Corrona, Daiichi-Sankyo, Kowa, and Behringer-Ingelheim; and received consultant fees from Eli Lilly, Daiichi-Sankyo, Taisho, Ayumi, Sanofi, GSK, and Abbvie.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.843809/full#supplementary-material
References
1. Weinberg JM. Herpes zoster: epidemiology, natural history, and common complications. J Am Acad Dermatol. (2007) 57(6 Suppl.):S130–5. doi: 10.1016/j.jaad.2007.08.046
2. Imafuku S, Dormal G, Goto Y, Jégou C, Rosillon D, Matsuki T. Risk of herpes zoster in the Japanese population with immunocompromising and chronic disease conditions: results from a claims database cohort study, from 2005 to 2014. J Dermatol. (2020) 47:236–44. doi: 10.1111/1346-8138.15214
3. Sato K, Adachi K, Nakamura H, Asano K, Watanabe A, Adachi R, et al. Burden of herpes zoster and postherpetic neuralgia in Japanese adults 60 years of age or older: results from an observational, prospective, physician practice-based cohort study. J Dermatol. (2017) 44:414–22. doi: 10.1111/1346-8138.13639
4. Arvin AM GD. Varicella-Zoster Virus. 6th ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins (2013).
5. Yamaoka K, Tanaka Y, Kameda H, Khan N, Sasaki N, Harigai M, et al. The safety profile of upadacitinib in patients with rheumatoid arthritis in Japan. Drug Saf. (2021) 44:711–22. doi: 10.1007/s40264-021-01067-x
6. Winthrop KL, Curtis JR, Lindsey S, Tanaka Y, Yamaoka K, Valdez H, et al. Herpes zoster and tofacitinib: clinical outcomes and the risk of concomitant therapy. Arthritis Rheumatol. (2017) 69:1960–8. doi: 10.1002/art.40189
7. Redeker I, Albrecht K, Kekow J, Burmester GR, Braun J, Schäfer M, et al. Risk of herpes zoster (shingles) in patients with rheumatoid arthritis under biologic, targeted synthetic and conventional synthetic DMARD treatment: data from the German RABBIT register. Ann Rheum Dis. (2022) 81:41–47.
8. Toyama N, Shiraki K, Dermatologists SotMP. Epidemiology of herpes zoster and its relationship to varicella in Japan: a 10-year survey of 48,388 herpes zoster cases in Miyazaki prefecture. J Med Virol. (2009) 81:2053–8. doi: 10.1002/jmv.21599
9. Tanaka Y, Tummala R. Anifrolumab, a monoclonal antibody to the type I interferon receptor subunit 1, for the treatment of systemic lupus erythematosus: an overview from clinical trials. Mod Rheumatol. (2021) 31:1–12. doi: 10.1080/14397595.2020.1812201
10. Winthrop KL, Yamanaka H, Valdez H, Mortensen E, Chew R, Krishnaswami S, et al. Herpes zoster and tofacitinib therapy in patients with rheumatoid arthritis. Arthritis Rheumatol. (2014) 66:2675–84. doi: 10.1002/art.38745
11. Bardach AE, Palermo C, Alconada T, Sandoval M, Balan DJ, Nieto Guevara J, et al. Herpes zoster epidemiology in Latin America: a systematic review and meta-analysis. PLoS ONE. (2021) 16:e0255877. doi: 10.1371/journal.pone.0255877
12. Bricout H, Haugh M, Olatunde O, Prieto RG. Herpes zoster-associated mortality in Europe: a systematic review. BMC Public Health. (2015) 15:466. doi: 10.1186/s12889-015-1753-y
13. Minassian C, Thomas SL, Smeeth L, Douglas I, Brauer R, Langan SM. Acute cardiovascular events after herpes zoster: a self-controlled case series analysis in vaccinated and unvaccinated older residents of the United States. PLoS Med. (2015) 12:e1001919. doi: 10.1371/journal.pmed.1001919
14. Gilden D, Cohrs RJ, Mahalingam R, Nagel MA. Varicella zoster virus vasculopathies: diverse clinical manifestations, laboratory features, pathogenesis, and treatment. Lancet Neurol. (2009) 8:731–40. doi: 10.1016/S1474-4422(09)70134-6
15. Patterson BJ, Rausch DA, Irwin DE, Liang M, Yan S, Yawn BP. Analysis of vascular event risk after herpes zoster from 2007 to 2014. US Insurance Claims Data. Mayo Clin Proc. (2019) 94:763–75. doi: 10.1016/j.mayocp.2018.12.025
16. Zhang Y, Luo G, Huang Y, Yu Q, Wang L, Li K. Risk of stroke/transient ischemic attack or myocardial infarction with herpes zoster: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. (2017) 26:1807–16. doi: 10.1016/j.jstrokecerebrovasdis.2017.04.013
17. Seo HM, Cha MJ, Han JH, Han K, Park SH, Bang CH, et al. Reciprocal relationship between herpes zoster and cardiovascular diseases: a nationwide population-based case-control study in Korea. J Dermatol. (2018) 45:1312–8. doi: 10.1111/1346-8138.14597
18. Breuer J, Pacou M, Gauthier A, Brown MM. Herpes zoster as a risk factor for stroke and TIA: a retrospective cohort study in the UK. Neurology. (2014) 82:206–12. doi: 10.1212/WNL.0000000000000038
19. Gil A, Gil R, Alvaro A, San Martín M, González A. Burden of herpes zoster requiring hospitalization in Spain during a seven-year period (1998-2004). BMC Infect Dis. (2009) 9:55. doi: 10.1186/1471-2334-9-55
20. Muramatsu K, Fujino Y, Kubo T, Otani M, Fushimi K, Matsuda S. Efficacy of Antimicrobial Catheters for Prevention of Catheter-Associated Urinary Tract Infection in Acute Cerebral Infarction. J Epidemiol. (2018) 28:54–8. doi: 10.2188/jea.JE20170022
21. Yasunaga H, Horiguchi H, Kuwabara K, Hashimoto H, Matsuda S. Clinical features of bowel anisakiasis in Japan. Am J Trop Med Hyg. (2010) 83:104–5. doi: 10.4269/ajtmh.2010.09-0780
22. Matsuda S. Development of case mix based evaluation system in Japan. Jpn Hosp. (2016) 2016:35–44.
23. Isogai T, Yasunaga H, Matsui H, Tanaka H, Hisagi M, Fushimi K. Factors affecting in-hospital mortality and likelihood of undergoing surgical resection in patients with primary cardiac tumors. J Cardiol. (2017) 69:287–92. doi: 10.1016/j.jjcc.2016.05.008
24. Iwagami M, Yasunaga H, Doi K, Horiguchi H, Fushimi K, Matsubara T, et al. Postoperative polymyxin B hemoperfusion and mortality in patients with abdominal septic shock: a propensity-matched analysis. Crit Care Med. (2014) 42:1187–93. doi: 10.1097/CCM.0000000000000150
25. Ishikawa Y, Nakano K, Tokutsu K, Miyata H, Fujino Y, Matsuda S, et al. Estimation of treatment and prognostic factors of pneumocystis pneumonia in patients with connective tissue diseases. RMD Open. (2021) 7:1508. doi: 10.1136/rmdopen-2020-001508
26. Dworkin RH, Johnson RW, Breuer J, Gnann JW, Levin MJ, Backonja M, et al. Recommendations for the management of herpes zoster. Clin Infect Dis. (2007) 44 Suppl 1:S1–26. doi: 10.1086/510206
27. Hansen MA, Samannodi MS, Castelblanco RL, Hasbun R. Clinical epidemiology, risk factors, and outcomes of encephalitis in older adults. Clin Infect Dis. (2020) 70:2377–85. doi: 10.1093/cid/ciz635
28. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. (2019). ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. (2019). 140:e596–646. doi: 10.1161/CIR.0000000000000725
29. Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, et al. Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association. Stroke. (2021) 52:e364–467. doi: 10.1161/STR.0000000000000375
30. Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant. (2013) 48:452–8. doi: 10.1038/bmt.2012.244
31. Ouchi Y, Rakugi H, Arai H, Akishita M, Ito H, Toba K, et al. Redefining the elderly as aged 75 years and older: Proposal from the Joint Committee of Japan Gerontological Society and the Japan Geriatrics Society. Geriatr Gerontol Int. (2017) 17:1045–7. doi: 10.1111/ggi.13118
32. Esteban-Vasallo MD, Domínguez-Berjón MF, Gil de Miguel Á, Astray-Mochales J, Blanco-Ancos LM, Gil-Prieto R. Characteristics of herpes zoster-associated hospitalizations in Madrid (SPAIN) before vaccine availability. J Infect. (2016) 72:70–9. doi: 10.1016/j.jinf.2015.10.003
33. Curtis JR, Xie F, Yun H, Bernatsky S, Winthrop KL. Real-world comparative risks of herpes virus infections into facitinib and biologic-treated patients with rheumatoid arthritis. Ann Rheum Dis. (2016) 75:1843–7. doi: 10.1136/annrheumdis-2016-209131
34. Grohskopf LA, Alyanak E, Ferdinands JM, Broder KR, Blanton LH, Talbot HK, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the advisory committee on immunization practices, United States, 2021-22 influenza season. MMWR Recomm Rep. (2021) 70:1–28. doi: 10.15585/mmwr.rr7005a1
35. Harbecke R, Cohen JI, Oxman MN. Herpes zoster vaccines. J Infect Dis. (2021) 224:S429–42. doi: 10.1093/infdis/jiab387
36. Tuttolomondo A, Pinto A, Corrao S, Di Raimondo D, Fernandez P, Di Sciacca R, et al. Immuno-inflammatory and thrombotic/fibrinolytic variables associated with acute ischemic stroke diagnosis. Atherosclerosis. (2009) 203:503–8. doi: 10.1016/j.atherosclerosis.2008.06.030
37. Della Corte V, Tuttolomondo A, Pecoraro R, Di Raimondo D, Vassallo V, Pinto A. Inflammation, endothelial dysfunction and arterial stiffness as therapeutic targets in cardiovascular medicine. Curr Pharm Des. (2016) 22:4658–68. doi: 10.2174/1381612822666160510124801
38. Persson R, Hagberg KW, Qian Y, Vasilakis-Scaramozza C, Jick S. The risk of myocardial infarction, stroke, and revascularization among patients with psoriasis treated with apremilast compared with biologics and disease-modifying antirheumatic drugs: a cohort study in the US MarketScan database. J Am Acad Dermatol. (2020) 83:271–4. doi: 10.1016/j.jaad.2020.03.043
39. Ozen G, Pedro S, Michaud K. The risk of cardiovascular events associated with disease-modifying antirheumatic drugs in rheumatoid arthritis. J Rheumatol. (2021) 48:648–55. doi: 10.3899/jrheum.200265
40. Bessant R, Duncan R, Ambler G, Swanton J, Isenberg DA, Gordon C, et al. Prevalence of conventional and lupus-specific risk factors for cardiovascularpa disease in patients with systemic lupus erythematosus: a case-control study. Arthritis Rheum. (2006) 55:892–9. doi: 10.1002/art.22343
41. Uscategui T, Dorée C, Chamberlain IJ, Burton MJ. Antiviral therapy for Ramsay Hunt syndrome (herpes zoster oticus with facial palsy) in adults. Cochrane Database Syst Rev. (2008) 2008:CD006851. doi: 10.1002/14651858.CD006851.pub2
42. Yasunaga H MH, Horiguchi H, Fushimi K, Matsuda S. Clinical epidemiology and health services research using the diagnosis procedure combination database in Japan. Asia Pacific J Dis Manage. (2013) 7:19–24. doi: 10.7223/apjdm.7.19
43. Yamana H, Moriwaki M, Horiguchi H, Kodan M, Fushimi K, Yasunaga H. Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J Epidemiol. (2017) 27:476–82. doi: 10.1016/j.je.2016.09.009
Keywords: herpes zoster (HZ), cerebrovascular event, glucocorticoids, DPC (Diagnosis Procedure Combination), nationwide administrative database, cardiovascular event
Citation: Ishikawa Y, Nakano K, Tokutsu K, Nakayamada S, Matsuda S, Fushimi K and Tanaka Y (2022) Short-Term Prognostic Factors in Hospitalized Herpes Zoster Patients and Its Associated Cerebro-Cardiovascular Events: A Nationwide Retrospective Cohort in Japan. Front. Med. 9:843809. doi: 10.3389/fmed.2022.843809
Received: 27 December 2021; Accepted: 28 January 2022;
Published: 04 March 2022.
Edited by:
Alessandra Casuccio, University of Palermo, ItalyReviewed by:
Natasa Krsto Rancic, University of Niš, SerbiaAntonino Tuttolomondo, University of Palermo, Italy
Copyright © 2022 Ishikawa, Nakano, Tokutsu, Nakayamada, Matsuda, Fushimi and Tanaka. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yoshiya Tanaka, dGFuYWthQG1lZC51b2VoLXUuYWMuanA=
 Yuichi Ishikawa
Yuichi Ishikawa Kazuhisa Nakano1,3
Kazuhisa Nakano1,3 Kei Tokutsu
Kei Tokutsu Shingo Nakayamada
Shingo Nakayamada Yoshiya Tanaka
Yoshiya Tanaka