- 1Laboratory of Cardio-Pulmonary Testing and Pulmonary Rehabilitation, Department of Respiratory Medicine, Faculty of Medicine, University of Thessaly, Larissa, Greece
- 2School of Physical Education and Sports Sciences, University of Thessaly, Trikala, Greece
- 3Institute of Sport, Faculty of Education Health and Wellbeing, University of Wolverhampton, Walsall, United Kingdom
- 4Department of Neurology, Faculty of Medicine, University of Cyprus, Lefkosia, Cyprus
- 5Department of Respiratory Medicine, Faculty of Medicine, University of Thessaly, Larissa, Greece
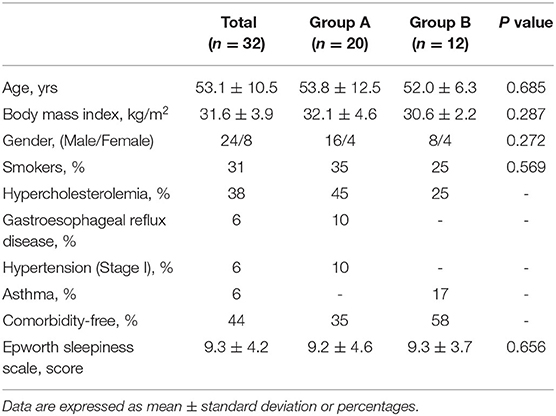
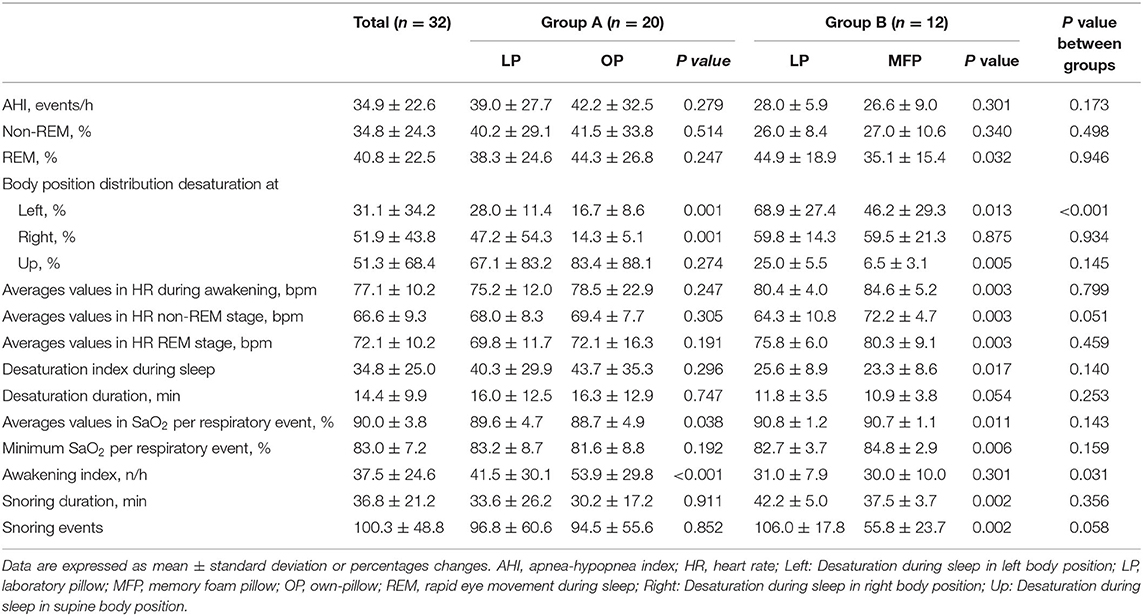
Specific pillow use is a seldom studied or controlled factor in the setting of sleep disordered breathing. The aim of this study was to investigate the effect of different pillows [own pillow (OP), memory foam pillow (MFP), generic laboratory pillow (LP)] on polysomnography (PSG)-derived parameters in patients with Obstructive Sleep Apnea Syndrome (OSAS). Thirty-two consecutive patients with OSAS were randomly allocated into two groups with randomized pillow usage [Group A: 3 h with LP and 3 h with OP (Age: 53.8 ± 12.5 years, BMI: 32.1 ± 4.6 kg/m2); Group B: 3 h with LP and 3 h with MFP (Age: 52.0 ± 6.3 years, BMI: 30.6 ± 2.2 kg/m2)]. Statistically significant differences between pillow types were detected in desaturation index and heart rate. In Group B (with MFP), a statistically significant decrease of 47.0 ± 15.9% was observed in snoring events (p < 0.05) and 10.6 ± 6.7% in their duration (p < 0.05) compared to LP. On the other hand, group A with OP recorded a decrease of 29.1 ± 32.1% in snoring events and 32.5 ± 33.1% in duration, but these values were not statistically significant (p > 0.05) compared to LP. These findings indicate that pillow type and usage, often uncontrolled in OSAS studies (contribution to the field), may impact several PSG parameters and are related to a snoring subtype of the syndrome. Secondly, they indicate that a focus on the treatment of the snoring OSAS subtype warrants further dedicated investigation.
Introduction
Pillows affect sleep quality by maintaining the natural curvature of the spine, thus ensuring optimal sleep posture (1). In patients with mild sleep-disordered breathing, optimal pillow usage may reduce snoring and improves sleep quality efficiency and, by extent, depth (2). Conversely, incorrect pillow placement, such as that occurs during travel, may be detrimental to sleep health (3). Considering Obstructive Sleep Apnea Syndrome's (OSAS's) heterogeneity (4) and the implication of other overlapping symptoms, such as snoring (5), it is necessary to assess the biological context of potential interventions.
Previous studies on pillow usage are limited in number and focus on the role of cervical positional therapy, collectively reporting an improvement on snoring (6–9). Previous research has suggested that the use of custom fitted pillows may represent an efficacious and cost-effective treatment option in mild to moderate OSAS (10), filling a niche where continuous positive airway pressure (CPAP) would not be indicated (11). Considering that pillow design can be guided (12, 13) to alleviate specific symptoms, an evaluation of pillow type impact on sleep health may be directly relevant to their efficacious implementation.
In this context, two major research questions regarding the implementation of specific pillows as a possible OSAS treatment arise: who will benefit and how? As a heterogeneous disease, OSAS' treatment goals extend from severity to phenomenology (4, 14). Toward this end, the effect of pillow usage should be evaluated in order to determine how it shapes polysomnography (PSG)-captured parameters and its implication in sleep disordered breathing phenotypes.
The aim of our study was to investigate the effect of different pillows [own pillow (OP), memory foam pillow (MFP), generic laboratory pillow (LP)] on PSG parameters in patients with OSAS.
Materials and Methods
Study Population
This was a single-center, randomized prospective study. Participants were recruited from the province of Thessaly region (Greece). The inclusion criteria were as follows: patients referred for potential sleep disordered breathing following a polysomnography study, an apnea-hypopnea index (AHI) of ≥5 events/h with LP, age between 20 and 80 years, BMI < 40 kg/m2, waist to hip ratio <1, and neck circumferences <40 cm. Exclusion criteria were as follows: neurological and psychiatric disorders, musculoskeletal disorders, and awakening during changing pillows.
The study was approved by the Institutional Ethics Committee of the University of Thessaly, Greece (No. 21/09-01-2017) and informed consents were obtained from all participants, in accordance with the Helsinki declaration.
Full Night Polysomnography
Overnight PSG was performed in accordance with the American Academy of Sleep Medicine (AASM) guidelines (15). PSG-included electroencephalography, electrooculography, submental electromyography, anterior tibialis electromyography, nasal cannula airflow signal using a nasal cannula/pressure transducer system, oral thermistor, electrocardiography, and body position (16). Respiratory efforts were monitored with abdominal and thoracic bands. Arterial SaO2 was measured using SpO2. Apnea was defined as complete cessation of airflow for at least 10 s in duration. Hypopnea was defined as one of the following three: (1) >50% reduction in airflow, (2) <50% reduction in airflow associated with a desaturation of >3%, or (3) a moderate reduction in airflow with associated arousal by electroencephalography. Apneas were classified as obstructive, central, or mixed according to the presence or absence of respiratory efforts. Snoring was measured by a microphone. Patients with predominant obstructive sleep apneas and AHI ≥ 5 events/h were diagnosed with the OSAS. PSG was performed at the Laboratory of Sleep Disorders (Department of Respiratory Medicine, Faculty of Medicine, University of Thessaly, Greece) using an Alice®4 computer system (Philips Respironics, PA, USA). PSG scoring was performed by specialists blinded to pillow usage and group allocation.
Learning Effect Attenuation
In an attempt to eliminate any PSG learning effect, volunteers were randomly divided into two groups, (Group A: 3 h with LP and 3 h with their OP; Group B: 3 h with LP and 3 h with MFP). The replacement of the pillow during PSG was (a) conducted by a sleep technician in a randomized order and (b) at the awaking phase.
Epworth Sleep Scale Questionnaire
Sleepiness was assessed using the validated Greek version of the Epworth Sleepiness Scale (ESS), (17) a self-administered questionnaire evaluating the possibility of dozing in a variety of situations (18).
Pillow Characteristics
The dimensions of the LPs were 12.0 × 60.0 × 36.0 cm (Height × Length × Width) and was made with microfiber. The pillows owned by patients had variant dimensions (14.2 ± 0.8 × 55.0 ± 3.4 × 44.2 ± 3.6 cm; Height x Length × Width) and were made of polyester (34%), foam shredded (29%), and goose feather (37%). The MFPs had dimensions of 16.0 × 70.0 × 40.0 cm (Height × Length × Width) and was made of memory foam with aloe vera extract (Media Strome®, Greece).
Statistical Analyses
Pairwise comparisons per group (Group A: LP vs. OP and Group B: LP vs. MFP) were performed with the dependent samples t-test. We calculated the standardized rates of change between sequential measurements via the formula [(Post-Pre)/Pre], where “post” refers to post-intervention and “pre” refers to pre-intervention. These rates were compared between intervention groups via the independent Samples t-test. Data are presented as absolute numbers, percentages, or mean values ±Sd where applicable. For all statistical analyses, a p-value < 0.05 was considered statistically significant. All analyses were performed via the IBM SPSS Statistics 25 (SPSS Inc., Chicago, IL, USA) software package.
Results
Out of the 147 individuals who were assessed for eligibility, 32 were included in the study (Figure 1). Demographic characteristics were not significantly different between groups (Table 1). Table 2 illustrates statistical differences in Heart Rate (HR) values between two types of pillows (LP vs. MFP) in awakening phase (p = 0.003), REM stage (p = 0.003), and non-REM stage (p = 0.003). The group with the MFP pillow showed higher values in HR during awakening phase and non-REM stage compared to the group with OP (p < 0.05). There were statistically significant differences between pillow types and the standardized rate of change for the arousal index and the number of snoring events (p < 0.05). Table 2 provides information on snoring duration and snoring events during PSG. Unlike Group A which demonstrated no statistical differences in snoring parameters, Group B recorded significantly lower number of snoring events by 47.0 ± 15.9 % (106.0 ± 17.8 vs. 55.8 ± 23.7 events, p = 0.002) and snoring duration by 10.6 ± 6.7% (42.2 ± 5.0 vs. 37.5 ± 3.7 min, p = 0.002) with MFP compared to LP.
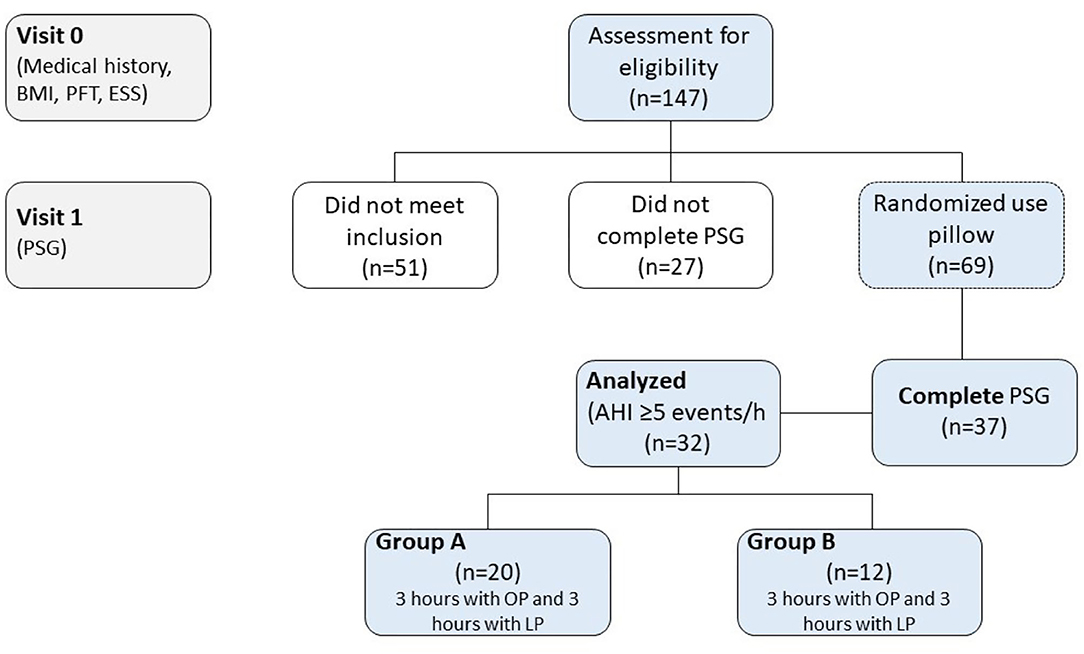
Figure 1. Study flow diagram. BMI, body mass index; ESS, Epworth sleepiness scale; LP, laboratory pillow; MFP, memory foam pillow; OP, own-pillow; PFT, pulmonary function test; PSG, polysomnography study.
Discussion
Our study aimed to investigate the effect of pillow type (OP and/or MFP vs. LP) in patients with OSAS and its effects on polysomnographic and phenotypic parameters of the syndrome. We report on preliminary results from our ongoing study, indicating that MFP improved several PSG-captured parameters in patients with OSAS, mainly the snoring phenotype. Reduction of quantity and intensity of snoring events, along with improved oxygenation relative to body position, were among the significant PSG-captured effects of MFP usage. These findings indicate that pillow type and usage, often uncontrolled in OSAS studies, impacts several PSG parameters and is related to a snoring subtype of the syndrome. Secondly, they indicate that a focus on the treatment of the snoring OSAS subtype warrants further, dedicated investigation.
In general, the supine position has been implicated in the exacerbation of apneic episodes in OSAS (19), whereas prone position may be alleviating (20). Our findings indicate that this alleviation may be captured by the improvement of desaturation index and snoring events, and thus may be more relevant to the snoring phenotype (21).
The use of different pillow types showed HR changes in both groups of patients with OSAS. However, the MFP sub-group showed higher values in HR around apneic episodes as recorded by awakening phase and minimum SaO2 per respiratory event compared to the OP sub-group. Before apneic episodes, bradycardia occurs, followed by HR increase that may or may not produce cortical arousals (22). The lower the HR variability, the lower the arousals that occur, leading to less sleep fragmentation and sleep quality. OSAS severity is associated with the abnormal adaptability of the autonomic nervous system (ANS), and this association is reversible up to an extent as the treatment of OSAS is implemented (23). The application of a more suitable pillow could reinforce the therapeutic effects.
The characteristics of snoring were also significantly ameliorated when the MFP was applied. Snoring is elicited by a Bernoulli effect on the soft palate, as negative pressure induces its vibration during an obstructive respiratory event (24). Maintaining airway patency via positional therapy could therefore be expected to reduce snoring events. The use of “smart” pillows for positional therapy in OSAS have reported a reduction of snoring events and overall better sleep quality (6) – findings that are similar to our own.
Positional therapy in OSAS phenotypes where obstructive events and snoring are central features has been previously proposed as a simple and effective intervention (25). Similarly, pillows designed to address cervical positioning and, by extension, airway patency have been associated with a reduction of snoring events and duration (7, 10).
Limitations
It is reasonable to assume that the present study might have been influenced by methodological limitations such as the lack of information on allergenic effects of synthetic pillows (26), although such effects were not diagnosed or reported in our study. Furthermore, longer follow-up studies are needed in order to determine whether the effects noted in our study are sustained. Another important limitation is that measurements of the mandibular plane-hyoid distance, the small posterior airway space diameters, and tongue volume were not included in our study (27). Finally, the production of groups via randomization process may have created groups with the potential to exhibit greater improvement following the implementation of different pillow types. This has been addressed with both between and within-group subject comparisons in order to simultaneously assess the effect of pillow placement and different pillow type. The randomization involved patient allocation rather than pillow placement post-allocation. In order to detect sequence effects, we would have to deploy a different design, i.e., MFP-LP-MFP vs. LP-MFP-LP, and then determine sequences within and then across groups. We did not deploy this aforementioned design on the premises of introducing additional disruption in the PSG that would correspondingly need to be accounted for.
Conclusions
Compared to either own or regular LPs, MFP seems to be more effective in decreasing snoring events and snoring duration. As a relatively easy to implement intervention, large studies should focus on the role of appropriate pillows as an adjunctive treatment modality of OSAS. Furthermore, our study indicates that the usage of the patient's OP rather than LPs may give a closer-to-life laboratory investigation of OSAS.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Ethics Committee of the University of Thessaly, Greece, No. 21/09-01-2017. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
VTS, YK, and KIG conceived and designed the experiments. VTS, GDV, EP, and FB analyzed the data. VTS, YK, KA, IS, and GDV wrote the paper. VTS, YK, GDV, and KIG edited the paper. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors acknowledged the staff of Respiratory Sleep Disorders Laboratory: Maria Pinaka, Dimitra Siachpazidou, Aleksandra Sistou (replacement of pillows during sleep), and George Seitanidis (assessment and scoring polysomnography study) for friendly cooperation. Moreover, the authors would also like to thank the participants of this study and acknowledge their willingness to contribute to our research effort.
References
1. Lin XY, Wu FG. Pillow shape design to enhance the sleep quality of middle-aged groups. Procedia Manuf. (2015) 3:4429–35. doi: 10.1016/j.promfg.2015.07.476
2. Liu SF, Lee YL, Liang JC. Shape design of an optimal comfortable pillow based on the analytic hierarchy process method. J Chiropr Med. (2011) 10:229–39. doi: 10.1016/j.jcm.2011.04.002
3. Stavrou VT, Astara K, Daniil Z, Gourgoulianis KI, Kalabakas K, Karagiannis D, et al. The reciprocal association between fitness indicators and sleep quality in the context of recent sport injury. Int J Environ Res Public Health. (2020) 17:4810. doi: 10.3390/ijerph17134810
4. Vavougios GD, George DG, Pastaka C, Zarogiannis SG, Gourgoulianis KI. Phenotypes of comorbidity in OSAS patients: combining categorical principal component analysis with cluster analysis. J Sleep Res. (2016) 25:31–8. doi: 10.1111/jsr.12344
5. Sowho M, Sgambati F, Guzman M, Schneider H, Schwartz A. Snoring: a source of noise pollution and sleep apnea predictor. Sleep. (2020) 15:zsz305. doi: 10.1093/sleep/zsz305
6. Chung TT, Lee MT, Ku MC, Yang KC, Wei CY. Efficacy of a smart antisnore pillow in patients with obstructive sleep apnea syndrome. Behav Neurol. (2021) 2021:8824011. doi: 10.1155/2021/8824011
7. Zuberi NA, Rekab K, Nguyen HV. Sleep apnea avoidance pillow effects on obstructive sleep apnea syndrome and snoring. Sleep Breath. (2004) 8:201–7. doi: 10.1055/s-2004-860897
8. Kushida CA, Rao S, Guilleminault C, Giraudo S, Hsieh J, Hyde P, et al. Cervical positional effects on snoring and apneas. Sleep Res Online. (1999) 2:7–10.
9. Chen WC, Lee LA, Chen NH, Fang TJ, Huang CG, Cheng WN Li HY. Treatment of snoring with positional therapy in patients with positional obstructive sleep apnea syndrome. Sci Rep. (2015) 11:18188. doi: 10.1038/srep18188
10. Kushida CA, Sherrill CM, Hong SC, Palombini L, Hyde P, Dement WC. Cervical positioning for reduction of sleep-disordered breathing in mild-to-moderate OSAS. Sleep Breath. (2001) 5:71–8. doi: 10.1055/s-2001-15797
11. Srijithesh PR, Aghoram R, Goel A, Dhanya J. Positional therapy for obstructive sleep apnoea. Cochrane Database Syst Rev. (2019) 1:CD010990. doi: 10.1002/14651858.CD010990.pub2
12. Son J, Jung S, Song H, Kim J, Bang S, Bahn S, et al. Survey of koreans on sleep habits and sleeping symptoms relating to pillow comfort and support. Int J Environ Res Public Health. (2020) 17:302. doi: 10.3390/ijerph17010302
13. Li Y, Wu J, Lu C, Tang Z, Li C. Pillow support model with partitioned matching based on body pressure distribution matrix. Healthcare (Basel). (2021) 9:571. doi: 10.3390/healthcare9050571
14. Al-Hussaini A, Berry S. An evidence-based approach to the management of snoring in adults. Clin Otolaryngol. (2015) 40:79–85. doi: 10.1111/coa.12341
15. Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American academy of sleep medicine clinical practice guideline. J Clin Sleep Med. (2017) 13:479–504. doi: 10.5664/jcsm.6506
16. Wolpert EA. A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Arch Gen Psychiatry. (1969) 20:246–7.
17. Tsara V, Serasli E, Amfilochiou A, Constantinidis T, Christaki P. Greek Version of the Epworth Sleepiness Scale. Sleep Breath. (2004) 8:91–5. doi: 10.1055/s-2004-829632
18. Iber C, Ancoli-Israel S, Chesson AL, Quan SF. American Academy of Sleep Medicine. In: The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. 1st ed. Westchester, IL: American Academy of Sleep Medicine. (2017).
19. Oksenberg A, Khamaysi I, Silverberg DS, Tarasiuk A. Association of body position with severity of apneic events in patients with severe nonpositional obstructive sleep apnea. Chest. (2000) 118:1018–24. doi: 10.1378/chest.118.4.1018
20. Afrashi A, Ucar ZZ. Effect of prone positioning in mild to moderate obstructive sleep apnea syndrome. Sleep Breath. (2015) 19:1027–34. doi: 10.1007/s11325-014-0985-x
21. Labarca G, Gower J, Lamperti L, Dreyse J, Jorquera J. Chronic intermittent hypoxia in obstructive sleep apnea: a narrative review from pathophysiological pathways to a precision clinical approach. Sleep Breath. (2000) 24:751–60. doi: 10.1007/s11325-019-01967-4
22. Zwillich C, Devlin T, White D, Douglas N, Weil J, Martin R. Bradycardia during sleep apnea. Characteristics and mechanism. J Clin Invest. (1982) 69:1286–92. doi: 10.1172/JCI110568
23. Sequeira VCC, Bandeira PM, Azevedo JCM. Heart rate variability in adults with obstructive sleep apnea: a systematic review. Sleep Sci. (2019) 12:214–21. doi: 10.5935/1984-0063.20190082
24. Fajdiga I. Snoring imaging: could Bernoulli explain it all? Chest. (2005) 128:896–901. doi: 10.1378/chest.128.2.896
25. Newell J, Mairesse O, Neu D. Can positional therapy be simple, effective and well tolerated all together? A prospective study on treatment response and compliance in positional sleep apnea with a positioning pillow. Sleep Breath. (2018) 22:1143–51. doi: 10.1007/s11325-018-1650-6
26. Shusterman D, Baroody FM, Craig T, Friedlander S, Nsouli T, Silverman B. American academy of allergy, asthma & immunology's rhinitis, rhinosinusitis and ocular allergy committee work group on rhinitis and sleep-disordered breathing. Role of the allergist-immunologist and upper airway allergy in sleep-disordered breathing. J Allergy Clin Immunol Pract. (2017) 5:628–39. doi: 10.1016/j.jaip.2016.10.007
Keywords: pillow, memory foam pillow, sleep quality, snoring, desaturation
Citation: Stavrou VT, Koutedakis Y, Astara K, Vavougios GD, Papayianni E, Stavrou IT, Bardaka F, Pastaka C and Gourgoulianis KI (2022) Memory Foam Pillow as an Intervention in Obstructive Sleep Apnea Syndrome: A Preliminary Randomized Study. Front. Med. 9:842224. doi: 10.3389/fmed.2022.842224
Received: 23 December 2021; Accepted: 07 February 2022;
Published: 09 March 2022.
Edited by:
Barbara Ruaro, University of Trieste, ItalyReviewed by:
Riccardo Pozzan, University of Trieste, ItalyAmanda Jane Piper, Royal Prince Alfred Hospital, Australia
Copyright © 2022 Stavrou, Koutedakis, Astara, Vavougios, Papayianni, Stavrou, Bardaka, Pastaka and Gourgoulianis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vasileios T. Stavrou, dmFzaWxlaW9zc3RhdnJvdUBob3RtYWlsLmNvbQ==
 Vasileios T. Stavrou
Vasileios T. Stavrou Yiannis Koutedakis2,3
Yiannis Koutedakis2,3 Kyriaki Astara
Kyriaki Astara George D. Vavougios
George D. Vavougios Eirini Papayianni
Eirini Papayianni