- 1Department of Obstetrics, Nanjing Maternity and Child Health Care Hospital, Women’s Hospital of Nanjing Medical University, Nanjing, China
- 2Department of Reproduction, Changzhou Maternal and Child Health Care Hospital, Changzhou Medical Center, Nanjing Medical University, Changzhou, China
- 3Nanjing Maternity and Child Health Care Institute, Nanjing Maternity and Child Health Care Hospital, Women’s Hospital of Nanjing Medical University, Nanjing, China
Background: With the progress of assisted reproductive technology (ART) and the increasing number of ART pregnancy, its safety has become the focus of attention. The present study aimed to explore the associations of ART pregnancy with maternal and neonatal outcomes, as compared with naturally pregnancy.
Methods: This retrospective cohort study included all pregnant women who delivered at Women’s Hospital of Nanjing Medical University in 2011–2020. We compared maternal characteristics and pregnancy outcomes between group of ART pregnancy and group of naturally pregnancy using Logistic regression adjusted for confounders.
Results: A total of 13,604 ART pregnancies and 198,002 naturally pregnancies were included. The proportion of ART pregnancies has increased every year for the past 10 years, peaking in 2020 (9.0%). Multivariable logistic regression analysis showed that the risks of gestational diabetes, preeclampsia, moderate or severe anemia, liver-related diseases, thyroid-related diseases, preterm birth, placenta previa, postpartum hemorrhage, and cesarean section were significantly increased in ART pregnancy. For neonatal outcomes, women conceived by ART were more likely to have twins or multiples, and the risk of stillbirth or abnormal development was also significantly increased. When restriction to singletons, these risks were reduced. And the effects of ART on the risk of premature rupture of membrane, cord entanglement, intrapartum fever, cesarean section, and stillbirth or abnormal development were more pronounced in singletons pregnancies compared with that in pregnancies of twins or multiples.
Conclusion: Women conceived by ART were at increased risks of several adverse pregnancy outcomes compared with women conceived naturally. Multiple pregnancies could partly explain this phenomenon. For ART pregnancy, prenatal and intrapartum monitoring should be strengthened, and neonatal outcomes should be closely observed.
Introduction
Since the birth of the first test-tube baby in 1978, assisted reproductive technology (ART) has become an effective treatment for infertility (1). With the progress of technology and provision of services, an increasing number of infants are born following ART therapy (1, 2). In developed countries, ART pregnancies account for 1.5–5.9% of all births (3–7), while in China, ART pregnancies account for 1.7% and are increasing year by year (2). ART is sometimes defined differently and is usually defined as the application of laboratory or clinical techniques to gametes and/or embryos for reproductive purposes, however it has been broadened to include not only in vitro procedures but also ovarian stimulation with gonadotropins or ovariotropic drugs (8, 9). As these and other reproductive technologies expand, leading to a substantial number of successful pregnancies and births, it is critical for prospective parents to understand the maternal and neonatal outcomes associated with ART.
Several studies have shown that ART pregnancies have an increased risk of multiple pregnancy and adverse pregnancy outcomes, including gestational diabetes, gestational hypertension, placenta previa, preterm birth, operative delivery, low birth weight, birth defects and perinatal mortality (10–16). However, other studies have concluded ART pregnancies do not have increased risks of adverse perinatal outcomes (7, 17–19). The incidences of small for gestational age, preterm birth and cesarean section are similar between ART and naturally pregnancies (13, 20). Nevertheless, pregnancy outcomes in ART pregnancies appear to be generally poorer due to the increased risk of multiple pregnancies. Multiple pregnancy is a post-processing confounding factor, which appears after ART treatment and may confound causal effects. Many previous studies did not adjust for maternal age, BMI and other confounding factors (12, 21–23). It is not clear whether the increased risk of adverse pregnancy outcomes is due to ART itself, multiple births, or potential infertility. At present, opinions are too far apart to reach a consensus.
The present retrospective cohort study was conducted to compare maternal and neonatal outcomes between ART and naturally pregnancies, and in addition to explore the association of ART with adverse pregnancy outcomes by stratifying on birth plurality and maternal age.
Materials and Methods
Study Design and Population
This retrospective cohort study included all pregnant women who delivered at Women’s Hospital of Nanjing Medical University in 2011–2020. The Women’s Hospital of Nanjing Medical University is the largest maternity hospital in Jiangsu province, China and delivers approximately 20,000 babies annually. After excluding women who had early abortions (≤12 weeks), or women who were discharged from care during pregnancy, a total of 211,606 pregnancies were included in the data analysis. Two cohorts were created: women who conceived by either intracytoplasmic sperm injection (ICSI), in vitro fertilization (IVF), ovulation induction (OI), gamete intra-fallopian transfer (GIFT), or artificial insemination (AI), were defined as group of ART pregnancy, and women who conceived naturally without ART, were considered as group of naturally pregnancy.
Data Collection
We obtained all maternal and neonatal information from Hospital Information System (HIS) Database. Data were collected from standardized clinical forms and hospital records after maternity discharge to form the research database. All data were extracted and cleaned by using Natural Language Processing (NLP) technique (24). Maternal characteristics of all pregnancies were firstly extracted, including maternal age (year), height (cm), intrapartum weight (kg), parity, birthplace (Jiangsu province in China, other provinces in China or other countries), menstrual cycle (21–35 days, 36 days- or irregularity), abnormal pregnancy history and history of uterine fibroids. Maternal age was divided into five groups: <25, 25–29, 30–34, 35–39, ≥40 years. Intrapartum body mass index (BMI, kg/m2) was calculated as maternal intrapartum weight divided by the square of height, and classified into four groups: <25, 25–29.9, 30–34.9, ≥35 kg/m2. Parity did not include this pregnancy and was divided into 0 (nulliparae) and ≥1 (multiparae). Abnormal pregnancy history refers to a history of early abortion (≥2 times), intermediate and late abortion, abnormal development, or ectopic pregnancy.
We also used the HIS Database to obtain data on pregnancy complications, perinatal complications and neonatal outcomes. Data on pregnancy complications included gestational diabetes (fasting glucose concentrations ≥ 5.5 mmol/l or 2-h plasma glucose concentrations ≥ 8.0 mmol/l), preeclampsia (hypertension from 20 weeks’ gestation and proteinuria; severe preeclampsia was defined as preeclampsia with either a diastolic blood pressure ≥ 110 mmHg or proteinuria ≥ 5 g/day or both), anemia (hemoglobin < 100 g/l and hematocrit < 0.30; moderate or severe anemia was defined as hemoglobin < 90 g/l or 60 g/l), liver-related diseases (cholestasis, hepatitis, liver function damage, etc.) and thyroid-related diseases (hyperthyroidism, hypothyroidism, thyroiditis, etc.). Data on perinatal complications included hospitalization time (day), preterm birth (<37 weeks’ gestation), premature rupture of membrane, amniotic fluid pollution (clear as 0°, I°, II°, or III°), polyhydramnios (>2,000 ml in the third trimester), oligohydramnios (<300 ml in the third trimester), cord entanglement, torsion of cord, intrapartum fever (intrapartum temperature > 38°C), placenta previa, antepartum hemorrhage, postpartum hemorrhage (measured blood loss ≥ 500 ml) and delivery mode (spontaneous labor or cesarean section). And data on neonatal outcomes included gestational weeks in birth, offspring gender, birth weight (g), macrosomia (birth weight ≥ 4,000 g), twins or multiples, fetal distress, stillbirth or abnormal development (fetal malformation).
Statistical Analyses
We compared maternal characteristics and pregnancy outcomes between group of ART pregnancy and group of naturally pregnancy. Continuous variables were described as mean and standard deviation ( ± s), and categorical variables were displayed as frequency (percentage). All comparisons between groups were conducted using standardized differences, which are not influenced by sample size and have been frequently used in previous large cohort studies (25–27). A standardized difference ≥ 0.1 indicates meaningful difference between groups. The association between ART using and pregnancy outcomes were evaluated by logistic regression analysis. The crude and adjusted odds ratio (OR) with 95% confidence intervals (95%CI) for pregnancy outcomes were calculated. Adjusted values were adjusted for maternal age, intrapartum BMI, parity, birth plurality and abnormal pregnancy history. All statistical analyses were two-sided and performed using R software (version 3.2.2).
Results
A total of 211,606 women were included in this retrospective analysis, of whom 13,604 women conceived by ART as group of ART pregnancy, and 198,002 women conceived naturally without ART as group of naturally pregnancy. Over the past 10 years, the proportion of ART pregnancy has increased each year, reaching a peak in 2020 (9.0%) (Figure 1A). Of the ART pregnancy, the proportion of pregnant women over 35 years old and multiparae increased mildly, while the proportion of women with intrapartum BMI greater than 30 kg/m2 decreased slightly. And with the implementation of the universal two-child policy in 2015, the proportion of women with abnormal pregnancy history in ART pregnancy decreased sharply, and then increased rapidly (Figure 1B).
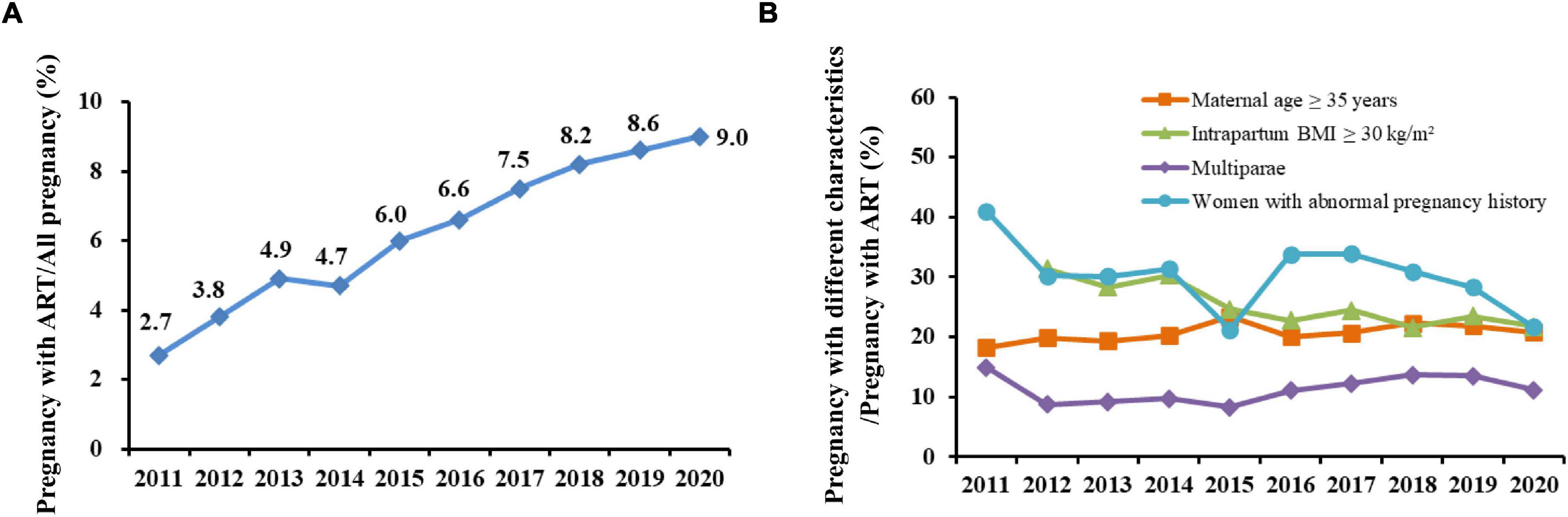
Figure 1. Yearly trends in percentage of assisted reproductive technology (ART) pregnancy and pregnancy with different characteristics from 2011 to 2020. (A) Percentage of ART pregnancy among all pregnancy; (B) Percentage of different characteristics among ART pregnancy.
Maternal characteristics between ART and naturally pregnancy is summarized in Table 1. The mean maternal age and intrapartum BMI of women conceived by ART were significantly higher than those of women conceived naturally (standardized difference = 0.547 and 0.309, respectively). And women conceived by ART were more likely to be nulliparae (88.5% vs. 75.4%, standardized difference = 0.345), more likely to have a long or irregular menstrual cycle (15.2% vs. 7.9%, standardized difference = 0.230) and an abnormal pregnancy history (including early abortion, intermediate and late abortion, abnormal development, or ectopic pregnancy, 29.1% vs. 9.9%, standardized difference = 0.500), and more likely to have uterine fibroids (8.3% vs. 5.1%, standardized difference = 0.128). There were no significant standardized differences in maternal height and birthplace between the two groups.

Table 1. Maternal characteristics between naturally pregnancy and assisted reproductive technology (ART) pregnancy.
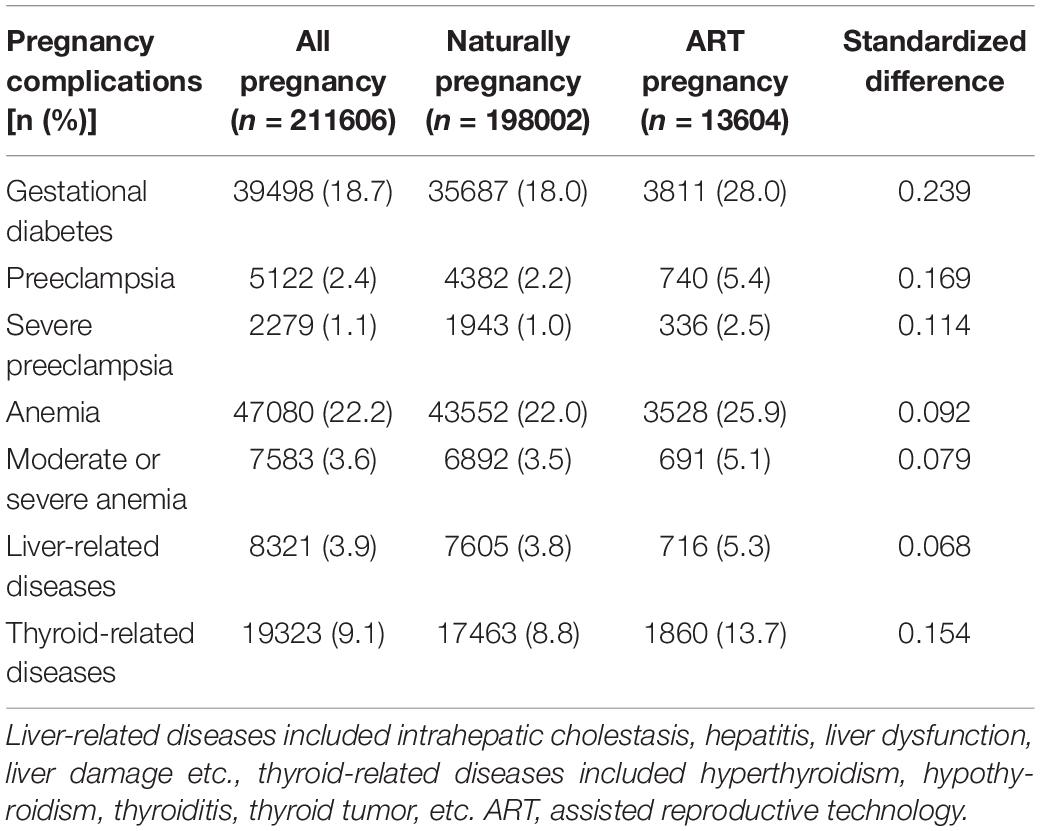
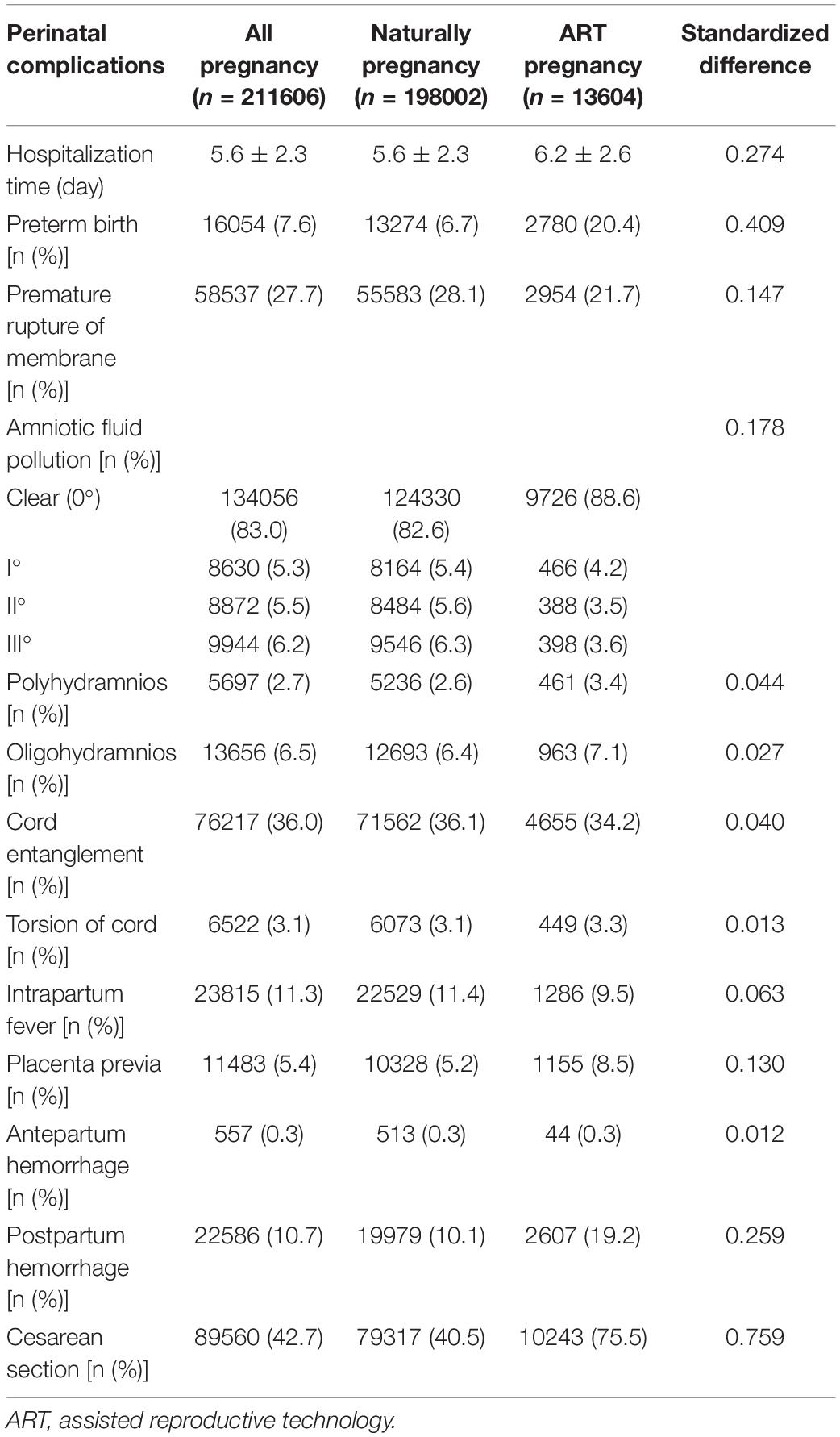
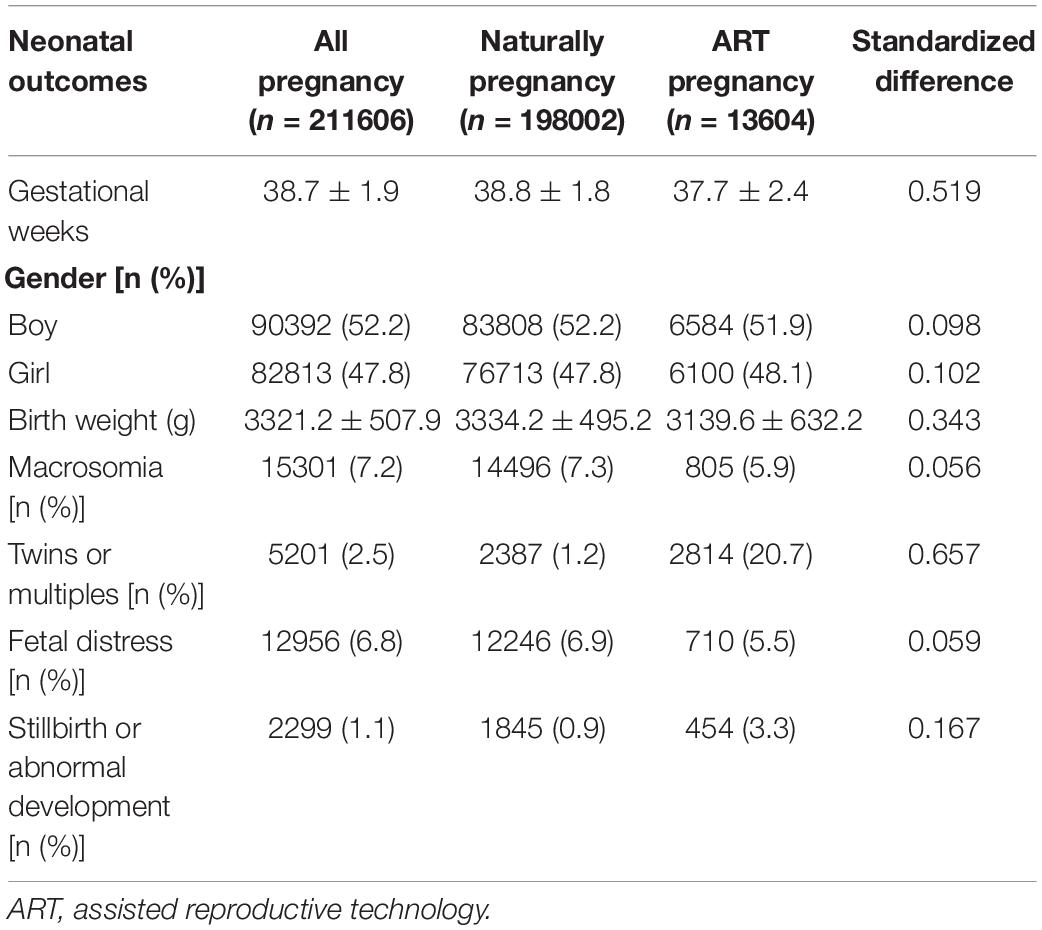
The incidences of pregnancy and perinatal complications in ART and naturally pregnancy was exhibited in Tables 2, 3. Statistically significant increases were noted in gestational diabetes (28.0%), preeclampsia (5.4%), thyroid-related diseases (13.7%), preterm birth (20.4%), placenta previa (8.5%), postpartum hemorrhage (19.2%) and cesarean section (75.5%) in ART pregnancy, compared to naturally pregnancy (standardized difference > 0.1). The occurring rates of anemia (25.9%), liver-related diseases (5.3%), polyhydramnios (3.4%), oligohydramnios (7.1%) and torsion of cord (3.3%) were also elevated in ART pregnancy, but with no significant difference (standardized difference < 0.1). In contrast, there was a decline in the incidences of premature rupture of membrane (21.7%) and amniotic fluid pollution (I°: 4.2%, II°: 3.5%, III°: 3.6%) in ART pregnancy (standardized difference > 0.1). We also analyzed neonatal outcomes between naturally pregnancy and ART pregnancy (Table 4). The mean birth weight of ART pregnancy was significantly lower than that of naturally pregnancy (standardized difference = 0.343). Moreover, significant rises of incidence were observed in twins or multiples (20.7%) and stillbirth or abnormal development (3.3%) in ART pregnancy (standardized difference > 0.1). No significant difference was noted in macrosomia and fetal distress between the two groups.
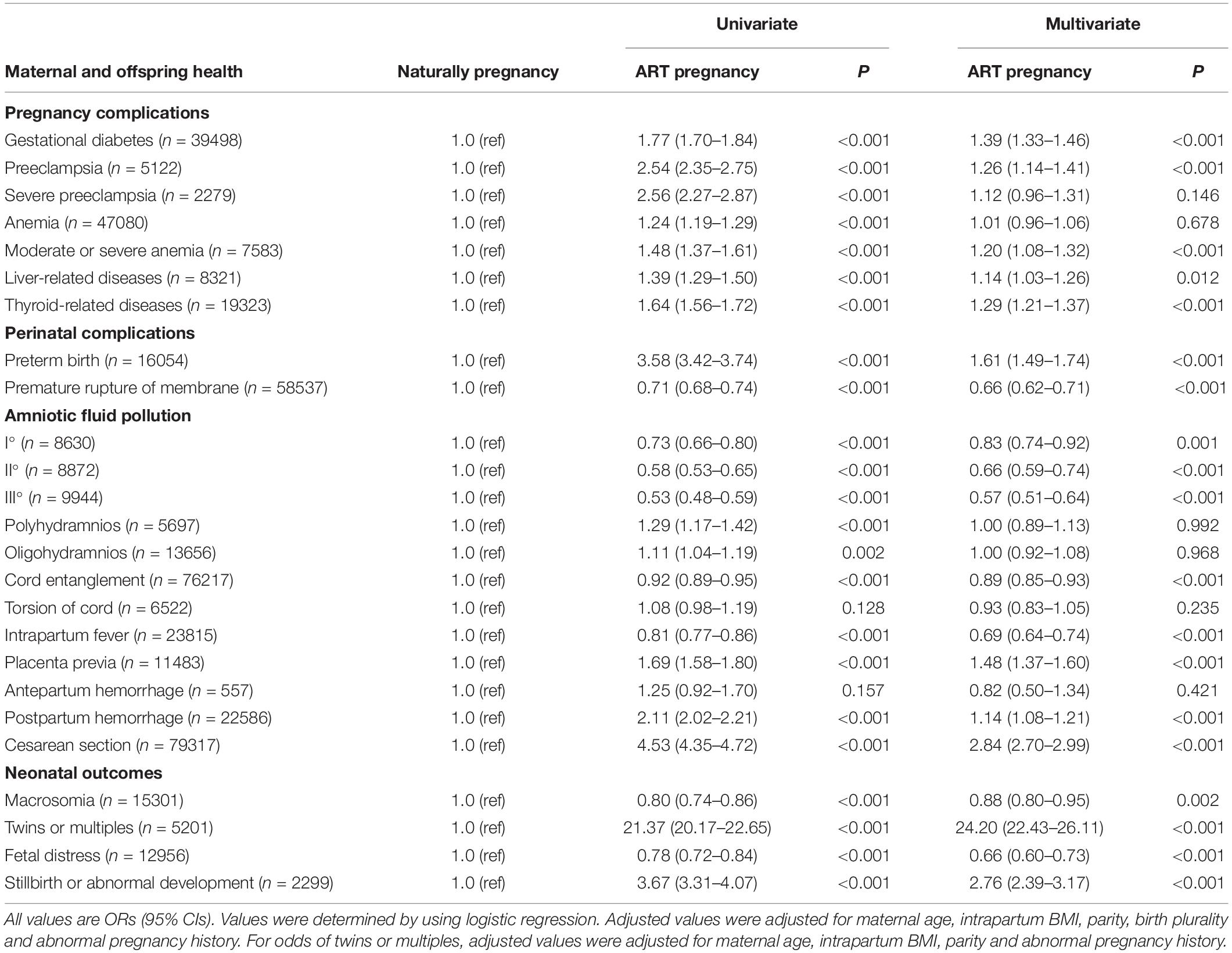
Multivariable logistic regression analysis showed that the association between ART and pregnancy outcomes were significant (Table 5). Nearly all the pregnancy complication listed, including gestational diabetes [aOR (95%CI) = 1.39 (1.33–1.46)], preeclampsia [aOR (95%CI) = 1.26 (1.14–1.41)], moderate or severe anemia [aOR (95%CI) = 1.20 (1.08–1.32)], liver-related diseases [aOR (95%CI) = 1.14 (1.03–1.26)], and thyroid-related diseases [aOR (95%CI) = 1.29 (1.21–1.37)], were more likely to occur among women conceived by ART. In terms of perinatal complications, the risk of preterm birth [aOR (95%CI) = 1.61 (1.49–1.74)], placenta previa [aOR (95%CI) = 1.48 (1.37–1.60)], postpartum hemorrhage [aOR (95%CI) = 1.14 (1.08–1.21)], and cesarean section [aOR (95%CI) = 2.84 (2.70–2.99)] were significantly increased, while the risk of premature rupture of membrane [aOR (95%CI) = 0.66 (0.62–0.71)], amniotic fluid pollution [I°: aOR (95%CI) = 0.83 (0.74–0.92); II°: aOR (95%CI) = 0.66 (0.59–0.74); III°: aOR (95%CI) = 0.57 (0.51–0.64)], cord entanglement [aOR (95%CI) = 0.89 (0.85–0.93)], and intrapartum fever [aOR (95%CI) = 0.69 (0.64–0.74)] were significantly decreased in ART pregnancy as compared with naturally pregnancy. For neonatal outcomes, women conceived by ART were more likely to have twins or multiples [aOR (95%CI) = 24.20 (22.43–26.11)], and the risk of stillbirth or abnormal development [aOR (95%CI) = 2.76 (2.39–3.17)] was also significantly increased. Moreover, the risk of macrosomia [aOR (95%CI) = 0.88 (0.80–0.95)] and fetal distress [aOR (95%CI) = 0.66 (0.60–0.73)] were significantly decreased in ART pregnancy (Table 5).
The association of ART with maternal and neonatal outcomes were also evaluated by stratifying on birth plurality and maternal age (Tables 6, 7). When restriction to singletons, the risks of adverse pregnancy outcomes as listed above were reduced. And the effects of ART on the risk of premature rupture of membrane, cord entanglement, intrapartum fever, cesarean section, and stillbirth or abnormal development (ART pregnancy vs. naturally pregnancy) were more pronounced among singleton pregnancies compared with that among pregnancies of twins or multiples, while the effect of ART on the risk of polyhydramnios was more prominent among pregnancies of twins or multiples (heterogeneity test: P < 0.05). When stratified by maternal age, we found the effects of ART on the risk of preterm birth, placenta previa, postpartum hemorrhage and cesarean section (ART pregnancy vs. naturally pregnancy) were more pronounced among women under 35 years compared with that among women over 30 years, while the effect of ART on the risk of polyhydramnios was more prominent among women over 35 years (heterogeneity test: P < 0.05).
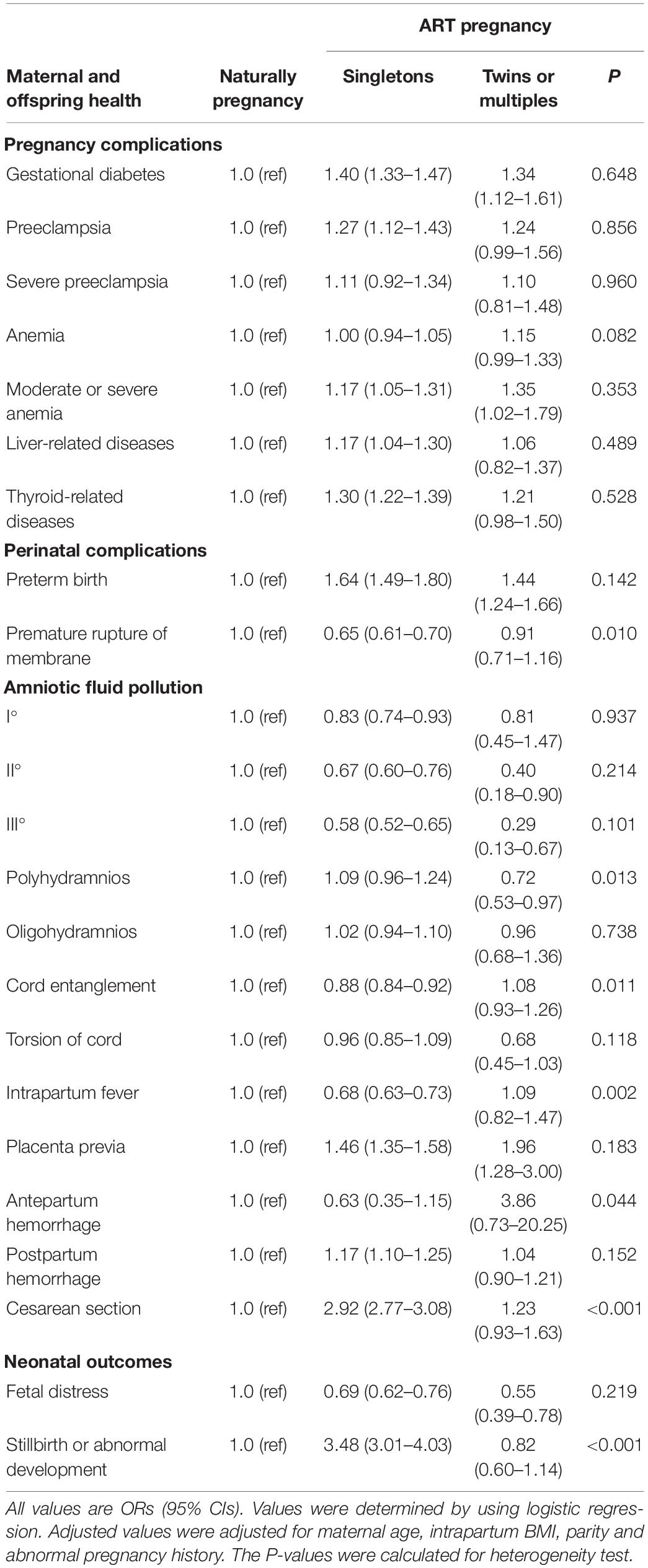
Table 6. Stratified analysis on the association of ART with maternal and offspring health by birth plurality.
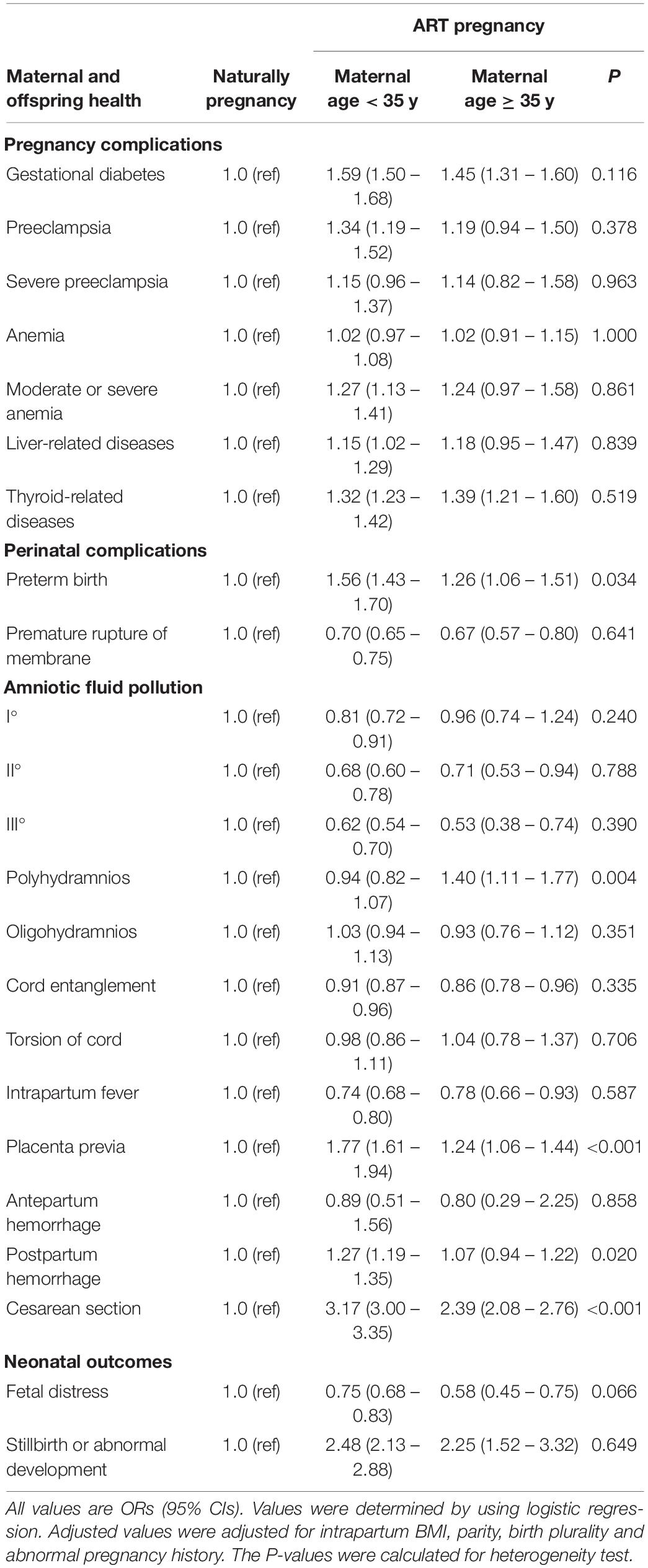
Table 7. Stratified analysis on the association of ART with maternal and offspring health by maternal age.
Discussion
This retrospective, hospital-based cohort study including 13,604 ART pregnancies and 198,002 naturally pregnancies was conducted in Nanjing, China from 2011 to 2020. The study showed the widespread application of ART in China, with the proportion of ART pregnancies increasing year by year in the past decade, and confirmed the increased risks of several adverse pregnancy outcomes in ART pregnancies. We found a 24.2-fold increase in the incidence of multiple births in ART pregnancies compared to naturally pregnancies, then stratified the analysis by birth plurality, suggesting multiple births are indeed an important factor leading to adverse pregnancy outcomes.
In the present study, the increased risks were found in ART pregnancy compared with naturally pregnancy: gestational diabetes (1.39-fold), preeclampsia (1.26-fold), moderate or severe anemia (1.20-fold), liver-related diseases (1.14-fold), thyroid-related diseases (1.29-fold), preterm birth (1.61-fold), placenta previa (1.48-fold), postpartum hemorrhage (1.14-fold), cesarean section (2.84-fold), and stillbirth or abnormal development (2.76-fold), which were largely consistent with the findings of previous studies (10, 28–32). Although these risks were reduced when restriction to singletons, significant differences remained. Some studies have suggested that infertility is one of the risk factors for adverse pregnancy outcomes (33). However, infertility factors cannot fully explain the associations. For infertile women, women conceived with ART had an increased risks of adverse pregnancy outcomes compared with women conceived with non-ART (34). Therefore, some researchers believe that the increased risks of adverse outcomes after ART conception are mainly related to ART manipulation factors (6), which is due to the addition of many non-physiological operations by ART. For example, the type of ovulation induction drugs used in the early stage, the composition of the culture medium, the storage time in the culture medium, the freezing and dissolution process of the embryo, polyspermic fertilization, and the hormone level at the time of implantation, all play an important role in the occurrence of adverse pregnancy outcomes (35). Other studies have pointed out that different methods of ART may lead to different types of adverse pregnancy outcomes (36). At the same time, the longer and more times of ART treatment, the greater the harm to women and their offspring (36). In addition, ART pregnancies may be more closely monitored than naturally pregnancies, which partly explains the higher incidence of adverse pregnancy outcomes in ART pregnancies (37). However, current studies and evidence cannot fully elucidate the mechanism by which ART increases the risk of adverse pregnancy outcomes, and the specific mechanism needs further research.
The main advantage of this study was the large sample size of pregnancy, which allowed us to conduct further subgroup analysis with enough power. And the data obtained from HIS database by using NLP technique is of high quality. However, there are some limitations in this study. First, the population we studied was limited to one city in eastern China (Nanjing). Therefore, we should be cautious in generalizing our findings to other regions. Second, we did not collect information on the ART form. The more intricate and invasive the ART form used, the more likely it was to cause adverse pregnancy outcomes. And the records of pre-pregnancy BMI, baseline endocrine level, causes of infertility, ovarian stimulation protocols, and quality of transferred embryos lacked in our database, were not included in this study. Third, the retrospective design of this study could not assess a causal relationship between ART and adverse pregnancy outcomes. These limitations should be considered in future studies.
Conclusion and Prospect
Women conceived by ART were at increased risks of several adverse pregnancy outcomes compared with women conceived naturally. Multiple pregnancies due to multiple embryos transferred could partly explain the increased risks. The transfer of single embryo of high quality should be promoted. However, ART singleton pregnancy still showed higher risks of several adverse pregnancy outcomes compared with naturally pregnancy, suggesting ART itself is also significantly correlated with pathological pregnancy. Therefore, policies related to ART indications should be strictly formulated to reverse the high rate of ART pregnancy. Given our findings, prenatal and intrapartum monitoring should be strengthened, and neonatal outcomes should be closely observed for ART pregnancy. And more research should be conducted to further clarify whether the increased risk of adverse pregnancy outcomes is due to ART itself, multiple births, or potential infertility.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics Statement
The studies involving human participants were reviewed and approved by the institutional review board of Women’s Hospital of Nanjing Medical University (2020KY-011). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
JW initiated, conceived, and supervised the study. WT and LH did data collection and performed the data analysis. All authors approved the final format of the submitted manuscript.
Funding
This work was supported by the Jiangsu provincial key research and development program (BE2020626).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ART, assisted reproductive technology; ICSI, intracytoplasmic sperm injection; IVF, in vitro fertilization; OI, ovulation induction; GIFT, gamete intra-fallopian transfer; AI, artificial insemination; HIS, hospital information system; NLP, natural language processing; BMI, body mass index; OR, odds ratio; CI, confidence intervals.
References
1. Hu L, Bu Z, Huang G, Sun H, Deng C, Sun Y. Assisted reproductive technology in China: results generated from data reporting system by CSRM from 2013 to 2016. Front Endocrinol (Lausanne). (2020) 11:458. doi: 10.3389/fendo.2020.00458
2. Bai F, Wang DY, Fan YJ, Qiu J, Wang L, Dai Y, et al. Assisted reproductive technology service availability, efficacy and safety in mainland China: 2016. Hum Reprod. (2020) 35:446–52. doi: 10.1093/humrep/dez245
3. European IVF-Monitoring Consortium [EIM] for the European Society of Human Reproduction and Embryology [ESHRE], Calhaz-Jorge C, de Geyter C, Kupka MS, de Mouzon J, Erb K, et al. Assisted reproductive technology in Europe, 2012: results generated from European registers by ESHRE. Hum Reprod. (2016) 31:1638–52. doi: 10.1093/humrep/dew151
4. Farhi A, Reichman B, Boyko V, Hourvitz A, Ron-El R, Lerner-Geva L. Maternal and neonatal health outcomes following assisted reproduction. Reprod Biomed Online. (2013) 26:454–61. doi: 10.1016/j.rbmo.2013.01.014
5. Malchau SS, Loft A, Larsen EC, Aaris Henningsen AK, Rasmussen S, Andersen AN, et al. Perinatal outcomes in 375 children born after oocyte donation: a Danish national cohort study. Fertil Steril. (2013) 99:1637–43. doi: 10.1016/j.fertnstert.2013.01.128
6. Hansen M, Kurinczuk JJ, de Klerk N, Burton P, Bower C. Assisted reproductive technology and major birth defects in Western Australia. Obstet Gynecol. (2012) 120:852–63. doi: 10.1097/AOG.0b013e318269c282
7. Fujii M, Matsuoka R, Bergel E, van der Poel S, Okai T. Perinatal risk in singleton pregnancies after in vitro fertilization. Fertil Steril. (2010) 94:2113–7. doi: 10.1016/j.fertnstert.2009.12.031
8. Rozdarz KM, Flatley CJ, Kumar S. Intrapartum and neonatal outcomes in singleton pregnancies following conception by assisted reproduction techniques. Aust N Z J Obstet Gynaecol. (2017) 57:588–92. doi: 10.1111/ajo.12620
9. Farquhar C, Rishworth JR, Brown J, Nelen WL, Marjoribanks J. Assisted reproductive technology: an overview of Cochrane Reviews. Cochrane Database Syst Rev. (2015) 7:CD010537. doi: 10.1002/14651858.CD010537.pub4
10. Qin J, Liu X, Sheng X, Wang H, Gao S. Assisted reproductive technology and the risk of pregnancy-related complications and adverse pregnancy outcomes in singleton pregnancies: a meta-analysis of cohort studies. Fertil Steril. (2016) 105:73–85.e71–76. doi: 10.1016/j.fertnstert.2015.09.007
11. Jackson S, Hong C, Wang ET, Alexander C, Gregory KD, Pisarska MD. Pregnancy outcomes in very advanced maternal age pregnancies: the impact of assisted reproductive technology. Fertil Steril. (2015) 103:76–80. doi: 10.1016/j.fertnstert.2014.09.037
12. Geisler ME, O’Mahony A, Meaney S, Waterstone JJ, O’Donoghue K. Obstetric and perinatal outcomes of twin pregnancies conceived following IVF/ICSI treatment compared with spontaneously conceived twin pregnancies. Eur J Obstet Gynecol Reprod Biol. (2014) 181:78–83. doi: 10.1016/j.ejogrb.2014.07.033
13. Li Z, Wang YA, Ledger W, Sullivan EA. Birthweight percentiles by gestational age for births following assisted reproductive technology in Australia and New Zealand, 2002-2010. Hum Reprod. (2014) 29:1787–800. doi: 10.1093/humrep/deu120
14. Okun N, Sierra S, Genetics C, Special C. Pregnancy outcomes after assisted human reproduction. J Obstet Gynaecol Can. (2014) 36:64–83.
15. Wen J, Jiang J, Ding C, Dai J, Liu Y, Xia Y, et al. Birth defects in children conceived by in vitro fertilization and intracytoplasmic sperm injection: a meta-analysis. Fertil Steril. (2012) 97:1331–7.e1–e4.
16. Schieve LA, Meikle SF, Ferre C, Peterson HB, Jeng G, Wilcox LS. Low and very low birth weight in infants conceived with use of assisted reproductive technology. N Engl J Med. (2002) 346:731–7. doi: 10.1056/nejmoa010806
17. Seggers J, Pontesilli M, Ravelli ACJ, Painter RC, Hadders-Algra M, Heineman MJ, et al. Effects of in vitro fertilization and maternal characteristics on perinatal outcomes: a population-based study using siblings. Fertil Steril. (2016) 105:590–8.e592.
18. De Neubourg D, Gerris J, Mangelschots K, Van Royen E, Vercruyssen M, Steylemans A, et al. The obstetrical and neonatal outcome of babies born after single-embryo transfer in IVF/ICSI compares favourably to spontaneously conceived babies. Hum Reprod. (2006) 21:1041–6. doi: 10.1093/humrep/dei424
19. De Geyter C, De Geyter M, Steimann S, Zhang H, Holzgreve W. Comparative birth weights of singletons born after assisted reproduction and natural conception in previously infertile women. Hum Reprod. (2006) 21:705–12. doi: 10.1093/humrep/dei378
20. Kozinszky Z, Zadori J, Orvos H, Katona M, Pal A, Kovacs L. Obstetric and neonatal risk of pregnancies after assisted reproductive technology: a matched control study. Acta Obstet Gynecol Scand. (2003) 82:850–6. doi: 10.1034/j.1600-0412.2003.00225.x
21. Woo I, Hindoyan R, Landay M, Ho J, Ingles SA, McGinnis LK, et al. Perinatal outcomes after natural conception versus in vitro fertilization (IVF) in gestational surrogates: a model to evaluate IVF treatment versus maternal effects. Fertil Steril. (2017) 108:993–8. doi: 10.1016/j.fertnstert.2017.09.014
22. Bu Z, Chen ZJ, Huang G, Zhang H, Wu Q, Ma Y, et al. Live birth sex ratio after in vitro fertilization and embryo transfer in China–an analysis of 121,247 babies from 18 centers. PLoS One. (2014) 9:e113522. doi: 10.1371/journal.pone.0113522
23. Moini A, Shiva M, Arabipoor A, Hosseini R, Chehrazi M, Sadeghi M. Obstetric and neonatal outcomes of twin pregnancies conceived by assisted reproductive technology compared with twin pregnancies conceived spontaneously: a prospective follow-up study. Eur J Obstet Gynecol Reprod Biol. (2012) 165:29–32. doi: 10.1016/j.ejogrb.2012.07.008
24. Brekke PH, Rama T, Pilan I, Nytro O, Ovrelid L. Synthetic data for annotation and extraction of family history information from clinical text. J Biomed Semantics. (2021) 12:11. doi: 10.1186/s13326-021-00244-2
25. Son M, Gallagher K, Lo JY, Lindgren E, Burris HH, Dysart K, et al. Coronavirus Disease 2019 (COVID-19) pandemic and pregnancy outcomes in a U.S. Population. Obstet Gynecol. (2021) 138:542–51. doi: 10.1097/AOG.0000000000004547
26. Flythe JE, Assimon MM, Tugman MJ, Chang EH, Gupta S, Shah J, et al. Characteristics and outcomes of individuals with pre-existing kidney disease and COVID-19 admitted to intensive care units in the United States. Am J Kidney Dis. (2021) 77:190-203.e191. doi: 10.1053/j.ajkd.2020.09.003
27. Stephenson AL, Sykes J, Stanojevic S, Quon BS, Marshall BC, Petren K, et al. Survival comparison of patients with cystic fibrosis in Canada and the United States: a population-based cohort study. Ann Intern Med. (2017) 166:537–46. doi: 10.7326/M16-0858
28. Nagata C, Yang L, Yamamoto-Hanada K, Mezawa H, Ayabe T, Ishizuka K, et al. Complications and adverse outcomes in pregnancy and childbirth among women who conceived by assisted reproductive technologies: a nationwide birth cohort study of Japan environment and children’s study. BMC Pregnancy Childbirth. (2019) 19:77. doi: 10.1186/s12884-019-2213-y
29. Vermey BG, Buchanan A, Chambers GM, Kolibianakis EM, Bosdou J, Chapman MG, et al. Are singleton pregnancies after assisted reproduction technology (ART) associated with a higher risk of placental anomalies compared with non-ART singleton pregnancies? A systematic review and meta-analysis. BJOG. (2019) 126:209–18. doi: 10.1111/1471-0528.15227
30. Qin J, Wang H, Sheng X, Liang D, Tan H, Xia J. Pregnancy-related complications and adverse pregnancy outcomes in multiple pregnancies resulting from assisted reproductive technology: a meta-analysis of cohort studies. Fertil Steril. (2015) 103:1492–508.e1491–7. doi: 10.1016/j.fertnstert.2015.03.018
31. Pandey S, Shetty A, Hamilton M, Bhattacharya S, Maheshwari A. Obstetric and perinatal outcomes in singleton pregnancies resulting from IVF/ICSI: a systematic review and meta-analysis. Hum Reprod Update. (2012) 18:485–503. doi: 10.1093/humupd/dms018
32. Esh-Broder E, Ariel I, Abas-Bashir N, Bdolah Y, Celnikier DH. Placenta accreta is associated with IVF pregnancies: a retrospective chart review. BJOG. (2011) 118:1084–9. doi: 10.1111/j.1471-0528.2011.02976.x
33. Lei LL, Lan YL, Wang SY, Feng W, Zhai ZJ. Perinatal complications and live-birth outcomes following assisted reproductive technology: a retrospective cohort study. Chin Med J (Engl). (2019) 132:2408–16. doi: 10.1097/CM9.0000000000000484
34. Pinborg A, Wennerholm UB, Romundstad LB, Loft A, Aittomaki K, Soderstrom-Anttila V, et al. Why do singletons conceived after assisted reproduction technology have adverse perinatal outcome? Systematic review and meta-analysis. Hum Reprod Update. (2013) 19:87–104. doi: 10.1093/humupd/dms044
35. Palomba S, Homburg R, Santagni S, La Sala GB, Orvieto R. Risk of adverse pregnancy and perinatal outcomes after high technology infertility treatment: a comprehensive systematic review. Reprod Biol Endocrinol. (2016) 14:76. doi: 10.1186/s12958-016-0211-8
36. Marino JL, Moore VM, Willson KJ, Rumbold A, Whitrow MJ, Giles LC, et al. Perinatal outcomes by mode of assisted conception and sub-fertility in an Australian data linkage cohort. PLoS One. (2014) 9:e80398. doi: 10.1371/journal.pone.0080398
Keywords: maternal outcomes, neonatal outcomes, art, cohort, China
Citation: Tai W, Hu L and Wen J (2022) Maternal and Neonatal Outcomes After Assisted Reproductive Technology: A Retrospective Cohort Study in China. Front. Med. 9:837762. doi: 10.3389/fmed.2022.837762
Received: 17 December 2021; Accepted: 09 March 2022;
Published: 05 April 2022.
Edited by:
Anis Feki, Fribourg Cantonal Hospital, SwitzerlandReviewed by:
Fangfang Chen, Capital Institute of Pediatrics, ChinaRong Li, Peking University Third Hospital, China
Riadh Ben Temime, Charles Nicolle Hospital, Tunisia
Jing He, Guangzhou Medical University, China
Yichun Guan, The Third Affiliated Hospital of Zhengzhou University, China
Copyright © 2022 Tai, Hu and Wen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lingmin Hu, aHVsaW5nbWluMTk4NkAxMjYuY29t; Juan Wen, d2VuajIwMTBAMTM5LmNvbQ==
 Wen Tai1
Wen Tai1 Juan Wen
Juan Wen