- 1AIXTRA—Competence Center for Training and Patient Safety, Medical Faculty, RWTH Aachen University, Aachen, Germany
- 2Department of Anaesthesiology, University Hospital RWTH Aachen, Medical Faculty, RWTH Aachen University, Aachen, Germany
- 3Center for Medical Simulation, Boston, MA, United States
- 4Department of Anaesthesiology, Critical Care and Pain Medicine, Massachusetts General Hospital, Harvard Medical School, Boston, MA, United States
Background: Sustaining Basic Life Support (BLS) training during the COVID-19 pandemic bears substantial challenges. The limited availability of highly qualified instructors and tight economic conditions complicates the delivery of these life-saving trainings. Consequently, innovative and resource-efficient approaches are needed to minimize or eliminate contagion while maintaining high training standards and managing learner anxiety related to infection risk.
Methods: In a non-inferiority trial 346 first-year medical, dentistry, and physiotherapy students underwent BLS training at AIXTRA—Competence Center for Training and Patient Safety at the University Hospital RWTH Aachen. Our objectives were (1) to examine whether peer feedback BLS training supported by tele-instructors matches the learning performance of standard instructor-guided BLS training for laypersons; and (2) to minimize infection risk during BLS training. Therefore, in a parallel group design, we compared arm (1) Standard Instructor Feedback (SIF) BLS training (Historical control group of 2019) with arm (2) a Tele-Instructor Supported Peer-Feedback (TPF) BLS training (Intervention group of 2020). Both study arms were based on Peyton's 4-step approach. Before and after each training session, objective data for BLS performance (compression depth and rate) were recorded using a resuscitation manikin. We also assessed overall BLS performance via standardized instructor evaluation and student self-reports of confidence via questionnaire. Non-inferiority margins for the outcome parameters and sample size calculation were based on previous studies with SIF. Two-sided 95% confidence intervals were employed to determine significance of non-inferiority.
Results: The results confirmed non-inferiority of TPF to SIF for all tested outcome parameters. A follow-up after 2 weeks found no confirmed COVID-19 infections among the participants.
Conclusion: Tele-instructor supported peer feedback is a powerful alternative to in-person instructor feedback on BLS skills during a pandemic, where infection risk needs to be minimized while maximizing the quality of BLS skill learning.
Trial registration: https://www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00025199, Trial ID: DRKS00025199.
Introduction
The COVID-19 pandemic poses challenges for nearly every aspect of healthcare and healthcare administration. Many of these challenges and risks can be mitigated by pausing or delaying certain kinds of care and encounters. Unfortunately, heart disease and cardiac arrest can neither be paused nor delayed. Sudden cardiac death remains the “top killer,” accounting for almost 9 million fatalities worldwide per year (1, 2). Thus, the need for emergency cardiac care remains constant. Starting CPR promptly with efficient BLS measures is the most important action before professional help arrives (3). Practical BLS training is therefore indispensable to qualify first responders as well as professionals (4–6). But how to prepare laypeople and new healthcare trainees to be ready with key skills, while mitigating infection risk and managing infection-related anxiety is a challenge.
BLS trainings are usually led by a trained instructor (7) and provided in an in-person setting. However, in a pandemic, clusters of people pose significant risk of virus transmission, accelerating the rate of new infections and resulting in a rising number of fatalities (8, 9). Reducing the number of participants trainings becomes extremely expensive making the spatial infrastructural requirements of practical training unattainable. Further, the number of available instructors might be reduced due to illness or quarantine requirements. Therefore, self-directed or peer-guided training approaches are of increasing interest when instructor-based trainings are not permitted or not feasible (10).
A pandemic requires inventive approaches to teaching and learning essential life-saving BLS skills to ensure personal protection and infection control (11, 12). The confluence of pressures to reduce expert input and test alternative peer-guided learning models with the imperatives of infection control during the pandemic urged us to evaluate a new approach. We reasoned that peer feedback aided by tele-instructor input would make it possible to reduce learner group size and to maintain physical distancing as well as infection control during the pandemic.
Peer-guided learning with peer feedback as a key component, is a promising technique in qualifying medical professionals and recommended by the 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care (13). A number of studies have shown positive effects of peer-guided learning for various teaching applications (14–17). It offers great potential to reduce the use of highly trained medical experts as instructors and to replace them completely or partially with peers (10, 17, 18). However, it is essential to assure that peer feedback is directed by the same clear and rigorous standards and instructions (19). We hypothesize that this can be addressed adequately by including a checklist.
Besides, we argue that it is beneficial to include a tele-instructor who can be consulted on demand and trouble-shoot the peer feedback. Remote guidance from a tele-instructor allows expert input, consults, and guidance to play a role in improving or adding to peer guidance. There are a number of examples where telemedicine approaches or telemedicine consultation of experts have been applied very successfully (20–23). This is particularly the case for the cross-location solution of clinical problems or feedback in decision support where the complexity is even higher (20, 21, 24).
Thus, our aim was to develop a tele-instructor supported peer feedback approach for BLS training and to test it for effectiveness with respect to essential learning outcomes. Even after the pandemic, this will ensure that efficient BLS training with comparable training results can be achieved in the absence of medical experts.
Methods
Ethics
Ethical approval (Ethical Committee 376/19 and 428/20) was provided 22.11.2019 and 12.11.2020 by the Ethical Committee of the University Hospital, RWTH Aachen, Pauwelsstraße 30, 52074 Aachen, Germany (Chairperson Prof. Dr. med. G. Schmalzing) and designed according to the ethical principles of the World Medical Association's Declaration of Helsinki (25).
Participants
Participants were students during the first 2 weeks of their medical, dental, or physiotherapy studies at the RWTH Aachen University, Germany. Data assessment took place during a mandatory introductory course on emergency medicine in October 2019 (historical control group) and November 2020 (intervention group). Written informed consent was obtained from all participants.
Study Design
We conducted an intervention study with a historical control group comparing two training methods for BLS skills. In detail, a well-established Standard Instructor Feedback (SIF) conducted by expert instructors (historical control group) was compared with an innovative composed Tele-Instructor Peer Feedback (TPF; intervention group). The TPF was based on peer-feedback, a checklist and optional self-created video recordings combined with an expert tele-instructor. As primary outcome parameters compression depth (CD) and compression rate (CR) within the BLS algorithm were investigated. Adherence to a BLS Algorithm (26, 27) and the assessed self-confidence of the learners were defined as secondary outcome parameters. In 2020, in acknowledgment of the increased risk of virus transmission via mouth-to-mouth ventilation, we omitted ventilations in accordance with the guidelines (26).
The trial aims to assess whether tele-instructor based BLS training was non-inferior to a conventional training approach (28). However, due to an increased infection risk in the 2020 COVID-19 pandemic, a control group using the conventional training approach with group sizes of 12 trainees was not possible. These circumstances led us to using a historical control group for the present study. To minimize any possible bias arising from the time lag, we selected a data set acquired with the conventional approach in the standard group size immediately before the pandemic (October 2019) as control group.
2019 Data Set
The 2019 data set was part of a larger study comparing conventional training to a video-instructed peer-feedback (VPF) training without tele-instructor in a parallel group design. Since it was of no relevance for the topic under investigation, the VPF study arm was not considered in the present study. Results from this condition will be reported elsewhere. No data or results from the 2019 data set have been published before.
2020 Data Set
Similarly, data acquisition in the 2020 study took place in two study arms. Since including an adequate control condition was not possible in 2020, we decided to collect data from a second intervention group, i.e., conventional training with a smaller group size (4 trainees), which can be equally compared with the historical control from 2019. Since this comparison was of no interest for the study presented here, it will be reported elsewhere.
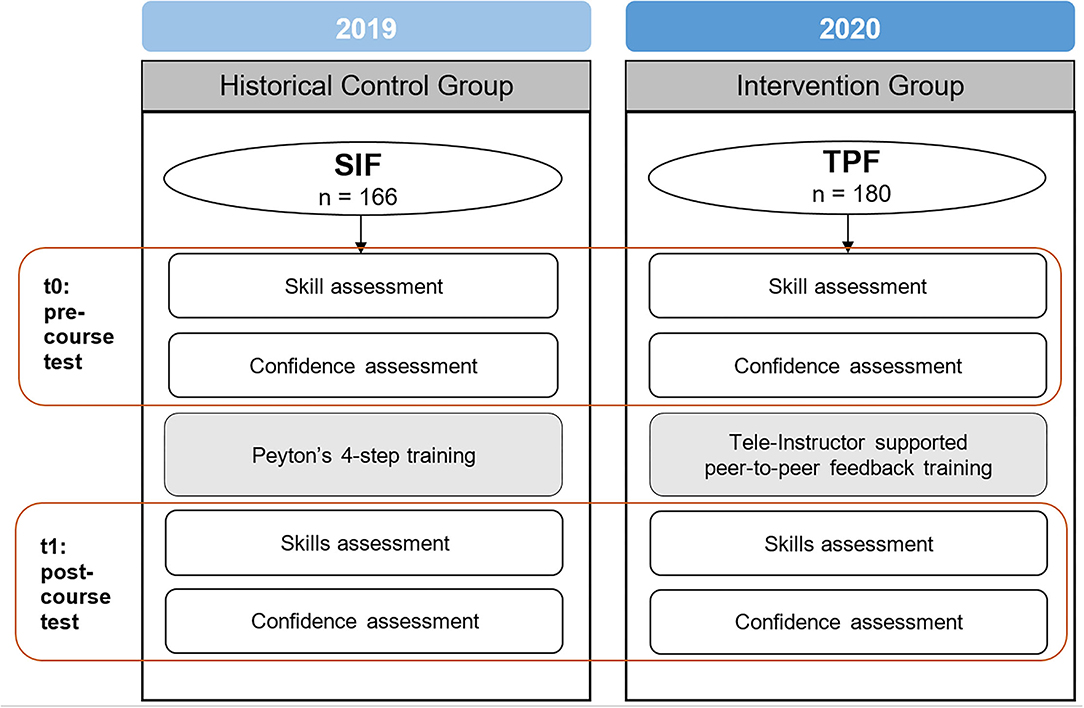
In both years, participants were randomly assigned to one of the two respective study arms (2019: video-instruction based training vs. conventional training in groups of twelve; 2020: tele-instructor-based training vs. conventional training in groups of four). A flow chart of this study is shown in Figure 1. To assure comparability of the training methods regarding complexity and time spent for training, study arms from both years followed a similar structure, based on Peyton's 4-step approach (29). Both training methods used a Resusci AnneTM manikin (Laerdal, Stavanger, Norway). This widely used approach for teaching practical skills like BLS is based on Albert Bandura's social learning theory that emphasizes the social facets of observation, imitation, and modeling (30).
Arm 1: Standard Instructor Feedback Practical Training (SIF) (In-person Groups of 12 Learners From 2019 Data Set)
Following the Peyton four-step model, in step 1, a trained instructor demonstrated correct BLS performance without commentary. In step 2, the demonstration was enriched with detailed step-by-step explanation deconstructing individual steps. In step 3, instructor and student switched roles. The instructor performed BLS guided by the students explaining the steps. In step 4, all learners performed BLS on the manikin themselves and received individual feedback from a qualified instructor. Each participant went through at least two rounds à 2 min of CPR (total duration: 90 min). Vicarious learning strengthens the process as the participants observed the other learners while performing BLS and receiving feedback.
Arm 2: Tele-Instructor Guided Practical Training (TPF) (In-person Groups of 4 Learners From 2020 Data Set)
Following a modified Peyton four-step approach, in step 1, participants watched a video showing a trained instructor demonstrating correct BLS performance without commentary. In step 2, participants watched a video showing a trained instructor demonstrating correct BLS performance with detailed step-by-step explanations. Step 3 was omitted. In step 4, all teams of four students trained independently using the two manikins, assisted by a checklist of quality characteristics. A sample video of an ideal BLS performance was provided for reference and comparison to one's own performance. Subsequently, the peers were allowed to film each other during BLS performance in order to analyse videos of their own performance using the quality checklist. This allowed for both direct and vicarious learning about BLS performance. These activities were repeated until all students got the subjective impression that they had reached an acceptable level of performance and confidence (total duration: 45 min).
Research Questions
RQ1 (Primary research question): Is TPF non-inferior to SIF with respect to BLS performance (CD and CR)?
RQ2: Is TPF non-inferior to SIF with respect to performance of the entire BLS algorithm?
RQ3: Is TPF non-inferior to SIF with respect to self-reported confidence concerning BLS skills?
Skill Assessment
BLS performance was assessed before (t0) and after (t1) the training using the same Resusci AnneTM (Laerdal, Stavanger, Norway) manikin. Students were instructed to imagine the manikin to be a person collapsing next to them and to take all required actions. The scenario was ended 120 s after the first chest compression. Compression depth (CD) and compression rate (CR) were recorded by the manikin's Laerdal PC SkillReporting System Software (Version 2.4.1, Laerdal, Stavanger, Norway).
Correct CD and CR after BLS training were the main learning outcomes. Based on the American Heart Association (AHA) guidelines (31), correct CD was defined as an average value between 50 and 59 mm (32–35). Correct CR was defined as an average rate of 100-120 compressions per minute (32, 36–38).
Participants' performance regarding the BLS algorithm was assessed by an expert rater via a standardized checklist covering safe approach, control of consciousness and of breathing, and emergency call. Sufficient adherence to the algorithm was approved if a participant performed more than 60% of the modified BLS-Algorithm adapted to the COVID-19 Pandemic (26) relevant items correctly.
Afterwards the participants rated their confidence (a) during CPR, (b) mastering an emergency situation and (c) applying BLS in a real-life situation with a non-responsive person. Ratings were obtained before and after training on a 6-point Likert scale (1 = “not at all confident,” 6 = “very confident”).
A graphical representation of the study design is depicted in Figure 1.
Definition of Non-inferiority Margins
The definition of non-inferiority margins was based on the results of previous studies at our training center (39, 40) quantifying the rates of successful BLS after training with Peyton's 4-step approach for various samples of BLS-naive subjects. The results from these studies covered a range of 19% points for both CD (45-64%) and CR (33-52%). Since this outcome variation was present with the standard approach, any outcomes of another training method within these ranges were considered as non-inferior. Thus, for the comparison of TPF and SIF, Δ = −19% was defined as non-inferiority margins for both CD and CR.
Non-inferiority margins for BLS performance were also based on the aforementioned studies, showing a range of 27 percentage points (65-92%). Therefore, Δ = −27% was defined as the non-inferiority margin of the BLS performance.
Since there was no comparable data available for confidence ratings, a difference of −0.5 points (~8%) on the six-point Likert scale was defined as the non-inferiority margin.
Sample Size Planning
Sample size planning for non-inferiority testing was performed in accordance with Blackwelder (41) with the Sealed Envelope Power Calculator (42). For an α significance level of.05 and a power (1 – β) of 90%, the required sample size was N = 236 for CD and N = 234 for CR. We decided for the larger sample size of N = 236 (118 per group).
Randomization
Before the study was conducted, students were allocated to groups of 12 (2019) or 4 (2020) persons by an independent administrative employee of the student's deanery, who was blinded to the study. Allocation was stratified by gender and age to create homogenous groups using a sequence of random numbers. In a next step, groups were assigned to the study arms using a sequence of random numbers taking personnel resources as well as the facilities room and manikin options into account.
Statistical Analysis
Data were analyzed with IBM SPSS Statistics Version 25 (IBM Corp., Armonk, NY, USA). Non-inferiority was assessed by comparing the percentage of successful performances (for CD and CR) after training in both study arms. We used two-sided 95% confidence intervals (CI, according to the recommendations of the CONSORT statement (43) to determine significance of non-inferiority. Significance of results was given for 95% CIs of empirical percentage differences excluding the non-inferiority margin values. CIs for the difference between percentages were calculated with the Wilson score interval method (44) for independent proportions. Analogously, the 95% CI of the difference between the Likert scale confidence ratings in both study arms was used.
Infection Control and Safety Precautions
Intending to minimize the infection risk, each group of students started their trainings with a time delay of 15 min. The wearing of face masks, compliance with distance regulations, and regular use of hand disinfection was compulsory. Upon entering the training center, the body temperature of each student was measured using a contactless infrared thermometer. Cut off for exclusion was >37.5°C. A questionnaire on the current state of health completed the assessment. The code of behavior in the training center was provided online via a learning management system and refreshed at the beginning of each training. To reduce the likelihood of encounters between persons, there was one ascending and one descending staircase, and all walking ways on each floor of the training center were strictly one-way. All materials, chairs, tables, and door handles were disinfected after use at the end of each session. Hand sanitizer was available in every training room and lavatory. Signs repeating all instructions were mounted at the entry to all staircases and on the floor, signs explaining proper use of hand sanitizer were attached next to every disinfectant dispenser. This bundle of measures was approved by the occupational safety department of RWTH Aachen University Hospital and the crisis management team of RWTH Aachen University. Prophylactic PCR testing for the SARS CoV-2 virus was not possible due to capacity and time constraints. Corona rapid tests were not available in sufficient numbers in Germany at the time of data collection or too expensive. In addition, the significance back then was estimated being too low. Two weeks after the training we assessed symptoms of respiratory infection and COVID-19 test results as follow up of the effectiveness of our measures. The following characteristic COVID-19 symptoms were assessed: shortness of breath, coughing, sore throat, limb pain, general feeling of illness, and altered sense of taste or smell.
Technical Requirements for the Peer-Feedback Arm
While no media support was required for the SIF method, in TPF group we used one notebook ensuring the tele-support and two tablets providing the instructional videos. Mobile as well as static solutions are possible.
Results
Sample Characteristics
Data from N = 395 participants (268 female, age 20.56 ± 3.68 years) were gathered. Due to absence during data collection, incomplete data or non-matching participant codes, 49 participants were excluded from the analyses leaving a final study sample of n = 346 (n = 180 in TPF; n = 166 SIF). Both study groups—SIF (2019) and TPF (2020)—were highly similar with respect to age (2019: 20.59 ± 3.64 years; 2020: 20.28 ± 2.79 years) and gender distribution (2019: 120 female, 55 male; 2020: 122 female, 57 male). Skills in resuscitation prior to participation in the study can be assumed for a part of the sample due to previous medical qualifications (2019: 17.6%; 2020: 23.3%), two-day courses in first aid (2019: 45.5%; 2020: 44.0% and 1-day courses in life-saving emergency measures (2019: 78.4%; 2020: 88.5%).
Descriptive Data
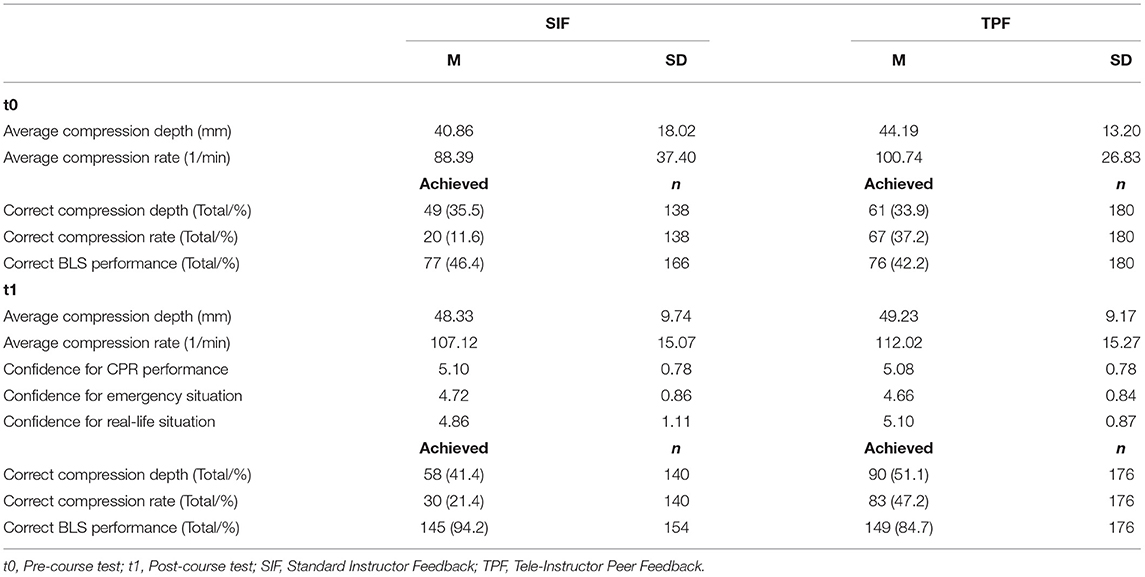
Pre-training performance data and self-reported confidence ratings for the SIF group and the TPF group are reported in Table 1.
Non-inferiority Analysis
Results of non-inferiority analyses are displayed in Figures 2, 3 which show the respective proportion differences between the SIF group of 2019 and the TPF group of 2020 on a 95% CI. Values < 0 favor SIF and values > 0 favor TPF. The blue line indicates the respective non-inferiority margin (Δ). For CD and CR, the inferiority margin was set at Δ = −19 % whereas for BLS performance data it was set at Δ = −27 % based on empirical values from prior data. The non-inferiority margin for confidence ratings was Δ = −0.5 points.
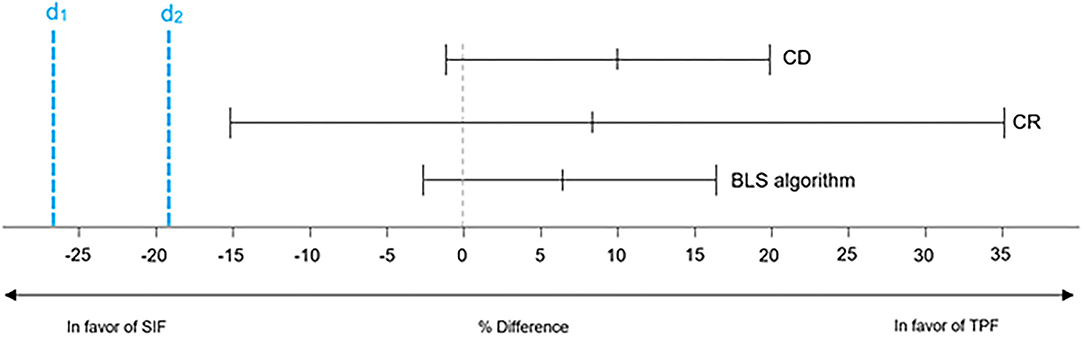
Figure 2. Non-Inferiority results for compression depth, compression rate and BLS algorithm. d1, non-inferiority margin set at Δ = −19% for compression depth and compression rate; d2, non-inferiority margin set at Δ = −27 % for BLS algorithm; CD, Compression depth; CR, Compression rate; BLS, Basic Life Support; SIF, Standard Instructor Feedback; TPF, Tele-Instructor Peer Feedback.
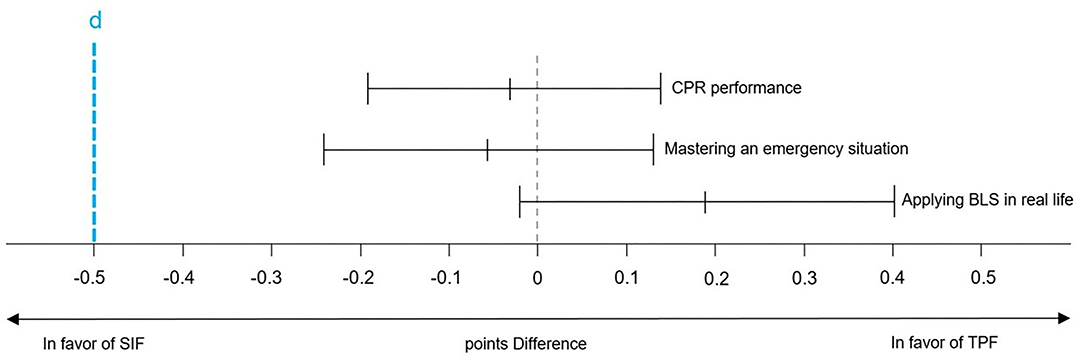
Figure 3. Non-inferiority confidence ratings. CPR, Cardiopulmonary Resuscitation; BLS, Basic Life Support; SIF, Standard Instructor Feedback; TPF, Tele-Instructor Peer Feedback.
Compression Depth
After training, 41.4 % of the participants in the SIF and 51.1 % in the TPF group achieved a correct CD, resulting in a proportion difference of 9.7 % in favor of TPF. The 95% CI for the proportion difference was −1.4-20.4%. The results indicate significant non-inferiority of the TPF group.
Compression Rate
After training, 21.4% of the participants in the SIF and 47.2% in the TPF group achieved a correct CR, resulting in a proportion difference of 25.8% in favor of TPF. The 95% CI for the proportion difference was 15.3-35.2%. The results indicate a significant non-inferiority of the TPF group.
BLS Performance
After training, 94.2% of the participants in the SIF and 84.7% in the TPF group achieved a correct CD, resulting in a proportion difference of 9.5% in favor of SIF. The 95% CI for the proportion difference was 2.8-16.2%. The results indicate significant non-inferiority of the TPF group.
Confidence Ratings
Mean differences between the two groups were 0.02 points (95 % CI: −0.14-0.19) regarding confidence in one's CPR performance, 0.06 points (95 % CI: −0.12-0.24) in terms of confidence in an emergency situation and 0.24 points (95 % CI: −0.40-0.23) in real-life situations. The results indicate significant non-inferiority of the TPF group for all three items. The results are depicted in Table 1 and Figure 3.
COVID-19 Health Measurements
Body Temperature
Average body temperature on the day of study participation was 35,99°C (SD: 0,69°C). One participant was excluded from the training due to high temperature (37,8°C).
Infection Risk
After 2 weeks, 243 participants responded to the follow-up questionnaire. Among these, 236 participants (97.1%) reported none of the assessed COVID-19 symptoms. No participant reported a positive PCR test. Among the remaining 7 participants, 2 reported coughing, 4 reported a sore throat, one reported shortness of breath, and one reported general feeling of illness. In summary, there was no indication for an increased prevalence of COVID-19 cases after training participation.
Tele-Instructor Peer Feedback Efficiency
It is important to highlight that the TPF group needed only half of the training time of SIF to accomplish comparable results. The essential instructors could offer support to the double number of participants. This does not take into account the savings made by halving the training time for the participants. From an economic point of view, personnel cost thus could be significantly reduced using TPF instead of SIF.
Discussion
In times of a pandemic, when physical distancing is one of the most important methods of infection control, how to both train large numbers of people and do it safely require innovation in training methods. In the present study, we investigated non-inferiority of a new pandemic-adapted learning approach addressing BLS, with respect to essential learning outcomes. The results confirmed non-inferiority of the tele-instructor guided peer feedback method with respect to compression depth and compression rate.
Furthermore, the overall performance of the BLS algorithm, and self-reported confidence were comparable between groups as well. Results of the health status follow-up showed no sign of an elevated COVID-19 infection risk for the BLS course participants. Thus, BLS training with tele-instructor guided peer feedback is a valuable and effective alternative to traditional large group in-person instructor training. It combines the spatial and temporal flexibility of peer teaching with the expert support of instructor guidance, while simultaneously allowing for small group sizes and low costs. This seems an optimal way to fight sudden cardiac death even in pandemic times.
Beyond aspects of practical realization, the use of peer feedback in medical education has long since been discussed and recommended (45). Nonetheless, it is not well anchored as a teaching method in current medical curricula. One reason could be a potential pitfall of peer teaching: peers are usually no experts, and feedback may sometimes be erroneous. Accordingly, it seems that some clinicians and medical educators do not trust the method and avoid it in their teaching (46). TPF can address this issue in a two-fold manner. First, the use of a checklist makes peer feedback and its underlying criteria more objective. Second, the consultation of a professional tele-instructor adds essential expert knowledge and can avoid errors and uncertainties. The TPF approach accordingly combines positive learning effects of peer feedback and instructor guidance. We therefore suggest that TPF can enhance clinical educator's trust in peer feedback and foster the implementation of peer feedback teaching in the medical curriculum.
Both interventions differed in a number of factors which may have contributed to the comparable training effects to varying degrees. A potential factor to students' non-inferior performance of CD and CR in the TPF group could be the possibility to analyse their own performance in detail by means of the video recordings. This hypothesis is in line with the findings by Bezemer et al. who found beneficial effects of video recordings on subsequent performance and team communication on the surgical ward (47). To continue, the amount of practice time on the manikin is likely to have differed among groups. Whereas the degree of peer observation was higher among participants in the SIF condition (12 participants and 1 manikin), the ratio of manikin to student in the TPF group was 1:2 and thus allowed for more practice-oriented experience. Referring to Bandura's Social Learning Theory (30), learning in the SIF notably occurred through observation of the instructor and peers, whereas learning in the TPF group was particularly enhanced by the practical reproduction of the acquired skill.
Amparore et al. exemplified the decline in continuing medical education during the pandemic in urology residents (48). Due to its low requirements, the TPF approach could be used for BLS trainings in other settings like universities, schools, sports clubs, companies etc. as well. Moreover, the teaching approach tested is not limited to BLS training. By supplying learners with excellent educational material in advance, practical training of almost every basic as well as some complex clinical skills (e.g., central venous catheters or airway management techniques) can be trained using a tele-instructor. Even continuing medical education in practical skills could be provided wider by means of TPF and thus be strengthened.
The necessary technical equipment can be acquired at low costs and easily adjusted to various settings in order to vastly reduce the deployment of instructors. Necessary skills using videoconferencing software (e.g., managing breakout sessions, using the chat) are easily acquired. Furthermore, the online support of trainees can be performed in home office. During a pandemic this can be an enormous advantage regarding the feasibility of BLS trainings. In addition to a minimized infection risk, instructors can back up each other, which remains relevant even after the pandemic. In our current situation, distance regulations required 4 m2 space per participant. Hand disinfection needed to be available in every room and lavatories had to be close by. An optimal floor plan is therefore required to ensure participants can enter and leave rooms without queuing and passing by other participants.
The present study has some limitations. Our study sample consisted of young, well-educated, and medically interested learners. Studies on comparable samples are widely distributed, and a potential transferability to the general population has been claimed as the participants had not yet entered the regular medical curriculum (49). Nevertheless, generalization of our findings requires investigations of other layperson populations. This could be achieved with a superiority trial based on an intention to treat sample in the context of public courses on resuscitation. Taking into account that the strength of TPF lies in its broad and easy applicability, this design might prove that TPF—on cohort level—achieves even better training results than SIF since it can reach more trainees. This is especially of interest in times of a pandemic. However, easier applicability may also promote population-wide BLS trainings beyond crisis situations.
Moreover, the TPF group could decide for themselves when to contact the tele-instructor, which bears the risk of undetected inaccurate performance. To reduce this threat, either contacting the tele-instructor could be mandatory or the training room could be under video surveillance while training takes place, empowering the tele-instructor to intervene if there is a need for improvement. The second option will make strict rules for privacy protection necessary.
Teaching the COVID-algorithm of BLS (26), this study does not permit any conclusion on rescue breathing. Acknowledging the possibility for untrained laypersons to perform compression-only CPR (31), this aspect may be considered negligible. However, as soon as it is reasonably possible to practice rescue breathing without elevated risk of infection, this aspect should also be examined in further investigations. Knowing that bag-mask ventilation with an HME filter could be an alternative to mouth-to-mouth ventilation for rescuers, we decided not to use this technique acknowledging of the lack of necessary equipment for laypersons.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethical Committee of the University Hospital Chairperson Prof. Dr. med. G. Schmalzing RWTH Aachen Pauwelsstraße 30 52074 Aachen Germany. Written informed consent was obtained from all participants.
Author Contributions
MTS contributed substantially to the designing of this study as well as the acquisition, analysis, and interpretation of the data and has written the manuscript. MS, MK, and SS contributed substantially to the planning and designing of this study, the statistical analysis as well as the interpretation of the data. JR critically revised the manuscript for important intellectual content and made substantial contributions to the manuscript. SL, LV, and SS assisted in critically reviewing the manuscript. AK substantially contributed to the practical implementation of the study. SS supervised the study and supported MTS as senior investigator. All authors have made contributions to the manuscript and reviewed and revised the manuscript.
Funding
This study was financed by regular departmental funding for research and education of RWTH Aachen.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.825823/full#supplementary-material
Abbreviations
BLS, Basic Life Support; CD, Compression Depth; CI, Confidence Interval; CPR, Cardiopulmonary Resuscitation; CR, Compression Rate; ECC, External Chest Compression; SIF, Standard Instructor Feedback; TPF, Tele-Instructor Peer-Feedback.
References
1. Wong CX, Brown A, Lau DH, Chugh SS, Albert CM, Kalman JM, et al. Epidemiology of sudden cardiac death: global and regional perspectives. Hear Lung Circ. (2019) 28:6–14. doi: 10.1016/j.hlc.2018.08.026
3. Herlitz J, Bång A, Alsén B, Aune S. Characteristics and outcome among patients suffering from in hospital cardiac arrest in relation to the interval between collapse and start of CPR. Resuscitation. (2002) 53:21–7. doi: 10.1016/S0300-9572(01)00485-3
4. Roshana S. Basic life support: knowledge and attitude of medical/paramedical professionals. World J Emerg Med. (2012) 3:141–5. doi: 10.5847/wjem.j.issn.1920-8642.2012.02.011
5. Wik L, Kramer-Johansen J, Myklebust H, Sørebø H, Svensson L, Fellows B, et al. Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. J Am Med Assoc. (2005) 293:299–304. doi: 10.1001/jama.293.3.299
6. Willmore RD. Do medical students studying in the United Kingdom have an adequate factual knowledge of basic life support? World J Emerg Med. (2019) 10:75–80. doi: 10.5847/wjem.j.1920-8642.2019.02.002
7. García-Suárez M, Méndez-Martínez C, Martínez-Isasi S, Gómez-Salgado J, Fernández-García D. Basic life support training methods for health science students: a systematic review. Int J Environ Res Public Health. (2019) 16:768. doi: 10.3390/ijerph16050768
8. Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. (2020) 395:1973–87. doi: 10.1016/S0140-6736(20)31142-9
9. Teslya A, Thi MP, Godijk NG, Kretzschmar ME, Bootsma MCJ, Rozhnova G. Impact of self-imposed prevention measures and short-term government-imposed social distancing on mitigating and delaying a COVID-19 epidemic : a modelling study. PLoS Med. (2020) 17:e10033166. doi: 10.1371/journal.pmed.1003166
10. Brydges R, Nair P, Ma I, Shanks D, Hatala R. Directed self-regulated learning versus instructor-regulated learning in simulation training. Med Educ. (2012) 46:648–56. doi: 10.1111/j.1365-2923.2012.04268.x
11. Bridgwood B, Sabbagh C, Houghton J, Pepper C, Sayers R. Medical education in a post COVID-19 era – remote teaching methods for cardiovascular knowledge and skills. MedEdPublish. (2021) 10:62. doi: 10.15694/mep.2021.000062.1
12. Kim Y, Han H, Lee S, Lee J. Effects of the non-contact cardiopulmonary resuscitation training using smart technology. Eur J Cardiovasc Nurs. (2021) 20:760-6. doi: 10.1093/eurjcn/zvaa030
13. Cheng A, Magid DJ, Auerbach M, Bhanji F, Bigham BL, Blewer AL, et al. Part 6: resuscitation education science: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. (2020) 142:551–79. doi: 10.1161/CIR.0000000000000903
14. Priftanji D, Cawley MJ, Finn LA, Hollands JM, Morel DW, Siemianowski LA, et al. Performance and retention of basic life support skills improve with a peer-led training program. Curr Pharm Teach Learn. (2018) 10:744–9. doi: 10.1016/j.cptl.2018.03.006
15. Sopka S, Beemelmanns S, Rex S, Beckers SK, Stieger L, Rossaint R, et al. Peer-assisted learning in intensive care graduate teaching - concerning value increase for intensive care medicine! Intensive Care Med. (2015) 56:206–15.
16. Field M, Burke JM, McAllister D, Lloyd DM. Peer-assisted learning: a novel approach to clinical skills learning for medical students. Med Educ. (2007) 41:411–8. doi: 10.1111/j.1365-2929.2007.02713.x
17. Hughes TC, Jiwaji Z, Lally K, Lloyd-Lavery A, Lota A, Dale A, et al. Advanced cardiac resuscitation evaluation (ACRE): a randomised single-blind controlled trial of peer-led vs. expert-led advanced resuscitation training. Scand J Trauma Resusc Emerg Med. (2010) 18:1–6. doi: 10.1186/1757-7241-18-3
18. Stenberg M, Mangrio E, Bengtsson M, Carlson E. Formative peer assessment in higher healthcare education programmes: a scoping review. BMJ Open. (2021) 11:e045345. doi: 10.1136/bmjopen-2020-045345
19. Tai J, Molloy E, Haines T, Canny B. Same-level peer-assisted learning in medical clinical placements: a narrative systematic review. Med Educ. (2016) 50:469–84. doi: 10.1111/medu.12898
20. Follmann A, Schröder H, Neff G, Rossaint R, Hirsch F, Felzen M. When emergency physician and tele-emergency physician save life together: a case description on the application of prehospital telemedicine for ventricular tachycardia with hemodynamic instability. Anaesthesist. (2021) 70:34–9. doi: 10.1007/s00101-020-00872-w
21. Gnirke A, Beckers SK, Gort S, Sommer A, Schröder H, Rossaint R, et al. Analgesia in the emergency medical service: comparison between tele-emergency physician and call back procedure with respect to application safety, effectiveness and tolerance. Anaesthesist. (2019) 68:665–75. doi: 10.1007/s00101-019-00661-0
22. Novara G, Checcucci E, Crestani A, Abrate A, Esperto F, Pavan N, et al. Telehealth in urology: a systematic review of the literature. how much can telemedicine be useful during and after the COVID-19 pandemic? Eur Urol. (2020) 78:786–811. doi: 10.1016/j.eururo.2020.06.025
23. Checcucci E, De Luca S, Alessio P, Verri P, Granato S, De Cillis S, et al. Implementing telemedicine for the management of benign urologic conditions: a single centre experience in Italy. World J Urol. (2021) 39:3109–15. doi: 10.1007/s00345-020-03536-x
24. Bergrath S, Reich A, Rossaint R, Rörtgen D, Gerber J, Fischermann H, et al. Feasibility of prehospital teleconsultation in acute stroke - a pilot study in clinical routine. PLoS ONE. (2012) 7:e36796. doi: 10.1371/journal.pone.0036796
25. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. (2013) 310:2191–4. doi: 10.1001/jama.2013.281053
26. Nolan JP, Monsieurs KG, Bossaert L, Böttiger BW, Greif R, Lott C, et al. European resuscitation council COVID-19 guidelines executive summary. Resuscitation. (2020) 153:145–55. doi: 10.1016/j.resuscitation.2020.06.001
27. Perkins GD, Handley AJ, Koster RW, Castrén M, Smyth MA, Olasveengen T, et al. European Resuscitation Council Guidelines for Resuscitation (2015) Section 2. Adult basic life support and automated external defibrillation. Resuscitation. (2015) 95:81–99. doi: 10.1016/j.resuscitation.2015.07.015
28. Klasen M, Sopka S. Demonstrating equivalence and non-inferiority of medical education concepts. Med Educ. (2020) 55:455–61. doi: 10.1111/medu.14420
29. Peyton JWR. Teaching in the theatre. In: Peyton JWR, editor. Teaching and Learning in Medical Practice. Rickmansworth: Manticore Europe (1998). p. 171–80.
31. Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG, et al. Part 3: adult basic and advanced life support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. (2020) 142:366–468. doi: 10.1161/CIR.0000000000000916
32. Stiell IG, Brown SP, Nichol G, Cheskes S, Vaillancourt C, Callaway CW, et al. What is the optimal chest compression depth during out-of-hospital cardiac arrest resuscitation of adult patients? Circulation. (2014) 130:1962–70. doi: 10.1161/CIRCULATIONAHA.114.008671
33. Stiell IG, Brown SP, Christenson J, Cheskes S, Nichol G, Powell J, et al. What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation? Crit Care Med. (2012) 40:1192–8. doi: 10.1097/CCM.0b013e31823bc8bb
34. Babbs CF, Kemeny AE, Quan W, Freeman G. A new paradigm for human resuscitation research using intelligent devices. Resuscitation. (2008) 77:306–15. doi: 10.1016/j.resuscitation.2007.12.018
35. Edelson DP, Abella BS, Kramer-Johansen J, Wik L, Myklebust H, Barry AM, et al. Effects of compression depth and pre-shock pauses predict defibrillation failure during cardiac arrest. Resuscitation. (2006) 71:137–45. doi: 10.1016/j.resuscitation.2006.04.008
36. Kilgannon JH, Kirchhoff M, Pierce L, Aunchman N, Trzeciak S, Roberts BW. Association between chest compression rates and clinical outcomes following in-hospital cardiac arrest at an academic tertiary hospital. Resuscitation. (2017) 110:154–61. doi: 10.1016/j.resuscitation.2016.09.015
37. Abella BS, Sandbo N, Vassilatos P, Alvarado JP, O'Hearn N, Wigder HN, et al. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrest. Circulation. (2005) 111:428–34. doi: 10.1161/01.CIR.0000153811.84257.59
38. Hwang SO, Cha KC, Kim K, Jo YH, Chung SP, You JS, et al. A randomized controlled trial of compression rates during cardiopulmonary resuscitation. J Korean Med Sci. (2016) 31:1491–8. doi: 10.3346/jkms.2016.31.9.1491
39. Sopka S, Biermann H, Rossaint R, Knott S, Skorning M, Brokmann JC, et al. Evaluation of a newly developed media-supported 4-step approach for basic life support training. Scand J Trauma Resusc Emerg Med. (2012) 20:37. doi: 10.1186/1757-7241-20-37
40. Sopka S, Biermann H, Rossaint R, Rex S, Jäger M, Skorning M, et al. Resuscitation training in small-group setting - gender matters. Scand J Trauma Resusc Emerg Med. (2013) 21:30. doi: 10.1186/1757-7241-21-30
41. Blackwelder WC. “Proving the null hypothesis” in clinical trials. Control Clin Trials. (1982) 3:345–53. doi: 10.1016/0197-2456(82)90024-1
43. Piaggio G, Elbourne DR, Altman DG, Pocock SJ, Evans SJW. Reporting of noninferiority and equivalence randomized trials: An extension of the CONSORT statement. J Am Med Assoc. (2006) 295:1152–60. doi: 10.1001/jama.295.10.1152
44. Newcombe RG. Interval estimation for the difference between independent proportions: comparison of eleven methods. Stat Med. (1998) 17:873–90.
46. Nelson AJ, Nelson S V, Linn AMJ, Raw LE, Kildea HB, Tonkin AL. Tomorrow's educators..today? Implementing near-peer teaching for medical students. Med Teach. (2013) 35:156–9. doi: 10.3109/0142159X.2012.737961
47. Bezemer J, Cope A, Korkiakangas T, Kress G, Murtagh G, Weldon SM, et al. Microanalysis of video from the operating room: An underused approach to patient safety research. BMJ Qual Saf. (2017) 26:583–7. doi: 10.1136/bmjqs-2016-005816
48. Amparore D, Claps F, Cacciamani GE, Esperto F, Fiori C, Liguori G, et al. Impact of the COVID-19 pandemic on urology residency training in Italy. Minerva Urol e Nefrol. (2020) 72:505–9. doi: 10.23736/S0393-2249.20.03868-0
Keywords: basic life support (BLS), Cardiopulmonary Resuscitation (CPR), external chest compression (ECC), tele-instructor, telehealth, historical control, peer-teaching, non-inferiority
Citation: Schauwinhold MT, Schmidt M, Rudolph JW, Klasen M, Lambert SI, Krusch A, Vogt L and Sopka S (2022) Innovative Tele-Instruction Approach Impacts Basic Life Support Performance: A Non-inferiority Trial. Front. Med. 9:825823. doi: 10.3389/fmed.2022.825823
Received: 30 November 2021; Accepted: 19 April 2022;
Published: 12 May 2022.
Edited by:
Artem N. Kuzovlev, Research Institute General Resuscitation im.V.A.Negovskogo, RussiaReviewed by:
Jacek Smereka, Wroclaw Medical University, PolandEnrico Checcucci, IRCCS Candiolo Cancer Institute, Italy
Copyright © 2022 Schauwinhold, Schmidt, Rudolph, Klasen, Lambert, Krusch, Vogt and Sopka. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michael Tobias Schauwinhold, bXNjaGF1d2luaG9sZEB1a2FhY2hlbi5kZQ==
 Michael Tobias Schauwinhold
Michael Tobias Schauwinhold Michelle Schmidt
Michelle Schmidt Jenny W. Rudolph3,4
Jenny W. Rudolph3,4 Martin Klasen
Martin Klasen Lina Vogt
Lina Vogt Saša Sopka
Saša Sopka