
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Med., 13 June 2022
Sec. Infectious Diseases – Surveillance, Prevention and Treatment
Volume 9 - 2022 | https://doi.org/10.3389/fmed.2022.822680
This article is part of the Research TopicImmune Responses to HIV Infection: Basic, Clinical and Translational Research in East and Southeast AsiaView all 43 articles
 Jianzhou Yang1†
Jianzhou Yang1† Maohe Yu2†
Maohe Yu2† Gengfeng Fu3†
Gengfeng Fu3† Guanghua Lan4†
Guanghua Lan4† Linghua Li5†
Linghua Li5† Ying Qiao6†
Ying Qiao6† Jin Zhao7†
Jin Zhao7† Han-Zhu Qian8
Han-Zhu Qian8 Xiangjun Zhang9
Xiangjun Zhang9 Xinchao Liu10
Xinchao Liu10 Xia Jin11
Xia Jin11 Guohong Chen3
Guohong Chen3 Yuan Fang12
Yuan Fang12 Zixin Wang13,*,‡
Zixin Wang13,*,‡ Junjie Xu14,*,‡
Junjie Xu14,*,‡People living with HIV (PLWH), if infected with Coronavirus Disease 2019 (COVID-19), had an increased risk of mortality compared to people without HIV infection. They are considered as a priority group to receive COVID-19 vaccination. This cross-sectional online survey investigated the prevalence of and factors associated with COVID-19 vaccination uptake among 2740 PLWH aged 18–65 years in eight Chinese metropolitan cities between January and February 2021. As validated by requesting participants to send an image of receipt hiding personal identification, 6.2% of PLWH had taken up COVID-19 vaccination. Participants living in cities where individuals could make an appointment to receive COVID-19 vaccination reported significantly higher uptake than those living in cities without such allowance (11.0 vs. 2.9%, p < 0.001). Being a member of priority groups to receive vaccination, concerning about the side effects of COVID-19 vaccination and its interaction with HIV treatment, and exposing to information on the Internet/social media supporting PLWH to receive COVID-19 vaccination were significantly associated with COVID-19 vaccination uptake in both groups of participants. Receiving advice from the staff of community-based organizations supporting COVID-19 vaccination was associated with higher uptake among participants living in cities where individuals could make an appointment to receive such vaccination, while a shortage in COVID-19 vaccine supply was associated with a lower uptake among participants living in other cities. Our findings presented a snapshot of COVID-19 vaccination uptake among PLWH in the early phase of vaccine rollout in China. It provided a knowledge basis to formulate interventions promoting COVID-19 vaccination for PLWH.
Coronavirus Disease 2019 (COVID-19) vaccination and other behavioural preventive measures can help to control the ongoing pandemic. Worldwide, COVID-19 vaccination programs started to rollout in December 2020. China initiated the nationwide COVID-19 vaccination program on December 15, 2020 (1, 2). The program was first scaled up in large cities. At the time when this study was conducted (January to February 2021), two COVID-19 vaccination delivery models were implemented simultaneously in China. Individuals could make an appointment to receive COVID-19 vaccination in some cities, whereas vaccination was mainly arranged by the employers, and did not allow individuals to make an appointment in other cities. People had the right to refuse the arrangement. Since the amount of vaccines was inadequate to cover the entire Chinese population during the early phase of rollout, priority was given to several subgroups with increased risks of COVID-19, including people who were working for pandemic control, border control, public transportation, cold-chain, and healthcare workers, as well as those who needed to travel abroad for work or study. Health risk groups (e.g., older adults, people with chronic conditions or immunodeficiency) were not listed as priority groups during the same period, partly due to the lack of sufficient evidence on immunogenicity and safety. Only two types of inactivated COVID-19 vaccines, the Sinovac CoronaVac and Sinopharm, were available during the study period. There were no differences in the availability or indications for these two inactivated vaccines during the study period. By the end of February 2021, 52.5 million doses of COVID-19 vaccines were administered in China (3).
A recent systematic review and meta-analysis suggested that as compared to people without HIV infection, people living with HIV (PLWH) had comparable risk of COVID-19 and risk of developing severe COVID-19 symptoms (4). PLWH, if infected with COVID-19, had an increased risk of mortality compared to those without HIV infection (4). COVID-19 vaccination was effective and safe for PLWH (5). The World Health Organization (WHO), the United States Department of Health and Human Services, the British HIV Association, and health authorities in Australia strongly recommend PLWH to receive COVID-19 vaccination regardless of their CD4+ T-cell counts (6–9). PLWH is one of the priority groups to receive COVID-19 vaccination in various countries (7–9). At the time when this study was conducted, people with immunodeficiency in China needed to seek advice from doctors about whether they should receive COVID-19 vaccination (10). The China national guideline on COVID-19 vaccination was updated 1 month after this study was completed and recommended COVID-19 vaccination to all PLWH (10).
The effectiveness of COVID-19 vaccination program is dependent on both the vaccines' effectiveness and people's willingness to be vaccinated. International health authorities advocate all people without a contraindication should receive COVID-19 vaccination (11). The WHO identified vaccine hesitancy as one major threat to global health (12). A systematic review reported that COVID-19 vaccine hesitancy was a global phenomenon (13, 14). Globally, the number of new COVID-19 cases is rising. Vaccine hesitancy constitutes a threat to tackling the pandemic (15).
Therefore, it is helpful for governments to plan interventions to reduce vaccine hesitancy. In order to promote the COVID-19 vaccination of PLWH, it is necessary to understand their facilitators and barriers to take up COVID-19 vaccination. However, most studies investigating COVID-19 vaccination hesitancy were conducted among the general population and medical professionals (13, 16), and the findings might not be applicable to PLWH. Our literature review identified three studies investigated the willingness to receive COVID-19 vaccination among PLWH in the United States, France and China (17–19). In France and the United States, the proportion of PLWH who were willing to receive COVID-19 vaccination was comparable to those of the general population (France: 72.3% in PLWH vs. 52–76% in the general population; the United States: 68% in PLWH vs. 44–75% in the general population) (17, 18, 20). Our published study showed that 57.2% of unvaccinated PLWH in China were willing to receive COVID-19 vaccination, which was lower than that of the general population (19, 20). Concerns about their health, and the belief that COVID-19 vaccination should be mandatory and important for people with chronic disease were associated with higher willingness to receive COVID-19 vaccination, while previous history of vaccination refusal, mistrust in public health information, and concerns related to side effects were shown to be barriers (17–19). Receiving advice supportive of COVID-19 vaccination for PLWH was associated with higher willingness to receive such vaccination (19). However, there were no studies looking at the actual uptake of COVID-19 vaccination among PLWH. Factors associated with the willingness and actual uptake of COVID-19 vaccination might be different (21). Investigating the willingness and actual uptake of COVID-19 vaccination has different implications. Understanding the willingness and associated factors would inform planning of future health promotion, while looking at the actual uptake provides a snapshot of the implementation of the vaccination program.
This study applied the socio-ecological model as the conceptual framework to explain factors associated with actual uptake of COVID-19 vaccination among PLWH (22). The model considers determinants of a health behavior at the individual, interpersonal and social-structural levels (22). Interventions addressing determinants of a health behavior at multiple levels are more likely to be successful. Previous studies on COVID-19 supported the applicability of the socio-ecological model (23).
This study investigated the prevalence of COVID-19 vaccination uptake among PLWH in China. This study investigated whether factors at different levels (socio-structural, interpersonal, and individual levels) associated with the actual uptake of COVID-19 vaccination were the same in cities with different vaccination delivery models (allowing and not allowing individuals to make an appointment) to receive such vaccine. Our hypotheses were: (1) prevalence of actual uptake of COVID-19 vaccination would be different in cities with different vaccination delivery models, and (2) factors associated with actual uptake would be different under different delivery models.
This is a multicenter cross-sectional online survey conducted between January and February 2021. The study sites covered eight conveniently selected large Chinese cities, including two in the North (Tianjin and Beijing), two in the Northeast (Shenyang, Hohhot), one in the East (Nanjing), and three in the South (Nanning, Guangzhou and Shenzhen). We selected these cities as the COVID-19 vaccination program was first scaled up in these cities. At the time of this study, people in Beijing, Guangzhou, and Shenzhen could make an appointment to receive COVID-19 vaccination. In these cities, people could download a smartphone application developed by the health bureau to schedule their COVID-19 vaccination. In the other five cities, vaccination was arranged by employers and did not allow individuals to make an appointment. Starting from February 2020, the number of daily-confirmed cases continued to decline and the country recorded zero local new cases on March 18, 2020. The number of daily-confirmed local cases remained low (0–12) between March 19 and June 12, 2020. Between June and November 2020, several small-scale outbreaks happened in Beijing (363 cases from June 11 to July 7, 2020), Xinjiang (826 cases between July and September 2020, 78 cases between July and August 2020), Dalian (99 cases between July and August 2020), and Qingdao (14 cases in October 2020). Between November 2020 and February 2021, more than 14 provinces in China reported outbreak and recorded 2286 local cases. The situation of COVID-19 in China between February 2020 and February 2021 was shown in Figure 1.
Study participants were individuals aged 18–65 years who received confirmatory diagnosis with HIV and were living in one of the eight cities at the time of the survey. Individuals who were illiterate and unable to complete the questionnaire survey, unwilling to provide informed consent, or with known contraindications of COVID-19 vaccination (e.g., pregnant and/or lactating women, people with severe allergy to previous vaccination) were excluded. We excluded participants aged over 65 years, as COVID-19 vaccination was not approved for this age group at the time of the survey. The study participants of this study were different from our published study on willingness to receive COVID-19 vaccination (18). This study was conducted among all PLWH, while the published paper focused on a sub-sample of this study who had never received COVID-19 vaccination (18).
Details of the recruitment and data collection were described by a published study focusing on a subgroup of unvaccinated PLWH of the study participants (19). Eight community-based organizations (CBOs) providing services to PLWH, one in each city, facilitated the recruitment through their networks. These CBOs have been working closely with HIV clinical service providers. WeChat, a live chat application, is the most common communication tool for the CBOs to connect with PLWH clients. CBO staff posted the study information in the WeChat groups involving PLWH clients and invited eligible PLWH to participate. They also sent out reminders through the WeChat groups. The CBO staff and prospective participants were asked not to disseminate the study information to anyone outside the PLWH WeChat groups. Interested PLWH could contact the staff through private WeChat messages or telephone calls. CBO staff screened prospective participants using the eligibility criteria, introduced the study purpose and procedures, answered questions, and explained the confidentiality of study participation. Participation in this study was voluntary, and participants could refuse to answer any of the questions and withdraw from the study at any time without any consequences. Participants signed an electronic consent form sent via WeChat messages. A link to access an online self-administered questionnaire was sent to the consented participants.
The questionnaire was developed using Golden Data, a commonly used, encrypted web-based survey platform in China. Each individual WeChat account was allowed to access the online questionnaire only once to avoid duplicate responses. The Golden Data tool performed completeness check before the questionnaire was submitted. Participants could review and change their responses when they completed the questionnaire. The survey took about 13–15 min to complete. An electronic coupon with a value of 20 Chinese yuan (3.1 US dollar) was sent to the participant upon the completion of a survey. A unique ID was assigned to each participant, which was to delink the study database from personal identifying data. All data collected by the online survey were stored in the Golden Data server and protected by a password. Only the designated research team members had access to the database. Signed electronic consent forms were kept separately from the empirical data and stored in a password-protected computer or a locked cabinet in the same locked office. The Institutional Review Boards of Changzhi Medical College (RT2021003) approved this study.
Participants were asked to report socio-demographic characteristics, lifestyles (smoking and alcohol drinking), height and weight, presence of chronic conditions, history of other vaccination in the past 3 years, and characteristics related to HIV infection.
Participants reported whether they had taken up any COVID-19 vaccination. Self-reported uptake of COVID-19 vaccination was validated by requesting participants to send the research team an image of their receipt hiding personal identification through WeChat. Some supplementary information was collected from vaccinated participants, including number of doses and types of COVID-19 vaccines received, presence of side effects and severity of such side effects.
The research team interviewed CDC staff who are responsible for implementing COVID-19 vaccination program about the delivery model and whether there was a shortage in COVID-19 vaccines during the project period in different study sites. Participants were asked whether they belonged to any of the priority groups to receive COVID-19 vaccination listed by the National Health Commission during the project period.
At individual level, this study measured perceptions based on the Theory of Planned Behaviour (TPB), which postulates that in order to perform a behaviour, one would evaluate the pros and cons of the behaviour (positive and negative attitudes), consider whether their significant others would support such behaviour (perceived subjective norm), and appraise how much control one has over the behaviour (perceived behavioural control) (24). The TPB was commonly used to explain a health behaviour and guide the behavioural intervention (25, 26), it has been successfully used to explain the willingness to receive COVID-19 vaccination among Chinese people (27). Four scales were constructed based on the TPB for this study. They were: (1) the five-item Positive Attitude Scale, (2) the five-item Negative Attitude Scale, (3) the four-item Perceived Subjective Norm Scale, and (4) the five-item Perceived Behavioral Control Scale. These scales were formed by summing up individual item score (1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, & 5 = strongly agree).
For interpersonal-level variables, participants were asked whether they received advice given by clinical doctors, CBO staff, friends and family members, and other PLWH regarding COVID-19 vaccination. Participants were also asked the overall opinion regarding COVID-19 vaccination they found on the Internet or social media (responses categories: 1=against taking up COVID-19 vaccination, 2 = no advice/neutral, and 3 = supportive to take up COVID-19 vaccination).
The target sample size was 2500. We estimated that 10% of the participants received COVID-19 vaccination. Given a statistical power of 0.80 and an alpha value of 0.05 and assuming the uptake rate of COVID-19 vaccination in the reference group (without a facilitating condition) to be 2–8%, the sample size could detect the smallest odds ratios (OR) of 1.47 between people with and without such facilitating conditions (PASS 11.0, NCSS LLS).
Self-reported uptake of any COVID-19 vaccination was used as the dependent variable. Since the associated factors under different COVID-19 vaccination delivery models would be largely different, this study investigated factors associated with the dependent variable in two sub-samples. Total scores of the Positive Attitude Scale, the Negative Attitude Scale, the Perceived Subjective Norm Scale, and the Perceived Behavioral Control Scale were used as independent variables in data analysis. Univariate logistic regression models first assessed the significance of the association between each variable and the dependent variable. Variables with P < 0.05 in univariate analysis were entered in a multivariate logistic regression model. Crude odds ratios (OR), adjusted odds ratios (AOR) and their 95% confidence interval (CI) are obtained. SPSS version 26.0 (IBM Corp, Armonk, NY) was used for data analysis, with P<0.05 considered statistically significant.
Out of 10,845 PLWH being approached, 8,692 accessed the online survey, and 2740 completed the online survey. Over half of the participants were younger than 40 years (74.4%), were male at birth (94.5%), were currently single (67.8%), received tertiary education (62.9%), were employed full-time (70.5%), had a monthly income <5000 Chinese Yuan (US$ 770) (57.8%), and with basic health insurance only (75.2%). Among the participants, 27.5% were current smokers, 19.6% were current drinkers, 33.3% reported having at least one chronic condition, 6% were using chronic diseases medications, and 23.0% had a history of other vaccination in the past year. Based on self-reported data on height and weight, over one quarter of the participants were overweight (BMI: 24.0–27.9, 22.0%) or obesity (BMI≥28, 5.0%), while 9.0% were underweight (BMI<18.5). Regarding characteristics related to HIV infection, 17.1% of the participants received their diagnosis within – year, 97.4% were on ART, 68.7% reported undetectable HIV viral load, and 47.0% reported their CD4+ T-cell count level was above 500/μl (Table 1).
Among the participants, 6.2% (n = 170) self-reported had taken up at least one dose of COVID-19 vaccine (one dose: n = 74, 2.7%; both doses: n = 9 6, 3.5%). All these participants were able to provide the receipt for verification. The prevalence of COVID-19 vaccination uptake ranged from 1.4% in Shenyang to 17.3% in Beijing. Among vaccinated participants (n = 170), 62 (36.5%) received Sinopharm, 58 (34.1%) received Sinovac CoronaVac, and 40 (23.5%) of them were not sure about which vaccine they received. Side effects of COVID-19 vaccination were reported by 55.9% of the participants. Common side effects included pain at injection site (n = 65, 38.2%), fatigue, headache, dizziness or drowsiness (n = 28, 16.5%), muscle pain or joint pain (n = 15, 8.8%), and redness, swelling, itching, induration or rash at injection site (n = 7, 4.1%). Very few vaccinated participants perceived their side effects to be serious (n = 2, 1.2%) (Table 2).
According to CDC staff who were responsible for implementing COVID-19 vaccination program in different study sites, people in Beijing, Guangzhou and Shenzhen could make an appointment to receive COVID-19 vaccination during the project period, while COVID-19 vaccination in the other five cities was arranged by the employers and did not allow individuals to make an appointment. A shortage of COVID-19 vaccines was encountered in Shenyang, Guangzhou, and Shenzhen. Among the participants, 20% identified themselves as priority groups to receive COVID-19 vaccination. The Cronbach's alpha of the scales based on the TPB ranged from 0.83 to 0.92, single factors were identified by exploratory factor analysis, explaining for 61.1–76.4% of total variance (Table 3).
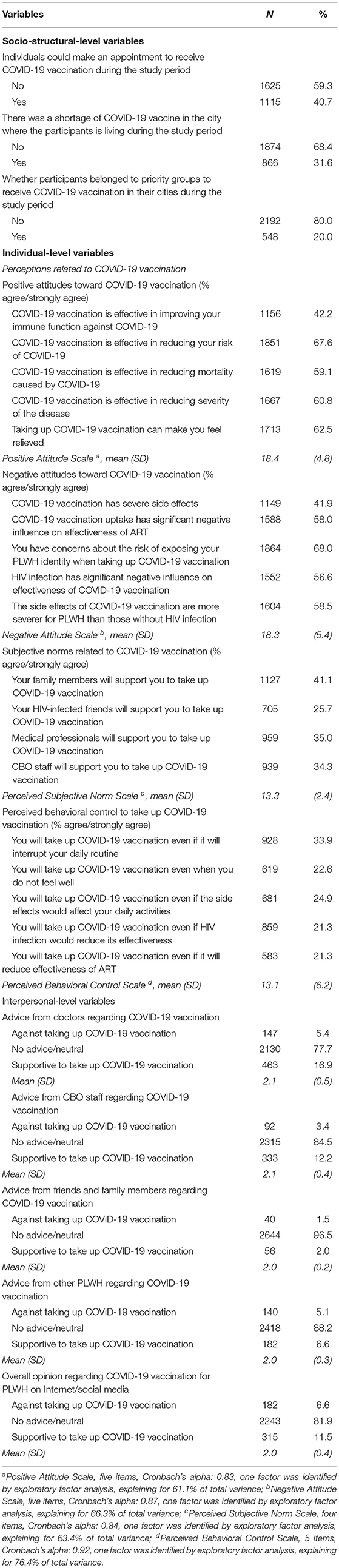
Table 3. Responses to survey items measuring socio-structural level, individual-level, and interpersonal-level variables (n = 2740).
Participants living in cities where individuals could make an appointment to receive COVID-19 vaccination reported significantly higher uptake than those living in cities without such allowance (11.0 vs. 2.9%, p < 0.001).
Among participants living in cities where individuals could make an appointment to receive COVID-19 vaccination (n = 1115), being a member of priority groups to receive vaccination (AOR: 1.88, 95%CI: 1.15, 3.09), receiving advice from CBO staff supporting COVID-19 vaccination (AOR: 2.06, 95%CI: 1.30, 3.26), and exposing to information on Internet/social media supporting PLWH to receive COVID-19 vaccination (AOR: 2.81, 95%CI: 1.74, 4.52) were associated with higher uptake. Shortage in COVID-19 vaccines (AOR: 0.21, 95%CI: 0.12, 0.38), and having negative attitudes toward COVID-19 vaccination (AOR: 0.85, 95%CI: 0.82, 0.89) were negatively associated with the uptake (Table 4).
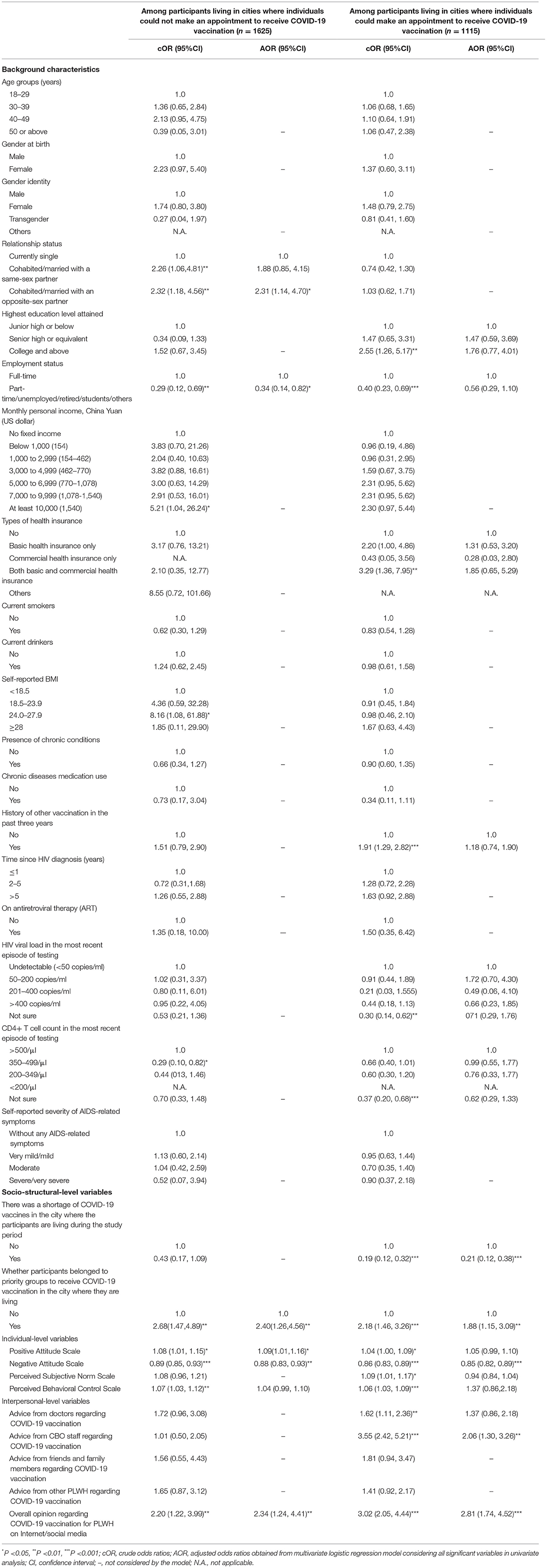
Table 4. Factors associated with COVID-19 vaccination uptake among participants living in cities/provinces where they can and cannot make an appointment to receive COVID-19 vaccines.
Among those living in cities where individuals could not make an appointment to receive COVID-19 vaccination (n = 1625), cohabited/married with an opposite-sex partner (AOR: 2.31, 95%CI: 1.14, 4.70), being a member of priority groups to receive vaccination (AOR: 2.40, 95%CI: 1.26, 4.56), having positive attitudes toward COVID-19 vaccination (AOR: 1.09, 95%CI: 1.01, 1.16), exposing to information on Internet/social media supporting PLWH to receive COVID-19 vaccination (AOR: 2.34, 95%CI: 1.24, 4.41) were associated with higher uptake. Without a full-time job (AOR: 0.34, 95%CI: 0.14, 0.82) and having negative attitudes toward COVID-19 vaccination (AOR: 0.88, 95%CI: 0.83, 0.93) were negatively associated with the dependent variable (Table 4).
To our knowledge, this is one of the first studies investigating COVID-19 vaccination uptake and its associated factors among PLWH in China. As compared to our published study looking at willingness to receive COVID-19 vaccination (18), this study has some different contributions. First, the findings represent the latest estimate of COVID-19 vaccination coverage in this group in the early phase of vaccine rollout, which provided a snapshot of the implementation of COVID-19 vaccination program among PLWH. Second, it addressed the research questions on whether the prevalence of actual uptake and factors associated with actual uptake were the same under different COVID-19 vaccination delivery models. Such information would inform policy makers' decision on which delivery model is more appropriate for PLWH, and provide knowledge basis to develop tailored strategies under each delivery model.
As compared to other countries, the COVID-19 pandemic was stable and under control in China between March 2020 and February 2021. It was possible that Chinese people perceived a lower risk of COVID-19. We found that the COVID-19 vaccination uptake was low (6.2%) and varied across cities (1.4–17.3%). Since there is no data on PLWH in other countries, we were not able to perform between-countries comparison. The COVID-19 vaccination coverage among PLWH was similar to that of the general population in the same cities during the same period. For example, 18% (3.63 million) and 3.6% (0.72 million) of the entire population in Beijing and Shenzhen received COVID-19 vaccination by February 2021, which was similar to our sampled PLWH in these two cities (17.3 and 3.2%) (28). There is a strong need to promote COVID-19 vaccination among both general population and specific sub-population at risk (e.g., PLWH).
Our first hypothesis was supported by the results, as COVID-19 vaccination uptake was much higher under the delivery model which allowed individuals to make an appointment to receive such vaccines. Such model might be easier for PLWH to transform motivation into actual behavior, as they do not have to wait for employer's arrangements. To our knowledge, more cities are switching their delivery model by allowing individuals to make appointments.
Our second hypothesis was partially supported by the results as some factors associated with actual uptake of COVID-19 vaccination was different under different vaccination delivery models. In cities where COVID-19 vaccination was mainly arranged by employers, more attention should be given to people without a full-time job as they could not benefit from such arrangement. Increasing positive attitudes toward COVID-19 vaccination may be an effective strategy to increase vaccination coverage among PLWH in these cities, as it was a facilitator. However, such strategy may not be applicable in cities where individuals could make an appointment to receive COVID-19 vaccination. It is possible that people would consider different factors when they proactively seek a service and when they decide to refuse an arrangement. Shortage in vaccine supply was a barrier of uptake in cities where individuals could make an appointment to receive COVID-19 vaccination, but not for the other delivery model. Allowing individuals to make appointments may result in a surge in the demand. Cities should ensure sufficient vaccine supply before they decide to switch to this delivery model. Shortage of vaccine might overwhelm any other barriers to take up COVID-19 vaccination. The findings also supported that CBO played an important role by motivating PLWH to receive COVID-19 vaccination when individuals could make an appointment to do so. Therefore, it is necessary for the government to empower more capable CBO workers to carry out publicity and education on the necessity and significance of PLWH in the future.
In addition, some similar strategies might be useful for promoting COVID-19 vaccination uptake under both delivery models. At socio-structural level, future intervention should give more attention to PLWH outside the priority groups as they reported lower COVID-19 vaccination uptake. In the initial phase of COVID-19 vaccination rollout and due to the insufficient supply, the government had to give COVID-19 vaccination to individuals at higher risk of COVID-19 first. To address the supply issue, China has rapidly increased its vaccine production capacity (29). It is necessary to shift the focus by emphasizing the importance of herd community targeting the entire population. About half of the participants had negative attitudes related to side effects, risk of exposing their PLWH identity, and potential interactions between COVID-19 vaccination and HIV infection/ART. It is necessary to remove these concerns, as they were barriers of COVID-19 vaccination uptake. Health communication messages should emphasize that ART and COVID-19 vaccination would not have negative impact on each other. Moreover, it is suggested that the health department should establish an online platform for the side effects and antiviral treatment effects of PLWH after receiving the COVID-19 vaccine to eliminate their concerns of COVID-19 vaccination with direct evidence and improve the coverage rate of the vaccine. Positive testimonials from vaccinated PLWH should be useful to remove their concerns related to side effects and privacy. Information about whether PLWH should receive COVID-19 vaccination are mixed on Internet/social media. Similar to the findings in the general population (27), exposure to information on the Internet or social media supporting PLWH to receive COVID-19 vaccination was a facilitator. Previous studies suggested that official web-based media operated by governmental organizations were considered as a credible source of information among Chinese people during the pandemic (30). Government should consider disseminating clear recommendation for PLWH to receive COVID-19 vaccination, and correct the misconception that PLWH could not benefit from such vaccination through these media outlets.
In this study, self-reported COVID-19 vaccination uptake was validated by the research team, which improved the reliability of the primary outcome. The study also has the strengths of covering multiple study sites in different geographic regions of China, a large sample size, and considering variables at all three levels suggested by the socio-ecological model. The findings extended the application of the socio-ecological model and provided empirical insights to inform COVID-19 vaccination promotion strategies. This study also had some limitations. First, this was a cross-sectional survey and could not establish causal relationships. Second, participants were recruited in large Chinese cities. As compared to representative samples of PLWH in China, higher proportion of our participants were male, younger, on ART, and with short duration since HIV diagnosis (31–33). Generalization should be made cautiously to PLWH in China. Third, we were not able to collect information from those who refused to complete the survey. Selection bias existed. Fourth, most items and scales used in this study were self-constructed based on those used in the general population. The reliability of these scales was acceptable. However, they were not used or validated in previous studies. Moreover, participants self-reported whether they belonged to a priority group to receive COVID-19 vaccination. Since we did not ask about participants' occupation and employers, we were not able to confirm whether such self-identification was correct. Furthermore, policies and situation related to COVID-19 vaccination had been changing rapidly; our findings were most applicable to the early phase of COVID-19 vaccination rollout in China. Currently, many low- and middle-income countries with high HIV disease burden were still in the early phase of COVID-19 vaccination rollout (34). Our findings have some reference values for these countries.
Our findings presented a snapshot of COVID-19 vaccination uptake among PLWH in the early phase of vaccine rollout in China. The socioecological model was useful to explain COVID-19 vaccination uptake among PLWH. The associated factors were not the same under different delivery models. This study provided a knowledge basis to formulate interventions promoting COVID-19 vaccination for PLWH. In order to promote COVID-19 vaccination uptake among PLWH, health authorities should provide clear recommendations of COVID-19 vaccination for PLWH, consider listing PLWH as a priority group to receive COVID-19 vaccination after obtaining sufficient evidence on immunogenicity and safety. Future programs should make use of the settings of hospitals and CBO, as PLWH need to visit these organizations for regular follow-ups. During the follow-up, staff of these organizations could address PLWH's concerns related to the interactions between COVID-19 vaccination and HIV.
The data presented in this study are available from the corresponding authors upon request. The data are not publicly available as they contain sensitive personal behaviors.
The study protocol was reviewed and approved by the Institutional Review Boards of Changzhi Medical College in Changzhi, China (RT2021003). Participants signed an electronic consent form to participate in the study.
ZW, JX, JY, and H-ZQ conceived and designed the research study. JY, MY, GF, GL, LL, YQ, JZ, XZ, XJ, and GC collected the data for the study. ZW and YF analyzed the data and interpreted the results. ZW wrote the first draft of the manuscript. JX, H-ZQ, JY, and XZ revised the manuscript. All authors contributed to the article and approved the submitted version.
This study was funded by the Academic technology leader project of Changzhi Medical College (Grant No. XSQ201902) and National Institute of Mental Health of the National Institutes of Health (Award Number R34MH119963). The funders had no role in study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We wish to acknowledge all the participants in this study.
1. Ministry of National Defense of the People's Republic of China. The Vaccine Administration Law of the People's Republic of China. (2019). Available online at: http://www.mod.gov.cn/big5/regulatory/2019-06/29/content_4844849.htm. [Accessed on December 2, 2020].
2. The State Council the People's Republic of China. Free COVID-19 Vaccination is Provided to All Residents. Available online at: http://www.gov.cn/fuwu/2021-01/09/content_5578430.htm. [Accessed May 14, 2021].
3. National Health Commission of the People's Republic of China. Situation of COVID-19 Vaccination in China. (2020). Available online at: http://www.nhc.gov.cn/jkj/s7915/202103/4e9f38edab0243e6ac433a181906e527.shtml. [Accessed on May 14, 2021].
4. Wang Y, Xie Y, Hu S, Ai W, Tao Y, Tang H, et al. Systematic Review and Meta-Analyses of The Interaction Between HIV Infection And COVID-19: Two Years' Evidence Summary. Front Immunol. (2022). Available online at: https://www.frontiersin.org/articles/10.3389/fimmu.2022.864838/abstract. [Accessed on April 22].
5. Huang X, Yan Y, Su B, Xiao D, Yu M, Jin X, et al. Comparing immune responses to inactivated vaccines against SARS-CoV-2 between people living with HIV and HIV-Negative individuals: a cross-sectional study in China. Viruses. (2022)14. doi: 10.3390/v14020277
6. World Health Organization. Coronavirus Disease (COVID-19): COVID-19 Vaccines and People Living With HIV. Retrieved from: https://www.who.int/news-room/q-a-detail/coronavirus-disease-(covid-19)-covid-19-vaccines-and-people-living-with-hiv. [Accessed August 19, 2021].
7. United States Department of Health Human Services. Guidance for COVID-19 and People with HIV. Retrieved from: https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/HIV_COVID_19_GL__2021.pdf. [Accessed on August 19, 2021].
8. British HIV. Association. SARS-CoV-2 Vaccine Advice for Adults Living With HIV: British HIV Association (BHIVA) & Terrence Higgins Trust (THT) Guidance. (2021). Retrieved from: https://wwwbhivaorg/SARS-CoV-2-vaccine-advice-for-adults-living-with-HIV-plain-english-version-update [Accessed on August 19].
9. ASHM COVID-19 Taskforce. Statement From the ASHM COVID-19 Taskforce Regarding the Prioritization of COVID-19 Vaccines for People Living With HIV. Retrieved from: https://www.ashm.org.au/covid-19/clinical-care/statement-regarding-the-prioritisation-of-covid-19-vaccines/. [Accessed on August 19, 2021].
10. National Health Commission of the People's Republic of China. Technical Guideline on COVID-19 Vaccination. 1st Ed (2021). Available online at: http://www.nhc.gov.cn/xcs/yqfkdt/202103/c2febfd04fc5498f916b1be080905771.shtml. (Accessed March 30, 2021).
11. Centers for Disease Control Prevention (CDC). COVID-19 ACIP Vaccine Recommendations. (2021). Available online at: https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/covid-19.html. [Accessed on September 24, 2021].
12. World Health Organization. Ten Threats to Global Health in 2019. Available online at: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019. (2019) [Accessed on September 20, 2021].
13. Sallam M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines. (2021) 9:160. doi: 10.3390/vaccines9020160
14. Sallam M, Al-Sanafi M, Sallam M, A global map of COVID-19 vaccine acceptance rates per country: an updated concise narrative review. J Multidiscip Healthc. (2022) 15:21–45. doi: 10.2147/JMDH.S347669
15. Diesel J, Sterrett N, Dasgupta S, Kriss JL, Barry V, Vanden Esschert K, et al. COVID-19 vaccination coverage among adults - United States, December 14, 2020-May 22, 2021. Morb Mortal Wkly Rep. (2021) 70:922–7. doi: 10.15585/mmwr.mm7025e1
16. Group C, A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. Lancet Infect Dis. (2020) 20:769–70. doi: 10.1016/S1473-3099(20)30426-6
17. Vallée A, Fourn E, Majerholc C, Touche P, Zucman D. COVID-19 vaccine hesitancy among French people living with HIV. Vaccines. (2021)9:302 doi: 10.3390/vaccines9040302
18. Bogart LM, Ojikutu BO, Tyagi K, Klein DJ, Mutchler MG, Dong L, et al. COVID-19 Related Medical Mistrust, Health Impacts, and Potential Vaccine Hesitancy Among Black Americans Living With HIV. J Acquir Immune Defic Syndr. (2021) 86:200–7. doi: 10.1097/QAI.0000000000002570
19. Huang X, Yu M, Fu G, Lan G, Li L, Yang J, et al. Willingness to receive COVID-19 vaccination among people living with HIV and AIDS in China: Nationwide Cross-sectional Online Survey. JMIR Public Health Surveill. (2021) 7:e31125. doi: 10.2196/31125
20. Robinson E, Jones A, Lesser I, Daly M. International estimates of intended uptake and refusal of COVID-19 vaccines: a rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. (2021) 39:2024–34. doi: 10.1016/j.vaccine.2021.02.005
21. Michie S, Johnston M, Francis J, Hardeman W, Eccle M. From theory to intervention: mapping theoretically derived behaviorual determinants to behaviour change techniques. Appl Psycho. (2008) 57:660–80. doi: 10.1111/j.1464-0597.2008.00341.x
22. McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. (1988) 15:351–77. doi: 10.1177/109019818801500401
23. Pan Y, Fang Y, Xin M, Dong W, Zhou L, Hou Q, et al. Self-reported compliance with personal preventive measures among chinese factory workers at the beginning of work resumption following the COVID-19 outbreak: cross-sectional survey study. J Med Int Res. (2020) 22:e22457. doi: 10.2196/22457
24. Ajzen I. The Theory of Planned Behaivor. Organ Behav Hum Decis. (1991) 50:179–211. doi: 10.1016/0749-5978(91)90020-T
25. Kinmonth AL, Wareham NJ, Hardeman W, Sutton S, Prevost AT, Fanshawe T, et al. Efficacy of a theory-based behavioural intervention to increase physical activity in an at-risk group in primary care (ProActive UK): a randomised trial. Lancet. (2008) 371:41–8. doi: 10.1016/S0140-6736(08)60070-7
26. Webb TL, Sniehotta FF, Michie S. Using theories of behaviour change to inform interventions for addictive behaviours. Addiction. (2010) 105:1879–92. doi: 10.1111/j.1360-0443.2010.03028.x
27. Zhang KC, Fang Y, Cao H, Chen H, Hu T, Chen Y, et al. Behavioral intention to receive a COVID-19 vaccination among Chinese factory workers: cross-sectional online survey. J Med Int Res. (2021) 23:e24673. doi: 10.2196/24673
28. ChinaNews. Over 3.62 Million in Beijing had Received COVID-19 Vaccination. (2021). Available online at: http://www.chinanews.com/gn/2021/02-22/9416694.shtml. [Accessed on June 3, 2021].
29. Chinanews. Official: China increases vaccine production capacity. Available at: https://www.chinanews.com/gn/2021/03-15/9432820.shtml. [Accessed on May 18, 2021].
30. Pan Y, Xin M, Zhang C, Dong W, Fang Y, Wu W, et al. Associations of mental health and personal preventive measure compliance with exposure to COVID-19 information during work resumption following the COVID-19 outbreak in China: cross-sectional survey study. J Med Int Res. (2020) 22:e22596. doi: 10.2196/22596
31. Zhao Y, Han MJ, Ma Y, Li D. Progress towards the 90-90-90 targets for controlling HIV – China, 2018. China CDC Weekly. (2019) 1:5–7. doi: 10.46234/ccdcw2019.003
32. Xu JJ, Han MJ, Jiang YJ, Ding HB Li X, Han XX, et al. Prevention and control of HIV/AIDS in China: lessons from the past three decades. Chin Med J. (2021) 134:2799–809. doi: 10.1097/CM9.0000000000001842
33. Chen WT, Shiu C, Yang JP, Tun MMM, Zhang L, Wang K, et al. Tobacco use and HIV symptom severity in Chinese people living with HIV. AIDS care. (2020) 32:217–22. doi: 10.1080/09540121.2019.1620169
34. Africa. WHOROf. Key Lessons From Africa's COVID-19 Vaccine Rollout. (2022). Available online at: https://www.afro.who.int/news/key-lessons-africas-covid-19-vaccine-rollout. [Accessed on April 19, 2022].
Keywords: people living with HIV, COVID-19 vaccination uptake, associated factors, socioecological model, China
Citation: Yang J, Yu M, Fu G, Lan G, Li L, Qiao Y, Zhao J, Qian H-Z, Zhang X, Liu X, Jin X, Chen G, Fang Y, Wang Z and Xu J (2022) COVID-19 Vaccination Uptake Among a Nationwide Sample of People Living With HIV During the Early Phase of Vaccine Rollout in China. Front. Med. 9:822680. doi: 10.3389/fmed.2022.822680
Received: 26 November 2021; Accepted: 06 May 2022;
Published: 13 June 2022.
Edited by:
Kiat Ruxrungtham, Chulalognkorn University, ThailandReviewed by:
Oana Sandulescu, Carol Davila University of Medicine and Pharmacy, RomaniaCopyright © 2022 Yang, Yu, Fu, Lan, Li, Qiao, Zhao, Qian, Zhang, Liu, Jin, Chen, Fang, Wang and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zixin Wang, d2FuZ3p4QGN1aGsuZWR1Lmhr; Junjie Xu, amp4dWVAY3ptYy5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
‡These authors have contributed equally to this work and share last authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.